Abstract
Both major depressive disorder and bipolar disorder are the subject of a voluminous imaging and genetics literature. Here, we attempt a comprehensive review of MRI and metabolic PET studies conducted to date on these two disorders, and interpret our findings from the perspective of developmental and degenerative models of illness. Elevated activity and volume loss of the hippocampus, orbital and ventral prefrontal cortex are recurrent themes in the literature. In contrast, dorsal aspects of the PFC tend to display hypometabolism. Ventriculomegaly and white matter hyperintensities are intimately associated with depression in elderly populations and likely have a vascular origin. Important confounding influences are medication, phenotypic and genetic heterogeneity, and technological limitations. We suggest that environmental stress and genetic risk variants interact with each other in a complex manner to alter neural circuitry and precipitate illness. Imaging genetic approaches hold out promise for advancing our understanding of affective illness.
Background
Depression is arguably the epidemic of our time. The lifetime prevalence of major depressive disorder (MDD) ranges from 10–30% (Kessler et al 2003) and depression arising within the context of bipolar disorder (BD) has equally serious implications for morbidity and mortality (Pini et al 2005).
Understanding the etiological and pathophysiological basis of affective illness is clearly an international imperative. Current nosological systems are based on symptomatology rather than etiology, and robust biological correlates of depression have not been identified. The identification of biomarkers of depression is crucial not only in the ascent towards etiological understanding, but also in evaluating the efficacy of treatment interventions.
While the limited resolution of previous generation neuroimaging paradigms blunted the sensitivity and specificity of preceding investigations; with the advent of new technology, glints of understanding are beginning to emerge. Neuroimaging data implicate a key emotion-regulating circuit, the visceromotor network, encompassing the medial prefrontal cortex (mPFC) and its reciprocal connections to the amygdala, hippocampus, ventral striatum, hypothalamus and brain-stem in the pathophysiology of both MDD and BD (Ongur and Price 2000a).
More specifically, regions of orbitofrontal cortex (OFC) and the mPFC have shown MRI and post-mortem-derived evidence of tissue loss. Parallel metabolic and volumetric changes to the limbic components of the visceromotor network such as the amygdala, hippocampus and ventral striatum have been widely recorded, although the data are often conflicting. Unfortunately, diminutive structures such as the habenula and periaqueductal gray (PAG), which play a prominent role in emotional behavior, remain largely unstudied because of technological limitations.
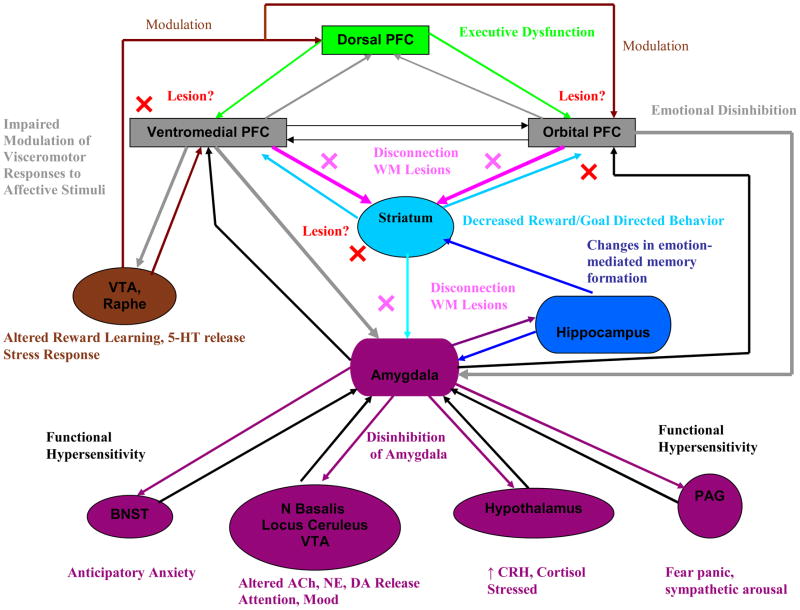
Here we review the biological correlates of MDD and BD as evinced by neuroimaging paradigms, and interpret these data from the perspective of neurodevelopmental and neurodegenerative pathoetiology. We attempt to integrate the conclusions drawn from the literature into a heuristic framework which characterizes affective illness as the consequence of a loss of top-down control (especially mPFC) over limbic structures such as the amygdala; or alternatively, the consequence of disinhibited limbic drive which overrides cortical regulation (Figure 1).
Figure 1. Amygdala-Centric Model of Potential Pathophysiological Changes in BD and MDD.
Lesions (red crosses) to the ventromedial, orbital PFC or basal ganglia may abrogate top-down control over the amygdala and deeper limbic structures (gray and purple lines). A similar PFC-limbic disconnection effect may result from white matter pathology (pink crosses). Alternatively, functional hypersensitivity of deeper limbic structures and/or the amygdala may disrupt prefrontal emotional regulation (black lines).
Methodology
A literature search of the PUBMED database up until September 2007 was carried out using the following key words: depression, bipolar disorder, neuroimaging, MRI, PET, fMRI, amygdala, hippocampus, basal ganglia, caudate, prefrontal cortex, orbital frontal cortex, dorsolateral prefrontal cortex, anterior cingulate, subgenual prefrontal cortex, white matter, and ventricle. Furthermore, review articles were searched, and other publications cross-referenced for additional published articles. Our inclusion criteria were heavily biased towards analyses of resting state metabolism rather than responses to cognitive, emotional or biochemical challenges. Thus, we although we highlight the result of certain fMRI studies (primarily in the discussion section), we make no attempt to cover the substantial, but as yet inchoate, functional magnetic resonance imaging (fMRI) and magnetic resonance spectroscopy (MRS) literature comprehensively. Positron emission tomography (PET) neuroreceptor studies are also beyond the scope of this review.
Further, the following exclusion criteria obtained: Papers that were not written in English, book chapters, conference abstracts, and case studies were not reviewed. Computerised tomography (CT) and Single Photon Emission Tomography (SPECT) studies were omitted. CT has a significantly lower tissue contrast and spatial resolution than MRI, and is also subject to bony artifacts in brain structures situated near the skull. SPECT has reduced sensitivity for detecting areas of increased perfusion due to its reliance on radioligands that are not freely diffusible across the blood brain barrier. Analyses of gross neuroanatomical structures such the entire frontal or temporal cortices were generally not discussed.
Extensive inter-connecting neural networks are involved in the generation and regulation of affect. These networks can be at least partly subsumed under the iterative activity of three cortical-striatal-limbic circuits encompassing a dorsolateral/dorsomedial prefrontal circuit, an orbital prefrontal circuit, and a ventromedial prefrontal circuit, including the anterior cingulate cortex (ACC) (Tekin and Cummings 2002) (Drevets 2001) (Price 1999). These circuits operate in parallel with prefrontal cortex-originating bidirectional projections to different nuclei of the perirhinal and entorhinal cortices, striatum, pallidum, thalamus, amygdala, hippocampus, hypothalamus, habenula, and periaqueductal grey (Tekin and Cummings 2002) (Price 1999).
Nevertheless, the limitations of current neuroimaging modalities make it unfeasible to reliably discriminate between individual nuclei within these structures. The amygdala, for example, is a heterogeneous structure of at least 14 different nuclei (Bachevalier and Loveland 2006). We will therefore discuss imaging studies of the amygdala, hippocampus, and striatum, separately, rather then placing them under the rubric of the dorsal prefrontal, orbital frontal, and ventromedial cortical-striatal-limbic circuits described above.
Results
The Amygdala
Despite its apparent heterogeneity of function, a degree of consensus that the amygdala plays a pivotal role in evaluating the emotional significance of perceptual data has been reached (Phillips et al 2003). In coloring perceptual stimuli with emotion, however, the amygdala appears to emphasise the hues of fear, anger and sadness (Gloor et al 1982) (Davidson 2002), providing prima facie evidence for its involvement in depression.
BD
Neuroimaging studies of the amygdala in patients with BD (Tables 1 and 2) are characterized by an interesting age-related dichotomy of findings. In adults, the predominant pattern is one of increased amygdala volume while in children and adolescents the reverse applies (Table 1). The findings in adults seem to hold even in samples with a long history of illness (Altshuler et al 2000) (Brambilla et al 2003a) (Frangou 2005).
Table 1.
Morphometric Studies of the Amygdala in Bipolar Disorder.
| Study | Sample | Age | Method | Age of Onset | Duration of Illness/# Episodes | Family History of Illness | Clinical Status at Testing | Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Pearlson et al 1997) | 27 BD 60 HC |
34.9±8.6 31.6±8 |
1.5T 3mm ROI |
NR | NR | NR | NR | NR | No substance abuse, other axis I conditions. | L amygdala volume decreased in BD |
| (Altshuler et al 1998) | 12 BD 18 HC |
50.8±13.3 53.4±11.1 |
1.5T 1.4mm ROI |
NR | NR | NR | Remitted | NR | No other axis I disorders | Bilateral enlargement of the amygdalae in BD |
| (Strakowski et al 1999) | 24 BD 22 HC |
27±6 28±6 |
MRI 1.5T 1mm ROI |
NR | 6±6 | NR | 14 manic, 10 mixed episode. | MS + AP | No substance abuse for 3+ months | Enlarged amygdala in BD. |
| (Altshuler et al 2000) | 24 BD 18 HC |
50.2±12.7 53.4±11.1 |
1.5T 1.5mm ROI |
26.6±10.4 | 23.6±11.4 | NR | Euthymic | AP, AD + MS | No substance dependence, alcohol abuse for 9+ months | Enlarged amygdala in BD |
| (Brambilla et al 2003a) | 24 BD 36 HC |
35±10 37±10 |
1.5T 1.5mm ROI |
19±7 | 15±9 | 11 with family history, 13 without | 13 euthymic, 10 depressed, 1 hypomanic | 15 patients on lithium. 9 not medicated. | No co-morbid conditions, including substance abuse. | Enlarged L amygdala in BD |
| (Blumberg et al 2003a) | 36 BD I 56 HC |
31±14.1 28.3±13.7 |
1.5T 1.2mm ROI |
Adults: 17.4±8 Adolescents: 13.1±9.5 |
NR | Yes | Adults: 32% manic, 23% depressed. Adolescents symptomatic | ±33% of adults + half of adolescents medication free. Balance on MS, AD + AP | ±33% of BD cohort with substance dependence. Adolescent BD with ADHD, ODD, PTSD, PD | Reduced BL amygdala volume in adolescents + adults with BD |
| (Chen et al 2004) | 16 BD (12 BD I, 3 BD II, 1 BD NOS) 21 HC |
16±3 17±4 |
1.5T 1.5mm ROI |
NR | NR | Yes | 14 euthymic, 2 mildly depresses | MS | 5 ADHD, 1 CD, 1 ODD | Trend for decreased L amygdala volume in BD. Patients with co-morbid diagnosis had smaller L amygdala than non-comorbid subjects |
| (DelBello et al 2004) | 23 BD 20 HC |
16±2 17±2 |
1.5T 1.5mm ROI |
14±3 | 2.4±2.1 | NR | Mixed or manic episode | 20 subjects on MS, 11 on AP. Minority on AD or stimulants. | No substance abuse in last 3 months. 10 subjects with ADHD. No head trauma or medical or neurological condition. | Decreased amygdala volume in BD |
| (Lyoo et al 2004a) | 39 BD I 43 HC |
38.3±11.6 35.7±10.1 |
1.5T 1.5mm VBM |
18.6±7.0 | 18.1±11.0 10.5±9.2 (manic episodes) 13.5±7.2 (depressive) |
NR | 22 depressed, 17 hypomanic/manic | ±50% on medication including lithium + MS. | No substance abuse in last 3 months, other axis I diagnosis, no antisocial PD, ADHD. | No difference in amygdala volume. |
| (Blumberg et al 2005b) | 10 BD 8 HC |
15.0±4.0 15.3±2.8 |
1.5T 1.2mm ROI |
NR | 2.5±0.4 | Yes | Both depressed + manic | Half of subjects on medication at first scan and 30% on medication at second scan. AP, MS, stimulants. | 1 ADHD, 2 LD, 1 social phobia, 1 ODD, 1 substance abuse. | Reduced amygdala volume in BD at both scans 1 and scan 2 (2-year interval). No longitudinal changes. |
| (Chang et al 2005b) | 20 BD 20 HC |
14.6±2.8 14.1±2.8 |
3T 1.5mm ROI |
NR | NR | Yes | Depressed + hypomanic | Patients on medication (MS, AD+ AP) except stimulants which were discontinued 24 hours prior to scan. | No pervasive developmental disorders, substance abuse. 16 ADHD, 7 anxiety disorder, 11 ODD. | Reduced BL amygdala volume in BD. Subjects with past lithium or valproate exposure had greater amygdala volumes |
| (Dickstein et al 2005) | 20 BD 20 HC |
13.4±2.5 13.3±2.3 |
1.5T 1.2mm VBM |
10.1±3.2 | NR | NR | Euthymic | AP, MS, AD | ADHD, psychosis, anxiety | Volume reduction of L amygdala in BD. 24; 5; −15 |
| (Frangou 2005) | 43 BD 43 HC |
42.9±11 | 1.5T 1.5mm VBM |
25.5±9.2 | 16.0±19.0 | Mixed | Remitted | MS + AP | NR | BL enlargement of amygdala in BD |
| (Rosso et al 2007) | 20 psychotic BD 23 HC |
23±3 25±3 |
1.5T 3mm ROI |
6 patients with family history. | 1st episode | 23±3 | 14 manic, 4 mixed, 2 depressed. | 40% lithium, 65% AP, 25% MS, 10% AD. | No substance abuse | Reduction in amygdala volume. More pronounced in RH and patients with a family history of illness |
| (Velakoulis et al 2006) | 34 affective psychosis 87 HC |
22.0±3.1 21.7±4.2 26.9±10 |
1.5T 1.5mm ROI |
NR | 1st episode | NR | NR | AP | No alcohol abuse, neurological disorders, head injuries. | Enlargement of R amygdala in both MDD and BD |
Table 2.
Functional Studies of the Amygdala in Bipolar Disorder.
| Study | Sample | Age | Method | Age of Onset |
Duration of Illness/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (al-Mousawi et al 1996) | 15 manic psychosis 10 depressed (6 psychotic) 10 HC |
44.4±11.7 50.5±20.5 40.1±12.4 |
18 F-FDG MRI 0.08T 12mm ROI |
NR | 119.47 months 137 months |
NR | Psychotic mania/depression | Benz, AD, MS + AP | No current substance abuse. | Decreased metabolism of L amygdala in manic group. | NR |
| (Yurgelun-Todd et al 2000) | 14 BD 10 HC |
31.5 NR |
fMRI 1.5T 6mm ROI |
22 | NR | NR | Stable out-patients | 85% MS 60% lith 92% AP |
No neurological disorder, head trauma, current substance abuse 30% with past history of substance abuse. | Increased activation of L amygdala in response to fearful but not happy faces in BD | NR |
| (Ketter et al 2001) | 43 BD 43 HC |
37.5±10.6 38.1±10.4 |
18 F-FDG | 18.8±9.9 | 18.3±10.4 | NR | Depressed, mildly depressed + euthymic | Unmedicated for 2+ weeks | NR | Increased metabolism of R amygdala in depressed BD patients only. | NR |
| (Drevets et al 2002b) | 15 BD 12 HC |
35±7.4 35±9.8 |
18 F-FDG 3.4mm MRI 1.5T ROI |
NR | NR | NR | 7 depressed, 7 remitted | No medication for 3+ weeks before study in depressed BD group Euthymic patients medicated with MS or AP | No substance abusers | Elevated activity of the L amygdala in depressed BD. Remitted BD patients showed intermediate activity levels. | −21; −7; 18 |
| (Lawrence et al 2004) | 12 BD 9 MDD 11 HC |
41±11 for full sample | fMRI 1.5T 7mm voxel-wise |
NR | 15.4±13.4 years (BD) 8±5 (MDD) |
NR | Mildly depressed (BD) Significantly depressed (MDD) |
BD: 5 AD, 5 AP, 7 MS, 3 lith MDD: 9 AD |
No head injury, substance abuse, comorbid conditions | BD patients showed a greater response to fearful and happy, but not sad faces in L amygdala. | −25; 10; −18 −15; 6; 16 |
| (Lennox et al 2004) | 10 BD 12 HC |
37.3±12.8 32.6±10.7 |
fMRI 3T voxel-wise |
NR | NR | NR | Manic | 8 Lith, 7 MS, 3 haloperidol, 4 olanzapine | NR | BD patients had attenuated BL activation of amygdala in response to sad faces | NR |
| (Altshuler et al 2005a) | 9 BD 9HC |
34.6±8 30.4±7.6 |
fMRI 3T 4mm (1mm gap) ROI |
NR | 14.8 years 4.2 manic episodes |
NR | Manic | 6 MS, 2 lith, 1 olanzapine | No left-handednesss, hypertension, head trauma | L amygdala overactivated in manic group in response to emotional faces | NR |
| (Bauer et al 2005) | 10 BD I 10 HC |
39.3±7.8 35.0±9.3 |
18 F-FDG Voxel-wise | NR | 20.4±7.0 | NR | Depressed | AD, MS, AP | NR | Activity in R amygdala and hippocampus decreased with levothyroxine treatment | 26; −2; −24 |
| (Blumberg et al 2005a) | 5 unmedicated BD 12 medicated BD 17 HC |
40.0±12.3 45±9.4 33.2±10.8 |
fMRI 7mm ROI |
NR | NR | NR | Various | 8 MS, 4 lith, 3 AD, 1 AP | 2 left-handers No comorbidity except 1 person with hypothyroidism |
Increased amygdala response to happy faces in unmedicated BD but decreased response in medicated BD | NR |
| (Rich et al 2006) | 22 BD 21 HC |
14.2±3.1 14.5±2.5 |
fMRI 3T ROI |
NR | NR | NR | Half euthymic, half depressed or hypomanic | 80% medicated | No pervasive developmental disorder, IQ<70, unstable medical illness, substance abuse for 2+ months | BD patients rated neutral faces as more hostile + fearful and showed greater activation of the L amygdala | −22; 4; −18 |
| (Mah et al 2007) | 13 BD II 18 HC |
43.0±8.4 39.0±8.0 |
18 F-FDG 4.25mm MRI 3T ROI |
20±10.5 | 22.9±12 | NR | Depressed | Lithium only | No substance abuse, psychotic features, rapid-cycling | Increased metabolism of BL amygdala | −24; −1; −20 22; −1; −18 |
| (Pavuluri et al 2007) | 10 BD 14 HC |
14.9±1.8 14.3±2.4 |
fMRI 3T 5mm (1mm gap) ROI |
NR | NR | NR | Euthymic | No medication for 1+ week. Previously on AP, MS and stimulants | No DSM comorbidity except ADHD. No neurological disorder, head trauma, substance use, IQ<80, medication affecting CBF | Increased activation of R amygdala in response to angry faces in BD | NR |
Resting state functional analyses have been largely limited to the adult population (Table 2) and are indicative of increased baseline amygdalar activity, (Ketter et al 2001) (Sheline et al 2001) (Drevets et al 2002b) (Bauer et al 2005) (Mah et al 2007) which correlates positively with severity of depression (Drevets et al 1992) (Ketter et al 2001).
MDD
The literature regarding the structural and functional changes of this region in MDD is in disagreement (Tables 3 and 4). Several studies have reported gray matter (GM) volume loss in euthymic (Sheline et al 1998) and depressed (von Gunten et al 2000) (Caetano et al 2004) (Hickie et al 2006), or psychotic (Keller et al 2008) patients, but many negative results have also been published. Resting state functional data are largely suggestive of hypermetabolism (Drevets et al 1992) (Drevets et al 2002b) (Anand et al 2005).
Table 3.
Morphometric Studies Implicating the Amygdala in Unipolar Depression.
| Study | Sample | Age | Method | Age of Onset | Duration of Illness/# Episodes | Family History of Illness | Clinical Status at Testing | Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Sheline et al 1998) | 20 MDD 20 HC |
54±18 53±17 |
1.5T 1.25mm |
NR | NR | NR | Largely euthymic | 14 patients on AD | No comorbid conditions | No group differences in overall amygdala volumes but BL reduction in core nuclei volumes in MDD. |
| (Bremner et al 2000) | 16 MDD 16 HC |
43±8 45±10 |
ROI | NR | 2±3 (episodes) | NR | Remitted | AD | No PTSD. 5 patients with history of substance abuse/dependence. 1 PD. | No between group differences |
| (von Gunten et al 2000) | 14 MDD (with memory complaints) 14 HC |
57.6 58.1 |
1.5T 5mm |
NR | ±6.5 | NR | Depressed | 7 AD, 2 BZ | No neurological disorders, substance abuse | Smaller L amygdala volume in MDD. |
| (Caetano et al 2004) | 31 MDD 31 HC |
39.2±11.9 36.7±10.7 |
1.5T 1.5mm ROI |
30.5±12.5 (remitted) 26.7±11.4 (depressed) |
12.3±8.4 (remitted) 11.0±11.7 (depressed) |
NR | 21 depressed; 10 remitted. | All patients off psychotropics for 2+ weeks. | No comorbid disorders except substance abuse in remission for 6+ months. | Trend towards smaller L amygdala volume in MDD |
| (Frodl et al 2004) | 30 MDD 30 HC |
48.4±13.4 45.7±12.9 |
1.5T 1.5mm ROI |
39.3±13.4 | 9.1±10.2 | NR | Depressed | AD + lithium | No co-morbid disorders | No differences in amygdala volumes |
| (Inagaki et al 2004) | 17 MDD 51 HC |
47.1±6 48.6±5 |
1.5T 1.5mm |
NR | 1.1±1.0 (episodes) | No | Remitted | No psychotropic medication for 1+ month but 29 on tamoxifen which may have anti-manic properties (Zarate et al 2007) | No substance abuse | No amygdala volume differences in cancer survivors |
| (Lange and Irle 2004) | 17 female MDD 17 female HC |
34±10 34±6 |
1.5T 1.3mm ROI |
29±10 | 5±5 | Yes – in 7 cases but no history of BD | Depressed | No history of psychosis. No PTSD, borderline PD | AD | Enlarged amygdala in MDD |
| (Hickie et al 2006) | 45 MDD 16 HC |
52.0±12.8 55.8±10.3 |
1.5T 1.5mm |
36.1±17.2 | 15.6±16.1 6.9±9.8 episodes |
NR | Depressed | 29/45 AD | No substance abuse but comorbid axis II disorders. No head injury, neurological illness, stroke, dementia | Smaller amygdala volume in MDD |
| (Frodl et al 2007) | 60 MDD 60 HC |
44.2±11.8 41.6±12.3 |
1.5T 1mm ROI |
37.7±11.7 | 6.7±8.7 | NR | Depressed | AD | No head injury, neurological disorders, substance abuse, and personality disorders, | No group differences |
| (Macmaster et al 2007) | 32 MDD 35 HC |
14.08±2.08 14.51±2.72 |
1.5T 1.5mm ROI |
11.77±2.92 | 27.70±27.68 months | Yes | Depressed | Medication naive | No psychosis, BD, OCD, PTSD, eating disorders, substance abuse, autism, LD, medical or neurological conditions | No group differences |
| (Tang et al 2007) | 14 MDD 13 HC |
29.5±6.84 29.46±6.86 |
1.5T 1.6mm ROI |
1st episode | 5.44±5.22 months | NR | Depressed | Medication naive | No medical or neurological disorder, head injury, substance abuse. 4 with GAD | Decreased volume of R amygdala in MDD. 22; 0; −16 |
| (Keller et al 2008) | 23 MDD (with psychosis) 19 MDD (without psychosis 22 HC |
36.5±13.2 36.6±11.9 32.2±11.5 |
3T 1.5mm ROI |
27.6±11.7 27.0±14.0 |
2.9±4.4 4.0±9.3 (episodes) |
NR | Depressed | AD, MS, AP, 4 no med 8 no med, 8 AD, 3 other |
No major medical illness, seizures, head trauma, unstable cerebrovascular, endocrine conditions. No treatment with steroids, hormone replacement therapy. No substance abuse within last 6 months | Smaller BL amygdala in psychotic but not non-psychotic MDD |
Table 4.
Functional Studies Implicating the Amygdala in Unipolar Depression.
| Study | Sample | Age | Method | Age of Onset |
Duration of Illness/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Drevets et al 1992) | 13 depressed MDD 10 remitted MDD 33 HC |
36.2±8.9 33.6±10.0 30.1±7.8 |
15O-H2O | NR | NR | Yes | Depressed/Remitted | Depressed sample unmediated for 3+ weeks before scan. Remitted sample unmedicated for at least 4 months. | No substance abusers, anti-social PD. No other axis I diagnoses. | Elevated activity of L amygdala in both remitted + depressed groups. | 21; 5; −14 |
| (Abercrombie et al 1998) | Sample 1: 10 MDD 11 HC Sample 2: 17 MDD 13 HC |
31.1±10.7 38.0±14.0 34.6±9.9 34.3±11.6 |
18 F-FDG ROI |
NR | NR | NR | Depressed | Medication free | No other axis I disorders except phobia and dysthymia. No DM, brain injury or thyroid disease. | No significant differences | NR |
| (Sheline et al 2001) | 11 MDD 11 HC |
40.3 39.8 |
fMRI 1.5T 8mm ROI |
NR | NR | NR | Depressed | Free of medication for 4+ weeks | No neurological trauma or disorder, physical illness, comorbid psychiatric disorder, substance abuse | MDD showed greater L amygdala activation to all faces, especially fearful faces which normalized with AD treatment | NR |
| (Thomas et al 2001) | 5 MDD 12 GAD 12 HC |
12.3±2.7 12.8±2.1 12.2±2.6 |
fMRI 5mm (2.5mm gap) ROI |
NR | NR | NR | Depressed | No medication for 2+ weeks | No nicotine, alcohol, drugs, psychotropic medication for 2+ weeks, medical or neurological illness, extreme obesity, eating disorders, schiz, LD, PTSD, IQ<80 | Compared with HC, anxious children showed exaggerated response to fearful faces while MDD showed blunted response in L amygdala. | −13; −4; −16 |
| (Drevets et al 2002b) | 12 MDD 12 HC |
36±8.7 35±9.8 |
18 F-FDG 3.4mm MRI 1.5T ROI |
NR | NR | Yes | Depressed | No medication for 3+ weeks before study in depressed BD group but euthymic patients medicated with MS or AP | No substance abusers | Elevated activity of the L amygdala in MDD | −21; −7; 18 |
| (Siegle et al 2002) | 7 MDD 10 HC |
34.3±8.8 36.1±6.7 |
fMRI 1.5T 3.8mm |
NR | 4 episodes | NR | Depressed | No tricyclics or nefazodone | No substance in last 6 months. No history of psychosis. | Sustained amygdala response to negative words in MDD relative to HC | −15; −4; −6 |
| (Davidson et al 2003) | 12 MDD 5 HC |
38.17±9.3 27.8±10.4 |
fMRI 1.5T 1mm ROI |
NR | NR | NR | Depressed | NR for baseline | No other axis I disorders except specific phobia or dysthymia. No neurological disorders | No group differences in BL amygdala activity in response to aversive visual stimuli. | −18; −6; −10 20; −4; −14 |
| (Canli et al 2004) | 15 MDD 15 HC |
35.1 30.7 |
fMRI 3T voxel-wise |
NR | NR | NR | Depressed | 7 patients on AD. | No history of psychosis, substance abuse in last 6 months, social anxiety disorder. | Decreased activity in R amygdala in response to happy stimuli. | 22; −6; −13 |
| (Fu et al 2004) | 21 MDD 19 HC |
43.2±8.8 42.8±6.7 |
fMRI 1.5T 8mm ROI |
NR | NR | NR | Depressed | No medication for 4+ weeks | No neurological trauma, disorder, comorbid axis I condition, substance within 2 months | Exaggerated response to sad faces in L amygdala which improved after treatment | −12; −5; −8 −11; −10; −12 |
| (Irwin et al 2004) | 12 MDD 14 HC |
38±3 28±2 |
fMRI 1.5T 7mm 18 F-FDG ROI |
NR | NR | NR | Depressed | Medication free | No axis I comorbidity, neurological trauma, disorder. | Reduced connectivity between L + R amygdala in MDD | 20; −4; −10 −21; −6; −9 |
| (Anand et al 2005) | 15 MDD 15 HC |
28±9 28±7 |
fMRI 1.5T |
NR | 19 | NR | Euthymic | Lithium | No medical illness | Increased activation of amygdala and insula in MDD. | NR |
| (Gotlib et al 2005) | 18 MDD 18 HC |
35.2 30.8 |
fMRI 3T voxel-wise |
NR | NR | NR | Depressed | 9 on AD | No brain injury, psychosis, social phobia, panic disorder + substance abuse in last 6 months | No significant differences in response to facial stimuli. | NR |
| (Surguladze et al 2005) | 16 MDD 14 HC |
42.3±8.4 35.1±13.2 |
fMRI 1.5T |
NR | 7.5±5.1 | NR | Depressed | AD | No head injury, substance abuse, dementia | MDD: Increased activation in amygdala to sad faces which was correlated with severity of depression. | −14; −7; −18 |
| (Neumeister et al 2006a) | 27 MDD 26 HC |
39.7±12.8 34.2±12.2 |
15O-H2O ROI |
NR | NR | NR | Remitted | Unmedicated | No medical illness | Greater rCBF in response to sad faces in MDD | NR |
| (Chen et al 2007b) | 19 MDD 19 HC |
43.3±8.6 42.8±6.7 |
fMRI 1.5T 7mm |
NR | NR | NR | Depressed | No medication for 4+ weeks prior to baseline scan | No axis I comorbidity, neurological trauma, disorder, substance abuse within 2 months | At baseline reduced functional coupling of amygdala with hippocampus, putamen, caudate, insula, temporal cortices, inferior and middle cortex in MDD. After 8 week treatment with fluoxetine no group differences. | 44; 42; 22 31; 32; 32 47; 37; 1 54; 18; 4 13; 49; 18 15; 22; 29 39; 30; 7 24; −1; 14 15; 14; 20 |
| (Dannlowski et al 2007) | 35 MDD | 38.6±12.2 | fMRI 3T ROI |
NR | 125±125.5 months 4.7 episodes |
NR | Depressed | AD | No history of mania, neurological illness, ECT, Benz treatment, age > 60, | Amygdala reactivity to masked negative faces predicted negative judgemental bias towards consciously viewed faces. | −18; −4; −12 22; 2; −20 |
| (Fales et al 2008b) | 27 MDD 24 HC |
33.4±8 36.4±9 |
fMRI 3T 3.2mm |
NR | NR | NR | Depressed | No medication for 4+ weeks | No axis I comorbidity, physical or neurological illness, brain trauma | Enhanced response of L amygdala to unattended fearful faces in MDD | −18; −5; −19 |
| (Siegle et al 2007) | 27 MDD 25 HC |
38±12.7 31.5±9.0 |
fMRI 3T 3.2mm |
NR | Median # episodes = 15+ | NR | Depressed | No medication for 2+ weeks | No excessive alcohol use. No physical illness, drug abuse for 6+ months. IQ>80 | MDD patients showed greater BL amygdala activity during the processing of emotionally-valenced verbal stimuli. | −22; −5; −15 |
The Hippocampus
The hippocampus, a key structure for the encoding of emotionally relevant data into memory, interacts with the amygdala to provide input regarding the context in which stimuli occur (LaBar and Cabeza 2006). This process is influenced by the hypothalamic-pituitary-adrenal (HPA) axis through the modulation of arousal (LaBar and Cabeza 2006) (Roozendaal et al 2006). In rodents the hippocampus in turn plays an inhibitory role in the regulation of the amygdala, and HPA axis activity (Jacobson and Sapolsky 1991).
MDD
Hippocampal volume reduction has been widely reported (Table 5). The authors of an earlier meta-analysis of the literature also came to the conclusion that hippocampal GM loss is characteristic of depression (Campbell et al 2004); an effect that (Stockmeier et al 2004) attribute to a decrease in neuropil - although see (Lucassen et al 2001).
Table 5.
Morphometric Studies of the Hippocampal Complex in MDD.
| Study | Sample | Age | Method | Age of Onset |
Duration of Illness/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Axelson et al 1993) | 19 MDD 30 HC |
46.7±7.4 56.6±19.1 |
1.5T 5mm ROI |
34±17 | 12.7±13.1 | NR | Depressed | NR | NR | No difference in hippocampal-amygdala complex volumes. Age negatively correlated with volume. |
| (Sheline et al 1996) | 10 MDD 10 HC |
68.5±10.4 68.0±9.5 |
1.5T 1.25mm ROI |
NR | 1293±1067 (days) | NR | Partially remitted | 8 AD | No drug or alcohol abuse | Smaller BL hippocampal volumes in MDD. Volume correlated negatively with duration of depression. |
| (Pantel et al 1997) | 19 MDD 13 HC |
72.4±8.8 68.2±5.3 |
1.5T 1.25mm |
64.2±9.2 | 26.7±6.6 (months) | NR | Depressed | NR | NR | No difference in hippocampal-amygdala complex volumes. |
| (Shah et al 1998) | 20 MDD (chronic) 20 MDD (remitted) 20 HC |
21–65 | VBM | NR | NR | NR | Depressed and remitted | AD | No mania, significant substance abuse, organic pathology or neurological illness | Chronic MDD group showed trend towards reduced GM density in the L hippocampus. −29; −18; −16 |
| (Ashtari et al 1999) | 40 MDD 40 HC |
74.3±6.0 71.4±0.3 |
1T 3.1mm ROI |
61.5±5.5 | 1.8±0.5 | NR | Depressed | NR | NR | No difference in hippocampal volumes. No relationship between # episodes + volume |
| (Sheline et al 1999) | 24 MDD 24 HC |
52.8±18.4 52.8±17.8 |
1.5T 1.25mm ROI |
NR | 1058±1032 (days) 4.8 (episodes) |
NR | Depressed | 16 on AD | No substance abuse, medical or neurological conditions | Smaller BL hippocampal volumes in MDD. No correlation between volume and age but duration of depression associated with volume |
| (Bremner et al 2000) | 16 MDD 16 HC |
43±8 45±10 |
ROI | NR | 2±3 (episodes) | NR | Remitted | AD | No PTSD. 5 patients with history of substance abuse/dependence. 1 PD. | Reduced L hippocampal volume in MDD. Trend for R hippocampus. No associationbetween volume and # episodes or hospitalisations |
| (Mervaala et al 2000) | 34 MDD (6 BD) 17 HC |
42.2±12.2 42.1±14.6 |
1.5T 8mm ROI |
NR | 31 months | NR | Depressed | AD | No substance abuse | Smaller L hippocampal volumes in MDD. Trend for R hippocampus. |
| (Steffens et al 2000) | 66 MDD 18 HC |
71.74±8.42 67.11±5.04 |
1.5T 3mm |
25.6 (N=28) 65.2 (N=38) |
NR | NR | Depressed | NR | No other “major” psychiatric illnesses. | Smaller BL hippocampal volumes in MDD. Weak negative association between age of onset and volume. No association between # of episodes + volume. |
| (Vakili et al 2000) | 38 MDD 20 HC |
38.5±10.0 40.3±10.4 |
1.5T 3mm ROI |
NR | NR | NR | Depressed | Fluoxetine | No active substance abuse | No significant differences in hippocampal volume. Negative correlation between severity of depression and volume. |
| (von Gunten et al 2000) | 14 MDD (with memory complaints) 14 HC |
57.6 58.1 |
1.5T 5mm |
NR | ±6.5 | NR | Depressed | 7 AD, 2 BZ | No neurological disorders, substance abuse | No difference in hippocampal volumes |
| (Rusch et al 2001) | 25 MDD 15 HC |
33.2±9.5 37.4±14.4 |
1.5T 1.2mm ROI |
NR | NR | Yes but not BD | Depressed | Free of medication for 4+ weeks. | No history of mania, psychosis or any other axis I disorder except dysthymia. | No hippocampal volume differences |
| (Bell-McGinty et al 2002) | 30 MDD 47 HC |
69.3±5.7 66.9±7.3 |
1.5T VBM |
NR | 1.8±0.9 (episodes) | NR | Depressed | NR | No other axis I disorders or substance abuse. No neurological disorders, untreated DM or hypertension | Smaller R hippocampal volume in MDD. Volume inversely correlated with age of onset. |
| (Frodl et al 2002) | 30 FE MDD 30 HC |
40.3±12.6 40.6±12.5 |
1.5T 3mm ROI |
40±12.5 | 0.71±0.9 | NR | Depressed | AD | No other axis I conditions, neurological disorders or had injury | Smaller L hippocampal GM volumes in male MDD. No association between illness duration or age and volume. |
| (Vythilingam et al 2002) | 21 MDD with history of childhood abuse 12 MDD without abuse 14 HC |
33±6 34±8 27±5 |
1.5T 1.5mm ROI |
NR | NR | NR | Depressed | NR | Anxiety disorders, especially PTSD more prevalent in abused MDD sample. | Smaller L hippocampal volume in MDD group with history of childhood abuse. |
| (MacQueen et al 2003) | 20 FE MDD. 17 multi-episode MDD. 20 HC 17HC |
28.4±11.8 35.9±11.1 28.4±11.5 36.2±11.9 |
1.5T 1.2mm ROI |
26.3±12 24.9±11.6 |
10 years 6 (episodes) |
Mixed | Depressed | FE MDD group medication naïve. AD in multi-episode group. | No substance abuse, anxiety disorders. | Hippocampal volume reduction in multi-episode patients. Correlation between duration of depression & hippocampal volume. |
| (Posener et al 2003) | 27 MDD 42 HC |
33.0±10.7 33.2±10.8 |
1.5T 1mm ROI |
NR | 0.8±1.2 (episodes) | NR | Depressed | Yes – not specified. | No substance abuse in last 3 months. No other axis I or II disorders. No neurological disorders, cardiovascular risk factors. | No differences in hippocampal volume but surface deformation |
| (Caetano et al 2004) | 31 MDD 31 HC |
39.2±11.9 36.7±10.7 |
1.5T 1.5mm ROI |
30.5±12.5 (remitted) 26.7±11.4 |
12.3±8.4 (remitted) 11.0±11.7 (depressed) |
Both | 21 depressed; 10 remitted. | All patients off psychotropics for 2+ weeks. | No comorbid disorders except substance abuse in remission for 6+ months. | Depressed patients had smaller hippocampal volumes than remitted patients. Inverse correlation between length of illness and L hippocampus. |
| (Frodl et al 2004) | 30 MDD 30 HC |
48.4±13.4 45.7±12.9 |
1.5T 1.5mm ROI |
39.3±13.4 | 9.1±10.2 | NR | Depressed | AD + lithium | No co-morbid disorders | No differences between hippocampal volumes in remitted group. Smaller R hippocampal volume in non-remitted group (N=12) at base-line and follow-up. No change in volumes over 1 year. |
| (Hastings et al 2004) | 18 MDD 18 HC |
38.9±11.4 34.8±13.6 |
1.5T 1.5mm ROI |
23±12.3 | 4.7±4.4 | Mixed | Depressed | NR | No current drug abuse | No volume changes of hippocampus. |
| (Inagaki et al 2004) | 17 MDD 51 HC |
47.1±6 48.6±5 |
1.5T 1.5mm |
NR | 1.1±1.0 | No | Remitted | No psychotropic medication for 1+ month. Tamoxifen. | No substance abuse | No hippocampal volume differences in cancer survivors |
| (Janssen et al 2004) | 28 MDD 41 HC |
64.04±10.9 62.37±11.38 |
1.5T 1.2–5mm ROI |
33.04±9.48 | 93.5±17.5 months | NR | Depressed | 22 AD, 4 lithium, 1 BZ. | NR | Smaller R hippocampal volume in MDD. |
| (Lange and Irle 2004) | 17 female MDD 17 female HC |
34±10 34±6 |
1.5T 1.3mm ROI |
29±10 | 5±5 | Yes – in 7 cases but no history of BD | Depressed | AD | No history of psychosis. No PTSD, borderline PD | Reduction in hippocampal volume in MDD |
| (Lloyd et al 2004) | 51 MDD (23 early onset; 28 late-onset) 39 HC |
72.7±6.7 75.1±5.8 73.1±6.7 |
1T 1mm |
38.7 (N=23) 72.0 (N=28) |
88.3 weeks; 5.1 (episodes) 24.3 weeks; 2.0 (episodes) |
NR | Depressed | AD | No drug or alcohol abuse | BL hippocampal atrophy in late-onset MDD compared with early-onset MDD + HC. No relationship between volume + lifetime duration of depression. |
| (MacMaster and Kusumakar 2004) | 17 MDD 17 HC |
16.67±1.83 16.23±1.61 |
1.5T 1.5mm ROI |
14.06±1.98 | 2.89±1.71 | Yes in 9/17 | Depressed | 14 treatment naive. 3 AD or methyphenidate | No neurological or serious medical illness. 2 substance abuse, 1 ODD. | BL (especially L) reduction in hippocampal volume in MDD |
| (O’Brien et al 2004) | 61 MDD 40 HC |
73.9±6.7 73.3±6.7 |
1T 1mm ROI |
NR | 2.2±2.7 (episodes) | NR | Depressed. 20% with psychotic features. | 51 AD, 7 lithium | No substance abuse, stroke, unstable medical illness | Decreased volume of hippocampus in MDD |
| (Hickie et al 2005) | 66 (14 BD) MDD 20 HC |
53.5±13.5 55.8±10.8 |
1.5T 1.5mm ROI |
38.4±16.3 | 15±15.8 | NR | Depressed | NR | No substance abuse | Reduced hippocampal volume. Effect stronger in late onset patients. Increasing age associated with smaller volumes |
| (Neumeister et al 2005) | 31 MDD 57 HC |
40.1±101 38.0±10.9 |
3T 0.6mm |
24.6±10.3 | 3.2±2.1 (episodes) | NR | Remitted | Unmedicated | No history of trauma or substance abuse | Total + posterior hippocampal volume reductions in MDD. |
| (Frodl et al 2006) | 34 MDD 34 HC |
45.5±11.9 43.6±13.2 |
1.5–3mm ROI |
38.8±12.4 | 6.8±8.8 | NR | Depressed | AD, 4 AP | No comorbidity | BL hippocampal GM + WM volume reductions in MDD. No correlation between illness duration + hippocampal volume. |
| (Hickie et al 2006) | 45 MDD 16 HC |
52.0±12.8 55.8±10.3 |
1.5T 1.5mm |
36.1±17.2 | 15.6±16.1 6.9±9.8 episodes |
NR | Depressed | 29/45 AD | No substance abuse but comorbid axis II disorders. No head injury, neurological illness, stroke, dementia | Smaller hippocampal volume in MDD |
| (Rydmark et al 2006) | 29 female MDD 28 HC |
47.7±4.9 47.6±4.2 |
1.5T VBM |
44.1±8.4 | Mostly 1st episode | NR | Partially remitted | AD | No hazardous alcohol or illicit drug use. | No hippocampal differences. |
| (Frodl et al 2007) | 60 MDD 60 HC |
44.2±11.8 41.6±12.3 |
1.5T 1mm ROI |
37.7±11.7 | 6.7±8.7 | NR | Depressed | AD | No head injury, neurological disorders, cortisol medication, substance abuse, and personality disorders, | Smaller hippocampal volumes in MDD. No association between duration of illness and volume |
| (Janssen et al 2007) | 13 early onset MDD 15 late-onset depression 22 HC |
70.38±8.3 72.67±6.7 71.05±7.5 |
1.5T | 33.62±8.8 69.93±6.4 |
NR | NR | Depressed | 4 lithium | Cerebrovascular risk factors not exclusion criterion. No neurological disorders, dementia, substance abuse | Smaller hippocampus in early-onset group only. |
| (Macmaster et al 2007) | 32 MDD 35 HC |
14.08±2.08 14.51±2.72 |
1.5T 1.5mm ROI |
11.77±2.92 | 27.70±27.68 months | Yes | Depressed | Medication naive | No psychosis, BD, OCD, PTSD, eating disorders, substance abuse, autism, learning disorders, medical or neurological conditions | Smaller L+R hippocampal volumes in MDD |
| (Keller et al 2008) | 23 MDD (with psychosis) 19 MDD (without psychosis 22 HC |
36.5±13.2 36.6±11.9 32.2±11.5 |
3T 1.5mm ROI |
27.6±11.7 27.0±14.0 |
2.9±4.4 4.0±9.3 (episodes) |
NR | Depressed | AD, MS, AP, 4 no med 8 no med, 8 AD, 3 other |
No major medical illness, seizures, head trauma, unstable cerebrovascular, endocrine conditions. No treatment with steroids, hormone replacement therapy. No substance abuse within last 6 months | No significant differences |
| (Tae et al 2008) | 21 MDD 20 HC |
41.7±11.0 41.9±10.3 |
1.5T 1.3mm ROI VBM |
33.2±13.0 | 3.9±3.3 (episodes) 80.0±67.0 months (duration) |
4 + 17 − |
Depressed | AD only | No childhood trauma, other axis I disorder, no current or past history of substance abuse/dependence, major medical illness, head trauma, steroid meds. | Smaller L hippocampus in MDD using both manual and VBM methods |
A significant number of studies have, however, failed to find evidence of hippocampal atrophy in depressed patients (Table 5) and based on these data we suggest that the following caveat obtains: The majority of studies reporting evidence of hippocampal atrophy have made use of elderly, middle-aged or chronically ill populations (see discussion).
BD
Regarding BD, although a few studies have indeed reported volumetric decrements, the majority of studies report preservation of hippocampal tissue (Table 7). Once again, pediatric and adult samples appear to produce different results with more evidence of volume loss in the former; although see (Ladouceur et al 2008) who found increased GM volume in the left hippocampus of the healthy offspring of parents with BD.
Table 7.
Morphometric Studies of the Hippocampus in BD.
| Study | Sample | Age | Method | Age of Onset | Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing | Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Altshuler et al 1991) | 10 BD I 10 HC |
39.8±9 37±12 |
0.5T 10mm |
NR | 2–39 years | NR | Euthymic | MS | NR | Decreased BL TL volume in BD. Duration of illness inversely correlated with TL volume in males |
| (Swayze et al 1992) | 48 BD 47 HC |
33.41 (M) 33.61 (F) |
0.5T 10mm ROI |
22.86±7.82 | 5.89±6.15 hospitalization | NR | NR | NR | NR | Volume of R hippocampus decreased in BD |
| (Pearlson et al 1997) | 27 BD 60 HC |
34.9±8.6 31.6±8 |
1.5T 3mm ROI |
NR | NR | NR | NR | NR | No substance abuse, other axis I conditions. | No hippocampal volume changes. |
| (Altshuler et al 1998) | 12 BD 18 HC |
50.8±13.3 53.4±11.1 |
1.5T 1.4mm ROI |
NR | NR | NR | Remitted | NR | No other axis I disorders | No hippocampal volume changes. |
| (Hirayasu et al 1998) | 16 FE affective psychosis (12 BD) 18 HC |
23.7±4 24.0±4.5 |
1.5T 1.5mm ROI |
NR | 1st episode | NR | 12 manic, 2 mixed, 2 depressed. | Medication naive | No substance abuse, head trauma, neurological disorders | Normal amygdala-hippocampal complex volume |
| (Sax et al 1999) | 17 BD 12HC |
27±6 27±5 |
1.5T 1mm ROI |
NR | NR | NR | Manic + mixed | 5 medication free. 12 on MS. 5 on AP. | NR | No change in hippocampal volume |
| (Strakowski et al 1999) | 24 BD 22 HC |
27±6 28±6 |
MRI 1.5T 1mm ROI |
NR | 6±6 | NR | 14 manic, 10 mixed episode. | MS + AP | No substance abuse for 3+ months | No change in hippocampal volume or association between length of illness and volume. |
| (Altshuler et al 2000) | 24 BD 18 HC |
50.2±12.7 53.4±11.1 |
1.5T 1.5mm ROI |
26.6±10.4 | 23.6±11.4 | NR | Euthymic | AP, AD + MS | No substance abusers but alcohol dependence included if patients sober for 9+ months. | No hippocampal volumes differences. |
| (Hauser et al 2000) | 25 BD I 22 BD II 19 HC |
41.8±10.5 39.4±10.2 33.2±7.1 |
0.5T 5mm ROI |
24 for BD I and 18 for BD II. | 18.2±11.8 (BD I) 21.1±9.1 (BD II) |
NR | Euthymic | NR | No substance abuse, chronic medical or neurological disorder | No change in hippocampal volume |
| (Strakowski et al 2002) | 18 FE BD 17 multiple episode BD 32 HC |
22±6 25±6 24±6 |
1.5T 1.5mm ROI |
1st episode: 20±5. Multiple episode: 15±4. | 2±3 10±5 |
NR | 32 psychotic, 16 mixed state | No prior treatment with medication in FE group. Multiple episode group on MS + AP | No substance abuse within 3+ months of scan. | No difference in hippocampal volume across groups. |
| (Blumberg et al 2003a) | 36 BD I 56 HC |
31±14.1 28.3±13.7 |
1.5T 1.2mm ROI |
Adults: 17.4±8 Adolescents: 13.1±9.5 |
NR | Yes | Adults: 45% euthymic, 32% hypomanic/manic, 23% depressed. All adolescents symptomatic | ±33% of adults + half of adolescents medication free. Balance of sample on MS, AD + AP | ±33% of BD cohort with substance dependence. # of adolescent BD with ADHD, ODD, learning disorders, PTSD + avoidant PD | Trend for reduced BL hippocampal volume in adolescents + adults with BD |
| (Brambilla et al 2003a) | 24 BD 36 HC |
35±10 37±10 |
1.5T 1.5mm ROI |
NR | 15±9 | 11 with family history. 13 without. | NR | 15 patients on lithium mono-therapy. 9 not medicated. | No comorbid disorders and substance abuse within last 6 months. | Normal hippocampal volume. Controlling for family history did not alter results. |
| (Beyer et al 2004b) | 36 BD 29 HC |
58.2±7.80 61.0±5.49 |
1.5T 3mm ROI |
NR | NR | NR | NR | 12 lithium, 5 valproate, 15 lithium-valpoate combination | No major psychiatric disorders, substance abuse. | Enlargement of L hippocampus in late-onset BD group. |
| (Lochhead et al 2004) | 11 (BD (7 BD I 4 BD II) 31 HC |
38.2±10 36±14 |
1.5T 1.5mm VBM |
24.3±9.2 | 9.0±6.4 episodes | NR | Depressed | No medication for 2+ weeks. | No comorbid disorders. | Decrease in volume of L parahippocampal gyrus −20; −21; −21 |
| (McDonald et al 2004a) | 38 BD 52 unaffected relatives 54 HC |
41±11.7 44±15.5 40.2±15.3 |
1.5T 1.5mm ROI |
22.6±5.5 | NR | Yes | NR | 33 BD on MS. 10 on AP. | No organic brain disease, head trauma, substance abuse in last 12 months. | Hippocampal volume preserved in BD |
| (Wilke et al 2004) | 10 BD 52 HC |
14.5±1.8 15±1 |
3T 1.5mm VBM |
NR | NR | NR | Six mixed and 4 manic | No medication 72 hours before scan. No data on medication type | No schizophrenia, learning disabilities or pervasive developmental disorders. | Reduced GM volume of BL medial TL |
| (Chang et al 2005b) | 20 BD 20 HC |
14.6±2.8 14.1±2.8 |
3T 1.5mm ROI |
NR | NR | Yes | Depressed + hypomanic | Patients on medication (MS, AD+ AP) except stimulants which were discontinued 24 hours prior to scan. | No pervasive developmental disorders, substance abuse. 16 ADHD, 7 anxiety disorder, 11 ODD. | No hippocampal volume differences between groups. |
| (Frazier et al 2005) | 43 BD 20 HC |
11.3±2.7 11.0±2.6 |
1.5T 1.5mm ROI |
7.0±3.8 | 2.8±3.1 | NR | 50% mixed, 16% manic, 11% depressed, 20% euthymic. | MS, AP, AD, stimulants, anticholinergics. | No substance abuse for 2+ months. No schizophrenia, autism, bulimia, anorexia or learning disorders. 27 ODD, 22 ADHD. | Reduced hippocampal volume in BD. Effect stronger in females. |
| (Strasser et al 2005) | 23 psychotic BD 15 non-psychotic BD 44 HC |
36.39±11.6 40.80±14.1 39.61±11.7 |
1.5T 1.5mm ROI |
NR | NR | Yes | NR | NR | No substance abuse | Significantly smaller L hippocampal volumes in psychotic BD |
| (McDonald et al 2006) | 38 BD 52 unaffected relatives 54 healthy controls |
41±11.7 44±15.5 40.2±15.3 |
1.5T 1.5mm ROI |
22.6±5.5 | 5.4±5.6 (hospitalizations) | Yes | NR | 33 MS. 10 AP | No substance abuse in last 12 months. | Hippocampal volume preserved in BD relatives |
| (Velakoulis et al 2006) | 34 affective psychosis (22 BD, 12 MDD) 87 HC |
22.0±3.1 21.7±4.2 26.9±10 |
1.5T 1.5mm ROI |
NR | 1st episode | NR | NR | AP | No alcohol abuse. | No hippocampal volume differences. |
| (Chen et al 2007c) | 24 BD I 25 HC |
38.2±11.0 38.4±11.1 |
1.5T 1.6mm VBM |
NR | 14.2±10.3 | Yes – in 14 subjects | NR | 12 Lith 12 MS |
No current substance use, neurological disease, head injury, other DSM diagnosis. | Increased L parahippocampal gyrus but smaller L middle temporal gyrus (BA 39) in BD −17; −19; −22 −44; −74; −13 |
| (Moorhead et al 2007) | 20 BD I 21 HC |
41.5±8.9 38.5±12.6 |
1.5T 1.7mm TBM |
NR | 14±8.4 |
NR | 45% euthymic (first round) 85% euthymic (second round) |
10 Lith 5 AP 7 MS |
No head injury, neurological disorder, drug dependence, LD. | Longitudinal study over 4 years. GM decline in L hippocampus in BD −39; −14; −18 |
| (Yucel et al 2007) | 28 BD 12 Lith+ 7 other MS 9 no meds 30 HC |
25.73±6.2 25.55±8.5 24.36±8.4 25.3±7.8 |
1.5T 1.2mm |
19.3±8.7 16±4.5 15.5±7.7 |
7±7.1 9.6±15.2 (episodes) 9.4±7.0 8.6±7.1 (episodes) 9.4±7.2 6.4±3.6 (episodes) |
NR | Mixed | 12 lith 7 MS 9 no med/AD |
No substance abuse, PTSD, untreated medical illness, head injury, neurological disorders, past history of drug treatment. | Larger hippocampal volume in Lith+ compared with untreated group. No difference between untreated group + HC |
| (Chepenik et al 2008) | 20 BD 18 HC |
40±9 28±12 |
1.5T 1.2mm ROI |
21±8 | 18 years (duration) | NR | 6 euthymic, 8 depressed, 5 manic | 6 no meds, 15 MS or AD | 2 panic disorder, 14 history of substance abuse. No medical neurological illness, head trauma | Smaller volume in BD |
The Basal Ganglia
The basal ganglia (BG), made up of the caudate, putamen, globus pallidus (GP), subthalamic nucleus (STN), and substantia nigra (SN) were traditionally conceptualized as a center of motoric integration (Pollack 2001) (DeLong and Wichmann 2007). This view evolved over time as the neuropsychiatric symptoms of Parkinson’s (Lieberman 2006) and Huntington’s disease (PD and HD) (Slaughter et al 2001) patients became clear, and neuropsychological case studies of affectively disturbed patients with BG lesions began to surface in the literature (Lauterbach et al 1997). More recently, deep brain stimulation of the STN, nucleus accumbens, ventromedial caudate, and GP has provided some relief to patients with obsessive compulsive disorder and PD-related depression (Kopell and Greenberg 2008). The current understanding is that motor, sensory and emotional data travel in parallel but segregated pathways between cortical and sub-cortical structures such as the BG.
For example, the dorsal and orbito-frontal aspects of the prefrontal cortex send major efferent projections to the dorsal, and anterior caudate, respectively, while the anterior cingulate cortex projects to the ventral surface of the striatum, respectively (Ferry et al 2000). In addition, the ventral or limbic striatum (ventral caudate, accumbens and olfactory tubercle), receives dopaminergic input from the SN and ventral tegmental area (VTA) (Utter and Basso 2007), glutamatergic input from the amygdala and thalamus, and serotonergic input from the dorsal raphe nucleus (Pollack 2001) (Bonelli et al 2006).
MDD
Several early studies raised the possibility of BG volume reductions in MDD, although with the exception of a recent pediatric study (Matsuo et al 2008), these data have generally not been replicated in subsequent analyses (Table 9). As in the case of BD there has been some suggestion that volume loss is associated with late age-of-onset (Greenwald et al 1997) and chronicity or severity of illness (Pillay et al 1998) (Lacerda et al 2003) - although see (Sheline et al 1999). Most recently, (Hickie et al 2006) failed to detect a MDD-associated decrease in striatal volumes. However, when the sample was stratified by serotonin transporter promoter polymorphism genotype (5-HTTLPR), striatal volume loss was observed in short allele carriers; indicating that genetic factors may contribute to the heterogeneity characteristic of the literature.
Table 9.
Morphometric Studies of the Basal Ganglia in Unipolar Depression.
| Study | Sample | Age | Method | Age of Onset | Duration of Illness/# Episodes | Family History of Illness | Clinical Status at Testing | Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Husain et al 1991) | 41 MDD 44 BD |
55.3±18.8 56.4±19.2 |
1.5T 5mm (2.5mm gap) |
NR | NR | NR | Depressed | NR | No major medical illness | Smaller putamen in MDD. Age negatively correlated with putamen size |
| (Krishnan et al 1992) | 50 MDD | 48.3±17 49.3±18 |
1.5T 5mm (2.5mm gap) |
NR | NR | NR | Depressed | NR | NR | BL reduction in caudate nucleus volumes in MDD |
| (Greenwald et al 1997) | 30 MDD 36 HC |
75.9±6.7 72.8±6.6 |
1T 3.1mm ROI |
45.7±14.1 (EO) 73.2±3.7 (LO) |
1.8±1.5 episodes | NR | Depressed | NR | No stroke, degenerative illness, other DSM diagnoses | Greater L caudate atrophy in late-onset (>60) compared with early-onset (<60) MDD |
| (Sheline et al 1998) | 20 MDD 20 HC |
54±18 53±17 |
1.5T 1.25mm |
NR | NR | NR | Largely euthymic | 14 patients on AD | No comorbid conditions | No differences in caudate |
| (Parashos et al 1998) | 72 MDD 38 HC |
55.4±16.8 55.1±17.1 |
1.5T 5mm ROI |
38.5±19.0 | NR | NR | Depressed | NR | NR | Reduced volume of caudate + putamen in MDD. Significant positive association between caudate volume + age of onset |
| (Pillay et al 1998) | 38 MDD 20 HC |
38.5±10.0 40.3±10.4 |
1.5T 3mm ROI |
NR | NR | NR | Mild to moderately depressed | No medication for 1+ week prior to study | No axis I disorders except phobias. No substance abuse, medical or neurological illness | No differences in caudate + lenticular nuclei. Severity of depression negatively correlated with L caudate volume |
| (Kim et al 1999) | 45 MDD | 65±7 |
1.5T 1.5mm ROI |
NR | NR | NR | Depressed | None | No other axis I disorders or substance abuse. No seizures, head trauma, cerebrovascular disease, neurological or medical illness | No significant differences between deluded + non-deluded MDD. |
| (Lenze and Sheline 1999) | 24 MDD 24 HC |
53 53 |
1.25mm ROI |
NR | NR | NR | Depressed | AD | No history of psychosis, psychiatric or medical conditions affecting the CNS | No significant differences in caudate + putamen. No effect of age of onset, severity of depression |
| (Bremner et al 2000) | 16 MDD 16 HC |
43±8 45±10 |
ROI | NR | 2±3 | NR | Remitted | AD | No PTSD. 5 patients with history of substance abuse/dependence. 1 PD. | No caudate volume differences |
| (Lacerda et al 2003) | 25 MDD 48 HC |
41±11 35±10 |
1.5T 5mm (1mm gap) ROI |
29.44±11.67 | 11.88±11.54 4.21±3.76 episodes |
NR | 10 euthymic, 15 depressed | Drug free for 2+ weeks before scan | No other axis I disorders, no substance abuse. | No differences in caudate, putamen + GP volumes. Inverse correlation between length of illness + L putamen volume |
| (Hannestad et al 2006) | 182 MDD 62 HC |
70.2±5.8 70.0±7.7 |
1.5T 3mm (3mm gap) ROI |
43.7±20.8 | NR | NR | Depressed | NR | No other DSM disorders, substance abuse, neurological illness. | No differences in caudate volume |
| (Hickie et al 2006) | 45 MDD 16 HC |
52.0±12.8 55.8±10.3 |
1.5T 1.5mm |
36.1±17.2 | 15.6±16.1 6.9±9.8 episodes |
NR | Depressed | 29/45 AD | No substance abuse but comorbid axis II disorders. No head injury, neurological illness, stroke, dementia | No differences in caudate + putamen but smaller caudate volumes in MDD subjects with S allele of 5-HTTLPR |
At least five studies (Table 10) have reported decreased activity of the striatum in MDD, and a tryptophan depletion study reported that severity of depression was associated with diminished activity of the caudate (Smith et al 1999).
Table 10.
Functional Studies of the Basal Ganglia in Unipolar Depression.
| Study | Sample | Age | Method | Age of Onset |
Duration of Illness/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Baxter et al 1985) | 11 MDD 9 HC |
34.7 30.8 |
18 F-FDG | NR | NR | NR | Depressed | Drug free for 1+ week prior to scanning | NR | Lower metabolic rate of caudate (normalized to whole hemisphere volume) in MDD | NR |
| (Baxter et al 1987) | 14 MDD 14 HC |
35.3±12.3 31.6±4.5 |
18 F-FDG | NR | NR | NR | Depressed | Free of drugs for 1+ week | NR | No significant differences in head of caudate | NR |
| (Drevets et al 1992) | 13 depressed MDD 10 remitted MDD 33 HC |
36.2±8.9 33.6±10.0 30.1±7.8 |
15O-H2O Voxel-wise | NR | NR | Yes | Depressed + euthymic | Depressed sample unmediated for 3+ weeks before scan. Remitted sample unmedicated for 4+ months. | No co-morbid conditions | Decreased activity in L caudate of depressed MDD | 8; 25; 16 |
| (Wu et al 1999) | 12 MDD responders 24 MDD non-responders 26 HC |
28.8±9.2 30.8±9.9 29.4±9.5 |
18 F-FDG | NR | NR | NR | Depressed | No medication for 2+ weeks | No axis I diagnoses or physical disorders | Decreased striatal metabolism in depressed patients. | −31; 21; 10 −22; −4; 10 |
| (Mayberg et al 2000) | 17 MDD | 49±9 | 18 F-FDG | NR | 2±1episodes | NR | Depressed | Scanned before and after treatment with fluoxetine | No history of psychosis or substance abuse. No other axis I disorders. No dementia, head injury, cerebrovascular illness | Decreased metabolism of caudate associated with treatment | −18; 16; 0 −16; 16; 2 18; 16; 0 |
| (Brody et al 2001) | 24 MDD 16 HC |
35.6±18.3 38.3±11.4 |
18 F-FDG | ±20 | NR | ±50% | Depressed | Scanned before and after treatment with paroxetine or psychotherapy. No medications for 2+ weeks prior to start of study. | Patients with history of substance abuse excluded. No other axis I disorders. | At baseline MDD group had greater activity in caudate | −16; 4; 16 14; −4; 14 |
| (Kennedy et al 2001) | 13 MDD 24 HC |
36±10 31.7±6.7 |
18 F-FDG | NR | 2.84±3.95 episodes | NR | Depressed | Scanned before and after treatment with paroxetine. Off medication of 4+ weeks prior to study. | No patients with concurrent DSM diagnosis. | Decreased metabolism of ventral striatum at baseline. Increase after treatment | 12; 20; −6 |
| (Videbech et al 2001) | 42 MDD 47 HC |
42±13 41±12 |
15O-H2O | NR | 2 episodes | NR | Moderately to severely depressed | AD | No substance abuse | No significant differences | NR |
| (Dunn et al 2002) | 31 MDD | 42.4±13.6 | 18 F-FDG | 15.9±13.1 | 26.7±14.6 | NR | Mildly to severely depressed | Unmedicated for 2+ weeks | No active substance abuse, eating disorder, OCD, dementia, medical illness | Anhedonia associated with decreased activity of the R striatum. | 14; 16; −4 32; 0; −4 |
| (Kegeles et al 2003) | 19 (14 MDD, 5 BD) 10 HC |
36±11 39±19 |
18 F-FDG | NR | NR | Yes | Depressed | BZ discontinued 24 hours before study in 12 cases. 7 subjects on BZ. Patients free of other medication for 2+ weeks. | 3 panic disorder, 2 dysthymia, 1 each with social phobia, simple phobia, anorexia + PTSD. No medical illness. | Lower activity of L putamen in MDD | −26; 8; −4 |
| (Saxena et al 2003) | 27 MDD | 38.1±11.3 | 18 F-FDG | NR | NR | NR | Depressed | Unmedicated for 4+ weeks | No axis I disorders, | Caudate activity not associated with response to paroxetine | NA |
| (Fu et al 2004) | 21 MDD 19 HC |
43.2±8.8 42.8±6.7 |
fMRI 1.5T 8mm ROI |
NR | NR | NR | Depressed | No medication for 4+ weeks | No neurological trauma, disorder, comorbid axis I condition, substance within 2 months | Exaggerated response to sad faces in L ventral striatum + caudate which improved after treatment | −21; −5; 12 −15; −4; −4 −20; 17; 16 −22; 12; 4 |
| (Holthoff et al 2004) | 41 MDD | 45.1±15.66 | 18 F-FDG voxelwise | NR | 1st episode in 54% of sample. 10 patients had more than 2 episodes | NR | Moderate to severely depressed | Treated with AD. BZ discontinued 3 days before baseline. | No substance abusers, axis II disorders | Decreased metabolism of the putamen upon recovery from depression | −24; 6; 14 26; 4; 14 |
| (Neumeister et al 2004) | 27 MDD 19 HC |
39.8±12.7 34.4±11.5 |
TD 18 F-FDG |
23.8±8.4 | 3.6±2.6 (episodes) | 23/27 | Euthymic | Unmedicated | No medical illness | TD associated with increased metabolism of ventral striatum | NR |
| (Mayberg et al 2005) | 6 MDD | 46±8 | 15O-H2O | 29.5±12 | 4.7±5 (episodes) | Yes - in 5 out of 6 subjects | Depressed | NR | No psychotic symptoms, substance abuse in last 3 months | Decreased metabolism of R caudate in MDD | 14; 2; 12 |
| (Neumeister et al 2006a) | 27 MDD 26 HC |
39.7±12.8 34.2±12.2 |
15O-H2O ROI |
NR | NR | NR | Remitted | Unmedicated | No medical illness | Reduced rCBF in ventral striatum in response to sad faces in MDD | NR |
| (Chen et al 2007a) | 17 MDD | 44.06±8.36 | fMRI 1.5T 3mm |
NR | NR | NR | Depressed | Scanned before and after treatment with fluoxetine. Patients off medication 4+ weeks before study. | No current axis I comorbidity or substance abuse within 2 months of study. Personality disorders not assessed. | Increased functional activation of caudate associated with decreased symptom severity at baseline | −11; 25; 1 |
BD
Compared to healthy controls, subjects with BD generally have not shown morphometric differences in the caudate or putamen (Table 11). These data are congruent with the reported absence of N-acetyl-aspartate (NAA) abnormalities in the BG of BD populations (Kato et al 1996) (Hamakawa et al 1998) (Ohara et al 1998). Nevertheless, a post-mortem study of a combined MDD and BD sample has reported volumetric reductions of the left nucleus accumbens, the bilateral pallidum, and the right putamen (Baumann et al 1999).
Table 11.
Morphometric Studies of the Basal Ganglia in BD.
| Study | Sample | Age | Method | Age of Onset | Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Swayze et al 1992) | 48 BD 47 HC |
33.41 (M)/33.61 (F) | 0.5T 10mm ROI |
22.86±7.82 | 5.89±6.15 (hosp) | NR | NR | NR | NR | No significant differences |
| (Strakowski et al 1993) | 17 BD 16 HC |
28.4±6.8 30.9±7.3 |
1.5T 6mm ROI |
NR | 1st episode | NR | Manic | Medication naive | No substance abuse for 1+ month | No significant differences |
| (Dupont et al 1995b) | 48 BD 47 HC |
33.41 (M)/33.61 (F) | 0.5T 10mm ROI |
22.86±7.82 | NR | NR | NR | NR | NR | No significant differences in the volume of caudate & putamen. |
| (Aylward et al 1994) | 30 BD 30 HC |
39.3±11.1 37.6±9.0 |
1.5T 5mm |
24.6±8.4 | NR | NR | 1 depressed, 2 manic, 2 mixed, 27 euthymic. | AD | No “substantial” substance abuse. No CNS illness, head injury, oral steroids. | Larger caudate in male BD |
| (Harvey et al 1994) | 26 BD 34 HC |
35.6 31.6 |
0.5T 5mm ROI |
23.2 | 4.1 (hosp) | NR | NR | 10 AD, 18 lithium | History of psychosis. No anorexia, alcohol abuse or hypertension | No difference in size of caudate |
| (Sax et al 1999) | 17 BD 12 HC |
27±6 27±5 |
1.5T 1mm ROI |
NR | NR | NR | Manic + mixed | 5 medication free, 12 MS, 5 AP | NR | No significant differences in caudate volume |
| (Strakowski et al 1999) | 24 BD 22 HC |
27±6 28±6 |
1.5T 1mm ROI |
NR | 6±6 | NR | 14 manic, 10 mixed episode. | MS + AP | No substance abuse for 3+ months | No significant differences in striatal volume. |
| (Brambilla et al 2001b) | 22 BD 22 HC |
36±10 38±10 |
1.5T 1.5mm |
20±7 | 16±9.15 | 10/12 | 10 depressed, 11 euthymic, 1 hypomanic | 14 lithium, 8 drug-free | No substance abuse for 6+ months | No differences in caudate, putamen or GP volumes. Length of illness predicted smaller L putamen |
| (Noga et al 2001) | 6 discordant BD TP 6 HC TP |
34.5±10.5 34.7±11 |
1.5T 2mm ROI |
23±9 | NR | Yes | NR | AP | No other axis I disorders. | Larger L caudate in affected & unaffected twins. Larger R caudate in affected BD twin compared to unaffected twin. |
| (Strakowski et al 2002) | 18 FE BD 17 multiple episode BD 32 HC |
22±6 25±6 24±6 |
1.5T 1.5mm ROI |
First episode: 20±5. Multiple episode: 15±4. | 2±3 10±5 |
NR | 32 psychotic, 16 mixed state | No prior treatment with medication in FE group. Multiple episode group on MS + AP | No substance abuse within 3+ months of scan. | No significant differences in putamen volume. Larger putamen in BD. |
| (Beyer et al 2004a) | 36 BD 35 HC |
58.8±7.91 63.2±5.25 |
1.5T 3mm (3mm gap) ROI |
NR | 15.92±16.58 | NR | NR | NR | NR | Smaller R caudate in BD. Effect stronger in late-onset cases, defined as > 45 years. |
| (DelBello et al 2004) | 23 BD 20 HC |
16±2 17±2 |
1.5T 1.5mm ROI |
14±3 | 2.4±2.1 | NR | Mixed or manic episode | 20 subjects on MS, 11 on AP. Minority on AD or stimulants. | No substance abuse in last 3 months or lifetime substance abuse of more than 1 year. 10 subjects with ADHD. | Enlarged putamen in BD |
| (Lochhead et al 2004) | 11 (BD (7 BD I 4 BD II) 31 HC |
38.2±10 36±14 |
1.5T 1.5mm VBM |
24.3±9.2 | 9.0±6.4 episodes | NR | Depressed | No medication for 2+ weeks. | No comorbid disorders. | No volumetric changes in BG |
| (McDonald et al 2004a) | 38 BD 52 unaffected relatives 54 HC |
41±11.7 44±15.5 40.2±15.3 |
1.5T 1.5mm ROI |
22.6±5.5 | NR | Yes | NR | 33 BD on MS. 10 on AP. | No organic brain disease, head trauma, substance abuse in last 12 months. | Increased genetic risk for BD associated with reduced volume of ventral striatum |
| (McIntosh et al 2004) | 26 BD 22 unaffected relatives 50 HC |
40.5±12.1 34.73±12.6 |
1.5T VBM |
NR | NR | Yes | NR | NR | NR | GM volume reductions in caudate in both BD subjects and their unaffected relatives. 2; −3; 13 −5; −1; 12 |
| (Wilke et al 2004) | 10 BD 52 HC |
14.5±1.8 15±1 |
3T 1.5mm VBM |
NR | NR | NR | Six mixed and 4 manic | No medication 72 hours before scan. No data on medication type | No schizophrenia, learning disabilities or pervasive developmental disorders. | Enlarged caudate + putamen in BD. |
| (Chang et al 2005b) | 20 BD 20 HC |
14.6±2.8 14.1±2.8 |
3T 1.5mm ROI |
NR | NR | Yes | Depressed + hypomanic | Patients on medication (MS, AD+ AP) except stimulants which were discontinued 24 hours prior to scan. | No pervasive developmental disorders, substance abuse. 16 ADHD, 7 anxiety disorder, 11 ODD. | No difference in caudate volumes. |
| (Dickstein et al 2005) | 20 BD 20 HC |
13.4±2.5 13.3±2.3 |
1.5T 1.2mm VBM |
10.1±3.2 | NR | NR | Euthymic | AP, MS, AD | No ADHD, psychosis, anxiety | Gray matter reduction in L nucleus accumbens. −6; 9; −7 |
| (Haznedar et al 2005) | 40 BD (BD I 17; BD II; 7 cyclothymia 16) 36 HC |
39.8±13.4 43.8±6.7 43.9±9.2 40.7±11.6 |
1.5T 1.2mm ROI |
NR | NR | Yes (10) | NR | BD II + cyclothymia samples medication free. BD I on MS + AP | “pathological gambling disorder”, 1 OCD, 1 panic disorder, 1 PTSD. No concurrent substance dependence, but previous history of abuse. | No differences in BG structures. |
| (Sanches et al 2005a) | 15 BD 21 HC |
15.9±3.2 16.9±3.8 |
1.5T 1.5mm ROI |
12±4.17 | 3.83±2.45 6.87±6.15 (episodes) |
Yes | Euthymic | 6 lithium, 4 valproate, 4 combination | No substance abuse in last six months | No differences in caudate and putamen volumes. |
| (Hwang et al 2006) | 21 drug-naïve BD 28 drug-treated BD 37 HC |
29.9±9.3 34.2±9.5 34.4±11.1 |
1.5T 1.5mm ROI |
NR | NR | NR | Depressed | 11 lithium, 7 MS, 10 AP. | No axis I or axis II disorders, substance abuse within last 3 months. | No differences in striatal volumes. R-sided shape differences in drug-free BD. |
| (Ahn et al 2007) | 46 BD 22 HC |
11.3±2.7 11.1±2.7 |
1.5T 1.5mm ROI |
6.8±4.1 | 2.6±2.9 | NR | 24 mixed, 8 manic, 9 euthymic, 5 depressed | 35 AP, 11 Lith, 18 MS, 15 AD, 11 stimulants, 7 alpha agonists, 2 benz | 35 ADHD, 18 psychosis, 12 anxiety. No LD, autism, eating disorders, schiz, current substance abuse, active medical or neurological disease | No significant differences in caudate, putamen, GP. |
There has however, been some suggestion of BD-associated striatal enlargement in adult (Aylward et al 1994); (Noga et al 2001); (Strakowski et al 2002) and pediatric (DelBello et al 2004); (Wilke et al 2004) samples, a point we will return to in the discussion.
To complicate matters further, reduced striatal volumes have been associated with length of bipolar illness (Brambilla et al 2001b) and an older age of onset (Beyer et al 2004a) suggesting a potential role for chronicity or cerebrovascular disease. This notion is consistent with reports of white matter lesions of the BG in elderly patients with MDD (Murphy et al 1992); (Greenwald et al 1996) (Iidaka et al 1996) although striatal volume reductions have also been reported to be a marker of disease-diathesis in the relatives of BD probands (McDonald et al 2004a); (McIntosh et al 2004).
Finally, metabolic activity or blood flow in the BG has been reported to be both increased and decreased in BD samples (Table 12). In manic or hypomanic samples striatal activity appears more generally increased relative to controls during tasks that normally activate the striatum (Blumberg et al 2000) (Caligiuri et al 2003) (Caligiuri et al 2006). For example, a recent fMRI study using a monetary incentive task noted that the expected differences in functional activity of the nucleus accumbens and ventral tegmentum in response to trials where a reward is received, compared to trials where a reward is not received, are attenuated in patients with mania (Abler et al 2008). In other words, subjects with mania show an inappropriate, generalized activation of reward circuitry. In bipolar depressed samples activity also is increased in the ventral striatum (Ketter et al 2001) (Bauer et al 2005) (Dunn et al 2002) (Mah et al 2007), but the direction and existence of physiological abnormalities in the remainder of the striatum has been more variable across studies (Table 12).
Table 12.
Functional Studies of the Basal Ganglia in BD.
| Study | Sample | Age | Method | Age of Onset |
Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Buchsbaum et al 1986) | 20 (16 BD + 4 MDD) 24 HC |
39±12.2 31±10.4 |
18 F-FDG | 24.8±10 | 16.8±11.5 | NR | NR | Unmedicated for 2+ weeks | NR | Decreased metabolism of the BG | NR |
| (Schwartz et al 1987) | 9 MDD 13 HC |
NR | 18 F-FDG | NR | NR | NR | Depressed | Drug free for 1+ week prior to scanning | NR | No difference in metabolic rate of caudate (normalized to whole hemisphere volume) in BD | NR |
| (Martinot et al 1990) | 7 BD 10 HC |
49±15 38±11 |
18 F-FDG | NR | NR | NR | Severely depressed | At baseline medicated with AP + BZ. Incomplete drug washout for other medications. | Substance abusers excluded. | No significant metabolic differences in striatal regions | NR |
| (Blumberg et al 2000) | 11 BD | 33.4±11.6 | 15O-H2O | NR | 14.2±14.9 (manic) 12.0±5.6 (euthymic) |
NR | 5 manic BD; 6 euthymic | MS, AP, AD, BZ | No comorbid axis I or II conditions. Substance abuse taking place > 5 years previously was allowed. | Increased L caudate activity in manic patients. | −16; 20; 0 |
| (Ketter et al 2001) | 43 BD I + II (treatment resistant) 43 HC |
37.5±10.6 38.1±10.4 |
18 F-FDG | 18.8±9.9 | 18.3±10.4 | NR | Depressed, mildly depressed + euthymic | Unmedicated for 2+ weeks | NR | Increased metabolism of ventral striatum in BD. | NR |
| (Dunn et al 2002) | 27 BD | 36.7±11.3 | 18 F-FDG | 18.0±9.9 | 16.7±14.6 | NR | Mildly to severely depressed | Unmedicated for 2+ weeks | No active substance abuse, eating disorder, OCD, dementia, medical illness | Anhedonia associated with decreased activity of the R striatum increased activity of L nucleus accumbens + caudate | 12; 18; 0 −4; 6; −4 |
| (Blumberg et al 2003c) | 10 BD 10 HC |
13.6±2.8 14.6±2.8 |
fMRI | NR | NR | Yes | Depressed | 4 lithium, 3 MS, 3 AD, 2 AP, 1 stimulant | No substance use within 24 hours of scan. 2 ADHD, 2 ODD, 2 substance abuse, 1 OCD, 1 anxiety, 1 phobia. | Elevated activity of L putamen during stroop. Greater depression associated with signal increase in ventral striatum. | NR |
| (Caligiuri et al 2003) | 24 BD 13 HC |
45.7±11.8 35.6±15.7 |
1.5T ROI Motor Probe |
NR | NR | NR | Manic + depressed | AP, MS, AD | No co-morbidity. Family-history of illness not exclusion criterion for HC. | Manic but not depressed patients showed elevated BOLD response in L GP + lower activity of R GP. Depressed subjects showed increases in caudate relative to manic patients. | NR |
| (Chang et al 2004) | 12 BD (I+II) 10 HC |
14.7±3.0 14.4±3.2 |
fMRI 3T Voxel-wise |
NR | 3.1 | Yes -56% | Euthymic | MS + AD. Stimulants discontinued 24 hours before screening. | 11/12 with ADHD. No substance abuse, pervasive developmental disorders. | Increased activation of L caudate in BD after working memory task. | −4; 14; 0 |
| (Bauer et al 2005) | 10 BD I 10 HC |
39.3±7.8 35.0±9.3 |
18 F-FDG voxelwise |
NR | 20.4±7.0 | NR | Depressed | AD, MS, AP | NR | Higher activity of the R vental striatum at baseline in BD | 18; 8; −8 |
| (Caligiuri et al 2006) | 10 BD | 49.5±11.9 | 1.5T ROI Motor Probe |
NR | NR | NR | 10 depressed, 2 manic, 1 mixed | 7 AD, 6 MS, 3 AP | NR | Greater caudate + L GP activity in euthymic + hypomanic subjects compared to normative sample. Negative correlation between severity of depression + activity of R GP | NR |
| (Mah et al 2007) | 13 BD II 18 HC |
43.0±8.4 39.0±8.0 |
18 F-FDG | 20±10.5 | 22.9±12 | NR | Depressed | Lithium | No substance abuse within 90 days, substance dependence within 5 years. No current psychotic features. 1 OCD, 1 eating disorder | Increased activity in the ventral striatum in BD | −14; 11; −7 16; 11; −6 −10; 10; 1 14; 10; 5 −22; 8; −2 26; 8; −2 30; 4; 0 18; 8; 5 |
Ventricular Abnormalities
Substantial tissue loss in the medial-temporal lobe, lateral PFC or BG in MDD or BD may be reflected by enlargement of the adjacent ventricular system. The evidence for ventricular enlargement (mostly of the third or lateral ventricles) in MDD and BD is mixed. Almost all reports of ventricular enlargement have been obtained in elderly or chonically depressed samples with late-onset illness (Coffey et al 1989) (Rabins et al 1991) (Salloway 1996) (Dahabra et al 1998) (Simpson et al 2001) and given the evidence that familial MDD usually manifests early in life (Kovacs et al 1997) (Kendler et al 2005) (Nierenberg et al 2007), this suggests that periventricular tissue loss does not have a purely genetic etiology. One possibility is cerebrovascular disease, as discussed in the following section.
White Matter Changes
A higher than normal incidence of deep frontal white matter hyperintensities (WMH), especially WMH of the deep frontal cortex and BG, appears characteristic of MDD and BD samples who manifest with late age-of-illness onset (Krishnan et al 1991); (Figiel et al 1991); (Hickie et al 1995) (Steffens et al 1999) (Hannestad et al 2006).
WMH appear as bright high intensity signals seen on T2-weighted MRI scans that are caused by circumscribed increases in water content (Ovbiagele and Saver 2006). As discussed by (Ovbiagele and Saver 2006) they are most likely indicative of leukoaraiosis: a decrease in the density of white matter due to demyelination, atrophy of the neuropil, and ischemia-associated microangiopathy, among others. The phenomenon is non-specific, being prevalent in elderly populations, generally. According to (Kertesz et al 1988) almost all individuals will display WMH by the age of 85.
Diffusion tensor imaging (DTI) is another method of assessing WM integrity. Theoretically, damage to cellular tissue causes parallel changes in the rate of diffusion of water across the affected cellular membranes, and this so-called proton diffusibility can be measured with DTI (Bammer 2003).
MDD
While the onset of MDD peaks in adolescence and young adulthood, an increased incidence is also seen in elderly individuals (Paykel et al 2005), contributing to the idea that vascular pathology plays a role. The term “vascular depression” was initially proposed to describe depressive symptomatology associated with multiple subcortical infarcts of an ischemic origin (Alexopoulos et al 1997) (Krishnan et al 1997).
With few exceptions (Dupont et al 1995a); (Greenwald et al 1996); (Sassi et al 2003); (Rainer et al 2006), extant evidence supports the existence of vascular depression. Both epidemiological studies of elderly community-based samples and cross-sectional analyses of matched control and MDD groups detail the intimate relationship between late-onset depression and WM lesions (Table 13).
Table 13.
White Matter Hyperintensities in MDD.
| Study | Sample | Age | Method | Age of Onset | Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status |
Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Coffey et al 1988) | 67 MDD referred for ECT | 71.6 (60–86) | Both MRI + CT MRI: 5mm (2.5mm gap). CT: 10mm |
After age 60 in 58% of cases | NR | Yes – 43% | Depressed | Tapered off medication | 35 heart disease or hypertension, 8 DM, 4 COPD, 2 DVT, 2 dementia | WMH found in 44 MDD |
| (Krishnan et al 1988) | 35 MDD | NR | 1.5T 10mm |
12<45 23>45 |
NR | NR | Depressed | AD | No dementia. Greater incidence of medical problems in older group. | Higher rate of PVH in late onset group |
| (Coffey et al 1989) | 51 MDD | 71.3 | 1.5T 5mm (2.5mm gap) |
80% > 60 | NR | NR | Depressed | Variety of medication for medical illness. 27% with a previous course of ECT. | 10 patients with history of dementia, 4 alcohol abuse. Cardiovascular risk factors in 58% of sample. | PVH in 100% of sample. WMH in 86% of sample. |
| (Dolan et al 1990) | 10 MDD 13 HC |
47±11 46±7 |
0.08T 12mm ROI |
31±9 | 11±7 | NR | Depressed | AD, BZ | No significant medical illness or alcohol abuse. | Greater mean T1 relaxation times in frontal WH in MDD. |
| (Zubenko et al 1990) | 67 MDD 44 HC |
73.2±6.5 68.0±6.2 |
1.5T 5mm 91-2.5mm gap) |
62.5±16.0 | NR | NR | Depressed | NR | NR | Increased incidence of infarcts + leukoencephalopathy in MDD |
| (Deicken et al 1991) | 90 psychiatric patients (31 MDD) | 43.9±21.5 46.7±21.9 |
0.5T 5mm (2.6mm gap) |
NR | NR | NR | NR | NR | Large variety of cardiovascular risk factors | 42% of patients + 12% of HC showed deep WMH. Mean age for patients with and without WMH was 62 and 32 |
| (Rabins et al 1991) | 21 MDD 14 HC |
23–79 60+ |
1.5T ROI |
54.2±17.1 | NR | NR | Depressed | NR | No neurological disease or head trauma | Greater severity of WMH but not PVH in MDD |
| (Guze and Szuba 1992) | 119 MDD (44 young + 75 old) 60 HC (30 young + 30 old). |
33.4 66.2 34.1 68.7 |
0.3T 7mm (3mm gap) |
21 (young) 43 (old) |
11.6 (young) 24.2 (old) |
NR | Depressed | NR | NR | Old MDD group had more WMH than young MDD and old HC. Young defined as less than 45 years of age |
| (Coffey et al 1993) | 48 MDD 76 HC |
62.4±16.4 61.6±15.9 |
1.5T 5mm (2.5mm gap) ROI |
NR | NR | NR | Severely depressed | 30 free of medication for 2.5 days (median). Remainder on Benz, AD + AP | No substance abuse, neurological disorder. 13 with hypertension or heart disease, 2 with COPD. | Greater number of PVH in MDD |
| (Fujikawa et al 1993) | (1) 31 young, early onset MDD (2) 70 young, late onset MDD (3) 41 old, early onset depression (4). 63 old, late-onset depression |
56.7±3.6 58.2±3.6 67.6±2.4 72.8±5.3 |
0.5T 10mm |
Early-onset < 50 Late-onset > 50 |
NR | NR | Depressed | NR | NR | Frequency of silent cortical infarcts: (1) 22.6% (2) 51.4% (3) 65.9% (4) 93.7% |
| (Howard 1993) | 12 MDD 12 HC |
76.0±6.5 77.7±7.9 |
1.5T 8mm (0.8mm gap) |
>45 | NR | NR | Severely depressed | NR | No neurological disorders, stroke or alcohol abuse. Groups matched for cardiovascular risk factors. | Trend for PVH + WMH to be more severe in MDD. |
| (Dupont et al 1995b) | 33 MDD 32 HC |
38.9±10.2 39.2±8.9 |
1.5T 5mm (2.5mm gaps) |
±25 | NR | Mixed | Depressed | 13 AD, 18 no medication | No substance abuse in last 5 years. No hypertension, head injury | No significant differences |
| (Hickie et al 1995) | 39 MDD | 64.4 | 1.5T 5mm (2.5mm gap) |
NR | 63±54.9 weeks | 19/39 | Severe depression with history of psychosis | AD, lithium, ECT | Positive history of hypertension + cerebrovascular risk factors. 6/39 with alcohol abuse. | Late onset group (>50) showed more WM changes than earlier onset group. WMH associated with negative family history of depression + poor response to treatment. |
| (Lewine et al 1995) | 27 MDD 150 HC |
40±11 33±9 |
1.5T 5–8mm |
±35 | NR | NR | NR | NR | No neurological or medical disorders. No current substance abuse. | Deep WMH more common in MDD |
| (Greenwald et al 1996) | 48 MDD 39 HC |
74.6±6.1 72.6±6.4 |
1T 7mm (0.7mm gap) |
62.4±15.2 | NR | NR | Depressed | NR | No dementia, history of stroke or other DSM diagnosis. 19 MDD with hypertension, 7 heart disease, 6 DM. Similar rates in HC. | No significant differences in WMH |
| (Iidaka et al 1996) | 30 MDD 30 HC |
67.7±5.4 66.3±4.7 |
1.5T 5mm |
61.8±9.4 | NR | 9/30 | Depressed | NR | Matched for cerebrovascular risk factors. | More PVH but not WMH in frontal lobes + BG in MDD |
| (O’Brien et al 1996) | 60 MDD 39 HC |
71.2±7.9 71.4±11.0 |
0.3T 5mm (0.5–2.5mm gap) |
NR | NR | NR | Depressed | NR | No PD, epilepsy, substance abuse, insulin-dependent DM | Deep WMH in BG and frontal lobes more common in MDD group. Patients with late-onset MDD had more WMH than early-onset MDD. |
| (Salloway et al 1996) | 30 MDD | Early onset: 73.3±7.8 Late onset: 77.5±4.4 |
1.5T 5mm (2.5mm gap) |
“Early” onset: 35.8±16.4 “Late” onset: 72.4±7.1 |
± 37 (early onset) ± 5 (late onset) |
NR | Depressed | NR | No neurological disorders or substance abuse | More deep WMH + PVH in late onset group. |
| (Dahabra et al 1998) | 23 MDD | 66.2±5.1 | 0.5T 7mm (1mm gap) |
12 >55 11 <50 |
NR | NR | Euthymic | AD, 7 lithium | No substance abuse, epilepsy, heart disease, neurological or endocrine disorders. | Greater severity of WMH in late-onset MDD |
| (Greenwald et al 1998) | 35 MDD 31 HC |
74.7±6.4 72.9±4.7 |
1T 5mm (2.5mm gap) ROI |
56.5±17.1 | NR | NR | Depressed | NR | No dementia, stroke, other DSM diagnoses. Patients and controls matched for other cerebrovascular risk factors. | Depression associated with L deep frontal and L putaminal WMH |
| (Lenze et al 1999) | 24 MDD 24 HC |
52.7±18.4 | 1.5T 5mm |
19 early onset (25.4±6.4). 5 late onset (59.2±6.6) | 151±147 (weeks) | Yes - 75% (79% early-onset; 60% late-onset) | Depressed | AD | No neurological, endocrine and cerebrovascular disorders. No hypertension. | No significant differences in total number of lesions |
| (Sato et al 1999) | 3371 people drawn from background population | 72.2 | 1.5T 5mm |
NR | NR | NR | NR | NR | No cancer but a variety of cardiovascular risk factors. | WMH associated with depressive symptomatology |
| (Steffens et al 1999) | 3660 people drawn from background population | Approximately 75 | 1.5T | NR | NR | NR | NR | NR | NR | Number of WMH in BG associated with depressive symptoms as measured with a psychometric scale after controlling for hypertension + cardiovascular disease. |
| (de Groot et al 2000) | 1077 non-demented adults. | 60–90 | 1.5T 5–6mm (20% gap) |
NR | NR | NR | NR | NR | No dementia | People with severe WMH were 3–5 times more likely to have symptoms of depression. WMH associated with older age of onset (>60). |
| (Kumar et al 2000) | 51 MDD 30 HC |
74.3±6.56 69.43±6.09 |
1.5T 5mm |
35 patients had onset after age 60 | NR | NR | Depressed | AD, BZ | No neurological disorders, dementia or substance abuse. Both MDD + HC had heart disease, DM | Increase in lesion volume in MDD |
| (MacFall et al 2001) | 88 MDD 47 HC |
72.6±7.9 72.2±6.3 |
1.5 3mm VBM |
49.3±22.6 | NR | NR | Depressed | NR | NR | Trend towards more deep WMH in MDD |
| (Murata et al 2001) | 20 early onset MDD 27 late onset MDD |
62.7±6.7 60.3±6.9 |
1.5T 5mm |
Early onset: 39.7±8.8 Late onset: 65.6±5.4 |
2.78±0.89 episodes (early) 1.47±0.68 episodes (late) |
NR | Depressed | AD, BZ | Incidence of cardiovascular risk factors not different across groups | More severe WMH in late onset group. |
| (Nebes et al 2001) | 92 healthy volunteers | 73.6±3.4 | 1.5T 5mm (1mm gap) |
NR | NR | NR | NR | 1 person on AD | No PD, HD, AD, schizophrenia, BD, alcoholism, head injury | Deep WMH but not PVH associated with level of depression. |
| (Tupler et al 2002) | 115 MDD (69 late-onset, 46 early onset) 37 HC |
66.7±10.9 65.9±9.4 |
1.5T 5mm (2.5mm gap) |
NR | NR | NR | Depressed | NR | No exclusion for comorbid medical illness except dementia | More severe WMH rating in deep frontal regions in late-onset cases. Early-onset defined as <50 |
| (Sassi et al 2003) | 17 MDD 38 HC |
42.8±9.2 36.8±9.7 |
1.5T 5mm |
7/17 <30 10/17 >30 |
NR | Mixed | NR | No medication for 2+ weeks before scan | No neurological disorders, axis I co-morbidity or substance abuse | MDD patients with longer illness duration had more WMH. The early-onset group had more WMH than HC. MDD subjects with a positive-family history had more WMH than their counterparts with no history. |
| (Silverstone et al 2003) | 11 MDD 19 HC |
34.4 35.9 |
0.5T 5mm (2.5mm gaps) |
26.6 | 7.8 | NR | Depressed | NR | No neurological disorders, cardiovascular disease, DM or head injury | No between group differences |
| (Firbank et al 2004) | 29 MDD 32 HC |
75.7±5.9 74.9±7.0 |
1.0T 5mm (1.5mm gap) VBM |
NR | ±21.5 ±4 episodes |
NR | Depressed | NR | No dementia, substance abuse, history of stroke, ischemic attack. Other vascular risk factors allowed. | Greater frontal lobe WM lesion volume in MDD. Differences between groups greater after exclusion of subjects with hypertension, DM and heart disease |
| (Janssen et al 2004) | 28 MDD 41 HC |
64.04±10.9 62.37±11.38 |
1.5T 1.2–5mm ROI |
33.04±9.48 | 93.5±17.5 months | NR | Depressed | 22 AD, 4 lithium, 1 BZ | NR | No differences in WMH |
| (Kumar et al 2004) | 8 MDD 8 HC |
71.5±5.13 74.1±8.90 |
MT-MRI 1.5T 3mm ROI |
NR | NR | NR | Depressed | Off medication for 2+ weeks | No neurological disorders including dementia | Abnormalities in the WM of the R caudate + R putamen in MDD |
| (Lloyd et al 2004) | 51 MDD (23 early onset; 28 late-onset) 39 HC |
72.7±6.7 75.1±5.8 73.1±6.7 |
1T 1mm |
38.7 (N=23) 72.0 (N=28) |
88.3 weeks; 5.1 (episodes) 24.3 weeks; 2.0 (episodes) |
NR | Depressed | AD | No drug or alcohol abuse, neurological or serious medical disorders. | No differences between groups |
| (Firbank et al 2005) | 629 subjects from background population | NR | 5mm | NR | NR | NR | NR | NR | 439 with hypertension, 184 with history of stroke, | Level of depression associated with severity of WMH |
| (Heiden et al 2005) | 31 MDD | 68.0±6.5 | 1.5T 6mm (0.6mm gap) |
47–51 | NR | NR | NR | AD | NR | Extent of WMH associated with severity of depression after 5 year follow-up. Severity of WMH associated with poorer outcome. |
| (Jorm et al 2005) | 475 background volunteers. 17 classified as MDD. | 60–64 | 1.5T 2mm |
NR | NR | NR | Depressed | NR | NR | Association between total brain WMH + depression. Remitted subjects taking AD intermediate to depressed patients + HC. |
| (Minett et al 2005) | 60 patients attending memory clinic (12 MDD) | 72.6±4.7 | 1.5T 5mm (0.5mm gap) |
NR | NR | NR | NR | NR | No dementia, severe medical or neurological disease, current psychiatric disorders or alcohol abuse | Late-onset depression associated with WMH severity |
| (Taylor et al 2005) | 253 MDD 146 HC |
70.48±6.23 69.85±7.54 |
1.5T 3mm |
NR | NR | NR | Depressed | NR | No other major psychiatric disorders such as BD. No substance abuse or neurological disorders. Hypertension + heart disease more common in MDD | Greater WM lesion volumes in MDD |
| (Bae et al 2006) | 106 MDD 84 HC |
70.4±6.4 71.7±6.0 |
DTI 1.5T 3mm ROI |
NR | NR | NR | Depressed | NR | NR | Loss of WM integrity in middle + superior frontal gyri + ACC |
| (Chen et al 2006) | 164 MDD 126 HC |
68.93±7.04 69.83±6.25 |
1.5T 3mm (3mm gap) |
NR | NR | NR | Depressed | Yes – not specified | No current substance abuse, psychiatric or neurological illness. | Greater volume of WM lesions at baseline + at 2-year + 4-year follow-up in MDD |
| (Hannestad et al 2006) | 182 MDD 62 HC |
70.2±5.8 70.0±7.7 |
1.5T 3mm (3mm gap) ROI |
43.7±20.8 | NR | NR | Depressed | NR | No other DSM disorders, substance abuse, neurological illness. | Greater volume of WML in MDD. |
| (Iosifescu et al 2006) | 84 MDD 35 HC |
40.7±10.2 39.3±9.8 |
1.5T 3mm |
NR | NR | NR | Depressed | No medication | No BD, psychosis, substance abuse within last 21 months, organic mental disorder, seizure disorder, unstable medical illness. | No difference in prevalence of WMH. WMH correlated with cardiovascular risk score. |
| (Nobuhara et al 2006) | 13 MDD 13 HC |
62.8±6.6 61.5±4.8 |
DTI 1.5T 6mm (2mm gap) ROI |
52.9±7.3 | 4.0±2.6 | NR | Depressed | AD | No dementia, severe medical illness, neurological disorders | Loss of integrity of WM frontal and temporal tracts. |
| (Rainer et al 2006) | 51 MDD 204 HC |
75.8 (whole sample) | 1T | >65 – not specified | NR | NR | Depressed | AD, BZ | Groups matched for cardiovascular risk factors. | No differences in incidence of WMH |
| (Versluis et al 2006) | 527 background population | 74.9 | 1.5T 3mm |
NR | NR | NR | NR | NR | Cerebrovascular risk factors not exclusion criterion | Presence of WMH at baseline was not predictive of depression at 33 month follow-up |
| (Godin et al 2007) | 1214 subjects followed for 4 years. 14.5% depressed at baseline | 72.5±4.1 | 1.5T 3.5mm (0.5mm gap) |
NR | NR | NR | Depressed | AD – not specified. | No pacemaker, vulvular prosthesis, history of neurosurgery or aneurysm. | Patients with baseline depression had more WMH at follow-up. Among non-depressed subjects at baseline, the higher the rate of WMH, the greater the risk of depression at follow-up |
| (Janssen et al 2007) | 13 early onset MDD 15 late-onset depression 22 HC |
70.38±8.3 72.67±6.7 71.05±7.5 |
1.5T | 33.62±8.8 69.93±6.4 |
NR | NR | Depressed | 4 lithium | Cerebrovascular risk factors not exclusion criterion. No neurological disorders, dementia, substance abuse | Greater severity of WMH in late-onset group. |
| (Ma et al 2007) | 14 MDD 14 HC |
28.9±8.0 27.1±6.7 |
1.5T 2mm DTI |
28.1±7.8 | 10.3±8.3 (months) | NR | Depressed | Treatment naive | No LOC, substance abuse in last 9 months, mental retardation, serious medical or neurological illness | Lower FA in WM of R middle frontal gyrus (dorsal PFC), parietal + occipito-temporal lobes |
| (Yang et al 2007) | 31 MDD 15 HC |
64.6±5.21 64.3±4.22 |
1.5T DTI 3mm ROI |
NR | NR | NR | Depressed | 24 AD, 7 drug-free | No substance abuse, major psychiatric or neurological disorders. | Decreased FA values in middle, superior frontal gyri, + R parahippocampal gyrus |
| (Zanetti et al 2008) | 28 MDD 102 HC |
30.5 30.4 |
1.5T 3mm |
NR | 34.1 (28.5) weeks | NR | Psychotic | 16 AP, 14 AD, 4 MS, 7 drug free | No organic, neurological illness, head injury, mental retardation. 6 individuals with substance abuse/dependence, 2 individuals with hypertension | No significant differences in prevalence or severity of WMH between groups. |
BD
In BD most studies suggestive of WM pathology involve DTI. Changes in diffusion coefficients, which are believed to reflect the integrity of WM fibres, have been reported in the WM bundles connecting the PFC (particularly BA 9 and 10) to subcortical regions (Adler et al 2004), OFC (Beyer et al 2005), internal capsule adjacent to the striatum and thalamus (Haznedar et al 2005), genu of the corpus callosum (Yurgelun-Todd et al 2007), and prefrontal and temporal cortex (Bruno et al 2008). Further, a DTI tractography (allows for the measurement of entire WM pathways) study reported a higher incidence of reconstructed WM fibres linking the left sgACC and the amygdalo-hippocampal complex in remitted adults with BD (Houenou et al 2007).
Most MRI-based reports of BD-associated WMH are, however, derived from pediatric samples. A significant minority of young BD patients with a relatively typical age-of-onset show WM abnormalities on MRI (Table 14).
Table 14.
White Matter Hyperintensities in BD.
| Study | Sample | Age | Method | Age of Onset | Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Medical + Psychiatric Comorbidity |
Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Dolan et al 1990) | 14 BD 13 HC |
39±9 46±7 |
0.08T 12mm ROI |
31±9 | 11±7 | NR | Depressed | Lith, AD, BZ | No significant medical illness or alcohol abuse. | No group differences |
| (Dupont et al 1990) | 19 BD 10 HC |
36.5±10 41±10 |
1.5T 5mm (2.5mm gap) |
25±7.5 | NR | Mixed – not specified | Mixed – not specified | Lith, MS. No Benz, ECT, antihypertensives. | No poorly controlled hypertension, head injury with neurological sequelae, substance abuse of greater than 5 years duration. | 9 out of 19 BD subjects and no HC showed deep frontal WMH. No differences in age, age of onset, family history of BD between those patients with WMH and those without, but WMH associated with more hospitalizations. |
| (Swayze et al 1990) | 48 BD 47 HC |
33.9 34.4 |
0.5T 10mm |
22.86±7.82 | 5.89±6.15 (hosp) | NR | Manic | Lithium, AP, ECT | 27 with drug abuse, 33 with alcohol abuse | 9 out of 48 BD and 2 out of 47 HC showed WMH |
| (Figiel et al 1991) | 18 BD 18 HC |
37.5 (26–56) 34.7 |
1.5T 5mm (2.5mm gap) |
NR | ±28 | NR | 12 manic, 6 depressed | NR | No dementia, neurological illnesses. Presence of atherosclerotic risk factors similar in BD and HC. | WMH in 8 out of 18 BD, 1 out of 18 HC. |
| (McDonald et al 1991) | 12 BD 12 HC |
68.3±7 67.7±7 |
1.5T 5mm (2.5mm gap) |
62±6 | NR | 3/12 | manic | NR | 1 patient with ataxia, 1 with peripheral neuropathy, 1 with tardive dyskinesia. All patients had cognitive dysfunction | More BL subcortical WMH in BD group |
| (Brown et al 1992) | 22 BD 154 HC |
37.7±7.6 34±9.5 |
0.5T and 1.5T 7mm |
NR | NR | NR | NR | NR | No history of cardiovascular risk factors, current drug abuse | No inter-group differences in WMH |
| (Strakowski et al 1993) | 18 BD 15 HC |
31±11.8 32.4±8.8 |
1.5T 5mm (2mm gap) |
NR | 1st episode | NR | Manic | Majority of patients medication naive | 5 BD with drug abuse. No major neurological or medical illness. | More WMH in BD but not statistically significant. |
| (Aylward et al 1994) | 30 BD 30 HC |
39.3±11.1 37.6±9.0 |
1.5T 5mm |
24.6±8.4 | NR | NR | 1 depressed, 2 manic, 2 mixed, 27 euthymic. | AD | No “substantial” substance abuse. 7 hypertension, 12 smokers, 3 cardiovascular disease, 3 elevated cholesterol, 1 DM. | Greater prevalence of deep WMH in BD but significant differences due to older BD group. |
| (Altshuler et al 1995) | 29 BD I 26 BD II 20 HC |
41.6±11.6 40.0±10.0 35.2±9.9 |
0.5T 10mm |
28.3±10.9 for BD I, 19.2±7 for BD II. | 14.2±8.7 (BD I) 18.9±7.7 (BD II) |
NR | Euthymic | 30 lithium, 10 carbamazepine, 3 AD | 1 DM, 4 hypertension, | No significant difference between groups in deep frontal WMH. Trend (2x) towards more PVH in BD I. Greater number of PVH was due to BD I subsample >30 years of age. |
| (Botteron et al 1995) | 11 BD 5 HC |
11.3±3.1 11.8±2.9 |
1.5T 4–5mm |
NR | NR | NR | Manic | NR | No autism, pervasive developmental disorder, anorexia, bulimia, major medical or neurological illness, head injury. | WMH in 2 BD patients |
| (Dupont et al 1995b) | 44 BD 32 HC |
36.6±10.7 39.2±8.9 |
1.5T 5mm (2.5mm gaps) |
23±8.0 | NR | Mixed | 28 BD in remission, others depressed or manic. | 26 lithium, 6 AD, 6 AP, 2 anticholinergics | No substance abuse in last 5 years. No hypertension, head injury | Greater number of WMH in BD (46% vs 22%). Not accounted for by age of onset. Higher (but not significant) rate of WMH in subjects with family history. |
| (Lewine et al 1995) | 20 BD 150 HC |
36±7 | 1.5T 5–8mm |
±30 | NR | NR | NR | NR | No neurological or medical disorders. No current substance abuse. | No significant differences |
| (Woods et al 1995) | 52 BD 38 HC |
36.3±15.1 36.3±11.4 |
1.5T 5mm (2.5mm gap) |
NR | 2.1±1.8 (hosp) | NR | NR | NR | NR | More deep WMH and PVH in BD |
| (Persaud et al 1997) | 26 BD 34 HC |
35.6 31.6 |
0.5T 5mm |
25 | NR | NR | Manic | NR | No hypertensives, anorexics, heavy drinkers | No significant differences |
| (Ahearn et al 1998) | 21 family members (9 BD, 2 MDD, 10 unaffected) | 41 (range 12–66) | 1.5T 4–6mm |
18 | NR | Yes | NR | NR | No substantial artherosclerotic risk factors. | WMH in 9 affecteds and 6 unaffecteds. |
| (McDonald et al 1999) | 79 BD 70 HC |
49.9±19.7 53.2±18.1 |
1.5T 5mm (2.5mm gap) |
38±17 | NR | NR | NR | NR | NR | 16% of young BD (35.9±11) vs 0% HC showed WMH. No difference between old (68.2±9) BD and old HC. |
| (Krabbendam et al 2000) | 21 BD 22 HC |
38.3±7.9 41.4±11.3 |
1.5T 5mm (0.5mm gap) |
32.2±9.4 | 6.2±5.1 dep episodes 3.9±3.7 manic episodes |
NR | Remitted | 16 Lith 6 MS |
No cerebrovascular disease; head injury, DM, hypertension; substance abuse in last year. | No significant differences |
| (Moore et al 2001) | 14 BD (good outcome) 15 BD (poor outcome) 15 HC |
47.4±10.10 42.1±13.9 41.9±12.6 |
0.5T 7mm (1mm gap) |
31.4 in good outcome and 26.3 in poor outcome groups | 16±7.9 8.6±6.0 episodes (good outcome) 15.8±10.8 8.9±4.3 episodes (poor outcome) |
4 in each group | Good outcome group euthymic Poor outcome group depressed. | Lithium in good outcome group, not specified in poor outcome. | No axis I comorbidity, learning disorders, neurological or cerebrovascular disease, head injury, hypertension, cardiovascular illness, drug abuse | Greater number of subcortical WMH in poor outcome BD (7/15) group than good outcome sample (1/14) or controls (0/15) |
| (Lopez-Larson et al 2002) | 17 BD 12 HC |
29±8 31±8 |
1.5T 1mm ROI |
NR | 7±6 | NR | Manic | 9 MS, 4 AP, 3 AD | No medical or neurological disorders, head injury, substance abuse in previous 3 months | No WM differences. |
| (Lyoo et al 2002b) | 56 BD 83 HC |
13.6±2.1 9.9±3.3 |
1.5T 5mm (2.5mm gap) |
NR | NR | NR | NR | NR | NR | Greater number of frontal WMH in BD (17.9%) compared with HC (1.2%) |
| (Pillai et al 2002) | 15 BD 16 HC |
15.0±2.4 16.0±1.8 |
1.5T 5mm (2mm gap) |
10±4.2 | 5±3.4 | NR | NR | NR | No significant neurological disorder, head injury with loss of consciousness for more than 20 min. No substance abuse | WMH present in 10 BD (67%) and 5 HC (31%) |
| (Sassi et al 2003) | 24 BD 17 MDD 38 HC |
34.2±9.9 42.8±9.2 36.8±9.7 |
1.5T 5mm |
14/24 <20 10/24 >21 |
NR | 12/24 | NR | Lithium | No neurological disorders, axis I comorbidity or substance abuse | No significant differences |
| (Silverstone et al 2003) | 13 BD 19 HC |
40.2 35.9 |
0.5T 5mm (2.5mm gaps) |
25.9 | 14.2 | NR | Depressed | NR | No neurological disorders, cardiovascular disease, DM or head injury | More BD subjects (56%) had deep frontal WMH than HC (26%). Effect strongest in older subjects. No differences in PVH. |
| (Adler et al 2004) | 9 BD 9 HC |
32±8 31±7 |
3T 5mm ROI |
NR | NR | NR | NR | MS, AP | No concurrent psychiatric or medical illness including substance abuse | Reduced fractional anisotropy in frontal regions of BD indicative of loss of bundle coherence of WM tracts |
| (Ahn et al 2004) | 43 BD 39 HC |
36.9±11.9 35.1±9.7 |
1.5T 3mm |
NR | NR | NR | NR | NR | No axis I disorders, substance abuse within 3 months of study, antisocial PD, neurological illnesses, head injury, seizure, ADHD. | Greater number of deep frontal WMH in BD (27.9%) compared with HC (7.7%) |
| (Beyer et al 2005) | 14 BD 21 HC |
44.0±17.6 44.6±13.5 |
1.5T 5mm (2.5mm gap) ROI |
NR | 13.6±12.1 | NR | 6 depressed, 5 manic, 3 euthymic | NR | No dementia, neurological or medical illnesses, other primary psychiatric diagnosis or recent substance abuse | WM of OFC exhibited higher apparent diffusion coefficients but not FA in BD |
| (Chang et al 2005a) | 20 BD 20 HC |
14.6±2.8 14.1±2.8 |
3T 1.5mm |
NR | 1.7±1.8 | NR | 3 manic, 3 mixed, 1 depressed, 13 euthymic | MS, AD, AP. Psychostimulants discontinued 24 hrs before scan. | No pervasive developmental disorders, neurological conditions, substance abuse. 85% had ADHD, 35% anxiety disorder, 60% ODD. | No difference between groups in prevalence of WMH. |
| (Adler et al 2006a) | 11 BD 17 HC |
14±2 | 3T 5mm ROI |
11±3 | 1st episode | NR | Manic or mixed episode | Nil | No substance abuse in last 3 months. No head trauma, unstable neurological or medical conditions | No differences in FA of medial and inferior frontal regions but FA of superior frontal cortex lower in BD |
| (de Asis et al 2006) | 40 BD 15 HC |
69.8±6.7 66.9±6.5 |
1.5T 5mm |
51.8±18.3 | NR | NR | Manic | NR | No dementia, medical illness | More severe deep frontal WMH in BD. Positive association between age of onset of mania + WMH |
| (El-Badri et al 2006) | 50 BD 26 HC |
30.2±6.2 30.2±6.2 |
0.5T | NR | 8.9±3.3 | NR | Euthymic | NR | No axis I comorbidity, learning disorders, neurological or cerebrovascular disease, head injury, hypertension, cardiovascular illness, drug abuse | Deep WMH found in 5 BD but no HC. |
| (Gulseren et al 2006) | 12 BD 1 12 siblings 12 HC |
30.9±3.6 29.5±5.8 30.4±3.6 |
0.5T 5mm |
24.8±3.6 | 6.1±3.2 | Yes - 2/12 | NR | Lithium | No substance abuse, hypertension, history of neurological disorders or head trauma. All subjects <45 years old | No difference in frequencies of WMH. Number of WMH correlated with # manic episodes |
| (Regenold et al 2006) | 8 severe BD 8 controls with neurological illness |
58.4±12.9 54.5±12.8 |
1.5T 5mm (1mm gap) ROI DTI |
32 | 25±7.2 (episodes) | NR | 4 manic, 3 mixed, 1 depressed | 7 MS, 7 AP, 2 AD, 2 Benz | 6 BD, 1 control smokers. No substance abuse | Elevated apparent diffusion coefficient as evinced by DTI – indicative of decreased integrity of WM in the frontal lobes of BD patients. |
| (Houenou et al 2007) | 16 BD 16 HC |
41.88±12.82 40.50±12.82 |
1.5T 1.3mm DTI |
18.13±3.77 | NR | NR | Euthymic | Lithium, AD | No neurological conditions, substance abuse, head injury. 1 patient with comorbid PD | Increased number of white matter tracts between the L sgACC and the amygdala-hippocampal complex. This result was not influenced by illness duration |
| (Yurgelun-Todd et al 2007) | 11 BPD 1 10 HC |
32.9±10.5 32.4±9.1 |
1.5T 5mm DTI |
21.7±5.4 | 12.0±9.8 | NR | Euthymic | Lith, MS, AP | No organic mental disorder, head injury, CNS disease, substance abuse in previous 6 months | BD patients had significantly higher FA in the midline of the genu but not splenium indicating changes in WM microstructure |
| (Zanetti et al 2008) | 25 BD 102 HC |
28.7 30.4 |
1.5T 3mm |
NR | 27.1±19.3 weeks | NR | Psychotic | 12 AP, 2 AD, 13 MS, 6 drug free | No organic, neurological illness, head injury, mental retardation. 5 individuals with substance abuse/dependence, 2 individuals with hypertension | No significant differences in prevalence or severity of WMH between groups. |
(Adler 2004) has hypothesized that the pattern of deep frontal WM pathology commonly seen in affective illness, results in a disruption of the pathways linking subcortical regions such as the striatum to functionally homologous regions of the prefrontal cortex – a version of the so-called “disconnection syndrome” (Geschwind 1965). In the following three sections we discuss key areas of the PFC involved in the regulation of emotional behavior.
The Orbital Frontal Cortex
The orbital frontal cortex (OFC) on the ventral surface of the frontal lobe receives inputs from the ventrolateral amygdala and other limbic structures such as the entorhinal and perirhinal cortices, and the hippocampal subiculum (Price 1999). The OFC also projects directly to the amygdala, hypothalamus, and brain stem, modulating limbic-driven behavior (Ongur and Price 2000b). More specifically, it acts to integrate limbic data with sensory input thus providing a first-pass analysis of the reward or aversive value of stimuli (Price 1999) (Kringelbach 2005). These data then feed into higher level processing circuits such as that of the mPFC (vide infra) which act together with the OFC to guide behaviour in terms of these expected contingencies (Kringelbach and Rolls 2004) (Amodio and Frith 2006).
MDD
Functional imaging analyses of the OFC in MDD (Table 15) are generally suggestive of increased metabolism or blood flow in the eyes closed or resting state in young to middle-aged samples (Drevets et al 1992) (Biver et al 1994) (Drevets et al 2002a) – particularly acutely depressed subjects (Drevets 2007). In contrast, while performing a probabilistic reversal learning task, MDD patients demonstrated attenuated hemodynamic activity in the lateral OFC/ventrolateral PFC and dorsomedial PFC relative to both healthy controls and BD subjects on trials in which misleading negative feedback triggered a behavioral response reversal, compared to trials in which misleading negative feedback did not precipitate reversal (Taylor Tavares et al 2008). This physiological difference was associated with an increased likelihood for the MDD subjects to switch their behavioral responses as a result of the misleading negative feedback, although basic object reversal learning is intact in depression. Another study showed an increased hemodynamic response in the posterior orbital cortex in depressed versus non-depressed BD subjects imaged while performing a color-word Stroop task (Blumberg et al 2003b).
Table 15.
Functional Analyses of the Orbitofrontal Cortex in MDD.
| Study | Sample | Age | Method | Age of Onset |
Duration of Illness/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Baxter et al 1987) | 14 MDD 14 HC |
35.3±12.3 31.6±4.5 |
18 F-FDG | NR | NR | NR | Depressed | Free of drugs for 1+ week | NR | No significant differences | NR |
| (Drevets et al 1992) | 13 depressed MDD 10 remitted MDD 33 HC |
36.2±8.9 33.6±10.0 30.1±7.8 |
15O-H2O voxel-wise | NR | NR | Yes | Depressed + euthymic | Depressed sample unmediated for 3+ weeks before scan. Remitted sample unmedicated for 4+ months. | No co-morbid conditions | Elevated BF in L PFC (which included a portion of the lateral OFC) of depressed MDD | 47; 41; 6 |
| (Biver et al 1994) | 12 MDD 12 HC |
37.6±13.2 31.08±5.4 |
18 F-FDG ROI |
NR | NR | NR | Depressed | Unmediated for 10+ days prior to scan | No neurological disorders or other medical conditions | Metabolic rate increased in OFC of MDD | NR |
| (Brody et al 1999) | 16 MDD | 39.3±9.5 |
18 F-FDG ROI |
NR | ± 1±1 (episodes) | NR | Depressed | No medication for 2+ weeks prior to scan | No axis I disorders, substance abuse, medical conditions | Decrease in metabolism from baseline of OFC in patients who responded to paroxetine | NR |
| (Drevets et al 2002a) | 20 MDD 14 HC |
36±10 34±9.1 |
18 F-FDG | NR | NR | NR | Depressed | Patients medication free for 3+ weeks prior to study. | No other psychiatric disorders or substance abuse | Greater baseline metabolic rate of lateral OFC in MDD | BA 47 |
| (Liotti et al 2002) | 10 remitted MDD 7 ill MDD 8 HC |
37±9 42±15 36±6 |
15O-H2O 6.5mm |
NR | NR | NR | Euthymic | AD | No other primary psychiatric or neurological disorder. No head injury, substance abuse | Mood provocation led to rCBF descreases in medial OFC in both MDD groups | BA 10+32 −4; 40; −2 4; 56; 8 4; 36; −10 2; 60; −2 0; 34; −14 |
| (Goldapple et al 2004) | 17 MDD | 41±9 | 18 F-FDG Voxel-wise | NR | NR | NR | Depressed | Unmedicated | No psychotic symptoms, axis I disorders and substance abuse | Successful treatment with CBT associated with decreased metabolism of medial OFC | BA 11 20; 52; −22 |
| (Mayberg et al 2005) | 6 MDD | 46±8 | 15O-H2O | 29.5±12 | 4.7±5 (episodes) | Yes - in 5 out of 6 subjects | Depressed | NR | No psychotic symptoms, substance abuse in last 3 months | Treatment with deep brain stimulation produced decreased metabolism of the OFC | BA 11 0; 34; −8 6; 46; 2 22; 60; −10 |
| (Chen et al 2007a) | 17 MDD | 44.06±8.36 | MRI 1.5T 3mm |
NR | NR | NR | Depressed | Scanned before and after treatment with fluoxetine. Patients off medication 4+ weeks before study. | No current axis I comorbidity or substance abuse within 2 months of study. Personality disorders not assessed. | Functional activation of OFC negatively associated with severity of depression at baseline | BA 11 5; 46; −14 −20; 46; −17 |
Concerning the structural neuroimaging data, a sample of elderly MDD patients were first reported by (Lai et al 2000) to show bilateral volume reduction of the OFC. This finding has been replicated a number of times in elderly populations with later-onset depression (Table 16) and a negative association between the integrity of the white matter tracts of the OFC and severity of depression in a late-onset MDD group has also been recorded (Nobuhara et al 2006). (Lacerda et al 2004) reported a reduction of right medial and left lateral OFC volume in a younger sample (mean age 39) although the effect was more pronounced in depressed compared with euthymic patients. Similar to the (Nobuhara et al 2006) report, (Chen et al 2007a) found that severity of depression correlated negatively with right OFC volume.
Table 16.
Morphometric Analyses of the Orbito-Frontal Cortex in MDD.
| Study | Sample | Age | Method | Age of Onset | Duration of Illness/# Episodes | Family History of Illness | Clinical Status at Testing | Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Parashos et al 1998) | 72 MDD 38 HC |
55.4±16.8 55.1±17.1 |
1.5T 5mm ROI |
38.5±19.0 | NR | NR | Depressed | NR | NR | No differences in OFC volume. |
| (Lai et al 2000) | 20 MDD 20 HC |
66.65±5.65 71.79±4.44 |
1.5T 3mm ROI |
44.75±18.03 | 3.75 (hosp) | NR | Moderately depressed | 15 AD | No major psychiatric disorder, substance dependence, primary neurological illness | Bilateral reduction of orbital PFC in MDD |
| (MacFall et al 2001) | 88 MDD 47 HC |
72.6±7.9 72.2±6.3 |
1.5 3mm VBM |
49.3±22.6 | NR | NR | Depressed | NR | NR | Increased lesion density of medial OFC which correlated with severity of depression. −18, 40, −10 |
| (Bremner et al 2002) | 15 MDD 20 HC |
43±8 45±11 |
1.5T 3mm ROI |
NR | 2±3 (episodes) | NR | Remitted | AD | Current substance abusers excluded. No history of schizophrenia, PTSD. About 20% of sample had past history of substance abuse. | Medial OFC (gyrus rectus) reduced by 32% in MDD. |
| (Steffens et al 2003) | 30 MDD 40 HC |
69.60±7.15 70.90±6.13 |
1.5T 3mm ROI |
NR | NR | NR | NR | NR | No other major psychiatric illness, substance dependence, primary neurological illness | Bilateral reduction of orbital PFC in MDD |
| (Taylor et al 2003) | 41 MDD 40 HC |
68.73±6.98 71.42±6.07 |
1.5T 3mm ROI |
NR | NR | NR | Depressed | AD | No other major psychiatric illness, substance dependence, primary neurological illness | Smaller medial orbitofrontal gyri volume in MDD. OFC volume also associated with functional impairment |
| (Ballmaier et al 2004) | 24 MDD 19 HC |
65.85±8.18 66.24±7.25 |
1.5T 1.4mm ROI |
35.0±3.45 | 2±3 (episodes) | NR | Depressed | No medication for 2+ weeks before imaging | No history of dementia, neurological disorder, BD, alcohol abuse | BL volume reduction of OFC (12%) + gyrus rectus (19–24%) in MDD |
| (Hastings et al 2004) | 18 MDD 18 HC |
38.9±11.4 34.8±13.6 |
1.5T 1.5mm ROI |
23±12.3 | 4.7±4.4 (episodes) | Mixed | Depressed | Not medicated at time of scan. | No other axis I disorders. No current drug abuse | No significant differences. |
| (Janssen et al 2004) | 28 MDD 41 HC |
64.04±10.9 62.37±11.38 |
1.5T 1.2–5mm ROI |
33.04±9.48 | 93.5±17.5 months | NR | Depressed | 22 AD, 4 lithium, 1 BZ. | NR | No significant differences in orbitofrontal volume |
| (Lacerda et al 2004) | 31 MDD 34 HC |
39.26±11.9 37.03±11.88 |
1.5T 1.5mm ROI |
27.94±11.64 | 11.42±10.47 | NR | 19 depressed, 12 euthymic | Patients drug free for 2+ weeks | No axis I comorbidity, head injury, substance abuse in last 6 months | GM decrease in R medial OFC + L lateral OFC in MDD. Trends for L medial + R lateral OFC. No volume differences between euthymic + acutely ill patients. |
| (Lavretsky et al 2004) | 41 MDD 41 HC |
70.5±7.6 72.2±7.3 |
1.5T 1.4mm |
48.5±23.5 | 2.7±2.7 (episodes) | NR | Depressed | No medication for 2+ weeks | No substance abuse, dementia or other neurological disorder | Smaller total and GM volumes of OFC in MDD |
| (Nobuhara et al 2006) | 13 MDD 13 HC |
62.8±6.6 61.5±4.8 |
DTI 1.5T 6mm (2mm gap) ROI |
52.9±7.3 | 4.0±2.6 | NR | Depressed | AD | No dementia, severe medical illness, neurological disorders | Negative association between integrity of WM tracts in medial orbital cortex + severity of depression. |
| (Chen et al 2007a) | 17 MDD | 44.06±8.36 | MRI 1.5T 3mm |
NR | NR | NR | Depressed | Scanned before and after treatment with fluoxetine. Patients off medication 4+ weeks before study. | No current axis I comorbidity or substance abuse within 2 months of study. Personality disorders not assessed. | Baseline severity of depression negatively correlated with GM volume of R OFC BA 11 34; 60; −6 |
BD
GM volume reductions of the OFC have also been reported in adult (Frangou 2005) (Haznedar et al 2005) (Lyoo et al 2006) (Nugent et al 2006) and pediatric BD samples (Wilke et al 2004) (Najt et al 2007); although see (Lopez-Larson et al 2002) and (Dickstein et al 2005). Thus unlike MDD, BD-associated volume reduction of the OFC appears to occur in individuals with a more typical age-of-onset (Table 18)
Table 18.
Morphometric Analyses of the Orbito-Frontal Cortex in BD.
| Study | Sample | Age | Method | Age of Onset | Duration of Illness/# Episodes | Family History of Illness | Clinical Status at Testing | Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Lopez-Larson et al 2002) | 17 BD 12 HC |
29±8 31±8 |
1.5T 1mm ROI |
NR | 7±6 | NR | Manic | 9 MS, 4 AP, 3 AD | No medical disorders, head injury, substance abuse for 3 months | No difference |
| (Wilke et al 2004) | 10 BD 52 HC |
14.5±1.8 15±1 |
3T 1.5mm VBM |
NR | NR | NR | Six mixed and 4 manic | No medication 72 hours before scan. | No schizophrenia, LD or PDD. | Reduction in OFC GM in BD |
| (Beyer et al 2005) | 14 BD 21 HC |
44.0±17.6 44.6±13.5 |
1.5T 5mm ROI |
NR | 13.6±12.1 | NR | 6 depressed, 5 manic, 3 euthymic | NR | No dementia, medical illnesses, other primary psychiatric diagnosis, recent substance abuse | WM of OFC - higher diffusion coefficients, but not FA, in BD |
| (Dickstein et al 2005) | 20 BD 20 HC |
13.4±2.5 13.3±2.3 |
1.5T 1.2mm VBM |
10.1±3.2 | NR | NR | Euthymic | AP, MS, AD | ADHD, psychosis, anxiety | No significant differences |
| (Frangou 2005) | 43 BD 43 HC |
42.9±11 | 1.5T 1.5mm VBM |
25.5±9.2 | 16.0±19.0 | Mixed | Remitted | MS + AP | NR | Reduced GM in orbitofrontal gyrus of BD BA 11 |
| (Haznedar et al 2005) | 40 BD (17 BD I 7 BD II, 17 sub-threshold) 36 HC |
39.8±13.4 43.8±6.7 43.9±9.2 40.7±11.6 |
1.5T 1.2mm ROI |
NR | NR | 10 yes. | NR | BD II + cyclothymia samples medication free. BD I on MS, AP. | 1 OCD, 1 panic disorder, 1 PTSD. No concurrent substance dependence | Reduced GM in OFC in BD BA 11 + 12 |
| (Lyoo et al 2006) | 25 BD (18 BD I, 7 BD II) 21 HC |
33.8±9.6 31.5±9.7 |
1.5T 1.5mm |
17.9±5.4 | 16.5±11.5 years | NR | Mixed | 6 Lith, 4 valproate, 8 others. | No substance abuse; comorbid axis I disorder in last 3 months, ASPD; medical illness, LD, ADHD. | Reduced cortical thickness of the R OFC in BD 10; 55; 0 |
| (Nugent et al 2006) | 36 BD 65 HC |
39±8.1 38±11.8 |
3T 1.2mm VBM |
Medicated: 18±8.8 Unmedicated: 21±6.5 |
23±9.0 17±10.0 |
NR | NR | 16 off medication for 4+ months. Rest on lithium or valproate | No neurological disorders, medical illnesses, substance abuse within last 90 days | GM volume reduction in L lateral OFC in BD −40, 52, −14 |
| (Najt et al 2007) | 14 BD 20 HC |
15.5±3.2 16.9±3.8 |
1.5T 1.5mm |
11.9 | 3.6±2.4 | Yes | Euthymic | Lithium + valproate | NR | Male BD smaller OFC volumes. Female BD large OFC volumes |
Concerning functional imaging studies of the OFC in BD (Table 17), (Blumberg et al 1999) showed that manic patients have reduced rCBF in this region while induction of a sad mood through psychological means resulted in decreased rCBF to the medial OFC in euthymic but not depressed patients compared with controls (Kruger et al 2003). A study using an affective Go/NoGo paradigm to examine neural activity during voluntary attentional control of emotion found that despite intact task performance, euthymic BD adults demonstrated abnormally increased activity in bilateral OFC and left dorsal ACC, together with increased activity in some subcortical limbic regions, when inhibiting responses to emotional versus neutral distractors (Wessa et al 2007).
Table 17.
Functional Analyses of the Orbito-Frontal Cortex in BD.
| Study | Sample | Age | Method | Age of Onset |
Duration of Illness/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status |
Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Cohen et al 1992) | 7 SAD (5 BD II, 2 MDD) 38 HC |
44.9±11.1 36.2±11 |
18 F-FDG | NR | NR | No MDD in relatives. | Depressed | No medication for 3+ weeks | No serious medical or psychiatric history | Increased acitivity of medial OFC in MDD | NR |
| (Blumberg et al 1999) | 5 manic 6 euthymic 5 HC |
34.2±12.2 32.5±11.0 30.0±6.7 |
15O-H2O | NR | NR | NR | 5 manic, 6 euthymic | AD, AP, MS, Benz | No axis I and II disorders or neurological/medical illness. | Decreased rCBF to OFC at rest in manic sample | BA 11 −2, 46, −28 |
| (Kruger et al 2003) | 11 depressed BD 9 remitted BD |
43±9 38±12 |
15O-H2O Voxel-wise | 22±6 | 8±3 (dep episodes) 3±2 (manic episodes) 8±5 (dep episodes) 3±2 (manic episodes) |
NR | Depressed/Remitted | MS | No axis I or II disorders. No substance abusers | rCBF decreases to R orbitofrontal region after sadness induction in both BD groups | BA 10/11 6; 42; −10 14; 46; −20 8; 56; −6 |
| (Rich et al 2006) | 22 BD 21 HC |
14.2±3.1 14.5±2.5 |
Voxelwise ROI used for amygdala, VPFC and ventral striatum. Facial processing task |
NR | NR | NR | Half euthymic, half depressed or hypomanic | 80% medicated | No pervasive developmental disorder, IQ<70, unstable medical illness, substance abuse for 2+ months | In L orbital cortex BD patients showed greater activation when rating the hostility of neutral face stimuli | −32; 20; −16 |
Other studies showed reduced activity in euthymic BD relative to healthy adults during automatic attentional control paradigms, such as the non-emotional Stroop color-word or counting task, in the left OFC/VLPFC and mPFC (Blumberg et al 2003b) (Kronhaus et al 2006), and the right mPFC (Strakowski et al 2005) and dorsal ACG, but also increased activity in right dorsolateral PFC (Gruber et al 2004). Subjects imaged during the depressed or manic phases of BD while performing similar paradigms also showed reduced left OFC activity relative to healthy controls (Blumberg et al 2003b), although these findings were not replicated by others (Marchand et al 2007). Most of these studies showed intact task performance in BD adults, although in other cases performance was impaired relative to healthy controls (Strakowski et al 2005).
The Ventro-Medial “Emotion” Circuit
Neuroimaging data suggest that the peri-callosal tissue of the ventro-medial prefrontal cortex known as the anterior cingulate cortex (ACC) (BA 24, 25, and 32) 1 (Figure 2) plays a pivotal role in translating OFC-derived valenced data into actions and behavior (Bush et al 2000) (Devinsky et al 1995) (Drevets 2000a).
Figure 2. Architectonic subdivisions of the medial surface of the human brain.
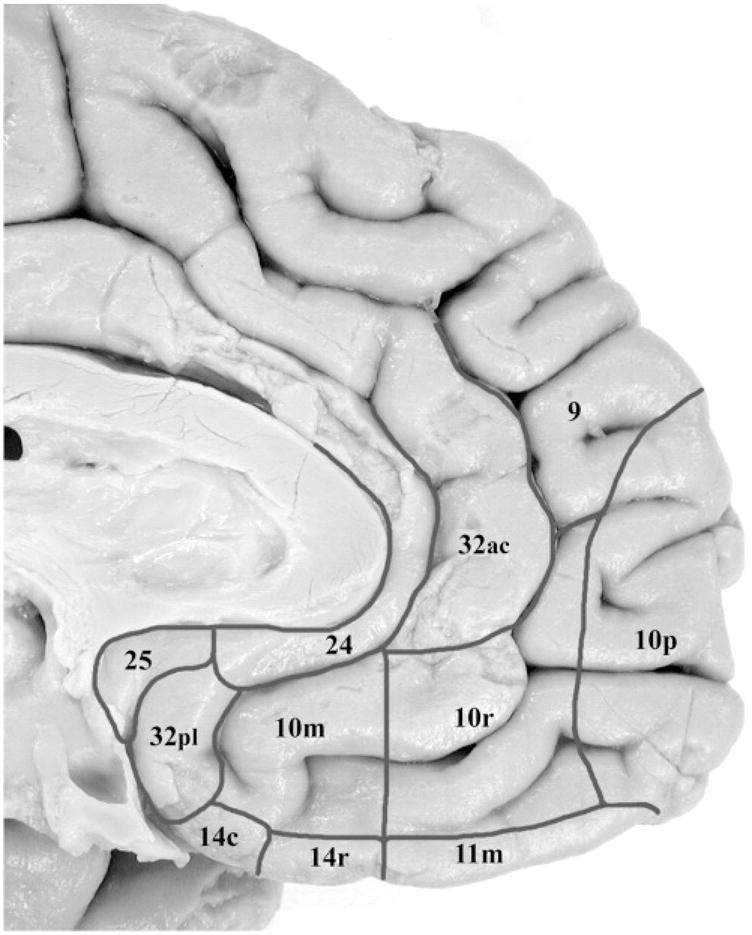
Ongur et al. (2003). J Comp Neurol. 460; 425–449
Drevets and colleagues (Drevets et al 1997) carried out the first well-controlled imaging study of the medial prefrontal cortex in affective illness. Both depressed BD and MDD patients with a family history of affective illness showed left hemisphere gray matter loss in a region immediately ventral to the genu of the corpus callosum – the subgenual anterior cingulate cortex (sgACC). Further, the medication free patients displayed reduced metabolism of the left sgACC as demonstrated by PET.
In the interim, at least seven other studies have provided further evidence for MDD or BD-associated GM loss in the sgACC (Hirayasu et al 1999b) (Botteron et al 2002) (Sharma et al 2003) (Hastings et al 2004) (Boes et al 2007) (Koo et al 2008) (Yucel et al 2008) (Tables 20 and 22). The recent meta-analysis of (Hajek et al 2008) confirms that on average both left and right sgACC volumes are decreased in mood disorders although interestingly, the effect (especially in the left hemisphere) appears to be driven by cases with a family history of illness.
Table 20.
Morphometric Analyses of the Ventral-Medial Prefrontal Cortex in MDD.
| Study | Sample | Age | Method | Age of Onset |
Duration of Illness/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Drevets et al 1997) | 10 MDD 21 HC |
39±7.3 34±8.2 |
1.5T 1mm slice ROI |
NR | NR | Yes | Depressed | Cohort not treated for 4 weeks prior to scans | NR | Decreased volume of L sgACC in MDD group. | 1; 25; −6 |
| (Shah et al 1998) | 20 MDD (chronic) 20 MDD (remitted) 20 HC |
21–65 | VBM | NR | NR | NR | Depressed and remitted | AD | No mania, significant substance abuse, organic pathology or neurological illness | Reduced GM volume of L inferior lateral frontal gyrus in chronic MDD | −55; 14; 14 |
| (Botteron et al 2002) | 30 MDD 8 HC |
20.2±1.6 | 1.5T 1mm ROI |
15.2±2.3 | NR | Yes | Depressed | Less than 10% of MDD sample on medication. | NR | Decreased volume of L sgACC in MDD | NR |
| (Bremner et al 2002) | 15 MDD 20 HC |
43±8 45±11 |
1.5T 3mm ROI |
NR | 2±3 (episodes) | NR | Remitted | AD | Current substance abusers excluded. No history of schizophrenia, PTSD. About 20% of sample had past history of substance abuse. | No volumetric changes of peri-callosal tissue | BA 24, 25 and 32 |
| (Kegeles et al 2003) | 19 (14 MDD, 5 BD) 10 HC |
36±11 39±19 |
1.5T 1.5mm ROI |
NR | NR | Yes | Depressed | BZ discontinued 24 hours before study in 12 cases. 7 subjects on BZ. Patients free of other medication for 2+ weeks. | 3 panic disorder, 2 dysthymia, 1 each with social phobia, simple phobia, anorexia + PTSD. No medical illness | No sgACC volumetric differences across groups. | NA |
| (Hastings et al 2004) | 18 MDD 18 HC |
38.9±11.4 34.8±13.6 |
1.5T 1.5mm ROI |
23±12.3 | 4.7±4.4 | Mixed | Depressed | No medicated at time of scan. | No other axis I disorders. No current drug abuse | Volume reduction in L inferior ACC in males only | NR |
| (Coryell et al 2005) | 10 MDD 10 HC |
21.9±4.9 22.1±6.0 |
1.5T 1mm ROI |
NR | 4.7±5.7 | NR | Depressed | NR | History of psychosis | Volume reductions in L posterior sgACC but not anterior sgACC in MDD | NR |
| (Lacerda et al 2005) | 22 MDD 39 HC |
41.4±11.1 35.8±10.5 |
1.5T 3mm ROI |
NR | 11.6±12.2 | 11 with family history, 11 without | NR | Drug-free for 2+ weeks | No comorbid disorders except substance abuse in remission for 6+ months. No medical problems | Patients with family-history of depression had larger genu and splenium volumes than HC and non-familial depressives. | NR |
| (Caetano et al 2006) | 31 MDD 31 HC |
39.2±11.9 36.7±10.7 |
1.5T 1.5mm ROI |
27.9±11.7 | 11.4±10.6 5.1±6.1 (episodes) |
NR | 21 depressed, 10 remitted | Unmedicated | No comorbid disorders except substance abuse in remission for 6+ months. | Currently depressed patients had smaller BL ACC volume. Remitted group had smaller L ACC volumes than HC | NR |
| (Boes et al 2007) | 31 HC – no family history 28 HC - + family history |
12.02±2.72 12.14±2.13 |
1.5T 1.5mm ROI |
NA | No DSM-IV-defined episodes | Mixed | Mixed | NR | No serious medial or neurological illness, psychiatric illness, learning disorder (but no clinical interview). | In boys (but not girls) with subclinical depression smaller L sgACC & pregenual PFC volumes. Similar effect in family-history + group. | BA 24, 33 but not 25. |
| (Chen et al 2007a) | 17 MDD | 44.06±8.36 | MRI 1.5T 3mm |
NR | NR | NR | Depressed | Scanned before and after treatment with fluoxetine. Patients off medication 4+ weeks before study. | No current axis I comorbidity or substance abuse within 2 months of study. Personality disorders not assessed. | Increased GM volume of pregenual ACC associated with lower symptom severity at baseline | BA 32 5; 44; 1 |
| (Tang et al 2007) | 14 MDD 13 HC |
29.5±6.84 29.46±6.86 |
1.5T 1.6mm ROI |
1st episode | 5.44±5.22 months | NR | Depressed | Medication naive | No medical or neurological disorder, head injury, substance abuse. 4 with GAD | Decreased volume of pregenual PFC in MDD | 2; 30; −2 |
Table 22.
Morphometric Studies of the Ventro-Medial Prefrontal Cortex in BD.
| Study | Sample | Age | Method | Age of Onset |
Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status |
Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Drevets et al 1997) | 21 BD 21 HC |
35±8.2 34±8.2 |
1.5T 1mm slice ROI |
NR | NR | Yes | Depressed | Cohort not treated for 4 weeks prior to scans | NR | Decreased volume of L sgACC in BD group. | 1; 25; −6 |
| (Hirayasu et al 1999a) | 21 BD 17 SZ 20 HC |
23.7±5.1 24.0±4.3 |
1.5T 1.5mm ROI |
23.7±5.1 | 1st hosp | 14 familial subjects | First episode manic psychosis (BD and SZ) | AP | No substance abuse within last 5 years | Decreased volume of L sgACC in familial BD patients. No significant changes in SZ. | NR |
| (Brambilla et al 2002) | 27 BD 38 HC |
35±11 37±10 |
1.5T 1.5mm ROI |
NR | NR | 12 familial, 12 non-familial | 11 mildly depressed, 1 hypomanic, 15 euthymic | No medication for 2+ weeks in 11 subjects, other 16 on lithium monotherapy. | No co-morbid psychiatric conditions. No current medical problems | No difference in sgACC volumes. No difference between familial and non-familial subjects. | NR |
| (Sharma et al 2003) | 12 BD 8 HC |
38±6 38±7 |
4T 3.3mm gap |
21.1±6.4 | 12±17.2 | 6 with family history, 6 without | Euthymic | MS, AD | No substance abuse in last 5 years. | Decreased volume of R sgACC in BD | NR |
| (Doris et al 2004) | 11 BD I 11 HC |
40.5±11.6 38.1±10.8 |
2T 1mm VBM |
24.3±5.1 | 16.2±11.1 7.8±3.4 (hosp) |
NR | Relatively euthymic | MS, AD, AP | No comorbid conditions. | Decreases in gray matter density of R medial frontal gyri | BA 10 9; 52; −2 |
| (Lyoo et al 2004a) | 39 BD I 43 HC |
38.3±11.6 35.7±10.1 |
1.5T 1.5mm VBM |
18.6±7.0 | 18.1±11.0 10.5±9.2 (manic episodes) 13.5±7.2 (depressive episodes) |
NR | Mixed manic and depressed. | Treated with lithium and other medications | No axis I disorders, substance abuse within last 3 months, antisocial PD | GM volume reduction of L medial frontal gyrus + R inferior frontal gyrus | BA 10 + BA 47 −8; 54; 16 39; 26; −11 |
| (McDonald et al 2004a) | 38 BD 52 unaffected relatives 54 HC |
41±11.7 44±15.5 40.2±15.3 |
1.5T 1.5mm ROI |
22.6±5.5 | NR | Yes | NR | 33 BD on MS. 10 on AP. | No organic brain disease, head trauma, substance abuse in last 12 months. | Increased genetic risk for BD associated with reduced volume of R ACC | BA 11, 24, 25. |
| (Sassi et al 2004) | 11 BD (unmedicated) 16 BD (medicated) 39 HC |
38±11 33±11 39±10 |
1.5T 1.5mm ROI |
20±6 | 16.9±10.7 16±16 (episodes) 12.67±7.4 17.8±19.5 (episodes) |
14 yes, 13 no. | 11 depressed, 16 euthymic | 11 free of medication; 16 treated with lithium | No comorbid conditions. | Decrease in volume of L ACC in untreated BD sample compared with both HC and lithium group. Family history and mood at scan did not alter results. | NR |
| (Wilke et al 2004) | 10 BD 52 HC |
14.5±1.8 15±1 |
3T 1.5mm VBM |
NR | NR | NR | Six mixed and 4 manic | No medication 72 hours before scan. No data on medication type | No schizophrenia, learning disabilities or pervasive developmental disorders. | Reduced gray matter volume of L sgACC | NR |
| (Adler et al 2005) | 32 BD 27 HC |
31.2±9.4 30.5±9.7 |
3T 1mm VBM |
22.5±7.7 | 8.7±9.2 2.9±3.2 (depressive episodes) 2.0±1.5 (manic episodes) |
Majority of patients on a range of medication | 25 euthymic. 7 manic or depressed. | 9 unmedicated, others on AP, MS, AD + BZ. | No comorbid conditions. | Increased GM volume of ACC in BD | BA 32 −3; 47; 6 3; 47; 6 |
| (Haznedar et al 2005) | 40 BD (BD I 17; BD II; 7 cyclothymia 16) 36 HC |
39.8±13.4 43.8±6.7 43.9±9.2 40.7±11.6 |
1.5T 1.2mm ROI |
NR | NR | 10 yes. | NR | BD II + cyclothymia samples medication free. BD I on MS + AP. | “pathological gambling disorder”, 1 OCD, 1 panic disorder, 1 PTSD. No concurrent substance dependence, but previous history of abuse. | BL loss of GM in inferior cingulate | BA 25 & 32 |
| (Kaur et al 2005) | 16 BD 21 HC |
15.5±3.4 16.9±3.8 |
1.5T 1.5mm ROI |
NR | NR | Yes | 2 depressed, 14 euthymic | 10 lithium, 3 AD, 1 AP, 1 stimulant, 1 BZ | No substance abuse. 5 ADHD, 1 ODD, 1 CD | Decrease in volume of L ACC which includes BA 24. | NR |
| (Sanches et al 2005b) | 15 BD (3 BD II, 1 BD NOS) 21 HC |
15.5±3.5 16.9±3.8 |
1.5T 1.5mm ROI |
NR | 3.8±2.4 | Yes | 13 euthymic, 2 mildly depressed. | 13 on MS | No substance abuse. 5 ADHD, 1 ODD, 1 CD | No group differences in sgACC volumes No differences between patients on and off medication. | NR |
| (Zimmerman et al 2006) | 27 BD 22 HC |
24.0±6.4 23.5±6.5 |
1.5T 1.5mm ROI |
NR | NR | NR | Manic or mixed episode | 28 MS, 3 AD, 18 AP, 7 BZ | NR | No volume differences between groups | NR |
| (Bearden et al 2007) | 28 BD (70% on lithium) 28 HC |
36.1±10.5 35.9±8.5 |
1.5T | 18.6±6.1 | 15.1±18.2 | NR | 30% depressed 70% euthymic |
Lithium for 2+ weeks (treated group). No lithium for 1+ month (untreated group) | No neurological, medical problems. No substance abuse, other psychiatric disorders. | Greater volumes of the anterior cingulate, including the sgACC in lithium treated group compared to HC and lithium negative BD | NR |
| (Chiu et al 2007) | 16 BP 15 HC |
10.63±4.56 10.94±1.65 |
1.5T 1.5mm |
NR | NR | NR | NR | 12 AD, 9 MS, 8 AP, 3 adrenergic agents | No CNS disease, serious medical problems, IQ<70 | Smaller L ACG (included both dorsal + ventral aspects) in BD | NR |
| (Koo et al 2008) | 41 first-episode affective psychosis (38 BD) 40 HC |
22.8±4.5 23±3.2 |
1.5T ROI |
First Episode | 8.2±13.2 weeks | 30 +ve 10 -ve |
Manic | Median of 1 week duration of AP treatment prior to scan. Range 0–26 weeks. | No seizures, head trauma, sinistrality, neurological disorders, lifetime drug or alcohol dependence | Volume of L + R sgACC smaller in patients than HC. Decrease in sgACC volume over 1.5 year follow-up period. | NR |
Similarly, decreased activity of in particular, the left sgACC has been recorded in other studies of MDD and BD samples (Tables 19 and 21). These data apply equally to males (Hastings et al 2004) and females (Botteron et al 2002) as well as psychotic (Hirayasu et al 1999a) (Coryell et al 2005) (Adler et al 2006b) and bipolar-spectrum illness (Haznedar et al 2005), respectively. There are also data to suggest that metabolic changes predate the onset of clinical symptoms. (Kumano et al 2006) followed a cohort of cancer patients and found that those individuals who went on to develop depression had lower baseline metabolic rates of the subgenual PFC compared to their counterparts who did not become depressed during the course of the study.
Table 19.
Functional Analyses of the Ventro-Medial Prefrontal Cortex in MDD.
| Study | Sample | Age | Method | Age of Onset |
Duration of Illness/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status |
Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Drevets et al 1992) | 13 depressed MDD 10 remitted MDD 33 HC |
36.2±8.9 33.6±10.0 30.1±7.8 |
15O-H2O Voxel-wise | NR | NR | Yes | Depressed + euthymic | Depressed unmediated for 3+ weeks before scan. Remitted unmedicated for 4+ months | No co-morbid conditions | Depressed patients showed increased rCBF of L pregenual ACC. Effects not seen in remitted group. | BA 32 7; 55; 6 |
| (Drevets et al 1997) | 10 MDD 21 HC |
39±7.3 34±8.2 |
1.5T 1mm slice ROI |
NR | NR | Yes | Depressed | Not treated for 4 weeks prior to scans | NR | Decreased metabolism of L sgACC in MDD group. | BA 24 1; 25; −6 |
| (Wu et al 1999) | 12 MDD responders 24 MDD non-responders 26 HC |
28.8±9.2 30.8±9.9 29.4±9.5 |
18 F-FDG | NR | NR | NR | Depressed | No medication for 2+ weeks | No axis I diagnoses or physical disorders | Responders had higher metabolic rates in sgACC at baseline. Change in metabolic rate of L mPFC correlated with Ham-D scores after sleep deprivation. ie metabolism = improved symptoms. | BA 24; 25 3; 25; −4 5; 48; −4 |
| (Mayberg et al 2000) | 17 MDD | 49±9 | 18 F-FDG | NR | 2±1 episodes | NR | Depressed | Scanned before and after treatment with fluoxetine | No history of psychosis or substance abuse. No other axis I disorders. No dementia, head injury, cerebrovascular illness | Improvement associated with decreased activity of sgACC. No subgenual cingulate changes in non-responders to fluoxetine. | BA 25 4; 2; −4 2; 26; −8 |
| (Kennedy et al 2001) | 13 MDD 24 HC |
36±10 31.7±6.7 |
18 F-FDG | NR | 2.84±3.95 episodes | NR | Depressed | Scanned before and after treatment with paroxetine | No patients with concurrent DSM diagnosis. | Depressed group had higher activity in R pregenual cingulate which increased further with treatment | BA 24 8; 36; −4 |
| (Drevets et al 2002a) | 20 MDD 14 HC |
36±10 34±9.1 |
18 F-FDG | NR | NR | NR | Depressed | Patients medication free for 3+ weeks prior to study | No other psychiatric disorders or substance abuse | At baseline metabolism decreased in sgACC anteromedial PFC. After treatment with sertraline significant decreases in activity of L sgACC | 3; 31; −10 |
| (Dunn et al 2002) | 31 MDD | 42.4±13.6 | 18 F-FDG | 15.9±13.1 | 26.7±14.6 | NR | Mildly to severely depressed | Unmedicated for 2+ weeks | No active substance abuse, eating disorder, OCD, dementia, medical illness | Anhedonia associated with greater activity of the L pgACC and mPFC | pgACC BA 24, 25, 32 −16; 44; 4 BA 10 |
| (Liotti et al 2002) | 10 remitted MDD 7 ill MDD 8 HC |
37±9 42±15 36±6 |
15O-H2O 6.5mm |
NR | NR | NR | Euthymic | AD | No other primary psychiatric or neurological disorder. No head injury, substance abuse | Decrease in rCBF to medial PFC and pregenual cingulate in acutely depressed and remitted group, respectively | BA 9 + 10 8; 54; 12 6; 40; 27 BA 24 12; 38; 16 |
| (Davidson et al 2003) | 12 MDD 5 HC |
38.17±9.3 27.8±10.4 |
fMRI 1.5T 1mm ROI Block design with alternating negative-neutral or positive-neutral visual stimuli |
NR | NR | NR | Depressed | NR for baseline | No other axis I disorders except specific phobia or dysthymia. No neurological disorders | Less activation of the L ACC at baseline which improved with treatment | NR |
| (Holthoff et al 2004) | 41 MDD No Controls |
45.1±15.66 |
18 F-FDG Voxel-wise ROI |
NR | 1st episode in 54% of sample. 10 patients had more than 2 episodes | NR | Moderate to severely depressed | Treated with AD. BZ discontinued 3 days before baseline. | No substance abusers, axis II disorders | Remission associated with decreased metabolism of L ventral PFC | −16; 40; −2 −14; 70; 0 −14; 68; −12 |
| (Pizzagalli et al 2004) | 38 MDD (20 melancholic) 18 non-melancholic 18 HC |
33.1±8.8 36.5±12.9 38.1±13.6 |
18 F-FDG MRI 1.5T Voxel-wise |
NR | NR | Yes - in 12 melancholic + 7 non-melancholic subjects | Depressed | Free of medication for 2+ months | No other axis I disorders except simple phobias and dysthymia. No history of psychosis + current substance abuse. No axis II assessment. | Decreased (16%) metabolism of sgACC in melancholic patients only | BA25 −3; 9; −6 |
| (Gotlib et al 2005) | 18 MDD 18 HC |
35.2 30.8 |
3T Voxel-wise | NR | NR | NR | Depressed | 9 on AD | No brain injury, psychosis, social phobia, panic disorder + substance abuse in last 6 months | Greater BOLD response to sad faces in L sgACC (BA 25) in MDD. Also greater perfusion of L BA 32/24 in response to happy faces | BA 25 – coordinates not given BA 32/24 −8; 31; 7 |
| (Mayberg et al 2005) | 6 MDD | 46±8 | 15O-H2O | 29.5±12 | 4.7±5 (episodes) | Yes - in 5 out of 6 subjects | Depressed | NR | No psychotic symptoms, substance abuse in last 3 months | Elevated CBF to the sgACC but decreased CBF BA 24b at baseline in MDD. Treatment with deep brain stimulation associated with reduced activity of BA 25 and elevated metabolism of BA 24b | Baseline: sgACC ~BA 24 −10; 28; −12 −2; 18; 28 Treatment: 3 months sgACC BA25 −2; 8; −10 BA 24 −2; 10; 28 6 months BA 25 10; 20; −4 BA24 −4; 4; 34 |
| (Clark et al 2006) | 5 MDD responders 17 MDD non-responders 8 HC |
43.4±6.1 42.0±10.8 35.0±9.5 |
fMRI 1.5T ASL At Rest |
NR | NR | NR | Depressed | Patients medication free for 2+ weeks prior to study; rescanned after sleep deprivation | No patients with history of substance abuse, concurrent axis I disorders. | At baseline, responders had higher activity of L ventral ACC (including sgACC) that correlated with depressed mood. After sleep deprivation perfusion decreased in L + R ventral ACC cingulate in responders | NR |
| (Kumano et al 2006) | 19 cancer patients followed longitudinally | 58.4±15.7 (deterioration group) 57.9±16.4 (no change sample) |
18 F-FDG | NR | NR | No | Depressed + euthymic | Cancer medication | NR | Patients who became more depressed over time showed prodromal hypermetabolism of R ACC + L subcallosal gyrus | BA 25 −4; 9; −12 2; 11; −7 |
| (Chen et al 2007a) | 17 MDD No Controls |
44.06±8.36 | MRI 1.5T 3mm Sad facial stimuli |
NR | NR | NR | Depressed | Scanned before and after treatment with fluoxetine. Patients off medication 4+ weeks before study. | No current axis I comorbidity or substance abuse within 2 months of study. Personality disorders not assessed. | Increased functional activation of pregenual ACC and medial frontal cortex associated with decreased symptom severity at baseline | BA 32 −2; 40; 15 BA 10 −1; 53; 4 |
| (Fales et al 2008b) | 27 MDD 24 HC |
33.4±8 36.4±9 |
3T fMRI ROI Emotional interference task: houses and faces. |
NR | NR | NR | Depressed | No medication for 4+ weeks | No axis I disorders preceding onset of MDD, acute physical illness, trauma with loss of consciousness, current neurological disorder. | Elevated activity of sgACC in MDD | BA 24: −10; 35; −2 0; 13; 29 0; 13; 34 |
| (Nahas et al 2007) | 17 MDD | 46.8±6.3 | fMRI 1.5T |
NR | 71.2±57.3 months (current episode) | NR | Depressed | Yes – not specified | NR | VNS decreased activity of the R sgACC | BA 25 0; 8; −16 |
Table 21.
Functional Anatomical Studies of the Ventro-Medial Prefrontal Cortex in BD.
| Study | Sample | Age | Method | Age of Onset |
Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Drevets et al 1997) | 21 BD 21 HC |
35±8.2 34±8.2 |
1.5T 1mm slice ROI |
NR | NR | Yes | Depressed | Cohort not treated for 4 weeks prior to scans | NR | Decreased metabolism of L sgACC in BD group. | 1; 25; −6 |
| (Blumberg et al 2000) | 11 BD | 33.4±11.6 | 15O-H2O | NR | 14.2±14.9 (manic) 12.0±5.6 (euthymic) |
NR | 5 manic BD; 6 euthymic | MS, AP, AD, BZ | No comorbid axis I or II conditions. Substance abuse taking place > 5 years previously was allowed. | Manic patients had greater rCBF in R ventral ACC than remitted subjects | BA 32 10; 26; −8 |
| (Ketter et al 2001) | 43 BD I + II (treatment resistant) 43 HC |
37.5±10.6 38.1±10.4 |
18 F-FDG | 18.8±9.9 | 18.3±10.4 | NR | Depressed, mildly depressed + euthymic | Unmedicated for 2+ weeks | NR | Decreased metabolism of L middle frontal and inferior frontal gyri in depressed BD patients only. Global cerebral metabolism decreased in depressed BD too. | BA 9 + 44 No coordinates given |
| (Drevets et al 2002a) | 20 MDD 14 HC |
36±10 34±9.1 |
18 F-FDG | NR | NR | NR | Depressed | Patients medication free for 3+ weeks prior to study. | No other psychiatric disorders or substance abuse | Reduced baseline metabolism of L sgACC PFC in MDD | NR |
| (Dunn et al 2002) | 27 BD | 36.7±11.3 | 18 F-FDG | 18.0±9.9 | 26.7±14.6 | NR | Mildly to severely depressed | Unmedicated for 2+ weeks | No active substance abuse, eating disorder, OCD, dementia, medical illness | Anhedonia associated with greater metabolism of R sgACC | 10; 42; −4 |
| (Kegeles et al 2003) | 19 (14 MDD, 5 BD) 10 HC |
36±11 39±19 |
18 F-FDG | NR | NR | Yes | Depressed | BZ discontinued 24 hours before study in 12 cases. 7 subjects on BZ. Patients free of other medication for 2+ weeks. | 3 panic disorder, 2 dysthymia, 1 each with social phobia, simple phobia, anorexia + PTSD. No medical illness | Lower metabolic activity of the R pregenual ACC in MDD. | BA 32 4; 34; −12 |
| (Kruger et al 2003) | 11 depressed BD 9 remitted BD |
43±9 38±12 |
15O-H2O Voxel-wise | 22±6 | 8±3 (dep episodes) 3±2 (manic episodes) 8±5 (dep episodes) 3±2 (manic episodes) |
NR | Depressed/Remitted | MS | No axis I or II disorders. No substance abusers | BL decreases in rCBF to ventral medial PFC after sadness induction in both BD groups | In remitted group increased rCBF to dorsal anterior cingulate – BA24a: 10; 20; 24. Decreased rCBF to orbitomedial and ventromedial cortex – BA 11: 6; 42; −10 14; 46; −20 20; 62; −4 −18; 54; 10 −14; 64; 0 In depressed group: decreased orbitomedial and ventromedial rCBF: 8; 56; −6 4; 58; 9 |
| (Lennox et al 2004) | 10 BD 12 HC |
37.3±12.8 32.6±10.7 |
fMRI 3T voxel-wise |
NR | NR | NR | Manic | 8 Lith, 7 MS, 3 haloperidol, 4 olanzapine | NR | BD patients had attenuated BL activation of sgACC in response to sad faces | −2; 20; −14 BA25 |
| (Bauer et al 2005) | 10 BD I 10 HC |
39.3±7.8 35.0±9.3 |
18 F-FDG | NR | 20.4±7.0 | NR | Depressed | AD + MS | No psychosis | Higher activity in R sgACC which decreased with treatment. | 8; 24; −6 |
| (Haldane et al 2007) | 8 BD I | 42.1±11.8 | fMRI 1.5T 7mm (0.7mm gap) |
23.1±5.6 | 10.1±6.5 episodes | NR | Mildly depressed | Lamotrigine | No alcohol or substance abuse, significant medical or neurological disorder, treatment resistance, suicide attempts, axis I comorbidity | Greater activation of L medial frontal gyrus + R ACC in response to angry faces after lamotrigine therapy relative to baseline. | BA 10 −4; 46; 10 BA 32/24 10; 36; 6 |
| (Mah et al 2007) | 13 BD II 18 HC |
43.0±8.4 39.0±8.0 |
18 F-FDG | 20±10.5 | 22.9±12 | NR | Depressed | Lithium | No substance abuse within 90 days, substance dependence within 5 years. No current psychotic features. 1 OCD, 1 eating disorder | Increased metabolism of R pregenual ACC in BD. | 12; 47; 5 |
Other researchers have however, produced evidence of increased MDD and BD-associated metabolic activity of the ventral emotion circuit (Tables 19 and 21). A highly consistent finding across the literature has been that activity is elevated in the sgACC in the depressed phase relative to the remitted phase of MDD (Drevets et al 2002a) (Mayberg et al 2005) (Clark et al 2006) (Neumeister et al 2006b) (Hasler et al 2008). Consistent with these data, an fMRI study reported decreased response to sad facial stimuli in the right sgACC after AD treatment (Keedwell et al 2008).
An anatomical region more rostral to the sgACC (24/25), BA 32 (Figure 2), is also an integral part of the ventral “emotion” circuit, and has been implicated in affective illness. A voxel-based morphometry (VBM) study reported a 7.3% decrease of the GM density of the left ventral aspect of this region in a sample of patients with BD I (Lyoo et al 2004a). The partially medicated BD I, BD II, and cyclothymic sample of (Haznedar et al 2005) yielded similar results with decreased white and GM volume of the BA 32 area, noted. In line with these data, (Kegeles et al 2003) noted hypometabolism of BA 32 in depression. In contrast, (Holthoff et al 2004) reported a remission-associated decrease in the activity of this region and (Nobler et al 2001) obtained analogous results after ECT administration.
Individuals with MDD display a predominantly left sided hypometabolism of the ventro-medial circuit (Table 19) (Drevets et al 1997) (Kumano et al 2006). Compatible with these findings, (Smith et al 2002) found that decreased metabolism of the right sgACC at baseline was predictive of an improved response to antidepressant therapy. Similarly, higher baseline activity of the left sgACC at baseline was positively correlated with response to sleep deprivation therapy; although after treatment, responders showed a drop in perfusion of the left ventral cingulate (Clark et al 2006). Parallel findings of volume reductions of the ventral aspects of the left ACC are observed in morphometric analyses (Table 20).
The volumetric reductions seen in the left SGACC in some mood disordered subgroups may contribute to the complex relationship between clinical state and sgACC metabolism. Partial volume effects may have contributed to the original suggestions of hypometabolism (see (Mah et al 2007) and discussion below).
A similar pattern obtains in BD with left-sided hypometabolism or right-sided hypermetabolism (Drevets et al 1997) (Bauer et al 2005) (Mah et al 2007), and left-sided tissue loss (Drevets et al 1997) (Hirayasu et al 1999a) (Sassi et al 2004) (Wilke et al 2004) (Kaur et al 2005) of the broader ventral ACC region (Tables 21 and 22). One might hypothesise the reverse pattern to apply to the manic state (Drevets et al 1997), a phenomenon observed in the sample of (Blumberg et al 2000) which was characterized by elevated rCBF in the left sgACC.
During functional brain mapping studies of BD a study employing an Affective Go/No Go task showed greater activity to happy distracters in left sgACC, medial PFC and bilateral DLPFC, and greater activity in response to sad relative to neutral distracters in right ventrolateral PFC and DLPFC, in manic BD versus healthy adults (Elliott et al 2004).
The Dorsal “Cognitive” Circuit
(Davidson and Irwin 1999) illustrate how the line between cognition and emotion is becoming increasingly blurred in their description of the DLPFC as mediator of “affective working memory” (Davidson and Irwin 1999) (p 11). The DLPFC allows for the initially “raw” limbic-derived emotional stimuli which is refined through rounds of ever more comprehensive processing in the orbital and ventromedial circuits to be represented “online” so that it can drive goal directed behaviour (Davidson and Irwin 1999). In this sense, the dorsal aspects of the PFC discharge traditionally characterized executive processes such as response selection, inhibition, and error detection - the monitoring of actions to insure that they match intentions.
As reviewed by (Davidson 2002), in depression, a deficit in the top-down inhibitory control of the DLPFC over the amygdala and sundry limbic tissue may result in chronic limbic over-activity and negative emotions. Implicit in this deliberately over-simplified description of the above model is the notion that positive affect is primarily a consequence of the suppression of negative emotions.
MDD
Hypometabolism of the dorsal PFC is one of the most robust findings in both MDD (Hurwitz et al 1990) (Cohen et al 1989) (Biver et al 1994) (Bench et al 1995) (Dunn et al 2002) (Davidson et al 2003) (Chen et al 2007a) and BD (Buchsbaum et al 1986) (Baxter et al 1989) (Drevets et al 2002a) (Kruger et al 2003), and in some studies appears to normalize with successful treatment (Mayberg et al 1999) (Mayberg et al 2000) (Kennedy et al 2001) (Mayberg et al 2005) (Fales et al 2008a), lending support to the veridicality of the above-mentioned model of depression.
Consistent with these data, (Chen et al 2007a) found that severity of depression correlated negatively with GM volume of DLPFC and (Davis et al 2004) reported global decrements of both GM and WM volume, including areas of the DLPFC. We note that there are conflicting reports in the literature – see (Brody et al 1999) (Brody et al 2001) (Drevets et al 2002a) (Table 24).
Table 24.
Volumetric Changes of Dorsal PFC in MDD.
| Study | Sample | Age | Method | Age of Onset |
Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status | Psychiatric Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Shah et al 1998) | 20 MDD (chronic) 20 MDD (remitted) 20 HC |
21–65 | VBM | NR | NR | NR | Depressed and remitted | AD | No mania, significant substance abuse, organic pathology or neurological illness | Reduced GM volume of L DLPFC chronic MDD | −56; 1; 32 |
| (Chen et al 2007a) | 17 MDD | 44.06±8.36 | MRI 1.5T 3mm |
NR | NR | NR | Depressed | Scanned before and after treatment with fluoxetine. Patients off medication 4+ weeks before study. | No current axis I comorbidity or substance abuse within 2 months of study. Personality disorders not assessed. | Severity of depression negatively correlated with GM volume of DLPFC. | BA 46 31; 53; 15 −31; 45; 17 BA 9 32; 34; 30 −15; 35; 42 |
Nevertheless, the vast area of cortex that is subsumed under the term dorsal or DLPFC make the functional data difficult to interpret. The dorsal PFC consists of distinct functional units, some of which play the traditionally-described cognitive role, while others have closer ties to the more medial and ventral aspects of the PFC. For example, part of BA 9 in the medio-dorsal PFC is probably an important constituent of the viscero-motor network with projections to the lateral column of the PAG in macaques (An et al 1998).
BD
Decreases in the volume of the dorsal cortex, although not always the lateral convexity, have been reported in BD (Table 23). More recently, (Frangou 2005) and (Haznedar et al 2005) described GM volume reductions of the DLPFC (BA 8, 9, 45, 46) in medicated and remitted BD I patients, and partially medicated, “stable” bipolar-spectrum individuals, respectively. More circumscribed volume reductions of BA 9 have also reported in a medicated, euthymic pediatric sample (Dickstein et al 2005). An optimized VBM analysis of a mixed BD I and BD II sample (Lochhead et al 2004) reported reduced GM volume of the ACC immediately dorsal to the corpus callosum (CC).
Table 23.
Structural Imaging Analyses of Dorsal PFC in BD.
| Study | Sample | Age | Method | Age of Onset |
Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status |
Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Lopez-Larson et al 2002) | 17 BD 12 HC |
29±8 31±8 |
1.5T 1mm ROI |
NR | 7±6 | NR | Manic | 9 MS, 4 AP, 3 AD | No medical disorders, head injury, substance abuse in previous 3 months | Smaller L middle + superior GM volumes in BD | NR |
| (Doris et al 2004) | 11 BD I 11 HC |
40.5±11.6 38.1±10.8 |
2T 1mm VBM |
24.3±5.1 | 16.2±11.1 7.8±3.4 (hosp) |
NR | Relatively euthymic | MS, AD, AP | No comorbid conditions. | Decreases in GM density of dorsal-medial frontal gyri | 45;30;28 |
| (Lochhead et al 2004) | 11 (BD (7 BD I 4 BD II) 31 HC |
38.2±10 36±14 |
1.5T 1.5mm VBM |
24.3±9.2 | 9.0±6.4 episodes | NR | Depressed | No medication for 2+ weeks. | No co-morbid disorders. | Decrease in volume of BL dorsomedial ACC | 0; 27; 21 |
| (Dickstein et al 2005) | 20 BD 20 HC |
13.4±2.5 13.3±2.3 |
1.5T 1.2mm VBM |
10.1±3.2 | NR | NR | Euthymic | AP, MS, AD | ADHD, psychosis, anxiety | GM volume reduction of L DLPFC | BA 9 −32; 42; 32 |
| (Frangou 2005) | 43 BD 43 HC |
42.9±11 | 1.5T 1.5mm VBM |
25.5±9.2 | 16.0±19.0 | Mixed | Remitted | MS + AP | NR | Volume reduction of L DLPFC in BD | BA 9/46 |
| (Haznedar et al 2005) | 40 BD (BD I 17; BD II; 7 cyclothymia 16) 36 HC |
39.8±13.4 43.8±6.7 43.9±9.2 40.7±11.6 |
1.5T 1.2mm ROI |
NR | NR | ±50% | “Stable” | BD I but not BD II, cyclothymia on MS + AP | 4 anxiety disorders 19 substance abuse |
BL loss of GM and WM in DLPFC | BA 8, 9, 45, 46 |
| (Soares et al 2005) | 32 BD I 32 HC |
34±10.5 NR |
Deformation-field morphometry 1.5T 1.5mm |
NR | NR | NR | NR | NR | No axis I diagnoses, substance abuse in previous 6 months + serious medical conditions. | Smaller L DLPFC in males only. | NR |
| (Yatham et al 2007) | 15 BD 15 HC |
36±13 36±13 |
1.5T 1.5mm VBM |
NR | 3.9±8.1 | NR | Manic | 8 medication naive, rest AD | No medical or neurological illness, substance abuse | 6% reduction (not significant) in L ACC of BD | BA 32 −6; 36; 17 |
The Corpus Callosum
There is some preliminary evidence for decreased volume of the corpus callosum (CC) in BD (Coffman et al 1990) (Brambilla et al 2003b) (Atmaca et al 2007) and MDD (Lyoo et al 2002a) (Table 25). A meta-analysis of the BD studies supported the hypothesis that the collosal region is reduced in volume in BD (Arnone et al 2008). Congruent with these data, (Yurgelun-Todd et al 2007) reported BD-associated WM changes in the genu of the CC as measured by DTI.
Table 25.
Abnormalities of the Corpus Callosum in BD and MDD
| Study | Sample | Age | Method | Age of Onset | Illness Duration/# Episodes | Family History of Illness | Clinical Status at Testing | Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Wu et al 1993) | 20 MDD 16 HC |
32.9±11.5 30.5±9.8 |
1.5T 5mm ROI |
NR | NR | NR | Depressed | Medication free for 2+ weeks | NR | Anterior + posterior CC larger in MDD |
| (Lyoo et al 2002a) | 40 MDD 42 HC |
21.4±2.1 20.9±2.8 |
1.5T 1.5mm ROI |
16.7±1.7 | 4.8±1.3 | NR | Mildly depressed | Medication naive | No axis I or II disorders. No medical illness, head trauma. | Smaller genu and CC in minor depression. |
| (Brambilla et al 2004) | 23 MDD 36 HC |
41±10 37±10 |
1.5T ROI |
NR | 11±9 4±3 (episodes) |
NR | 9 euthymic 14 depressed | Off drugs for 2+ weeks. | No comorbid disorders. No substance abuse in previous 6 months. | No difference in CC signal intensity |
| (Bae et al 2006) | 106 MDD 84 HC |
70.4±6.4 71.7±6.0 |
DTI 1.5T 3mm ROI |
NR | NR | NR | Depressed | NR | NR | No WM changes in CC |
| (Nobuhara et al 2006) | 13 MDD 13 HC |
62.8±6.6 61.5±4.8 |
DTI 1.5T 6mm ROI |
52.9±7.3 | 4.0±2.6 | NR | Depressed | AD | No dementia, severe medical illness, neurological disorders | No WM changes in CC |
| (Yasar et al 2006) | 16 BD 21 HC |
15.5±3.4 16.9±3.8 |
1.5T 3mm ROI |
NR | NR | Yes | 2 depressed, 14 euthymic | Yes – not specified | 5 ADHD, 1 CD, 1 ODD. No substance abuse | No difference in CC |
| (Atmaca et al 2007) | 12 BD I 12 HC |
28.2±6.5 26.8±7.6 |
1.5T 2.4mm ROI |
27.4±6.1 | 0.3±0.4 | NR | 10 manic, 2 mixed | medication-naïve | No axis I conditions, substance abuse for 6+ months. 2 OCD, 2 PD. | CC significantly smaller in BD |
| (Ballmaier et al 2007) | 24 early-onset 24 late-onset 34 HC |
68.00±5.83 74.50±8.09 72.38±6.93 |
1.5T 1.4mm ROI |
33.25±16.05 71.27±7.23 |
4.80±4.13 episodes 0.50±0.90 episodes | NR | Depressed | Free of medication for 2+ weeks | No neurological illness, alcohol abuse/dependence, long-term AD use, comorbidity. | CC thinning in genu of early-onset MDD and genu and splenium of late-onset MDD. |
| (Yurgelun-Todd et al 2007) | 11 BPD 10 HC |
32.9±10.5 32.4±9.1 |
1.5T 5mm DTI |
21.7±5.4 | 12.0±9.8 | NR | Euthymic | Lith, MS, AP | No head injury, CNS disease, substance abuse for 6+ months | Higher FA in the midline of the genu but not splenium in BD |
Key to Table Abbreviations. AD=Antidepressants; ADHD=Attention Deficit Hyperactivity Disorder; AP=Anti-Psychotics; BA=Brodmann’s Area; BD=Bipolar Disorder; Benz=Benzodiazepines; BL=Bilateral; CD=Conduct Disorder; DM=Diabetes Mellitus; HC=Healthy Control; Hosp=Hospitalizations; L=Left; LD=Learning Disorder; Lith=Lithium; MS=Mood Stabilizers; NR=Not Reported; OCD=Obsessive Compulsive Disorder; ODD=Oppositional Defiant Disorder; PD=Personality Disorder; PDD=Pervasive Developmental Disorder; PTSD=Post-Traumatic Stress Disorder; R=Right; RH=Right Hemisphere; ROI= Region of Interest; TD=Tryptophan Depletion; MDD=Unipolar Depression; VBM=Voxel-Based Method.
Slice thickness is shown in methodology column. Stereotaxic coordinates are shown as x, y and z axes. For functional scans 18 F-FDG=[18F]-fluorodeoxyglucose; 15O-H2O=15O-Water
It is unclear from the above studies, however, whether the genu or splenium is preferentially affected. (Ballmaier et al 2007) have proposed that the effect is age of onset-specific: they reported genu-specific thinning in early-onset depressed patients but evidence of thinning of both the genu and splenium in late-onset MDD.
Discussion
The Amygdala
MDD
The finding of increased amygdala reactivity to negative stimuli is one of the most consistent findings in the literature (Thomas et al 2001) (Fu et al 2004) (Surguladze et al 2005) (Neumeister et al 2006a). In addition, (Siegle et al 2002) found that amygdalar responses to negative words were no longer visible after 10 seconds in healthy controls but persisted in depressed patients for at least 25 seconds, on average. Similarly, patients with MDD reportedly remember negative words better than positive words (Watkins et al 1992), a finding that correlates with increased BOLD activity of the right amygdala (Hamilton and Gotlib 2008).
The phenomenon may be reversed by antidepressant treatment. (Sheline et al 2001) showed that the elevated BOLD response seen in the left amygdala of depressed patients in response to masked fearful faces was reduced by sertraline. The apparent efficacy of antidepressant medications in attenuating this hyper-reactivity has received support from more recent studies (Fu et al 2004) (Chen et al 2007b). There is some suggestion that rather than being a stable trait, baseline hypermetabolic activity seen in MDD samples may be reflective of acute depression (Abercrombie et al 1998) (Drevets et al 2002b) (Surguladze et al 2005).
The inconsistency in the volumetric MRI literature in MDD may reflect the intrinsic problem that all analyses of the amygdala conducted to date were acquired using 1.5T scanners, which do not have the resolution to allow for the adequate definition of the boundaries of this diminutive region because of its proximity to other grey matter structures such as the claustrum, entorhinal cortex, hippocampus, and basal forebrain.
BD
Increased metabolism of the amygdala – both at base-line, and in response to emotional challenges such as negatively valenced faces (Yurgelun-Todd et al 2000) (Lawrence et al 2004) (Rich et al 2006) (Pavuluri et al 2007) - is commonly reported in BD samples, and may be attenuated by lamotrigine (Chang et al 2008). This increase in amygdala activity is often associated with greater MRI volume.
The amygdala may be an exception to this pattern with neuronal and dendritic hypertrophy reported in parallel to hypermetabolism (Vyas et al 2002) Elevated activity may be an adaptive mechanism that enhances sensitivity to aversive stimuli, thereby facilitating fear conditioning and anxiety-related phenomenology (McEwen and Chattarji 2004) (Radley and Morrison 2005).
Nevertheless, this hypothetical phenomenon cannot explain the decreased neuronal somal size (suggestive of reduced axo-dendritic connections) in the lateral amygdaloid and accessory basal parvocellular nuclei (Bezchlibnyk et al 2007), and the decreased number and density of lateral amygdaloid nucleus neurons (Berretta et al 2007) reported in postmortem BD subjects. The postulated hypertrophy of the amygdala is also inconsistent with the putative volume decrements seen in childhood BD, and a minority of adult samples (Pearlson et al 1997) (Blumberg et al 2003a).
One possibility is that studies reporting enlarged amygdala volumes in BD may be at least partly confounded by medication effects. (Chang et al 2005b) has suggested that hypertrophy of the amygdala may be related to exposure to mood stabilizers. This topic is addressed in detail below.
Amygdala Abnormalities and the Signs and Symptoms of MDD and BD
The amygdala plays a central role in the modulation of monoamine and corticosteroid release in response to aversive or novel stimuli. Disruption of the amygdala’s afferent and efferent connections may thus have negative implications for the regulation of mood and affect (Figure 1).
The Hippocampus
MDD
Hippocampal volume loss appears to be a sequala of depression, particularly in elderly or chronically ill samples. Further, hippocampal volume has been reported to be negatively related to risk of depressive relapse in patients followed over 2 years (Kronmuller et al 2008). Recurrent depressive illness appears to exert an insidious pathological effect on neural, and in particular, hippocampal tissue. Stress-induced dendritic atrophy has been shown to be mediated by an interaction of glucocorticoid receptor stimulation and excitatory amino acid transmission (specifically NMDA receptor stimulation) (McEwen and Magarinos 2001).
Notably, in rodents, the CA3 region of the dorsal hippocampus is the hippocampal area that shows the greatest vulnerability to excitotoxic processes (Sloviter 1996) (Ben-Ari and Cossart 2000) (Dudek and Sutula 2007). In humans with MDD and PTSD, the posterior hippocampus (the putative homologue of the rodent dorsal hippocampus) shows the most prominent reduction in volume relative to healthy controls (Neumeister et al 2005) (Bonne et al 2008).
At sufficiently high concentrations, glutamate acts as an excitotoxin and neuronal death may follow from intra-cellular calcium-driven cytoskeletal degeneration and free radical production (Lee et al 2002). At lower glutamate concentrations, hippocampal neurogenesis is inhibited and dendritic atrophy occurs in association with stress-induced glucocorticoid hormone secretion (McEwen and Magarinos 2001).
The latter effect may be mediated at least in part by down-regulated gene expression of brain-derived neurotrophic factor (BDNF) and other neurotrophins (Duman and Monteggia 2006). Rats exposed to corticosteroids or stressors show decreased expression of BDNF in the hippocampus (Gronli et al 2006) (Jacobsen and Mork 2006) (Tsankova et al 2006) (Xu et al 2006) although the effect may be limited to particular splice-variants of the protein (Nair et al 2006) (Tsankova et al 2006). Similarly humans with mood disorders have shown decreased serum (Karege et al 2002) and hippocampal BDNF levels at post-mortem (Dwivedi et al 2003) (Karege et al 2005).
Stress-induced plasticity of the hippocampus appears to be crucial for effective learning and memory, maintenance of goal directed behavior, and modulation of emotional behavior by contextual information (LeDoux 2000) (Frank et al 2006) (Morris 2006) (Hasler et al 2007). Prolonged prenatal and adult stress in primates, rodents and tree shrews leads to selective hippocampal damage including apoptosis, depressed long term potentiation (LTP) and neurogenesis, as well as, apical dendritic atrophy (Uno et al 1989) (Sapolsky et al 1990) (Watanabe et al 1992) (Magarinos et al 1996) (Czeh et al 2001). Similar effects have been noted in stress-related psychiatric disorders such as post-traumatic stress disorder (PTSD) (Bremner et al 1995) (Vythilingam et al 2005).
If the excitotoxic hypothesis holds true in humans then one would expect to see a negative correlation between the duration or severity of illness and hippocampal volume. There is mixed evidence for this potential effect (Table 5).
BD
In BD the data are less clear, perhaps because of the widespread use of mood stabilizers which appear to increase gray matter volume. Animal studies have demonstrated that lithium promotes hippocampal neurogenesis (Kim et al 2004) and long term potentiation (LTP) (Son et al 2003). A sample of BD patients treated for 4 weeks with lithium showed a 3% (24 cm3) increase in whole brain gray matter volumes from baseline (Moore et al 2000), an effect that appears to result from the neurotrophic effect of the drug (Manji et al 2000). Four more recent studies (Beyer et al 2004b) (Sassi et al 2004) (Bearden et al 2007) (Yucel et al 2007) comparing lithium-treated and non-lithium treated groups demonstrated similar effects in large cortical areas, including the hippocampus. The phenomenon may not be restricted to lithium with comparable effects noted with other classes of mood stabilizers, especially valproate (Mark et al 1995) (Hao et al 2004). In contrast, with the exception of tianeptine (Watanabe et al 1992) (McEwen et al 2002) (McEwen and Olie 2005), the neurotrophic properties of antidepressants are less persuasive - although see (Stewart and Reid 2000) and (Duman and Monteggia 2006).
An alternative explanation for the differential impact of MDD and BD on hippocampal structure is that the two disorders differ in etiology. This hypothesis, however, stands in contradistinction to evidence that MDD tends to aggregate in the relatives of individuals with BD (McGuffin and Katz 1989).
Hippocampal Changes and the Signs and Symptoms of MDD and BD
A disruption of hippocampal function may contribute to the deficits in executive performance, learning and emotion-mediated memory formation observed in mood disorders (Figure 1).
The Basal Ganglia
MDD
Both hypometabolism or blood flow and reduced grey matter volume have commonly been reported in the MDD literature (Tables 9 and 10). The former result may thus reflect a partial volume averaging effect rather than a genuine diminution in metabolic activity. Interpretation of imaging studies is, however, rendered difficult by the mass of contradictory results yielded through diverse scanning methodologies and population samples. We suggest that medication and age of onset are important confounding factors. In contrast, increased resting metabolic activity of the anteroventral striatum is apparent during depression, and may be linked particularly to anhedonic symptoms (Hasler et al 2008), consistent with evidence that depressives show blunted caudate activation during exposure to positively valenced sensory stimuli (Epstein et al 2006).
BD
No clear conclusions can yet be drawn from studies of the BG. There is some suggestion of increased striatal metabolism and volumetric GM increases in BD. As in the case of the hippocampus, it is plausible that these analyses are confounded by treatment effects. Enlargement of the BG nuclei is a well known effect of anti-psychotic drugs (Jernigan et al 1991); (Swayze et al 1992); (Chakos et al 1995); (Frazier et al 1996) and a perusal of Table 11 indicates that three of the studies reporting BG enlargement made use of partially manic samples treated with anti-psychotic medication (Strakowski et al 2002); (DelBello et al 2004); (Wilke et al 2004).
Metabolic activity or blood flow was consistently elevated in manic or hypomanic samples (Blumberg et al 2000) (Caligiuri et al 2003) (Caligiuri et al 2006) (Table 10). Nevertheless, hypermetabolism of the BG has also been reported in depressed samples, specifically in the ventral striatum (Ketter et al 2001) (Bauer et al 2005) (Mah et al 2007).
Potential Relationship of BG Changes to the Signs and Symptoms of BD and MDD
Impaired striatal function may explain the anhedonia and reduction in goal-seeking behavior that is observed in some patients with MDD and depressed BD cases. Conversely, the elevation in psychomotor activity is congruent with reports of increased metabolism or blood flow in more dorsal regions of the striatum in the manic phase of BD.
Ventriculomegaly and White Matter Pathology
MDD
Ventricular enlargement, usually of the third or lateral ventricles, is characteristic of older and chronically ill patients with depression, or patients with a late age of depression-onset. The white matter hyperintensities seen concomitantly in these patient groups raise the possibility of a vascular etiology for depression (Krishnan 2002) (Knopman et al 2005) (Sneed et al 2008).
Clearly, the hypothesized excitotoxic processes which may be operating in medial temporal and striatal tissue could theoretically cause ventricular enlargement. Nevertheless, the degree of subcortical atrophy needed to manifest as ventricular enlargement remains unclear. If long-term pathological processes are a prerequisite for ventriculomegaly then this may explain why the phenomenon appears to predominate in elderly populations. Factors such as chronic alcohol abuse (Anstey et al 2006) and incipient neurological disorders with prodromal depression may also contribute to enlargement of ventricles.
These data are congruent with the neuropathological studies of (Thomas et al 2002) and (Thomas et al 2003) which describe WM disease of the DLPFC in a sample of elderly depressed patients, a result replicated in a middle-aged sample of depressed individuals who showed reduced levels of myelin staining in the deep WM tracts of the DLPFC (Regenold et al 2007). One possible explanation for this potential demyelination is change in oligodendrocyte function. At least three post-mortem studies have reported a down-regulation of oligodendrocyte-related gene expression in MDD and BD (Hakak et al 2001) (Tkachev et al 2003) (Aston et al 2005), while decreased oligodendrocyte density has also been noted in several studies (Cotter et al 2002) (Hamidi et al 2004) (Uranova et al 2004) (Vostrikov et al 2007).
An unresolved issue is whether the WM pathology-depression relationship is one of cause or effect. Certainly, there appear to be cases that are precipitated by subcortical infarcts. For example, depression is a relatively common sequala of the genetic disorder, cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) (Chabriat et al 1995) (Desmond et al 1999). Similarly, given the increased rate of risk factors for cerebrovascular disease observed in MDD samples (Steffens et al 1999); (Lyness et al 2000) (Wassertheil-Smoller et al 2004), it is likely that subcortical ischemic events play a role in the development of late-onset MDD.
Nevertheless, some studies have made attempts to match patients and controls (or statistically control) for the presence of cerebrovascular risk factors and still find elevated rates of WMH in their MDD samples (Table 13). A possible explanation is that depression may predispose to the development of small WM lesions via some as yet occult pathophysiological mechanism.
Based on extant evidence in the literature (Biegon et al 1990) (Musselman et al 1996); (Lenze et al 1999) and (Nemeroff and Musselman 2000) have speculated that excess depression-associated secretion of serotonin by blood platelet cells facilitates cellular aggregation and therefore predisposes to atherosclerosis, thrombosis and vasoconstriction. Another possibility is impaired regulation of vascular tone. Cerebrovascular reactivity, which describes the compensatory dilatory capacity of arterioles to dilatory stimuli, has been reported to be reduced in acutely depressed patients without any neurological, cardiac or vascular risk factors (de Castro et al 2006).
BD
Ventriculomegaly is more commonly observed in BD across different age groups (Swayze et al 1990); (Figiel et al 1991); (Strakowski et al 1993); (Botteron et al 1995); (Zipursky et al 1997); (Lim et al 1999); (Strakowski et al 1999); (Hauser et al 2000); (Brambilla et al 2001a); (Strakowski et al 2002); (Davis et al 2004); (Strasser et al 2005); (Soares et al 2005).
It is plausible that as in the case of MDD, WM abnormalities are a long-term consequence rather than a cause of bipolar illness. One possibility is that people with BD have an excess of atherosclerotic risk factors that lead to microvascular pathology at an even earlier age than MDD. As reviewed by (Kilbourne et al 2004) and (Newcomer 2006), BD is associated with a significantly increased prevalence of cardiovascular disease risk factors such as smoking, obesity, diabetes mellitus (DM), hypertension and dyslipidemia. Hypertension (Dufouil et al 2001) (Gunstad et al 2005), obesity (Gustafson et al 2004), smoking (Dager and Friedman 2000) and DM (Novak et al 2006) have in turn been directly associated with the development of WMH. Further, drug abuse is prevalent in BD populations and stimulant drug-induced vasoconstriction may lead to WMH (Dupont et al 1990) (Lyoo et al 2004b). Marijuana may also interact in an additive fashion with WMH to predispose to depressive symptomatology (Medina et al 2007).
Although most published studies make an attempt to exclude patients with potentially confounding conditions, the whole gamut of risk conditions is very rarely controlled for, raising the possibility that WMH in BD are an artifact of medical co-morbidity ischemic risk factors.
Nevertheless, this hypothesis fails to account for the WM pathology noted in pediatric BD samples (Botteron et al 1995); (Lyoo et al 2002b); (Pillai et al 2002) as well as the high concentration of WMH in both BD subjects and their unaffected relatives reported by (Ahearn et al 1998). We suggest that although a proportion of BD individuals with significant WM pathology will present with cardiovascular risk factors, WMH may less commonly also co-occur with some kind of developmental insult. In other words, the WMH seen in pediatric or young adult BD samples are likely to have a different origin to those seen in older populations.
The etiology of these precocious lesions is unclear. Obstetric complications are well known to be associated with schizophrenia (see meta-analysis of (Cannon et al 2002)), but with a few exceptions (Kinney et al 1993); (Kinney et al 1998), appear less salient in BD. Nevertheless, it is possible that perinatal hypoxic events precipitate bipolar illness in a vulnerable minority (Pavuluri et al 2006).
The high incidence of familial WMH seen in the (Ahearn et al 1998) sample suggests that genetic factors may also be at play. A number of post-mortem analyses provided evidence for the altered gene expression of genes impacting myelin or oligodendrocyte function in both MDD and BD (Tkachev et al 2003) (Aston et al 2005) (Sequeira et al 2006). As reviewed by (Carter 2007a), (Carter 2007b), and (Sokolov 2007) variants of some of these genes such as oligodendrocyte lineage transcription factor 2 (OLIG2) [NCBI accession number 10215] Neuregulin 1 (NRG1) [3084], and v-erb-a erythroblastic leukemia viral oncogene homolog 4 (ERBB4) [2066] have been directly associated with affective illness and may determine how resilient these cells are to environmental stressors2. This hypothesis will be discussed in greater detail below.
Potential Relationship of WM Lesions to the Signs and Symptoms of BD and MDD
Lesions to the deep WM tracts of the frontal cortex and BG disrupt communication between key components of the viscero-motor network, resulting in a so-called “disconnection syndrome” with sequalae that bear some resemblance to the symptomatology induced by GM lesions to the individual components of the network.
The OFC
MDD
The evidence for increased metabolism of the OFC in depressed samples receives support from serotonin and catecholamine depletion studies which have elicited a similar effect in remitted patients as they develop depressive relapse (Neumeister et al 2004) (Hasler et al 2008). Congruent with these data, treatment with antidepressant medication (Brody et al 1999), psychotherapy (Goldapple et al 2004), and deep-brain stimulation (Mayberg et al 2005) has been associated with decreased metabolism of the OFC. The combination of elevated OFC activity and tissue loss in MDD samples is consistent with the operation of an excitotoxic process.
The structural MRI-derived evidence of OFC volume loss (Table 16) is supported by the post-mortem analysis of (Rajkowska et al 1999) which uncovered a 12% decrease in the thickness of the rostral (but not the caudal) OFC, and a 15% decrease in the middle OFC in depressed patients compared to healthy controls; a finding attributed to neuronal shrinkage with attendant reduction in volume of the neuropil. Further, a 15% decrease in glial cell density was observed in the caudal OFC.
Nevertheless, we note that a significant number of the patients in the samples demonstrating volume reductions became ill after the age of 40, raising the issue of etiological heterogeneity.
BD
BD samples also appear to be characterized by tissue loss in the OFC as measured by MRI. These data are supported by the post-mortem analysis of (Cotter et al 2005) who found evidence of reduced glial cell density and neuronal size in the caudal OFC of patients with BD. Further, the structural integrity of WM tracts in the OFC, as measured by diffusion tensor imaging (DTI), may also be compromised in adult (Beyer et al 2005) (Haznedar et al 2005) and pediatric (Frazier et al 2007) patients. GM loss secondary to excitatory metabolic disturbances is supported by the MRS study of (Cecil et al 2002) who recorded reduction of NAA and choline concentrations in the orbitofrontal GM of a BD sample.
Too few resting state studies have been conducted to reach a conclusion about BD-associated OFC metabolism. Nevertheless, fMRI studies using cognitive probes of behavioral inhibition and decision-making, have reported decreased OFC BOLD response in patients with mania (Elliott et al 2004) (Altshuler et al 2005b). Similarly, the passive viewing of emotional material has been associated with a relative decrease in the BOLD response of the left OFC in a patient with post-partum psychosis compared with her monozygotic cotwin (Fahim et al 2007). It is unclear how these fMRI finding relate to the putative OFC volume loss observed in BD.
Potential Relationship of Changes in the OFC to the Signs and Symptoms of BD and MDD
The OFC plays major roles in the regulation of emotional and by implication, social behaviour. Lesions to the OFC have been associated with depression, mood instability and anxiety in other clinical case-studies (Grafman et al 1996) (MacFall et al 2001), providing further evidence that this part of the brain is critical for the self-regulation of emotion and behaviour.
Theoretically, therefore, volumetric and perhaps metabolic changes to the OFC may account for the emotional and cognitive disinhibition often characteristic of affective illness. Reduced orbitofrontal activity in BD patients during performance of an emotional go/no-go task (Elliott et al 2002) (Elliott et al 2004) as well as the Stroop task, a measure of cognitive control, (Kronhaus et al 2006) has previously been noted. These data are relevant because impaired performance on the Stroop and go/no-go tasks have been separately demonstrated in MDD and BD samples (Erickson et al 2005) (Savitz et al 2007b).
Ventro-Medial “Emotion” Circuit
The modulation of visceral responses to affective stimuli seems to be crucial for translating OFC-derived valenced data into actions and behaviour (Ongur et al 2003), an idea popularized by Damasio and colleagues (Damasio 1996) (Bechara et al 1997) as the “somatic marker” (SM) hypothesis.
According to the SM conjecture, a somatic marker, an unpleasant or positive viscerally-generated stimulus such as anxiety or reward, is temporally-paired with a predicted future outcome. This juxtaposition of cognitive and emotional inputs ensures competent decision-making in complex situations because it allows individuals to anticipate the future positive and negative consequences of their actions. When this process goes awry, as in the case of individuals with lesions to the ventro-medial cortex, impaired judgment results (Damasio 1996).
Recent studies are indicative of increased metabolism of the sgACC in the depressed phase relative to the remitted phase of MDD patients (Drevets et al 2008). Congruent with these data, a tryptophan depletion study of healthy subjects showed that serotonin depletion resulted in increased rCBF in the sgACC (BA 24 and 25) (Talbot and Cooper 2006). (Neumeister et al 2004) had previously reported the same phenomenon using glucose metabolic measures in remitted, unmedicated patients with a history of MDD. Similarly, the depressive relapse associated with alpha-methyl-para-tyrosine induced catecholamine depletion in remitted MDD subjects was also associated with increased metabolism in the sgACC (Hasler et al 2008).
Changes in the metabolic activity of the ventro-medial circuit have also been reported after treatment and improvement in symptomatology. (Mayberg et al 2000) found that people who responded to a trial of fluoxetine showed decreased bilateral activity of the sgACC, while treatment with sertraline resulted in significant decreases in the activity of the left sgACC (Drevets et al 2002a). Two sleep deprivation studies showed a drop in elevated baseline levels of sgACC activity in depressed patients who responded to treatment (Wu et al 1999) (Clark et al 2006). In another indication that these changes may be independent of treatment modality, a deep-brain stimulation study (Mayberg et al 2005) showed reduced perfusion of both the anterior and posterior portions of the sgACC (BA 25 and part of 24, respectively; Figure 2) in treatment responders..
The ventral ACC has also been demonstrated to mediate fluctuations within the normal range of emotion. For example, (Mayberg et al 1999) asked healthy and depressed subjects to recall sad personal experiences and found that negative mood induction was associated with increased activity of the sgACC. On the other hand, women grieving the break-up of a romantic relationship have been reported to display reduced activity in the left pregenual and sgACC (Najib et al 2004).
Anatomical MRI studies have provided evidence for decreased sgACC volume in both MDD and BD (Drevets et al 2008). Moreover, (Ongur et al 1998) found a reduction in the number of glial cells together with an increase in neuronal density in the sgACC of patients with familial BD and MDD, suggesting that the reduction in neuropil is accounted for by the reduction in sgACC volumes reported in the literature. Using the same set of brain tissue, these findings were partially replicated by (Cotter et al 2001) who detected reduced glial density and neuronal size (but not density) in the region of pregenual ACC in patients with major depression. An analogous effect in the sgACC in both familial and non-familial depression with glial cell density reductions of 24% and 41%, respectively (Ongur et al 1998) (Drevets 2000b). These data receive support from animal models of depression.
Rats subjected to 3 weeks of repeated restraint stress show a 16–20% reduction of apical dendritic spine density in the anterior cingulate region of the medial PFC (Liston et al 2006) (Radley et al 2006). A corresponding effect has also been noted in the pups of mothers exposed to prenatal stress (Murmu et al 2006). This dendritic remodeling process has been shown to depend on interactions between NMDA receptor stimulation and glucocorticoid release during chronic or repeated stress, suggesting that the dendritic atrophy is a type stress-induced, slow excitotoxicity (Reagan and McEwen 1997).
These anatomical changes may correlate with behavior: Restraint stress-associated retraction of apical dendrites in the medial PFC of rodents has been associated with retarded extinction learning (Miracle et al 2006). The same effect may hold in humans. Healthy individuals with thinner ventromedial PFC tissue show a greater galvanic skin response to conditioned stimuli during extinction learning (Milad et al 2005). Chronic psychosocial stress may also impact glial cell function: rats exposed to 5 weeks of daily social defeat have been reported to show a suppression of gliogenesis in the medial PFC; an effect reversed by fluoxetine (Czeh et al 2007).
Interestingly, ibotenic acid-induced lesions of the rat mPFC (infralimbic/prelimbic and ACC cortices) have been shown to produce evidence for a lateralized effect: right but not left-sided lesions were anxiolytic (Sullivan and Gratton 2002). In contrast, left-sided lesions are anxiogenic, and result in increased sympathetic activity and corticosterone response to stress. This result is reminiscent of an earlier study in which dopamine depletion of the left but not right medial PFC rendered animals vulnerable to stress-associated ulceration (Sullivan and Szechtman 1995). Further, (Sullivan and Gratton 1999) found that left-sided lesions potentiate autonomic stress responses to restraint stress while right-sided lesions diminish these endocrine reactions. The putatively differential effect of the two hemispheres appears to follow a phylogenetic continuum.
Babinski (Babinski 1914) first discussed the anosognosic and manic sequelae of right-sided lesions while Goldstein (Goldstein 1939) coined the term, “catastrophic reaction” to describe the emotional distress and depressive symptomatology associated with left-hemisphere lesions. More modern structural imaging studies have lent support to the original clinical reports (Robinson et al 1984) (Morris et al 1996) and studies of idiopathic anxiety, depression, and BD have produced analogous findings (Silberman and Weingartner 1986) (Davidson 1992) (Pascual-Leone et al 1996) (Savitz et al 2004) (McDonald et al 2004b).
The physiological mechanisms underlying these effects have been extensively debated. Explanations generally circle around the theme of a positive emotion-producing, appetitive, reward-seeking circuit in the left PFC which interacts in a dialectical manner with a mirror neural network in the right-hemisphere (Flor-Henry 1979) (Sackeim et al 1982) (Savitz et al 2007a). Conceivably, a disruption of the regulatory capacity of these circuits, such as disinhibition of the right hemisphere after left hemisphere damage, may lead to affective illness.
Consistent with the above hypothesis, differential hemispheric functional activity of the mPFC has been reported in the literature. Nevertheless, caution should be exerted in interpreting these data because the PET data are too low in resolution to accurately resolve left from right in regions close to the midline.
Since the vast majority of the studies samples were limited to currently depressed patients, it is unclear whether the possible dichotomy in hemispheric activity is a stable trait which applies to euthymic populations. There is some evidence that it is more likely to be a state-dependent phenomenon. In both the (Drevets et al 1997) and the (Blumberg et al 2000) cohorts, the manic subjects had greater rCBF or metabolism in the ACC then in depressed or remitted individuals (in contrast, the volumetric deficit in the sgACC persisted across illness phases). Further, (Liotti et al 2002) reported that after the execution of a sadness-induction paradigm, rCBF was higher in the sgACC in healthy controls compared to remitted depressives.
It should be noted that a minority of researchers have reported the diametric pattern of right-sided hypometabolism or volume loss and left-sided hypermetabolism in MDD (Drevets et al 1992) (Wu et al 1999) (Kennedy et al 2001) and BD (Kegeles et al 2003) (Sharma et al 2003). In the case of the latter study, however, the sample was euthymic while the (Kegeles et al 2003) cohort was composed of both BD and MDD patients with comorbid anxiety disorders and was characterized by benzodiazepine (BZ) use at the time of the scanning. Further, these researchers reported right-sided hypometabolism of the pregenual as opposed to the sgACC and this may have accounted for the discrepancy in results.
Nevertheless, (Davidson and Irwin 1999) warn that most claims about hemispheric asymmetry of function are methodologically flawed because they are based on the observation that voxel-based activity in only one hemisphere reaches statistical significance. It does not, however, necessarily follow from this that the two hemispheres are significantly different from each other. This hypothesis needs to be tested by examining group or condition × hemisphere interactions (Davidson and Irwin 1999).
(Fornito et al 2007) favor a developmental rather than a stress-driven explanation for the sgACC volumetric changes believed to be characteristic of affective illness. These authors examined the folding patterns of the ACC, and reported a lower incidence of the adjacent paracingulate sulcus (PCS) in BD subjects compared with controls. Nevertheless, given the fact that the PCS is absent in many healthy individuals, the functional significance of this pattern of cortical folding is unclear.
Potential Relationship of Changes in the Ventro-Medial Circuit to the Signs and Symptoms of BD and MDD
Autonomic, endocrine and metabolic (McIntyre et al 2007) (Rottenberg 2007) (Smolin et al 2007) (Harvey 2008) (Surtees et al 2008) abnormalities are over-represented in individuals with affective illness. The ventromedial PFC, with its connections to the hypothalamus and brain-stem, modulates visceral output in response emotional stimuli (Price 2007). Conceivably, therefore, damage to the ventromedial PFC may not only dysregulate emotional function, but may play a pathoetiological role in the development of comorbid medical conditions.
The DLPFC
MDD
Hypometabolism and to a lesser extent GM volume decrements of particularly the left DLPFC have been widely reported in people suffering from depression. These data are consistent with the executive and working memory deficits characteristic of many such patients (Savitz et al 2005). They are also congruent with fMRI analyses that have reported altered BOLD signal in the DLPFC of MDD patients challenged with cognitive tasks that require executive control (Harvey et al 2005) (Matsuo et al 2007) (Siegle et al 2007).
As is the case with other neural networks, one complication of this literature is the potentially lateralized function of the PFC. Based on our rudimentary understanding of how emotional processing is lateralized in the brain, one would expect a preponderance of left dorsal cortex hypoactivation in depression. We are aware of at least 9 studies that have recorded left-sided hypofunction or GM loss of the dorsal PFC in MDD (Bench et al 1995) (Shah et al 1998) (Kennedy et al 2001) (Drevets et al 2002a) and BD (Baxter et al 1989) (Martinot et al 1990) (Lopez-Larson et al 2002) (Frangou 2005) (Dickstein et al 2005). Furthermore, right hemisphere hypoactiviation in MDD responders to sleep deprivation has been recorded (Clark et al 2006). Congruent with these reports, (Beauregard et al 2006) found that those individuals who experienced difficulty actively down-regulating sad thoughts showed a greater (presumably compensatory) response in the left mPFC (BA 10). More recently, (Grimm et al 2007) reported left-sided hypoactivity and right-sided hyperactivity in MDD patients, who as a group, tended to judge pictures as more negatively valenced than healthy controls.
This hypothetical lateralization of function could theoretically explain the minority of studies detailing increased activity of the DLPFC in MDD (Brody et al 2001) (Holthoff et al 2004). Nevertheless, none of these studies reported exclusive hypermetabolism of the right hemisphere. However, in one study the patients were only withdrawn from benzodiazepines three days prior to scanning, potentially confounding the metabolic measures (Holthoff et al 2004). Decreased activity of the right (Hurwitz et al 1990) DLPFC in depressed MDD patients has also been noted but again the withdrawal of benzodiazepines one day prior to scanning is a significant limitation.
Consistent with the notion of GM atrophy, histological changes to the DLPFC have been reported. Although no significant differences in cortical density were apparent across their MDD and control groups, (Rajkowska et al 1999) noted a depression-associated decrease in neuronal size with a concomitant decline in large cell density and increase in small neuronal cell density. Further, suicide has been associated with microgliosis of the DLPFC in a post-mortem schizophrenia and MDD sample (Steiner et al 2008)
BD
BD samples have tended to display evidence of dorsal PFC GM volume loss, and these putative changes are consistent with reports of aberrant dorsal PFC gene expression in patients with BD (Nakatani et al 2006) (Beneyto and Meador-Woodruff 2007) (Kanazawa et al 2007) (Pennington et al 2007) (Pillai 2008) (Shao and Vawter 2008) (Silberberg et al 2008) – although see (Ryan et al 2006) for a negative report. The mechanism by which these putative molecular changes impinge on the development of gross anatomical structures such as the DLPFC is not yet understood.
The Corpus Callosum
The functional consequences of callosal WM abnormalities are unclear. One proposal is that a disruption to inter-hemispheric transmission impairs cognitive function in people with mood disorders (Brambilla et al 2004). Damage to the CC, however, may retard the transfer of visual, motor, linguistic and somatosensory information in a regionally specific manner, and moreover, there may be some redundancy in these information highways, both within the CC itself, and subcortical circuitry (Gazzaniga 2005). Given the absence of salient deficits in these domains in affective illness, it seems likely that any lesions of the CC would preferentially affect cognitive or emotional processing. One possibility is that volume loss of the CC is secondary to abnormalities of the surrounding GM. Further work is needed to clarify the relationship between potential demyelination of the CC and cognitive and/or emotional impairment.
Over-Arching Discussion
Neurodevelopment Versus Neurodegeneration
The heritability of BD converges on the 60–80% range (McGuffin et al 2003) (Kieseppa et al 2004) while the heritability score for MDD is closer to the 40% mark (Agrawal et al 2004) (Boomsma et al 2005). Thus although genetic factors play an important etiological role in affective disorders, the importance of environmental variables should not be discounted. In fact, the average concordance rate among monozygotic (MZ) and dizygotic (DZ) twins stands at approximately 40% and 10%, respectively, for BD (McGuffin et al 2003) (Kieseppa et al 2004), and approximately 30% and 20% for MDD (Lyons et al 1998) (Kendler and Prescott 1999).
One potentially important environmental variable is exposure to adversity: stressful life events are known to precipitate bouts of affective illness in both BD (Kessing et al 2004); (Johnson 2005) and MDD (Kendler et al 1999) (Hettema et al 2006) populations.
Current models of pathological change in affective illness are deeply rooted to these environmental contingencies, as functional and anatomical change in depression is often viewed as degenerative: stress-induced, glutamate-mediated excitotoxicity leads to metabolic changes or decreases in GM volume. In contrast, the role of genetically-mediated neuroplasticity is not usually explicitly addressed in contemporary models of illness-associated neuropathology. We will first discuss the neurodegenerative hypothesis, which conceptualises GM or WM volume loss as a downstream effect of an unspecified environmental pathogen, such as psychological stress.
The degenerative model is based on the premise that psychological stress or some other pathophysiological insult is a necessary determinant of affective illness. Given the clustering of MDD and BD in families, and some reports that GM volume loss only occurs in familial cases (Drevets et al 1997) (Hirayasu et al 1999a) (Ongur et al 1998) (Brambilla et al 2001a) (Kegeles et al 2003) (Lacerda et al 2005) (Kogelnik et al 2006), one possibility is that psychological stress must also be familial in order for this conceptualization of illness to be valid.
Actually, there may be a familial or genetic component to the experience of life stress because of a phenomenon known as gene-environment correlation (Bergeman et al 1988); (Rutter 2007). (Rowe 1981) first reported this counter-intuitive notion by showing that adolescent twins’ reports of their parents’ levels of accepting and rejecting behaviour were under genetic influence; a finding that has been extended to retrospective measures of family warmth and parental control (Plomin et al 1988) as well as family cohesion and encouragement of growth (Bouchard et al 1990).
There are at least three ways in which gene-environment correlation might apply in the case of the degenerative hypothesis. The parental genotype or affective disorder may exert an effect on parental behaviour such that their children are reared in a high-stress environment. Here there is a correlation between passing on “stress-provoking” genes and providing a stressful family environment.
Secondly, it can be argued that people are selecting and shaping their environmental experiences on the basis of their genetic heritage, leading to preferential exposure to significantly stressful events and depression-associated neuroplastic changes in a subset of the population. This phenomenon may be related to the way in which individuals perceive or process information in their environment; an intrinsic bias often described as temperament.
Certainly, so-called dysthymic or anxiety-related personality traits have been widely described in MDD individuals, while BD is characterized by various combinations of dysthymic, cyclothymic-unstable and hypomanic traits (Evans et al 2005) (Savitz and Ramesar 2006) (Savitz et al 2008a) (Savitz et al 2008b). Since these traits are likely underpinned by genetic factors (reviewed in (Savitz and Ramesar 2004) (Ebstein 2006)), temperament may mediate the impact of genes on environmental experiences (Savitz and Ramesar 2006).
Yet a third possibility is that genetic effects play no role in influencing exposure to stressors but moderate the physiological effect of these events on neural tissue. One class of proteins potentially involved in this type of gene-environment interaction is the neurotrophins.
As reviewed by (Poo 2001), one of these enzymes, brain-derived neurotrophic factor (BDNF) [627], increases forebrain serotonin fibre density and neurogenesis, prevents spontaneous and neurotoxin-induced cell death, and modulates the formation of synaptic connections, particularly in the PFC and hippocampus.
Recent studies have suggested that the low expression (met) allele of a functional single nucleotide polymorphism (SNP) (Val66Met) of the BDNF gene may increase the probability of developing depression (Kaufman et al 2006) and cognitive impairment (Savitz et al 2007c) after exposure to childhood maltreatment. Perhaps through its reduced ability to protect against neurotoxicity, the met allele has also been reported to increase the risk of developing depression after stroke (Kim et al 2007).
Another potential moderator of the stress-response is central serotonergic activity. As reviewed by (Drevets 2000b), the binding of serotonin to post-synaptic 5-HT1A receptors not only enhances the negative feedback inhibition of cortisol release but also prevents dendritic cytoskeletal breakdown by catalyzing the release of the neurotrophic factor, S100β, and indirectly inhibiting protein kinase-induced apoptosis (Szatmari et al 2007). The regulation of 5-HT1A receptors in the raphe is at least partly controlled by functional variants of the HTR1A [3350] (−1019C/G; rs6295) (Lemonde et al 2003) (Parsey et al 2006) and the SLC6A4 [6532] (promoter region length polymorphism) (David et al 2005) genes, respectively.
In contradistinction to the degenerative model, the developmental model advocates that neuroanatomical changes precede the onset of affective illness. An interesting set of animal experiments has lent credence to this hypothesis: A line of rats, genetically-bred to suffer from learned helplessness display baseline hypometabolism of the amygdalae, BG, VTA, dorsal-frontal, medial-OFC and ACC, but increased metabolism of the infraradiata (sgACC), hippocampi and habenula (Shumake et al 2000); (Shumake et al 2002). To further control for the effects of early-life stress, (Shumake et al 2004) examined the brains of this genetic line of rats at birth and again found hypo or hypermetabolism of most of these regions. Moreover, the midbrain and brain-stem regions were found to be disconnected from limbic forebrain regulation, suggesting to the authors that the fundamental disturbance in depression is one of top-down regulatory control (Shumake et al 2004).
In humans one way of examining this issue is to compare the degree of variation in regions of interest across the life-span. (Lupien et al 2007) found that there was just as much variability in the hippocampal volumes of healthy young adults as in older individuals, implying that volume decrements attributed to aging or stress could be reflective of neurodevelopmental differences. Specifically, a quarter of their subjects in the 18–24-year age group had hippocampal volumes as small as the average hippocampal size in their 60–75-year-old sample, and the mean difference in hippocampal volumes between the upper and lower quartiles of the young age group (12–16%) was greater than volumetric reductions typically seen in depressed samples (Lupien et al 2007). These data are congruent with an earlier study (Gilbertson et al 2002) which reported an association between post-traumatic stress disorder (PTSD) and smaller hippocampal volume in war veterans. Intriguingly, the MZ twin brothers of the PTSD cohort who did not serve in the military also presented with smaller hippocampi than the PTSD group, raising the possibility that reduced hippocampal volumes are a contributing cause rather than an effect of PTSD.
Recent findings from the emerging field of imaging genomics also emphasize the importance of genetic influences. A variant of the neuregulin 1 (NRG1) [3084] gene, which is involved in the myelination process, and has been implicated in both BD and schizophrenia, may be associated with WM density and integrity of the internal capsule (McIntosh et al 2007). In another study, the short (s) allele of the serotonin transporter (5-HTT) gene (SLC6A4) [6532] promoter polymorphism has been shown to be associated with increased resting CBF in the amygdala and decreased perfusion of the ventromedial PFC in healthy individuals (Rao et al 2007).
The neurodevelopmental hypothesis can also be evaluated by searching for neural changes in unaffected family members who presumably share a genetic diathesis for the disorder with their ill relatives. (Noga et al 2001) compared MZ pairs discordant for BD with a control group of unaffected twins, and found that the right hippocampus was smaller in the affected twins, but that both ill and well twins had larger caudate nuclei than the control pairs. (McDonald et al 2004a) reported that genetic risk for BD was associated with reduced volume of the right anterior cingulate gyrus and ventral striatum. Similarly, a compensatory hypermetabolic response to a sadness induction paradigm was observed in the medial PFC of healthy BD relatives compared with background controls (Kruger et al 2006). Conversely, (McIntosh et al 2006) and (Munn et al 2007) failed to detect any significant neural changes in at-risk BD relatives.
Concerning MDD, (Monk et al 2007) reported that the pediatric offspring of parents with MDD displayed greater amygdala and accumbens area activity in response to fearful faces, and lower accumbens area activation in response to happy faces than a low-risk control group. A small number of serotonin depletion experiments have succeeded in inducing depressive symptoms in otherwise healthy relatives of MDD probands. Six out of 20 healthy males with a family-history of affective illness but 0 out of 19 male controls displayed a lowering of mood in response to tryptophan depletion (Benkelfat et al 1994). More recently, (van der Veen et al 2007) reported a greater lowering of mood, and stronger amygdala response to fearful faces under tryptophan depletion in healthy individuals with a family history of depression compared with controls. (Neumeister et al 2002) showed that this effect may be mediated by the SLC6A4 promoter length polymorphism: family-history-positive heterozygotes showed a greater mood-lowering effect than their heterozygote counterparts without a history of depression.
These potential neuroimaging endophenotypes are most likely genetically-driven. For example, serotonergic activity not only plays an important role in modulating the impact of stressful events, but is a key regulator of neural development influencing neurogenesis, apoptosis and dendritic growth (Gaspar et al 2003). Fluoxetine-induced suppression of the serotonin transporter during development has been shown to result in abnormalities of emotional behaviour in mice (Ansorge et al 2004). Recent data have also shown the direct effect of the 5-HTT polymorphism on neural tissue with increased hemodynamic response of the amygdala (Hariri et al 2002); (Heinz et al 2005); (Pezawas et al 2005); (Dannlowski et al 2006) to fearful faces (versus geometric images or neutral faces) in s allele carriers.
The distinction between early, developmental, and later-onset stress-induced pathology may be partly artificial. Genetically-determined subtleties of brain-wiring may sensitise the individual to the effect of ubiquitous, relatively mild stressors.
The s allele of the above-mentioned 5-HTT gene insertion/deletion polymorphism, first associated with anxiety-related personality traits more than a decade ago (Lesch et al 1996), is now one of the prototypical examples of a risk variant that interacts with adverse life experiences to predispose to psychopathology (Caspi et al 2003); (Kaufman et al 2004).
(Pezawas et al 2005) investigated the neurobiology behind this process. The authors demonstrated that healthy carriers of the s allele of the polymorphism display reduced functional connectivity between the amygdala and the sgACC. The latter structure exerts an inhibitory effect on the amygdala3 and thus a genetically-determined attenuation of this negative-feedback loop may increase sensitivity to environmental adversity and by implication, lead to maladaptive neuroplastic changes (Pezawas et al 2005).
A nascent trend in the study of psychiatric disorders is a recognition of the potentially important role of epigenetic mechanisms in disease causation (see (Mill and Petronis 2007)). Epigenetic inheritance refers to a regulated pattern of gene expression which is transmitted intact from one or other of the parents to their offspring. The process is mediated by the methylation and histone acetylation of cytosine residues and chromatin, respectively, leading to the activation or silencing of particular genes. The phenomenon is epigenetic because it results in phenotypic traits that are inherited independently of the informational content of DNA.
(Meaney and Szyf 2005) review rodent studies which demonstrate that stress sensitivity in rat pups is modulated by parental grooming behavior that exerts its effect through a histone modification-driven regulation of glucocorticoid receptor gene expression. If these biological mechanisms generalize to humans then exposure to adversity may modify gene expression in pathways that impact neuroplasticity.
Methodological and Theoretical Issues
(1). A common confounding variable is medical treatment. As (Drevets 1998) notes, rCBF and metabolism of various neuroanatomical regions may be reduced by antidepressants, anti-psychotics and anxiolytics. Further, psychotropic drugs have been shown to alter both the behavioral and the neurophysiological response to the environmentally valenced stimuli used as neurocognitive probes in fMRI studies.
Recent studies have detailed the neurotrophic effects of lithium and mood stabilizers on hippocampal and other neural tissue. In fact, there has been some suggestion that AD may also exert a neurotrophic effect in particular regions of the brain (Stewart and Reid 2000) (Rocher et al 2004) (Duman and Monteggia 2006). These data are supported by an fMRI study which showed that depressed patients suffer from reduced functional coupling of the amygdala with diverse brain regions including the hippocampus, caudate, putamen, and ACC; an effect reversed by treatment with fluoxetine (Chen et al 2007b). Similarly, a decrease in left amygdala activity to normal has been observed after antidepressant treatment (Drevets et al 2002a). Interestingly, a decrement in amygdala activity in response to aversive stimuli also been observed in healthy individuals treated with citalopram (Harmer et al 2006) and reboxetine (Norbury et al 2007).
Neuroleptics, which are commonly used to treat BD, may also exert a neurotrophic effect, with reports of post-treatment increases in basal ganglia volumes (or shape) in patients with BD (Hwang et al 2006) and schizophrenia (Chakos et al 1994) (Gur et al 1998) (Massana et al 2005) (Glenthoj et al 2007) (Okugawa et al 2007).
The association between imaging changes and medication is rendered even more complicated by the possibility that treatment may be a proxy variable for genetic etiology. In other words, the hippocampal or sgACC volumetric changes associated with a drug like lithium, for example, could theoretically be characteristic of a particular subtype of BD that just happens to be responsive to lithium (Moore et al In press). This is one example of etiological heterogeneity that may be a significant contributor to inter-study variability.
(2). Another example of disease heterogeneity is the difference in the pathophysiological mechanisms underlying early-onset and late-onset depression discussed above. Other hidden etiological differences may be an even more pernicious source of bias. In genetic studies, a distinction is often made between those patients who are recurrently ill and those subjects who have experienced one life-time episode of depression (Zubenko et al 2002), but this is rarely seen in the imaging literature. Further, the degree to which MDD or BD runs in the families of recruited subjects or whether MDD patients are recruited from BPD families is not always detailed. Differences between psychotic and non-psychotic “subtypes” of BD may also contribute to inter-study variability in findings. Approximately 50% of BD I patients experience psychosis (Keck et al 2003) (Ketter et al 2004) and recent evidence suggests that working memory deficits may be specific to those patients with a history of psychosis (Glahn et al 2007) (Savitz et al in press).
Information about obstetric or other developmental problems is rarely reported. The diagnosis of BD in children has increased sharply (mostly in the Unites States) in recent years, yet it is unclear as to whether children diagnosed with BD actually suffer from the same disorder as adults (Duffy 2007). This is particularly true when the broader phenotype of severe mood dysregulation (irritability and hyperarousal), which overlaps with ADHD, is used (Duffy 2007). A narrower pediatric clinical phenotype may more faithfully represent adult nosological categories (Brotman et al 2007). Caution should therefore be exerted in extrapolating neuroimaging findings from these pediatric populations to adults and vice versa, particularly when broad diagnostic criteria are used. This caveat is illustrated by (Biederman et al 2007) who reported that pediatric BD patients with co-morbid ADHD show additive patterns of MRI-evinced volume loss characteristic of both disorders when studied independently.
(3). State versus trait outcome differences do not always receive the attention that they merit: identification of the neuroanatomical or functional changes associated with the acute effects of depression and mania may serve as a useful means of evaluating the efficacy of treatments. Conversely, mood-independent abnormalities may be endophenotypes that can be exploited for genetic studies.
(4). While functional and morphometric analyses of affective illness often receive separate treatment in the literature, these two factors cannot be divorced from each other on either theoretical or methodological grounds. As alluded to above, GM volume loss may occur secondary to glutamate-driven excitotoxicity, a phenomenon which presumably correlates with elevated glucose metabolic activity (Shulman et al 2004). Volume loss may however, lead to an underestimation of metabolic activity because of partial voluming effects: the inclusion of hypometabolic WM or CSF in putatively GM-containing voxels.
An example of this potential confound can be found in our own work. Initially, we found evidence of reduced metabolic activity in conjunction with reduced volume of the subgenual ACC in the depressed phase of both MDD and BD (Drevets et al 1997) (Drevets et al 2002a). Compatible with this hypothesis, depressed BD samples treated chronically with lithium indeed showed elevated sgACC metabolism irrespective of correction for partial volume effects (Bauer et al 2005) (Mah et al 2007), consistent with evidence that lithium treatment is associated increase in the sgACC GM volume (Moore et al In press).
Another example can be found in studies of the amygdala. Despite reports of volume reductions, hypermetabolism of the amygdala is a consistent feature of the literature, which suggests that the increase in activity, if genuine, may be substantial – on the order of 70%, even though state-of-the-art PET imaging technology detects this as only a 6% difference between depressives and controls due to spatial resolution (i.e., partial volume) limitations (Drevets et al 1992). The partial voluming effect can be attenuated to some extent by region of interest (ROI) based analyses of a small central region of the ROI as implemented by the Drevets group, presumably facilitated their finding of substantially increased amygdalar activity (Drevets et al 2002b).
Limitations in spatial resolution also have impinged on the efficacy of volumetric MRI measures. Further, most of the older and even current imaging platforms do not have the necessary spatial resolution to accurately detail volumetric changes in dimunitive anatomical structures such as individual amygdalar nuclei. This limitation may lead to the implicit reification of neuroanatomical function; that is, the notion that gross anatomical structures should be uniformally affected by mood disorders simply because they are imagable units.
If one takes this argument to its logical extreme it becomes questionable as to what constitutes a replication. In other words, how similar do the functional or structural changes reported across studies have to be in order to establish that the identical functional units are affected?
(5). A comparison of the analytical methods used in imaging analysis is beyond the scope of this review. Nevertheless, a brief discussion of the 2 primary analytical approaches to imaging data analysis bears mentioning. Voxel-based analysis (as implemented in imaging analysis software such as the Statistical Parametric Mapping [SPM] series) is based on a mass-univariate statistical approach that compares the differences between two or more subject groups at each individual voxel in the brain (Ashburner and Friston 2000). As such, Gaussian random field theory is used to correct for the multiple dependent comparisons that would, if uncorrected, lead to false positive results (Ashburner and Friston 2000).
Voxel-wise analyses, however, are also highly sensitive to Type II errors because spatial normalization algorithms cannot precisely overlay small structures like the amygdala and sgACC across subjects, exaggerating the statistical variance. Possibly therefore, voxelwise analyses should not be the method of choice when diminutive, subcortical structures are the subject of study (Bookstein 2001) (Nugent et al 2006). Despite this limitation, voxel-wise analysis affords the advantage of allowing agnosticism with respect to the pathophysiology of the disorder under investigation.
On the other hand, the region-of-interest (ROI) approach relies on extant empirical or theoretical data to identify candidate regions that may show inter-group differences. Thus, assuming the veridicality of the disease model, Bayesian inference suggests that the probability of a significant ROI result being a true positive, is higher than in cases where convergent a priori data are absent. Nonetheless, the ROI approach is time and resource intensive especially when subject groups are large. The strength of the method is critically dependent on the precision of ROI segmentation, which depends heavily on the reproducibility of the anatomical landmarks chosen to delineate the target structure.
To our knowledge, very few comparisons of ROI and voxel-wise approaches have been made in psychiatrically ill samples. In one such study, (Kubicki et al 2002) that the voxel-wise approach for comparing cerebral volumes, termed “voxel-based morphometry (VBM)”, produced an analogous finding (volume of STG) to their previously published ROI study, but also showed changes in other regions, one of which had not been previously implicated in schizophrenia. Later schizophrenia studies produced reasonably convergent results across ROI and VBM analyses in cortical regions (Job et al 2002) (Giuliani et al 2005). (Douaud et al 2006) extended the correspondence in VBM-ROI results to the striatum in a case-control study of Huntington’s disease; although it is unclear whether a VBM analysis would be able to detect the more subtle subcortical changes characteristic of affective illness. In at least one case, however, PTSD-associated hippocampal changes have been obtained in the same sample using both ROI and VBM approaches (Emdad et al 2006).
We did not identify a clear difference in the results of VBM and ROI analyses in the BD and MDD literature (Tables 1 through 25), possibly because there are very few published VBM studies of subcortical regions.
(6). Genetic association studies are plagued by false positive results: with approximately 20, 000 genes, and multiple variants within each gene of interest, the a priori probability of a true association is low. Sample sizes in analyses which combine genetic and imaging data are by nature small, although this is offset to some extent by the relative precision of the phenotypic data that are collected. The problem can be partially ameliorated by targeted hypotheses.
A Heuristic Model
Top-down and bottom-up disruptions to cortico-striatal-limbic circuits are the most straightforward method of describing the pathophysiological and symptomatological changes associated with affective illness. We have not made any attempt to distinguish between MDD and BD, here. A graphical representation is provided in Figure 1.
As discussed above, projections from the orbital and medial PFC to the amygdala and its associated limbic and brainstem nuclei form a “visceromotor network” that modulates endocrine, autonomic, and behavioral aspects of emotion (Ongur et al 2003).
In the top-down model, impaired PFC function, or cortical-subcortical “disconnection” disinhibits downstream limbic projections, altering emotional behavior. For example, disinhibition of the amygdala projections to the bed nucleus of the stria-terminalus (BNST), hypothalamus and periaqueductal gray matter (PAG) (Behbehani 1995) (Sah et al 2003) may increase cortisol releasing hormone (CRH) release and anxiety symptoms. Disinhibition of projections from the amygdala to the nucleus basalis, locus ceruleus and ventral tegmental area (VTA) (Davis and Whalen 2001) (Sah et al 2003) could account for the alterations in cholinergic (ACh), noradrenergic (NE) and dopaminergic (DA) transmission which may affect mood and attention. Finally, disinhibition of amygdala projections to the ventral striatum (Cardinal et al 2002) would attenuate reward-seeking and goal-directed behavior, potentially contributing to the anhedonia and amotivation characteristic of depression. According to the bottom-up model, a functional hypersensitivity of limbic nuclei such as the amygdala, raphe and parahippocampus would predispose to dysregulation of PFC-mediated regulatory mechanisms.
In reality, the distinction between bottom-up and top-down models is artifical. If MDD and BD are polygenic disorders underpinned by many genes of small effect size, affected individuals are likely to possess many different risk variants affecting multiple neuroanatomical pathways and a single point of origin is unlikely.
The etiology of the suspected hypersensitivity or lesions4 is unclear but most likely involves complex gene-environment interactions. For example, the s allele of the 5-HTT promoter variant may predispose to reduced functional connectivity between the amygdala and perigenual PFC (Pezawas et al 2005), which may be maladaptive under stress. Similarly, the NRG1 gene may impact the myelination process and therefore predispose to WM lesions and a disruption to cortical-subcortical connections in the presence of cardiovascular risk factors. Two nonsynonymous SNPs of another gene, proline dehydrogenase (oxidase) 1 (PRODH) [5625] have also been associated with frontal WM volume reductions in schizophrenia (Zinkstok et al 2007).
Other potential examples are the −1019C/G single nucleotide polymorphism (rs6295) of the HTR1A gene promoter which disrupts a glucocorticoid binding site and modulates raphe-PFC serotonergic transmission (Lemonde et al 2003), and the val66met change in the BDNF gene which appears to impact hippocampal volumes in schizophrenic (Szeszko et al 2005) (Ho et al 2006), healthy (Pezawas et al 2004) (Bueller et al 2006), BD (Chepenik et al 2008) and depressed (Frodl et al 2007) individuals.
Many other similar examples are likely to emerge over time and hold out great promise for disinterring the latent pathophysiological basis of affective illness.
Table 6.
Functional Studies Reporting a Significant Difference in the Hippocampus in MDD.
| Study | Sample | Age | Method | Age of Onset | Duration of Illness/# Episodes | Family History of Illness | Clinical Status at Testing | Medication Status | Comorbidity | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| (Kennedy et al 2001) | 13 MDD 24 HC |
36±10 31.7±6.7 |
18 F-FDG | NR | 2.84±3.95 episodes | NR | Depressed | Scanned before and after treatment with paroxetine. Off medication of 4+ weeks prior to study. | No patients with concurrent DSM diagnosis. | Recovery associated with decreased hippocampal metabolism 30; −28; −12 |
| (Videbech et al 2001) | 42 MDD 47 HC |
42±13 41±12 |
15O-H2O | NR | 2 episodes | NR | Moderately to severely depressed | AD | No substance abuse | Increased activity of R hippocampus in MDD. 29; −9; −20 |
| (Goldapple et al 2004) | 17 MDD | 41±9 | 18 F-FDG Voxel-wise | NR | NR | NR | Depressed | Unmedicated | No psychotic symptoms, axis I disorders and substance abuse | Response to cognitive behavior therapy associated with increased metabolism of hippocampus −26; −36; −8 38; −10; −14 |
Table 8.
Functional Analyses Reporting Differences in the Hippocampus in BD.
| Study | Sample | Age | Method | Age of Onset |
Illness Duration/# Episodes |
Family History of Illness |
Clinical Status at Testing |
Medication Status |
Comorbidity | Findings | Brodmann Map/Stereotaxic Coordinates |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Bauer et al 2005) | 10 BD I 10 HC |
39.3±7.8 35.0±9.3 |
18 F-FDG voxelwise | NR | 20.4±7.0 | NR | Depressed | AD + MS | No psychosis | Activity in R hippocampus decreased with successful treatment with thyroxine. BD group still showed elevated metabolism of R hippocampus after treatment. | 34; −26; −8 |
| (Mah et al 2007) | 13 BD II 18 HC |
43.0±8.4 39.0±8.0 |
18 F-FDG | 20±10.5 | 22.9±12 | NR | Depressed | Lithium | No substance abuse within 90 days, substance dependence within 5 years. No current psychotic features. 1 OCD, 1 eating disorder | Increased metabolism of L parahippocampal gyrus. | −22; −35; −7 |
Footnotes
Perhaps because of inadequate differentiation between non-human primate and human neuroanatomy, the literature is characterized by inconsistent usage of Brodmann map areas which make up the sgACC. We recommend the human anatomical schema of Price and colleagues which can be found in Figure 3. Nevertheless, in Tables 21 through 24 we have cited the authors’ original anatomical descriptions, verbatim.
Oligodendrocytes have a high density of glutamate receptors and also are particularly vulnerable to glutamate-induced excitotoxicity.
The regulation of the amygdala by the sgACC is proving to be increasingly complicated. Recent evidence suggests that although area 25 does indeed exert inhibitory effects, projections from area 24 actually have an excitatory effect on the amygdala. Vidal-Gonzalez I, Vidal-Gonzalez B, Rauch SL, Quirk GJ (2006): Microstimulation reveals opposing influences of prelimbic and infralimbic cortex on the expression of conditioned fear. Learn Mem 13:728–733.
Here we use the term “lesion”, loosely, to signify any illness predisposing change in neurochemical function or neuroanatomical structure.
References
- Abercrombie HC, Schaefer SM, Larson CL, Oakes TR, Lindgren KA, Holden JE, et al. Metabolic rate in the right amygdala predicts negative affect in depressed patients. Neuroreport. 1998;9:3301–3307. doi: 10.1097/00001756-199810050-00028. [DOI] [PubMed] [Google Scholar]
- Abler B, Greenhouse I, Ongur D, Walter H, Heckers S. Abnormal reward system activation in mania. Neuropsychopharmacology. 2008;33:2217–2227. doi: 10.1038/sj.npp.1301620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler CM, Adams J, DelBello MP, Holland SK, Schmithorst V, Levine A, et al. Evidence of white matter pathology in bipolar disorder adolescents experiencing their first episode of mania: a diffusion tensor imaging study. Am J Psychiatry. 2006a;163:322–324. doi: 10.1176/appi.ajp.163.2.322. [DOI] [PubMed] [Google Scholar]
- Adler CM, Delbello MP, Jarvis K, Levine A, Adams J, Strakowski SM. Voxel-Based Study of Structural Changes in First-Episode Patients with Bipolar Disorder. Biol Psychiatry. 2006b doi: 10.1016/j.biopsych.2006.05.042. [DOI] [PubMed] [Google Scholar]
- Adler CM, Holland SK, Schmithorst V, Wilke M, Weiss KL, Pan H, Strakowski SM. Abnormal frontal white matter tracts in bipolar disorder: a diffusion tensor imaging study. Bipolar Disord. 2004;6:197–203. doi: 10.1111/j.1399-5618.2004.00108.x. [DOI] [PubMed] [Google Scholar]
- Adler CM, Levine AD, DelBello MP, Strakowski SM. Changes in gray matter volume in patients with bipolar disorder. Biol Psychiatry. 2005;58:151–157. doi: 10.1016/j.biopsych.2005.03.022. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. A population based twin study of sex differences in depressive symptoms. Twin Res. 2004;7:176–181. doi: 10.1375/136905204323016159. [DOI] [PubMed] [Google Scholar]
- Ahearn EP, Steffens DC, Cassidy F, Van Meter SA, Provenzale JM, Seldin MF, et al. Familial leukoencephalopathy in bipolar disorder. Am J Psychiatry. 1998;155:1605–1607. doi: 10.1176/ajp.155.11.1605. [DOI] [PubMed] [Google Scholar]
- Ahn KH, Lyoo IK, Lee HK, Song IC, Oh JS, Hwang J, et al. White matter hyperintensities in subjects with bipolar disorder. Psychiatry Clin Neurosci. 2004;58:516–521. doi: 10.1111/j.1440-1819.2004.01294.x. [DOI] [PubMed] [Google Scholar]
- Ahn MS, Breeze JL, Makris N, Kennedy DN, Hodge SM, Herbert MR, et al. Anatomic brain magnetic resonance imaging of the basal ganglia in pediatric bipolar disorder. J Affect Disord. 2007;104:147–154. doi: 10.1016/j.jad.2007.04.015. [DOI] [PubMed] [Google Scholar]
- al-Mousawi AH, Evans N, Ebmeier KP, Roeda D, Chaloner F, Ashcroft GW. Limbic dysfunction in schizophrenia and mania. A study using 18F-labelled fluorodeoxyglucose and positron emission tomography. Br J Psychiatry. 1996;169:509–516. doi: 10.1192/bjp.169.4.509. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997;54:915–922. doi: 10.1001/archpsyc.1997.01830220033006. [DOI] [PubMed] [Google Scholar]
- Altshuler L, Bookheimer S, Proenza MA, Townsend J, Sabb F, Firestine A, et al. Increased amygdala activation during mania: a functional magnetic resonance imaging study. Am J Psychiatry. 2005a;162:1211–1213. doi: 10.1176/appi.ajp.162.6.1211. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Bartzokis G, Grieder T, Curran J, Jimenez T, Leight K, et al. An MRI study of temporal lobe structures in men with bipolar disorder or schizophrenia. Biol Psychiatry. 2000;48:147–162. doi: 10.1016/s0006-3223(00)00836-2. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Bartzokis G, Grieder T, Curran J, Mintz J. Amygdala enlargement in bipolar disorder and hippocampal reduction in schizophrenia: an MRI study demonstrating neuroanatomic specificity. Arch Gen Psychiatry. 1998;55:663–664. doi: 10.1001/archpsyc.55.7.663. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Bookheimer SY, Townsend J, Proenza MA, Eisenberger N, Sabb F, et al. Blunted activation in orbitofrontal cortex during mania: a functional magnetic resonance imaging study. Biol Psychiatry. 2005b;58:763–769. doi: 10.1016/j.biopsych.2005.09.012. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Conrad A, Hauser P, Li XM, Guze BH, Denikoff K, et al. Reduction of temporal lobe volume in bipolar disorder: a preliminary report of magnetic resonance imaging. Arch Gen Psychiatry. 1991;48:482–483. doi: 10.1001/archpsyc.1991.01810290094018. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Curran JG, Hauser P, Mintz J, Denicoff K, Post R. T2 hyperintensities in bipolar disorder: magnetic resonance imaging comparison and literature meta-analysis. Am J Psychiatry. 1995;152:1139–1144. doi: 10.1176/ajp.152.8.1139. [DOI] [PubMed] [Google Scholar]
- Amodio DM, Frith CD. Meeting of minds: the medial frontal cortex and social cognition. Nat Rev Neurosci. 2006;7:268–277. doi: 10.1038/nrn1884. [DOI] [PubMed] [Google Scholar]
- An X, Bandler R, Ongur D, Price JL. Prefrontal cortical projections to longitudinal columns in the midbrain periaqueductal gray in macaque monkeys. J Comp Neurol. 1998;401:455–479. [PubMed] [Google Scholar]
- Anand A, Li Y, Wang Y, Wu J, Gao S, Bukhari L, et al. Activity and connectivity of brain mood regulating circuit in depression: a functional magnetic resonance study. Biol Psychiatry. 2005;57:1079–1088. doi: 10.1016/j.biopsych.2005.02.021. [DOI] [PubMed] [Google Scholar]
- Ansorge MS, Zhou M, Lira A, Hen R, Gingrich JA. Early-life blockade of the 5-HT transporter alters emotional behavior in adult mice. Science. 2004;306:879–881. doi: 10.1126/science.1101678. [DOI] [PubMed] [Google Scholar]
- Anstey KJ, Jorm AF, Reglade-Meslin C, Maller J, Kumar R, von Sanden C, et al. Weekly alcohol consumption, brain atrophy, and white matter hyperintensities in a community-based sample aged 60 to 64 years. Psychosom Med. 2006;68:778–785. doi: 10.1097/01.psy.0000237779.56500.af. [DOI] [PubMed] [Google Scholar]
- Arnone D, McIntosh AM, Chandra P, Ebmeier KP. Meta-analysis of magnetic resonance imaging studies of the corpus callosum in bipolar disorder. Acta Psychiatr Scand. 2008 doi: 10.1111/j.1600-0447.2008.01229.x. [DOI] [PubMed] [Google Scholar]
- Ashburner J, Friston KJ. Voxel-based morphometry--the methods. Neuroimage. 2000;11:805–821. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- Ashtari M, Greenwald BS, Kramer-Ginsberg E, Hu J, Wu H, Patel M, et al. Hippocampal/amygdala volumes in geriatric depression. Psychol Med. 1999;29:629–638. doi: 10.1017/s0033291799008405. [DOI] [PubMed] [Google Scholar]
- Aston C, Jiang L, Sokolov BP. Transcriptional profiling reveals evidence for signaling and oligodendroglial abnormalities in the temporal cortex from patients with major depressive disorder. Mol Psychiatry. 2005;10:309–322. doi: 10.1038/sj.mp.4001565. [DOI] [PubMed] [Google Scholar]
- Atmaca M, Ozdemir H, Yildirim H. Corpus callosum areas in first-episode patients with bipolar disorder. Psychol Med. 2007:1–6. doi: 10.1017/S0033291706009743. [DOI] [PubMed] [Google Scholar]
- Axelson DA, Doraiswamy PM, McDonald WM, Boyko OB, Tupler LA, Patterson LJ, et al. Hypercortisolemia and hippocampal changes in depression. Psychiatry Res. 1993;47:163–173. doi: 10.1016/0165-1781(93)90046-j. [DOI] [PubMed] [Google Scholar]
- Aylward EH, Roberts-Twillie JV, Barta PE, Kumar AJ, Harris GJ, Geer M, et al. Basal ganglia volumes and white matter hyperintensities in patients with bipolar disorder. Am J Psychiatry. 1994;151:687–693. doi: 10.1176/ajp.151.5.687. [DOI] [PubMed] [Google Scholar]
- Babinski J. Contribution a l’etude des troubles mentaux dans l’hemiplegia organique cerebrale. Revue Neurologique. 1914;1:845–848. [Google Scholar]
- Bachevalier J, Loveland KA. The orbitofrontal-amygdala circuit and self-regulation of social-emotional behavior in autism. Neurosci Biobehav Rev. 2006;30:97–117. doi: 10.1016/j.neubiorev.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Bae JN, Macfall JR, Krishnan KR, Payne ME, Steffens DC, Taylor WD. Dorsolateral prefrontal cortex and anterior cingulate cortex white matter alterations in late-life depression. Biol Psychiatry. 2006;60:1356–1363. doi: 10.1016/j.biopsych.2006.03.052. [DOI] [PubMed] [Google Scholar]
- Ballmaier M, Kumar A, Elderkin-Thompson V, Narr KL, Luders E, Thompson PM, et al. Mapping Callosal Morphology in Early- and Late-Onset Elderly Depression: An Index of Distinct Changes in Cortical Connectivity. Neuropsychopharmacology. 2007 doi: 10.1038/sj.npp.1301538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballmaier M, Toga AW, Blanton RE, Sowell ER, Lavretsky H, Peterson J, et al. Anterior cingulate, gyrus rectus, and orbitofrontal abnormalities in elderly depressed patients: an MRI-based parcellation of the prefrontal cortex. Am J Psychiatry. 2004;161:99–108. doi: 10.1176/appi.ajp.161.1.99. [DOI] [PubMed] [Google Scholar]
- Bammer R. Basic principles of diffusion-weighted imaging. Eur J Radiol. 2003;45:169–184. doi: 10.1016/s0720-048x(02)00303-0. [DOI] [PubMed] [Google Scholar]
- Bauer M, London ED, Rasgon N, Berman SM, Frye MA, Altshuler LL, et al. Supraphysiological doses of levothyroxine alter regional cerebral metabolism and improve mood in bipolar depression. Mol Psychiatry. 2005;10:456–469. doi: 10.1038/sj.mp.4001647. [DOI] [PubMed] [Google Scholar]
- Baumann B, Danos P, Krell D, Diekmann S, Leschinger A, Stauch R, et al. Reduced volume of limbic system-affiliated basal ganglia in mood disorders: preliminary data from a postmortem study. J Neuropsychiatry Clin Neurosci. 1999;11:71–78. doi: 10.1176/jnp.11.1.71. [DOI] [PubMed] [Google Scholar]
- Baxter LR, Jr, Phelps ME, Mazziotta JC, Guze BH, Schwartz JM, Selin CE. Local cerebral glucose metabolic rates in obsessive-compulsive disorder. A comparison with rates in unipolar depression and in normal controls. Arch Gen Psychiatry. 1987;44:211–218. doi: 10.1001/archpsyc.1987.01800150017003. [DOI] [PubMed] [Google Scholar]
- Baxter LR, Jr, Phelps ME, Mazziotta JC, Schwartz JM, Gerner RH, Selin CE, Sumida RM. Cerebral metabolic rates for glucose in mood disorders. Studies with positron emission tomography and fluorodeoxyglucose F 18. Arch Gen Psychiatry. 1985;42:441–447. doi: 10.1001/archpsyc.1985.01790280019002. [DOI] [PubMed] [Google Scholar]
- Baxter LR, Schwartz JM, Phelps ME, Mazziotta JC, Guze BH, Selin CE, et al. Reduction of prefrontal cortex glucose metabolism common to three types of depression. Arch Gen Psychiatry. 1989;46:243–250. doi: 10.1001/archpsyc.1989.01810030049007. [DOI] [PubMed] [Google Scholar]
- Bearden CE, Thompson PM, Dalwani M, Hayashi KM, Lee AD, Nicoletti M, et al. Greater Cortical Gray Matter Density in Lithium-Treated Patients with Bipolar Disorder. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2006.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauregard M, Paquette V, Levesque J. Dysfunction in the neural circuitry of emotional self-regulation in major depressive disorder. Neuroreport. 2006;17:843–846. doi: 10.1097/01.wnr.0000220132.32091.9f. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Tranel D, Damasio AR. Deciding advantageously before knowing the advantageous strategy. Science. 1997;275:1293–1295. doi: 10.1126/science.275.5304.1293. [DOI] [PubMed] [Google Scholar]
- Behbehani MM. Functional characteristics of the midbrain periaqueductal gray. Prog Neurobiol. 1995;46:575–605. doi: 10.1016/0301-0082(95)00009-k. [DOI] [PubMed] [Google Scholar]
- Bell-McGinty S, Butters MA, Meltzer CC, Greer PJ, Reynolds CF, 3rd, Becker JT. Brain morphometric abnormalities in geriatric depression: long-term neurobiological effects of illness duration. Am J Psychiatry. 2002;159:1424–1427. doi: 10.1176/appi.ajp.159.8.1424. [DOI] [PubMed] [Google Scholar]
- Ben-Ari Y, Cossart R. Kainate, a double agent that generates seizures: two decades of progress. Trends Neurosci. 2000;23:580–587. doi: 10.1016/s0166-2236(00)01659-3. [DOI] [PubMed] [Google Scholar]
- Bench CJ, Frackowiak RS, Dolan RJ. Changes in regional cerebral blood flow on recovery from depression. Psychol Med. 1995;25:247–261. doi: 10.1017/s0033291700036151. [DOI] [PubMed] [Google Scholar]
- Beneyto M, Meador-Woodruff JH. Lamina-Specific Abnormalities of NMDA Receptor-Associated Postsynaptic Protein Transcripts in the Prefrontal Cortex in Schizophrenia and Bipolar Disorder. Neuropsychopharmacology. 2007 doi: 10.1038/sj.npp.1301604. [DOI] [PubMed] [Google Scholar]
- Benkelfat C, Ellenbogen MA, Dean P, Palmour RM, Young SN. Mood-lowering effect of tryptophan depletion. Enhanced susceptibility in young men at genetic risk for major affective disorders. Arch Gen Psychiatry. 1994;51:687–697. doi: 10.1001/archpsyc.1994.03950090019003. [DOI] [PubMed] [Google Scholar]
- Bergeman CS, Plomin R, McClearn GE, Pedersen NL, Friberg LT. Genotype-environment interaction in personality development: identical twins reared apart. Psychol Aging. 1988;3:399–406. doi: 10.1037//0882-7974.3.4.399. [DOI] [PubMed] [Google Scholar]
- Berretta S, Pantazopoulos H, Lange N. Neuron numbers and volume of the amygdala in subjects diagnosed with bipolar disorder or schizophrenia. Biol Psychiatry. 2007;62:884–893. doi: 10.1016/j.biopsych.2007.04.023. [DOI] [PubMed] [Google Scholar]
- Beyer JL, Kuchibhatla M, Payne M, Moo-Young M, Cassidy F, MacFall J, Krishnan KR. Caudate volume measurement in older adults with bipolar disorder. Int J Geriatr Psychiatry. 2004a;19:109–114. doi: 10.1002/gps.1030. [DOI] [PubMed] [Google Scholar]
- Beyer JL, Kuchibhatla M, Payne ME, Moo-Young M, Cassidy F, Macfall J, Krishnan KR. Hippocampal volume measurement in older adults with bipolar disorder. Am J Geriatr Psychiatry. 2004b;12:613–620. doi: 10.1176/appi.ajgp.12.6.613. [DOI] [PubMed] [Google Scholar]
- Beyer JL, Taylor WD, MacFall JR, Kuchibhatla M, Payne ME, Provenzale JM, et al. Cortical white matter microstructural abnormalities in bipolar disorder. Neuropsychopharmacology. 2005;30:2225–2229. doi: 10.1038/sj.npp.1300802. [DOI] [PubMed] [Google Scholar]
- Bezchlibnyk YB, Sun X, Wang JF, Macqueen GM, McEwen BS, Young LT. Neuron somal size is decreased in the lateral amygdalar nucleus of subjects with bipolar disorder. J Psychiatry Neurosci. 2007;32:203–210. [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Makris N, Valera EM, Monuteaux MC, Goldstein JM, Buka S, et al. Towards further understanding of the co-morbidity between attention deficit hyperactivity disorder and bipolar disorder: a MRI study of brain volumes. Psychol Med. 2007:1–12. doi: 10.1017/S0033291707001791. [DOI] [PubMed] [Google Scholar]
- Biegon A, Essar N, Israeli M, Elizur A, Bruch S, Bar-Nathan AA. Serotonin 5-HT2 receptor binding on blood platelets as a state dependent marker in major affective disorder. Psychopharmacology (Berl) 1990;102:73–75. doi: 10.1007/BF02245747. [DOI] [PubMed] [Google Scholar]
- Biver F, Goldman S, Delvenne V, Luxen A, De Maertelaer V, Hubain P, et al. Frontal and parietal metabolic disturbances in unipolar depression. Biol Psychiatry. 1994;36:381–388. doi: 10.1016/0006-3223(94)91213-0. [DOI] [PubMed] [Google Scholar]
- Blumberg HP, Donegan NH, Sanislow CA, Collins S, Lacadie C, Skudlarski P, et al. Preliminary evidence for medication effects on functional abnormalities in the amygdala and anterior cingulate in bipolar disorder. Psychopharmacology (Berl) 2005a;183:308–313. doi: 10.1007/s00213-005-0156-7. [DOI] [PubMed] [Google Scholar]
- Blumberg HP, Fredericks C, Wang F, Kalmar JH, Spencer L, Papademetris X, et al. Preliminary evidence for persistent abnormalities in amygdala volumes in adolescents and young adults with bipolar disorder. Bipolar Disord. 2005b;7:570–576. doi: 10.1111/j.1399-5618.2005.00264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg HP, Kaufman J, Martin A, Whiteman R, Zhang JH, Gore JC, et al. Amygdala and hippocampal volumes in adolescents and adults with bipolar disorder. Arch Gen Psychiatry. 2003a;60:1201–1208. doi: 10.1001/archpsyc.60.12.1201. [DOI] [PubMed] [Google Scholar]
- Blumberg HP, Leung HC, Skudlarski P, Lacadie CM, Fredericks CA, Harris BC, et al. A functional magnetic resonance imaging study of bipolar disorder: state- and trait-related dysfunction in ventral prefrontal cortices. Arch Gen Psychiatry. 2003b;60:601–609. doi: 10.1001/archpsyc.60.6.601. [DOI] [PubMed] [Google Scholar]
- Blumberg HP, Martin A, Kaufman J, Leung HC, Skudlarski P, Lacadie C, et al. Frontostriatal abnormalities in adolescents with bipolar disorder: preliminary observations from functional MRI. Am J Psychiatry. 2003c;160:1345–1347. doi: 10.1176/appi.ajp.160.7.1345. [DOI] [PubMed] [Google Scholar]
- Blumberg HP, Stern E, Martinez D, Ricketts S, de Asis J, White T, et al. Increased anterior cingulate and caudate activity in bipolar mania. Biol Psychiatry. 2000;48:1045–1052. doi: 10.1016/s0006-3223(00)00962-8. [DOI] [PubMed] [Google Scholar]
- Blumberg HP, Stern E, Ricketts S, Martinez D, de Asis J, White T, et al. Rostral and orbital prefrontal cortex dysfunction in the manic state of bipolar disorder. Am J Psychiatry. 1999;156:1986–1988. doi: 10.1176/ajp.156.12.1986. [DOI] [PubMed] [Google Scholar]
- Boes AD, McCormick LM, Coryell WH, Nopoulos P. Rostral Anterior Cingulate Cortex Volume Correlates with Depressed Mood in Normal Healthy Children. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2007.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonelli RM, Kapfhammer HP, Pillay SS, Yurgelun-Todd DA. Basal ganglia volumetric studies in affective disorder: what did we learn in the last 15 years? J Neural Transm. 2006;113:255–268. doi: 10.1007/s00702-005-0372-7. [DOI] [PubMed] [Google Scholar]
- Bonne O, Vythilingam M, Inagaki M, Wood S, Neumeister A, Nugent AC, et al. Reduced posterior hippocampal volume in posttraumatic stress disorder. J Clin Psychiatry. 2008;69:1087–1091. doi: 10.4088/jcp.v69n0707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bookstein FL. “Voxel-based morphometry” should not be used with imperfectly registered images. Neuroimage. 2001;14:1454–1462. doi: 10.1006/nimg.2001.0770. [DOI] [PubMed] [Google Scholar]
- Boomsma DI, van Beijsterveldt CE, Hudziak JJ. Genetic and environmental influences on Anxious/Depression during childhood: a study from the Netherlands Twin Register. Genes Brain Behav. 2005;4:466–481. doi: 10.1111/j.1601-183X.2005.00141.x. [DOI] [PubMed] [Google Scholar]
- Botteron KN, Raichle ME, Drevets WC, Heath AC, Todd RD. Volumetric reduction in left subgenual prefrontal cortex in early onset depression. Biol Psychiatry. 2002;51:342–344. doi: 10.1016/s0006-3223(01)01280-x. [DOI] [PubMed] [Google Scholar]
- Botteron KN, Vannier MW, Geller B, Todd RD, Lee BC. Preliminary study of magnetic resonance imaging characteristics in 8- to 16-year-olds with mania. J Am Acad Child Adolesc Psychiatry. 1995;34:742–749. doi: 10.1097/00004583-199506000-00014. [DOI] [PubMed] [Google Scholar]
- Bouchard TJ, Jr, Lykken DT, McGue M, Segal NL, Tellegen A. Sources of human psychological differences: the Minnesota Study of Twins Reared Apart. Science. 1990;250:223–228. doi: 10.1126/science.2218526. [DOI] [PubMed] [Google Scholar]
- Brambilla P, Harenski K, Nicoletti M, Mallinger AG, Frank E, Kupfer DJ, et al. MRI study of posterior fossa structures and brain ventricles in bipolar patients. J Psychiatr Res. 2001a;35:313–322. doi: 10.1016/s0022-3956(01)00036-x. [DOI] [PubMed] [Google Scholar]
- Brambilla P, Harenski K, Nicoletti M, Sassi RB, Mallinger AG, Frank E, et al. MRI investigation of temporal lobe structures in bipolar patients. J Psychiatr Res. 2003a;37:287–295. doi: 10.1016/s0022-3956(03)00024-4. [DOI] [PubMed] [Google Scholar]
- Brambilla P, Harenski K, Nicoletti MA, Mallinger AG, Frank E, Kupfer DJ, et al. Anatomical MRI study of basal ganglia in bipolar disorder patients. Psychiatry Res. 2001b;106:65–80. doi: 10.1016/s0925-4927(01)00073-7. [DOI] [PubMed] [Google Scholar]
- Brambilla P, Nicoletti M, Sassi RB, Mallinger AG, Frank E, Keshavan MS, Soares JC. Corpus callosum signal intensity in patients with bipolar and unipolar disorder. J Neurol Neurosurg Psychiatry. 2004;75:221–225. [PMC free article] [PubMed] [Google Scholar]
- Brambilla P, Nicoletti MA, Harenski K, Sassi RB, Mallinger AG, Frank E, et al. Anatomical MRI study of subgenual prefrontal cortex in bipolar and unipolar subjects. Neuropsychopharmacology. 2002;27:792–799. doi: 10.1016/S0893-133X(02)00352-4. [DOI] [PubMed] [Google Scholar]
- Brambilla P, Nicoletti MA, Sassi RB, Mallinger AG, Frank E, Kupfer DJ, et al. Magnetic resonance imaging study of corpus callosum abnormalities in patients with bipolar disorder. Biol Psychiatry. 2003b;54:1294–1297. doi: 10.1016/s0006-3223(03)00070-2. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Narayan M, Anderson ER, Staib LH, Miller HL, Charney DS. Hippocampal volume reduction in major depression. Am J Psychiatry. 2000;157:115–118. doi: 10.1176/ajp.157.1.115. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Randall P, Scott TM, Bronen RA, Seibyl JP, Southwick SM, et al. MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995;152:973–981. doi: 10.1176/ajp.152.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Vythilingam M, Vermetten E, Nazeer A, Adil J, Khan S, et al. Reduced volume of orbitofrontal cortex in major depression. Biol Psychiatry. 2002;51:273–279. doi: 10.1016/s0006-3223(01)01336-1. [DOI] [PubMed] [Google Scholar]
- Brody AL, Saxena S, Silverman DH, Alborzian S, Fairbanks LA, Phelps ME, et al. Brain metabolic changes in major depressive disorder from pre- to post-treatment with paroxetine. Psychiatry Res. 1999;91:127–139. doi: 10.1016/s0925-4927(99)00034-7. [DOI] [PubMed] [Google Scholar]
- Brody AL, Saxena S, Stoessel P, Gillies LA, Fairbanks LA, Alborzian S, et al. Regional brain metabolic changes in patients with major depression treated with either paroxetine or interpersonal therapy: preliminary findings. Arch Gen Psychiatry. 2001;58:631–640. doi: 10.1001/archpsyc.58.7.631. [DOI] [PubMed] [Google Scholar]
- Brotman MA, Kassem L, Reising MM, Guyer AE, Dickstein DP, Rich BA, et al. Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. Am J Psychiatry. 2007;164:1238–1241. doi: 10.1176/appi.ajp.2007.06101619. [DOI] [PubMed] [Google Scholar]
- Brown FW, Lewine RJ, Hudgins PA, Risch SC. White matter hyperintensity signals in psychiatric and nonpsychiatric subjects. Am J Psychiatry. 1992;149:620–625. doi: 10.1176/ajp.149.5.620. [DOI] [PubMed] [Google Scholar]
- Bruno S, Cercignani M, Ron MA. White matter abnormalities in bipolar disorder: a voxel-based diffusion tensor imaging study. Bipolar Disord. 2008;10:460–468. doi: 10.1111/j.1399-5618.2007.00552.x. [DOI] [PubMed] [Google Scholar]
- Buchsbaum MS, Wu J, DeLisi LE, Holcomb H, Kessler R, Johnson J, et al. Frontal cortex and basal ganglia metabolic rates assessed by positron emission tomography with [18F]2-deoxyglucose in affective illness. J Affect Disord. 1986;10:137–152. doi: 10.1016/0165-0327(86)90036-4. [DOI] [PubMed] [Google Scholar]
- Bueller JA, Aftab M, Sen S, Gomez-Hassan D, Burmeister M, Zubieta JK. BDNF Val66Met allele is associated with reduced hippocampal volume in healthy subjects. Biol Psychiatry. 2006;59:812–815. doi: 10.1016/j.biopsych.2005.09.022. [DOI] [PubMed] [Google Scholar]
- Bush G, Luu P, Posner MI. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci. 2000;4:215–222. doi: 10.1016/s1364-6613(00)01483-2. [DOI] [PubMed] [Google Scholar]
- Caetano SC, Hatch JP, Brambilla P, Sassi RB, Nicoletti M, Mallinger AG, et al. Anatomical MRI study of hippocampus and amygdala in patients with current and remitted major depression. Psychiatry Res. 2004;132:141–147. doi: 10.1016/j.pscychresns.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Caetano SC, Kaur S, Brambilla P, Nicoletti M, Hatch JP, Sassi RB, et al. Smaller cingulate volumes in unipolar depressed patients. Biol Psychiatry. 2006;59:702–706. doi: 10.1016/j.biopsych.2005.10.011. [DOI] [PubMed] [Google Scholar]
- Caligiuri MP, Brown GG, Meloy MJ, Eberson S, Niculescu AB, Lohr JB. Striatopallidal regulation of affect in bipolar disorder. J Affect Disord. 2006;91:235–242. doi: 10.1016/j.jad.2006.01.014. [DOI] [PubMed] [Google Scholar]
- Caligiuri MP, Brown GG, Meloy MJ, Eberson SC, Kindermann SS, Frank LR, et al. An fMRI study of affective state and medication on cortical and subcortical brain regions during motor performance in bipolar disorder. Psychiatry Res. 2003;123:171–182. doi: 10.1016/s0925-4927(03)00075-1. [DOI] [PubMed] [Google Scholar]
- Campbell S, Marriott M, Nahmias C, MacQueen GM. Lower hippocampal volume in patients suffering from depression: a meta-analysis. Am J Psychiatry. 2004;161:598–607. doi: 10.1176/appi.ajp.161.4.598. [DOI] [PubMed] [Google Scholar]
- Canli T, Sivers H, Thomason ME, Whitfield-Gabrieli S, Gabrieli JD, Gotlib IH. Brain activation to emotional words in depressed vs healthy subjects. Neuroreport. 2004;15:2585–2588. doi: 10.1097/00001756-200412030-00005. [DOI] [PubMed] [Google Scholar]
- Cannon M, Jones PB, Murray RM. Obstetric complications and schizophrenia: historical and meta-analytic review. Am J Psychiatry. 2002;159:1080–1092. doi: 10.1176/appi.ajp.159.7.1080. [DOI] [PubMed] [Google Scholar]
- Cardinal RN, Parkinson JA, Hall J, Everitt BJ. Emotion and motivation: the role of the amygdala, ventral striatum, and prefrontal cortex. Neurosci Biobehav Rev. 2002;26:321–352. doi: 10.1016/s0149-7634(02)00007-6. [DOI] [PubMed] [Google Scholar]
- Carter CJ. EIF2B and Oligodendrocyte Survival: Where Nature and Nurture Meet in Bipolar Disorder and Schizophrenia? Schizophr Bull. 2007a doi: 10.1093/schbul/sbm007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter CJ. Multiple genes and factors associated with bipolar disorder converge on growth factor and stress activated kinase pathways controlling translation initiation: implications for oligodendrocyte viability. Neurochem Int. 2007b;50:461–490. doi: 10.1016/j.neuint.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cecil KM, DelBello MP, Morey R, Strakowski SM. Frontal lobe differences in bipolar disorder as determined by proton MR spectroscopy. Bipolar Disord. 2002;4:357–365. doi: 10.1034/j.1399-5618.2002.02235.x. [DOI] [PubMed] [Google Scholar]
- Chabriat H, Vahedi K, Iba-Zizen MT, Joutel A, Nibbio A, Nagy TG, et al. Clinical spectrum of CADASIL: a study of 7 families. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Lancet. 1995;346:934–939. doi: 10.1016/s0140-6736(95)91557-5. [DOI] [PubMed] [Google Scholar]
- Chakos MH, Lieberman JA, Alvir J, Bilder R, Ashtari M. Caudate nuclei volumes in schizophrenic patients treated with typical antipsychotics or clozapine. Lancet. 1995;345:456–457. doi: 10.1016/s0140-6736(95)90441-7. [DOI] [PubMed] [Google Scholar]
- Chakos MH, Lieberman JA, Bilder RM, Borenstein M, Lerner G, Bogerts B, et al. Increase in caudate nuclei volumes of first-episode schizophrenic patients taking antipsychotic drugs. Am J Psychiatry. 1994;151:1430–1436. doi: 10.1176/ajp.151.10.1430. [DOI] [PubMed] [Google Scholar]
- Chang K, Adleman NE, Dienes K, Simeonova DI, Menon V, Reiss A. Anomalous prefrontal-subcortical activation in familial pediatric bipolar disorder: a functional magnetic resonance imaging investigation. Arch Gen Psychiatry. 2004;61:781–792. doi: 10.1001/archpsyc.61.8.781. [DOI] [PubMed] [Google Scholar]
- Chang K, Barnea-Goraly N, Karchemskiy A, Simeonova DI, Barnes P, Ketter T, Reiss AL. Cortical magnetic resonance imaging findings in familial pediatric bipolar disorder. Biol Psychiatry. 2005a;58:197–203. doi: 10.1016/j.biopsych.2005.03.039. [DOI] [PubMed] [Google Scholar]
- Chang K, Karchemskiy A, Barnea-Goraly N, Garrett A, Simeonova DI, Reiss A. Reduced amygdalar gray matter volume in familial pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005b;44:565–573. doi: 10.1097/01.chi.0000159948.75136.0d. [DOI] [PubMed] [Google Scholar]
- Chang KD, Wagner C, Garrett A, Howe M, Reiss A. A preliminary functional magnetic resonance imaging study of prefrontal-amygdalar activation changes in adolescents with bipolar depression treated with lamotrigine. Bipolar Disord. 2008;10:426–431. doi: 10.1111/j.1399-5618.2007.00576.x. [DOI] [PubMed] [Google Scholar]
- Chen BK, Sassi R, Axelson D, Hatch JP, Sanches M, Nicoletti M, et al. Cross-sectional study of abnormal amygdala development in adolescents and young adults with bipolar disorder. Biol Psychiatry. 2004;56:399–405. doi: 10.1016/j.biopsych.2004.06.024. [DOI] [PubMed] [Google Scholar]
- Chen CH, Ridler K, Suckling J, Williams S, Fu CH, Merlo-Pich E, Bullmore E. Brain Imaging Correlates of Depressive Symptom Severity and Predictors of Symptom Improvement After Antidepressant Treatment. Biol Psychiatry. 2007a doi: 10.1016/j.biopsych.2006.09.018. [DOI] [PubMed] [Google Scholar]
- Chen CH, Suckling J, Ooi C, Fu CH, Williams SC, Walsh ND, et al. Functional Coupling of the Amygdala in Depressed Patients Treated with Antidepressant Medication. Neuropsychopharmacology. 2007b doi: 10.1038/sj.npp.1301593. [DOI] [PubMed] [Google Scholar]
- Chen PS, McQuoid DR, Payne ME, Steffens DC. White matter and subcortical gray matter lesion volume changes and late-life depression outcome: a 4-year magnetic resonance imaging study. Int Psychogeriatr. 2006;18:445–456. doi: 10.1017/S1041610205002796. [DOI] [PubMed] [Google Scholar]
- Chen X, Wen W, Malhi GS, Ivanovski B, Sachdev PS. Regional gray matter changes in bipolar disorder: a voxel-based morphometric study. Aust N Z J Psychiatry. 2007c;41:327–336. doi: 10.1080/00048670701213229. [DOI] [PubMed] [Google Scholar]
- Chepenik LG, Fredericks C, Papademetris X, Spencer L, Lacadie C, Wang F, et al. Effects of the Brain-Derived Neurotrophic Growth Factor Val66Met Variation on Hippocampus Morphology in Bipolar Disorder. Neuropsychopharmacology. 2008 doi: 10.1038/npp.2008.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu S, Widjaja F, Bates ME, Voelbel GT, Pandina G, Marble J, et al. Anterior cingulate volume in pediatric bipolar disorder and autism. J Affect Disord. 2007 doi: 10.1016/j.jad.2007.04.019. [DOI] [PubMed] [Google Scholar]
- Clark CP, Brown GG, Frank L, Thomas L, Sutherland AN, Gillin JC. Improved anatomic delineation of the antidepressant response to partial sleep deprivation in medial frontal cortex using perfusion-weighted functional MRI. Psychiatry Res. 2006;146:213–222. doi: 10.1016/j.pscychresns.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey CE, Figiel GS, Djang WT, Cress M, Saunders WB, Weiner RD. Leukoencephalopathy in elderly depressed patients referred for ECT. Biol Psychiatry. 1988;24:143–161. doi: 10.1016/0006-3223(88)90270-3. [DOI] [PubMed] [Google Scholar]
- Coffey CE, Figiel GS, Djang WT, Saunders WB, Weiner RD. White matter hyperintensity on magnetic resonance imaging: clinical and neuroanatomic correlates in the depressed elderly. J Neuropsychiatry Clin Neurosci. 1989;1:135–144. doi: 10.1176/jnp.1.2.135. [DOI] [PubMed] [Google Scholar]
- Coffey CE, Wilkinson WE, Weiner RD, Parashos IA, Djang WT, Webb MC, et al. Quantitative cerebral anatomy in depression. A controlled magnetic resonance imaging study. Arch Gen Psychiatry. 1993;50:7–16. doi: 10.1001/archpsyc.1993.01820130009002. [DOI] [PubMed] [Google Scholar]
- Coffman JA, Bornstein RA, Olson SC, Schwarzkopf SB, Nasrallah HA. Cognitive impairment and cerebral structure by MRI in bipolar disorder. Biol Psychiatry. 1990;27:1188–1196. doi: 10.1016/0006-3223(90)90416-y. [DOI] [PubMed] [Google Scholar]
- Cohen RM, Gross M, Nordahl TE, Semple WE, Oren DA, Rosenthal N. Preliminary data on the metabolic brain pattern of patients with winter seasonal affective disorder. Arch Gen Psychiatry. 1992;49:545–552. doi: 10.1001/archpsyc.1992.01820070039006. [DOI] [PubMed] [Google Scholar]
- Cohen RM, Semple WE, Gross M, Nordahl TE, King AC, Pickar D, Post RM. Evidence for common alterations in cerebral glucose metabolism in major affective disorders and schizophrenia. Neuropsychopharmacology. 1989;2:241–254. doi: 10.1016/0893-133x(89)90028-6. [DOI] [PubMed] [Google Scholar]
- Coryell W, Nopoulos P, Drevets W, Wilson T, Andreasen NC. Subgenual prefrontal cortex volumes in major depressive disorder and schizophrenia: diagnostic specificity and prognostic implications. Am J Psychiatry. 2005;162:1706–1712. doi: 10.1176/appi.ajp.162.9.1706. [DOI] [PubMed] [Google Scholar]
- Cotter D, Hudson L, Landau S. Evidence for orbitofrontal pathology in bipolar disorder and major depression, but not in schizophrenia. Bipolar Disord. 2005;7:358–369. doi: 10.1111/j.1399-5618.2005.00230.x. [DOI] [PubMed] [Google Scholar]
- Cotter D, Mackay D, Chana G, Beasley C, Landau S, Everall IP. Reduced neuronal size and glial cell density in area 9 of the dorsolateral prefrontal cortex in subjects with major depressive disorder. Cereb Cortex. 2002;12:386–394. doi: 10.1093/cercor/12.4.386. [DOI] [PubMed] [Google Scholar]
- Cotter D, Mackay D, Landau S, Kerwin R, Everall I. Reduced glial cell density and neuronal size in the anterior cingulate cortex in major depressive disorder. Arch Gen Psychiatry. 2001;58:545–553. doi: 10.1001/archpsyc.58.6.545. [DOI] [PubMed] [Google Scholar]
- Czeh B, Michaelis T, Watanabe T, Frahm J, de Biurrun G, van Kampen M, et al. Stress-induced changes in cerebral metabolites, hippocampal volume, and cell proliferation are prevented by antidepressant treatment with tianeptine. Proc Natl Acad Sci U S A. 2001;98:12796–12801. doi: 10.1073/pnas.211427898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeh B, Muller-Keuker JI, Rygula R, Abumaria N, Hiemke C, Domenici E, Fuchs E. Chronic social stress inhibits cell proliferation in the adult medial prefrontal cortex: hemispheric asymmetry and reversal by fluoxetine treatment. Neuropsychopharmacology. 2007;32:1490–1503. doi: 10.1038/sj.npp.1301275. [DOI] [PubMed] [Google Scholar]
- Dager SR, Friedman SD. Brain imaging and the effects of caffeine and nicotine. Ann Med. 2000;32:592–599. doi: 10.3109/07853890009002029. [DOI] [PubMed] [Google Scholar]
- Dahabra S, Ashton CH, Bahrainian M, Britton PG, Ferrier IN, McAllister VA, et al. Structural and functional abnormalities in elderly patients clinically recovered from early- and late-onset depression. Biol Psychiatry. 1998;44:34–46. doi: 10.1016/s0006-3223(98)00003-1. [DOI] [PubMed] [Google Scholar]
- Damasio AR. The somatic marker hypothesis and the possible functions of the prefrontal cortex. Philos Trans R Soc Lond B Biol Sci. 1996;351:1413–1420. doi: 10.1098/rstb.1996.0125. [DOI] [PubMed] [Google Scholar]
- Dannlowski U, Ohrmann P, Bauer J, Kugel H, Arolt V, Heindel W, et al. Amygdala reactivity to masked negative faces is associated with automatic judgmental bias in major depression: a 3 T fMRI study. J Psychiatry Neurosci. 2007;32:423–429. [PMC free article] [PubMed] [Google Scholar]
- Dannlowski U, Ohrmann P, Bauer J, Kugel H, Baune BT, Hohoff C, et al. Serotonergic genes modulate amygdala activity in major depression. Genes Brain Behav. 2006 doi: 10.1111/j.1601-183X.2006.00297.x. [DOI] [PubMed] [Google Scholar]
- David SP, Murthy NV, Rabiner EA, Munafo MR, Johnstone EC, Jacob R, et al. A functional genetic variation of the serotonin (5-HT) transporter affects 5-HT1A receptor binding in humans. J Neurosci. 2005;25:2586–2590. doi: 10.1523/JNEUROSCI.3769-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ. Anterior cerebral asymmetry and the nature of emotion. Brain Cogn. 1992;20:125–151. doi: 10.1016/0278-2626(92)90065-t. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. Anxiety and affective style: role of prefrontal cortex and amygdala. Biol Psychiatry. 2002;51:68–80. doi: 10.1016/s0006-3223(01)01328-2. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Irwin W. The functional neuroanatomy of emotion and affective style. Trends Cogn Sci. 1999;3:11–21. doi: 10.1016/s1364-6613(98)01265-0. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Irwin W, Anderle MJ, Kalin NH. The neural substrates of affective processing in depressed patients treated with venlafaxine. Am J Psychiatry. 2003;160:64–75. doi: 10.1176/appi.ajp.160.1.64. [DOI] [PubMed] [Google Scholar]
- Davis KA, Kwon A, Cardenas VA, Deicken RF. Decreased cortical gray and cerebral white matter in male patients with familial bipolar I disorder. J Affect Disord. 2004;82:475–485. doi: 10.1016/j.jad.2004.03.010. [DOI] [PubMed] [Google Scholar]
- Davis M, Whalen PJ. The amygdala: vigilance and emotion. Mol Psychiatry. 2001;6:13–34. doi: 10.1038/sj.mp.4000812. [DOI] [PubMed] [Google Scholar]
- de Asis JM, Greenwald BS, Alexopoulos GS, Kiosses DN, Ashtari M, Heo M, Young RC. Frontal signal hyperintensities in mania in old age. Am J Geriatr Psychiatry. 2006;14:598–604. doi: 10.1097/01.JGP.0000200603.70504.d5. [DOI] [PubMed] [Google Scholar]
- de Castro AG, Bajbouj M, Schlattmann P, Lemke H, Heuser I, Neu P. Cerebrovascular reactivity in depressed patients without vascular risk factors. J Psychiatr Res. 2006 doi: 10.1016/j.jpsychires.2006.10.001. [DOI] [PubMed] [Google Scholar]
- de Groot JC, de Leeuw FE, Oudkerk M, Hofman A, Jolles J, Breteler MM. Cerebral white matter lesions and depressive symptoms in elderly adults. Arch Gen Psychiatry. 2000;57:1071–1076. doi: 10.1001/archpsyc.57.11.1071. [DOI] [PubMed] [Google Scholar]
- Deicken RF, Reus VI, Manfredi L, Wolkowitz OM. MRI deep white matter hyperintensity in a psychiatric population. Biol Psychiatry. 1991;29:918–922. doi: 10.1016/0006-3223(91)90058-t. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Zimmerman ME, Mills NP, Getz GE, Strakowski SM. Magnetic resonance imaging analysis of amygdala and other subcortical brain regions in adolescents with bipolar disorder. Bipolar Disord. 2004;6:43–52. doi: 10.1046/j.1399-5618.2003.00087.x. [DOI] [PubMed] [Google Scholar]
- DeLong MR, Wichmann T. Circuits and circuit disorders of the basal ganglia. Arch Neurol. 2007;64:20–24. doi: 10.1001/archneur.64.1.20. [DOI] [PubMed] [Google Scholar]
- Desmond DW, Moroney JT, Lynch T, Chan S, Chin SS, Mohr JP. The natural history of CADASIL: a pooled analysis of previously published cases. Stroke. 1999;30:1230–1233. doi: 10.1161/01.str.30.6.1230. [DOI] [PubMed] [Google Scholar]
- Devinsky O, Morrell MJ, Vogt BA. Contributions of anterior cingulate cortex to behaviour. Brain. 1995;118 (Pt 1):279–306. doi: 10.1093/brain/118.1.279. [DOI] [PubMed] [Google Scholar]
- Dickstein DP, Milham MP, Nugent AC, Drevets WC, Charney DS, Pine DS, Leibenluft E. Frontotemporal alterations in pediatric bipolar disorder: results of a voxel-based morphometry study. Arch Gen Psychiatry. 2005;62:734–741. doi: 10.1001/archpsyc.62.7.734. [DOI] [PubMed] [Google Scholar]
- Dolan RJ, Poynton AM, Bridges PK, Trimble MR. Altered magnetic resonance white-matter T1 values in patients with affective disorder. Br J Psychiatry. 1990;157:107–110. doi: 10.1192/bjp.157.1.107. [DOI] [PubMed] [Google Scholar]
- Doris A, Belton E, Ebmeier KP, Glabus MF, Marshall I. Reduction of cingulate gray matter density in poor outcome bipolar illness. Psychiatry Res. 2004;130:153–159. doi: 10.1016/j.pscychresns.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Douaud G, Gaura V, Ribeiro MJ, Lethimonnier F, Maroy R, Verny C, et al. Distribution of grey matter atrophy in Huntington’s disease patients: a combined ROI-based and voxel-based morphometric study. Neuroimage. 2006;32:1562–1575. doi: 10.1016/j.neuroimage.2006.05.057. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Functional neuroimaging studies of depression: the anatomy of melancholia. Annu Rev Med. 1998;49:341–361. doi: 10.1146/annurev.med.49.1.341. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Functional anatomical abnormalities in limbic and prefrontal cortical structures in major depression. Prog Brain Res. 2000a;126:413–431. doi: 10.1016/S0079-6123(00)26027-5. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Neuroimaging studies of mood disorders. Biol Psychiatry. 2000b;48:813–829. doi: 10.1016/s0006-3223(00)01020-9. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Neuroimaging and neuropathological studies of depression: implications for the cognitive-emotional features of mood disorders. Curr Opin Neurobiol. 2001;11:240–249. doi: 10.1016/s0959-4388(00)00203-8. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Orbitofrontal Cortex Function and Structure in Depression. Ann N Y Acad Sci. 2007 doi: 10.1196/annals.1401.029. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Bogers W, Raichle ME. Functional anatomical correlates of antidepressant drug treatment assessed using PET measures of regional glucose metabolism. Eur Neuropsychopharmacol. 2002a;12:527–544. doi: 10.1016/s0924-977x(02)00102-5. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Price JL, Bardgett ME, Reich T, Todd RD, Raichle ME. Glucose metabolism in the amygdala in depression: relationship to diagnostic subtype and plasma cortisol levels. Pharmacol Biochem Behav. 2002b;71:431–447. doi: 10.1016/s0091-3057(01)00687-6. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Price JL, Simpson JR, Jr, Todd RD, Reich T, Vannier M, Raichle ME. Subgenual prefrontal cortex abnormalities in mood disorders. Nature. 1997;386:824–827. doi: 10.1038/386824a0. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Savitz J, Trimble M. The subgenual anterior cingulate cortex in mood disorders. CNS Spectr. 2008;13:663–681. doi: 10.1017/s1092852900013754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drevets WC, Videen TO, Price JL, Preskorn SH, Carmichael ST, Raichle ME. A functional anatomical study of unipolar depression. J Neurosci. 1992;12:3628–3641. doi: 10.1523/JNEUROSCI.12-09-03628.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudek FE, Sutula TP. Epileptogenesis in the dentate gyrus: a critical perspective. Prog Brain Res. 2007;163:755–773. doi: 10.1016/S0079-6123(07)63041-6. [DOI] [PubMed] [Google Scholar]
- Duffy A. Does bipolar disorder exist in children? A selected review. Can J Psychiatry. 2007;52:409–417. doi: 10.1177/070674370705200702. [DOI] [PubMed] [Google Scholar]
- Dufouil C, de Kersaint-Gilly A, Besancon V, Levy C, Auffray E, Brunnereau L, et al. Longitudinal study of blood pressure and white matter hyperintensities: the EVA MRI Cohort. Neurology. 2001;56:921–926. doi: 10.1212/wnl.56.7.921. [DOI] [PubMed] [Google Scholar]
- Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006;59:1116–1127. doi: 10.1016/j.biopsych.2006.02.013. [DOI] [PubMed] [Google Scholar]
- Dunn RT, Kimbrell TA, Ketter TA, Frye MA, Willis MW, Luckenbaugh DA, Post RM. Principal components of the Beck Depression Inventory and regional cerebral metabolism in unipolar and bipolar depression. Biol Psychiatry. 2002;51:387–399. doi: 10.1016/s0006-3223(01)01244-6. [DOI] [PubMed] [Google Scholar]
- Dupont RM, Butters N, Schafer K, Wilson T, Hesselink J, Gillin JC. Diagnostic specificity of focal white matter abnormalities in bipolar and unipolar mood disorder. Biol Psychiatry. 1995a;38:482–486. doi: 10.1016/0006-3223(95)00100-u. [DOI] [PubMed] [Google Scholar]
- Dupont RM, Jernigan TL, Butters N, Delis D, Hesselink JR, Heindel W, Gillin JC. Subcortical abnormalities detected in bipolar affective disorder using magnetic resonance imaging. Clinical and neuropsychological significance. Arch Gen Psychiatry. 1990;47:55–59. doi: 10.1001/archpsyc.1990.01810130057008. [DOI] [PubMed] [Google Scholar]
- Dupont RM, Jernigan TL, Heindel W, Butters N, Shafer K, Wilson T, et al. Magnetic resonance imaging and mood disorders. Localization of white matter and other subcortical abnormalities. Arch Gen Psychiatry. 1995b;52:747–755. doi: 10.1001/archpsyc.1995.03950210041009. [DOI] [PubMed] [Google Scholar]
- Dwivedi Y, Rizavi HS, Conley RR, Roberts RC, Tamminga CA, Pandey GN. Altered gene expression of brain-derived neurotrophic factor and receptor tyrosine kinase B in postmortem brain of suicide subjects. Arch Gen Psychiatry. 2003;60:804–815. doi: 10.1001/archpsyc.60.8.804. [DOI] [PubMed] [Google Scholar]
- Ebstein RP. The molecular genetic architecture of human personality: beyond self-report questionnaires. Mol Psychiatry. 2006;11:427–445. doi: 10.1038/sj.mp.4001814. [DOI] [PubMed] [Google Scholar]
- El-Badri SM, Cousins DA, Parker S, Ashton HC, McAllister VL, Ferrier IN, Moore PB. Magnetic resonance imaging abnormalities in young euthymic patients with bipolar affective disorder. Br J Psychiatry. 2006;189:81–82. doi: 10.1192/bjp.bp.105.011098. [DOI] [PubMed] [Google Scholar]
- Elliott R, Ogilvie A, Rubinsztein JS, Calderon G, Dolan RJ, Sahakian BJ. Abnormal ventral frontal response during performance of an affective go/no go task in patients with mania. Biol Psychiatry. 2004;55:1163–1170. doi: 10.1016/j.biopsych.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Elliott R, Rubinsztein JS, Sahakian BJ, Dolan RJ. The neural basis of mood-congruent processing biases in depression. Arch Gen Psychiatry. 2002;59:597–604. doi: 10.1001/archpsyc.59.7.597. [DOI] [PubMed] [Google Scholar]
- Emdad R, Bonekamp D, Sondergaard HP, Bjorklund T, Agartz I, Ingvar M, Theorell T. Morphometric and psychometric comparisons between non-substance-abusing patients with posttraumatic stress disorder and normal controls. Psychother Psychosom. 2006;75:122–132. doi: 10.1159/000090897. [DOI] [PubMed] [Google Scholar]
- Epstein J, Pan H, Kocsis JH, Yang Y, Butler T, Chusid J, et al. Lack of ventral striatal response to positive stimuli in depressed versus normal subjects. Am J Psychiatry. 2006;163:1784–1790. doi: 10.1176/ajp.2006.163.10.1784. [DOI] [PubMed] [Google Scholar]
- Erickson K, Drevets WC, Clark L, Cannon DM, Bain EE, Zarate CA, Jr, et al. Mood-congruent bias in affective go/no-go performance of unmedicated patients with major depressive disorder. Am J Psychiatry. 2005;162:2171–2173. doi: 10.1176/appi.ajp.162.11.2171. [DOI] [PubMed] [Google Scholar]
- Evans L, Akiskal HS, Keck PE, Jr, McElroy SL, Sadovnick AD, Remick RA, Kelsoe JR. Familiality of temperament in bipolar disorder: support for a genetic spectrum. J Affect Disord. 2005;85:153–168. doi: 10.1016/j.jad.2003.10.015. [DOI] [PubMed] [Google Scholar]
- Fahim C, Stip E, Mancini-Marie A, Potvin S, Malaspina D. Orbitofrontal dysfunction in a monozygotic twin discordant for postpartum affective psychosis: a functional magnetic resonance imaging study. Bipolar Disord. 2007;9:541–545. doi: 10.1111/j.1399-5618.2007.00404.x. [DOI] [PubMed] [Google Scholar]
- Fales CL, Barch DM, Rundle MM, Mintun MA, Mathews J, Snyder AZ, Sheline YI. Antidepressant treatment normalizes hypoactivity in dorsolateral prefrontal cortex during emotional interference processing in major depression. J Affect Disord. 2008a doi: 10.1016/j.jad.2008.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fales CL, Barch DM, Rundle MM, Mintun MA, Snyder AZ, Cohen JD, et al. Altered emotional interference processing in affective and cognitive-control brain circuitry in major depression. Biol Psychiatry. 2008b;63:377–384. doi: 10.1016/j.biopsych.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferry AT, Ongur D, An X, Price JL. Prefrontal cortical projections to the striatum in macaque monkeys: evidence for an organization related to prefrontal networks. J Comp Neurol. 2000;425:447–470. doi: 10.1002/1096-9861(20000925)425:3<447::aid-cne9>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Figiel GS, Krishnan KR, Rao VP, Doraiswamy M, Ellinwood EH, Jr, Nemeroff CB, et al. Subcortical hyperintensities on brain magnetic resonance imaging: a comparison of normal and bipolar subjects. J Neuropsychiatry Clin Neurosci. 1991;3:18–22. doi: 10.1176/jnp.3.1.18. [DOI] [PubMed] [Google Scholar]
- Firbank MJ, Lloyd AJ, Ferrier N, O’Brien JT. A volumetric study of MRI signal hyperintensities in late-life depression. Am J Geriatr Psychiatry. 2004;12:606–612. doi: 10.1176/appi.ajgp.12.6.606. [DOI] [PubMed] [Google Scholar]
- Firbank MJ, O’Brien JT, Pakrasi S, Pantoni L, Simoni M, Erkinjuntti T, et al. White matter hyperintensities and depression--preliminary results from the LADIS study. Int J Geriatr Psychiatry. 2005;20:674–679. doi: 10.1002/gps.1342. [DOI] [PubMed] [Google Scholar]
- Flor-Henry P. On certain aspects of the localization of the cerebral systems regulating and determining emotion. Biol Psychiatry. 1979;14:677–698. [PubMed] [Google Scholar]
- Fornito A, Malhi GS, Lagopoulos J, Ivanovski B, Wood SJ, Velakoulis D, et al. In vivo evidence for early neurodevelopmental anomaly of the anterior cingulate cortex in bipolar disorder. Acta Psychiatr Scand. 2007;116:467–472. doi: 10.1111/j.1600-0447.2007.01069.x. [DOI] [PubMed] [Google Scholar]
- Frangou S. The Maudsley Bipolar Disorder Project. Epilepsia. 2005;46(Suppl 4):19–25. doi: 10.1111/j.1528-1167.2005.463005.x. [DOI] [PubMed] [Google Scholar]
- Frank LM, Brown EN, Stanley GB. Hippocampal and cortical place cell plasticity: implications for episodic memory. Hippocampus. 2006;16:775–784. doi: 10.1002/hipo.20200. [DOI] [PubMed] [Google Scholar]
- Frazier JA, Breeze JL, Papadimitriou G, Kennedy DN, Hodge SM, Moore CM, et al. White matter abnormalities in children with and at risk for bipolar disorder. Bipolar Disord. 2007;9:799–809. doi: 10.1111/j.1399-5618.2007.00482.x. [DOI] [PubMed] [Google Scholar]
- Frazier JA, Chiu S, Breeze JL, Makris N, Lange N, Kennedy DN, et al. Structural brain magnetic resonance imaging of limbic and thalamic volumes in pediatric bipolar disorder. Am J Psychiatry. 2005;162:1256–1265. doi: 10.1176/appi.ajp.162.7.1256. [DOI] [PubMed] [Google Scholar]
- Frazier JA, Giedd JN, Kaysen D, Albus K, Hamburger S, Alaghband-Rad J, et al. Childhood-onset schizophrenia: brain MRI rescan after 2 years of clozapine maintenance treatment. Am J Psychiatry. 1996;153:564–566. doi: 10.1176/ajp.153.4.564. [DOI] [PubMed] [Google Scholar]
- Frodl T, Meisenzahl EM, Zetzsche T, Born C, Groll C, Jager M, et al. Hippocampal changes in patients with a first episode of major depression. Am J Psychiatry. 2002;159:1112–1118. doi: 10.1176/appi.ajp.159.7.1112. [DOI] [PubMed] [Google Scholar]
- Frodl T, Meisenzahl EM, Zetzsche T, Hohne T, Banac S, Schorr C, et al. Hippocampal and amygdala changes in patients with major depressive disorder and healthy controls during a 1-year follow-up. J Clin Psychiatry. 2004;65:492–499. doi: 10.4088/jcp.v65n0407. [DOI] [PubMed] [Google Scholar]
- Frodl T, Schaub A, Banac S, Charypar M, Jager M, Kummler P, et al. Reduced hippocampal volume correlates with executive dysfunctioning in major depression. J Psychiatry Neurosci. 2006;31:316–323. [PMC free article] [PubMed] [Google Scholar]
- Frodl T, Schule C, Schmitt G, Born C, Baghai T, Zill P, et al. Association of the brain-derived neurotrophic factor Val66Met polymorphism with reduced hippocampal volumes in major depression. Arch Gen Psychiatry. 2007;64:410–416. doi: 10.1001/archpsyc.64.4.410. [DOI] [PubMed] [Google Scholar]
- Fu CH, Williams SC, Cleare AJ, Brammer MJ, Walsh ND, Kim J, et al. Attenuation of the neural response to sad faces in major depression by antidepressant treatment: a prospective, event-related functional magnetic resonance imaging study. Arch Gen Psychiatry. 2004;61:877–889. doi: 10.1001/archpsyc.61.9.877. [DOI] [PubMed] [Google Scholar]
- Fujikawa T, Yamawaki S, Touhouda Y. Incidence of silent cerebral infarction in patients with major depression. Stroke. 1993;24:1631–1634. doi: 10.1161/01.str.24.11.1631. [DOI] [PubMed] [Google Scholar]
- Gaspar P, Cases O, Maroteaux L. The developmental role of serotonin: news from mouse molecular genetics. Nat Rev Neurosci. 2003;4:1002–1012. doi: 10.1038/nrn1256. [DOI] [PubMed] [Google Scholar]
- Gazzaniga MS. Forty-five years of split-brain research and still going strong. Nat Rev Neurosci. 2005;6:653–659. doi: 10.1038/nrn1723. [DOI] [PubMed] [Google Scholar]
- Geschwind N. Disconnexion syndromes in animals and man. II. Brain. 1965;88:585–644. doi: 10.1093/brain/88.3.585. [DOI] [PubMed] [Google Scholar]
- Gilbertson MW, Shenton ME, Ciszewski A, Kasai K, Lasko NB, Orr SP, Pitman RK. Smaller hippocampal volume predicts pathologic vulnerability to psychological trauma. Nat Neurosci. 2002;5:1242–1247. doi: 10.1038/nn958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliani NR, Calhoun VD, Pearlson GD, Francis A, Buchanan RW. Voxel-based morphometry versus region of interest: a comparison of two methods for analyzing gray matter differences in schizophrenia. Schizophr Res. 2005;74:135–147. doi: 10.1016/j.schres.2004.08.019. [DOI] [PubMed] [Google Scholar]
- Glahn DC, Bearden CE, Barguil M, Barrett J, Reichenberg A, Bowden CL, et al. The Neurocognitive Signature of Psychotic Bipolar Disorder. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Glenthoj A, Glenthoj BY, Mackeprang T, Pagsberg AK, Hemmingsen RP, Jernigan TL, Baare WF. Basal ganglia volumes in drug-naive first-episode schizophrenia patients before and after short-term treatment with either a typical or an atypical antipsychotic drug. Psychiatry Res. 2007;154:199–208. doi: 10.1016/j.pscychresns.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Gloor P, Olivier A, Quesney LF, Andermann F, Horowitz S. The role of the limbic system in experiential phenomena of temporal lobe epilepsy. Ann Neurol. 1982;12:129–144. doi: 10.1002/ana.410120203. [DOI] [PubMed] [Google Scholar]
- Godin O, Dufouil C, Maillard P, Delcroix N, Mazoyer B, Crivello F, et al. White Matter Lesions as a Predictor of Depression in the Elderly: The 3C-Dijon Study. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Goldapple K, Segal Z, Garson C, Lau M, Bieling P, Kennedy S, Mayberg H. Modulation of cortical-limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Arch Gen Psychiatry. 2004;61:34–41. doi: 10.1001/archpsyc.61.1.34. [DOI] [PubMed] [Google Scholar]
- Goldstein K. The Organism. New York: American Books; 1939. [Google Scholar]
- Gotlib IH, Sivers H, Gabrieli JD, Whitfield-Gabrieli S, Goldin P, Minor KL, Canli T. Subgenual anterior cingulate activation to valenced emotional stimuli in major depression. Neuroreport. 2005;16:1731–1734. doi: 10.1097/01.wnr.0000183901.70030.82. [DOI] [PubMed] [Google Scholar]
- Grafman J, Schwab K, Warden D, Pridgen A, Brown HR, Salazar AM. Frontal lobe injuries, violence, and aggression: a report of the Vietnam Head Injury Study. Neurology. 1996;46:1231–1238. doi: 10.1212/wnl.46.5.1231. [DOI] [PubMed] [Google Scholar]
- Greenwald BS, Kramer-Ginsberg E, Bogerts B, Ashtari M, Aupperle P, Wu H, et al. Qualitative magnetic resonance imaging findings in geriatric depression. Possible link between later-onset depression and Alzheimer’s disease? Psychol Med. 1997;27:421–431. doi: 10.1017/s0033291796004576. [DOI] [PubMed] [Google Scholar]
- Greenwald BS, Kramer-Ginsberg E, Krishnan KR, Ashtari M, Auerbach C, Patel M. Neuroanatomic localization of magnetic resonance imaging signal hyperintensities in geriatric depression. Stroke. 1998;29:613–617. doi: 10.1161/01.str.29.3.613. [DOI] [PubMed] [Google Scholar]
- Greenwald BS, Kramer-Ginsberg E, Krishnan RR, Ashtari M, Aupperle PM, Patel M. MRI signal hyperintensities in geriatric depression. Am J Psychiatry. 1996;153:1212–1215. doi: 10.1176/ajp.153.9.1212. [DOI] [PubMed] [Google Scholar]
- Grimm S, Beck J, Schuepbach D, Hell D, Boesiger P, Bermpohl F, et al. Imbalance between Left and Right Dorsolateral Prefrontal Cortex in Major Depression Is Linked to Negative Emotional Judgment: An fMRI Study in Severe Major Depressive Disorder. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2007.05.033. [DOI] [PubMed] [Google Scholar]
- Gronli J, Bramham C, Murison R, Kanhema T, Fiske E, Bjorvatn B, et al. Chronic mild stress inhibits BDNF protein expression and CREB activation in the dentate gyrus but not in the hippocampus proper. Pharmacol Biochem Behav. 2006;85:842–849. doi: 10.1016/j.pbb.2006.11.021. [DOI] [PubMed] [Google Scholar]
- Gruber SA, Rogowska J, Yurgelun-Todd DA. Decreased activation of the anterior cingulate in bipolar patients: an fMRI study. J Affect Disord. 2004;82:191–201. doi: 10.1016/j.jad.2003.10.010. [DOI] [PubMed] [Google Scholar]
- Gulseren S, Gurcan M, Gulseren L, Gelal F, Erol A. T2 hyperintensities in bipolar patients and their healthy siblings. Arch Med Res. 2006;37:79–85. doi: 10.1016/j.arcmed.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Gunstad J, Cohen RA, Tate DF, Paul RH, Poppas A, Hoth K, et al. Blood pressure variability and white matter hyperintensities in older adults with cardiovascular disease. Blood Press. 2005;14:353–358. doi: 10.1080/08037050500364117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gur RE, Maany V, Mozley PD, Swanson C, Bilker W, Gur RC. Subcortical MRI volumes in neuroleptic-naive and treated patients with schizophrenia. Am J Psychiatry. 1998;155:1711–1717. doi: 10.1176/ajp.155.12.1711. [DOI] [PubMed] [Google Scholar]
- Gustafson DR, Steen B, Skoog I. Body mass index and white matter lesions in elderly women. An 18-year longitudinal study. Int Psychogeriatr. 2004;16:327–336. doi: 10.1017/s1041610204000353. [DOI] [PubMed] [Google Scholar]
- Guze BH, Szuba MP. Leukoencephalopathy and major depression: a preliminary report. Psychiatry Res. 1992;45:169–175. doi: 10.1016/0925-4927(92)90024-x. [DOI] [PubMed] [Google Scholar]
- Hajek T, Kozeny J, Kopecek M, Alda M, Hoschl C. Reduced subgenual cingulate volumes in mood disorders: a meta-analysis. J Psychiatry Neurosci. 2008;33:91–99. [PMC free article] [PubMed] [Google Scholar]
- Hakak Y, Walker JR, Li C, Wong WH, Davis KL, Buxbaum JD, et al. Genome-wide expression analysis reveals dysregulation of myelination-related genes in chronic schizophrenia. Proc Natl Acad Sci U S A. 2001;98:4746–4751. doi: 10.1073/pnas.081071198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haldane M, Jogia J, Cobb A, Kozuch E, Kumari V, Frangou S. Changes in brain activation during working memory and facial recognition tasks in patients with bipolar disorder with Lamotrigine monotherapy. Eur Neuropsychopharmacol. 2007 doi: 10.1016/j.euroneuro.2007.05.009. [DOI] [PubMed] [Google Scholar]
- Hamakawa H, Kato T, Murashita J, Kato N. Quantitative proton magnetic resonance spectroscopy of the basal ganglia in patients with affective disorders. Eur Arch Psychiatry Clin Neurosci. 1998;248:53–58. doi: 10.1007/s004060050017. [DOI] [PubMed] [Google Scholar]
- Hamidi M, Drevets WC, Price JL. Glial reduction in amygdala in major depressive disorder is due to oligodendrocytes. Biol Psychiatry. 2004;55:563–569. doi: 10.1016/j.biopsych.2003.11.006. [DOI] [PubMed] [Google Scholar]
- Hamilton JP, Gotlib IH. Neural Substrates of Increased Memory Sensitivity for Negative Stimuli in Major Depression. Biol Psychiatry. 2008 doi: 10.1016/j.biopsych.2007.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannestad J, Taylor WD, McQuoid DR, Payne ME, Krishnan KR, Steffens DC, Macfall JR. White matter lesion volumes and caudate volumes in late-life depression. Int J Geriatr Psychiatry. 2006;21:1193–1198. doi: 10.1002/gps.1640. [DOI] [PubMed] [Google Scholar]
- Hao Y, Creson T, Zhang L, Li P, Du F, Yuan P, et al. Mood stabilizer valproate promotes ERK pathway-dependent cortical neuronal growth and neurogenesis. J Neurosci. 2004;24:6590–6599. doi: 10.1523/JNEUROSCI.5747-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariri AR, Mattay VS, Tessitore A, Kolachana B, Fera F, Goldman D, et al. Serotonin transporter genetic variation and the response of the human amygdala. Science. 2002;297:400–403. doi: 10.1126/science.1071829. [DOI] [PubMed] [Google Scholar]
- Harmer CJ, Mackay CE, Reid CB, Cowen PJ, Goodwin GM. Antidepressant drug treatment modifies the neural processing of nonconscious threat cues. Biol Psychiatry. 2006;59:816–820. doi: 10.1016/j.biopsych.2005.10.015. [DOI] [PubMed] [Google Scholar]
- Harvey BH. Is major depressive disorder a metabolic encephalopathy? Hum Psychopharmacol. 2008 doi: 10.1002/hup.946. [DOI] [PubMed] [Google Scholar]
- Harvey I, Persaud R, Ron MA, Baker G, Murray RM. Volumetric MRI measurements in bipolars compared with schizophrenics and healthy controls. Psychol Med. 1994;24:689–699. doi: 10.1017/s0033291700027847. [DOI] [PubMed] [Google Scholar]
- Harvey PO, Fossati P, Pochon JB, Levy R, Lebastard G, Lehericy S, et al. Cognitive control and brain resources in major depression: an fMRI study using the n-back task. Neuroimage. 2005;26:860–869. doi: 10.1016/j.neuroimage.2005.02.048. [DOI] [PubMed] [Google Scholar]
- Hasler G, Fromm S, Alvarez RP, Luckenbaugh DA, Drevets WC, Grillon C. Cerebral blood flow in immediate and sustained anxiety. J Neurosci. 2007;27:6313–6319. doi: 10.1523/JNEUROSCI.5369-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler G, Fromm S, Carlson PJ, Luckenbaugh DA, Waldeck T, Geraci M, et al. Neural response to catecholamine depletion in unmedicated subjects with major depressive disorder in remission and healthy subjects. Arch Gen Psychiatry. 2008;65:521–531. doi: 10.1001/archpsyc.65.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastings RS, Parsey RV, Oquendo MA, Arango V, Mann JJ. Volumetric analysis of the prefrontal cortex, amygdala, and hippocampus in major depression. Neuropsychopharmacology. 2004;29:952–959. doi: 10.1038/sj.npp.1300371. [DOI] [PubMed] [Google Scholar]
- Hauser P, Matochik J, Altshuler LL, Denicoff KD, Conrad A, Li X, Post RM. MRI-based measurements of temporal lobe and ventricular structures in patients with bipolar I and bipolar II disorders. J Affect Disord. 2000;60:25–32. doi: 10.1016/s0165-0327(99)00154-8. [DOI] [PubMed] [Google Scholar]
- Haznedar MM, Roversi F, Pallanti S, Baldini-Rossi N, Schnur DB, Licalzi EM, et al. Fronto-thalamo-striatal gray and white matter volumes and anisotropy of their connections in bipolar spectrum illnesses. Biol Psychiatry. 2005;57:733–742. doi: 10.1016/j.biopsych.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Heiden A, Kettenbach J, Fischer P, Schein B, Ba-Ssalamah A, Frey R, et al. White matter hyperintensities and chronicity of depression. J Psychiatr Res. 2005;39:285–293. doi: 10.1016/j.jpsychires.2004.07.004. [DOI] [PubMed] [Google Scholar]
- Heinz A, Braus DF, Smolka MN, Wrase J, Puls I, Hermann D, et al. Amygdala-prefrontal coupling depends on a genetic variation of the serotonin transporter. Nat Neurosci. 2005;8:20–21. doi: 10.1038/nn1366. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Kuhn JW, Prescott CA, Kendler KS. The impact of generalized anxiety disorder and stressful life events on risk for major depressive episodes. Psychol Med. 2006;36:789–795. doi: 10.1017/S0033291706007367. [DOI] [PubMed] [Google Scholar]
- Hickie I, Naismith S, Ward PB, Turner K, Scott E, Mitchell P, et al. Reduced hippocampal volumes and memory loss in patients with early- and late-onset depression. Br J Psychiatry. 2005;186:197–202. doi: 10.1192/bjp.186.3.197. [DOI] [PubMed] [Google Scholar]
- Hickie I, Scott E, Mitchell P, Wilhelm K, Austin MP, Bennett B. Subcortical hyperintensities on magnetic resonance imaging: clinical correlates and prognostic significance in patients with severe depression. Biol Psychiatry. 1995;37:151–160. doi: 10.1016/0006-3223(94)00174-2. [DOI] [PubMed] [Google Scholar]
- Hickie IB, Naismith SL, Ward PB, Scott EM, Mitchell PB, Schofield PR, et al. Serotonin transporter gene status predicts caudate nucleus but not amygdala or hippocampal volumes in older persons with major depression. J Affect Disord. 2006 doi: 10.1016/j.jad.2006.07.010. [DOI] [PubMed] [Google Scholar]
- Hirayasu Y, Shenton ME, Salisbury DF, Dickey CC, Fischer IA, Mazzoni P, et al. Lower left temporal lobe MRI volumes in patients with first-episode schizophrenia compared with psychotic patients with first-episode affective disorder and normal subjects. Am J Psychiatry. 1998;155:1384–1391. doi: 10.1176/ajp.155.10.1384. [DOI] [PubMed] [Google Scholar]
- Hirayasu Y, Shenton ME, Salisbury DF, Kwon JS, Wible CG, Fischer IA, et al. Subgenual cingulate cortex volume in first-episode psychosis. Am J Psychiatry. 1999a;156:1091–1093. doi: 10.1176/ajp.156.7.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirayasu Y, Shenton ME, Salisbury DF, Kwon JS, Wible CG, Fischer IA, et al. Subgenual cingulate cortex volume in first-episode psychosis. Am J Psychiatry. 1999b;156:1091–1093. doi: 10.1176/ajp.156.7.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho BC, Milev P, O’Leary DS, Librant A, Andreasen NC, Wassink TH. Cognitive and magnetic resonance imaging brain morphometric correlates of brain-derived neurotrophic factor Val66Met gene polymorphism in patients with schizophrenia and healthy volunteers. Arch Gen Psychiatry. 2006;63:731–740. doi: 10.1001/archpsyc.63.7.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holthoff VA, Beuthien-Baumann B, Zundorf G, Triemer A, Ludecke S, Winiecki P, et al. Changes in brain metabolism associated with remission in unipolar major depression. Acta Psychiatr Scand. 2004;110:184–194. doi: 10.1111/j.1600-0447.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- Houenou J, Wessa M, Douaud G, Leboyer M, Chanraud S, Perrin M, et al. Increased white matter connectivity in euthymic bipolar patients: diffusion tensor tractography between the subgenual cingulate and the amygdalo-hippocampal complex. Mol Psychiatry. 2007 doi: 10.1038/sj.mp.4002010. [DOI] [PubMed] [Google Scholar]
- Howard R, Beats B, Forstl H, Graves P, Bingham J, Levy R. White matter changes in late onset depression: A magnetic resonance imaging study. Int J Geriatr Psychiatry. 1993;8:183–185. [Google Scholar]
- Hurwitz TA, Clark C, Murphy E, Klonoff H, Martin WR, Pate BD. Regional cerebral glucose metabolism in major depressive disorder. Can J Psychiatry. 1990;35:684–688. doi: 10.1177/070674379003500807. [DOI] [PubMed] [Google Scholar]
- Husain MM, McDonald WM, Doraiswamy PM, Figiel GS, Na C, Escalona PR, et al. A magnetic resonance imaging study of putamen nuclei in major depression. Psychiatry Res. 1991;40:95–99. doi: 10.1016/0925-4927(91)90001-7. [DOI] [PubMed] [Google Scholar]
- Hwang J, Lyoo IK, Dager SR, Friedman SD, Oh JS, Lee JY, et al. Basal ganglia shape alterations in bipolar disorder. Am J Psychiatry. 2006;163:276–285. doi: 10.1176/appi.ajp.163.2.276. [DOI] [PubMed] [Google Scholar]
- Iidaka T, Nakajima T, Kawamoto K, Fukuda H, Suzuki Y, Maehara T, Shiraishi H. Signal hyperintensities on brain magnetic resonance imaging in elderly depressed patients. Eur Neurol. 1996;36:293–299. doi: 10.1159/000117275. [DOI] [PubMed] [Google Scholar]
- Inagaki M, Matsuoka Y, Sugahara Y, Nakano T, Akechi T, Fujimori M, et al. Hippocampal volume and first major depressive episode after cancer diagnosis in breast cancer survivors. Am J Psychiatry. 2004;161:2263–2270. doi: 10.1176/appi.ajp.161.12.2263. [DOI] [PubMed] [Google Scholar]
- Iosifescu DV, Renshaw PF, Lyoo IK, Lee HK, Perlis RH, Papakostas GI, et al. Brain white-matter hyperintensities and treatment outcome in major depressive disorder. Br J Psychiatry. 2006;188:180–185. doi: 10.1192/bjp.188.2.180. [DOI] [PubMed] [Google Scholar]
- Irwin W, Anderle MJ, Abercrombie HC, Schaefer SM, Kalin NH, Davidson RJ. Amygdalar interhemispheric functional connectivity differs between the non-depressed and depressed human brain. Neuroimage. 2004;21:674–686. doi: 10.1016/j.neuroimage.2003.09.057. [DOI] [PubMed] [Google Scholar]
- Jacobsen JP, Mork A. Chronic corticosterone decreases brain-derived neurotrophic factor (BDNF) mRNA and protein in the hippocampus, but not in the frontal cortex, of the rat. Brain Res. 2006;1110:221–225. doi: 10.1016/j.brainres.2006.06.077. [DOI] [PubMed] [Google Scholar]
- Jacobson L, Sapolsky R. The role of the hippocampus in feedback regulation of the hypothalamic-pituitary-adrenocortical axis. Endocrine Reviews. 1991;12:118–134. doi: 10.1210/edrv-12-2-118. [DOI] [PubMed] [Google Scholar]
- Janssen J, Hulshoff Pol HE, de Leeuw FE, Schnack HS, Lampe IK, Kok RM, et al. Hippocampal volume and subcortical white matter lesions in late-life depression: comparison of early- and late-onset depression. J Neurol Neurosurg Psychiatry. 2007 doi: 10.1136/jnnp.2006.098087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen J, Hulshoff Pol HE, Lampe IK, Schnack HG, de Leeuw FE, Kahn RS, Heeren TJ. Hippocampal changes and white matter lesions in early-onset depression. Biol Psychiatry. 2004;56:825–831. doi: 10.1016/j.biopsych.2004.09.011. [DOI] [PubMed] [Google Scholar]
- Jernigan TL, Zisook S, Heaton RK, Moranville JT, Hesselink JR, Braff DL. Magnetic resonance imaging abnormalities in lenticular nuclei and cerebral cortex in schizophrenia. Arch Gen Psychiatry. 1991;48:881–890. doi: 10.1001/archpsyc.1991.01810340013002. [DOI] [PubMed] [Google Scholar]
- Job DE, Whalley HC, McConnell S, Glabus M, Johnstone EC, Lawrie SM. Structural gray matter differences between first-episode schizophrenics and normal controls using voxel-based morphometry. Neuroimage. 2002;17:880–889. [PubMed] [Google Scholar]
- Johnson SL. Life events in bipolar disorder: towards more specific models. Clin Psychol Rev. 2005;25:1008–1027. doi: 10.1016/j.cpr.2005.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF, Anstey KJ, Christensen H, de Plater G, Kumar R, Wen W, Sachdev P. MRI hyperintensities and depressive symptoms in a community sample of individuals 60–64 years old. Am J Psychiatry. 2005;162:699–705. doi: 10.1176/appi.ajp.162.4.699. [DOI] [PubMed] [Google Scholar]
- Kanazawa T, Chana G, Glatt SJ, Mizuno H, Masliah E, Yoneda H, et al. The utility of SELENBP1 gene expression as a biomarker for major psychotic disorders: Replication in schizophrenia and extension to bipolar disorder with psychosis. Am J Med Genet B Neuropsychiatr Genet. 2007 doi: 10.1002/ajmg.b.30664. [DOI] [PubMed] [Google Scholar]
- Karege F, Perret G, Bondolfi G, Schwald M, Bertschy G, Aubry JM. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res. 2002;109:143–148. doi: 10.1016/s0165-1781(02)00005-7. [DOI] [PubMed] [Google Scholar]
- Karege F, Vaudan G, Schwald M, Perroud N, La Harpe R. Neurotrophin levels in postmortem brains of suicide victims and the effects of antemortem diagnosis and psychotropic drugs. Brain Res Mol Brain Res. 2005;136:29–37. doi: 10.1016/j.molbrainres.2004.12.020. [DOI] [PubMed] [Google Scholar]
- Kato T, Hamakawa H, Shioiri T, Murashita J, Takahashi Y, Takahashi S, Inubushi T. Choline-containing compounds detected by proton magnetic resonance spectroscopy in the basal ganglia in bipolar disorder. J Psychiatry Neurosci. 1996;21:248–254. [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Yang BZ, Douglas-Palumberi H, Grasso D, Lipschitz D, Houshyar S, et al. Brain-derived neurotrophic factor-5-HTTLPR gene interactions and environmental modifiers of depression in children. Biol Psychiatry. 2006;59:673–680. doi: 10.1016/j.biopsych.2005.10.026. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Yang BZ, Douglas-Palumberi H, Houshyar S, Lipschitz D, Krystal JH, Gelernter J. Social supports and serotonin transporter gene moderate depression in maltreated children. Proc Natl Acad Sci U S A. 2004;101:17316–17321. doi: 10.1073/pnas.0404376101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur S, Sassi RB, Axelson D, Nicoletti M, Brambilla P, Monkul ES, et al. Cingulate cortex anatomical abnormalities in children and adolescents with bipolar disorder. Am J Psychiatry. 2005;162:1637–1643. doi: 10.1176/appi.ajp.162.9.1637. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, McElroy SL, Havens JR, Altshuler LL, Nolen WA, Frye MA, et al. Psychosis in bipolar disorder: phenomenology and impact on morbidity and course of illness. Compr Psychiatry. 2003;44:263–269. doi: 10.1016/S0010-440X(03)00089-0. [DOI] [PubMed] [Google Scholar]
- Keedwell P, Drapier D, Surguladze S, Giampietro V, Brammer M, Phillips M. Neural markers of symptomatic improvement during antidepressant therapy in severe depression: subgenual cingulate and visual cortical responses to sad, but not happy, facial stimuli are correlated with changes in symptom score. J Psychopharmacol. 2008 doi: 10.1177/0269881108093589. [DOI] [PubMed] [Google Scholar]
- Kegeles LS, Malone KM, Slifstein M, Ellis SP, Xanthopoulos E, Keilp JG, et al. Response of cortical metabolic deficits to serotonergic challenge in familial mood disorders. Am J Psychiatry. 2003;160:76–82. doi: 10.1176/appi.ajp.160.1.76. [DOI] [PubMed] [Google Scholar]
- Keller J, Shen L, Gomez RG, Garrett A, Solvason HB, Reiss A, Schatzberg AF. Hippocampal and amygdalar volumes in psychotic and nonpsychotic unipolar depression. Am J Psychiatry. 2008;165:872–880. doi: 10.1176/appi.ajp.2008.07081257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gatz M, Gardner CO, Pedersen NL. Age at onset and familial risk for major depression in a Swedish national twin sample. Psychol Med. 2005;35:1573–1579. doi: 10.1017/S0033291705005714. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA. A population-based twin study of lifetime major depression in men and women. Arch Gen Psychiatry. 1999;56:39–44. doi: 10.1001/archpsyc.56.1.39. [DOI] [PubMed] [Google Scholar]
- Kennedy SH, Evans KR, Kruger S, Mayberg HS, Meyer JH, McCann S, et al. Changes in regional brain glucose metabolism measured with positron emission tomography after paroxetine treatment of major depression. Am J Psychiatry. 2001;158:899–905. doi: 10.1176/appi.ajp.158.6.899. [DOI] [PubMed] [Google Scholar]
- Kertesz A, Black SE, Tokar G, Benke T, Carr T, Nicholson L. Periventricular and subcortical hyperintensities on magnetic resonance imaging. ‘Rims, caps, and unidentified bright objects’. Arch Neurol. 1988;45:404–408. doi: 10.1001/archneur.1988.00520280050015. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Agerbo E, Mortensen PB. Major stressful life events and other risk factors for first admission with mania. Bipolar Disord. 2004;6:122–129. doi: 10.1111/j.1399-5618.2004.00102.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) Jama. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Ketter TA, Kimbrell TA, George MS, Dunn RT, Speer AM, Benson BE, et al. Effects of mood and subtype on cerebral glucose metabolism in treatment-resistant bipolar disorder. Biol Psychiatry. 2001;49:97–109. doi: 10.1016/s0006-3223(00)00975-6. [DOI] [PubMed] [Google Scholar]
- Ketter TA, Wang PW, Becker OV, Nowakowska C, Yang Y. Psychotic bipolar disorders: dimensionally similar to or categorically different from schizophrenia? J Psychiatr Res. 2004;38:47–61. doi: 10.1016/s0022-3956(03)00099-2. [DOI] [PubMed] [Google Scholar]
- Kieseppa T, Partonen T, Haukka J, Kaprio J, Lonnqvist J. High concordance of bipolar I disorder in a nationwide sample of twins. Am J Psychiatry. 2004;161:1814–1821. doi: 10.1176/ajp.161.10.1814. [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, Cornelius JR, Han X, Pincus HA, Shad M, Salloum I, et al. Burden of general medical conditions among individuals with bipolar disorder. Bipolar Disord. 2004;6:368–373. doi: 10.1111/j.1399-5618.2004.00138.x. [DOI] [PubMed] [Google Scholar]
- Kim DK, Kim BL, Sohn SE, Lim SW, Na DG, Paik CH, et al. Candidate neuroanatomic substrates of psychosis in old-aged depression. Prog Neuropsychopharmacol Biol Psychiatry. 1999;23:793–807. doi: 10.1016/s0278-5846(99)00041-x. [DOI] [PubMed] [Google Scholar]
- Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Kim YH, Yoon JS. BDNF genotype potentially modifying the association between incident stroke and depression. Neurobiol Aging. 2007 doi: 10.1016/j.neurobiolaging.2006.11.021. [DOI] [PubMed] [Google Scholar]
- Kim JS, Chang MY, Yu IT, Kim JH, Lee SH, Lee YS, Son H. Lithium selectively increases neuronal differentiation of hippocampal neural progenitor cells both in vitro and in vivo. J Neurochem. 2004;89:324–336. doi: 10.1046/j.1471-4159.2004.02329.x. [DOI] [PubMed] [Google Scholar]
- Kinney DK, Yurgelun-Todd DA, Levy DL, Medoff D, Lajonchere CM, Radford-Paregol M. Obstetrical complications in patients with bipolar disorder and their siblings. Psychiatry Res. 1993;48:47–56. doi: 10.1016/0165-1781(93)90112-t. [DOI] [PubMed] [Google Scholar]
- Kinney DK, Yurgelun-Todd DA, Tohen M, Tramer S. Pre- and perinatal complications and risk for bipolar disorder: a retrospective study. J Affect Disord. 1998;50:117–124. doi: 10.1016/s0165-0327(98)00015-9. [DOI] [PubMed] [Google Scholar]
- Knopman DS, Mosley TH, Catellier DJ, Sharrett AR. Cardiovascular risk factors and cerebral atrophy in a middle-aged cohort. Neurology. 2005;65:876–881. doi: 10.1212/01.wnl.0000176074.09733.a8. [DOI] [PubMed] [Google Scholar]
- Kogelnik AM, Loomis K, Hoegh-Petersen M, Rosso F, Hischier C, Montoya JG. Use of valganciclovir in patients with elevated antibody titers against Human Herpesvirus-6 (HHV-6) and Epstein-Barr Virus (EBV) who were experiencing central nervous system dysfunction including long-standing fatigue. J Clin Virol. 2006;37(Suppl 1):S33–38. doi: 10.1016/S1386-6532(06)70009-9. [DOI] [PubMed] [Google Scholar]
- Koo MS, Levitt JJ, Salisbury DF, Nakamura M, Shenton ME, McCarley RW. A cross-sectional and longitudinal magnetic resonance imaging study of cingulate gyrus gray matter volume abnormalities in first-episode schizophrenia and first-episode affective psychosis. Arch Gen Psychiatry. 2008;65:746–760. doi: 10.1001/archpsyc.65.7.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopell BH, Greenberg BD. Anatomy and physiology of the basal ganglia: implications for DBS in psychiatry. Neurosci Biobehav Rev. 2008;32:408–422. doi: 10.1016/j.neubiorev.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Devlin B, Pollock M, Richards C, Mukerji P. A controlled family history study of childhood-onset depressive disorder. Arch Gen Psychiatry. 1997;54:613–623. doi: 10.1001/archpsyc.1997.01830190033004. [DOI] [PubMed] [Google Scholar]
- Krabbendam L, Honig A, Wiersma J, Vuurman EF, Hofman PA, Derix MM, et al. Cognitive dysfunctions and white matter lesions in patients with bipolar disorder in remission. Acta Psychiatr Scand. 2000;101:274–280. [PubMed] [Google Scholar]
- Kringelbach ML. The human orbitofrontal cortex: linking reward to hedonic experience. Nat Rev Neurosci. 2005;6:691–702. doi: 10.1038/nrn1747. [DOI] [PubMed] [Google Scholar]
- Kringelbach ML, Rolls ET. The functional neuroanatomy of the human orbitofrontal cortex: evidence from neuroimaging and neuropsychology. Prog Neurobiol. 2004;72:341–372. doi: 10.1016/j.pneurobio.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Krishnan KR. Biological risk factors in late life depression. Biol Psychiatry. 2002;52:185–192. doi: 10.1016/s0006-3223(02)01349-5. [DOI] [PubMed] [Google Scholar]
- Krishnan KR, Doraiswamy PM, Figiel GS, Husain MM, Shah SA, Na C, et al. Hippocampal abnormalities in depression. J Neuropsychiatry Clin Neurosci. 1991;3:387–391. doi: 10.1176/jnp.3.4.387. [DOI] [PubMed] [Google Scholar]
- Krishnan KR, Goli V, Ellinwood EH, France RD, Blazer DG, Nemeroff CB. Leukoencephalopathy in patients diagnosed as major depressive. Biol Psychiatry. 1988;23:519–522. doi: 10.1016/0006-3223(88)90025-x. [DOI] [PubMed] [Google Scholar]
- Krishnan KR, Hays JC, Blazer DG. MRI-defined vascular depression. Am J Psychiatry. 1997;154:497–501. doi: 10.1176/ajp.154.4.497. [DOI] [PubMed] [Google Scholar]
- Krishnan KR, McDonald WM, Escalona PR, Doraiswamy PM, Na C, Husain MM, et al. Magnetic resonance imaging of the caudate nuclei in depression. Preliminary observations. Arch Gen Psychiatry. 1992;49:553–557. doi: 10.1001/archpsyc.1992.01820070047007. [DOI] [PubMed] [Google Scholar]
- Kronhaus DM, Lawrence NS, Williams AM, Frangou S, Brammer MJ, Williams SC, et al. Stroop performance in bipolar disorder: further evidence for abnormalities in the ventral prefrontal cortex. Bipolar Disord. 2006;8:28–39. doi: 10.1111/j.1399-5618.2006.00282.x. [DOI] [PubMed] [Google Scholar]
- Kronmuller KT, Pantel J, Kohler S, Victor D, Giesel F, Magnotta VA, et al. Hippocampal volume and 2-year outcome in depression. Br J Psychiatry. 2008;192:472–473. doi: 10.1192/bjp.bp.107.040378. [DOI] [PubMed] [Google Scholar]
- Kruger S, Alda M, Young LT, Goldapple K, Parikh S, Mayberg HS. Risk and resilience markers in bipolar disorder: brain responses to emotional challenge in bipolar patients and their healthy siblings. Am J Psychiatry. 2006;163:257–264. doi: 10.1176/appi.ajp.163.2.257. [DOI] [PubMed] [Google Scholar]
- Kruger S, Seminowicz D, Goldapple K, Kennedy SH, Mayberg HS. State and trait influences on mood regulation in bipolar disorder: blood flow differences with an acute mood challenge. Biol Psychiatry. 2003;54:1274–1283. doi: 10.1016/s0006-3223(03)00691-7. [DOI] [PubMed] [Google Scholar]
- Kubicki M, Shenton ME, Salisbury DF, Hirayasu Y, Kasai K, Kikinis R, et al. Voxel-based morphometric analysis of gray matter in first episode schizophrenia. Neuroimage. 2002;17:1711–1719. doi: 10.1006/nimg.2002.1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumano H, Ida I, Oshima A, Takahashi K, Yuuki N, Amanuma M, et al. Brain metabolic changes associated with predispotion to onset of major depressive disorder and adjustment disorder in cancer patients -A preliminary PET study. J Psychiatr Res. 2006 doi: 10.1016/j.jpsychires.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Kumar A, Bilker W, Jin Z, Udupa J. Atrophy and high intensity lesions: complementary neurobiological mechanisms in late-life major depression. Neuropsychopharmacology. 2000;22:264–274. doi: 10.1016/S0893-133X(99)00124-4. [DOI] [PubMed] [Google Scholar]
- Kumar A, Gupta RC, Albert Thomas M, Alger J, Wyckoff N, Hwang S. Biophysical changes in normal-appearing white matter and subcortical nuclei in late-life major depression detected using magnetization transfer. Psychiatry Res. 2004;130:131–140. doi: 10.1016/j.pscychresns.2003.12.002. [DOI] [PubMed] [Google Scholar]
- LaBar KS, Cabeza R. Cognitive neuroscience of emotional memory. Nat Rev Neurosci. 2006;7:54–64. doi: 10.1038/nrn1825. [DOI] [PubMed] [Google Scholar]
- Lacerda AL, Brambilla P, Sassi RB, Nicoletti MA, Mallinger AG, Frank E, et al. Anatomical MRI study of corpus callosum in unipolar depression. J Psychiatr Res. 2005;39:347–354. doi: 10.1016/j.jpsychires.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Lacerda AL, Keshavan MS, Hardan AY, Yorbik O, Brambilla P, Sassi RB, et al. Anatomic evaluation of the orbitofrontal cortex in major depressive disorder. Biol Psychiatry. 2004;55:353–358. doi: 10.1016/j.biopsych.2003.08.021. [DOI] [PubMed] [Google Scholar]
- Lacerda AL, Nicoletti MA, Brambilla P, Sassi RB, Mallinger AG, Frank E, et al. Anatomical MRI study of basal ganglia in major depressive disorder. Psychiatry Res. 2003;124:129–140. doi: 10.1016/s0925-4927(03)00123-9. [DOI] [PubMed] [Google Scholar]
- Ladouceur CD, Almeida JR, Birmaher B, Axelson DA, Nau S, Kalas C, et al. Subcortical gray matter volume abnormalities in healthy bipolar offspring: potential neuroanatomical risk marker for bipolar disorder? J Am Acad Child Adolesc Psychiatry. 2008;47:532–539. doi: 10.1097/CHI.0b013e318167656e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai T, Payne ME, Byrum CE, Steffens DC, Krishnan KR. Reduction of orbital frontal cortex volume in geriatric depression. Biol Psychiatry. 2000;48:971–975. doi: 10.1016/s0006-3223(00)01042-8. [DOI] [PubMed] [Google Scholar]
- Lange C, Irle E. Enlarged amygdala volume and reduced hippocampal volume in young women with major depression. Psychol Med. 2004;34:1059–1064. doi: 10.1017/s0033291703001806. [DOI] [PubMed] [Google Scholar]
- Lauterbach EC, Jackson JG, Wilson AN, Dever GE, Kirsh AD. Major depression after left posterior globus pallidus lesions. Neuropsychiatry Neuropsychol Behav Neurol. 1997;10:9–16. [PubMed] [Google Scholar]
- Lavretsky H, Kurbanyan K, Ballmaier M, Mintz J, Toga A, Kumar A. Sex differences in brain structure in geriatric depression. Am J Geriatr Psychiatry. 2004;12:653–657. doi: 10.1176/appi.ajgp.12.6.653. [DOI] [PubMed] [Google Scholar]
- Lawrence NS, Williams AM, Surguladze S, Giampietro V, Brammer MJ, Andrew C, et al. Subcortical and ventral prefrontal cortical neural responses to facial expressions distinguish patients with bipolar disorder and major depression. Biol Psychiatry. 2004;55:578–587. doi: 10.1016/j.biopsych.2003.11.017. [DOI] [PubMed] [Google Scholar]
- LeDoux JE. Emotion circuits in the brain. Annu Rev Neurosci. 2000;23:155–184. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- Lee AL, Ogle WO, Sapolsky RM. Stress and depression: possible links to neuron death in the hippocampus. Bipolar Disord. 2002;4:117–128. doi: 10.1034/j.1399-5618.2002.01144.x. [DOI] [PubMed] [Google Scholar]
- Lemonde S, Turecki G, Bakish D, Du L, Hrdina PD, Bown CD, et al. Impaired repression at a 5-hydroxytryptamine 1A receptor gene polymorphism associated with major depression and suicide. J Neurosci. 2003;23:8788–8799. doi: 10.1523/JNEUROSCI.23-25-08788.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennox BR, Jacob R, Calder AJ, Lupson V, Bullmore ET. Behavioural and neurocognitive responses to sad facial affect are attenuated in patients with mania. Psychol Med. 2004;34:795–802. doi: 10.1017/s0033291704002557. [DOI] [PubMed] [Google Scholar]
- Lenze E, Cross D, McKeel D, Neuman RJ, Sheline YI. White matter hyperintensities and gray matter lesions in physically healthy depressed subjects. Am J Psychiatry. 1999;156:1602–1607. doi: 10.1176/ajp.156.10.1602. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Sheline YI. Absence of striatal volume differences between depressed subjects with no comorbid medical illness and matched comparison subjects. Am J Psychiatry. 1999;156:1989–1991. doi: 10.1176/ajp.156.12.1989. [DOI] [PubMed] [Google Scholar]
- Lesch KP, Bengel D, Heils A, Sabol SZ, Greenberg BD, Petri S, et al. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science. 1996;274:1527–1531. doi: 10.1126/science.274.5292.1527. [DOI] [PubMed] [Google Scholar]
- Lewine RR, Hudgins P, Brown F, Caudle J, Risch SC. Differences in qualitative brain morphology findings in schizophrenia, major depression, bipolar disorder, and normal volunteers. Schizophr Res. 1995;15:253–259. doi: 10.1016/0920-9964(94)00055-d. [DOI] [PubMed] [Google Scholar]
- Lieberman A. Depression in Parkinson’s disease -- a review. Acta Neurol Scand. 2006;113:1–8. doi: 10.1111/j.1600-0404.2006.00536.x. [DOI] [PubMed] [Google Scholar]
- Lim KO, Rosenbloom MJ, Faustman WO, Sullivan EV, Pfefferbaum A. Cortical gray matter deficit in patients with bipolar disorder. Schizophr Res. 1999;40:219–227. doi: 10.1016/s0920-9964(99)00063-8. [DOI] [PubMed] [Google Scholar]
- Liotti M, Mayberg HS, McGinnis S, Brannan SL, Jerabek P. Unmasking disease-specific cerebral blood flow abnormalities: mood challenge in patients with remitted unipolar depression. Am J Psychiatry. 2002;159:1830–1840. doi: 10.1176/appi.ajp.159.11.1830. [DOI] [PubMed] [Google Scholar]
- Liston C, Miller MM, Goldwater DS, Radley JJ, Rocher AB, Hof PR, et al. Stress-induced alterations in prefrontal cortical dendritic morphology predict selective impairments in perceptual attentional set-shifting. J Neurosci. 2006;26:7870–7874. doi: 10.1523/JNEUROSCI.1184-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd AJ, Ferrier IN, Barber R, Gholkar A, Young AH, O’Brien JT. Hippocampal volume change in depression: late- and early-onset illness compared. Br J Psychiatry. 2004;184:488–495. doi: 10.1192/bjp.184.6.488. [DOI] [PubMed] [Google Scholar]
- Lochhead RA, Parsey RV, Oquendo MA, Mann JJ. Regional brain gray matter volume differences in patients with bipolar disorder as assessed by optimized voxel-based morphometry. Biol Psychiatry. 2004;55:1154–1162. doi: 10.1016/j.biopsych.2004.02.026. [DOI] [PubMed] [Google Scholar]
- Lopez-Larson MP, DelBello MP, Zimmerman ME, Schwiers ML, Strakowski SM. Regional prefrontal gray and white matter abnormalities in bipolar disorder. Biol Psychiatry. 2002;52:93–100. doi: 10.1016/s0006-3223(02)01350-1. [DOI] [PubMed] [Google Scholar]
- Lucassen PJ, Muller MB, Holsboer F, Bauer J, Holtrop A, Wouda J, et al. Hippocampal apoptosis in major depression is a minor event and absent from subareas at risk for glucocorticoid overexposure. Am J Pathol. 2001;158:453–468. doi: 10.1016/S0002-9440(10)63988-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien SJ, Evans A, Lord C, Miles J, Pruessner M, Pike B, Pruessner JC. Hippocampal volume is as variable in young as in older adults: Implications for the notion of hippocampal atrophy in humans. Neuroimage. 2007;34:479–485. doi: 10.1016/j.neuroimage.2006.09.041. [DOI] [PubMed] [Google Scholar]
- Lyness JM, King DA, Conwell Y, Cox C, Caine ED. Cerebrovascular risk factors and 1-year depression outcome in older primary care patients. Am J Psychiatry. 2000;157:1499–1501. doi: 10.1176/appi.ajp.157.9.1499. [DOI] [PubMed] [Google Scholar]
- Lyons MJ, Eisen SA, Goldberg J, True W, Lin N, Meyer JM, et al. A registry-based twin study of depression in men. Arch Gen Psychiatry. 1998;55:468–472. doi: 10.1001/archpsyc.55.5.468. [DOI] [PubMed] [Google Scholar]
- Lyoo IK, Kim MJ, Stoll AL, Demopulos CM, Parow AM, Dager SR, et al. Frontal lobe gray matter density decreases in bipolar I disorder. Biol Psychiatry. 2004a;55:648–651. doi: 10.1016/j.biopsych.2003.10.017. [DOI] [PubMed] [Google Scholar]
- Lyoo IK, Kwon JS, Lee SJ, Han MH, Chang CG, Seo CS, et al. Decrease in genu of the corpus callosum in medication-naive, early-onset dysthymia and depressive personality disorder. Biol Psychiatry. 2002a;52:1134–1143. doi: 10.1016/s0006-3223(02)01436-1. [DOI] [PubMed] [Google Scholar]
- Lyoo IK, Lee HK, Jung JH, Noam GG, Renshaw PF. White matter hyperintensities on magnetic resonance imaging of the brain in children with psychiatric disorders. Compr Psychiatry. 2002b;43:361–368. doi: 10.1053/comp.2002.34636. [DOI] [PubMed] [Google Scholar]
- Lyoo IK, Streeter CC, Ahn KH, Lee HK, Pollack MH, Silveri MM, et al. White matter hyperintensities in subjects with cocaine and opiate dependence and healthy comparison subjects. Psychiatry Res. 2004b;131:135–145. doi: 10.1016/j.pscychresns.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Lyoo IK, Sung YH, Dager SR, Friedman SD, Lee JY, Kim SJ, et al. Regional cerebral cortical thinning in bipolar disorder. Bipolar Disord. 2006;8:65–74. doi: 10.1111/j.1399-5618.2006.00284.x. [DOI] [PubMed] [Google Scholar]
- Ma N, Li L, Shu N, Liu J, Gong G, He Z, et al. White matter abnormalities in first-episode, treatment-naive young adults with major depressive disorder. Am J Psychiatry. 2007;164:823–826. doi: 10.1176/ajp.2007.164.5.823. [DOI] [PubMed] [Google Scholar]
- MacFall JR, Payne ME, Provenzale JE, Krishnan KR. Medial orbital frontal lesions in late-onset depression. Biol Psychiatry. 2001;49:803–806. doi: 10.1016/s0006-3223(00)01113-6. [DOI] [PubMed] [Google Scholar]
- MacMaster FP, Kusumakar V. Hippocampal volume in early onset depression. BMC Med. 2004;2:2. doi: 10.1186/1741-7015-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmaster FP, Mirza Y, Szeszko PR, Kmiecik LE, Easter PC, Taormina SP, et al. Amygdala and Hippocampal Volumes in Familial Early Onset Major Depressive Disorder. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2007.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacQueen GM, Campbell S, McEwen BS, Macdonald K, Amano S, Joffe RT, et al. Course of illness, hippocampal function, and hippocampal volume in major depression. Proc Natl Acad Sci U S A. 2003;100:1387–1392. doi: 10.1073/pnas.0337481100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magarinos AM, McEwen BS, Flugge G, Fuchs E. Chronic psychosocial stress causes apical dendritic atrophy of hippocampal CA3 pyramidal neurons in subordinate tree shrews. J Neurosci. 1996;16:3534–3540. doi: 10.1523/JNEUROSCI.16-10-03534.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mah L, Zarate CA, Jr, Singh J, Duan YF, Luckenbaugh DA, Manji HK, Drevets WC. Regional cerebral glucose metabolic abnormalities in bipolar II depression. Biol Psychiatry. 2007;61:765–775. doi: 10.1016/j.biopsych.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Manji HK, Moore GJ, Chen G. Clinical and preclinical evidence for the neurotrophic effects of mood stabilizers: implications for the pathophysiology and treatment of manic-depressive illness. Biol Psychiatry. 2000;48:740–754. doi: 10.1016/s0006-3223(00)00979-3. [DOI] [PubMed] [Google Scholar]
- Marchand WR, Lee JN, Thatcher J, Thatcher GW, Jensen C, Starr J. A preliminary longitudinal fMRI study of frontal-subcortical circuits in bipolar disorder using a paced motor activation paradigm. J Affect Disord. 2007;103:237–241. doi: 10.1016/j.jad.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Mark RJ, Ashford JW, Goodman Y, Mattson MP. Anticonvulsants attenuate amyloid beta-peptide neurotoxicity, Ca2+ deregulation, and cytoskeletal pathology. Neurobiol Aging. 1995;16:187–198. doi: 10.1016/0197-4580(94)00150-2. [DOI] [PubMed] [Google Scholar]
- Martinot JL, Hardy P, Feline A, Huret JD, Mazoyer B, Attar-Levy D, et al. Left prefrontal glucose hypometabolism in the depressed state: a confirmation. Am J Psychiatry. 1990;147:1313–1317. doi: 10.1176/ajp.147.10.1313. [DOI] [PubMed] [Google Scholar]
- Massana G, Salgado-Pineda P, Junque C, Perez M, Baeza I, Pons A, et al. Volume changes in gray matter in first-episode neuroleptic-naive schizophrenic patients treated with risperidone. J Clin Psychopharmacol. 2005;25:111–117. doi: 10.1097/01.jcp.0000155818.29091.53. [DOI] [PubMed] [Google Scholar]
- Matsuo K, Glahn DC, Peluso MA, Hatch JP, Monkul ES, Najt P, et al. Prefrontal hyperactivation during working memory task in untreated individuals with major depressive disorder. Mol Psychiatry. 2007;12:158–166. doi: 10.1038/sj.mp.4001894. [DOI] [PubMed] [Google Scholar]
- Matsuo K, Rosenberg DR, Easter PC, MacMaster FP, Chen HH, Nicoletti M, et al. Striatal volume abnormalities in treatment-naive patients diagnosed with pediatric major depressive disorder. J Child Adolesc Psychopharmacol. 2008;18:121–131. doi: 10.1089/cap.2007.0026. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Brannan SK, Tekell JL, Silva JA, Mahurin RK, McGinnis S, Jerabek PA. Regional metabolic effects of fluoxetine in major depression: serial changes and relationship to clinical response. Biol Psychiatry. 2000;48:830–843. doi: 10.1016/s0006-3223(00)01036-2. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, Jerabek PA, et al. Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. Am J Psychiatry. 1999;156:675–682. doi: 10.1176/ajp.156.5.675. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45:651–660. doi: 10.1016/j.neuron.2005.02.014. [DOI] [PubMed] [Google Scholar]
- McDonald C, Bullmore ET, Sham PC, Chitnis X, Wickham H, Bramon E, Murray RM. Association of genetic risks for schizophrenia and bipolar disorder with specific and generic brain structural endophenotypes. Arch Gen Psychiatry. 2004a;61:974–984. doi: 10.1001/archpsyc.61.10.974. [DOI] [PubMed] [Google Scholar]
- McDonald C, Marshall N, Sham PC, Bullmore ET, Schulze K, Chapple B, et al. Regional brain morphometry in patients with schizophrenia or bipolar disorder and their unaffected relatives. Am J Psychiatry. 2006;163:478–487. doi: 10.1176/appi.ajp.163.3.478. [DOI] [PubMed] [Google Scholar]
- McDonald C, Zanelli J, Rabe-Hesketh S, Ellison-Wright I, Sham P, Kalidindi S, et al. Meta-analysis of magnetic resonance imaging brain morphometry studies in bipolar disorder. Biol Psychiatry. 2004b;56:411–417. doi: 10.1016/j.biopsych.2004.06.021. [DOI] [PubMed] [Google Scholar]
- McDonald WM, Krishnan KR, Doraiswamy PM, Blazer DG. Occurrence of subcortical hyperintensities in elderly subjects with mania. Psychiatry Res. 1991;40:211–220. doi: 10.1016/0925-4927(91)90013-g. [DOI] [PubMed] [Google Scholar]
- McDonald WM, Tupler LA, Marsteller FA, Figiel GS, DiSouza S, Nemeroff CB, Krishnan KR. Hyperintense lesions on magnetic resonance images in bipolar disorder. Biol Psychiatry. 1999;45:965–971. doi: 10.1016/s0006-3223(98)00341-2. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Chattarji S. Molecular mechanisms of neuroplasticity and pharmacological implications: the example of tianeptine. Eur Neuropsychopharmacol. 2004;14(Suppl 5):S497–502. doi: 10.1016/j.euroneuro.2004.09.008. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Magarinos AM. Stress and hippocampal plasticity: implications for the pathophysiology of affective disorders. Hum Psychopharmacol. 2001;16:S7–S19. doi: 10.1002/hup.266. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Magarinos AM, Reagan LP. Structural plasticity and tianeptine: cellular and molecular targets. Eur Psychiatry. 2002;17(Suppl 3):318–330. doi: 10.1016/s0924-9338(02)00650-8. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Olie JP. Neurobiology of mood, anxiety, and emotions as revealed by studies of a unique antidepressant: tianeptine. Mol Psychiatry. 2005;10:525–537. doi: 10.1038/sj.mp.4001648. [DOI] [PubMed] [Google Scholar]
- McGuffin P, Katz R. The genetics of depression and manic-depressive disorder. Br J Psychiatry. 1989;155:294–304. doi: 10.1192/bjp.155.3.294. [DOI] [PubMed] [Google Scholar]
- McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry. 2003;60:497–502. doi: 10.1001/archpsyc.60.5.497. [DOI] [PubMed] [Google Scholar]
- McIntosh AM, Job DE, Moorhead TW, Harrison LK, Forrester K, Lawrie SM, Johnstone EC. Voxel-based morphometry of patients with schizophrenia or bipolar disorder and their unaffected relatives. Biol Psychiatry. 2004;56:544–552. doi: 10.1016/j.biopsych.2004.07.020. [DOI] [PubMed] [Google Scholar]
- McIntosh AM, Job DE, Moorhead WJ, Harrison LK, Whalley HC, Johnstone EC, Lawrie SM. Genetic liability to schizophrenia or bipolar disorder and its relationship to brain structure. Am J Med Genet B Neuropsychiatr Genet. 2006;141:76–83. doi: 10.1002/ajmg.b.30254. [DOI] [PubMed] [Google Scholar]
- McIntosh AM, Moorhead TW, Job D, Lymer GK, Munoz Maniega S, McKirdy J, et al. The effects of a neuregulin 1 variant on white matter density and integrity. Mol Psychiatry. 2007 doi: 10.1038/sj.mp.4002103. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Soczynska JK, Konarski JZ, Woldeyohannes HO, Law CW, Miranda A, et al. Should Depressive Syndromes Be Reclassified as “Metabolic Syndrome Type II”? Ann Clin Psychiatry. 2007;19:257–264. doi: 10.1080/10401230701653377. [DOI] [PubMed] [Google Scholar]
- Meaney MJ, Szyf M. Maternal care as a model for experience-dependent chromatin plasticity? Trends Neurosci. 2005;28:456–463. doi: 10.1016/j.tins.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Medina KL, Nagel BJ, Park A, McQueeny T, Tapert SF. Depressive symptoms in adolescents: associations with white matter volume and marijuana use. J Child Psychol Psychiatry. 2007;48:592–600. doi: 10.1111/j.1469-7610.2007.01728.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervaala E, Fohr J, Kononen M, Valkonen-Korhonen M, Vainio P, Partanen K, et al. Quantitative MRI of the hippocampus and amygdala in severe depression. Psychological Medicine. 2000;30:117–125. doi: 10.1017/s0033291799001567. [DOI] [PubMed] [Google Scholar]
- Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci U S A. 2005;102:10706–10711. doi: 10.1073/pnas.0502441102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mill J, Petronis A. Molecular studies of major depressive disorder: the epigenetic perspective. Mol Psychiatry. 2007 doi: 10.1038/sj.mp.4001992. [DOI] [PubMed] [Google Scholar]
- Minett TS, Dean JL, Firbank M, English P, O’Brien JT. Subjective memory complaints, white-matter lesions, depressive symptoms, and cognition in elderly patients. Am J Geriatr Psychiatry. 2005;13:665–671. doi: 10.1176/appi.ajgp.13.8.665. [DOI] [PubMed] [Google Scholar]
- Miracle AD, Brace MF, Huyck KD, Singler SA, Wellman CL. Chronic stress impairs recall of extinction of conditioned fear. Neurobiol Learn Mem. 2006;85:213–218. doi: 10.1016/j.nlm.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Monk CS, Klein RG, Telzer EH, Schroth EA, Mannuzza S, Moulton JL, 3rd, et al. Amygdala and Nucleus Accumbens Activation to Emotional Facial Expressions in Children and Adolescents at Risk for Major Depression. Am J Psychiatry. 2007 doi: 10.1176/appi.ajp.2007.06111917. [DOI] [PubMed] [Google Scholar]
- Moore G, Cortese B, Glitz D, Zajac-Benitez C, Quiroz J, Uhde T, et al. Lithium increases gray matter in the prefrontal and subgenual prefrontal cortices in treatment responsive bipolar patients. Journal of Clinical Psychiatry. doi: 10.4088/JCP.07m03745. In press. [DOI] [PubMed] [Google Scholar]
- Moore GJ, Bebchuk JM, Wilds IB, Chen G, Manji HK. Lithium-induced increase in human brain grey matter. Lancet. 2000;356:1241–1242. doi: 10.1016/s0140-6736(00)02793-8. [DOI] [PubMed] [Google Scholar]
- Moore PB, Shepherd DJ, Eccleston D, Macmillan IC, Goswami U, McAllister VL, Ferrier IN. Cerebral white matter lesions in bipolar affective disorder: relationship to outcome. Br J Psychiatry. 2001;178:172–176. doi: 10.1192/bjp.178.2.172. [DOI] [PubMed] [Google Scholar]
- Moorhead TW, McKirdy J, Sussmann JE, Hall J, Lawrie SM, Johnstone EC, McIntosh AM. Progressive Gray Matter Loss in Patients with Bipolar Disorder. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Morris PL, Robinson RG, Raphael B, Hopwood MJ. Lesion location and poststroke depression. J Neuropsychiatry Clin Neurosci. 1996;8:399–403. doi: 10.1176/jnp.8.4.399. [DOI] [PubMed] [Google Scholar]
- Morris RG. Elements of a neurobiological theory of hippocampal function: the role of synaptic plasticity, synaptic tagging and schemas. Eur J Neurosci. 2006;23:2829–2846. doi: 10.1111/j.1460-9568.2006.04888.x. [DOI] [PubMed] [Google Scholar]
- Munn MA, Alexopoulos J, Nishino T, Babb CM, Flake LA, Singer T, et al. Amygdala volume analysis in female twins with major depression. Biol Psychiatry. 2007;62:415–422. doi: 10.1016/j.biopsych.2006.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murata T, Kimura H, Omori M, Kado H, Kosaka H, Iidaka T, et al. MRI white matter hyperintensities, (1)H-MR spectroscopy and cognitive function in geriatric depression: a comparison of early- and late-onset cases. Int J Geriatr Psychiatry. 2001;16:1129–1135. doi: 10.1002/gps.501. [DOI] [PubMed] [Google Scholar]
- Murmu MS, Salomon S, Biala Y, Weinstock M, Braun K, Bock J. Changes of spine density and dendritic complexity in the prefrontal cortex in offspring of mothers exposed to stress during pregnancy. Eur J Neurosci. 2006;24:1477–1487. doi: 10.1111/j.1460-9568.2006.05024.x. [DOI] [PubMed] [Google Scholar]
- Murphy DG, DeCarli C, Schapiro MB, Rapoport SI, Horwitz B. Age-related differences in volumes of subcortical nuclei, brain matter, and cerebrospinal fluid in healthy men as measured with magnetic resonance imaging. Arch Neurol. 1992;49:839–845. doi: 10.1001/archneur.1992.00530320063013. [DOI] [PubMed] [Google Scholar]
- Musselman DL, Tomer A, Manatunga AK, Knight BT, Porter MR, Kasey S, et al. Exaggerated platelet reactivity in major depression. Am J Psychiatry. 1996;153:1313–1317. doi: 10.1176/ajp.153.10.1313. [DOI] [PubMed] [Google Scholar]
- Nahas Z, Teneback C, Chae JH, Mu Q, Molnar C, Kozel FA, et al. Serial Vagus Nerve Stimulation Functional MRI in Treatment-Resistant Depression. Neuropsychopharmacology. 2007 doi: 10.1038/sj.npp.1301288. [DOI] [PubMed] [Google Scholar]
- Nair A, Vadodaria KC, Banerjee SB, Benekareddy M, Dias BG, Duman RS, Vaidya VA. Stressor-Specific Regulation of Distinct Brain-Derived Neurotrophic Factor Transcripts and Cyclic AMP Response Element-Binding Protein Expression in the Postnatal and Adult Rat Hippocampus. Neuropsychopharmacology. 2006 doi: 10.1038/sj.npp.1301276. [DOI] [PubMed] [Google Scholar]
- Najib A, Lorberbaum JP, Kose S, Bohning DE, George MS. Regional brain activity in women grieving a romantic relationship breakup. Am J Psychiatry. 2004;161:2245–2256. doi: 10.1176/appi.ajp.161.12.2245. [DOI] [PubMed] [Google Scholar]
- Najt P, Nicoletti M, Chen HH, Hatch JP, Caetano SC, Sassi RB, et al. Anatomical measurements of the orbitofrontal cortex in child and adolescent patients with bipolar disorder. Neurosci Lett. 2007 doi: 10.1016/j.neulet.2006.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakatani N, Hattori E, Ohnishi T, Dean B, Iwayama Y, Matsumoto I, et al. Genome-wide expression analysis detects eight genes with robust alterations specific to bipolar I disorder: relevance to neuronal network perturbation. Hum Mol Genet. 2006;15:1949–1962. doi: 10.1093/hmg/ddl118. [DOI] [PubMed] [Google Scholar]
- Nebes RD, Vora IJ, Meltzer CC, Fukui MB, Williams RL, Kamboh MI, et al. Relationship of deep white matter hyperintensities and apolipoprotein E genotype to depressive symptoms in older adults without clinical depression. Am J Psychiatry. 2001;158:878–884. doi: 10.1176/appi.ajp.158.6.878. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB, Musselman DL. Are platelets the link between depression and ischemic heart disease? Am Heart J. 2000;140:57–62. doi: 10.1067/mhj.2000.109978. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Drevets WC, Belfer I, Luckenbaugh DA, Henry S, Bonne O, et al. Effects of a alpha 2C-adrenoreceptor gene polymorphism on neural responses to facial expressions in depression. Neuropsychopharmacology. 2006a;31:1750–1756. doi: 10.1038/sj.npp.1301010. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Hu XZ, Luckenbaugh DA, Schwarz M, Nugent AC, Bonne O, et al. Differential effects of 5-HTTLPR genotypes on the behavioral and neural responses to tryptophan depletion in patients with major depression and controls. Arch Gen Psychiatry. 2006b;63:978–986. doi: 10.1001/archpsyc.63.9.978. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Konstantinidis A, Stastny J, Schwarz MJ, Vitouch O, Willeit M, et al. Association between serotonin transporter gene promoter polymorphism (5HTTLPR) and behavioral responses to tryptophan depletion in healthy women with and without family history of depression. Arch Gen Psychiatry. 2002;59:613–620. doi: 10.1001/archpsyc.59.7.613. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Nugent AC, Waldeck T, Geraci M, Schwarz M, Bonne O, et al. Neural and behavioral responses to tryptophan depletion in unmedicated patients with remitted major depressive disorder and controls. Arch Gen Psychiatry. 2004;61:765–773. doi: 10.1001/archpsyc.61.8.765. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Wood S, Bonne O, Nugent AC, Luckenbaugh DA, Young T, et al. Reduced hippocampal volume in unmedicated, remitted patients with major depression versus control subjects. Biol Psychiatry. 2005;57:935–937. doi: 10.1016/j.biopsych.2005.01.016. [DOI] [PubMed] [Google Scholar]
- Newcomer JW. Medical risk in patients with bipolar disorder and schizophrenia. J Clin Psychiatry. 2006;67(Suppl 9):25–30. discussion 36–42. [PubMed] [Google Scholar]
- Nierenberg AA, Trivedi MH, Fava M, Biggs MM, Shores-Wilson K, Wisniewski SR, et al. Family history of mood disorder and characteristics of major depressive disorder: a STAR*D (sequenced treatment alternatives to relieve depression) study. J Psychiatr Res. 2007;41:214–221. doi: 10.1016/j.jpsychires.2006.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobler MS, Oquendo MA, Kegeles LS, Malone KM, Campbell CC, Sackeim HA, Mann JJ. Decreased regional brain metabolism after ect. Am J Psychiatry. 2001;158:305–308. doi: 10.1176/appi.ajp.158.2.305. [DOI] [PubMed] [Google Scholar]
- Nobuhara K, Okugawa G, Sugimoto T, Minami T, Tamagaki C, Takase K, et al. Frontal white matter anisotropy and symptom severity of late-life depression: a magnetic resonance diffusion tensor imaging study. J Neurol Neurosurg Psychiatry. 2006;77:120–122. doi: 10.1136/jnnp.2004.055129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noga JT, Vladar K, Torrey EF. A volumetric magnetic resonance imaging study of monozygotic twins discordant for bipolar disorder. Psychiatry Res. 2001;106:25–34. doi: 10.1016/s0925-4927(00)00084-6. [DOI] [PubMed] [Google Scholar]
- Norbury R, Mackay CE, Cowen PJ, Goodwin GM, Harmer CJ. Short-term antidepressant treatment and facial processing. Functional magnetic resonance imaging study. Br J Psychiatry. 2007;190:531–532. doi: 10.1192/bjp.bp.106.031393. [DOI] [PubMed] [Google Scholar]
- Novak V, Last D, Alsop DC, Abduljalil AM, Hu K, Lepicovsky L, et al. Cerebral blood flow velocity and periventricular white matter hyperintensities in type 2 diabetes. Diabetes Care. 2006;29:1529–1534. doi: 10.2337/dc06-0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nugent AC, Milham MP, Bain EE, Mah L, Cannon DM, Marrett S, et al. Cortical abnormalities in bipolar disorder investigated with MRI and voxel-based morphometry. Neuroimage. 2006;30:485–497. doi: 10.1016/j.neuroimage.2005.09.029. [DOI] [PubMed] [Google Scholar]
- O’Brien J, Desmond P, Ames D, Schweitzer I, Harrigan S, Tress B. A magnetic resonance imaging study of white matter lesions in depression and Alzheimer’s disease. Br J Psychiatry. 1996;168:477–485. doi: 10.1192/bjp.168.4.477. [DOI] [PubMed] [Google Scholar]
- O’Brien JT, Lloyd A, McKeith I, Gholkar A, Ferrier N. A longitudinal study of hippocampal volume, cortisol levels, and cognition in older depressed subjects. Am J Psychiatry. 2004;161:2081–2090. doi: 10.1176/appi.ajp.161.11.2081. [DOI] [PubMed] [Google Scholar]
- Ohara K, Isoda H, Suzuki Y, Takehara Y, Ochiai M, Takeda H, et al. Proton magnetic resonance spectroscopy of the lenticular nuclei in bipolar I affective disorder. Psychiatry Res. 1998;84:55–60. doi: 10.1016/s0925-4927(98)00050-x. [DOI] [PubMed] [Google Scholar]
- Okugawa G, Nobuhara K, Takase K, Saito Y, Yoshimura M, Kinoshita T. Olanzapine increases grey and white matter volumes in the caudate nucleus of patients with schizophrenia. Neuropsychobiology. 2007;55:43–46. doi: 10.1159/000103575. [DOI] [PubMed] [Google Scholar]
- Ongur D, Drevets WC, Price JL. Glial reduction in the subgenual prefrontal cortex in mood disorders. Proc Natl Acad Sci U S A. 1998;95:13290–13295. doi: 10.1073/pnas.95.22.13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ongur D, Ferry AT, Price JL. Architectonic subdivision of the human orbital and medial prefrontal cortex. J Comp Neurol. 2003;460:425–449. doi: 10.1002/cne.10609. [DOI] [PubMed] [Google Scholar]
- Ongur D, Price JL. The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cereb Cortex. 2000a;10:206–219. doi: 10.1093/cercor/10.3.206. [DOI] [PubMed] [Google Scholar]
- Ongur D, Price JL. The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cereb Cortex. 2000b;10:206–219. doi: 10.1093/cercor/10.3.206. [DOI] [PubMed] [Google Scholar]
- Ovbiagele B, Saver JL. Cerebral white matter hyperintensities on MRI: Current concepts and therapeutic implications. Cerebrovasc Dis. 2006;22:83–90. doi: 10.1159/000093235. [DOI] [PubMed] [Google Scholar]
- Pantel J, Schroder J, Essig M, Popp D, Dech H, Knopp MV, et al. Quantitative magnetic resonance imaging in geriatric depression and primary degenerative dementia. J Affect Disord. 1997;42:69–83. doi: 10.1016/s0165-0327(96)00105-x. [DOI] [PubMed] [Google Scholar]
- Parashos IA, Tupler LA, Blitchington T, Krishnan KR. Magnetic-resonance morphometry in patients with major depression. Psychiatry Res. 1998;84:7–15. doi: 10.1016/s0925-4927(98)00042-0. [DOI] [PubMed] [Google Scholar]
- Parsey RV, Oquendo MA, Ogden RT, Olvet DM, Simpson N, Huang YY, et al. Altered serotonin 1A binding in major depression: a [carbonyl-C-11]WAY100635 positron emission tomography study. Biol Psychiatry. 2006;59:106–113. doi: 10.1016/j.biopsych.2005.06.016. [DOI] [PubMed] [Google Scholar]
- Pascual-Leone A, Catala MD, Pascual-Leone Pascual A. Lateralized effect of rapid-rate transcranial magnetic stimulation of the prefrontal cortex on mood. Neurology. 1996;46:499–502. doi: 10.1212/wnl.46.2.499. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Henry DB, Nadimpalli SS, O’Connor MM, Sweeney JA. Biological risk factors in pediatric bipolar disorder. Biol Psychiatry. 2006;60:936–941. doi: 10.1016/j.biopsych.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, O’Connor MM, Harral E, Sweeney JA. Affective neural circuitry during facial emotion processing in pediatric bipolar disorder. Biol Psychiatry. 2007;62:158–167. doi: 10.1016/j.biopsych.2006.07.011. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Brugha T, Fryers T. Size and burden of depressive disorders in Europe. Eur Neuropsychopharmacol. 2005;15:411–423. doi: 10.1016/j.euroneuro.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Pearlson GD, Barta PE, Powers RE, Menon RR, Richards SS, Aylward EH, et al. Ziskind-Somerfeld Research Award 1996. Medial and superior temporal gyral volumes and cerebral asymmetry in schizophrenia versus bipolar disorder. Biol Psychiatry. 1997;41:1–14. doi: 10.1016/s0006-3223(96)00373-3. [DOI] [PubMed] [Google Scholar]
- Pennington K, Beasley CL, Dicker P, Fagan A, English J, Pariante CM, et al. Prominent synaptic and metabolic abnormalities revealed by proteomic analysis of the dorsolateral prefrontal cortex in schizophrenia and bipolar disorder. Mol Psychiatry. 2007 doi: 10.1038/sj.mp.4002098. [DOI] [PubMed] [Google Scholar]
- Persaud R, Russow H, Harvey I, Lewis SW, Ron M, Murray RM, du Boulay G. Focal signal hyperintensities in schizophrenia. Schizophr Res. 1997;27:55–64. doi: 10.1016/S0920-9964(97)00060-1. [DOI] [PubMed] [Google Scholar]
- Pezawas L, Meyer-Lindenberg A, Drabant EM, Verchinski BA, Munoz KE, Kolachana BS, et al. 5-HTTLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nat Neurosci. 2005;8:828–834. doi: 10.1038/nn1463. [DOI] [PubMed] [Google Scholar]
- Pezawas L, Verchinski BA, Mattay VS, Callicott JH, Kolachana BS, Straub RE, et al. The brain-derived neurotrophic factor val66met polymorphism and variation in human cortical morphology. J Neurosci. 2004;24:10099–10102. doi: 10.1523/JNEUROSCI.2680-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips ML, Drevets WC, Rauch SL, Lane R. Neurobiology of emotion perception I: The neural basis of normal emotion perception. Biol Psychiatry. 2003;54:504–514. doi: 10.1016/s0006-3223(03)00168-9. [DOI] [PubMed] [Google Scholar]
- Pillai A. Decreased expression of Sprouty2 in the dorsolateral prefrontal cortex in schizophrenia and bipolar disorder: a correlation with BDNF expression. PLoS ONE. 2008;3:e1784. doi: 10.1371/journal.pone.0001784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillai JJ, Friedman L, Stuve TA, Trinidad S, Jesberger JA, Lewin JS, et al. Increased presence of white matter hyperintensities in adolescent patients with bipolar disorder. Psychiatry Res. 2002;114:51–56. doi: 10.1016/s0925-4927(01)00129-9. [DOI] [PubMed] [Google Scholar]
- Pillay SS, Renshaw PF, Bonello CM, Lafer BC, Fava M, Yurgelun-Todd D. A quantitative magnetic resonance imaging study of caudate and lenticular nucleus gray matter volume in primary unipolar major depression: relationship to treatment response and clinical severity. Psychiatry Res. 1998;84:61–74. doi: 10.1016/s0925-4927(98)00048-1. [DOI] [PubMed] [Google Scholar]
- Pini S, de Queiroz V, Pagnin D, Pezawas L, Angst J, Cassano GB, Wittchen HU. Prevalence and burden of bipolar disorders in European countries. Eur Neuropsychopharmacol. 2005;15:425–434. doi: 10.1016/j.euroneuro.2005.04.011. [DOI] [PubMed] [Google Scholar]
- Pizzagalli DA, Oakes TR, Fox AS, Chung MK, Larson CL, Abercrombie HC, et al. Functional but not structural subgenual prefrontal cortex abnormalities in melancholia. Mol Psychiatry. 2004;9:325, 393–405. doi: 10.1038/sj.mp.4001501. [DOI] [PubMed] [Google Scholar]
- Plomin R, Pedersen NL, McClearn GE, Nesselroade JR, Bergeman CS. EAS temperaments during the last half of the life span: twins reared apart and twins reared together. Psychol Aging. 1988;3:43–50. doi: 10.1037//0882-7974.3.1.43. [DOI] [PubMed] [Google Scholar]
- Pollack AE. Anatomy, physiology, and pharmacology of the basal ganglia. Neurol Clin. 2001;19:523–534. v. doi: 10.1016/s0733-8619(05)70032-3. [DOI] [PubMed] [Google Scholar]
- Poo MM. Neurotrophins as synaptic modulators. Nat Rev Neurosci. 2001;2:24–32. doi: 10.1038/35049004. [DOI] [PubMed] [Google Scholar]
- Posener JA, Wang L, Price JL, Gado MH, Province MA, Miller MI, et al. High-dimensional mapping of the hippocampus in depression. Am J Psychiatry. 2003;160:83–89. doi: 10.1176/appi.ajp.160.1.83. [DOI] [PubMed] [Google Scholar]
- Price J. Prefrontal Cortical networks Related to Visceral Function and Mood. Annals of the New York Academy of Sciences. 1999;877:383–396. doi: 10.1111/j.1749-6632.1999.tb09278.x. [DOI] [PubMed] [Google Scholar]
- Price JL. Definition of the orbital cortex in relation to specific connections with limbic and visceral structures and other cortical regions. Ann N Y Acad Sci. 2007;1121:54–71. doi: 10.1196/annals.1401.008. [DOI] [PubMed] [Google Scholar]
- Rabins PV, Pearlson GD, Aylward E, Kumar AJ, Dowell K. Cortical magnetic resonance imaging changes in elderly inpatients with major depression. Am J Psychiatry. 1991;148:617–620. doi: 10.1176/ajp.148.5.617. [DOI] [PubMed] [Google Scholar]
- Radley JJ, Morrison JH. Repeated stress and structural plasticity in the brain. Ageing Res Rev. 2005;4:271–287. doi: 10.1016/j.arr.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Radley JJ, Rocher AB, Miller M, Janssen WG, Liston C, Hof PR, et al. Repeated stress induces dendritic spine loss in the rat medial prefrontal cortex. Cereb Cortex. 2006;16:313–320. doi: 10.1093/cercor/bhi104. [DOI] [PubMed] [Google Scholar]
- Rainer MK, Mucke HA, Zehetmayer S, Krampla W, Kuselbauer T, Weissgram S, et al. Data from the VITA Study do not support the concept of vascular depression. Am J Geriatr Psychiatry. 2006;14:531–537. doi: 10.1097/01.JGP.0000218326.91287.66. [DOI] [PubMed] [Google Scholar]
- Rajkowska G, Miguel-Hidalgo JJ, Wei J, Dilley G, Pittman SD, Meltzer HY, et al. Morphometric evidence for neuronal and glial prefrontal cell pathology in major depression. Biol Psychiatry. 1999;45:1085–1098. doi: 10.1016/s0006-3223(99)00041-4. [DOI] [PubMed] [Google Scholar]
- Rao H, Gillihan SJ, Wang J, Korczykowski M, Sankoorikal GM, Kaercher KA, et al. Genetic variation in serotonin transporter alters resting brain function in healthy individuals. Biol Psychiatry. 2007;62:600–606. doi: 10.1016/j.biopsych.2006.11.028. [DOI] [PubMed] [Google Scholar]
- Reagan LP, McEwen BS. Controversies surrounding glucocorticoid-mediated cell death in the hippocampus. J Chem Neuroanat. 1997;13:149–167. doi: 10.1016/s0891-0618(97)00031-8. [DOI] [PubMed] [Google Scholar]
- Regenold WT, D’Agostino CA, Ramesh N, Hasnain M, Roys S, Gullapalli RP. Diffusion-weighted magnetic resonance imaging of white matter in bipolar disorder: a pilot study. Bipolar Disord. 2006;8:188–195. doi: 10.1111/j.1399-5618.2006.00281.x. [DOI] [PubMed] [Google Scholar]
- Regenold WT, Phatak P, Marano CM, Gearhart L, Viens CH, Hisley KC. Myelin staining of deep white matter in the dorsolateral prefrontal cortex in schizophrenia, bipolar disorder, and unipolar major depression. Psychiatry Res. 2007;151:179–188. doi: 10.1016/j.psychres.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Rich BA, Vinton DT, Roberson-Nay R, Hommer RE, Berghorst LH, McClure EB, et al. Limbic hyperactivation during processing of neutral facial expressions in children with bipolar disorder. Proc Natl Acad Sci U S A. 2006;103:8900–8905. doi: 10.1073/pnas.0603246103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson RG, Kubos KL, Starr LB, Rao K, Price TR. Mood disorders in stroke patients. Importance of location of lesion. Brain. 1984;107 (Pt 1):81–93. doi: 10.1093/brain/107.1.81. [DOI] [PubMed] [Google Scholar]
- Rocher C, Spedding M, Munoz C, Jay TM. Acute stress-induced changes in hippocampal/prefrontal circuits in rats: effects of antidepressants. Cereb Cortex. 2004;14:224–229. doi: 10.1093/cercor/bhg122. [DOI] [PubMed] [Google Scholar]
- Roozendaal B, Okuda S, Van der Zee EA, McGaugh JL. Glucocorticoid enhancement of memory requires arousal-induced noradrenergic activation in the basolateral amygdala. Proc Natl Acad Sci U S A. 2006;103:6741–6746. doi: 10.1073/pnas.0601874103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosso IM, Killgore WD, Cintron CM, Gruber SA, Tohen M, Yurgelun-Todd DA. Reduced amygdala volumes in first-episode bipolar disorder and correlation with cerebral white matter. Biol Psychiatry. 2007;61:743–749. doi: 10.1016/j.biopsych.2006.07.035. [DOI] [PubMed] [Google Scholar]
- Rottenberg J. Cardiac vagal control in depression: a critical analysis. Biol Psychol. 2007;74:200–211. doi: 10.1016/j.biopsycho.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Rowe DC. Environmental and genetic influences on dimensions of perceived parenting: A twin study. Developmental Psychology. 1981;30:32–43. [Google Scholar]
- Rusch BD, Abercrombie HC, Oakes TR, Schaefer SM, Davidson RJ. Hippocampal morphometry in depressed patients and control subjects: relations to anxiety symptoms. Biol Psychiatry. 2001;50:960–964. doi: 10.1016/s0006-3223(01)01248-3. [DOI] [PubMed] [Google Scholar]
- Rutter M. Gene-environment interdependence. Dev Sci. 2007;10:12–18. doi: 10.1111/j.1467-7687.2007.00557.x. [DOI] [PubMed] [Google Scholar]
- Ryan MM, Lockstone HE, Huffaker SJ, Wayland MT, Webster MJ, Bahn S. Gene expression analysis of bipolar disorder reveals downregulation of the ubiquitin cycle and alterations in synaptic genes. Mol Psychiatry. 2006;11:965–978. doi: 10.1038/sj.mp.4001875. [DOI] [PubMed] [Google Scholar]
- Rydmark I, Wahlberg K, Ghatan PH, Modell S, Nygren A, Ingvar M, et al. Neuroendocrine, cognitive and structural imaging characteristics of women on longterm sickleave with job stress-induced depression. Biol Psychiatry. 2006;60:867–873. doi: 10.1016/j.biopsych.2006.04.029. [DOI] [PubMed] [Google Scholar]
- Sackeim HA, Greenberg MS, Weiman AL, Gur RC, Hungerbuhler JP, Geschwind N. Hemispheric asymmetry in the expression of positive and negative emotions. Neurologic evidence. Arch Neurol. 1982;39:210–218. doi: 10.1001/archneur.1982.00510160016003. [DOI] [PubMed] [Google Scholar]
- Sah P, Faber ES, Lopez De Armentia M, Power J. The amygdaloid complex: anatomy and physiology. Physiol Rev. 2003;83:803–834. doi: 10.1152/physrev.00002.2003. [DOI] [PubMed] [Google Scholar]
- Salloway S. Clinical-pathological case conference: depression, behavior change, and subcortical dementia in a 57-year-old woman. J Neuropsychiatry Clin Neurosci. 1996;8:215–221. doi: 10.1176/jnp.8.2.215. [DOI] [PubMed] [Google Scholar]
- Salloway S, Malloy P, Kohn R, Gillard E, Duffy J, Rogg J, et al. MRI and neuropsychological differences in early- and late-life-onset geriatric depression. Neurology. 1996;46:1567–1574. doi: 10.1212/wnl.46.6.1567. [DOI] [PubMed] [Google Scholar]
- Sanches M, Roberts RL, Sassi RB, Axelson D, Nicoletti M, Brambilla P, et al. Developmental abnormalities in striatum in young bipolar patients: a preliminary study. Bipolar Disord. 2005a;7:153–158. doi: 10.1111/j.1399-5618.2004.00178.x. [DOI] [PubMed] [Google Scholar]
- Sanches M, Sassi RB, Axelson D, Nicoletti M, Brambilla P, Hatch JP, et al. Subgenual prefrontal cortex of child and adolescent bipolar patients: a morphometric magnetic resonance imaging study. Psychiatry Res. 2005b;138:43–49. doi: 10.1016/j.pscychresns.2004.11.004. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM, Uno H, Rebert CS, Finch CE. Hippocampal damage associated with prolonged glucocorticoid exposure in primates. J Neurosci. 1990;10:2897–2902. doi: 10.1523/JNEUROSCI.10-09-02897.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sassi RB, Brambilla P, Hatch JP, Nicoletti MA, Mallinger AG, Frank E, et al. Reduced left anterior cingulate volumes in untreated bipolar patients. Biol Psychiatry. 2004;56:467–475. doi: 10.1016/j.biopsych.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Sassi RB, Brambilla P, Nicoletti M, Mallinger AG, Frank E, Kupfer DJ, et al. White matter hyperintensities in bipolar and unipolar patients with relatively mild-to-moderate illness severity. J Affect Disord. 2003;77:237–245. doi: 10.1016/s0165-0327(02)00170-2. [DOI] [PubMed] [Google Scholar]
- Sato R, Bryan RN, Fried LP. Neuroanatomic and functional correlates of depressed mood: the Cardiovascular Health Study. Am J Epidemiol. 1999;150:919–929. doi: 10.1093/oxfordjournals.aje.a010100. [DOI] [PubMed] [Google Scholar]
- Savitz J, Solms M, Pietersen E, Ramesar R, Flor-Henry P. Dissociative identity disorder associated with mania and change in handedness. Cogn Behav Neurol. 2004;17:233–237. [PubMed] [Google Scholar]
- Savitz J, Solms M, Ramesar R. Neuropsychological dysfunction in bipolar affective disorder: a critical opinion. Bipolar Disord. 2005;7:216–235. doi: 10.1111/j.1399-5618.2005.00203.x. [DOI] [PubMed] [Google Scholar]
- Savitz J, van-der-Merwe L, Stein D, Solms M, Ramesar R. Neuropsychological Status of Bipolar Disorder Type I: The Impact of Psychosis. British Journal of Psychiatry. doi: 10.1192/bjp.bp.108.052001. in press. [DOI] [PubMed] [Google Scholar]
- Savitz J, van der Merwe L, Ramesar R. Dysthymic and anxiety-related personality traits in bipolar spectrum illness. J Affect Disord. 2008a;109:305–311. doi: 10.1016/j.jad.2007.12.006. [DOI] [PubMed] [Google Scholar]
- Savitz J, van der Merwe L, Ramesar R. Hypomanic, cyclothymic and hostile personality traits in bipolar spectrum illness: A family-based study. J Psychiatr Res. 2008b;42:920–929. doi: 10.1016/j.jpsychires.2007.10.011. [DOI] [PubMed] [Google Scholar]
- Savitz J, van der Merwe L, Solms M, Ramesar R. Lateralization of hand skill in bipolar affective disorder. Genes Brain Behav. 2007a;6:698–705. doi: 10.1111/j.1601-183X.2006.00299.x. [DOI] [PubMed] [Google Scholar]
- Savitz J, van der Merwe L, Solms M, Ramesar R. Neurocognitive function in an extended Afrikaner-ancestry family with affective illness. J Psychiatry Neurosci. 2007b;32:116–120. [PMC free article] [PubMed] [Google Scholar]
- Savitz J, van der Merwe L, Stein DJ, Solms M, Ramesar R. Genotype and childhood sexual trauma moderate neurocognitive performance: a possible role for brain-derived neurotrophic factor and apolipoprotein E variants. Biol Psychiatry. 2007c;62:391–399. doi: 10.1016/j.biopsych.2006.10.017. [DOI] [PubMed] [Google Scholar]
- Savitz JB, Ramesar RS. Genetic variants implicated in personality: a review of the more promising candidates. Am J Med Genet B Neuropsychiatr Genet. 2004;131:20–32. doi: 10.1002/ajmg.b.20155. [DOI] [PubMed] [Google Scholar]
- Savitz JB, Ramesar RS. Personality: is it a viable endophenotype for genetic studies of bipolar affective disorder? Bipolar Disord. 2006;8:322–337. doi: 10.1111/j.1399-5618.2006.00309.x. [DOI] [PubMed] [Google Scholar]
- Sax KW, Strakowski SM, Zimmerman ME, DelBello MP, Keck PE, Jr, Hawkins JM. Frontosubcortical neuroanatomy and the continuous performance test in mania. Am J Psychiatry. 1999;156:139–141. doi: 10.1176/ajp.156.1.139. [DOI] [PubMed] [Google Scholar]
- Saxena S, Brody AL, Ho ML, Zohrabi N, Maidment KM, Baxter LR., Jr Differential brain metabolic predictors of response to paroxetine in obsessive-compulsive disorder versus major depression. Am J Psychiatry. 2003;160:522–532. doi: 10.1176/appi.ajp.160.3.522. [DOI] [PubMed] [Google Scholar]
- Schwartz JM, Baxter LR, Jr, Mazziotta JC, Gerner RH, Phelps ME. The differential diagnosis of depression. Relevance of positron emission tomography studies of cerebral glucose metabolism to the bipolar-unipolar dichotomy. Jama. 1987;258:1368–1374. doi: 10.1001/jama.258.10.1368. [DOI] [PubMed] [Google Scholar]
- Sequeira A, Gwadry FG, Ffrench-Mullen JM, Canetti L, Gingras Y, Casero RA, Jr, et al. Implication of SSAT by gene expression and genetic variation in suicide and major depression. Arch Gen Psychiatry. 2006;63:35–48. doi: 10.1001/archpsyc.63.1.35. [DOI] [PubMed] [Google Scholar]
- Shah PJ, Ebmeier KP, Glabus MF, Goodwin GM. Cortical grey matter reductions associated with treatment-resistant chronic unipolar depression. Controlled magnetic resonance imaging study. Br J Psychiatry. 1998;172:527–532. doi: 10.1192/bjp.172.6.527. [DOI] [PubMed] [Google Scholar]
- Shao L, Vawter MP. Shared Gene Expression Alterations in Schizophrenia and Bipolar Disorder. Biol Psychiatry. 2008 doi: 10.1016/j.biopsych.2007.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma V, Menon R, Carr TJ, Densmore M, Mazmanian D, Williamson PC. An MRI study of subgenual prefrontal cortex in patients with familial and non-familial bipolar I disorder. J Affect Disord. 2003;77:167–171. doi: 10.1016/s0165-0327(02)00109-x. [DOI] [PubMed] [Google Scholar]
- Sheline YI, Barch DM, Donnelly JM, Ollinger JM, Snyder AZ, Mintun MA. Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: an fMRI study. Biol Psychiatry. 2001;50:651–658. doi: 10.1016/s0006-3223(01)01263-x. [DOI] [PubMed] [Google Scholar]
- Sheline YI, Gado MH, Price JL. Amygdala core nuclei volumes are decreased in recurrent major depression. Neuroreport. 1998;9:2023–2028. doi: 10.1097/00001756-199806220-00021. [DOI] [PubMed] [Google Scholar]
- Sheline YI, Sanghavi M, Mintun MA, Gado MH. Depression duration but not age predicts hippocampal volume loss in medically healthy women with recurrent major depression. J Neurosci. 1999;19:5034–5043. doi: 10.1523/JNEUROSCI.19-12-05034.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheline YI, Wang PW, Gado MH, Csernansky JG, Vannier MW. Hippocampal atrophy in recurrent major depression. Proc Natl Acad Sci U S A. 1996;93:3908–3913. doi: 10.1073/pnas.93.9.3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shulman RG, Rothman DL, Behar KL, Hyder F. Energetic basis of brain activity: implications for neuroimaging. Trends Neurosci. 2004;27:489–495. doi: 10.1016/j.tins.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Shumake J, Conejo-Jimenez N, Gonzalez-Pardo H, Gonzalez-Lima F. Brain differences in newborn rats predisposed to helpless and depressive behavior. Brain Res. 2004;1030:267–276. doi: 10.1016/j.brainres.2004.10.015. [DOI] [PubMed] [Google Scholar]
- Shumake J, Edwards E, Gonzalez-Lima F. Dissociation of septo-hippocampal metabolism in the congenitally helpless rat. Neuroscience. 2002;114:373–377. doi: 10.1016/s0306-4522(02)00297-x. [DOI] [PubMed] [Google Scholar]
- Shumake J, Poremba A, Edwards E, Gonzalez-Lima F. Congenital helpless rats as a genetic model for cortex metabolism in depression. Neuroreport. 2000;11:3793–3798. doi: 10.1097/00001756-200011270-00040. [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Steinhauer SR, Thase ME, Stenger VA, Carter CS. Can’t shake that feeling: event-related fMRI assessment of sustained amygdala activity in response to emotional information in depressed individuals. Biol Psychiatry. 2002;51:693–707. doi: 10.1016/s0006-3223(02)01314-8. [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Thompson W, Carter CS, Steinhauer SR, Thase ME. Increased amygdala and decreased dorsolateral prefrontal BOLD responses in unipolar depression: related and independent features. Biol Psychiatry. 2007;61:198–209. doi: 10.1016/j.biopsych.2006.05.048. [DOI] [PubMed] [Google Scholar]
- Silberberg G, Levit A, Collier D, St Clair D, Munro J, Kerwin RW, et al. Stargazin involvement with bipolar disorder and response to lithium treatment. Pharmacogenet Genomics. 2008;18:403–412. doi: 10.1097/FPC.0b013e3282f974ca. [DOI] [PubMed] [Google Scholar]
- Silberman EK, Weingartner H. Hemispheric lateralization of functions related to emotion. Brain Cogn. 1986;5:322–353. doi: 10.1016/0278-2626(86)90035-7. [DOI] [PubMed] [Google Scholar]
- Silverstone T, McPherson H, Li Q, Doyle T. Deep white matter hyperintensities in patients with bipolar depression, unipolar depression and age-matched control subjects. Bipolar Disord. 2003;5:53–57. doi: 10.1034/j.1399-5618.2003.01208.x. [DOI] [PubMed] [Google Scholar]
- Simpson SW, Baldwin RC, Burns A, Jackson A. Regional cerebral volume measurements in late-life depression: relationship to clinical correlates, neuropsychological impairment and response to treatment. Int J Geriatr Psychiatry. 2001;16:469–476. doi: 10.1002/gps.364. [DOI] [PubMed] [Google Scholar]
- Slaughter JR, Martens MP, Slaughter KA. Depression and Huntington’s disease: prevalence, clinical manifestations, etiology, and treatment. CNS Spectr. 2001;6:306–326. doi: 10.1017/s109285290002201x. [DOI] [PubMed] [Google Scholar]
- Sloviter RS. Hippocampal pathology and pathophysiology in temporal lobe epilepsy. Neurologia. 1996;11(Suppl 4):29–32. [PubMed] [Google Scholar]
- Smith GS, Kramer E, Hermann CR, Goldberg S, Ma Y, Dhawan V, et al. Acute and chronic effects of citalopram on cerebral glucose metabolism in geriatric depression. Am J Geriatr Psychiatry. 2002;10:715–723. [PubMed] [Google Scholar]
- Smith KA, Morris JS, Friston KJ, Cowen PJ, Dolan RJ. Brain mechanisms associated with depressive relapse and associated cognitive impairment following acute tryptophan depletion. Br J Psychiatry. 1999;174:525–529. doi: 10.1192/bjp.174.6.525. [DOI] [PubMed] [Google Scholar]
- Smolin B, Klein E, Levy Y, Ben-Shachar D. Major depression as a disorder of serotonin resistance: inference from diabetes mellitus type II. Int J Neuropsychopharmacol. 2007;10:839–850. doi: 10.1017/S1461145707007559. [DOI] [PubMed] [Google Scholar]
- Sneed JR, Rindskopf D, Steffens DC, Krishnan KR, Roose SP. The vascular depression subtype: evidence of internal validity. Biol Psychiatry. 2008;64:491–497. doi: 10.1016/j.biopsych.2008.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares JC, Kochunov P, Monkul ES, Nicoletti MA, Brambilla P, Sassi RB, et al. Structural brain changes in bipolar disorder using deformation field morphometry. Neuroreport. 2005;16:541–544. doi: 10.1097/00001756-200504250-00004. [DOI] [PubMed] [Google Scholar]
- Sokolov BP. Oligodendroglial abnormalities in schizophrenia, mood disorders and substance abuse. Comorbidity, shared traits, or molecular phenocopies? Int J Neuropsychopharmacol. 2007:1–9. doi: 10.1017/S1461145706007322. [DOI] [PubMed] [Google Scholar]
- Son H, Yu IT, Hwang SJ, Kim JS, Lee SH, Lee YS, Kaang BK. Lithium enhances long-term potentiation independently of hippocampal neurogenesis in the rat dentate gyrus. J Neurochem. 2003;85:872–881. doi: 10.1046/j.1471-4159.2003.01725.x. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Byrum CE, McQuoid DR, Greenberg DL, Payne ME, Blitchington TF, et al. Hippocampal volume in geriatric depression. Biol Psychiatry. 2000;48:301–309. doi: 10.1016/s0006-3223(00)00829-5. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Helms MJ, Krishnan KR, Burke GL. Cerebrovascular disease and depression symptoms in the cardiovascular health study. Stroke. 1999;30:2159–2166. doi: 10.1161/01.str.30.10.2159. [DOI] [PubMed] [Google Scholar]
- Steffens DC, McQuoid DR, Welsh-Bohmer KA, Krishnan KR. Left orbital frontal cortex volume and performance on the benton visual retention test in older depressives and controls. Neuropsychopharmacology. 2003;28:2179–2183. doi: 10.1038/sj.npp.1300285. [DOI] [PubMed] [Google Scholar]
- Steiner J, Bielau H, Brisch R, Danos P, Ullrich O, Mawrin C, et al. Immunological aspects in the neurobiology of suicide: elevated microglial density in schizophrenia and depression is associated with suicide. J Psychiatr Res. 2008;42:151–157. doi: 10.1016/j.jpsychires.2006.10.013. [DOI] [PubMed] [Google Scholar]
- Stewart CA, Reid IC. Repeated ECS and fluoxetine administration have equivalent effects on hippocampal synaptic plasticity. Psychopharmacology (Berl) 2000;148:217–223. doi: 10.1007/s002130050045. [DOI] [PubMed] [Google Scholar]
- Stockmeier CA, Mahajan GJ, Konick LC, Overholser JC, Jurjus GJ, Meltzer HY, et al. Cellular changes in the postmortem hippocampus in major depression. Biol Psychiatry. 2004;56:640–650. doi: 10.1016/j.biopsych.2004.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strakowski SM, Adler CM, Holland SK, Mills NP, DelBello MP, Eliassen JC. Abnormal FMRI brain activation in euthymic bipolar disorder patients during a counting Stroop interference task. Am J Psychiatry. 2005;162:1697–1705. doi: 10.1176/appi.ajp.162.9.1697. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, DelBello MP, Sax KW, Zimmerman ME, Shear PK, Hawkins JM, Larson ER. Brain magnetic resonance imaging of structural abnormalities in bipolar disorder. Arch Gen Psychiatry. 1999;56:254–260. doi: 10.1001/archpsyc.56.3.254. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, DelBello MP, Zimmerman ME, Getz GE, Mills NP, Ret J, et al. Ventricular and periventricular structural volumes in first- versus multiple-episode bipolar disorder. Am J Psychiatry. 2002;159:1841–1847. doi: 10.1176/appi.ajp.159.11.1841. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, Woods BT, Tohen M, Wilson DR, Douglass AW, Stoll AL. MRI subcortical signal hyperintensities in mania at first hospitalization. Biol Psychiatry. 1993;33:204–206. doi: 10.1016/0006-3223(93)90140-9. [DOI] [PubMed] [Google Scholar]
- Strasser HC, Lilyestrom J, Ashby ER, Honeycutt NA, Schretlen DJ, Pulver AE, et al. Hippocampal and ventricular volumes in psychotic and nonpsychotic bipolar patients compared with schizophrenia patients and community control subjects: a pilot study. Biol Psychiatry. 2005;57:633–639. doi: 10.1016/j.biopsych.2004.12.009. [DOI] [PubMed] [Google Scholar]
- Sullivan RM, Gratton A. Lateralized effects of medial prefrontal cortex lesions on neuroendocrine and autonomic stress responses in rats. J Neurosci. 1999;19:2834–2840. doi: 10.1523/JNEUROSCI.19-07-02834.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan RM, Gratton A. Behavioral effects of excitotoxic lesions of ventral medial prefrontal cortex in the rat are hemisphere-dependent. Brain Res. 2002;927:69–79. doi: 10.1016/s0006-8993(01)03328-5. [DOI] [PubMed] [Google Scholar]
- Sullivan RM, Szechtman H. Asymmetrical influence of mesocortical dopamine depletion on stress ulcer development and subcortical dopamine systems in rats: implications for psychopathology. Neuroscience. 1995;65:757–766. doi: 10.1016/0306-4522(94)00531-9. [DOI] [PubMed] [Google Scholar]
- Surguladze S, Brammer MJ, Keedwell P, Giampietro V, Young AW, Travis MJ, et al. A differential pattern of neural response toward sad versus happy facial expressions in major depressive disorder. Biol Psychiatry. 2005;57:201–209. doi: 10.1016/j.biopsych.2004.10.028. [DOI] [PubMed] [Google Scholar]
- Surtees PG, Wainwright NW, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Depression and ischemic heart disease mortality: evidence from the EPIC-Norfolk United Kingdom prospective cohort study. Am J Psychiatry. 2008;165:515–523. doi: 10.1176/appi.ajp.2007.07061018. [DOI] [PubMed] [Google Scholar]
- Swayze VW, 2nd, Andreasen NC, Alliger RJ, Ehrhardt JC, Yuh WT. Structural brain abnormalities in bipolar affective disorder. Ventricular enlargement and focal signal hyperintensities. Arch Gen Psychiatry. 1990;47:1054–1059. doi: 10.1001/archpsyc.1990.01810230070011. [DOI] [PubMed] [Google Scholar]
- Swayze VW, 2nd, Andreasen NC, Alliger RJ, Yuh WT, Ehrhardt JC. Subcortical and temporal structures in affective disorder and schizophrenia: a magnetic resonance imaging study. Biol Psychiatry. 1992;31:221–240. doi: 10.1016/0006-3223(92)90046-3. [DOI] [PubMed] [Google Scholar]
- Szatmari E, Kalita KB, Kharebava G, Hetman M. Role of kinase suppressor of Ras-1 in neuronal survival signaling by extracellular signal-regulated kinase 1/2. J Neurosci. 2007;27:11389–11400. doi: 10.1523/JNEUROSCI.3473-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szeszko PR, Lipsky R, Mentschel C, Robinson D, Gunduz-Bruce H, Sevy S, et al. Brain-derived neurotrophic factor val66met polymorphism and volume of the hippocampal formation. Mol Psychiatry. 2005;10:631–636. doi: 10.1038/sj.mp.4001656. [DOI] [PubMed] [Google Scholar]
- Tae WS, Kim SS, Lee KU, Nam EC, Kim KW. Validation of hippocampal volumes measured using a manual method and two automated methods (FreeSurfer and IBASPM) in chronic major depressive disorder. Neuroradiology. 2008;50:569–581. doi: 10.1007/s00234-008-0383-9. [DOI] [PubMed] [Google Scholar]
- Talbot PS, Cooper SJ. Anterior cingulate and subgenual prefrontal blood flow changes following tryptophan depletion in healthy males. Neuropsychopharmacology. 2006;31:1757–1767. doi: 10.1038/sj.npp.1301022. [DOI] [PubMed] [Google Scholar]
- Tang Y, Wang F, Xie G, Liu J, Li L, Su L, et al. Reduced ventral anterior cingulate and amygdala volumes in medication-naive females with major depressive disorder: A voxel-based morphometric magnetic resonance imaging study. Psychiatry Res. 2007;156:83–86. doi: 10.1016/j.pscychresns.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Taylor Tavares JV, Clark L, Furey ML, Williams GB, Sahakian BJ, Drevets WC. Neural basis of abnormal response to negative feedback in unmedicated mood disorders. Neuroimage. 2008;42:1118–1126. doi: 10.1016/j.neuroimage.2008.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor WD, MacFall JR, Payne ME, McQuoid DR, Steffens DC, Provenzale JM, Krishnan RR. Greater MRI lesion volumes in elderly depressed subjects than in control subjects. Psychiatry Res. 2005;139:1–7. doi: 10.1016/j.pscychresns.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Taylor WD, Steffens DC, McQuoid DR, Payne ME, Lee SH, Lai TJ, Krishnan KR. Smaller orbital frontal cortex volumes associated with functional disability in depressed elders. Biol Psychiatry. 2003;53:144–149. doi: 10.1016/s0006-3223(02)01490-7. [DOI] [PubMed] [Google Scholar]
- Tekin S, Cummings JL. Frontal-subcortical neuronal circuits and clinical neuropsychiatry: an update. J Psychosom Res. 2002;53:647–654. doi: 10.1016/s0022-3999(02)00428-2. [DOI] [PubMed] [Google Scholar]
- Thomas AJ, O’Brien JT, Barber R, McMeekin W, Perry R. A neuropathological study of periventricular white matter hyperintensities in major depression. J Affect Disord. 2003;76:49–54. doi: 10.1016/s0165-0327(02)00064-2. [DOI] [PubMed] [Google Scholar]
- Thomas AJ, O’Brien JT, Davis S, Ballard C, Barber R, Kalaria RN, Perry RH. Ischemic basis for deep white matter hyperintensities in major depression: a neuropathological study. Arch Gen Psychiatry. 2002;59:785–792. doi: 10.1001/archpsyc.59.9.785. [DOI] [PubMed] [Google Scholar]
- Thomas KM, Drevets WC, Dahl RE, Ryan ND, Birmaher B, Eccard CH, et al. Amygdala response to fearful faces in anxious and depressed children. Arch Gen Psychiatry. 2001;58:1057–1063. doi: 10.1001/archpsyc.58.11.1057. [DOI] [PubMed] [Google Scholar]
- Tkachev D, Mimmack ML, Ryan MM, Wayland M, Freeman T, Jones PB, et al. Oligodendrocyte dysfunction in schizophrenia and bipolar disorder. Lancet. 2003;362:798–805. doi: 10.1016/S0140-6736(03)14289-4. [DOI] [PubMed] [Google Scholar]
- Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ. Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat Neurosci. 2006;9:519–525. doi: 10.1038/nn1659. [DOI] [PubMed] [Google Scholar]
- Tupler LA, Krishnan KR, McDonald WM, Dombeck CB, D’Souza S, Steffens DC. Anatomic location and laterality of MRI signal hyperintensities in late-life depression. J Psychosom Res. 2002;53:665–676. doi: 10.1016/s0022-3999(02)00425-7. [DOI] [PubMed] [Google Scholar]
- Uno H, Tarara R, Else JG, Suleman MA, Sapolsky RM. Hippocampal damage associated with prolonged and fatal stress in primates. J Neurosci. 1989;9:1705–1711. doi: 10.1523/JNEUROSCI.09-05-01705.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uranova NA, Vostrikov VM, Orlovskaya DD, Rachmanova VI. Oligodendroglial density in the prefrontal cortex in schizophrenia and mood disorders: a study from the Stanley Neuropathology Consortium. Schizophr Res. 2004;67:269–275. doi: 10.1016/S0920-9964(03)00181-6. [DOI] [PubMed] [Google Scholar]
- Utter AA, Basso MA. The basal ganglia: An overview of circuits and function. Neurosci Biobehav Rev. 2007 doi: 10.1016/j.neubiorev.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Vakili K, Pillay SS, Lafer B, Fava M, Renshaw PF, Bonello-Cintron CM, Yurgelun-Todd DA. Hippocampal volume in primary unipolar major depression: a magnetic resonance imaging study. Biol Psychiatry. 2000;47:1087–1090. doi: 10.1016/s0006-3223(99)00296-6. [DOI] [PubMed] [Google Scholar]
- van der Veen FM, Evers EA, Deutz NE, Schmitt JA. Effects of acute tryptophan depletion on mood and facial emotion perception related brain activation and performance in healthy women with and without a family history of depression. Neuropsychopharmacology. 2007;32:216–224. doi: 10.1038/sj.npp.1301212. [DOI] [PubMed] [Google Scholar]
- Velakoulis D, Wood SJ, Wong MT, McGorry PD, Yung A, Phillips L, et al. Hippocampal and amygdala volumes according to psychosis stage and diagnosis: a magnetic resonance imaging study of chronic schizophrenia, first-episode psychosis, and ultra-high-risk individuals. Arch Gen Psychiatry. 2006;63:139–149. doi: 10.1001/archpsyc.63.2.139. [DOI] [PubMed] [Google Scholar]
- Versluis CE, van der Mast RC, van Buchem MA, Bollen EL, Blauw GJ, Eekhof JA, et al. Progression of cerebral white matter lesions is not associated with development of depressive symptoms in elderly subjects at risk of cardiovascular disease: The PROSPER Study. Int J Geriatr Psychiatry. 2006;21:375–381. doi: 10.1002/gps.1477. [DOI] [PubMed] [Google Scholar]
- Vidal-Gonzalez I, Vidal-Gonzalez B, Rauch SL, Quirk GJ. Microstimulation reveals opposing influences of prelimbic and infralimbic cortex on the expression of conditioned fear. Learn Mem. 2006;13:728–733. doi: 10.1101/lm.306106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Videbech P, Ravnkilde B, Pedersen AR, Egander A, Landbo B, Rasmussen NA, et al. The Danish PET/depression project: PET findings in patients with major depression. Psychol Med. 2001;31:1147–1158. doi: 10.1017/s0033291701004469. [DOI] [PubMed] [Google Scholar]
- von Gunten A, Fox NC, Cipolotti L, Ron MA. A volumetric study of hippocampus and amygdala in depressed patients with subjective memory problems. J Neuropsychiatry Clin Neurosci. 2000;12:493–498. doi: 10.1176/jnp.12.4.493. [DOI] [PubMed] [Google Scholar]
- Vostrikov VM, Uranova NA, Orlovskaya DD. Deficit of perineuronal oligodendrocytes in the prefrontal cortex in schizophrenia and mood disorders. Schizophr Res. 2007;94:273–280. doi: 10.1016/j.schres.2007.04.014. [DOI] [PubMed] [Google Scholar]
- Vyas A, Mitra R, Shankaranarayana Rao BS, Chattarji S. Chronic stress induces contrasting patterns of dendritic remodeling in hippocampal and amygdaloid neurons. J Neurosci. 2002;22:6810–6818. doi: 10.1523/JNEUROSCI.22-15-06810.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vythilingam M, Heim C, Newport J, Miller AH, Anderson E, Bronen R, et al. Childhood trauma associated with smaller hippocampal volume in women with major depression. Am J Psychiatry. 2002;159:2072–2080. doi: 10.1176/appi.ajp.159.12.2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vythilingam M, Luckenbaugh DA, Lam T, Morgan CA, 3rd, Lipschitz D, Charney DS, et al. Smaller head of the hippocampus in Gulf War-related posttraumatic stress disorder. Psychiatry Res. 2005;139:89–99. doi: 10.1016/j.pscychresns.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Wassertheil-Smoller S, Shumaker S, Ockene J, Talavera GA, Greenland P, Cochrane B, et al. Depression and cardiovascular sequelae in postmenopausal women. The Women’s Health Initiative (WHI) Arch Intern Med. 2004;164:289–298. doi: 10.1001/archinte.164.3.289. [DOI] [PubMed] [Google Scholar]
- Watanabe Y, Gould E, Daniels DC, Cameron H, McEwen BS. Tianeptine attenuates stress-induced morphological changes in the hippocampus. Eur J Pharmacol. 1992;222:157–162. doi: 10.1016/0014-2999(92)90830-w. [DOI] [PubMed] [Google Scholar]
- Watkins PC, Mathews A, Williamson DA, Fuller RD. Mood-congruent memory in depression: emotional priming or elaboration? J Abnorm Psychol. 1992;101:581–586. doi: 10.1037//0021-843x.101.3.581. [DOI] [PubMed] [Google Scholar]
- Wessa M, Houenou J, Paillere-Martinot ML, Berthoz S, Artiges E, Leboyer M, Martinot JL. Fronto-striatal overactivation in euthymic bipolar patients during an emotional go/nogo task. Am J Psychiatry. 2007;164:638–646. doi: 10.1176/ajp.2007.164.4.638. [DOI] [PubMed] [Google Scholar]
- Wilke M, Kowatch RA, DelBello MP, Mills NP, Holland SK. Voxel-based morphometry in adolescents with bipolar disorder: first results. Psychiatry Res. 2004;131:57–69. doi: 10.1016/j.pscychresns.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Woods BT, Yurgelun-Todd D, Mikulis D, Pillay SS. Age-related MRI abnormalities in bipolar illness: a clinical study. Biol Psychiatry. 1995;38:846–847. doi: 10.1016/0006-3223(95)00363-0. [DOI] [PubMed] [Google Scholar]
- Wu J, Buchsbaum MS, Gillin JC, Tang C, Cadwell S, Wiegand M, et al. Prediction of antidepressant effects of sleep deprivation by metabolic rates in the ventral anterior cingulate and medial prefrontal cortex. Am J Psychiatry. 1999;156:1149–1158. doi: 10.1176/ajp.156.8.1149. [DOI] [PubMed] [Google Scholar]
- Wu JC, Buchsbaum MS, Johnson JC, Hershey TG, Wagner EA, Teng C, Lottenberg S. Magnetic resonance and positron emission tomography imaging of the corpus callosum: size, shape and metabolic rate in unipolar depression. J Affect Disord. 1993;28:15–25. doi: 10.1016/0165-0327(93)90073-s. [DOI] [PubMed] [Google Scholar]
- Xu Y, Ku B, Tie L, Yao H, Jiang W, Ma X, Li X. Curcumin reverses the effects of chronic stress on behavior, the HPA axis, BDNF expression and phosphorylation of CREB. Brain Res. 2006;1122:56–64. doi: 10.1016/j.brainres.2006.09.009. [DOI] [PubMed] [Google Scholar]
- Yang Q, Huang X, Hong N, Yu X. White matter microstructural abnormalities in late-life depression. Int Psychogeriatr. 2007:1–10. doi: 10.1017/S1041610207004875. [DOI] [PubMed] [Google Scholar]
- Yasar AS, Monkul ES, Sassi RB, Axelson D, Brambilla P, Nicoletti MA, et al. MRI study of corpus callosum in children and adolescents with bipolar disorder. Psychiatry Res. 2006;146:83–85. doi: 10.1016/j.pscychresns.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Lyoo IK, Liddle P, Renshaw PF, Wan D, Lam RW, Hwang J. A magnetic resonance imaging study of mood stabilizer- and neuroleptic-naive first-episode mania. Bipolar Disord. 2007;9:693–697. doi: 10.1111/j.1399-5618.2007.00414.x. [DOI] [PubMed] [Google Scholar]
- Yucel K, McKinnon MC, Chahal R, Taylor VH, Macdonald K, Joffe R, Macqueen GM. Anterior Cingulate Volumes in Never-Treated Patients with Major Depressive Disorder. Neuropsychopharmacology. 2008 doi: 10.1038/npp.2008.40. [DOI] [PubMed] [Google Scholar]
- Yucel K, Taylor VH, McKinnon MC, Macdonald K, Alda M, Young LT, Macqueen GM. Bilateral Hippocampal Volume Increase in Patients with Bipolar Disorder and Short-term Lithium Treatment. Neuropsychopharmacology. 2007 doi: 10.1038/sj.npp.1301405. [DOI] [PubMed] [Google Scholar]
- Yurgelun-Todd DA, Gruber SA, Kanayama G, Killgore WD, Baird AA, Young AD. fMRI during affect discrimination in bipolar affective disorder. Bipolar Disord. 2000;2:237–248. doi: 10.1034/j.1399-5618.2000.20304.x. [DOI] [PubMed] [Google Scholar]
- Yurgelun-Todd DA, Silveri MM, Gruber SA, Rohan ML, Pimentel PJ. White matter abnormalities observed in bipolar disorder: a diffusion tensor imaging study. Bipolar Disord. 2007;9:504–512. doi: 10.1111/j.1399-5618.2007.00395.x. [DOI] [PubMed] [Google Scholar]
- Zanetti MV, Schaufelberger MS, de Castro CC, Menezes PR, Scazufca M, McGuire PK, et al. White-matter hyperintensities in first-episode psychosis. Br J Psychiatry. 2008;193:25–30. doi: 10.1192/bjp.bp.107.038901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarate CA, Jr, Singh JB, Carlson PJ, Quiroz J, Jolkovsky L, Luckenbaugh DA, Manji HK. Efficacy of a protein kinase C inhibitor (tamoxifen) in the treatment of acute mania. a pilot study. Bipolar Disord. 2007;9:561–570. doi: 10.1111/j.1399-5618.2007.00530.x. [DOI] [PubMed] [Google Scholar]
- Zimmerman ME, DelBello MP, Getz GE, Shear PK, Strakowski SM. Anterior cingulate subregion volumes and executive function in bipolar disorder. Bipolar Disord. 2006;8:281–288. doi: 10.1111/j.1399-5618.2006.00298.x. [DOI] [PubMed] [Google Scholar]
- Zinkstok J, Schmitz N, van Amelsvoort T, Moeton M, Baas F, Linszen D. Genetic variation in COMT and PRODH is associated with brain anatomy in patients with schizophrenia. Genes Brain Behav. 2007 doi: 10.1111/j.1601-183X.2007.00326.x. [DOI] [PubMed] [Google Scholar]
- Zipursky RB, Seeman MV, Bury A, Langevin R, Wortzman G, Katz R. Deficits in gray matter volume are present in schizophrenia but not bipolar disorder. Schizophr Res. 1997;26:85–92. doi: 10.1016/s0920-9964(97)00042-x. [DOI] [PubMed] [Google Scholar]
- Zubenko GS, Hughes HB, 3rd, Maher BS, Stiffler JS, Zubenko WN, Marazita ML. Genetic linkage of region containing the CREB1 gene to depressive disorders in women from families with recurrent, early-onset, major depression. Am J Med Genet. 2002;114:980–987. doi: 10.1002/ajmg.b.10933. [DOI] [PubMed] [Google Scholar]
- Zubenko GS, Sullivan P, Nelson JP, Belle SH, Huff FJ, Wolf GL. Brain imaging abnormalities in mental disorders of late life. Arch Neurol. 1990;47:1107–1111. doi: 10.1001/archneur.1990.00530100075016. [DOI] [PubMed] [Google Scholar]