Abstract
Angiogenesis is an early and a critical event in the pathogenesis of Rheumatoid arthritis (RA). Neovascularization is dependent on endothelial cell activation, migration and proliferation, and inhibition of angiogenesis may provide a novel therapeutic approach in RA. In this study, we document a novel role of IL-17 in mediating angiogenesis. Local expression of IL-17 in mouse ankles increases vascularity. We further demonstrate that IL-17 is angiogenic, by showing its ability to promote blood vessel growth in matrigel plugs in vivo. Additionally, IL-17, in concentrations present in the RA joint, induces human microvascular endothelial cell (HMVEC) migration mediated through the PI3K/AKT1 pathway. Further, suppression of the PI3K pathway markedly reduces IL-17-induced tube formation. We also show that both IL-17-induced HMVEC chemotaxis and tube formation are mediated primarily through IL-17 receptor (R) C. Neutralization of either IL-17 in RA synovial fluids or IL-17RC on HMVECs significantly reduces the induction of HMVEC migration by RA synovial fluid. Finally, RA synovial fluid immunoneutralized with IL-17 and VEGF does not reduce HMVEC migration beyond the effect detected with each factor alone. These observations identify a novel function for IL-17 as an angiogenic mediator in RA, supporting IL-17 as a therapeutic target in RA.
Keywords: IL-17, angiogenesis, HMVECs, migration, rheumatoid arthritis
INTRODUCTION
T-helper 17 (TH-17) cells are a newly discovered CD4(+) helper T-cell subset that produce interleukin-17A (also known as IL-17). IL-17 binds to transmembrane receptors, which exist as IL-17 receptor A (IL-17RA) homodimers or IL-17RA/RC heterodimers (1). IL-17 RA and RC are widely expressed in endothelial cells, B and T cells, fibroblasts and monocytes (2, 3). TGF-β, IL-6, IL-1β and IL-21 have been shown to drive the differentiation of TH-17 cells (4–6), although variation between humans and mice has been described (2, 6–8). In humans, IL-1β is the most effective inducer of TH-17 cell differentiation, although this process is enhanced by IL-6 and IL-23 (6).
IL-17 has been shown to have a profound effect in experimental models of arthritis. Local expression of IL-17 in mouse joints results in acute inflammation and cartilage proteoglycan depletion (9). The incidence and severity of collagen-induced arthritis (CIA) was markedly attenuated in IL-17-deficient mice (10). IL-17 also plays an important role downstream of IL-1 signaling and in response to TLR4 ligands (11, 12). Spontaneous IL-1 receptor antagonist (Ra) knockout mice develop a polyarthritis, which is completely suppressed when these mice are crossed with IL-17-deficient mice (13), suggesting that TH-17 cell differentiation may be the reason for the arthritis.
IL-17 is found in RA synovial tissue and fluid, and the percentage of TH-17 cells is significantly higher in RA synovial fluid compared to RA or normal peripheral blood (3, 14). IL-17 may play an important role in the pathogenesis of RA by inducing the production of proinflammatory cytokines and chemokines from RA synovial tissue fibroblasts including IL-6, CXCL8/IL-8, CCL2/MIP-3α, CXCL1/GRO-α and CXCL2/GRO-β (15–17). IL-17 is also capable of activating macrophages to expression of IL-1, TNF-α, cyclooxygenase (COX)2, prostaglandin (PG)E2 and matrix metalloproteinase (MMP)-9 (18–20). We recently demonstrated that IL-17 is directly chemotactic for monocytes(21), and others have shown that IL-17 activates neutrophil recruitment through the stimulation of chemokines such as CXCL1 in rats and CXCL8/IL-8 in humans (22, 23).
Angiogenesis, the development of new capillaries, is involved in leukocyte ingress into the synovium during the development and progression of RA(24, 25). However, the role of IL-17 in angiogenesis is undefined. There are contradictory results regarding the role of IL-17 on tumor development and angiogenesis. In mice, tumors transfected with IL-17 demonstrated markedly less growth compared to control tumors (26). Additionally, tumor growth and lung metastasis were increased in IL-17-deficient mice (27), suggesting that IL-17 inhibits tumor development and neovascularization. Others have shown that IL-17 increases blood vessel development in rat cornea and tumor vascularity in animal models, indicating that IL-17 may be important for angiogenesis (28). However, there are also data to suggest that IL-17 alone is unable to induce angiogenesis, but can indirectly mediate human microvascular endothelial cell (HMVEC) growth by promoting the mitogenic activity of vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF) and hepatocyte growth factor (HGF) (29, 30). Therefore, based on the existing data it is unclear whether IL-17 can promote angiogenesis in RA and whether IL-17 acts directly on endothelial cells through binding to its receptors, or indirectly by inducing proangiogenic factors from cells present in the RA synovium.
In the current study, we have therefore evaluated the role of IL-17 in HMVEC migration and tube formation as well as blood vessel development. Our results demonstrate that local expression of IL-17 increases vascularity in mouse ankle joints. Employing a matrigel plug assay, we demonstrate that IL-17 enhances blood vessel formation in vivo. Although HMVECs express both IL-17RA and RC, IL-17-induced HMVEC chemotaxis and tube formation are mediated by binding primarily to IL-17RC and activation of the PI3K pathway. We report that RA synovial fluid-mediated endothelial migration is significantly reduced by IL-17 and/or IL-17RC neutralization. Finally, we show that IL-17 and VEGF neutralization in RA synovial fluid does not significantly reduce HMVEC migration beyond the effect of one factor alone. Hence, therapy directed against IL-17 may reduce leukocyte migration by inhibiting angiogenesis in RA.
MATERIALS AND METHODS
Study protocol for local expression of IL-17 in mouse ankle joints
The animal studies were approved by the Northwestern University Institutional Review Board. Adenovirus (Ad) constructed as reported previously to contain an IL-17 payload was provided by J. K. Kolls (31). 4–6 week old C57BL/6 mice were injected intra-articularly with 107 PFU Ad-IL-17 or Ad-CMV control. Ankle circumference and articular index score were determined on days 4 and 10 post-Ad-IL-17 injection and compared to the control group (data not shown). Ankles were harvested on day 10 post-Ad-IL-17 injection for histological studies. Levels of IL-17 were quantified by ELISA on days 4 and 10 from ankles treated with Ad-IL-17 or Ad-CMV control.
Antibodies and immunohistochemistry
Mouse ankles were decalcified, formalin fixed and paraffin embedded, and sectioned in the pathology core facility of Northwestern University. Mouse ankles were immunoperoxidase-stained using Vector Elite ABC Kits (Vector Laboratories), with diaminobenzidine (Vector Laboratories) as a chromogen. Slides were deparaffinized in xylene for 20 min at room temperature, followed by rehydration by transfer through graded alcohols. Antigens were unmasked by first incubating slides in boiling citrate buffer for 15 min, followed by type II trypsin digestion for 30 min at 37°C. Endogenous peroxidase activity was blocked by incubation with 3% H2O2 for 5 min. Nonspecific binding of avidin and biotin was blocked using an avidin/biotin blocking kit (Vector Laboratories). Nonspecific binding of antibodies to the tissues was blocked by pretreatment of tissues with diluted normal goat serum. Tissues were incubated with rabbit polyclonal antibody to Von Willebrand factor (1/100 dilution; Serotec), or a rabbit IgG control antibody (Beckman Coulter). Slides were counterstained with Harris hematoxylin and treated with lithium carbonate for bluing. Each slide was evaluated by a blinded observer (32–35) (M.V.V). Tissue sections were assigned a vascular score representing the number of blood vessels in each section. A semi-quantitative score of 1 represented a tissue with few blood vessels, whereas a score of 4 represented a highly vascularized tissue. Scoreddata were pooled, and the mean ± SEM was calculated ineach data group, (n=5).
Matrigel plug assay in vivo
To examine the effect of IL-17 on angiogenesis in vivo, we used a matrigel plug assay. 4 to 6 week old C57BL/6 mice were injected subcutaneously in the dorsal area with 500 μl matrigel. Matrigel plus PBS served as negative control, matrigel containing bFGF (20 ng/ml) served as positive control, and experimental conditions included matrigel with mouse recombinant IL-17 (2 μg). After 10 days, mice were sacrificed, matrigel plugs were carefully dissected out, surrounding connective tissue was removed, and plugs were analyzed for vascularity by hemoglobin measurement or by histology. For hemoglobin measurement, plugs were weighed by placing them into 1 ml pre-weighed ddH20 and then homogenized for 5–10 min on ice and spun. Employing methemoglobin, serial dilutions were prepared to generate a standard curve from 70 to 1.1 g/dl (36, 37). Fifty microliters of supernatant or standard were added to a 96-wellplate in duplicate and 50 μl tetramethylbenzidine was added to each sample. The plate was allowed to develop at room temperature for 15–20 min with gentle shaking, and the reaction was terminated with 150 μl 2 N H2SO4 for 3–5 min. Absorbance was read with an ELISA plate reader at 450 nm. To calculatehemoglobin concentrations, the values (g/dl) were normalized to the weights of the plugs (g) (36, 37). On day 10, IL-17 concentrations were quantified in matrigel plugs harvested from the IL-17 treated group employing ELISA.
For histology, plugs were embedded in paraffin and sectioned in the pathology core facility of Northwestern University. Histology slides from different groups were examined by H&E and Masson’s trichrome staining (37, 38) and scored by a blinded observer (A.M.M.) based on a scale of 0–4 where 0 = no tubules, 1 = tubules only, 2 = tubules containing red blood cells, 3 = tubules with multilayer wall and 4 = tubules with multilayer walls with connective tissues surrounding them.
HMVEC chemotaxis
To examine chemotaxis, HMVECs were incubated in endothelial basal medium (EBM) with 0% FBS and no growth factors for 2h before use. HMVECs (1.25 × 104 cells/25 μl EBM with 0.1% FBS) were then placed in the bottom wells of a 48-well Boyden chemotaxis chamber (NeuroProbe, Cabin John, MD) with gelatin-coated polycarbonate membranes (8 μm pore size; Nucleopore, Pleasant, CA) (37, 39). The chambers were inverted and incubated at 37°C for 2h, allowing endothelial cell attachment to the membrane. The chamber was reinverted, and PBS, positive control VEGF (10ng/ml; R&D Systems), or IL-17 at varying concentrations from 0.001 to 100ng/ml (R&D Systems) was added to the upper wells, and the chamber was further incubated for 2h at 37°C. The membranes were then removed, fixed and stained with the Protocol HEMA 3 stain set (Fisher Scientific 122–911). Readings represent the number of cells migratingthrough the membrane (the average of three high power ×40 fields/well, averaged for each triplicate of wells). To test specificity of IL-17-induced HMVEC migration, HMVEC chemotaxis was examined with heat-inactivated IL-17 (10 and 50ng/ml incubated at 100°C for 15min) or IL-17 neutralized by anti-IL-17 antibody or IgG control (10μg/ml for 1hr in 37°C) (R&D Systems) (21). To examine for chemokinesis, a series of checkerboard experiments were performed by placing increasing concentrations of IL-17 (0, 0.01, 1 and 10ng/ml) together with HMVECs in the bottom wells with different concentrations of IL-17 in the top wells. To determine which IL-17 receptors are important for IL-17 HMVEC migration, antibodies to IL-17RA (R&D MAB177; 10μg/ml), IL-17RC (R&D AF2269; 10μg/ml), both antibodies, or IgG control were added to HMVECs, incubated for 1h at 37°C, and further incubated for 2h in the Boyden chamber with IL-17 (50ng/ml). To define which signaling pathway(s) mediated IL-17-induced HMVEC chemotaxis, HMVECs were incubated with inhibitors to PI3K (LY294002; 1 and 5 μM), ERK (PD98059; 1 and 5 μM), JNK (SP600125; 1 and 5 μM) or DMSO for 2h in the Boyden chamber with IL-17 (50ng/ml). HMVEC chemotaxis induced by RA synovial fluids was examined following 1hr incubation (37°C) of fluids with control IgG or neutralizing anti-IL-17 antibody (10μg/ml). The fluids were diluted 1:20 before addition to the top wells (21). To examine whether IL-17 receptors are involved in RA synovial fluid-induced HMVEC chemotaxis, HMVECs were incubated with antibodies to IL-17RA and RC (10 μg/ml) or both antibodies, as well as IgG control (1hr at 37°C) before adding the RA synovial fluid to the top wells (21). HMVEC chemotaxis was performed in order to examine the synergistic effect of IL-17 and/or VEGF in RA synovial fluid induced HMVEC migration. Chemotaxis induced by RA synovial fluids was examined following incubation of fluids (diluted 1:20) (n=8 fluids) with control IgG, anti-IL-17, anti VEGF or both antibodies (10μg/ml) for 1h prior to performing the assay.
Quantification of IL-17RA and RC expression on HMVECs
Skin and lung HMVECs, human umbilical vein endothelial cells (HUVEC) and human embryonic kidney (HEK) 293 were cultured in EGM-2, EGM and 10% DMEM, respectively. Total cellular RNA was extracted using Trizol (Invitrogen, Carlsbad, CA) from all different cell types. Subsequently, reverse transcription and real-time RT-PCR were performed to determine IL-17RA and IL-17RC expression level as previously described (14, 21, 40). Relative gene expression was determined by the ΔΔCt method, and results were expressed as fold increase above levels detected in HEK 293 cells.
Characterization of IL-17 signaling pathways in HMVECs
HMVECs (passage 3–8) were grown to 80% confluence in EGM-2 MV bullet kit (Lonza). Cells were then switched to EGM-MV (EBM plus SingleQuots of growth supplements) for 2 days and were incubated in EBM with 0% FBS for 2hr prior to treatment. Cells were then untreated or treated with IL-17 (50ng/ml) for 15 to 75min. Cell lysates were examined by Western blot analysis, as previously described(21, 40, 41). Blots were probed with phospho (p)-AKT, pERK and pJNK (Cell Signaling; 1:1000 dilution) overnight and after stripping, were probed with AKT, ERK and JNK (Cell Signaling; 1:3000 dilution) overnight.
HMVEC tube formation assay
To perform the matrigel tube formation assay, BD Matrigel Matrix (BD BioCoat tube formation kit, 50 μl) was polymerized for 30 min at 37°C in a 96-well plate. To determine which IL-17 receptors play a role in IL-17-induced HMVEC tube formation, trypsinized HMVECs were resuspended (4×105 cells/ml) in EBM without growth factors with 2% FBS and incubated with antibodies to IL-17RA, IL-17RC, both IL-17RA and RC or IgG for 45 minutes at 37°C. Cells were then added to polymerized matrigel, IL-17 (50ng/ml) was added to the wells, and the plate was incubated for 16h at 37°C. To examine which signaling pathways contribute to IL-17-mediated HMVEC tube formation, cells were incubated with inhibitors to PI3K (LY294002; 1 and 5 μM), ERK (PD98059; 1 and 5 μM), JNK (SP600125; 1 and 5 μM) or DMSO for 45 minutes at 37°C prior to adding to polymerized matrigel. As above, IL-17 (50ng/ml) was then added to the wells and the plate was incubated for 16h at 37°C. Each condition was performed in triplicate, FGF (20 ng/ml) was used as a positive control, and PBS was used as a negative control. Following incubation, culture media was removed and cells were washed with Hanks’ Balanced Salt Solution (HBSS). Thereafter, tube formation was quantified using calcein AM fluorescent dye (BD BioCoat kit) diluted with HBSS and DMSO according to the manufacturer’s instructions, for 30 min. Subsequently, the plates were washed with HBSS, and the number of branch points/tubes was quantified as previously described (36, 37).
Statistical Analysis
The data was analyzed using 2-tailed Student’s t tests for paired and unpaired samples. P values < 0.05 were considered significant.
RESULTS
Local expression of IL-17 in mouse ankles induces joint inflammation and vascularity
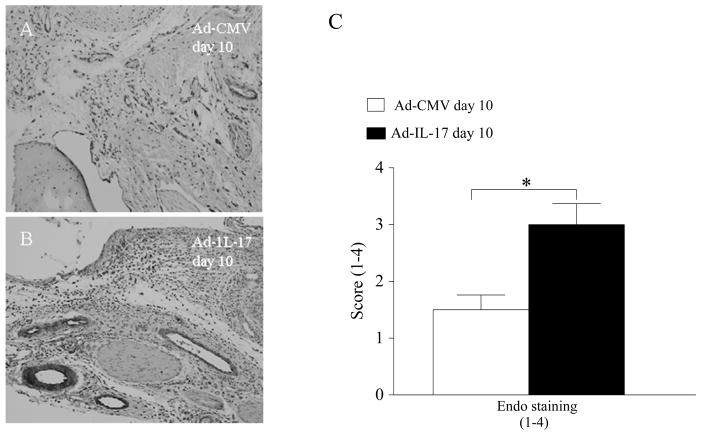
Local expression of IL-17 using an adenoviral vector (107 PFU) resulted in increased inflammation, synovial lining thickness, and bone erosion in the ankles of C57/BL6 mice, compared to Ad-CMV-infected controls (107 PFU) (data not shown). The Ad-IL-17-treated group demonstrated significantly greater ankle circumference (data not shown) on days 4 and 10 post-injection compared to the control group. Von Willebrand factor staining of ankles harvested from day 10 post-injection demonstrated that Ad-IL-17-treated mice have significantly higher endothelial staining compared with the control group (Figure 1). The concentration of joint IL-17 in the IL-17-induced arthritis model was 1200 pg/mg and 400 pg/mg compared to 47 pg/mg and 31 pg/mg detected in the Ad-CMV control group on days 4 and 10 post-Ad injection. These results suggest that IL-17 may be important for angiogenesis in vivo.
Figure 1. Local expression of IL-17 increases vascularity in mouse ankles.
Ad-IL-17 or Ad-CMV control was injected intra-articularly into the ankle joints of 4–6 week old C57BL/6 mice. Ankles from day 10 post-Ad injection were harvested, paraffin embedded and decalcified. Ankles were stained with Von Willebrand factor for identifying endothelial cells (Endo) and scored on a 1–4 scale. Control ankles (A) had significantly lower endothelial staining compared to ankles locally expressing IL-17 (B) (original magnification × 200). C. Quantification of each of the parameters in the Ad-CMV control and Ad-IL-17 groups. Values demonstrate mean ± SE, n=5. * denotes p<0.05.
IL-17 induces angiogenesis in vivo in matrigel plugs
The role of IL-17 on angiogenesis in vivo was assessed by determining its effect on blood vessel formation in matrigel plugs in mice by employing hemoglobin quantification, as well as Masson’s trichrome staining. The hemoglobin content of the IL-17 treated group was 10 times greater (p<0.05) than the PBS control (Figure 2A). Matrigel blood vessel formation was also examined histologically by employing H&E (Figure 2C, 2E and 2G) and Masson’s trichrome staining (Figure 2D, 2F and 2H). The histological analysis demonstrated that IL-17 markedly enhances (p<0.05) blood vessel growth compared to the control group (Figure 2B). The levels of IL-17 detected in matrigel plugs harvested on day 10 were 198±35 pg/ml which is within the range detected in IL-17-induced arthritis model as well as in the RA synovial fluid (mean was 233 pg/ml). These results support the role of IL-17 in angiogenesis in vivo.
Figure 2. IL-17 enhances blood vessel growth in matrigel plugs in vivo. A.
IL-17 (2 μg) induced angiogenesis in the matrigel plugs to a significantly greater degree compared to PBS control. Matrigel containing bFGF (20 ng/ml) served as positive control. The values represent the concentration of hemoglobin (g/dl)/plug weight (g) ± SE, with n=10. B. The histology was quantified on a score of 0-4 scale in matrigel plugs that contained PBS, IL-17 or VEGF employing H&E and Masson’s trichrome staining. A representative assay shows H&E (C, E and G) and Masson’s trichrome (D, F and H) staining of blood vessels in paraffin sections of matrigel plugs containing PBS (C and D), IL-17 (E and F) and FGF (G and H) that was histologically scored in B (original magnification × 200). Values demonstrate mean ± SE, with n=5. * represents p<0.05.
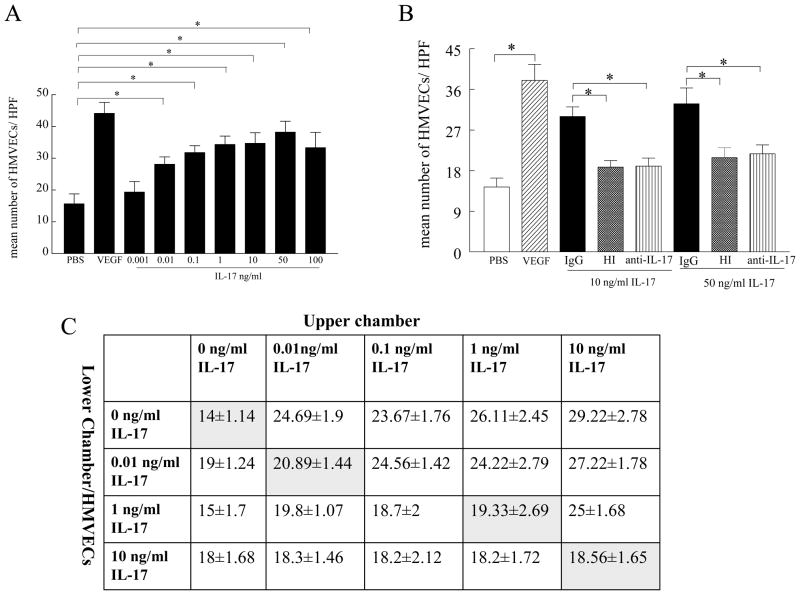
IL-17 induces endothelial (HMVEC) migration
Experiments were performed to determine whether IL-17 is directly chemotactic for endothelial cells. For this purpose, chemotaxis was performed in a Boyden chamber with varying concentrations of IL-17, as well as positive (VEGF, 10ng/ml) and negative (PBS) controls. IL-17 was chemotactic for HMVECs at concentrations ranging from 0.01 ng/ml (p<0.05) to 100 ng/ml (p<0.05) (n=5) (Figure 3A). The mean concentration of IL-17 in the 30 RA SF analyzed was 233 ± 64 pg/ml (21), a concentration that was highly chemotactic for HMVEC migration. IL-17’s endotoxin levels were quantified by employing Limulus amebocyte cell lysate assay. At a concentration of IL-17 10-fold higher than that used in the HMVEC chemotaxis assay (500 ng/ml), the level of endotoxin was below the detection limit for this assay (<0.01 ng/ml LPS) (data not shown), suggesting that our results are specifically due to IL-17 and not endotoxin contamination. Supporting this interpretation, heat inactivation of IL-17 or incubation of IL-17 (50 ng/ml) with neutralizing antibody to IL-17 suppressed HMVEC migration (Figure 3B).
Figure 3. IL-17 induces HMVEC migration and not chemokinesis.
A. Dose response curve of IL-17-induced HMVEC chemotaxis. IL-17 HMVEC chemotaxis was performed in a Boyden chemotaxis chamber with varying concentrations of IL-17. Values demonstrate mean ± SE from five different experiments. B. IL-17-induced HMVEC chemotaxis was suppressed by heat inactivating IL-17 (both 10 and 50 ng/ml incubated in 100°C for 15min) or neutralization of IL-17 (10 and 50 ng/ml) by anti-IL-17 antibody but not by IgG control (10 μg/ml 1h in 37°C) for 2h. Values are the mean ± SE from three different experiments. * represents p <0.05. C. A series of checkerboard experiments was performed by placing increasing doses of IL-17 together with HMVECs in the lower well in addition to placing different concentrations of IL-17 in the top well of the chemotaxis chamber. The experiment was read at 2h. Results are representative of three different experiments.
We next determined the effect of IL-17 on chemokinesis. In the absence of IL-17 in the lower chamber, IL-17 in the upper chamber was chemotactic for HMVECs. When equivalent or higher concentrations of IL-17 were present in the lower compartment, no enhanced migration of HMVECs occurred (Figure 3C). Taken together, our results suggest that IL-17 is chemotactic, not chemokinetic, for endothelial cells.
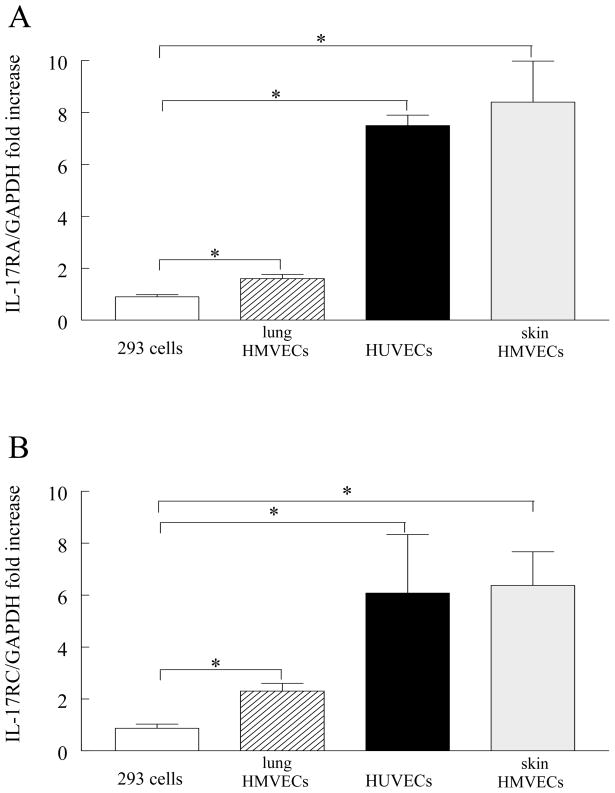
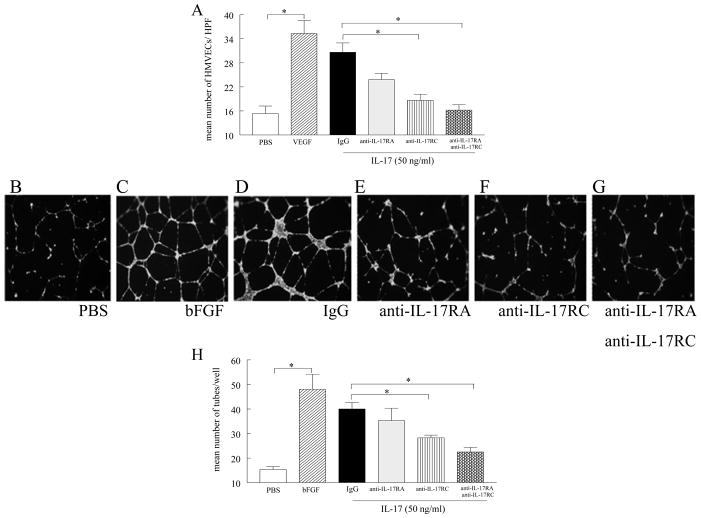
IL-17 receptors are involved in IL-17-induced HMVEC chemotaxis and HMVEC tube formation
Our results demonstrate that skin and lung HMVECs as well as HUVECs express significantly higher levels of IL-17RA and IL-17RC compared to HEK 293 cells (Figure 4A and B). These experiments were performed to determine which IL-17 receptor is involved in HMVEC chemotaxis and tube formation. Although some reduction of HMVEC chemotaxis was noted with an anti-IL-17RA antibody, it was not significant. Inhibition of chemotaxis was significant when IL-17RC (40%) or both receptors (47%) were neutralized (Figure 5A). IL-17 also induced HMVEC tube formation in matrigel. Employing concentrations of IL-17 ranging from 0.001 ng/ml to 100 ng/ml, the optimal concentration of IL-17 to induce HMVEC tube formation was 50 ng/ml (p<0.05) (data not shown). Consistent with the HMVEC chemotaxis data, neutralization of IL-17RC (30%) or both IL-17 receptors (45%) on HMVECs significantly decreased (p<0.05) IL-17-mediated HMVEC tube formation (Figure 5B–H). Blockade of IL-17RA alone was inefficient in this process. Collectively, our data suggest that IL-17RC plays a more important role in IL-17-mediated HMVEC chemotaxis and tube formation compared to IL-17RA.
Figure 4. HMVECs express IL-17RA and RC.
Skin and lung HMVECs, HUVEC and HEK 293 were cultured and real-time RT-PCR were performed to determine IL-17RA and IL-17RC expression level. The relative gene expression levels were normalized by GAPDH and determined by the ΔΔCt method, and results were expressed as fold increase above levels detected in HEK 293 cells. Values are the mean ± SE, n=3–6. * represents p <0.05.
Figure 5. IL-17-mediated HMVEC chemotaxis and tube formation are regulated through both IL-17RA and IL-17RC.
A. HMVECs were incubated with mouse anti-human IL-17RA and IL-17 RC antibodies (10μg/ml) or control IgG (10μg/ml) for 1h. Thereafter HMVEC chemotaxis was performed in response to IL-17 (50 ng/ml) for 2h. PBS was used as a negative control, and VEGF (60 nM) as a positive control. HMVECs were incubated with antibodies to IL-17RA, IL-17RC, both IL-17RA and RC or IgG for 45 minutes at 37°C. Cells were then added to polymerized matrigel, IL-17 (50ng/ml), placed in the wells, and the plate was incubated for 16h at 37°C (in triplicate). Photomicrographs taken of representative wells treated with PBS (B), FGF (20 ng/ml) (C), IL-17 (50 ng/ml) plus IgG (D), IL-17 (50 ng/ml) plus anti-IL-17RA (10μg/ml) (E), IL-17 (50ng/ml) plus anti-IL-17RC (10μg/ml) (F) and IL-17 (50ng/ml) plus anti-IL-17RA and RC (10μg/ml) (G) in which IL-17-induced tube formation is significantly reduced by the neutralization of IL-17RC or both receptors (p<0.05). H. Data presented demonstrates mean number of branch points/tubes in each treatment group. Values are the mean ± SE, n=3. * represents p <0.05.
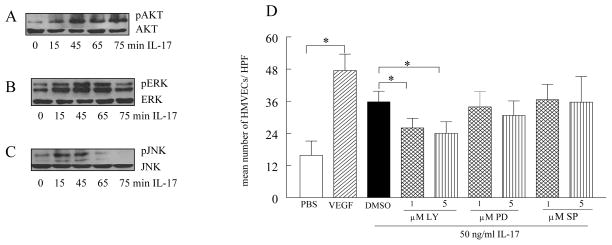
IL-17 activates ERK, JNK and PI3K pathways in HMVECs, however only inhibition of PI3K reduces IL-17-induced HMVEC chemotaxis and tube formation
To determine which signaling pathways in HMVECs are activated by IL-17, phosphorylation of the MAPK and AKT pathways was determined by immunoblot analysis. Our data demonstrate that IL-17 phosphorylates ERK, JNK and AKT1 as early as 15 min. While the activation of ERK and JNK is gradually reduced at 75 and 65 min (Figure 6B–C), respectively, AKT1 is still strongly phosphorylated at 75min (Figure 6A). The p38 pathway was not activated by IL-17 in HMVECs (data not shown). To determine which signaling pathways mediate HMVEC migration, chemical inhibitors at concentrations of 1 and 5 μM were utilized, while 10 μM was toxic and resulted in cell death, as determined by trypan blue staining (data not shown). Inhibition of ERK and JNK was ineffective in suppressing IL-17-induced HMVEC chemotaxis, while inhibition of PI3K reduced (p<0.05) chemotaxis starting at 1 μM (Figure 6D). Similarly, while inhibition of PI3K (starting at 1 μM) reduced IL-17-mediated tube formation by 30–40% (p<0.05) (Figure 7), suppression of ERK and JNK had no effect on this process. These results suggest that IL-17-induced HMVEC chemotaxis and tube formation are mediated through the PI3K/AKT1 pathway.
Figure 6. IL-17-induced HMVEC migration is suppressed by PI3K inhibition.
In order to determine the mechanism of IL-17 in HMVECs, cells were stimulated with IL-17 (50 ng/ml) for 0–75 minutes, and the cell lysates were probed for p-AKT (A), pERK (B), or pJNK (C). These results are representative of 3 experiments. D. To determine signaling pathways associated with IL-17 HMVEC migration, cells were treated with the identified chemical inhibitors for PI3K (LY294002; 1 and 5μM) or ERK (PD98059; 1 and 5 μM) as well as JNK (SP600125; 1, 5μM) 2h in the Boyden chamber. Only inhibition of PI3K downregulated IL-17-induced HMVEC migration. Values demonstrate mean ± SE of three experiments in triplicate. * represents p <0.05.
Figure 7. IL-17-mediated tube formation is reduced by inhibition of PI3K.
HMVECs were incubated with inhibitors to PI3K (LY294002; 1 and 5 μM), ERK (PD98059; 1 and 5 μM), JNK (SP600125; 1 and 5 μM) or DMSO for 45 minutes at 37°C prior adding to polymerized matrigel. IL-17 (50ng/ml) was then added to the wells and the plate was incubated for 16h at 37°C (in triplicate). Photomicrographs taken of representative wells treated with PBS (A), FGF (20 ng/ml) (B), IL-17 (50ng/ml) plus DMSO (C), IL-17 (50ng/ml) plus LY294002 (5 μM) (D), IL-17 (50ng/ml) plus PD98059 (5 μM)(E) and IL-17 (50ng/ml) plus SP600125 (5 μM) (F) in which IL-17-induced tube formation is significantly reduced by the inhibition of PI3K/AKT1 pathway (p<0.05). G. demonstrates mean number of tubes/well where LY294002 (1 and 5 μM; PI3K/AKT1 inhibitor) significantly reduces the number of branch points induced by IL-17 activation in matrigel tube formation assay whereas ERK (PD98059; 1 and 5 μM) and JNK inhibitors (SP600125; 1 and 5 μM) were ineffective. Values are the mean ± SE, n=3. * represents p <0.05.
IL-17 and its receptor are involved in RA synovial fluid-mediated HMVEC chemotaxis
Next we asked whether the IL-17 identified in human RA synovial fluid is chemotactic for HMVECs. In these experiments, we demonstrated that human RA synovial fluid is chemotactic for HMVECs, similar to positive control VEGF (Figure 8A). Furthermore, human RA synovial fluid immunodepleted with anti-IL-17 significantly reduced HMVEC chemotaxis (p<0.05), compared with control IgG-treated fluids. Neutralization of IL-17RA and RC on HMVECs showed that only IL-17RC was effective in suppressing human RA synovial fluid-mediated HMVEC migration (Figure 8B). These results suggest that IL-17 and its receptor IL-17RC may play an important role in angiogenesis in RA. Further we demonstrate that immunodepletion of IL-17 and VEGF in RA synovial fluids does not have an additive or synergistic effect in reduction of HMVEC migration beyond the effect noted with neutralization of one factor alone (Figure 8C) suggesting that both IL-17 and VEGF may be mediating HMVEC migration through the same signaling pathway.
Figure 8. RA synovial fluid-induced HMVEC chemotaxis is mediated by IL-17 through ligation to IL-17RC and IL-17 does not synergize with VEGF in RA synovial fluid induced HMVEC migration.
A. anti-IL-17 (10 μg/ml) or control IgG was added to RA synovial fluids from 8 patients (1:20 dilution) (1h at 37°C) prior to performing HMVEC chemotaxis in response to human RA synovial fluids. B. HMVECs were incubated with antibodies to IL-17 RA and RC (10 μg/ml), as well as isotype control for 1h prior to performing HMVEC chemotaxis in response to 8 human RA synovial fluids. C. RA synovial fluids from 8 patients (1:20 dilution) were incubated with antibodies to IL-17 (10 μg/ml), VEGF (10 μg/ml), or both as well as isotype control or PBS or VEGF for 1h prior to performing HMVEC chemotaxis in response to RA synovial fluids. The values represent the mean ± SE. * represents p <0.05.
DISCUSSION
In this study, we show that IL-17 increases vascularity in experimental arthritis and induces blood vessel development in matrigel plugs in vivo. Therefore, studies were performed to determine whether IL-17 might directly mediate angiogenesis and whether IL-17 contributes to neovascularization in RA. Our data demonstrate that IL-17 induces HMVEC chemotaxis at concentrations present in human RA synovial fluid. This effect is directly mediated by IL-17, since heat inactivation and neutralizing antibodies to IL-17 and/or IL-17 receptors abrogate IL-17-induced HMVEC chemotaxis. We further demonstrate that IL-17-induced HMVEC chemotaxis and tube formation are mediated primarily through ligation to IL-17RC on HMVECs and activation of PI3K. We show that human RA synovial fluid-mediated HMVEC chemotaxis is markedly reduced by neutralization of IL-17 in the synovial fluids or blocking of IL-17RC on HMVECs. Lastly, we demonstrate that IL-17 and VEGF immunodepleted RA synovial fluid does not reduce HMVEC chemotaxis any further than neutralization of each factor by itself.
In this manuscript we confirm the results of others demonstrating that the local expression of IL-17 in mouse ankle joints induces arthritis (9). Histological analysis of mice receiving intra-articular injections of IL-17 demonstrated that IL-17 plays an important role in joint neutrophil migration (42). In this study, we demonstrate that IL-17-induced arthritis is associated with increased vascularity. Others have shown that IL-17 can promote tumor growth by upregulating proangiogenic factors such as VEGF and MMP9 from tumor cells, suggesting that IL-17 is indirectly associated with angiogenesis (43). We have also shown that forced ectopic expression of IL-17 induces expression of proangiogenic CXC (ELR+) chemokines in mouse ankles (unpublished data).
Based on our results from the IL-17-induced arthritis model, we hypothesized that IL-17 may be important for angiogenesis in RA. Since there is some evidence demonstrating that IL-17 alone is unable to induce angiogenesis, but can indirectly promote HMVEC chemotaxis by producing proangiogenic factors (29, 30) from RA synovial tissue fibroblasts, we investigated the role of IL-17 on HMVEC migration and tube formation. Our results demonstrate that IL-17 induces HMVEC chemotaxis at concentrations available in the human RA joint, which is mostly due to its ligation to IL-17RC. Although IL-17RC plays a major role in IL-17-mediated HMVEC chemotaxis and tube formation, neutralization of both receptors is more effective in this process compared to IL-17RC alone. Like monocytes, HMVECs express both IL-17RA and IL-17RC (21). However, in contrast to HMVEC chemotaxis, IL-17-mediated monocyte migration is induced through both IL-17RA and RC (21). Interestingly, a novel IL-17 receptor-like protein has been identified in HUVEC that interacts with fibroblast growth factor receptor (FGF)1 and inhibits activation of the ERK pathway and production of FGF, indicating that various IL-17 receptors may modulate angiogenesis differently (44).
Next, experiments were performed to investigate signaling pathways that were associated with IL-17-induced HMVEC chemotaxis and tube formation. Inhibition of the IL-17-activated pathways in HMVECs demonstrated that only activation of PI3K significantly reduces IL-17-mediated chemotaxis and tube formation, and suppression of ERK and JNK pathways were ineffective in this process. Consistently, CCL2/MCP-1-mediated endothelial chemotaxis is through activation of PI3K, as well as the ERK pathway (45). Further, others have shown that PI3K signaling plays an important role in regulation of VEGF production as well as VEGF-mediated endothelial migration (46, 47), suggesting that PI3K is involved in the mediation of angiogenesis by various proinflammatory factors. A recently published paper shows that increased expression of IL-17 in IFNγ −/− mice mediates tumor growth and angiogenesis through STAT3 phosphorylation (43). In contrast to IL-17, which promotes angiogenesis, IL-17F inhibits HUVEC tube formation, indicating that different IL-17 isoforms may modulate angiogenesis differently (48).
A recent publication demonstrated that tumor growth in subcutaneous and lung metastases are enhanced in IL-17−/− mice compared to the wild type controls, suggesting that IL-17 may suppress tumor development (27). Conversely, others have shown that IL-17 markedly increases neovascularization in rat cornea (28) and vascularization in tumors (49), indicating that IL-17 may promote angiogenesis. However, there is also evidence demonstrating that IL-17 induces production of proangiogenic factors including nitric oxide (NO), hepatocyte growth factor (HGF), CXCL1/KC, CXCL2/MIP-2, prostaglandin (PGE)1, PGE2 and VEGF from RA synovial fibroblasts, and the production of some of these factors is further enhanced by TNF-α (50). Therefore, we investigated the contribution of IL-17 to human RA synovial fluid-mediated HMVEC chemotaxis. Neutralization of IL-17 in RA synovial fluid partially reduced RA synovial fluid-mediated HMVEC chemotaxis. RA synovial fluid-mediated HMVEC chemotaxis was mediated through IL-17RC, confirming the importance of this receptor in IL-17-mediated angiogenesis. Interestingly, angiogenic factors present in human RA synovial fluid are mostly produced by RA synovial tissue fibroblasts (VEGF, bFGF, VCAM1, IL-6 and ELR+ CXC chemokines) or macrophages (TNF-α, IL-8 and IL-1β) (25). IL-17 is the only lymphokine that contributes to human RA synovial fluid-mediated angiogenesis, suggesting that T cells may also be important in this process. The data presented in this study, together with our previously reported evidence demonstrating that IL-17 is important for monocyte migration(21) in RA synovial fluids, highlight the importance of IL-17 in RA pathogenesis.
Interestingly, our results show that neutralization of IL-17 and VEGF do not synergize in reducing rheumatoid arthritis synovial fluid-induced HMVEC migration beyond the effect detected with one factor alone. As shown with IL-17, VEGF-induced HMVEC chemotaxis is mediated through PI3K (46, 51). Therefore the lack of synergy between IL-17 and VEGF in inducing HMVEC chemotaxis may be due to that both mediators are utilizing the same signaling pathway or that as shown previously HMVEC cell migration is within a bell shaped curve (37, 52) therefore the synergistic effect could not be detected.
In conclusion, endothelial migration and tube formation induced by IL-17 were mediated through activation of the PI3K pathway and ligation to both IL-17 receptors. However, neutralization of only IL-17 or IL-17RC significantly downregulated human RA synovial fluid-mediated endothelial migration, suggesting that IL-17 plays an important role in RA angiogenesis.
Acknowledgments
This work was supported in part by awards from the National Institutes of Health (AR056099, AR055240, AR048269 and NS34510), Arthritis National Research Foundation and grants from Within Our Reach from The American College of Rheumatology.
References
- 1.Dong C. TH17 cells in development: an updated view of their molecular identity and genetic programming. Nat Rev Immunol. 2008;8:337–348. doi: 10.1038/nri2295. [DOI] [PubMed] [Google Scholar]
- 2.Nistala K, Wedderburn LR. Th17 and regulatory T cells: rebalancing pro- and anti-inflammatory forces in autoimmune arthritis. Rheumatology. 2009;48:602–606. doi: 10.1093/rheumatology/kep028. [DOI] [PubMed] [Google Scholar]
- 3.Stamp LK, James MJ, Cleland LG. Interleukin-17: the missing link between T-cell accumulation and effector cell actions in rheumatoid arthritis? Immunology and cell biology. 2004;82:1–9. doi: 10.1111/j.1440-1711.2004.01212.x. [DOI] [PubMed] [Google Scholar]
- 4.Manel N, Unutmaz D, Littman DR. The differentiation of human T(H)-17 cells requires transforming growth factor-beta and induction of the nuclear receptor RORgammat. Nat Immunol. 2008;9:641–649. doi: 10.1038/ni.1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volpe E, Servant N, Zollinger R, Bogiatzi SI, Hupe P, Barillot E, Soumelis V. A critical function for transforming growth factor-beta, interleukin 23 and proinflammatory cytokines in driving and modulating human T(H)-17 responses. Nat Immunol. 2008;9:650–657. doi: 10.1038/ni.1613. [DOI] [PubMed] [Google Scholar]
- 6.Annunziato F, Cosmi L, Liotta F, Maggi E, Romagnani S. Type 17 T helper cells-origins, features and possible roles in rheumatic disease. Nat Rev Rheumatol. 2009;5:325–331. doi: 10.1038/nrrheum.2009.80. [DOI] [PubMed] [Google Scholar]
- 7.Gabay C, I, McInnes B. The biological and clinical importance of the ‘new generation’ cytokines in rheumatic diseases. Arthritis Res Ther. 2009;11:230. doi: 10.1186/ar2680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pernis AB. Th17 cells in rheumatoid arthritis and systemic lupus erythematosus. J Intern Med. 2009;265:644–652. doi: 10.1111/j.1365-2796.2009.02099.x. [DOI] [PubMed] [Google Scholar]
- 9.Koenders MI, Lubberts E, van de Loo FA, Oppers-Walgreen B, van den Bersselaar L, Helsen MM, Kolls JK, Di Padova FE, Joosten LA, van den Berg WB. Interleukin-17 acts independently of TNF-alpha under arthritic conditions. J Immunol. 2006;176:6262–6269. doi: 10.4049/jimmunol.176.10.6262. [DOI] [PubMed] [Google Scholar]
- 10.Nakae S, Nambu A, Sudo K, Iwakura Y. Suppression of immune induction of collagen-induced arthritis in IL-17-deficient mice. J Immunol. 2003;171:6173–6177. doi: 10.4049/jimmunol.171.11.6173. [DOI] [PubMed] [Google Scholar]
- 11.Abdollahi-Roodsaz S, Joosten LA, Helsen MM, Walgreen B, van Lent PL, van den Bersselaar LA, Koenders MI, van den Berg WB. Shift from toll-like receptor 2 (TLR-2) toward TLR-4 dependency in the erosive stage of chronic streptococcal cell wall arthritis coincident with TLR-4-mediated interleukin-17 production. Arthritis Rheum. 2008;58:3753–3764. doi: 10.1002/art.24127. [DOI] [PubMed] [Google Scholar]
- 12.Koenders MI, Devesa I, Marijnissen RJ, Abdollahi-Roodsaz S, Boots AM, Walgreen B, di Padova FE, Nicklin MJ, Joosten LA, van den Berg WB. Interleukin-1 drives pathogenic Th17 cells during spontaneous arthritis in interleukin-1 receptor antagonist-deficient mice. Arthritis Rheum. 2008;58:3461–3470. doi: 10.1002/art.23957. [DOI] [PubMed] [Google Scholar]
- 13.Nakae S, Saijo S, Horai R, Sudo K, Mori S, Iwakura Y. IL-17 production from activated T cells is required for the spontaneous development of destructive arthritis in mice deficient in IL-1 receptor antagonist. Proc Natl Acad Sci USA. 2003;100:5986–5990. doi: 10.1073/pnas.1035999100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shahrara S, Huang Q, Mandelin AM, 2nd, Pope RM. TH-17 cells in rheumatoid arthritis. Arthritis Res Ther. 2008;10:R93. doi: 10.1186/ar2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katz Y, Nadiv O, Beer Y. Interleukin-17 enhances tumor necrosis factor alpha-induced synthesis of interleukins 1,6, and 8 in skin and synovial fibroblasts: a possible role as a “fine-tuning cytokine” in inflammation processes. Arthritis Rheum. 2001;44:2176–2184. doi: 10.1002/1529-0131(200109)44:9<2176::aid-art371>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 16.Chabaud M, Page G, Miossec P. Enhancing Effect of IL-1, IL-17, and TNF-alpha on Macrophage Inflammatory Protein-3alpha Production in Rheumatoid Arthritis: Regulation by Soluble Receptors and Th2 Cytokines. J Immunol. 2001;167:6015–6020. doi: 10.4049/jimmunol.167.10.6015. [DOI] [PubMed] [Google Scholar]
- 17.Kehlen A, Thiele K, Riemann D, Langner J. Expression, modulation and signalling of IL-17 receptor in fibroblast-like synoviocytes of patients with rheumatoid arthritis. Clin Exp Immunol. 2002;127:539–546. doi: 10.1046/j.1365-2249.2002.01782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jovanovic DV, Di Battista JA, Martel-Pelletier J, Jolicoeur FC, He Y, Zhang M, Mineau F, Pelletier JP. IL-17 stimulates the production and expression of proinflammatory cytokines, IL-beta and TNF-alpha, by human macrophages. J Immunol. 1998;160:3513–3521. [PubMed] [Google Scholar]
- 19.Jovanovic DV, Di Battista JA, Martel-Pelletier J, Reboul P, He Y, Jolicoeur FC, Pelletier JP. Modulation of TIMP-1 synthesis by antiinflammatory cytokines and prostaglandin E2 in interleukin 17 stimulated human monocytes/macrophages. J Rheumatol. 2001;28:712–718. [PubMed] [Google Scholar]
- 20.Jovanovic DV, Martel-Pelletier J, Di Battista JA, Mineau F, Jolicoeur FC, Benderdour M, Pelletier JP. Stimulation of 92-kd gelatinase (matrix metalloproteinase 9) production by interleukin-17 in human monocyte/macrophages: a possible role in rheumatoid arthritis. Arthritis Rheum. 2000;43:1134–1144. doi: 10.1002/1529-0131(200005)43:5<1134::AID-ANR24>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 21.Shahrara S, Pickens SR, Dorfleutner A, Pope RM. IL-17 induces monocyte migration in rheumatoid arthritis. J Immunol. 2009;182:3884–3891. doi: 10.4049/jimmunol.0802246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laan M, Cui ZH, Hoshino H, Lotvall J, Sjostrand M, Gruenert DC, Skoogh BE, Linden A. Neutrophil recruitment by human IL-17 via C-X-C chemokine release in the airways. J Immunol. 1999;162:2347–2352. [PubMed] [Google Scholar]
- 23.Luzza F, Parrello T, Monteleone G, Sebkova L, Romano M, Zarrilli R, Imeneo M, Pallone F. Up-regulation of IL-17 is associated with bioactive IL-8 expression in Helicobacter pylori-infected human gastric mucosa. J Immunol. 2000;165:5332–5337. doi: 10.4049/jimmunol.165.9.5332. [DOI] [PubMed] [Google Scholar]
- 24.Szekanecz Z, Koch AE. Mechanisms of Disease: angiogenesis in inflammatory diseases. Nat Clin Pract Rheumatol. 2007;3:635–643. doi: 10.1038/ncprheum0647. [DOI] [PubMed] [Google Scholar]
- 25.Szekanecz Z, Koch AE. Angiogenesis and its targeting in rheumatoid arthritis. Vascul Pharmacol. 2009;51:1–7. doi: 10.1016/j.vph.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Benchetrit F, Ciree A, Vives V, Warnier G, Gey A, Sautes-Fridman C, Fossiez F, Haicheur N, Fridman WH, Tartour E. Interleukin-17 inhibits tumor cell growth by means of a T-cell-dependent mechanism. Blood. 2002;99:2114–2121. doi: 10.1182/blood.v99.6.2114. [DOI] [PubMed] [Google Scholar]
- 27.Kryczek I, Wei S, Szeliga W, Vatan L, Zou W. Endogenous IL-17 contributes to reduced tumor growth and metastasis. Blood. 2009 doi: 10.1182/blood-2008-09-177360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Numasaki M, Fukushi J, Ono M, Narula SK, Zavodny PJ, Kudo T, Robbins PD, Tahara H, Lotze MT. Interleukin-17 promotes angiogenesis and tumor growth. Blood. 2003;101:2620–2627. doi: 10.1182/blood-2002-05-1461. [DOI] [PubMed] [Google Scholar]
- 29.Ryu S, Lee JH, Kim SI. IL-17 increased the production of vascular endothelial growth factor in rheumatoid arthritis synoviocytes. Clin Rheumatol. 2006;25:16–20. doi: 10.1007/s10067-005-1081-1. [DOI] [PubMed] [Google Scholar]
- 30.Honorati MC, Neri S, Cattini L, Facchini A. Interleukin-17, a regulator of angiogenic factor release by synovial fibroblasts. Osteoarthritis Cartilage. 2006;14:345–352. doi: 10.1016/j.joca.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Schwarzenberger P, La Russa V, Miller A, Ye P, Huang W, Zieske A, Nelson S, Bagby GJ, Stoltz D, Mynatt RL, Spriggs M, Kolls JK. IL-17 stimulates granulopoiesis in mice: use of an alternate, novel gene therapy-derived method for in vivo evaluation of cytokines. J Immunol. 1998;161:6383–6389. [PubMed] [Google Scholar]
- 32.Ruth JH, Volin MV, Haines GK, III, Woodruff DC, Katschke KJ, Jr, Woods JM, Park CC, Morel JCM, Koch AE. Fractalkine, a novel chemokine in rheumatoid arthritis and in rat adjuvant-induced arthritis. Arthritis Rheum. 2001;44:1568–1581. doi: 10.1002/1529-0131(200107)44:7<1568::AID-ART280>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 33.Koch AE, Nickoloff BJ, Holgersson J, Seed B, Haines GK, Burrows JC, Leibovich SJ. 4A11, a monoclonal antibody recognizing a novel antigen expressed on aberrant vascular endothelium. Upregulation in an in vivo model of contact dermatitis. Am J Pathol. 1994;144:244–259. [PMC free article] [PubMed] [Google Scholar]
- 34.Shahrara S, Proudfoot AE, Woods JM, Ruth JH, Amin MA, Park CC, Haas CS, Pope RM, Haines GK, Zha YY, Koch AE. Amelioration of rat adjuvant-induced arthritis by Met-RANTES. Arthritis Rheum. 2005;52:1907–1919. doi: 10.1002/art.21033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shahrara S, Proudfoot AE, Park CC, Volin MV, Haines GK, Woods JM, Aikens CH, Handel TM, Pope RM. Inhibition of monocyte chemoattractant protein-1 ameliorates rat adjuvant-induced arthritis. J Immunol. 2008;180:3447–3456. doi: 10.4049/jimmunol.180.5.3447. [DOI] [PubMed] [Google Scholar]
- 36.Haas CS, Amin MA, Ruth JH, Allen BL, Ahmed S, Pakozdi A, Woods JM, Shahrara S, Koch AE. In vivo inhibition of angiogenesis by interleukin-13 gene therapy in a rat model of rheumatoid arthritis. Arthritis Rheum. 2007;56:2535–2548. doi: 10.1002/art.22823. [DOI] [PubMed] [Google Scholar]
- 37.Park CC, Morel JC, Amin MA, Connors MA, Harlow LA, Koch AE. Evidence of IL-18 as a novel angiogenic mediator. J Immunol. 2001;167:1644–1653. doi: 10.4049/jimmunol.167.3.1644. [DOI] [PubMed] [Google Scholar]
- 38.Kumar P, Amin MA, Harlow LA, Polverini PJ, Koch AE. Src and phosphatidylinositol 3-kinase mediate soluble E-selectin-induced angiogenesis. Blood. 2003;101:3960–3968. doi: 10.1182/blood-2002-04-1237. [DOI] [PubMed] [Google Scholar]
- 39.Koch AE, Halloran MM, Haskell CJ, Shah MR, Polverini PJ. Angiogenesis mediated by soluble forms of E-selectin and vascular cell adhesion molecule-1. Nature. 1995;376:517–519. doi: 10.1038/376517a0. [DOI] [PubMed] [Google Scholar]
- 40.Shahrara S, Park CC, Temkin V, Jarvis JW, Volin MV, Pope RM. RANTES modulates TLR4-induced cytokine secretion in human peripheral blood monocytes. J Immunol. 2006;177:5077–5087. doi: 10.4049/jimmunol.177.8.5077. [DOI] [PubMed] [Google Scholar]
- 41.Shahrara S, Castro-Rueda HP, Haines GK, Koch AE. Differential expression of the FAK family kinases in rheumatoid arthritis and osteoarthritis synovial tissues. Arthritis Res Ther. 2007;9:R112. doi: 10.1186/ar2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lubberts E, Joosten LA, Oppers B, van den Bersselaar L, Coenen-de Roo CJ, Kolls JK, Schwarzenberger P, van de Loo FA, van den Berg WB. IL-1-independent role of IL-17 in synovial inflammation and joint destruction during collagen-induced arthritis. J Immunol. 2001;167:1004–1013. doi: 10.4049/jimmunol.167.2.1004. [DOI] [PubMed] [Google Scholar]
- 43.Wang L, Yi T, Kortylewski M, Pardoll DM, Zeng D, Yu H. IL-17 can promote tumor growth through an IL-6-Stat3 signaling pathway. J Exp Med. 2009;206:1457–1464. doi: 10.1084/jem.20090207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang RB, Ng CK, Wasserman SM, Komuves LG, Gerritsen ME, Topper JN. A novel interleukin-17 receptor-like protein identified in human umbilical vein endothelial cells antagonizes basic fibroblast growth factor-induced signaling. J Biol Chem. 2003;278:33232–33238. doi: 10.1074/jbc.M305022200. [DOI] [PubMed] [Google Scholar]
- 45.Arefieva TI, Kukhtina NB, Antonova OA, Krasnikova TL. MCP-1-stimulated chemotaxis of monocytic and endothelial cells is dependent on activation of different signaling cascades. Cytokine. 2005;31:439–446. doi: 10.1016/j.cyto.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 46.Jiang BH, Liu LZ. AKT signaling in regulating angiogenesis. Curr Cancer Drug Targets. 2008;8:19–26. doi: 10.2174/156800908783497122. [DOI] [PubMed] [Google Scholar]
- 47.Hayashi H, Nakagami H, Takami Y, Koriyama H, Mori M, Tamai K, Sun J, Nagao K, Morishita R, Kaneda Y. FHL-2 Suppresses VEGF-Induced Phosphatidylinositol 3-Kinase/Akt Activation via Interaction With Sphingosine Kinase-1. Arterioscler Thromb Vasc Biol. 2009 doi: 10.1161/ATVBAHA.108.178541. [DOI] [PubMed] [Google Scholar]
- 48.Starnes T, Robertson MJ, Sledge G, Kelich S, Nakshatri H, Broxmeyer HE, Hromas R. Cutting edge: il-17f, a novel cytokine selectively expressed in activated t cells and monocytes, regulates angiogenesis and endothelial cell cytokine production. J Immunol. 2001;167:4137–4140. doi: 10.4049/jimmunol.167.8.4137. [DOI] [PubMed] [Google Scholar]
- 49.Numasaki M, Watanabe M, Suzuki T, Takahashi H, Nakamura A, McAllister F, Hishinuma T, Goto J, Lotze MT, Kolls JK, Sasaki H. IL-17 enhances the net angiogenic activity and in vivo growth of human non-small cell lung cancer in SCID mice through promoting CXCR-2-dependent angiogenesis. J Immunol. 2005;175:6177–6189. doi: 10.4049/jimmunol.175.9.6177. [DOI] [PubMed] [Google Scholar]
- 50.Numasaki M, Lotze MT, Sasaki H. Interleukin-17 augments tumor necrosis factor-alpha-induced elaboration of proangiogenic factors from fibroblasts. Immunol Lett. 2004;93:39–43. doi: 10.1016/j.imlet.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 51.Nakashio A, Fujita N, Tsuruo T. Topotecan inhibits VEGF- and bFGF-induced vascular endothelial cell migration via downregulation of the PI3K-Akt signaling pathway. Int J Cancer. 2002;98:36–41. doi: 10.1002/ijc.10166. [DOI] [PubMed] [Google Scholar]
- 52.Volin MV, Harlow LA, Woods JM, Campbell PL, Amin MA, Tokuhira M, Koch AE. Treatment with sulfasalazine or sulfapyridine, but not 5-aminosalicyclic acid, inhibits basic fibroblast growth factor-induced endothelial cell chemotaxis. Arthritis Rheum. 1999;42:1927–1935. doi: 10.1002/1529-0131(199909)42:9<1927::AID-ANR19>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]