Abstract
Objective: To compare effectiveness and acceptability of early discharge to a hospital at home scheme with that of routine discharge from acute hospital.
Design: Pragmatic randomised controlled trial.
Setting: Acute hospital wards and community in north of Bristol, with a catchment population of about 224 000 people.
Subjects: 241 hospitalised but medically stable elderly patients who fulfilled criteria for early discharge to hospital at home scheme and who consented to participate.
Interventions: Patients’ received hospital at home care or routine hospital care.
Main outcome measures: Patients’ quality of life, satisfaction, and physical functioning assessed at 4 weeks and 3 months after randomisation to treatment; length of stay in hospital and in hospital at home scheme after randomisation; mortality at 3 months.
Results: There were no significant differences in patient mortality, quality of life, and physical functioning between the two arms of the trial at 4 weeks or 3 months. Only one of 11 measures of patient satisfaction was significantly different: hospital at home patients perceived higher levels of involvement in decisions. Length of stay for those receiving routine hospital care was 62% (95% confidence interval 51% to 75%) of length of stay in hospital at home scheme.
Conclusions: The early discharge hospital at home scheme was similar to routine hospital discharge in terms of effectiveness and acceptability. Increased length of stay associated with the scheme must be interpreted with caution because of different organisational characteristics of the services.
Key messages
Pressure on hospital beds, the increasing age of the population, and high costs associated with acute hospital care have fuelled the search for alternatives to inpatient hospital care
There were no significant differences between early discharge to hospital at home scheme and routine hospital care in terms of patient quality of life, physical functioning, and most measures of patient satisfaction
Length of stay for hospital patients was significantly shorter than that of hospital at home patients, but, owing to qualitative differences between the two interventions, this does not necessarily mean differences in effectiveness
Early discharge to hospital at home provides an acceptable alternative to routine hospital care in terms of effectiveness and patient acceptability
Introduction
Alternatives to inpatient hospital care have become a focus of interest among health service strategists working towards a primary care led NHS.1 They seem to offer potential for reducing both the number of admissions and the length of hospital stay.2 The search for alternative settings for care has arisen because of several factors, including pressure on hospital beds and the increasing age of the population, with the concomitant increase in morbidity and the high costs of maintaining patients in acute hospitals.1,3 At the same time, home healthcare technology is becoming more sophisticated, and standards of the home environment have improved. These changes facilitate home management of certain groups of patients.1,4
“Hospital at home” is a generic term, referring to a package of home based nursing and rehabilitation services.1,4 Schemes can be divided into two main groups: those that prevent admission into an acute hospital and those facilitating the early discharge of patients from an acute hospital.5–8 In both cases the purpose of hospital at home is to provide a substitute for hospital care, although in practice some evaluations have found that hospital at home is an additional rather than a substitute service.9,10
Previous evaluations of early discharge, hospital at home schemes for orthopaedic patients in Britain have indicated that such schemes may reduce total length of hospital stay,5,8,11 although a recent evaluation found the opposite.9 One British evaluation of an early discharge service with a varied case mix also concluded that it was a cost effective alternative to hospital care.6 Estimates of the inpatient orthopaedic bed days saved by early discharge schemes vary considerably, from 5 days8 up to 9.6 days.5 The potential for saving inpatient bed days will vary depending on a patient’s condition and the baseline efficiency in bed use of a particular hospital.
There are substantial methodological problems with previous evaluations, and to date no randomised trials have evaluated the effectiveness and acceptability of early discharge, hospital at home schemes. This paper reports the results of effectiveness and acceptability from a pragmatic randomised controlled trial of such a scheme operating in Bristol. This service caters for two main types of patients, emergency admissions from a variety of specialties and elective patients undergoing hip or knee replacement.
Subjects and methods
Patient selection
Patients suitable for early discharge to hospital at home care were identified by ward staff from general medical, care of the elderly, orthopaedic, and general surgical specialties. The box shows patient selection criteria, remit of the team, and staffing of the hospital at home scheme. All patients were assessed for suitability by the hospital at home coordinator (MAD), who then obtained informed consent for entry into the trial from the patients and, when appropriate, carers. Consent from next of kin was provided for patients who were unable to provide such consent themselves (these patients were not asked to complete any measures themselves). The local ethics committee gave approval for this study.
Hospital at home scheme: patient suitability, remit, and staffing
Patient suitability (assessed by hospital at home coordinator)
Adult patient (all but 16 were aged over 65 years) on an acute hospital ward and resident within catchment area of Frenchay NHS Trust
Positive rehabilitative outcome expected
Appropriate home circumstances (that is, adequate heating, safety in relation to patient’s disability) and, if necessary, adequate support from carers available
Patient would require further hospital care if team were not available
Patient should not be awaiting a nursing home place or input of social care alone
Patient expected to remain in hospital for between 1 and 28 days
Patient’s general practitioner accepts clinical responsibility
Remit of scheme
Maximum case load of 12 patients (orthopaedic) at any one time, or less if higher dependency patients (such as stroke) managed
Care routinely provided between 8 30 am and 11 pm; exceptionally, care provided outside these times
Service provided is for health care, with minimal essential domestic tasks performed
Discharge from hospital at home when patient could be managed by routinely available community services
Staffing of scheme
1 whole time equivalent G grade district nurse coordinator
1 whole time equivalent E grade registered nurse
0.8 whole time equivalent senior 1 physiotherapist
0.5 whole time equivalent senior 1 occupational therapist
3 part time B grade support workers (20-27 hours each per week)
1 occupational therapy technician as required (6-12 hours per month)
Treatment schedules
Patients suitable for the hospital at home scheme were randomised to hospital at home or acute hospital care in a ratio of 2:1 in order to maintain sufficient patients for the scheme. Randomisation (in blocks of six) was stratified by type of admission (elective or emergency) and done by means of sealed envelopes produced independently of the research and clinical staff.
Patients within the hospital arm of the trial received usual hospital care. Patients in the hospital at home scheme received rehabilitative care at home (see box) until they were either discharged from the team or readmitted to hospital.
Patient assessment
Emergency patients who were deemed appropriate for the hospital at home scheme completed a baseline interview in hospital and were then randomised. For pragmatic reasons, the small number of elective patients was randomised before surgery at a stage when a home assessment by the hospital at home team would, in practice, be made. This was to assist discharge planning for both treatment arms and to ensure that patients did not experience unnecessary uncertainty about their care after surgery. The baseline interview was conducted to mimic the interview timing of emergency patients (about 5 days postoperatively), and randomisation was considered to become effective at this point. It was not possible to blind the researcher during the baseline interview of elective patients.
Follow up assessments were conducted 4 weeks and 3 months after randomisation (this was taken as the date of the baseline interview for all patients). A combination of self completed and interviewer administered instruments was used.
Baseline interview
Sociodemographic information, including age, sex, living circumstances, social class, longstanding health,12 and information about the patient’s hospital stay was collected.
Cognitive ability was assessed by mean of the Folstein mini-mental state examination.13
Functional ability was assessed with the Barthel activities of daily living index14 scored using investigation criteria derived from Collin et al.15
Quality of life was assessed with two generic quality of life measures, the EuroQol EQ-5D16 and the COOP-WONCA charts.17 While the former had a one day time frame, the baseline COOP-WONCA charts were the subject of a nested trial of the standard 2 week and a 48 hour time frame.18
Four week and three month follow ups
Patient mortality was ascertained from general practitioner and hospital records.
Post-randomisation length of stay was defined as the period for which a patient was supervised by a service, either hospital or hospital at home, from the (effective) date of randomisation. For hospital patients, the length of stay was therefore from randomisation date until discharge from hospital. For hospital at home patients, length of stay was from randomisation date until discharge from hospital plus total stay in hospital at home plus any readmission occurring while the hospital at home care was being provided.
In addition, we assessed the patients’ functional ability (Barthel index), quality of life (EQ-5D and COOP-WONCA with standard time frame), and satisfaction with the primary and secondary care services received.
Sample size considerations
With a two sided 5% significance level, a total sample size of 250 (with 2:1 randomisation ratio) would yield about 85% power to detect a standardised difference of 0.4 standard deviations on outcome measures. In terms of length of stay, based on routine data from patients with conditions similar to those expected to be cared for by the hospital at home scheme, the study would be able to detect a difference in the mean length of stay of between 2.8 and 5.2 days.
Data handling and statistical methods
We performed data analysis with the SAS statistical package and carried out all comparisons of outcomes on an intention to treat basis. Skewed distributions meant that we analysed length of stay and the COOP-WONCA pain chart using Mann-Whitney U tests. Log transformed data were used for the length of stay confidence intervals. We analysed satisfaction questions using the Mann-Whitney U test for ordinal data and χ2 or exact methods for categorical data. A two sided 5% significance level was used throughout.
We analysed the Barthel index, remaining COOP-WONCA charts, and EQ-5D (score and thermometer) using multivariate repeated measures analysis of variance methods for the baseline, 4 week, and 3 month measurements. The results of the nested trial of time frame for the COOP-WONCA charts18 indicated that the baseline assessments for all charts except pain could be used in this way. Confidence intervals for differences through time were obtained from separate (univariate) analyses of covariance for the two follow up assessments adjusted for baseline.
Results
Recruitment and patient progression through study
The hospital at home scheme for acute admissions began operating in April 1994, but recruitment of patients into the trial did not begin until July 1994 to allow the team to develop its practices. Elective surgical patients were referred to the team from April 1995, but recruitment of such patients did not begin until June 1995. Recruitment was complete by October 1995.
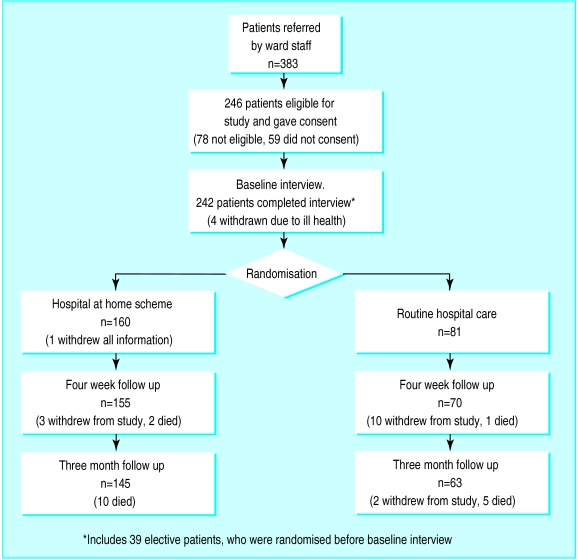
A total of 383 patients were referred by ward staff to the hospital at home scheme during the recruitment period (see figure). Of these, 78 were not appropriate for hospital at home care and 59 did not consent to take part. The 246 suitable and consenting patients were subsequently randomised (203 emergency and 43 elective admissions). Four patients undergoing elective procedures never became appropriate for the scheme because of ill health after surgery, and one emergency patient randomised to the hospital at home scheme requested that all study information be withdrawn. Of the remaining 241 patients, 160 were randomised to the hospital at home scheme (two of whom subsequently developed complications and remained in hospital and four of whom were readmitted to hospital from hospital at home) and 81 to routine hospital discharge. Eleven of these patients had consent provided by next of kin as they were unable to provide consent themselves.
By the 4 week interview, information was available for 225 (93%) of the patients, and, by 3 months, information was available for 208 patients (86%).
Characteristics of patients at baseline
Most of the patients (68%) had been admitted for orthopaedic procedures. The largest diagnostic category was fractured neck of femur (31%), with the rest being other fractures (21%), elective hip replacement (11%), cerebrovascular accidents (10%), elective knee replacement (5%), and miscellaneous reasons (22%) such as chest infection or falls without fractures.
Table 1 summarises the trial patients’ sociodemographic characteristics and their health status at the time of recruitment (including cognitive and functional ability). Most of the patients were elderly and female, and about half were living alone before their hospitalisation. The two groups were broadly similar for sociodemographic variables. There were differences between the two arms of the trial in terms of the EuroQol EQ-5D score, however, with hospital at home patients reporting lower levels of overall health than the hospital patients. To correct for these observed differences, all subsequent analyses of EQ-5D were adjusted for the relevant baseline assessment. Similar adjustments were made for the COOP-WONCA charts. Potentially, the most important aspect that differed markedly between the groups was that a main carer was identified by a higher proportion of hospital at home patients (58%) than by hospital patients (49%). Since the carers were identified before randomisation, this discrepancy occurred by chance.
Table 1.
Sociodemographic characteristics and health status of 241 patients at baseline by treatment allocated
| Rehabilitative care
|
||
|---|---|---|
| Hospital (n=81) | Hospital at home (n=160) | |
| Sociodemographic characteristics | ||
| Median (interquartile range) age (years) | 79 (74-84) | 79 (72-84) |
| No (%) women | 58 (72) | 109 (68) |
| No (%) married | 29 (36) | 60 (38) |
| No (%) retired (n=239) | 63/80 (79) | 112/159 (70) |
| No (%) living alone | 45 (56) | 82 (51) |
| No (%) identifying a main carer | 40 (49) | 93 (58) |
| No (%) in manual social classes (n=239) | 36/80 (45) | 54/159 (34) |
| Health status at randomisation | ||
| Median (interquartile range) Folstein score (n=229) | 26 (23-28) | 26 (23-28) |
| Median (interquartile range) Barthel score | 16 (14-17) | 16 (14-17) |
| No (%) with longstanding limiting disability | 34 (42) | 59 (37) |
| Median (interquartile range) EQ-5D: | ||
| Score (n=220) | 0.52 (0.26-0.69) | 0.43 (0.26-0.64) |
| Thermometer (n=196) | 65 (50-75) | 68 (50-80) |
| Median (interquartile range) COOP-WONCA chart: | ||
| Physical fitness | 5 (4-5) | 5 (4-5) |
| Feelings | 2 (1-3) | 2 (1-3) |
| Daily activities | 4 (3-5) | 4 (2-5) |
| Social activities | 3 (1-4) | 2 (1-4) |
| Change in health | 2 (1-3) | 2 (1-3) |
| Overall health | 3 (3-4) | 3 (3-4) |
| Pain | 3 (2-4) | 4 (2-4) |
Those patients who refused consent to participate in the trial were of broadly similar age distribution to those who did participate (table 1), with a median age of 78 years (interquartile range 68-83 years). A higher proportion of those who refused consent were female (80%) compared with those who participated.
Outcome measures
Mortality
—By the 3 month follow up, 18 patients (7%) had died, and these deaths were distributed proportionately across the two arms of the trial (12 hospital at home patients, 6 hospital patients; 95% confidence interval for difference in mortality −7% to 7%).
Length of stay
after randomisation was significantly longer in the hospital at home scheme (table 2). Based on the geometric means, the length of stay after randomisation in the hospital group was 62% of that in the hospital at home group (51% to 75%; P<0.0001).
Table 2.
Length of stay in rehabilitative care after randomisation among 237 patients by treatment allocated
| Rehabilitative care
|
||
|---|---|---|
| Length of stay (days) | Hospital (n=79) | Hospital at home (n=158) |
| Mean | 12.2 | 16.8* |
| Median | 9.0 | 14.0 |
| Geometric mean | 8.6 | 14.0 |
Mean length of stay for hospital at home patients comprises a mean of 2.8 days in hospital after randomisation plus a mean of 12.8 days in hospital at home plus a mean of 0.9 days in hospital due to readmission from hospital at home scheme (based on 152 patients for whom it was possible to subdivide data).
Functional ability
—Table 3 shows the changes in total Barthel scores between the baseline and each of the follow up assessments, the positive differences indicating improvement. Repeated measures analysis of variance showed no significant difference between the two arms of the trial in terms of changes in functional ability over time (P=0.19). After adjustment for baseline values, the differences in Barthel score between the groups (hospital minus hospital at home) was −0.33 (−1.20 to 0.54) at 4 weeks and 0.17 (−0.76 to 1.10) at 3 months.
Table 3.
Changes in functional ability (Barthel index score) among 241 patients from baseline to follow up, at 4 weeks and 3 months, by rehabilitative care allocated
| Time period | Hospital care
|
Hospital at home care
|
|||
|---|---|---|---|---|---|
| No of patients | Mean (SD) change in total Barthel score* | No of patients | Mean (SD) change in total Barthel score* | ||
| Baseline to 4 weeks | 69 | 1.0 (2.82) | 152 | 1.5 (2.93) | |
| Baseline to 3 months | 60 | 1.7 (2.68) | 141 | 1.9 (3.22) | |
Possible range of score 0-20.
Quality of life
—Table 4 shows changes in the EQ-5D and thermometer scores at 4 weeks and 3 months, with positive differences being in favour of the hospital at home group. Again there were no significant differences between the two groups. Similar results were observed for the COOP-WONCA charts (table 5), although the difference for the daily activities chart approached significance at the 5% level. For the pain chart, the analysis of which formed part of a nested trial reported elsewhere,18 analysis of absolute values at follow up showed no significant differences at either 4 weeks (P=0.55) or 3 months (P=0.99).
Table 4.
Differences between mean EQ-5D and thermometer scores of patients allocated hospital at home care and those of patients allocated hospital care after adjustment for baseline assessments*
| Difference (95% CI )† | P value‡ | |
|---|---|---|
| EQ-5D score§: | ||
| At 4 weeks’ follow up | 0.00 (−0.09 to 0.10) | 0.20 |
| At 3 months’ follow up | −0.04 (−0.13 to 0.06) | |
| Thermometer¶: | ||
| At 4 weeks’ follow up | −1.9 (−7.9 to 4.1) | 0.47 |
| At 3 months’ follow up | −4.6 (−11.0 to 2.0) |
From (separate) univariate analyses of covariance for the two follow up assessments.
Scores for hospital at home care minus those for hospital care.
From (a single) multivariate repeated measures analysis of variance.
Possible range 5-15.
Possible range 0-100.
Table 5.
Differences between mean COOP-WONCA chart scores of patients allocated hospital at home care and those of patients allocated hospital care, after adjustment for baseline assessments*
| Difference (95% CI)†
|
|||
|---|---|---|---|
| COOP-WONCA scores‡ | At 4 weeks’ follow up | At 3 months’ follow up | P value§ |
| Physical fitness | −0.02 (−0.20 to 0.17) | −0.05 (−0.28 to 0.19) | 0.83 |
| Feelings | 0.25 (−0.09 to 0.59) | −0.09 (−0.50 to 0.32) | 0.54 |
| Daily activities | 0.51 (0.13 to 0.89) | −0.04 (−0.47 to 0.38) | 0.054 |
| Social activities | 0.10 (−0.35 to 0.54) | 0.07 (−0.38 to 0.52) | 0.90 |
| Change in health | 0.08 (−0.24 to 0.41) | −0.01 (−0.34 to 0.31) | 0.58 |
| Overall health | 0.14 (−0.12 to 0.40) | 0.10 (−0.21 to 0.42) | 0.86 |
From (separate) univariate analyses of covariance for the two follow up assessments.
Scores for hospital at home care minus those for hospital care.
Possible range 1-5.
From (a single) multivariate repeated measures analyses of variance.
Patient satisfaction
—As most patient responses to the five point Likert scales of patient satisfaction were in the top two categories (for example, “good” and “excellent”), we compared the proportions in the highest category in the two treatment arms (table 6, with positive differences in favour of hospital at home). We found significant differences between the groups for only one of the 11 questions at 4 weeks (“discussions with staff”), which was in favour of the hospital at home patients. The confidence intervals were often quite wide. A similar pattern was observed in the patient satisfaction questionnaires at 3 months (data not shown).
Table 6.
Patients’ satisfaction with care received expressed at 4 week follow up (values are percentages unless stated otherwise)
| Rehabilitative care
|
Difference (95% CI) | P value | ||
|---|---|---|---|---|
| Hospital (n=70) | Hospital at home (n=155) | |||
| Quality of service (excellent) | 44.6 | 50.7 | 6.1 (−8.6 to 20.8) | 0.49* |
| Received needed services (all of the time) | 60.0 | 63.0 | 3.0 (−11.5 to 17.4) | 0.81* |
| Content with care (all of the time) | 56.9 | 69.6 | 12.7 (−1.6 to 27.0) | 0.12* |
| Received all help needed (yes) | 75.4 | 83.8 | 8.4 (−3.7 to 20.6) | 0.15† |
| Discussions with staff (excellent) | 27.7 | 47.4 | 19.7 (5.9 to 33.5) | 0.024* |
| Involved in decision making (as much as wanted) | 71.7 | 79.4 | 7.7 (−5.7 to 21.1) | 0.41‡ |
| Information about illness (as much as wanted) | 80.0 | 76.7 | −3.3 (−15.7 to 9.2) | 0.75‡ |
| Information on treatment (as much as wanted) | 80.7 | 77.5 | −3.2 (−11.2 to 17.8) | 0.77‡ |
| Privacy (as much as wanted) | 88.1 | 84.7 | −3.4 (−13.7 to 6.9) | 0.88‡ |
| Informal practical support (as much as wanted) | 93.2 | 87.0 | −6.2 (−14.8 to 2.4) | 0.73‡ |
| Informal emotional support (as much as wanted) | 96.6 | 93.9 | −2.7 (−8.9 to 3.5) | 0.92‡ |
Mann-Whitney U test. †χ2 test. ‡Fisher’s exact test.
Discussion
This study compared the effectiveness and acceptability of early discharge to a hospital at home scheme with that of routine hospital care. There were few significant differences between routine hospital care and the hospital at home scheme across a wide range of outcomes. Specifically, there were no differences in terms of mortality, functional ability, quality of life, and most measures of satisfaction at the 4 week and 3 month follow ups.
The main significant difference between the two forms of care was the length of stay after randomisation. The geometric mean of the length of stay in the hospital group was 62% of that in the hospital at home group (95% confidence interval 51% to 75%; P<0.0001). Caution is needed in interpreting this result with regard to its implications for cost. The length of stay after randomisation represented the time during which a patient was supervised by a service. In hospital this is indicative of bed occupancy and hence is strongly related to cost. However, hospital at home care can be of variable intensity, tailing off towards the end of an episode of care, and, therefore, length of stay may be less strongly related to cost. The observed differences in length of stay are of obvious importance in terms of resource allocation within acute care, and a full economic evaluation of these data is reported elsewhere.19
At the 4 week follow up, the patients receiving hospital at home care reported significantly higher levels of perceived involvement in decisions pertaining to their care than did the hospital patients. By the 3 month follow up, however, there were no differences in levels of patient satisfaction. As this was the only significant result in the context of multiple statistical tests, it should be viewed with caution. The remaining measures of patient satisfaction were similar in the two treatment arms. The widths of confidence intervals for the data on patient satisfaction were quite broad, however, which suggests that the sample size (based on expected length of stay) may not be sufficiently large to identify important differences in acceptability between the two groups.
Limitations of study
For the small subgroup of patients (43 in total) undergoing elective procedures, randomisation to treatment occurred before the baseline interview. Thus, it was not possible to fully blind patients or interviewer to the treatment during the baseline interview. Further, for all patients it was not possible to blind the interviewer during the follow up interviews.
The hospital at home team under evaluation admitted patients with a wide range of diagnoses. However, the sample size of individual groups (including elective admissions) was too small to detect clinically important differential effects.
There was a limited choice of outcome measures for rehabilitation in an elderly population. We selected the Barthel index because of its wide use in rehabilitative clinical practice, but it has the disadvantage that it is relatively insensitive to change, particularly at the top end of the scale.
For every two patients discharged early to the hospital at home scheme, one patient remained in hospital for routine discharge. Thus, there may have been periods when the scheme was underused. This is likely to have most impact on the economic analysis, but it could also explain, in part, the increased length of stay in the hospital at home group. During the trial, the workload of the hospital at home team might not have been as intense as it would have been without the concurrent evaluation, and therefore the impetus to discharge patients from the scheme might have been less.
Conclusions
In terms of effectiveness and acceptability, our study does not indicate that one scheme is substantially preferable to the other. However, the decision to implement an early discharge, hospital at home scheme for emergency and elective patients should not be made purely on effectiveness grounds; costs are clearly also important, and we report on these in the associated paper.19 More research into the most appropriate case mix and size of hospital at home schemes is required.
Figure.
Passage of patients through trial of hospital at home scheme
Acknowledgments
We thank the staff of the Frenchay Healthcare Trust and the Avon Orthopaedic Centre at Southmead Hospital, whose cooperation was essential. We also thank Maggie Somerset, Margaret Evans, and Sara Brookes (department of social medicine, University of Bristol) for their valuable assistance with data collection. The department of social medicine at the University of Bristol is part of the MRC Health Services Research Collaboration.
Footnotes
Funding: The study was funded by the South and West National Health Service Research and Development Directorate. The hospital at home team was funded by Avon Health Authority.
Conflict of interest: MAD was, and still is, employed as a member of the hospital at home scheme.
References
- 1.Marks L. Home and hospital care: redrawing the boundaries. London: King’s Fund; 1990. [Google Scholar]
- 2.Coast J, Inglis A, Frankel S. Alternatives to hospital care: what are they and who should decide. BMJ. 1996;312:162–166. doi: 10.1136/bmj.312.7024.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Council on Scientific Affairs. Home care in the 1990s. JAMA. 1990;263:1241–1244. [PubMed] [Google Scholar]
- 4.Costain D, Warner M, eds. From hospital to home care. London: King’s Fund, 1992.
- 5.Pryor GA, Williams DRR. Rehabilitation after hip fractures. Home and hospital management compared. J Bone Joint Surg Br. 1989;71:471–473. doi: 10.1302/0301-620X.71B3.2722942. [DOI] [PubMed] [Google Scholar]
- 6.Knowelden J, Westlake L, Wright KG, Clarke SJ. Peterborough hospital at home: an evaluation. J Pub Health Med. 1991;13:182–188. doi: 10.1093/oxfordjournals.pubmed.a042616. [DOI] [PubMed] [Google Scholar]
- 7.Gould MM, Iliffe S. Hospital at home: a case study in service development. Br J Health Care Manage. 1995;1:809–812. [Google Scholar]
- 8.Closs SJ, Stewart LSP, Brand E, Currie CT. A scheme of early supported discharge for elderly trauma patients the views of patients, carers and community staff. Br J Occup Ther. 1995;58:373–376. [Google Scholar]
- 9.Fulop NJ, Hood S, Parsons S. Does the National Health Service want hospital at home? J R Soc Med. 1997;90:212–215. doi: 10.1177/014107689709000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hensher M, Fulop N, Hood S, Ujah S. Does hospital-at-home make economic sense? Early discharge versus standard care for orthopaedic patients. J R Soc Med. 1996;89:548–551. doi: 10.1177/014107689608901003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Cathain A. Evaluation of a hospital at home scheme for the early discharge of patients with fractured neck of femur. J Pub Health Med. 1994;16:205–210. doi: 10.1093/oxfordjournals.pubmed.a042958. [DOI] [PubMed] [Google Scholar]
- 12.Office of Population Censuses and Surveys, Social Survey Division. General household survey: results from the 1994 general household survey. London: HMSO; 1994. [Google Scholar]
- 13.Folstein MF, Folstein SE. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 14.Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Maryland State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 15.Collin C, Wade DT, Davies S, Horn V. The Barthel ADL index. A reliability study. Int Disabil Stud. 1988;10:61–63. doi: 10.3109/09638288809164103. [DOI] [PubMed] [Google Scholar]
- 16.Brooks R EuroQol Group. EuroQol: the current state of play. Health Pol. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 17.Scholten JHG, Van Weel C. Functional status assessment in family practice. The Dartmouth COOP functional health assessment charts/WONCA. Lelystad: MediTekst; 1992. [Google Scholar]
- 18.Peters TJ, Coast J, Richards SH, Gunnell DJ. Effect of varying the time frame for COOP-WONCA functional health status charts: a nested randomised controlled trial in Bristol, UK. J Epidemiol Community Health. 1998;52:59–64. doi: 10.1136/jech.52.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coast J, Richards SH, Peters TJ, Gunnell DJ, Pounsford JC, Darlow MA. Hospital at home or acute hospital care? A cost minimisation analysis. BMJ. 1998;316:1802–1806. doi: 10.1136/bmj.316.7147.1802. [DOI] [PMC free article] [PubMed] [Google Scholar]