Abstract
OBJECTIVE
Nonalcoholic fatty liver disease is highly prevalent in obese and type 2 diabetic individuals and is strongly associated with dyslipidemia and inflammation. Weight loss and/or pharmacotherapy are commonly used to correct these abnormalities.
RESEARCH DESIGN AND METHODS
We performed a 16-week intervention trial of a hypocaloric, low-fat diet plus 10 mg/day ezetimibe (n = 15) versus a hypocaloric, low-fat diet alone (n = 10) on intrahepatic triglyceride (IHTG) content, plasma high sensitivity–C-reactive protein (hs-CRP), adipocytokines, and fetuin-A concentrations and apolipoprotein (apo)B-100 kinetics in obese subjects. ApoB-100 metabolism was assessed using stable isotope tracer kinetics and compartmental modeling; liver and abdominal fat contents were determined by magnetic resonance techniques.
RESULTS
Both weight loss and ezetimibe plus weight loss significantly (all P < 0.05) reduced body weight, visceral and subcutaneous adipose tissues, insulin resistance and plasma triglycerides, VLDL–apoB-100, apoC-III, fetuin-A, and retinol-binding protein-4 and increased plasma adiponectin concentrations. Compared with weight loss alone, ezetimibe plus weight loss significantly (all P < 0.05) decreased IHTG content (−18%), plasma hs-CRP (−53%), interleukin-6 (−24%), LDL cholesterol (−18%), campesterol (−59%), and apoB-100 (−14%) levels, with a significant increase in plasma lathosterol concentrations (+43%). The LDL–apoB-100 concentration also significantly fell with ezetimibe plus weight loss (−12%), chiefly owing to an increase in the corresponding fractional catabolic rate (+29%). The VLDL–apoB-100 secretion rate fell with both interventions, with no significant independent effect of ezetimibe.
CONCLUSIONS
Addition of ezetimibe to a moderate weight loss diet in obese subjects can significantly improve hepatic steatosis, inflammation, and LDL–apoB-100 metabolism.
The prevalence of nonalcoholic fatty liver disease (NAFLD) in the general population is up to 30% but is higher in those with type 2 diabetes and obesity (1,2). NAFLD is also strongly associated with dyslipidemia and inflammation, which may account for increased risk of cardiovascular disease (CVD) in these subjects (2). Reducing intrahepatic triglyceride (IHTG) content may help to reduce risk of hepatic and cardiovascular complications.
Visceral fat accumulation in obese subjects increases the portal delivery of free fatty acids to the liver, which not only stimulates hepatic gluconeogenesis and triglyceride synthesis but also impairs hepatic extraction of insulin (3). Insulin resistance increases IHTG and hepatic secretion of apolipoprotein (apo)B by several mechanisms (4,5). These include increased fatty acid flux to the liver, increased de novo lipogenesis related to increased expression of sterol regulatory element–binding protein-1c (SREBP-lc), decreased expression of peroxisome proliferator–activated receptors, increased triglyceride availability owing to increased expression of microsomal triglyceride transfer protein, and resistance to a direct inhibitory effect of insulin on apoB secretion. Insulin resistance also decreases the catabolism of LDL by down-regulating LDL receptor expression and activity (6).
Weight reduction through dietary intervention is the cornerstone of management of obesity and/or NAFLD (1,7). We have reported previously that weight reduction (>10% body weight) with a low-fat diet effectively decreases plasma triglycerides and apoB-100 (8). However, such intensive weight loss is difficult to achieve and maintain. Moderate weight loss of 3–7% is therefore a more realistic goal to be implemented in clinical practice. Whether this level of weight loss could lead to adequate improvement in fatty liver and its associated metabolic disorders remains unclear.
Ezetimibe is a potent cholesterol absorption inhibitor that has been shown to reduce cholesterol absorption and LDL cholesterol concentrations (9,10). Whereas ezetimibe treatment has been shown to increase LDL–apoB-100 catabolism (11,12), its effect on VLDL–apoB-100 transport is less consistent, with either no effect or an increased secretion rate as reported previously. Therefore, the combination of ezetimibe and weight loss could be an optimal approach in the clinical setting to improve dyslipidemia by harnessing the complementary mechanism of action of these interventions. Moreover, ezetimibe has recently been shown to improve liver steatosis and fibrosis in animal models of metabolic syndrome (13). The effect of ezetimibe on IHTG content and the associated metabolic factors needs to be demonstrated in humans.
In the present study, we tested the hypothesis that the addition of ezetimibe to a weight loss diet improves hepatic steatosis and apoB-100 metabolism in subjects with obesity. We also wished to explore the effects of ezetimibe in this setting on plasma high-sensitivity (hs) C-reactive protein (CRP), fetuin-A, and adipocytokine concentration.
RESEARCH DESIGN AND METHODS
Twenty-five centrally obese subjects who were consuming, ad libitum, weight-maintaining diets were recruited for the study. None of the subjects had type 2 diabetes, the APOE2/E2 genotype, macroproteinuria, creatininemia (>120 μmol/l), hypothyroidism, or abnormal liver enzymes (alanine aminotransferase [ALT] >3 times the upper limit of normal, i.e., 120 units/l for men and 90 units/l for women) or consumed more than 20 g alcohol/day. None reported a history of CVD or was taking antihypertensive medications or other agents known to affect lipid metabolism. The study was approved by the Ethics Committee of the Royal Perth Hospital, and informed consent was obtained.
Clinical protocols
The study was a randomized, single-blind intervention trial. Twenty-five eligible patients entered a 4-week run-in diet-stabilizing period, at the end of which they were switched to a hypocaloric diet for 16 weeks immediately followed by a 6-week weight stabilization period with an isocaloric diet. During the 22-week dietary intervention period, these subjects were also randomly assigned to 10 mg/day ezetimibe (nine men and six women) or matching placebo (six men and four women). Body composition was estimated using a Holtain Body Composition Analyser (Holtain, Dyfed, U.K.) from which total fat and fat-free mass (FFM) were derived. Dietary intake was assessed for energy and major nutrients using DIET 4 nutrient calculation software (Xyris Software, Highgate Hill, QL, Australia). The clinical protocol for administration of [d3]-leucine infusion and blood sampling was described previously (14).
Liver and abdominal fat measurements
Proton magnetic resonance imaging of liver and abdominal fat was performed during the week of isotope infusion studies. A single volume-stimulated echo acquisition mode sequence was used. The manufacturer's magnetic resonance spectroscopy processing software was used to obtain the liver fat–to–liver water signal ratio, which was converted to liver fat percentage.
Magnetic resonance imaging of eight transaxial segments at intervertebral disc levels from T11 to S1 was performed using a 1.0T Picker magnetic resonance scanner (Picker International, Cleveland, OH) and a T1-weighted fast spin echo sequence with a high fat–to–water signal ratio. Visceral and subcutaneous abdominal adipose tissue areas were measured at the level of the L3 vertebra.
Measurement of isotopic enrichments and calculation of kinetic parameters
VLDL, intermediate-density lipoprotein (IDL), and LDL were isolated from 2 ml of plasma by sequential ultracentrifugation. The isolation procedures and the multicompartmental model used to describe apoB-100 leucine tracer-to-tracee ratios were described previously (14). The fractional catabolic rates (FCRs) of VLDL, IDL, and LDL–apoB-100 were derived from the model parameters giving the best fit. The pool sizes of VLDL, IDL, and LDL–apoB-100 were calculated as the product of corresponding concentration (milligram per liter) and plasma volume (0.045 l/kg body weight). The secretion rate was calculated by multiplying FCR by pool size (milligrams per kilogram of FFM per day).
Biochemical analytes
Plasma lipid and glucose concentrations were determined by enzymatic methods. LDL cholesterol was calculated by the Friedewald calculation. Plasma total apoA-I, apoB-100, and hs-CRP concentrations were determined by immunonephelometry (Dade Behring, Deerfield, IL). Plasma insulin was measured by a chemiluminescent immunometric assay (Diagnostic Products, Los Angeles, CA), and insulin resistance was estimated by the homeostasis model assessment (HOMA) score. ApoB-100 concentrations in VLDL, IDL, and LDL fractions were measured as described by Beghin et al. (15). Plasma lathosterol and campesterol concentrations were assayed using gas chromatography–mass spectrometry. Plasma retinol-binding protein-4 (RBP-4), fetuin-A, adiponectin, interleukin-6 (IL-6), and tumor necrosis factor-α concentrations were determined using an enzyme immunoassay (R&D Systems, Minneapolis, MN).
Statistical analysis
All analyses were carried out using SPSS 15 (SPSS, Chicago, IL). Associations were examined using the simple linear regression method. Paired t tests were used to assess changes within both treatment groups for all variables. Adjustment for differences in baseline covariates and changes in variables during the study were performed by ANCOVA using general linear models. Statistical significance was defined at the 5% level.
RESULTS
Subject characteristics
The subjects were middle-aged (mean ± SD, 57 ± 8 years), normotensive (blood pressure 133 ± 19/75 ± 10 mmHg), centrally obese (waist circumference 106 ± 9 cm and BMI 33 ± 4 kg/m2), insulin resistant (HOMA score 3.0 ± 1.4), and mildly dyslipidemic (total cholesterol 5.8 ± 1.0 mmol/l and triglycerides 1.8 ± 0.7 mmol/l). Of the subjects, 21 had NAFLD as defined by IHTG content >5%.
Dietary compliance
The reductions in total dietary energy in the weight loss and ezetimibe plus weight loss groups (8,269 ± 789 vs. 5,811 ± 437 KJ and 8,365 ± 531 vs. 6,167 ± 316 KJ, respectively) and fat intake (36 ± 2 vs. 27 ± 1% and 38 ± 1 vs. 30 ± 1%, respectively) were similar; increased carbohydrate intake was also similar in both groups (weight loss 40 ± 2 vs. 49 ± 1% and ezetimibe plus weight loss 38 ± 1 vs. 46 ± 2%, respectively). All changes were statistically significant (P < 0.01). There was no change in reported physical activity levels during the study in either the weight loss or ezetimibe plus weight loss groups (data not shown).
Body weight, body composition, and biochemical characteristics
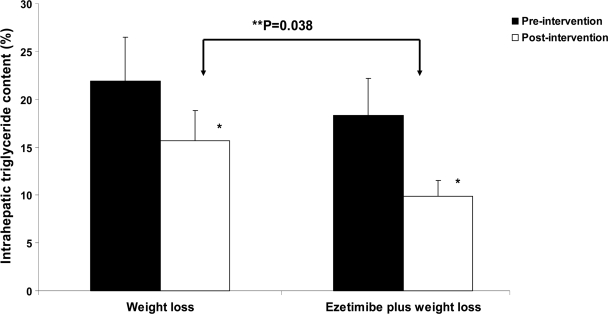
The effects of weight loss and ezetimibe plus weight loss on body weight, body composition, and biochemical characteristics are shown in Table 1. Despite the preintervention, IHTG and visceral and subcutaneous fat contents were numerically higher in the weight loss group, but the group differences were not significant (all P > 0.05). Both treatments (weight loss and ezetimibe plus weight loss) resulted in significant reductions in body weight, BMI, waist circumference, total fat mass, visceral and subcutaneous abdominal adipose tissue areas, plasma concentrations of triglycerides, and apoC-III as well as insulin and HOMA score. However, the magnitude of these changes was not significantly different between treatment groups (all P > 0.05). With weight loss, there was also a significant reduction in plasma lathosterol (−16%). IHTG content decreased significantly in both weight loss and ezetimibe plus weight loss groups. The reduction in IHTG was significantly (P < 0.05) greater in the ezetimibe plus weight loss (−46%) than in the weight loss (−28%) group (Fig. 1).
Table 1.
Clinical and biochemical characteristics before and after intervention in the weight loss and ezetimibe plus weight loss groups
| Weight loss |
Ezetimibe plus weight loss |
|||
|---|---|---|---|---|
| 0 | 22 weeks | 0 | 22 weeks | |
| n | 10 | 15 | ||
| Body weight (kg) | 100 ± 6 | 94 ± 5* | 94 ± 3 | 87 ± 3* |
| BMI (kg/m2) | 33 ± 1 | 31 ± 1* | 32 ± 1 | 31 ± 1* |
| Waist (cm) | 107 ± 4 | 98 ± 4* | 106 ± 2 | 96 ± 2* |
| Total fat mass (kg) | 39 ± 4 | 35 ± 4* | 37 ± 3 | 32 ± 3* |
| Fat-free mass (kg) | 60 ± 3 | 59 ± 3 | 56 ± 3 | 55 ± 3 |
| Visceral fat at L3 vertebra (cm2) | 278 ± 38 | 228 ± 36† | 257 ± 25 | 213 ± 22* |
| Subcutaneous fat at L3 vertebra (cm2) | 358 ± 43 | 316 ± 36† | 278 ± 30 | 257 ± 28† |
| Intrahepatic triglyceride content (%) | 22 ± 5 | 16 ± 4* | 18 ± 3 | 10 ± 2*‡ |
| Alanine aminotransferase (U/l) | 32 ± 5 | 26 ± 4 | 29 ± 2 | 30 ± 3 |
| Cholesterol (mmol/l) | 5.8 ± 0.2 | 5.5 ± 0.2 | 5.8 ± 0.3 | 4.9 ± 0.3*‡ |
| Triglyceride (mmol/l) | 1.7 ± 0.3 | 1.3 ± 0.2† | 2.0 ± 0.2 | 1.5 ± 0.1* |
| Nonesterified fatty acids (mEq/l) | 0.62 ± 0.07 | 0.56 ± 0.06 | 0.74 ± 0.11 | 0.75 ± 0.10 |
| HDL cholesterol (mmol/l) | 1.3 ± 0.2 | 1.3 ± 0.1 | 1.1 ± 0.1 | 1.1 ± 0.1 |
| LDL cholesterol (mmol/l) | 3.7 ± 0.2 | 3.7 ± 0.2 | 3.8 ± 0.3 | 3.1 ± 0.2*‡ |
| Lathosterol (μmol/l) | 12 ± 1 | 10 ± 2* | 12 ± 1 | 15 ± 2† |
| Campesterol (μmol/l) | 5.4 ± 0.9 | 4.9 ± 0.7 | 9.1 ± 1.5 | 3.2 ± 0.5* |
| ApoA-I (g/l) | 1.5 ± 0.1 | 1.5 ± 0.1 | 1.4 ± 0.1 | 1.4 ± 0.1 |
| ApoB-100 (g/l) | 1.2 ± 0.1 | 1.1 ± 0.1 | 1.2 ± 0.1 | 0.9 ± 0.1*‡ |
| ApoC-III (mg/l) | 176 ± 15 | 153 ± 16* | 186 ± 12 | 160 ± 13* |
| Glucose (mmol/l) | 5.5 ± 0.2 | 5.7 ± 0.2 | 5.5 ± 0.2 | 5.6 ± 0.1 |
| Insulin (mU/l) | 12 ± 2 | 10 ± 2† | 12 ± 1 | 9 ± 1† |
| HOMA score | 3.1 ± 0.5 | 2.6 ± 0.4† | 2.9 ± 0.3 | 2.2 ± 0.3† |
Data are means ± SEM. There was no significant group difference in the variables at baseline.
*P < 0.01, value significantly different from baseline value.
†P < 0.05.
‡P< 0.05, value significantly different using general linear modeling after adjustment for relative changes in the weight loss group.
Figure 1.
Effects of weight loss and ezetimibe plus weight loss on intrahepatic triglyceride content in obese subjects. There was no significant group difference in preintervention intrahepatic triglyceride content (P > 0.05). *P < 0.05, value significantly different from baseline value. **Value significantly different using general linear modeling after adjustment for weight loss group.
Compared with weight loss alone, ezetimibe plus weight loss also significantly (P < 0.05) reduced plasma concentrations of total cholesterol (−11%), LDL cholesterol (−18%), apoB-100 (−14%), and campesterol (−59%) but increased plasma lathosterol (+43%). Plasma concentrations of glucose, HDL cholesterol, apoA-I, and ALT were not altered with either treatment. Changes in ALT concentrations and IHTG content in individual subjects before and after intervention are shown in supplementary Table A (available in an online appendix at http://care.diabetesjournals.org/cgi/content/full/dc09-1765/DC1).
Plasma hs-CRP, adipocytokine, and fetuin-A concentrations
The effects of weight loss and ezetimibe plus weight loss on plasma hs-CRP, adipocytokine, and fetuin-A concentrations are shown in Table 2. Compared with weight loss, ezetimibe plus weight loss significantly (P < 0.05) lowered plasma hs-CRP (−53%) and IL-6 (−24%) concentrations. Both weight loss and ezetimibe plus weight loss treatments resulted in a significant decrease in RBP-4 (−11 and −9%, respectively) and plasma fetuin-A (−37 and −22%, respectively). The plasma adiponectin concentration increased significantly in both groups (+13 and +24%, respectively). Ezetimibe plus weight loss treatment was also associated with a significant decrease in plasma tumor necrosis factor-α concentration. However, the relative changes were not significantly different between the weight loss and ezetimibe plus weight loss groups (all P > 0.05). In univariate analysis, a reduction in plasma hs-CRP with ezetimibe was not associated with a corresponding change in IHTG nor with the plasma IL-6 concentration (r = 0.328 and 0.089, respectively).
Table 2.
Plasma hs-CRP, adipocytokine, and fetuin-A concentrations before and after intervention in the weight loss and ezetimibe plus weight loss groups
| Weight loss |
Ezetimibe plus weight loss |
|||
|---|---|---|---|---|
| 0 | 22 weeks | 0 | 22 weeks | |
| n | 10 | 15 | ||
| hs-CRP (mg/l) | 2.2 ± 0.4 | 2.4 ± 0.5 | 3.9 ± 1.0 | 2.2 ± 0.7*† |
| Interleukin-6 (ng/l) | 0.87 ± 0.08 | 0.91 ± 0.14 | 1.1 ± 0.1 | 0.91 ± 0.14*† |
| Tumor necrosis factor-α (ng/l) | 5.4 ± 0.5 | 5.4 ± 0.6 | 6.3 ± 0.5 | 5.4 ± 0.6* |
| Retinol-binding protein-4 (mg/l) | 27 ± 16 | 24 ± 8‡ | 27 ± 17 | 25 ± 20‡ |
| Adiponectin (mg/l) | 5.9 ± 0.7 | 6.8 ± 0.8‡ | 4.9 ± 0.7 | 6.1 ± 0.9* |
| Fetuin-A (mg/l) | 303 ± 31 | 189 ± 15* | 284 ± 24 | 221 ± 18‡ |
Data are means ± SEM.
*P <0.01, value significantly different from baseline value.
†P < 0.05.
‡P< 0.05, value significantly different using general linear modeling after adjustment for relative changes in the weight loss group.
ApoB-100 kinetics
The effects of weight loss and ezetimibe plus weight loss on apoB-100 in VLDL, IDL, and LDL are shown in Table 3. Both weight loss and ezetimibe plus weight loss resulted in significant reductions in the concentrations (−13 and −19%, respectively) and secretion rates of VLDL–apoB-100 (−29 and −13%, respectively) without significant changes in VLDL–apoB-100 FCR (+3 and +8%, respectively). The decreases in VLDL–apoB-100 concentrations and secretion rates were not significantly different between the groups. Compared with weight loss alone, ezetimibe plus weight loss significantly decreased the plasma concentration of LDL–apoB-100 (−12%) owing to a significant increase in FCR (+29%). There was no significant difference in the production rate of LDL–apoB-100.
Table 3.
Kinetic indices for apoB-100 before and after intervention in the weight loss and ezetimibe plus weight loss groups
| Weight loss |
Ezetimibe plus weight loss |
|||
|---|---|---|---|---|
| 0 | 22 weeks | 0 | 22 weeks | |
| n | 10 | 15 | ||
| VLDL–apoB-100 | ||||
| Concentration (mg/l) | 142 ± 123 | 123 ± 19† | 134 ± 12 | 109 ± 11† |
| Fractional catabolic rate (pools/day) | 4.8 ± 1.1 | 3.8 ± 0.4 | 3.9 ± 0.4 | 4.2 ± 0.3 |
| Production rate (mg/kg FFM/day) | 41 ± 5 | 29 ± 7† | 38 ± 3 | 32 ± 4† |
| IDL–apoB-100 | ||||
| Concentration (mg/l) | 76 ± 10 | 74 ± 12 | 82 ± 9 | 65 ± 9§ |
| Fractional catabolic rate (pools/day) | 3.9 ± 0.7 | 3.6 ± 0.3 | 3.5 ± 0.4 | 4.5 ± 0.5§ |
| Production rate (mg/kg FFM/day) | 20 ± 3 | 18 ± 2 | 20 ± 2 | 18 ± 2 |
| LDL–apoB-100 | ||||
| Concentration (mg/l) | 957 ± 61 | 885 ± 36 | 952 ± 76 | 774 ± 62*‡ |
| Fractional catabolic rate (pools/day) | 0.35 ± 0.03 | 0.34 ± 0.03 | 0.31 ± 0.02 | 0.39 ± 0.03*‡ |
| Production rate (mg/kg FFM/day) | 26 ± 3 | 22 ± 2 | 22 ± 1 | 21 ± 2 |
Data are means ± SEM.
*P <0.01, value significantly different from baseline value.
†P < 0.05.
‡P< 0.05, value significantly different using general linear modeling after adjustment for relative changes in the weight loss group.
§P = 0.06, value different from baseline value.
CONCLUSIONS
We provide new information concerning the effect of inhibiting intestinal cholesterol absorption with ezetimibe in addition to weight loss alone on intrahepatic triglyceride content, markers of inflammation, and apoB-100 metabolism in subjects with obesity. Our results demonstrate that relative to weight loss, ezetimibe further decreases IHTG content and plasma hs-CRP and IL-6 concentrations. Ezetimibe also significantly reduced the concentration of plasma LDL–apoB-100 by increasing its fractional catabolic rate. These changes were demonstrated against the background of the favorable effects of weight loss alone on VLDL–apoB-100 metabolism, insulin sensitivity, and plasma concentrations of adipocytokines and fetuin-A.
This is the first study to demonstrate the combined effects of ezetimibe and weight loss on apoB-100 kinetics and related metabolic indexes in obese subjects. Few kinetic studies have examined the effect of ezetimibe on apoB-100 metabolism in humans. In two separate studies by Tremblay et al. (11,12), ezetimibe monotherapy or coadministration with simvastatin increased the FCRs of VLDL, IDL, and LDL–apoB-100 in men with primary hypercholesterolemia and mixed hyperlipidemia. However, the effect of ezetimibe on the VLDL–apoB-100 secretion rate was not consistent. Ezetimibe could increase the VLDL–apoB-100 secretion rate by a mechanism involving a compensatory increase in hepatic cholesterol synthesis with ezetimibe. We confirm our previous report that weight loss decreases VLDL–apoB-100 secretion in obesity (8) but now report that ezetimibe does not decrease this further. Although we did not confirm that weight loss alone significantly increased the FCR of LDL–apoB-100, we now show that ezetimibe did increase LDL–apoB-100 FCR in insulin-resistant obese subjects.
It is likely that the combination of central obesity and insulin resistance collectively accounts for the dysregulation of apoB-100 metabolism (3,4). Therefore, weight loss with a low-fat diet could potentially correct the abnormalities in apoB-100 metabolism by an improvement in insulin sensitivity and reductions in abdominal adipose tissue. Consistent with this hypothesis, we found that both weight loss and ezetimibe plus weight loss interventions significantly reduced the plasma VLDL–apoB-100 concentration and secretion rate, probably owing to a concomitant reduction in visceral and subcutaneous adipose tissues and an improvement in insulin resistance.
Low adiponectin and elevated RBP-4 and fetuin-A concentrations are known to be closely related to obesity and insulin resistance (16,17). Our findings demonstrate that weight loss and ezetimibe plus weight loss interventions increased plasma adiponectin and decreased RPB-4 and fetuin-A concentrations, in agreement with other reports on weight loss. Given that none of these changes, including the VLDL–apoB-100 concentration and secretion rate, differed between the weight loss and ezetimibe plus weight loss groups, it is conceivable that all of these favorable changes are chiefly driven by the effects of weight loss.
In contrast with our previous report (8), weight loss did not increase the FCR of LDL–apoB-100 in this study. Discrepancies between the two studies might have been due to different experimental protocols. In particular, we only examined the effect of moderate weight loss (3–7%) in this study compared with >10% weight loss in our previous study. Despite this difference, we found that, compared with weight loss alone, addition of ezetimibe to weight loss resulted in a significant decrease in the plasma LDL–apoB-100 concentration, chiefly by increasing its catabolism. This result is consistent with the mechanism of action of ezetimibe that inhibition of intestinal cholesterol absorption results in reduced hepatic cholesterol concentrations and, subsequently, upregulates the LDL receptor and enhances LDL–apoB-100 clearance (18). Although we found that ezetimibe significantly reduced cholesterol absorption, endogenous cholesterol synthesis increased with ezetimibe treatment, as reflected by the increase in plasma lathosterol concentrations. As mentioned earlier, it is likely that hepatic cholesterol depletion with ezetimibe is accompanied by a compensatory increase in hepatic cholesterol synthesis. It is also important to note that the reduction in the VLDL–apoB-100 secretion rate was numerically smaller in the ezetimibe plus weight loss group than in the weight loss group (−13 vs. −29%). The increased cholesterol synthesis with ezetimibe may blunt the fall in VLDL–apoB-100 secretion with weight loss alone.
Another important finding from this study was that addition of ezetimibe to the weight loss diet further decreased IHTG content in the setting of similar changes in body weight, abdominal visceral and subcutaneous fat areas, and HOMA score between groups. Although there has long been speculation that ezetimibe may reduce IHTG content, ours is the first report to show that ezetimibe reduces IHTG content in humans. Telford et al. (18) found that hepatic SREBP1c mRNA was reduced with ezetimibe treatment in miniature pigs. This reduction could in turn inactivate the hepatic expression of genes involved for lipogenesis. Inhibition of dietary cholesterol absorption with ezetimibe may also reduce hepatic dietary cholesterol availability for activation of SREBP1c and subsequent lipogenesis (19). Evidence supports the fact that oxidized cholesterol is involved in hepatic accumulation of triglycerides (20). Ezetimibe inhibits the intestinal absorption of oxidized cholesterol (21), which may be responsible for the reduction in IHTG. Despite the significant effect of ezetimibe on IHTG, plasma ALT (a surrogate marker of IHTG) was not altered. Given that the plasma ALT concentration at baseline was on average within the normal reference range, it is possible that the plasma ALT concentration was less sensitive than magnetic resonance spectroscopy to test between-group differences in IHTG. The observed differences in preintervention IHTG and abdominal fat content might have confounded the results. However, the differences were not significant, and the preintervention variables had been used as covariates in general linear modeling, thereby adjusting for any group differences.
The present data show that the combined effect of ezetimibe plus weight loss significantly reduced the plasma hs-CRP concentration compared with weight loss alone. Previous studies have consistently shown that ezetimibe reduces plasma hs-CRP concentrations when given in combination with a statin (22,23). It is tempting to speculate that similar mechanisms of action of ezetimibe are also involved in the setting of moderate weight loss, although the exact mechanisms by which ezetimibe reduces hs-CRP are not fully understood. Consistent with the regulatory role of IL-6 on CRP synthesis (24), the significant reduction in plasma IL-6 concentrations with ezetimibe in our study may therefore partly account for the reduction in plasma hs-CRP concentrations. However, the finding that the reduction in plasma hs-CRP was not directly associated with a change in IL-6 or IHTG suggests that other factors could also account for the fall in plasma hs-CRP with ezetimibe. Previous human studies have shown that dietary cholesterol is associated with increased CRP (25). Therefore, it is possible that decreased cholesterol absorption with ezetimibe may also account for the reduction in plasma hs-CRP. This speculation requires further investigation.
The increased cardiovascular morbidity and mortality in human obesity and type 2 diabetes may be caused by the combination of insulin resistance, dyslipidemia, and inflammation. Our data suggest that the combination of ezetimibe and weight loss reduces plasma LDL cholesterol and apoB-100 concentrations, two independent predictors of treatment benefits on cardiovascular outcomes. In light of recent evidence suggesting the impact of NAFLD and hs-CRP on CVD, our new data also indicate that addition of ezetimibe to weight loss reduces hepatic steatosis and inflammation. Whether this combined treatment improves clinical outcomes remains to be fully demonstrated in clinical trials.
Supplementary Material
Acknowledgments
This study was funded by research grants from the National Health and Medical Research Council (NHMRC) and the National Heart Foundation of Australia (NHF). D.C.C. is a Career Development Fellow of the NHMRC. P.H.R.B. is an NHMRC Senior Research Fellow.
No potential conflicts of interest relevant to this article were reported.
We thank the nursing staff of the Clinical Research Studies Unit of the School of Medicine and Pharmacology (Royal Perth Hospital, University of Western Australia) for providing expert clinical assistance.
Footnotes
Clinical trial reg. no. ACTRN12606000152527, ANZCTR.org.au.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Torres DM, Harrison SA: Diagnosis and therapy of nonalcoholic steatohepatitis. Gastroenterology 2008; 134: 1682– 1698 [DOI] [PubMed] [Google Scholar]
- 2.Kotronen A, Yki-Järvinen H: Fatty liver: a novel component of the metabolic syndrome. Arterioscler Thromb Vasc Biol 2008; 28: 27– 38 [DOI] [PubMed] [Google Scholar]
- 3.Wajchenberg BL: Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev 2000; 21: 697– 738 [DOI] [PubMed] [Google Scholar]
- 4.Ginsberg HN, Huang LS: The insulin resistance syndrome: impact on lipoprotein metabolism and atherothrombosis. J Cardiovasc Risk 2000; 7: 325– 331 [DOI] [PubMed] [Google Scholar]
- 5.Utzschneider KM, Kahn SE: The role of insulin resistance in nonalcoholic fatty liver disease. J Clin Endocrinol Metab 2006; 91: 4753– 4761 [DOI] [PubMed] [Google Scholar]
- 6.Mazzone T, Foster D, Chait A: In vivo stimulation of low-density lipoprotein degradation by insulin. Diabetes 1984; 33: 333– 338 [DOI] [PubMed] [Google Scholar]
- 7.Van Gaal LF, Wauters MA, De Leeuw IH: The beneficial effects of modest weight loss on cardiovascular risk factors. Int J Obes Relat Metab Disord 1997; 21: S5– S9 [PubMed] [Google Scholar]
- 8.Riches FM, Watts GF, Hua J, Stewart GR, Naoumova RP, Barrett PH: Reduction in visceral adipose tissue is associated with improvement in apolipoprotein B-100 metabolism in obese men. J Clin Endocrinol Metab 1999; 84: 2854– 2861 [DOI] [PubMed] [Google Scholar]
- 9.Jeu L, Cheng JW: Pharmacology and therapeutics of ezetimibe (SCH 58235), a cholesterol-absorption inhibitor. Clin Ther 2003; 25: 2352– 2387 [DOI] [PubMed] [Google Scholar]
- 10.Temel RE, Tang W, Ma Y, Rudel LL, Willingham MC, Ioannou YA, Davies JP, Nilsson LM, Yu L: Hepatic Niemann-Pick C1-like 1 regulates biliary cholesterol concentration and is a target of ezetimibe. J Clin Invest 2007; 117: 1968– 1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tremblay AJ, Lamarche B, Cohn JS, Hogue JC, Couture P: Effect of ezetimibe on the in vivo kinetics of apoB-48 and apoB-100 in men with primary hypercholesterolemia. Arterioscler Thromb Vasc Biol 2006; 26: 1101– 1106 [DOI] [PubMed] [Google Scholar]
- 12.Tremblay AJ, Lamarche B, Hogue JC, Couture P: Effects of ezetimibe and simvastatin on apolipoprotein B metabolism in males with mixed hyperlipidemia. J Lipid Res 2009; 50: 1463– 1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deushi M, Nomura M, Kawakami A, Haraguchi M, Ito M, Okazaki M, Ishii H, Yoshida M: Ezetimibe improves liver steatosis and insulin resistance in obese rat model of metabolic syndrome. FEBS Lett 2007; 581: 5664– 5670 [DOI] [PubMed] [Google Scholar]
- 14.Watts GF, Barrett PH, Ji J, Serone AP, Chan DC, Croft KD, Loehrer F, Johnson AG: Differential regulation of lipoprotein kinetics by atorvastatin and fenofibrate in subjects with the metabolic syndrome. Diabetes 2003; 52: 803– 811 [DOI] [PubMed] [Google Scholar]
- 15.Beghin L, Duhal N, Poulain P, Hauw P, Lacroix B, Lecerf JM, Bonte JP, Fruchart JC, Luc G: Measurement of apolipoprotein B concentration in plasma lipoproteins by combining selective precipitation and mass spectrometry. J Lipid Res 2000; 41: 1172– 1176 [PubMed] [Google Scholar]
- 16.Rasouli N, Kern PA: Adipocytokines and the metabolic complications of obesity. J Clin Endocrinol Metab 2008; 93: s64– s73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ix JH, Shlipak MG, Brandenburg VM, Ali S, Ketteler M, Whooley MA: Association between human fetuin-A and the metabolic syndrome: data from the Heart and Soul Study. Circulation 2006; 113: 1760– 1767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Telford DE, Sutherland BG, Edwards JY, Andrews JD, Barrett PH, Huff MW: The molecular mechanisms underlying the reduction of LDL apoB-100 by ezetimibe plus simvastatin. J Lipid Res 2007; 48: 699– 708 [DOI] [PubMed] [Google Scholar]
- 19.Horton JD, Goldstein JL, Brown MS: SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest 2002; 109: 1125– 1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schroepfer GJ, Jr: Oxysterols: modulators of cholesterol metabolism and other processes. Physiol Rev 2000; 80: 361– 554 [DOI] [PubMed] [Google Scholar]
- 21.Staprans I, Pan XM, Rapp JH, Moser AH, Feingold KR: Ezetimibe inhibits the incorporation of dietary oxidized cholesterol into lipoproteins. J Lipid Res 2006; 47: 2575– 2580 [DOI] [PubMed] [Google Scholar]
- 22.Sager PT, Capece R, Lipka L, Strony J, Yang B, Suresh R, Mitchel Y, Veltri E: Effects of ezetimibe coadministered with simvastatin on C-reactive protein in a large cohort of hypercholesterolemic patients. Atherosclerosis 2005; 179: 361– 367 [DOI] [PubMed] [Google Scholar]
- 23.Pearson TA, Ballantyne CM, Veltri E, Shah A, Bird S, Lin J, Rosenberg E, Tershakovec AM: Pooled analyses of effects on C-reactive protein and low density lipoprotein cholesterol in placebo-controlled trials of ezetimibe monotherapy or ezetimibe added to baseline statin therapy. Am J Cardiol 2009; 103: 369– 374 [DOI] [PubMed] [Google Scholar]
- 24.Weinhold B, Rüther U: Interleukin-6-dependent and -independent regulation of the human C-reactive protein gene. Biochem J 1997; 327: 425– 429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tannock LR, O'Brien KD, Knopp RH, Retzlaff B, Fish B, Wener MH, Kahn SE, Chait A: Cholesterol feeding increases C-reactive protein and serum amyloid A levels in lean insulin-sensitive subjects. Circulation 2005; 111: 3058– 3062 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.