Abstract
OBJECTIVE
Ljungan virus (LjV) has been proposed as a potential environmental factor for type 1 diabetes. The objective was to test for any association of LjV with type 1 diabetes.
RESEARCH DESIGN AND METHODS
A nested case-control design was used to test for any association between the development of pre-diabetic autoimmunity and presence of LjV in stool samples (n = 3,803) in the Norwegian Environmental Triggers of Type 1 Diabetes (MIDIA) study. The children followed were 27 infants who developed pre-diabetic autoimmunity during or shortly after the sampling period, 54 matched control subjects, and 94 other children.
RESULTS
No LjV RNA was detected.
CONCLUSIONS
The results indicate that LjV is rare in young children. LjV does not seem to be involved in the development of human type 1 diabetes.
Ljungan virus (LjV), a rodent virus described by Niklasson et al. (1), has been associated with a variety of conditions in rodents, including type 1 diabetes (2), myocarditis (3), and intrauterine death (4). In humans, LjV has been associated with intrauterine fetal death (5), anencephaly (6), and sudden infant death syndrome (7) and has been suggested as a factor in type 1 diabetes (2). LjV belongs to the viral family Picornaviridae, genus Parechovirus. The genus also includes human parechovirus (HPeV), which is common in infancy and replicates mainly in the gut. A possible role of LjV in type 1 diabetes is of particular interest because of the strong association found in captive bank voles (2,3,8).
The aim of the study was to investigate the presence of LjV RNA in stool samples to find a possible association with type 1 diabetes.
RESEARCH DESIGN AND METHODS
A nested case-control study was conducted, using 2,054 stool samples from 81 children (27 case subjects, 54 control subjects) all carrying the DRB1*0401-DQA1*03-DQB1*0302/DRB1*03-DQA1*05-DQB1*02 HLA genotype, which gives the highest risk for type 1 diabetes. Case subjects (10 boys, 17 girls) were defined on development of type 1 diabetes or of diabetes-associated autoimmunity (being positive for two or three autoantibodies: GAD, IA2, or IAA). Control children (31 boys, 23 girls) were matched for birth date and geographical residence. This dataset was merged with a previously published dataset investigating parechovirus infections (9) in 1,941 stool samples from 102 children (51 with the high-risk genotype and 51 without). In total, there were 3,803 unique samples from 175 children (86 boys, 89 girls), since some children participated in both studies. The children represented 16 of 19 municipalities in Norway.
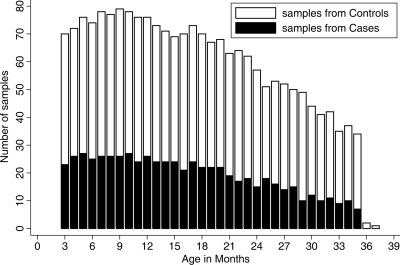
Monthly stool samples, from 3 to 35 months of age, were collected by parents as previously described (10); the age distribution is shown in Fig. 1. The samples were collected between 2001 and 2008; because most children were followed for at least 1 year, there was an equal seasonal distribution of samples. The median follow-up was 30 months for the stool samples (range 9–37 months), with median end point (autoimmunity) of the cases at 20.5 months (range 6–43). The presence of LjV was examined by extraction of RNA/DNA, reverse transcription (RT), and real-time PCR as described by Tapia et al. (9), with minor modifications of the protocol due to introduction of a 96-well format and the use of the antisense primer described by Donoso Mantke et al. (11) as the RT primer. Two positive control subjects were included from extraction to PCR run (140 and 70 copies of a transcript from a plasmid containing a cDNA clone of LjV prototype strain 87-012, provided by Professor Lindberg, University of Kalmar, Sweden). A fragment of West Nile Virus RNA was spiked into the samples as an exogenous internal control (10). The study was approved by the Regional Committee for Medical Research Ethics and the Norwegian Data Inspectorate.
Figure 1.
Age distribution of the samples. The number of samples from case children (■) and the total number of samples (□) distributed by month of age are shown.
RESULTS
No LjV RNA was detected in any of the stool samples investigated, neither from the 27 children who had developed autoimmunity, nor from the 54 matched control subjects and the 94 healthy children previously tested. The positive LjV control was consistently detected, and the West Nile Virus Armored RNA used as an exogenous internal control in each sample was consistently positive.
CONCLUSIONS
Considering the follow-up time, the number of tested samples, and that both pre-diabetic and healthy children were tested, these results indicate that LjV is very rare in the stool of Norwegian infants. The typical stool quantities of human enterovirus and HPeV in samples from the Norwegian Environmental Triggers of Type 1 Diabetes (MIDIA) cohort study were two to five orders of magnitude higher than the detection limit for LjV (9,12); presumably any appreciable replication of LjV in the gut would be detected. The detection of the exogenously added West Nile virus RNA safeguards against the presence of inhibitors and RNA degradation. The primers used consistently detected the positive LjV RNA controls included in each run and are expected to detect all strains of LjV. No change in sensitivity was detected with the introduction of a 96-well extraction method. The use of the antisense primer in the RT reaction could be presumed to increase the sensitivity at the cost of the formation of more spurious products, but was chosen to ensure that any possible positive sample would be detected. The lack of evidence for the presence of LjV suggests that this virus rarely infects the gut of Norwegian infants, and it seems unlikely that the virus is the cause of the autoimmunity observed in the present study.
Picornaviruses may also replicate outside the intestinal tract and may cause viremia or respiratory infections. Although one would expect a gastrointestinal route of infection in the case of LjV, the virus might reach the pancreas even after limited replication in the gut. Although data supporting LjV infections in humans have been published, there is so far no conclusive evidence. The arguably strongest evidence stems from prenatal studies (5,6). In these studies, the presence of virus has been suggested partly by serology and partly by PCR; but, as pointed out by Bergstrom et al. (13), different methods do not seem to give congruent results. Moreover, the PCR positivity observed in the earlier studies is not reported to have been confirmed by sequencing. Although the evidence suggests possible human LjV infections, the data also indicate that it is a rare event and primarily during the prenatal period.
The likelihood of infection may also be geographically specific and dependent on the cycles of its natural reservoir, which presumably are bank voles in Scandinavia. Although common in Norway, their prevalence in the communities from which infants in the present study was recruited is not known. Thus, the possibility that the infants investigated were never exposed cannot be ruled out.
In conclusion, although the present data do not rule out the possibility that LjV can cause type 1 diabetes, they do suggest that this virus is not a common risk factor in the etiology of the disease in Norway.
Acknowledgments
This study and the MIDIA project were funded by the Norwegian Organization for Health and Rehabilitation (Grant 2005/2/0128), European Economic Area and Norway Grants (Grant A/CZ0046/1/0014 through the Research Support Fund, Prague, the Czech Republic), the Ministry of Education of the Czech Republic (Grant MSM0021620814), the Research Council of Norway (Grants 135893/330, 155300/320, 156477/730, and 166515/V50), the Norwegian Diabetes Association, the Children With Diabetes Foundation (Denver, CO), and NewGeneris (Grant Food-CT- 2005-016320).
No potential conflicts of interest relevant to this article were reported.
We thank the public health care nurses for their effort in the recruitment to the MIDIA study and for the follow-up of high-risk children and the staff at the Biobank, Norwegian Institute of Public Health, for DNA extraction, and genotyping. In particular, we would like to express our gratitude to all the parents for their efforts in handling their child's type 1 diabetes risk and for providing delivered blood and fecal samples from their children and completing questionnaires.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Niklasson B, Kinnunen L, Hörnfeldt B, Hörling J, Benemar C, Hedlund KO, Matskova L, Hyypiä T, Winberg G: A new picornavirus isolated from bank voles (Clethrionomys glareolus). Virology 1999; 255: 86– 93 [DOI] [PubMed] [Google Scholar]
- 2.Niklasson B, Heller KE, Schønecker B, Bildsøe M, Daniels T, Hampe CS, Widlund P, Simonson WT, Schaefer JB, Rutledge E, Bekris L, Lindberg AM, Johansson S, Ortqvist E, Persson B, Lernmark A: Development of type 1 diabetes in wild bank voles associated with islet autoantibodies and the novel ljungan virus. Int J Exp Diabesity Res 2003; 4: 35– 44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niklasson B, Nyholm E, Feinstein RE, Samsioe A, Hörnfeldt B: Diabetes and myocarditis in voles and lemmings at cyclic peak densities: induced by Ljungan virus? Oecologia 2006; 150: 1– 7 [DOI] [PubMed] [Google Scholar]
- 4.Samsioe A, Sjöholm A, Niklasson B, Klitz W: Fetal death persists through recurrent pregnancies in mice following Ljungan virus infection. Birth Defects Res B Dev Reprod Toxicol 2008; 83: 507– 510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Samsioe A, Papadogiannakis N, Hultman T, Sjöholm A, Klitz W, Niklasson B: Ljungan virus present in intrauterine fetal death diagnosed by both immunohistochemistry and PCR. Birth Defects Res A Clin Mol Teratol 2009; 85: 227– 229 [DOI] [PubMed] [Google Scholar]
- 6.Niklasson B, Samsioe A, Papadogiannakis N, Gustafsson S, Klitz W: Zoonotic Ljungan virus associated with central nervous system malformations in terminated pregnancy. Birth Defects Res A Clin Mol Teratol 2009; 85: 542– 545 [DOI] [PubMed] [Google Scholar]
- 7.Niklasson B, Almqvist PR, Hornfeldt B, Klitz W: Sudden infant death syndrome and Ljungan virus. Forensic Sci Med Pathol 2009; 5: 274– 279 [DOI] [PubMed] [Google Scholar]
- 8.Niklasson B, Samsioe A, Blixt M, Sandler S, Sjöholm A, Lagerquist E, Lernmark A, Klitz W: Prenatal viral exposure followed by adult stress produces glucose intolerance in a mouse model. Diabetologia 2006; 49: 2192– 2199 [DOI] [PubMed] [Google Scholar]
- 9.Tapia G, Cinek O, Witsø E, Kulich M, Rasmussen T, Grinde B, Rønningen KS: Longitudinal observation of parechovirus in stool samples from Norwegian infants. J Med Virol 2008; 80: 1835– 1842 [DOI] [PubMed] [Google Scholar]
- 10.Cinek O, Witsø E, Jeansson S, Rasmussen T, Drevinek P, Wetlesen T, Vavrinec J, Grinde B, Rønningen KS: Longitudinal observation of enterovirus and adenovirus in stool samples from Norwegian infants with the highest genetic risk of type 1 diabetes. J Clin Virol 2006; 35: 33– 40 [DOI] [PubMed] [Google Scholar]
- 11.Donoso Mantke O, Kallies R, Niklasson B, Nitsche A, Niedrig M: A new quantitative real-time reverse transcriptase PCR assay and melting curve analysis for detection and genotyping of Ljungan virus strains. J Virol Methods 2007; 141: 71– 77 [DOI] [PubMed] [Google Scholar]
- 12.Witsø E, Palacios G, Cinek O, Stene LC, Grinde B, Janowitz D, Lipkin WI, Rønningen KS: High prevalence of human enterovirus a infections in natural circulation of human enteroviruses. J Clin Microbiol 2006; 44: 4095– 4100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bergstrom T, Liljeqvist JA: [Irrelevant about Ljungan virus]. Lakartidningen 2009; 106: 1110. [PubMed] [Google Scholar]