Abstract
OBJECTIVE
To investigate relationships between baseline factors and treatment-associated efficacy changes in type 2 diabetes.
RESEARCH DESIGN AND METHODS
Multivariable analyses of treatment response in 1,229 type 2 diabetic patients with hypercholesterolemia who received ezetimibe/simvastatin or atorvastatin in a randomized double-blind 6-week study.
RESULTS
Increasing age was related to improvements in all lipid assessments. Men had greater triglyceride and non-HDL cholesterol reductions than women, and black/Hispanic patients had less favorable lipid effects than other races/ethnicities. Increasing baseline LDL cholesterol was associated with improvements in most lipids; higher baseline non-HDL cholesterol with improved HDL cholesterol and triglycerides; higher baseline HDL cholesterol with greater non-HDL cholesterol and high-sensitivity C-reactive protein (hs-CRP) reductions; and higher baseline hs-CRP with smaller LDL cholesterol, non-HDL cholesterol, and apolipoprotein B reductions. Patients with high baseline non-HDL cholesterol or triglycerides less frequently attained LDL cholesterol targets. Obesity was inversely related to HDL cholesterol and hs-CRP changes, and higher baseline A1C to smaller apolipoprotein B reductions. Metabolic syndrome was not a significant predictor.
CONCLUSIONS
Treatment responses in type 2 diabetic patients were related to baseline factors, although treatment effects (ezetimibe/simvastatin being more effective than atorvastatin) remained consistent. The presence of predictive factors should be considered in planning lipid-altering therapy.
Treatment response to statins can vary in patients with type 2 diabetes, attributed to various patient-related characteristics, including demographic and metabolic factors, baseline lipid levels, genetic polymorphisms, and the metabolic syndrome (MetS) (1–6). This analysis explored relationships between various baseline characteristics and changes in lipids and high-sensitivity C-reactive protein (hs-CRP) in the presence/absence of MetS in the Vytorin versus Atorvastatin in Patients With Type 2 Diabetes Mellitus and Hypercholesterolemia (VYTAL) study (7).
RESEARCH DESIGN AND METHODS
This was a post hoc analysis of the randomized double-blind 6-week VYTAL study in 1,229 type 2 diabetic patients with hypercholesterolemia who received ezetimibe/simvastatin (10/20 mg/day) versus atorvastatin (10 and 20 mg/day) or 10/40 mg ezetimibe/simvastatin versus 40 mg atorvastatin (7). Type 2 diabetic patients, 18–80 years, with A1C levels ≤8.5%, triglycerides ≤4.52 mmol/l, and LDL cholesterol levels ≥2.59 mmol/l were included.
This analysis was performed in randomized patients who had baseline and one or more postbaseline measurements (modified-intent-to-treat population) (7). Prespecified baseline factors found significant by univariate analysis for association with week 6 percent changes from baseline in lipids and hs-CRP were assessed in multivariable linear regression models using continuous and categorical variables in separate analyses. Factors were identified for inclusion in the final model using a model-based variable deletion process. Triglycerides and hs-CRP were analyzed in this model using normal-score rank transformations for percent changes. Proportions of patients attaining prespecified LDL cholesterol levels (<1.81 and <2.59 mmol/l) were assessed using similar logistic regression models.
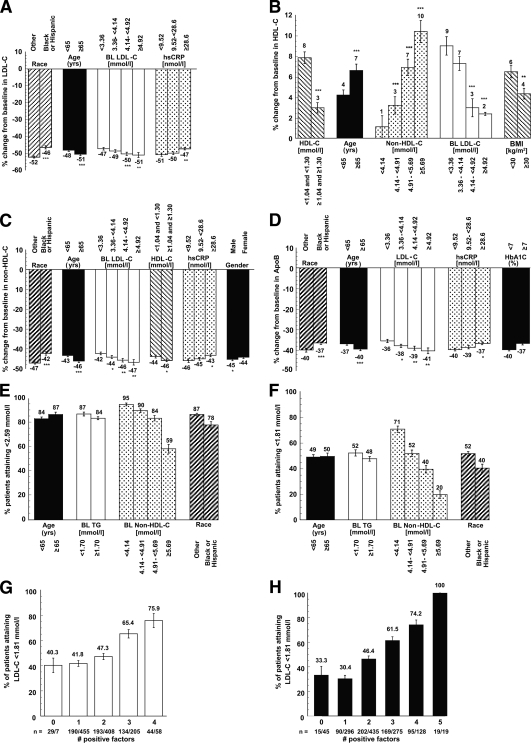
RESULTS
Baseline characteristics and levels of efficacy parameters at baseline and study end are provided in the online appendix (supplementary Tables A and B, available at http://care.diabetesjournals.org/cgi/content/full/dc09-1762/DC1) (7). Baseline factors found to be significant predictors of percent change by univariate analysis (supplementary Table C) were further assessed by multivariable analysis. Results of the analyses of baseline predictors on percent changes from baseline are displayed in Fig. 1 and supplementary Fig. S1 (categorical) and supplementary Table D (continuous). Increasing age was significantly related to all efficacy parameters analyzed except hs-CRP. Patients aged ≥65 vs. <65 years had greater reductions from baseline in LDL cholesterol, non-HDL cholesterol, apolipoprotein B, and triglycerides; better LDL cholesterol target attainment; and larger HDL cholesterol and apolipoprotein A-I increases. Black/Hispanic patients had smaller LDL cholesterol, non-HDL cholesterol, and apolipoprotein B reductions and less LDL cholesterol target attainment than white/other races/ethnicities. Men had greater triglyceride and non-HDL cholesterol reductions than women. Higher baseline LDL cholesterol was associated with greater reductions in most lipids as well as smaller HDL cholesterol increases and triglyceride reductions and increasing baseline non-HDL cholesterol with improvements in HDL cholesterol and triglycerides. Higher baseline HDL cholesterol was related to greater non-HDL cholesterol and hs-CRP reductions and smaller HDL cholesterol and apolipoprotein A-I increases. Patients with higher baseline non-HDL cholesterol or triglycerides attained LDL cholesterol targets less frequently. Higher baseline hs-CRP levels were related to smaller LDL cholesterol, non-HDL cholesterol, and apolipoprotein B reductions and larger hs-CRP reductions. Higher baseline BMI was associated with smaller HDL cholesterol increases and hs-CRP reductions and higher baseline A1C with smaller apolipoprotein B reductions. The presence of MetS had no effect. Ezetimibe/simvastatin treatment (versus atorvastatin) was associated with significantly greater improvements in all efficacy variables.
Figure 1.
Multivariable association of categorical factors with the percent change from baseline in LDL cholesterol (LDL-C) (A), HDL cholesterol (HDL-C) (B), non–HDL cholesterol (C), and apolipoprotein B (D). P values (*P < 0.05, **P < 0.01, ***P < 0.001) in A–D correspond to the significance of marked (*) category compared with lowest category for the variable. Association (logistic regression) of categorical factors with the attainment of LDL cholesterol <2.59 mmol/l (<100 mg/dl) (E) and <1.81 mmol/l (<70 mg/dl) (F) is shown. (Note: When non-HDL cholesterol was removed from the multivariable model, baseline LDL cholesterol was a significant factor for attainment of these LDL cholesterol levels, presumably because of the high correlation [r = 0.90] of baseline non-HDL cholesterol with baseline LDL cholesterol levels.) G and H: Proportion of patients who attained LDL cholesterol <1.81 mmol/l (<70 mg/dl) by the number of positive predictive factors in the multivariate model. The four baseline factors associated with LDL cholesterol <1.81 mmol/l, i.e., age ≥65 years, baseline triglycerides <1.70 mmol/l (<150 mg/dl), baseline non-HDL cholesterol <4.14 mmol/l (160 mg/dl), and race/ethnicity other than black or Hispanic, are shown in G. The four baseline factors additionally with ezetimibe/simvastatin (vs. atorvastatin) treatment are shown in H. n = the number of patients with the indicated number of positive factors in the category of all patients assessed for that number. To convert mmol/l to mg/dl, divide by 0.0259. BL, baseline. TG, triglyceride.
The likelihood of attaining LDL cholesterol <1.81 mmol/l was related to the number of positive predictive baseline factors (Fig. 1G and H). Approximately 31% of patients with zero or one factor achieved LDL cholesterol <1.81 mmol/l compared with 46.4% with two factors, 61.5% with three factors, 74.2% with four factors, and 100% with all five factors. Without the treatment factor in the model, 41.6% with zero to one factor and 75.9% with all four factors achieved LDL cholesterol <1.81 mmol/l.
CONCLUSIONS
In this study, age and race/ethnicity significantly predicted LDL lowering, consistent with previous findings in statin-treated patients (4,5,8). These effects were not attributable to differences in study therapy adherence, which was high for both age (98.1–98.2%) and race/ethnicity (95.9–98.7%) subgroups. Alterations in LDL metabolism (e.g., diminished VLDL particle production) may account for the more robust therapeutic LDL cholesterol lowering in older patients (9,10). Attenuated LDL cholesterol–lowering responses in black patients after statin treatment have been linked to single-nucleotide polymorphisms in HMG-CoA reductase (11). The age-associated HDL cholesterol increases observed in this study may reflect altered HDL-mediated cholesterol efflux and/or other physiological functions in older patients (12).
The diminished LDL cholesterol–lowering response observed in hypertriglyceridemic patients may be attributed to the increased prevalence of small dense LDL particles in these patients that bind less effectively to LDL receptors (5,6). Higher baseline HDL cholesterol levels were negatively related to percent change from baseline in HDL cholesterol, as reported previously (5). Whether MetS provides greater clinical value than its individual components is debated (13). In this analysis, factors that contribute to MetS (BMI, A1C, triglycerides, HDL cholesterol) and the inflammatory marker hs-CRP were significant predictors of lipid changes; however, MetS itself was not related to treatment responses, although there were relatively few subjects without MetS (2,3,6). Higher baseline hs-CRP levels were associated with attenuated LDL cholesterol lowering, an effect not previously noted to our knowledge, and perhaps related to heightened levels of inflammation (9). Obesity-related changes in HDL cholesterol metabolism may account for the smaller HDL cholesterol increases associated with higher BMI (5,14). Because adipose tissue inflammation in obese patients may strongly influence hs-CRP levels, smaller hs-CRP reductions observed in obese patients could reflect lesser statin effectiveness in suppressing adipose versus vascular sources of inflammation (6,9). The association between increasing baseline A1C and smaller apolipoprotein B reductions may be related to the presence of small dense LDL particles in these patients that vary inversely with A1C levels (15).
When considered cumulatively, the baseline factors positive for treatment response, namely age ≥65 years, baseline triglycerides <1.7 mmol/l, baseline non-HDL cholesterol <4.14 mmol/l, and race/ethnicity other than black/Hispanic, predicted attainment of LDL cholesterol <1.81 mmol/l irrespective of treatment. These results indicated that black or Hispanic subjects, individuals aged <65 years, and patients with elevated triglycerides and non-HDL cholesterol levels may require more intensive therapy to attain LDL cholesterol goal than patients without these factors.
It should be noted this exploratory analysis had limited statistical power, and some observations may have been influenced by chance variation because of multiple comparisons. Nonetheless, several observations, notably the impact of age and race/ethnicity, are consistent with previous statin studies. In summary, patient-related characteristics can influence efficacy in type 2 diabetic patients with hypercholesterolemia after ezetimibe/simvastatin and atorvastatin treatment. These factors, and particularly the collective presence of positive predictors, should be considered in planning lipid-altering therapies in these patients.
Supplementary Material
Acknowledgments
Funding for this study was provided by Merck/Schering-Plough Pharmaceuticals, North Wales, Pennsylvania. The study sponsor, Merck & Co., facilitated the design and conduct of the study and collection and analysis of the study data.
All authors jointly developed the manuscript content and were involved in at least one of the following: conception, design, data acquisition, analysis, statistical analysis, interpretation of data, drafting the manuscript, and/or revising the manuscript for important intellectual content. All authors provided final approval of the version to be published. Editorial assistance was provided by Stephen W. Gutkin, Rete Biomedical Communications (Wyckoff, NJ).
R.B.G., J.R.G., T.M., and R.S.W. were investigators in the VYTAL study and have received honoraria from Merck/Schering-Plough Pharmaceuticals. R.B.G. has received research grants and honoraria from Merck & Co., Merck-Schering-Plough, Takeda, Abbott, GlaxoSmithKline, and Dalichi-Sankyo and has served on the speaker's bureaus and as a consultant and/or advisory board member for those companies. J.R.G. has received grant support and honoraria from Merck & Co., Pfizer, Schering-Plough Pharmaceuticals, and Abbott and has served on an advisory board for Schering-Plough Pharmaceuticals. T.M. has received honoraria from Merck & Co., has served on Merck's speaker's bureau, has received grant support from Takeda, and has served as a consultant for Merck & Co., Abbott, and Takeda. R.S.W. has participated in clinical trials sponsored by Biodel, Eli Lilly, Pfizer, GlaxoSmithKline, Merck & Co., and Novartis, has received research grants/support from Merck & Co. and Pfizer and honoraria from Merck & Co. A.B.P., J.E.T., and A.M.T. are employees of Merck & Co. and own stock and/or stock options in the company. D.T. provided statistical analysis support funded by Merck/Schering-Plough Pharmaceuticals. No other potential conflicts of interest relevant to this article were reported.
Parts of this study were previously presented at the 68th Scientific Sessions of the American Diabetes Association, 6–10 June 2008, San Francisco, California.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ: the National Heart, Lung, and Blood Institute, the American College of Cardiology Foundation, the American Heart Association. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004; 110: 227– 239 [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA, Costa F: the American Heart Association, the National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735– 2752 [DOI] [PubMed] [Google Scholar]
- 3.Brunzell JD, Davidson M, Furberg CD, Goldberg RB, Howard BV, Stein JH, Witztum JL: the American Diabetes Association, the American College of Cardiology Foundation. Lipoprotein management in patients with cardiometabolic risk: consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care 2008; 31: 811– 822 [DOI] [PubMed] [Google Scholar]
- 4.Simon JA, Lin F, Hulley SB, Blanche PJ, Waters D, Shiboski S, Rotter JI, Nickerson DA, Yang H, Saad M, Krauss RM: Phenotypic predictors of response to simvastatin therapy among African-Americans and Caucasians: the Cholesterol and Pharmaeogenetics (CAP) Study. Am J Cardiol 2006; 97: 843– 850 [DOI] [PubMed] [Google Scholar]
- 5.Streja L, Packard CJ, Shepherd J, Cobbe S, Ford I: the WOSCOPS Group. Factors affecting low-density lipoprotein and high-density lipoprotein cholesterol response to pravastatin in the West of Scotland Coronary Prevention Study (WOSCOPS). Am J Cardiol 2002; 90: 731– 736 [DOI] [PubMed] [Google Scholar]
- 6.Caslake MJ, Packard CJ: Phenotypes, genotypes and response to statin therapy. Curr Opin Lipidol 2004; 15: 387– 392 [DOI] [PubMed] [Google Scholar]
- 7.Goldberg RB, Guyton JR, Mazzone T, Weinstock RS, Polis A, Edwards P, Tomassini JE, Tershakovec AM: Ezetimibe/simvastatin vs atorvastatin in patients with type 2 diabetes mellitus and hypercholesterolemia: the VYTAL study. Mayo Clinic Proceedings2006; 81: 1579– 1588 [DOI] [PubMed] [Google Scholar]
- 8.Shear CL, Franklin FA, Stinnett S, Hurley DP, Bradford RH, Chremos AN, Nash DT, Langendorfer A: Expanded Clinical Evaluation of Lovastatin (Excel) study results: effect of patient characteristics on lovastatin-induced changes in plasma-concentrations of lipids and lipoproteins. Circulation 1992; 85: 1293– 1303 [DOI] [PubMed] [Google Scholar]
- 9.Diabetes Prevention Program Research Group. Lipid, lipoproteins, C-reactive protein, and hemostatic factors at baseline in the Diabetes Prevention Program. Diabetes Care 2005; 28: 2472– 2479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ericsson S, Berglund L, Frostegård J, Einarsson K, Angelin B: The influence of age on low density lipoprotein metabolism: effects of cholestyramine treatment in young and old healthy male subjects. J Intern Med 1997; 242: 329– 337 [DOI] [PubMed] [Google Scholar]
- 11.Krauss RM, Mangravite LM, Smith JD, Medina MW, Wang D, Guo X, Rieder MJ, Simon JA, Hulley SB, Waters D, Saad M, Williams PT, Taylor KD, Yang H, Nickerson DA, Rotter JI: Variation in the 3- hydroxyl-3-methylglutaryl coenzyme a reductase gene is associated with racial differences in low-density lipoprotein cholesterol response to simvastatin treatment. Circulation 2008; 117: 1537– 1544 [DOI] [PubMed] [Google Scholar]
- 12.Berrougui H, Isabelle M, Cloutier M, Grenier G, Khalil A: Age-related impairment of HDL-mediated cholesterol efflux. J Lipid Res 2007; 48: 328– 336 [DOI] [PubMed] [Google Scholar]
- 13.Deedwania P, Barter P, Carmena R, Fruchart JC, Grundy SM, Haffner S, Kastelein JJ, LaRosa JC, Schachner H, Shepherd J, Waters DD: the Treating to New Targets Investigators. Reduction of low-density lipoprotein cholesterol in patients with coronary heart disease and metabolic syndrome: analysis of the Treating to New Targets study. Lancet 2006; 368: 919– 928 [DOI] [PubMed] [Google Scholar]
- 14.Rashid S, Genest J: Effect of obesity on high-density lipoprotein metabolism. Obesity 2007; 15: 2875– 2888 [DOI] [PubMed] [Google Scholar]
- 15.Lee W, Min WK, Chun S, Jang S, Kim JQ, Lee DH, Park JY, Park H, Son JE: Low-density lipoprotein subclass and its correlating factors in diabetics. Clin Biochem 2003; 36: 657– 661 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.