Abstract
OBJECTIVE
Individuals with diabetes are at higher risk for depression than the general population. Although depression can be treated with antidepressant medications, patients with diabetes and comorbid depression often go untreated. The goal of this study was to examine racial disparities in the treatment of depression with antidepressant medication in the southeastern U.S.
RESEARCH DESIGN AND METHODS
Cross-sectional data were collected at baseline from 69,068 participants (71% African American, 60% female, and 82% with incomes <$25,000) recruited from community health centers and enrolled in the Southern Cohort Community Study (SCCS). The SCCS is a prospective epidemiological cohort study designed to explore causes of health disparities in adults aged 40–79 years. Binary logistic regression was used to identify factors associated with antidepressant use among those with diabetes (n = 14,279).
RESULTS
Individuals with diagnosed diabetes (14,279) were classified with no depressive symptoms (54.7%), or with mild (24.2%), moderate (12.8%), or severe depressive symptoms (8.3%). After controlling for sex, age, insurance, income, education, BMI, smoking status, alcohol consumption, and level of depression, African Americans with diabetes were much less likely to report taking antidepressant medication than whites (adjusted odds ratio 0.32 [95% CI 0.29–0.35], P < 0.0001).
CONCLUSIONS
Antidepressant use is much less common among African Americans than among whites with diabetes. Reasons for racial disparities in treatment of depressive symptoms are unclear but may include a combination of differential diagnosis and treatment by health professionals as well as cultural differences in seeking help for emotional distress.
Depression is one of the most common psychiatric disorders. Almost one of every five people in the U.S. will experience a major depressive episode during their lifetime. Individuals with diabetes are as much as twice as likely as those without diabetes to experience depression (1). Despite its relevance to the course of diabetes, it is estimated that depression is recognized and treated in <25–50% of individuals with diabetes who are depressed (2). Women are more likely to be recognized (1), as are those with panic attacks, frequent primary care visits, and poorer health (3). Less is known about the identification of depression in specific racial and ethnic groups with diabetes. Variation in the identification of depression might explain noted racial/ethnic disparities in diabetes outcomes (i.e., why, on average, African Americans have worse control of their disease, and experience more diabetes-related complications and mortality than whites do).
In diabetes, comorbid depression has been associated with difficulty performing diabetes self-care behaviors (4), worse glycemic control (5–7), and adverse health outcomes (8). In large cohort studies, comorbid depression was associated with a 36–38% increased risk in all-cause mortality compared with that in individuals with diabetes alone (9); in a separate cohort study, it was associated with a 1.3-fold increase risk in all-cause mortality (10). The human toll of diabetes and depression translates into a 50% increase in health care costs compared to the cost of treating diabetes alone (8).
The successful treatment of depression may reduce health care costs (11) by improving glycemic control, overall functioning, and the quality of life of individuals with diabetes (2). Studies show that psychotherapeutic and pharmacological treatment is effective for patients with diabetes and comorbid depression (12). Such treatment has been associated with a reduction in depressive symptoms (6) and improvements in glycemic control (5–7) and may ultimately reduce the risk of adverse health outcomes associated with depression and diabetes.
In an effort to reduce and eventually eliminate well-documented racial/ethnic disparities in diabetes outcomes, it is important to know whether certain racial/ethnic groups with diabetes and comorbid depression are differentially identified and/or treated for depression. In this study, we investigated racial variation in self-reported 1) physician-diagnosed diabetes, 2) the presence and severity of depressive symptoms, and 3) the treatment for depression in a large cohort of low-income adults with diabetes.
RESEARCH DESIGN AND METHODS
The Southern Community Cohort Study (SCCS) is a prospective cohort study designed to identify causes of health disparities between African Americans and whites in the incidence and mortality rates of several cancers and other chronic diseases (13). The study was approved by the institutional review boards at Vanderbilt University and Meharry Medical College. Participants were enrolled in person at Community Health Centers (CHCs) in the states of Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia. Participants were enrolled by approaching people entering the CHCs (patients and individuals accompanying patients) and screening them for eligibility and interest in study participation. Participants were required to be between the ages of 40 and 79, to speak English, and to not have been treated for cancer (excluding nonmelanoma skin cancer) within the past year. After providing informed consent, trained interviewers collected baseline data using a computer-assisted personal interview. The baseline interview contained questions on demographic information, medical history, family history, environmental and occupational exposures, diet, physical activity, and psychosocial variables.
Measures
Depression.
Depressive symptoms were assessed using a 10-item version of the Centers for Epidemiological Studies Depression (CES-D) scale, a valid and reliable measure of the presence and severity of depressive symptoms (14). Cutoffs of 10, 15, and 20 define mild, moderate, and severe levels of depressive symptoms (14). The CES-D has demonstrated measurement equivalency in samples with differential characteristics including race and sex (15).
Antidepressant use.
Participants were asked if they were taking any antidepressant medication or antianxiety medication and then asked for the name(s) of all medications of this type being taken.
Selection of subjects for analysis
The initial dataset consisted of 69,068 individuals. Individuals with missing values for BMI (n = 1,575), education (n = 45), income (n = 736), smoking status (n = 100), marital status (n = 8), insurance (n = 336), and alcohol consumption (n = 310) and those who were aged <40 years (n = 2), had a depressive symptoms score (n = 99), did not answer the question about having diabetes or hypertension (n = 53), or did not answer the question about using antidepressants (n = 37) were excluded, resulting in 65,767 individuals selected for analysis. Participants with diabetes were identified using the question, “Has a doctor ever told you that you have diabetes?” Participants who answered “yes” to this question were selected for analysis, consisting of 21.7% of the original sample or 14,279 individuals. In two validation studies, one involving a review of medical records and the other assessing A1C percentages, the self-reported diagnoses were confirmed for 98% of those reporting diabetes (16).
Statistical analysis
Data were analyzed using means, frequencies, and cross-tabulations to calculate descriptive statistics. The main study hypothesis was tested using binary logistic regression analysis. Antidepressant use was coded as absent = 0 and present = 1 and served as the dependent variable. The model was built in three steps. In step 1, sex, age, insurance status, income, education, BMI, smoking status, and alcohol consumption were entered. In step 2, level of depressive symptoms (no depressive symptoms, mild depressive symptoms, moderate depressive symptoms, or severe depressive symptoms) was entered. In the final step, race was coded into three categories (whites, African Americans, and others/mixed race) and was entered into the regression model, with whites used as the reference group for calculating odds ratios (ORs). In the same model, two-way interactions between race and the other predictor variables were also examined. This analytic strategy tested whether rates of antidepressant use differed for African Americans and others/mixed race relative to whites after controlling for sex, age, insurance status, income, education, BMI, smoking status, alcohol consumption, and level of depressive symptoms. All analyses were done using SPSS (version 17.0; SPSS, Chicago, IL).
RESULTS
Description of the sample
The mean ± SD age of the sample with diabetes was 54.5 ± 9.0, with African Americans being slightly but significantly younger (P < 0.0001) than whites (54.2 vs. 55.4 years). Table 1 provides a description of the 14,279 participants who reported a diabetes diagnosis stratified by race. Level of income reported in this sample was very low, with ≥61% of each race/ethnicity subgroup reporting <$15,000 per year in family income. There were significant racial differences in the crude (i.e., unadjusted) demographic variables. Specifically, insurance status, income, education, BMI, smoking status, alcohol consumption, depressive symptoms, and antidepressant use differed by race. African Americans were more likely to report having health insurance, incomes of <$15,000, dropping out of high school, lower BMI levels, never having smoked, and consuming more alcohol on a daily basis than whites or others/mixed race. African Americans were more likely to have no depressive symptoms, whereas whites and others/mixed race were more likely to have moderate and severe depressive symptoms. Finally, among participants reporting diabetes, 17.4% of African Americans reported using antidepressant medications compared with 39.0% of whites and 31.3% of individuals of other/mixed race.
Table 1.
Characteristics of 14,279 participants in the SCCS reporting a diagnosis of diabetes
| Variable and categories | White only |
African American only |
Others/mixed race |
|||
|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | Frequency | % | |
| n | 3,552 | 10,164 | 563 | |||
| Sex (P < 0.057) | ||||||
| Male | 1,136 | 32.0 | 3,419 | 33.6 | 205 | 36.4 |
| Female | 2,416 | 68.0 | 6,745 | 66.4 | 358 | 63.6 |
| Age (P < 0.0001) | ||||||
| 40–49 years | 1,072 | 30.2 | 3,469 | 34.1 | 176 | 31.3 |
| 50–59 years | 1,304 | 36.7 | 3,954 | 38.9 | 235 | 41.7 |
| 60–69 years | 919 | 25.9 | 2,046 | 20.1 | 119 | 21.1 |
| 70–79 years | 257 | 7.2 | 695 | 6.8 | 33 | 5.9 |
| Insured (P = 0.001) | ||||||
| Yes | 2,246 | 63.2 | 6,771 | 66.6 | 365 | 64.8 |
| No | 1,306 | 36.8 | 3,393 | 33.4 | 198 | 35.2 |
| Income (P < 0.0001) | ||||||
| <$15,000 | 2,241 | 63.1 | 6,673 | 65.7 | 343 | 60.9 |
| $15,000–$24,999 | 720 | 20.3 | 2,165 | 21.3 | 127 | 22.6 |
| $25,000–$49,999 | 416 | 11.7 | 1,026 | 10.1 | 62 | 11.0 |
| ≥$50,000 | 175 | 4.9 | 300 | 3.0 | 31 | 5.5 |
| Education (P < 0.0001) | ||||||
| Less than high school | 1,188 | 33.4 | 3,936 | 38.7 | 188 | 33.4 |
| High school or GED | 1,415 | 39.8 | 3,826 | 37.6 | 166 | 29.5 |
| Some college or votech school | 636 | 17.9 | 1,650 | 16.2 | 147 | 26.1 |
| Graduated from college | 229 | 6.4 | 527 | 5.2 | 43 | 7.6 |
| Graduate or professional school | 84 | 2.4 | 225 | 2.2 | 19 | 3.4 |
| BMI category (P < 0.0001) | ||||||
| Underweight (<18.5) | 45 | 1.3 | 149 | 1.5 | 5 | 0.9 |
| Normal (18.5–24.9) | 300 | 8.4 | 1,031 | 10.1 | 55 | 9.8 |
| Overweight (25–29.9) | 743 | 20.9 | 2,415 | 23.8 | 136 | 24.2 |
| Obese-I (30–34.9) | 934 | 26.3 | 2,665 | 26.2 | 150 | 26.6 |
| Obese-II (35–39.9) | 700 | 19.7 | 1,920 | 18.9 | 109 | 19.4 |
| Obese-III (≥40) | 830 | 23.4 | 1,984 | 19.5 | 108 | 19.2 |
| Smoking status (P < 0.0001) | ||||||
| Never | 1,286 | 36.2 | 4,368 | 43.0 | 183 | 32.5 |
| Former smoker | 1,160 | 32.7 | 2,704 | 26.6 | 197 | 35.0 |
| Current smoker | 1,106 | 31.1 | 3,092 | 30.4 | 183 | 32.5 |
| Alcohol consumption (P < 0.0001) | ||||||
| Never | 2,448 | 68.9 | 6,339 | 62.4 | 356 | 63.2 |
| <1 drink/day | 909 | 25.6 | 2,577 | 25.4 | 156 | 27.7 |
| 1–3 drinks/day | 108 | 3.0 | 742 | 7.3 | 32 | 5.7 |
| ≥4 drinks/day | 87 | 2.4 | 506 | 5.0 | 19 | 3.4 |
| Depressive symptoms (P < 0.0001) | ||||||
| None | 1,764 | 49.7 | 5,785 | 56.9 | 264 | 46.9 |
| Mild | 808 | 22.7 | 2,502 | 24.6 | 142 | 25.2 |
| Moderate | 551 | 15.5 | 1,191 | 11.7 | 89 | 15.8 |
| Severe | 429 | 12.1 | 686 | 6.7 | 68 | 12.1 |
| Antidepressant (P < 0.0001) | ||||||
| Present | 1,385 | 39.0 | 1,770 | 17.4 | 176 | 31.3 |
| Absent | 2,167 | 61.0 | 8,394 | 82.6 | 387 | 68.7 |
χ2 test for categorical variables. GED, general education degree. Votech, vocational/technical.
Disparities in antidepressant use
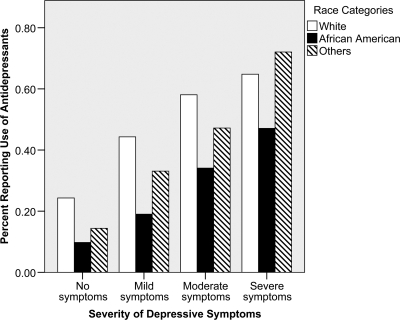
Figure 1 presents a bar graph of the rates of antidepressant use stratified by race. There were disparities in antidepressant use at all levels of depressive symptoms. Whites and others/mixed race were more likely to report using antidepressants than African Americans, regardless of the severity of depressive symptoms.
Figure 1.
Depressive symptoms and antidepressant use by racial group.
Table 2 presents the results (ORs and 95% confidence limits) of the logistic regression analysis predicting antidepressant use. Sex and health insurance status were strong predictors of antidepressant use, with women and insured individuals being approximately twice as likely to be taking antidepressants as men and uninsured individuals. Usage tended to decrease with advancing age and increasing income but rose with education and (slightly) with increasing BMI. Use of antidepressant medications was also positively associated with smoking, with former smokers being 1.21 times and current smokers being 1.46 times more likely to report antidepressant use than participants who had never smoked, but inversely associated with alcohol consumption. As expected, use of antidepressant medications was strongly associated with the level of depressive symptoms. Participants with severe symptoms were 6.55 times more likely to be taking antidepressants than those with the lowest level of depressive symptoms.
Table 2.
Logistic regression predicting antidepressant use from sex, age, insurance status, income, education, BMI, smoking status, alcohol consumption, severity of depressive symptoms, and race
| Predictor | OR (95% CI) |
|---|---|
| Female (male)* | 1.93 (1.74–2.14) |
| Age | 0.98 (0.97–0.98) |
| Uninsured (insured) | 0.54 (0.49–0.60) |
| Income (<$15,000) | |
| $15,000–$25,000 | 0.72 (0.65–0.81) |
| $25,000–$50,000 | 0.62 (0.53–0.72) |
| ≥$50,000 | 0.48 (0.36–0.63) |
| Education (dropout) | |
| High school or GED | 1.14 (1.03–1.27) |
| Some college or votech school | 1.62 (1.43–1.84) |
| Graduated from college | 1.77 (1.45–2.16) |
| Graduate or professional school | 1.77 (1.29–2.44) |
| BMI | 1.01 (1.00–1.01) |
| Smoking status (never) | |
| Former smoker | 1.21 (1.08–1.35) |
| Current smoker | 1.46 (1.31–1.63) |
| Alcohol consumption (never) | |
| <1 drink/day | 0.99 (0.90–1.10) |
| 1–3 drinks/day | 0.74 (0.60–0.90) |
| ≥4 drinks/day | 0.83 (0.65–1.05) |
| Depressive symptoms (none) | |
| Mild | 2.18 (1.96–2.42) |
| Moderate | 4.24 (3.75–4.78) |
| Severe | 6.55 (5.68–7.56) |
| Race (white only) | |
| African American only | 0.32 (0.29–0.36) |
| Other/mixed race | 0.63 (0.51–0.78) |
Data are OR (95% CI). GED, general education degree.
*Reference group used to calculate ORs is in parentheses. Votech, vocational/technical.
After controlling for these variables, race was significantly associated with antidepressant use (P < 0.0001). African Americans were 0.32 times as likely and others/mixed race were 0.63 times as likely to be taking antidepressants than whites. There were significant interactions for race and income (P = 0.004), race and smoking status (P = 0.001), and race and level of depressive symptoms (P = 0.009). An examination of these interactions showed that the direction of the effect was always consistent, with only a modest change in the magnitude of the effect across the various strata.
CONCLUSIONS
We investigated the relationship between racial status and antidepressant use in a large low-income cohort of individuals with diabetes. Although rates of antidepressant use increased as levels of depressive symptoms increased, a large number of individuals with moderate and severe depressive symptoms were not being treated with antidepressant medication. There was a racial disparity in the use of antidepressants at all levels of depressive symptoms. After adjustment for confounders, for every 10 white participants only 3 African American participants were likely to receive antidepressant medications. The prevalence of antidepressant use was consistently lowest for African Americans, even after controlling for factors that interacted with racial status (e.g., income, smoking, and severity of depressive symptoms).
The present study was conducted among a diverse sample of adults receiving care from CHCs in the southeastern U.S. Two other studies performed in other regions of the U.S. also reported racial disparities in antidepressant medication use among persons with diabetes (17,18). However, to our knowledge, our study is the first to show this disparity in a large low-income cohort of older adults with diabetes and depressive symptoms. Although socioeconomic status has been an important determinant of many health disparities (19), socioeconomic status measured by self-reported household income and education was associated with antidepressant use in this study, but the patterns were conflicting, with lower income and higher education being associated with greater antidepressant use. The disparity between African Americans and whites in this sample is unlikely to be explained by differences in income or education, as the difference persisted after adjustment for these factors.
The reasons for a disparity in antidepressant use are not easily apparent and probably represent a combination of factors including the recognition and diagnosis of depression in African Americans, as well as access and attitudes toward antidepressant medication in this population. In some primary care settings, providers recognize depression and recommend treatment for African Americans at rates equal to those for whites (20). However, even when depression is recognized, African Americans were less likely to take antidepressant medications than whites. Attitudes toward medications, particularly antidepressant medication, may contribute to this disparity. African Americans are less likely than whites to accept antidepressant treatment (20) and have been shown to prefer counseling over antidepressant medication (21). African Americans may also use spirituality and religion as a coping mechanism more frequently than whites.
There are several study limitations to acknowledge. First, because this is a cross-sectional study, inferences regarding causal relationships cannot be made. Second, diagnosis of diabetes was self-reported and not based on chart review or biological testing. In a separate validation study, 124 medical records of SCCS participants reporting a prior diagnosis of diabetes were reviewed, and 98% of the self-reports were validated based on criteria including ICD-9 codes, physician notes or prescriptions, and/or A1C or blood glucose measurements from the medical records (16). Third, antidepressant use may have been differentially reported because of differences in beliefs, attitudes, and preferences for treatment (20,21). Fourth, unmeasured differences in presenting depression-related complaints were unaccounted for, as were physicians' treatment priorities. Providers may be less likely to discuss depression treatment with African Americans who are often sicker when seeking care and present with more somatic attributions (22). Finally, although the CES-D has been validated in various populations, including multiethnic groups with diabetes (23), it may not be psychometrically equivalent across race-ethnicity or immigrant generations (24) and has demonstrated false-positive rates in low-income CHC settings. In one study, the standard cutoff for major depressive disorder yielded a sensitivity of 0.95 and specificity of 0.70, but more than two-thirds of those who screened positive did not actually meet the criteria for major depressive disorder (25). Thus, it is possible that depression would not be diagnosed in some study participants who reported mild and moderate depressive symptoms or they would not be considered good candidates for treatment after a clinician conducted a careful diagnostic interview.
Despite these limitations, our findings suggest a sizable racial disparity in antidepressant use in a large, low-income cohort of individuals with diabetes and depressive symptoms. Given this is a population with large numbers of people with diabetes and with limited access to health care services, our findings provide important evidence of the need for appropriate management of depression as part of regular diabetes care. Treatment for depression in individuals with diabetes may improve glycemic control, overall functioning, and quality of life (2), thereby reducing one's risk of adverse health outcomes associated with untreated depression. Conversely, untreated depression might contribute to racial disparities in diabetes outcomes, complications, and premature death. The mechanisms underlying the association between racial status and antidepressant use is likely to be multifactorial. Prospective studies are needed to more closely examine the association between racial status and depression treatment in low-income, ethnic minority, adults with diabetes.
Acknowledgments
This research was funded with support by the National Institutes of Health (Grants R01-CA-92447, HL-67715, and P01-DK-20593). C.Y.O. is supported by a Diversity Supplement Award, National Institute of Diabetes and Digestive and Kidney Diseases (P60-DK-020593).
No potential conflicts of interest relevant to this article were reported.
Parts of this study were presented in poster form at the 31st annual meeting of the Society for Behavioral Medicine, Seattle, Washington, 7–10 April 2010.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ: The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2001; 24: 1069– 1078 [DOI] [PubMed] [Google Scholar]
- 2.Rubin RR, Ciechanowski P, Egede LE, Lin EH, Lustman PJ: Recognizing and treating depression in patients with diabetes. Curr Diab Rep 2004; 4: 119– 125 [DOI] [PubMed] [Google Scholar]
- 3.Katon WJ, Simon G, Russo J, Von Korff M, Lin EH, Ludman E, Ciechanowski P, Bush T: Quality of depression care in a population-based sample of patients with diabetes and major depression. Med Care 2004; 42: 1222– 1229 [DOI] [PubMed] [Google Scholar]
- 4.Egede LE, Ellis C: The effects of depression on diabetes knowledge, diabetes self-management, and perceived control in indigent patients with type 2 diabetes. Diabetes Technol Ther 2008; 10: 213– 219 [DOI] [PubMed] [Google Scholar]
- 5.Lustman PJ, Clouse RE, Nix BD, Freedland KE, Rubin EH, McGill JB, Williams MM, Gelenberg AJ, Ciechanowski PS, Hirsch IB: Sertraline for prevention of depression recurrence in diabetes mellitus: a randomized, double-blind, placebo-controlled trial. Arch Gen Psychiatry 2006; 63: 521– 529 [DOI] [PubMed] [Google Scholar]
- 6.Lustman PJ, Freedland KE, Griffith LS, Clouse RE: Fluoxetine for depression in diabetes: a randomized double-blind placebo-controlled trial. Diabetes Care 2000; 23: 618– 623 [DOI] [PubMed] [Google Scholar]
- 7.Lustman PJ, Clouse RE: Treatment of depression in diabetes: impact on mood and medical outcome. J Psychosom Res 2002; 53: 917– 924 [DOI] [PubMed] [Google Scholar]
- 8.Egede LE: Effect of depression on self-management behaviors and health outcomes in adults with type 2 diabetes. Curr Diabetes Rev 2005; 1: 235– 243 [DOI] [PubMed] [Google Scholar]
- 9.Katon W, Fan MY, Unützer J, Taylor J, Pincus H, Schoenbaum M: Depression and diabetes: a potentially lethal combination. J Gen Intern Med 2008; 23: 1571– 1575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Egede LE, Nietert PJ, Zheng D: Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care 2005; 28: 1339– 1345 [DOI] [PubMed] [Google Scholar]
- 11.Katon WJ, Russo JE, Von Korff M, Lin EH, Ludman E, Ciechanowski PS: Long-term effects on medical costs of improving depression outcomes in patients with depression and diabetes. Diabetes Care 2008; 31: 1155– 1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lustman PJ, Clouse RE: Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complications 2005; 19: 113– 122 [DOI] [PubMed] [Google Scholar]
- 13.Signorello LB, Hargreaves MK, Steinwandel MD, Zheng W, Cai Q, Schlundt DG, Buchowski MS, Arnold CW, McLaughlin JK, Blot WJ: Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc 2005; 97: 972– 979 [PMC free article] [PubMed] [Google Scholar]
- 14.Andresen EM, Malmgren JA, Carter WB, Patrick DL: Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 1994; 10: 77– 84 [PubMed] [Google Scholar]
- 15.Nguyen HT, Kitner-Triolo M, Evans MK, Zonderman AB: Factorial invariance of the CES-D in low socioeconomic status African Americans compared with a nationally representative sample. Psychiatry Res 2004; 126: 177– 187 [DOI] [PubMed] [Google Scholar]
- 16.Huizinga M, Elasy T, Villegas R, Signorello L, Blot W, Cavanaugh K: Validation of diabetes self-report and characteristics of undiagnosed diabetes in the Southern Community Cohort Study (Abstract). In Proceedings of the 69th Annual Meeting of the American Diabetes Association, New Orleans, LA, 2009. Alexandria, VA, American Diabetes Association; p. A279 [Google Scholar]
- 17.Sambamoorthi U, Olfson M, Wei W, Crystal S: Diabetes and depression care among medicaid beneficiaries. J Health Care Poor Underserved 2006; 17: 141– 161 [DOI] [PubMed] [Google Scholar]
- 18.Wagner J, Tsimikas J, Abbott G, de Groot M, Heapy A: Racial and ethnic differences in diabetic patient-reported depression symptoms, diagnosis, and treatment. Diabetes Res Clin Pract 2007; 75: 119– 122 [DOI] [PubMed] [Google Scholar]
- 19.Signorello LB, Schlundt DG, Cohen SS, Steinwandel MD, Buchowski MS, McLaughlin JK, Hargreaves MK, Blot WJ: Comparing diabetes prevalence between African Americans and whites of similar socioeconomic status. Am J Public Health 2007; 97: 2260– 2267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miranda J, Cooper LA: Disparities in care for depression among primary care patients. J Gen Intern Med 2004; 19: 120– 126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB: Treatment preferences among depressed primary care patients. J Gen Intern Med 2000; 15: 527– 534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghods BK, Roter DL, Ford DE, Larson S, Arbelaez JJ, Cooper LA: Patient-physician communication in the primary care visits of African Americans and whites with depression. J Gen Intern Med 2008; 23: 600– 606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stahl D, Sum CF, Lum SS, Liow PH, Chan YH, Verma S, Chua HC, Chong SA: Screening for depressive symptoms: validation of the center for epidemiologic studies depression scale (CES-D) in a multiethnic group of patients with diabetes in Singapore. Diabetes Care 2008; 31: 1118– 1119 [DOI] [PubMed] [Google Scholar]
- 24.Perreira KM, Deeb-Sossa N, Harris KM, Bollen K: What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Social Forces 2005; 83: 1567– 1602 [Google Scholar]
- 25.Thomas JL, Jones GN, Scarinci IC, Mehan DJ, Brantley PJ: The utility of the CES-D as a depression screening measure among low-income women attending primary care clinics. The Center for Epidemiologic Studies-Depression. Int J Psychiatry Med 2001; 31: 25– 40 [DOI] [PubMed] [Google Scholar]