Abstract
Objectives
Although osteoporosis treatment with a combination of calcium, vitamin D (Cal+D) and an antiresorptive or bone-forming drug can dramatically reduce fracture risk, rates of treatment following hip fracture remain low. In-hospital initiation of recommended medications has improved outcomes in heart disease; hospitalization for hip fracture may represent a similar opportunity for improvement. Our objective was to examine rates of in-hospital treatment with 1) Cal+D and 2) antiresorptive or bone-forming medications in patients hospitalized for hip fractures.
Design, Setting, Participants and Measurements
Using pharmacy and discharge records from Perspective, a database developed to measure quality and health care utilization, we examined in-hospital osteoporosis treatment in 51,346 patients over age 65 hospitalized for osteoporotic hip fracture at 318 hospitals between October 2003 and September 2005. Our main outcome measures were the in-hospital administration of 1) Cal+D and 2) antiresorptive or bone-forming medications.
Results
3,405 patients (6.6%) received Cal+D anytime after a procedure to correct femoral fracture. 3,763 patients (7.3%) received antiresorptive or bone-forming medications. Only 1023 patients (2%) were prescribed ideal therapy, receiving Cal+D and an antiresorptive or bone-forming medication. Treatment rates remained low across virtually all patient, provider, and hospital level characteristics. The strongest predictor of treatment with Cal+D was the receipt of an antiresorptive or bone-forming medication (Adjusted OR=5.50, 95% CI: 4.84–6.25); however, only 27% of patients who received these medications also received Cal+D.
Conclusion
Rates of in-hospital initiation of osteoporosis treatment for hip fracture patients are very low and may represent an opportunity to improve care.
Keywords: Osteoporosis, Hip Fracture, Calcium, Vitamin D
INTRODUCTION
Osteoporotic hip fractures are common, disabling, and identify a group of older Americans who are at high risk for future fractures. Of the estimated 300,000 cases of hip fracture in the US annually, (1) one in four will require long-term nursing home care (2, 3) and one in five will die in the year following fracture. (4) Hip fractures are also a potent risk factor for future fractures. Patients who suffer a hip fracture are two to four times more likely to have a recurrent hip fracture, with ten percent having another fracture within one year. (5)
Although guideline-recommended osteoporosis treatment (2, 3) with a combination of calcium, vitamin D (Cal+D) and antiresorptive drugs can dramatically reduce fracture risk by up to 50%, (6–8) rates of treatment following hip fracture are low. (9–12) Previous studies have shown improved rates of osteoporosis treatment using multidisciplinary in-hospital consultations and case managers to encourage outpatient primary care physicians to initiate treatment. (13–19) However, these interventions have not been widely adopted, resulting in continuing low rates of osteoporosis treatment. (11, 12, 20, 21)
One intervention that may improve osteoporosis treatment rates is the in-hospital initiation of osteoporosis medications for hip fracture patients. (15, 16, 18, 20) Studies in acute coronary syndromes and heart failure have found that in-hospital initiation of medications improves long-term compliance and mortality. (22, 23) Furthermore, in-hospital pneumococcal vaccination and smoking cessation counseling highlight the effectiveness of using the hospital setting to identify and initiate treatment for high-risk populations. (24, 25) Hospitalization for hip fracture may represent a similar opportunity to identify high-risk patients with osteoporosis and initiate treatment. (13–20) Because previous studies have generally focused on the outpatient initiation of osteoporosis treatment, (9–20) the rates of in-hospital initiation of osteoporosis treatment after hip fracture are unknown.
Our objective was to examine the rates of in-hospital treatment with Cal+D in a large, national cohort of patients hospitalized for osteoporotic hip fractures and identify factors associated with non-treatment. We also examined the rates and predictors of treatment with antiresorptive and bone-forming medications, including bisphosphonates, estrogen, raloxifene, teriparatide and calcitonin.
METHODS
Setting and subjects
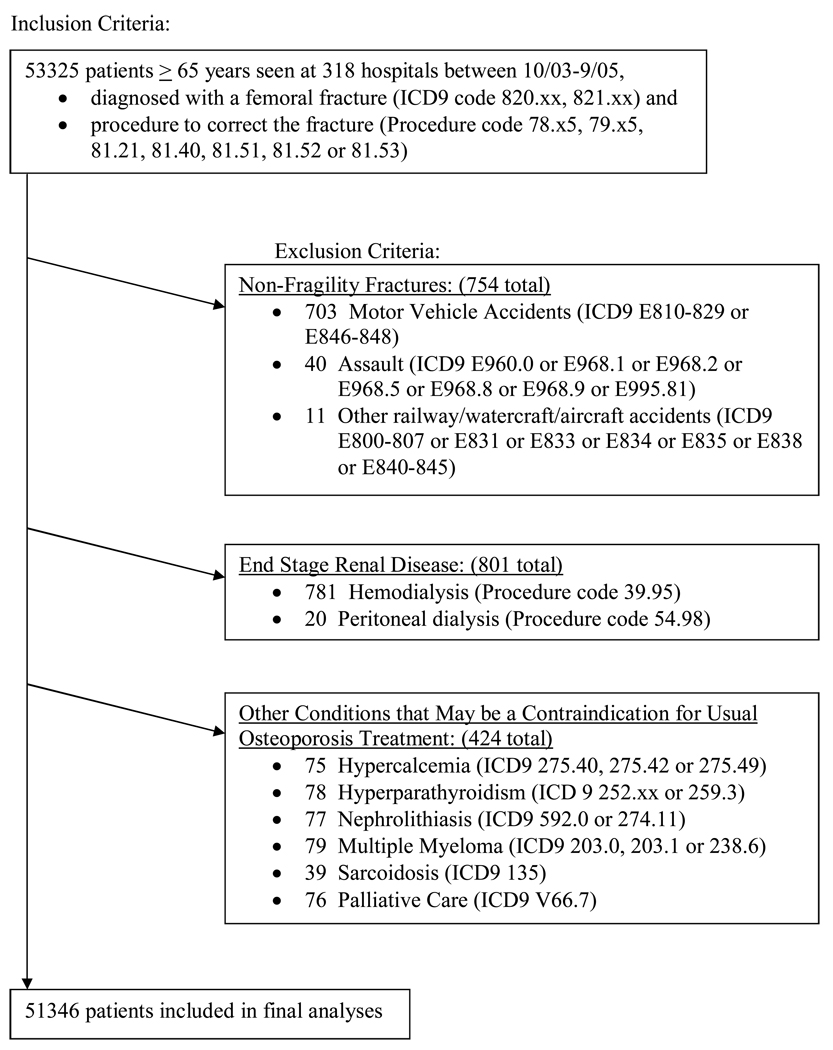
A total of 53,325 patients over age 65 were admitted to 318 Perspective hospitals between October 2003 and September 2005 with a diagnosis of a femoral fracture and had a procedure to correct the fracture as defined by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. Patients were excluded if they sustained a non-fragility fracture associated with significant trauma, such as a motor vehicle accident (n = 754), or if they had a secondary diagnosis associated with altered calcium metabolism that would contraindicate the receipt of Cal+D supplements, including end-stage renal disease requiring peritoneal or hemodialysis (n = 801), or conditions associated with hypercalcemia, including hyperparathyroidism, nephrolithiasis, sarcoidosis, and multiple myeloma (n = 348). Patients were also excluded if they were receiving palliative care (n = 76), leading to the final analytic cohort of 51,346 patients. ICD-9-CM codes used to define our patient population are detailed in Figure 1.
Figure 1.
Criteria Used to Define the Final Cohort of Patients Eligible for Osteoporosis Treatment.
The Perspective database (Premier Inc., Charlotte, North Carolina) was developed to monitor the clinical and financial aspects of hospital operations. Participating hospitals represent all regions of the United States, are predominantly small to mid-size non-teaching facilities, and serve a largely urban patient population. In addition to the clinical and demographic information available in the standard hospital discharge file, the Perspective database contains a date-stamped log of all billed items for each patient, including medications, laboratory, diagnostic, and therapeutic services. Because Premier is a group purchasing organization that provides hospitals with supplies including medications, there is a strong incentive for individual hospitals to capture and relay all pharmacy charges to the Perspective database, resulting in a remarkably complete database that has been successfully used in previous research. (26, 27)
Outcome Measures
Our primary outcome was the in-hospital receipt of at least 100mg of elemental calcium and 200 International Units (IU) of vitamin D anytime after the procedure to correct the fracture. Subjects were considered to have received Cal+D if they were charged for separate tablets of calcium and vitamin D or a combination tablet of calcium and vitamin D. Receipt of any calcium preparation with 100mg of elemental calcium, including calcium carbonate, calcium citrate, calcium acetate, or any one of 22 brand name calcium-containing medications qualified patients as having received calcium. Receipt of any vitamin D preparations, including ergocalciferol, cholecalciferol, 1,25 dihydroxycholecalciferol or brand name vitamin D preparations qualified patients as having received vitamin D. Patients who received a multivitamin were considered to have received vitamin D but not calcium since most preparations contain greater than 200 IU of vitamin D but less than 100mg of elemental calcium. (28)
Our secondary outcome was the receipt of antiresorptive or bone-forming osteoporosis medications. Receipt of any one of 35 generic or brand name osteoporosis medications (bisphosphonates, estrogen and selective estrogen receptor modulators, calcitonin or teriparatide) anytime after hip fracture surgery qualified patients as having received an antiresorptive or bone-forming medication.
Predictor Measures
We examined a variety of factors that may affect the outcome, including age, gender, ethnicity, and marital status. We accounted for comorbidities using the Elixhauser method. (29) Admit source, All Patient Refined Diagnosis Related Groups (APR DRG) risk of mortality (Version 15.0; 3M Corporation, Minneapolis, MN), and the specialty of the attending and consult physicians were obtained from the Perspective discharge file. We grouped Internal Medicine, Family or General Medicine, Hospital Medicine, Geriatrics, Critical Care Medicine, and other medicine subspecialties as medicine providers when considering attending and consult physician. In addition to patient level data, we also considered hospital-level covariates including each hospital’s teaching status, bed size, geographic region, and whether the institution served an urban or rural population.
Statistical Analysis
Age was categorized into five year intervals up to age ninety. The 80–84 year old age group was the largest group and thus used as the reference group. Other factors were coded as dichotomous (e.g. gender) or nominal (e.g. race/ethnicity) variables. We first characterized association between predictors and the outcome using univariate logistic regression. Multivariate results were obtained using alternating logistic models (30) (SAS proc genmod), which allowed us to account for the clustering of patients within physicians and physicians within hospitals. Variables were selected for inclusion in models based on the level of association with the outcome of interest, because of observed confounding, or to maintain face validity of the model.
To test the robustness of our findings, we repeated our analysis using alternate outcome measures, including the receipt of Cal+D and other osteoporosis medications at any point during the hospitalization and in the last three days of hospital stay. Also, given recent research suggesting that older patients who suffer a traumatic fracture are at equally high risk for osteoporosis and adverse outcomes, (31) we repeated our analysis including the 754 subjects who suffered a traumatic fracture. Results from these analyses were very similar to our primary analysis, so only the primary results are shown. Additionally, to gauge the completeness of our pharmacy records, we measured the receipt of DVT prophylaxis (dalteparin, enoxaparin, fondaparinux, heparin, and warfarin) and antibiotic prophylaxis (53 antibiotics) on the day of surgery and post-operative day 1.
All analyses were carried out using the SAS version 9.1 (SAS Institute, Inc. Cary, NC). The Committee on Human Research at the University of California, San Francisco approved our study. The funding sources had no role in the design or conduct of the study, data management or analysis, or manuscript preparation or review.
RESULTS
Patient characteristics (Table 1)
Table 1.
Characteristics of Study Participants
| Patient Level Variables | Percentage (N=51346) |
|---|---|
| Age | |
| 65–69 | 6% |
| 70–74 | 10% |
| 75–79 | 17% |
| 80–84 | 26% |
| 85–89 | 24% |
| 90+ | 18% |
| Female | 76% |
| Race/Ethnicity | |
| White | 78% |
| Black | 4% |
| Hispanic | 2% |
| Other | 15% |
| APR DRG Risk of Mortality* | |
| 1 | 30% |
| 2 | 52% |
| 3 | 14% |
| 4 | 4% |
| ICU Stay | 8% |
| Selected Elixhauser Comorbidities | |
| Congestive heart failure | 18% |
| Hypertension | 65% |
| Chronic pulmonary disease | 21% |
| Depression | 11% |
|
Provider and Hospital Level Variables |
|
| Attending and Consulting Physicians Medicine Attending |
41% |
| Orthopedic Attending with Medicine Consult |
27% |
| Orthopedic Attending without Medicine Consult |
30% |
| Number of beds | |
| 500+ | 31% |
| 400–499 | 14% |
| 300–399 | 21% |
| 200–299 | 18% |
| 1–199 | 16% |
| Teaching hospital | 20% |
All Patient Refined Diagnosis Related Groups (APR DRG) risk of mortality (Version 15.0; 3M Corporation, Minneapolis, MN)
A total of 51,346 patients, aged sixty-five or over, had a procedure to correct a femoral fracture between October 2003 and September 2005. Most were female, white, and age 75 or older. Sixty-eight percent had a medicine attending provider or a medicine consult. Common comorbidities in our cohort were hypertension (65%), chronic pulmonary disease (21%), congestive heart failure (18%), and depression (11%). Most patients received care at nonteaching hospitals in the South; thirty-one percent of patients received care at large hospitals with more than five hundred beds.
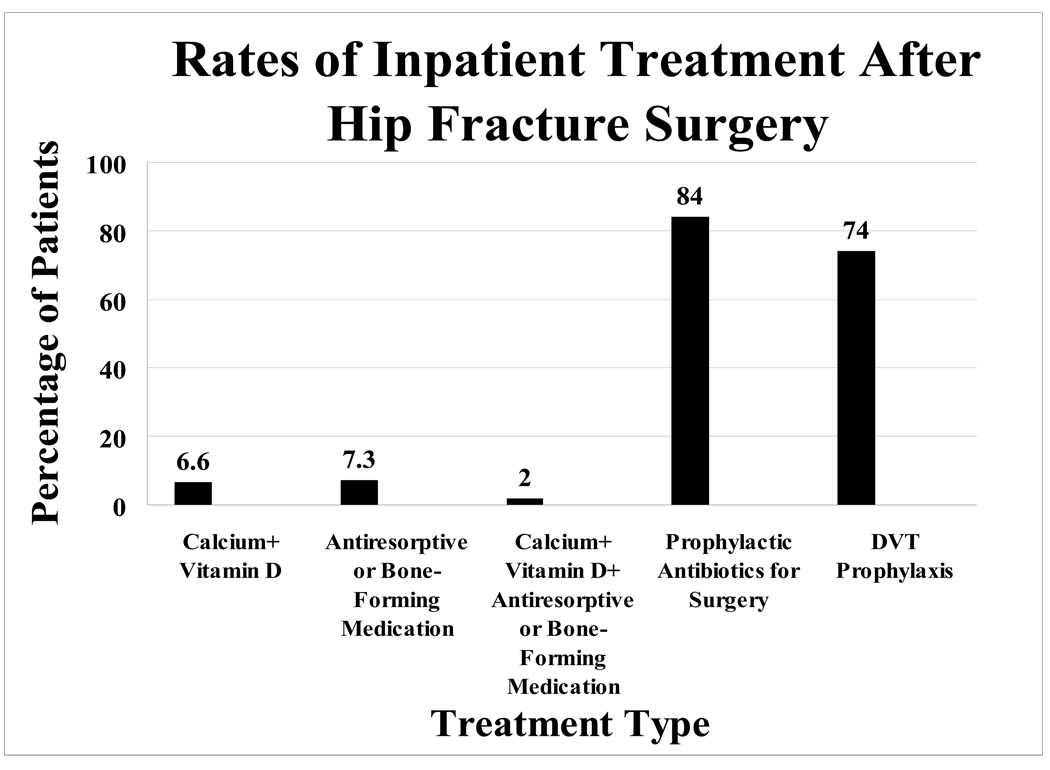
Rates of Treatment with Calcium/Vitamin D or Antiresorptive/Bone-Forming Medications (Figure 2)
Figure 2.
Rates of Inpatient Treatment After Hip Fracture Surgery
Prophylactic Antibiotics for Surgery and DVT prophylaxis rates were determined for the day of surgery and post-operative day 1.
3,405 patients (6.6%) received Cal+D anytime after procedure to correct femoral fracture. 3,763 patients (7.3%) received an antiresorptive or bone-forming medication, such as a bisphosphonate, estrogen, raloxifene, teriparatide, or calcitonin. Only 1023 patients (2%) were prescribed ideal therapy, receiving Cal+D and another medication for osteoporosis. In contrast to the low rates of osteoporosis medications, 84% of patients received perioperative antibiotic prophylaxis and 74% of patients received DVT prophylaxis. The rates of DVT and antibiotic prophylaxis were high and similar to prior studies, (32) arguing against substantial omissions in the Perspective pharmacy records data.
Predictors of Treatment with Calcium and Vitamin D (Table 2)
Table 2.
Percentages and Odds Ratios of Participants Receiving Calcium and Vitamin D by Patient, Provider and Hospital Characteristics
| Characteristic | Percentage of Calcium and Vitamin D No. (%) |
Unadjusted Odds Ratio (95% CI) |
Adjusted Odds Ratio (95% CI) |
|---|---|---|---|
| Patient level characteristics | |||
| Age | |||
| 65–69 | 173 (5.9%) | 0.86 (0.72, 1.01) | 0.91 (0.75, 1.09) |
| 70–74 | 280 (5.6%) | 0.81 (0.71, 0.93) | 0.87 (0.76, 1.00) |
| 75–79 | 523 (6.0%) | 0.87 (0.78, 0.97) | 0.91 (0.81, 1.03) |
| 80–84 | 895 (6.8%) | Ref | Ref |
| 85–89 | 904 (7.5%) | 1.10 (1.00, 1.21) | 1.11 (1.00, 1.22) |
| 90+ | 630 (6.7%) | 0.98 (0.88, 1.09) | 1.02 (0.91, 1.14) |
| Gender | |||
| Female | 2978 (7.6%) | Ref | Ref |
| Male | 427 (3.5%) | 0.44 (0.40, 0.49) | 0.58 (0.52, 0.65) |
| Race/Ethnicity | |||
| White | 2689 (6.7%) | Ref | Ref |
| Black | 104 (4.9%) | 0.71 (0.58, 0.87) | 0.66 (0.54, 0.83) |
| Hispanic | 71 (5.6%) | 0.82 (0.64, 1.05) | 1.19 (0.87, 1.62) |
| Other | 541 (7.1%) | 1.07 (0.97, 1.17) | 1.01 (0.85, 1.19) |
| APR DRG Risk of Mortality | |||
| 1 | 959 (6.1%) | Ref | Ref |
| 2 | 1836 (6.9%) | 1.14 (1.05, 1.23) | 1.04 (0.94, 1.16) |
| 3 | 491 (6.9%) | 1.14 (1.02, 1.27) | 1.06 (0.91, 1.24) |
| 4 | 119 (6.3%) | 1.03 (0.85, 1.25) | 1.04 (0.82, 1.31) |
| Received other Osteoporosis Medications |
|||
| No | 2382 (5.0%) | Ref | Ref |
| Yes | 1023 (27.2%) | 7.08 (6.52, 7.70) | 5.50 (4.84, 6.25) |
|
Provider and Hospital level characteristics |
|||
| Providers | |||
| Medicine attending | 1337 (6.4%) | Ref | Ref |
| Orthopedic attending with Medicine consult |
980 (7.2%) | 1.13 (1.04, 1.24) | 0.93 (0.82, 1.06) |
| Orthopedic attending without Medicine consult |
999 (6.5%) | 1.02 (0.94, 1.11) | 0.84 (0.75, 0.94) |
| Teaching Hospital | |||
| No | 2627 (6.4%) | Ref | Ref |
| Yes | 778 (7.7%) | 1.23 (1.13, 1.34) | 1.13 (0.78, 1.62) |
| Hospital Size, beds | |||
| 500+ | 1056 (6.7%) | Ref | Ref |
| 400–499 | 641 (8.7%) | 1.33 (1.20, 1.47) | 1.39 (0.90, 2.15) |
| 300–399 | 737 (6.7%) | 1.01 (0.92, 1.11) | 1.06 (0.76, 1.50) |
| 200–299 | 593 (6.5%) | 0.97 (0.88, 1.08) | 0.91 (0.64, 1.30) |
| 1–199 | 378 (4.7%) | 0.69 (0.61, 0.78) | 0.69 (0.48, 0.99) |
Adjusted Odds Ratios adjusted for all variables listed in this table, as well as marital status, admission source, hospital region, and all comorbidity adjustment using the Elixhauser method (those with prevalence of ≥1%), and for clustering at the hospital and attending provider levels.
Rates of Cal+D administration were less than 8% across virtually all patient, provider and hospital level characteristics. Rates were <8% across all age groups and all APR DRG Mortality Risk groups. Rates were <9% across all types of providers, all geographic regions, and all hospital sizes. Only prescription of an antiresorptive or bone-forming medication was associated with a substantially higher rate of Cal+D administration at 27%.
Being male was associated with worse odds of receiving Cal+D (Adjusted OR=0.58, 95% CI: 0.52–0.65), as was being black (Adjusted OR=0.66, 95% CI: 0.54–0.83). Odds of receiving Cal+D did not differ across age groups, APR DRG Mortality Risk group, provider, or hospital size.
Predictors of Treatment with any other Osteoporosis Medication (Table 3)
Table 3.
Percentages and Odds Ratios of Participants Receiving Other Osteoporosis Medications by Patient, Provider and Hospital Characteristics
| Characteristic | Percentage of Osteoporosis Medications N (%) |
Unadjusted Odds Ratio (95% CI) |
Adjusted Odds Ratio (95% CI) |
|---|---|---|---|
| Patient level Characteristics | |||
| Age | |||
| 65–69 | 222 (7.6%) | 0.96 (0.83, 1.12) | 1.10 (0.94, 1.29) |
| 70–74 | 379 (7.6%) | 0.97 (0.86, 1.09) | 1.06 (0.93, 1.21) |
| 75–79 | 683 (7.8%) | 1.00 (0.90, 1.10) | 1.04 (0.93, 1.16) |
| 80–84 | 1028 (7.8%) | Ref | Ref |
| 85–89 | 900 (7.4%) | 0.95 (0.86, 1.04) | 0.90 (0.81, 0.99) |
| 90+ | 551 (5.9%) | 0.73 (0.66, 0.82) | 0.71 (0.63, 0.81) |
| Gender | |||
| Female | 3495 (8.9%) | Ref | Ref |
| Male | 268 (2.2%) | 0.23 (0.20, 0.26) | 0.26 (0.23, 0.29) |
| Race/Ethnicity | |||
| White | 3003 (7.5%) | Ref | Ref |
| Black | 88 (4.1%) | 0.53 (0.43, 0.66) | 0.68 (0.55, 0.85) |
| Hispanic | 81 (6.3%) | 0.84 (0.67, 1.05) | 0.98 (0.72, 1.34) |
| Other | 591 (7.7%) | 1.04 (0.95, 1.14) | 1.04 (0.90, 1.19) |
| APR DRG Risk of Mortality | |||
| 1 | 1212 (7.7%) | Ref | Ref |
| 2 | 1982 (7.4%) | 0.96 (0.89, 1.03) | 1.06 (0.96, 1.16) |
| 3 | 477 (6.7%) | 0.86 (0.77, 0.96) | 1.04 (0.91, 1.19) |
| 4 | 92 (4.9%) | 0.61 (0.49, 0.76) | 0.84 (0.65, 1.08) |
| Received Calcium and Vitamin D |
|||
| No | 2740 (5.7%) | Ref | Ref |
| Yes | 1023 (30.0%) | 7.08 (6.52, 7.70) | 6.19 (5.47, 7.00) |
| Provider and Hospital level characteristics | |||
| Providers | |||
| Medicine attending | 1399 (6.7%) | Ref | Ref |
| Orthopedic attending with Medicine consult |
1053 (7.7%) | 1.17 (1.08, 1.27) | 1.01 (0.90, 1.12) |
| Orthopedic attending without Medicine consult |
1214 (7.9%) | 1.20 (1.11, 1.30) | 1.07 (0.96, 1.18) |
| Teaching Hospital | |||
| No | 3070 (7.4%) | Ref | Ref |
| Yes | 693 (6.9%) | 0.92 (0.84, 1.00) | 1.07 (0.87, 1.32) |
| Hospital Size, beds | |||
| 500+ | 1133 (7.2%) | Ref | Ref |
| 400–499 | 498 (6.7%) | 0.94 (0.84, 1.04) | 0.91 (0.73, 1.13) |
| 300–399 | 858 (7.8%) | 1.10 (1.01, 1.21) | 1.07 (0.87, 1.32) |
| 200–299 | 778 (8.5%) | 1.21 (1.10, 1.33) | 1.13 (0.91, 1.41) |
| 1–199 | 496 (6.2%) | 0.86 (0.77, 0.95) | 0.87 (0.70, 1.09) |
Adjusted Odds Ratios adjusted for all variables listed in this table, as well as for marital status, admission source, hospital region, and all comorbidity adjustment using the Elixhauser method (those with prevalence of >=1%), and clustering at the hospital and attending provider levels.
Rates of treatment with antiresorptive and bone-forming medications were similar to Cal+D rates and were less than 9% across virtually all patient, provider and hospital level characteristics. Rates were <8% across all age groups and all APR DRG Mortality Risk groups. Rates were <9% across all types of providers, all geographic regions, and all hospital sizes. Only prescription of Cal+D was associated with a substantially higher rate of administration of another osteoporosis medication at 30%.
Again, being male was associated with worse odds of receiving an antiresorptive or bone-forming medication (Adjusted OR=0.26, 95% CI: 0.23–0.29), as was being black (Adjusted OR=0.68, 95% CI: 0.55–0.85). Odds of receiving osteoporosis treatment did not differ across age groups, APR DRG Mortality Risk group, provider, or hospital size.
DISCUSSION
We found that the rates of osteoporosis treatment for patients hospitalized for hip fracture were very low. Rates of treatment with Cal+D were 6.6% and the rates of treatment with antiresorptive or bone-forming medications were 7.3%. Across virtually all patient, provider, and hospital level characteristics, treatment rates remained low, and the odds of treatment did not differ based on age, risk of mortality, or comorbidities. The strongest predictor of treatment with Cal+D was the receipt of an antiresorptive or bone-forming medication (Adjusted OR=5.50, 95% CI: 4.84–6.25). Although the relative odds of treatment was greatly increased, in absolute terms only 27% of patients who received antiresorptive or bone-forming medications also received Cal+D. Finally, only two percent of patients were prescribed ideal therapy as recommended by current national guidelines, (2, 3) and received Cal+D and an antiresorptive or bone-forming medication for osteoporosis.
Although osteoporosis treatment after hip fracture has traditionally been viewed as an outpatient issue, several factors are focusing more attention on the in-hospital initiation of osteoporosis treatment. First, new medications for osteoporosis such as intravenous (IV) bisphosphonates (approved in 2007 for the treatment of osteoporosis), do not require patients to remain upright and are easier to tolerate in the post-operative period, (6) making in-hospital initiation more practical. Second, prior studies have identified patient compliance with osteoporosis medications as a barrier to treatment, (33, 34) and the once-yearly in-hospital administration of IV bisphosphonates may effectively circumvent this barrier. Third, intervention studies to improve osteoporosis treatment after hip fracture through enhanced outpatient follow-up have resulted in only modest improvements, (10, 17, 19, 35, 36) suggesting additional interventions, including in-hospital initiation, may be needed to dramatically improve rates of appropriate treatment. (21) Fourth, the American Orthopaedic Association has led the development of the “Own the Bone” initiative, which aims to improve the “treatment of osteoporosis after fragility fracture” and focuses on the hospitalization, recognizing that the “seriousness of the fracture episode provides physicians with a definite ‘teachable moment’ in which it is possible to make a major impact on patients’ and primary care physicians’ behaviors.” (20, 37) Lastly, the National Osteoporosis Foundation’s “National Action Plan for Bone Health” focuses on fracture as a sentinel event, stating that “Just as a heart attack is seen as a sentinel event for treating cardiovascular disease, a first fragility fracture must be seen as an intervention opportunity.” (38) Compared to rates of in-hospital lipid diagnosis in cardiovascular patients (81% in 2006) (38), the low rates of in-hospital osteoporosis treatment for hip fracture patients in this study serve as a call to action as well as a baseline measure for current and future improvement initiatives.
There are several possible explanations for the low rates of in-hospital osteoporosis treatment. First, hospital physicians may be reluctant to address an issue that has traditionally been considered an outpatient issue. This may be the reason why our rates of in-hospital osteoporosis treatment for hip fracture patients are lower than previously published rates of outpatient osteoporosis treatment. (9–12) However, given the current low rates of appropriate treatment when this issue is deferred to the rehabilitation and outpatient settings, we believe the benefits of initiating osteoporosis treatment in the hospital outweigh the risks. Second, Cal+D alone have not been shown to definitively reduce fracture risk, which may lead physicians to discount their role in osteoporosis treatment. (7, 39) However, all osteoporosis treatments rely on adequate intake of Cal+D and guidelines recommend Cal+D supplementation for all older Americans who have suffered a hip fracture. (2, 3) Third, patients often do not recognize osteoporosis as the underlying cause of their fracture (40, 41) and may be reluctant to start osteoporosis medications in the hospital. Given the many competing acute issues that need to be addressed during hospitalization, clinicians may find it challenging to educate patients and their families on the importance of osteoporosis treatment.
Finally, concerns remain that bisphosphonates may have a negative effect on fracture healing by disrupting the usual bone remodeling process. Although animal studies have been reassuring, (42, 43) a recent case-control study found that the risk of humerus fracture non-union may be increased with outpatient bisphosphonate use, though the absolute rates of non-union appear very low. (44) Also, the randomized trial of IV zolendronic acid for the treatment of osteoporosis after hip fracture found no difference in delayed fracture healing or fracture nonunion between subjects receiving zolendronic acid versus placebo, (6) casting doubt on the case-control findings. Thus, even if the bisphosphonate non-union association is confirmed in cohort studies, we believe the low absolute risk of non-union would be outweighed by even small increases in osteoporosis treatment due to in-hospital initiation.
Although in-hospital bisphosphonate therapy offers the potential for improved osteoporosis treatment rates, significant practical challenges remain. First, IV bisphosphonates in vitamin D deficient cancer patients have led to reports of symptomatic hypocalcemia. (45) Since many hip fracture patients are vitamin D deficient, (6) further study is needed to clarify the risks associated with in-hospital IV bisphosphonate therapy for hip fracture patients. Second, the Medicare inpatient prospective payment system may not reimburse hospitals for additional interventions (such as bone mineral density testing or the administration of IV bisphosphonates) during a hip fracture admission. (46) Thus, there may be a financial disincentive for hospitals to provide this service, even if it is found to be safe and effective. Although these issues need to be addressed for in-hospital administration of IV bisphosphonates, they are not relevant for Cal+D, suggesting that in-hospital initiation of these medications may be a good first step to improving osteoporosis care in hip fracture patients.
Although we found that the rates of osteoporosis treatment were low, certain characteristics were associated with different treatment rates. Consistent with prior studies, we found that treatment rates were lower in patient groups at lower baseline risk for osteoporosis, such as men and African-Americans, (47, 48) highlighting the importance of educating patients and providers that fragility hip fractures should prompt treatment in all patients.
Our study has several limitations. First, we did not have information on discharge medications or subsequent outpatient diagnostic or treatment interventions such as bone mineral density testing or initiation of bisphosphonate therapy, and it is probable that some patients were started on osteoporosis treatment after hospitalization. Second, we were not able to determine which patients were receiving treatment for osteoporosis prior to the hospitalization, and some providers may have assumed that osteoporosis treatment would be continued post-hospitalization by the patient’s primary care physician. However, previous studies in the outpatient setting have shown that osteoporosis treatment rates at one year after hip fracture remain low, with most studies reporting rates below thirty percent. (9–12) Third, it is possible that some patients may have had contraindications to treatment which would suggest that lower treatment rates may be appropriate. Although we excluded patients with conditions affecting calcium metabolism, more detailed clinical information may have identified more subjects who were inappropriate for osteoporosis treatment. However, given the markedly low rates of treatment, we believe it is unlikely that additional clinical information would substantially change our findings. Finally, our measures of Cal+D (100mg and 200 IU, respectively) are significantly lower than the guideline-recommended amounts. (2) We chose this lower threshold to minimize the chances that we would overlook a subject receiving Cal+D. Even with our low threshold, we found low rates of Cal+D supplementation suggesting that the rates of hip fracture patients receiving guideline-recommended doses may be even lower.
Strengths of our study include our large, national sample which captured almost 10% of hip fracture patients in the US over a two year period. (1) Also, our rates of DVT and antibiotic prophylaxis were similar to previously reported national rates, suggesting that our pharmacy data is reliable and complete. Finally, performing this study in the inpatient setting allowed us to fully capture the rates of Cal+D supplement use. Because Cal+D are over-the-counter and widely available outside of the hospital, it would have been difficult to objectively capture Cal+D use in the outpatient setting.
In summary, we found in a national sample of US hospitals that the rates of in-hospital treatment for osteoporosis are very low. Our results indicate that despite proven therapies for osteoporosis, hip fracture patients remain grossly undertreated, placing them at higher risk for future fractures and resultant morbidity and mortality. Future research should focus on identifying barriers and testing interventions to improve the rates of in-hospital initiation of guideline-recommended osteoporosis treatment for this vulnerable population.
ACKNOWLEDGEMENTS
Funding Sources
Dr. Lee was supported by the Hartford Geriatric Health Outcomes Research Scholars Award and KL2RR024130 from the National Center for Research Resources, a component of the NIH. Dr. Auerbach was supported by 5R01HL086473 from the National Heart, Lung and Blood Institute and 5R21AG026668 from the National Institute on Aging.
Sponsor’s Role:
The funding sources had no role in the design or conduct of the study, data management or analysis, or manuscript preparation.
Footnotes
Previous Presentations
This work was presented at the 2008 American College of Physicians Northern California Chapter Scientific Meeting in San Francisco, CA in November 2008 and at the Society of General Internal Medicine Annual Meeting in Miami, Florida in May 2009.
Conflict of Interest Disclosures:
Author Contributions
Dr. Jennings designed the study, interpreted the data and wrote the manuscript.
Drs. Auerbach, Pekow and Lindenauer provided critical revisions of the manuscript.
Ms. Maselli provided statistical support.
Dr. Lee provided supervision in all phases of the study.
No other parties contributed substantially to this research or to preparation of this manuscript.
| Elements of Financial/Personal Conflicts |
LAJ | ADA | JM | PSP | PKL | SJL | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
|
Employment or Affiliation |
X | X | X | X | X | X | ||||||
| Grants/Funds | X | X | X | X | X | X | ||||||
| Honoraria | X | X | X | X | X | X | ||||||
| Speaker Forum | X | X | X | X | X | X | ||||||
| Consultant | X | X | X | X | X | X | ||||||
| Stocks | X | X | X | X | X | X | ||||||
| Royalties | X | X | X | X | X | X | ||||||
| Expert Testimony | X | X | X | X | X | X | ||||||
| Board Member | X | X | X | X | X | X | ||||||
| Patents | X | X | X | X | X | X | ||||||
|
Personal Relationship |
X | X | X | X | X | X | ||||||
REFERENCES
- 1.Fast Facts on Osteoporosis. National Institute of Arthritis, Musculoskeletal and Skin Diseases. 2009 April 13; Available from http://www.nof.org/osteoporosis/diseasefacts.htm.
- 2.Clinician's Guide to Prevention and Treatment of Osteoporosis. National Osteoporosis Foundation. 2009 April 13; Available from http://www.nof.org/professionals/NOF_Clinicians_Guide.pdf.
- 3.Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001 Feb 14;285(6):785–795. doi: 10.1001/jama.285.6.785. [DOI] [PubMed] [Google Scholar]
- 4.Bliuc D, Nguyen ND, Milch VE, et al. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009 Feb 4;301(5):513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 5.Center JR, Bliuc D, Nguyen TV, et al. Risk of subsequent fracture after low-trauma fracture in men and women. JAMA. 2007 Jan 24;297(4):387–394. doi: 10.1001/jama.297.4.387. [DOI] [PubMed] [Google Scholar]
- 6.Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic Acid in Reducing Clinical Fracture and Mortality after Hip Fracture. N Engl J Med. 2007;357(18):1799–1809. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacLean C, Newberry S, Maglione M, et al. Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med. 2008 Feb 5;148(3):197–213. doi: 10.7326/0003-4819-148-3-200802050-00198. [DOI] [PubMed] [Google Scholar]
- 8.Morin S, Rahme E, Behlouli H, et al. Effectiveness of antiresorptive agents in the prevention of recurrent hip fractures. Osteoporos Int. 2007 Dec;18(12):1625–1632. doi: 10.1007/s00198-007-0421-1. [DOI] [PubMed] [Google Scholar]
- 9.Cadarette SM, Katz JN, Brookhart MA, et al. Trends in drug prescribing for osteoporosis after hip fracture, 1995–2004. J Rheumatol. 2008 Feb;35(2):319–326. [PMC free article] [PubMed] [Google Scholar]
- 10.Elliot-Gibson V, Bogoch ER, Jamal SA, et al. Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int. 2004 Oct;15(10):767–778. doi: 10.1007/s00198-004-1675-5. [DOI] [PubMed] [Google Scholar]
- 11.Giangregorio L, Papaioannou A, Cranney A, et al. Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum. 2006 Apr;35(5):293–305. doi: 10.1016/j.semarthrit.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Rabenda V, Vanoverloop J, Fabri V, et al. Low incidence of anti-osteoporosis treatment after hip fracture. J Bone Joint Surg Am. 2008 Oct;90(10):2142–2148. doi: 10.2106/JBJS.G.00864. [DOI] [PubMed] [Google Scholar]
- 13.Davis JC, Guy P, Ashe MC, et al. HipWatch: osteoporosis investigation and treatment after a hip fracture: a 6-month randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2007 Aug;62(8):888–891. doi: 10.1093/gerona/62.8.888. [DOI] [PubMed] [Google Scholar]
- 14.Edwards BJ, Bunta AD, Madison LD, et al. An osteoporosis and fracture intervention program increases the diagnosis and treatment for osteoporosis for patients with minimal trauma fractures. Jt Comm J Qual Patient Saf. 2005 May;31(5):267–274. doi: 10.1016/s1553-7250(05)31034-8. [DOI] [PubMed] [Google Scholar]
- 15.Gardner MJ, Brophy RH, Demetrakopoulos D, et al. Interventions to improve osteoporosis treatment following hip fracture. A prospective, randomized trial. J Bone Joint Surg Am. 2005 Jan;87(1):3–7. doi: 10.2106/JBJS.D.02289. [DOI] [PubMed] [Google Scholar]
- 16.Jachna CM, Whittle J, Lukert B, et al. Effect of hospitalist consultation on treatment of osteoporosis in hip fracture patients. Osteoporos Int. 2003 Aug;14(8):665–671. doi: 10.1007/s00198-003-1413-4. [DOI] [PubMed] [Google Scholar]
- 17.Majumdar SR, Beaupre LA, Harley CH, et al. Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med. 2007 Oct 22;167(19):2110–2115. doi: 10.1001/archinte.167.19.2110. [DOI] [PubMed] [Google Scholar]
- 18.McLellan AR, Gallacher SJ, Fraser M, et al. The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int. 2003 Dec;14(12):1028–1034. doi: 10.1007/s00198-003-1507-z. [DOI] [PubMed] [Google Scholar]
- 19.Morrish DW, Beaupre LA, Bell NR, et al. Facilitated bone mineral density testing versus hospital-based case management to improve osteoporosis treatment for hip fracture patients: additional results from a randomized trial. Arthritis Rheum. 2009 Feb 15;61(2):209–215. doi: 10.1002/art.24097. [DOI] [PubMed] [Google Scholar]
- 20.Tosi LL, Gliklich R, Kannan K, et al. The American Orthopaedic Association's "own the bone" initiative to prevent secondary fractures. J Bone Joint Surg Am. 2008 Jan;90(1):163–173. doi: 10.2106/JBJS.G.00682. [DOI] [PubMed] [Google Scholar]
- 21.Curtis JR, Adachi JD, Saag KG. Bridging the osteoporosis quality chasm. J Bone Miner Res. 2009 Jan;24(1):3–7. doi: 10.1359/jbmr.081116. [DOI] [PubMed] [Google Scholar]
- 22.Fonarow GC, Gheorghiade M, Abraham WT. Importance of in-hospital initiation of evidence-based medical therapies for heart failure-a review. Am J Cardiol. 2004 Nov 1;94(9):1155–1160. doi: 10.1016/j.amjcard.2004.07.083. [DOI] [PubMed] [Google Scholar]
- 23.Muhlestein JB, Horne BD, Bair TL, et al. Usefulness of in-hospital prescription of statin agents after angiographic diagnosis of coronary artery disease in improving continued compliance and reduced mortality. Am J Cardiol. 2001 Feb 1;87(3):257–261. doi: 10.1016/s0002-9149(00)01354-0. [DOI] [PubMed] [Google Scholar]
- 24.Fedson DS, Harward MP, Reid RA, et al. Hospital-based pneumococcal immunization. Epidemiologic rationale from the Shenandoah study. JAMA. 1990 Sep 5;264(9):1117–1122. [PubMed] [Google Scholar]
- 25.Rigotti NA, Munafo MR, Stead LF. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2007 Mar; doi: 10.1002/14651858.CD001837.pub2. CD001837. [DOI] [PubMed] [Google Scholar]
- 26.Lindenauer PK, Pekow P, Wang K, et al. Lipid-lowering therapy and in-hospital mortality following major noncardiac surgery. JAMA. 2004 May 5;291(17):2092–2099. doi: 10.1001/jama.291.17.2092. [DOI] [PubMed] [Google Scholar]
- 27.Lindenauer PK, Pekow P, Wang K, et al. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med. 2005 Jul 28;353(4):349–361. doi: 10.1056/NEJMoa041895. [DOI] [PubMed] [Google Scholar]
- 28.Drug Facts and Comparisons 4.0 [database on the Internet] Wolters Kluwer Health, Inc; 2008. [Google Scholar]
- 29.Elixhauser A, Steiner C, Fraser I. Volume thresholds and hospital characteristics in the United States. Health Affairs (Millwood) 2003 Mar–Apr;22(2):167–177. doi: 10.1377/hlthaff.22.2.167. [DOI] [PubMed] [Google Scholar]
- 30.Carey VZS, Diggle P. Modeling multivariate binary data with alternating logistic regression. Biometrika. 1993;80:517–526. [Google Scholar]
- 31.Mackey DC, Lui LY, Cawthon PM, et al. High-trauma fractures and low bone mineral density in older women and men. JAMA. 2007 Nov 28;298(20):2381–2388. doi: 10.1001/jama.298.20.2381. [DOI] [PubMed] [Google Scholar]
- 32.Lieberman JR, Romano PS, Mahendra G, et al. The treatment of hip fractures: variations in care. Clin Orthop Relat Res. 2006 Jan;442:239–244. doi: 10.1097/01.blo.0000188558.67172.4e. [DOI] [PubMed] [Google Scholar]
- 33.Palacios S, Sanchez-Borrego R, Neyro JL, et al. Knowledge and compliance from patients with postmenopausal osteoporosis treatment. Menopause Int. 2009 Sep;15(3):113–119. doi: 10.1258/mi.2009.009029. [DOI] [PubMed] [Google Scholar]
- 34.Papaioannou A, Kennedy CC, Dolovich L, et al. Patient adherence to osteoporosis medications: problems, consequences and management strategies. Drugs Aging. 2007;24(1):37–55. doi: 10.2165/00002512-200724010-00003. [DOI] [PubMed] [Google Scholar]
- 35.Feldstein AC, Vollmer WM, Smith DH, et al. An outreach program improved osteoporosis management after a fracture. J Am Geriatr Soc. 2007 Sep;55(9):1464–1469. doi: 10.1111/j.1532-5415.2007.01310.x. [DOI] [PubMed] [Google Scholar]
- 36.Hooven F, Gehlbach SH, Pekow P, et al. Follow-up treatment for osteoporosis after fracture. Osteoporos Int. 2005 Mar;16(3):296–301. doi: 10.1007/s00198-004-1676-4. [DOI] [PubMed] [Google Scholar]
- 37.Own the Bone. The American Orthopaedic Association. 2009 April 13; Available from http://www.ownthebone.org/providers/about_aoa.
- 38.National Action Plan for Bone Health: Recommendations from the Summit for a National Action Plan for Bone Health. National Coalition for Osteoporosis and Related Bone Diseases. 2009 September 25;:27. Available from http://ww.nof.org/BoneHealthReport.pdf.
- 39.Tang BM, Eslick GD, Nowson C, et al. Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet. 2007 Aug 25;370(9588):657–666. doi: 10.1016/S0140-6736(07)61342-7. [DOI] [PubMed] [Google Scholar]
- 40.Giangregorio L, Papaioannou A, Thabane L, et al. Do patients perceive a link between a fragility fracture and osteoporosis? BMC Musculoskelet Disord. 2008;9:38. doi: 10.1186/1471-2474-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mauck KF, Cuddihy MT, Trousdale RT, et al. The decision to accept treatment for osteoporosis following hip fracture: exploring the woman's perspective using a stage-of-change model. Osteoporos Int. 2002 Jul;13(7):560–564. doi: 10.1007/s001980200073. [DOI] [PubMed] [Google Scholar]
- 42.Amanat N, Brown R, Bilston L, et al. A single systemic dose of pamidronate improves bone mineral content and accelerates restoration of strength in a rat model of fracture repair. J Orthop Res. 2005 Sep;23(5):1029–1034. doi: 10.1016/j.orthres.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 43.Fleisch H. Can bisphosphonates be given to patients with fractures? J Bone Miner Res. 2001 Mar;16(3):437–440. doi: 10.1359/jbmr.2001.16.3.437. [DOI] [PubMed] [Google Scholar]
- 44.Solomon DH, Hochberg MC, Mogun H, et al. The relation between bisphosphonate use and non-union of fractures of the humerus in older adults. Osteoporos Int. 2008 Oct 9; doi: 10.1007/s00198-008-0759-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chennuru S, Koduri J, Baumann MA. Risk factors for symptomatic hypocalcaemia complicating treatment with zoledronic acid. Intern Med J. 2008 Aug;38(8):635–637. doi: 10.1111/j.1445-5994.2007.01580.x. [DOI] [PubMed] [Google Scholar]
- 46.Overview Acute Inpatient Prospective Payment System. US Department of Health and Human Services. Centers for Medicare and Medicaid Services. 2009 September 25; Available from http://www.cms.hhs.gov/AcuteInpatientPPS/
- 47.Farley JF, Cline RR, Gupta K. Racial variations in antiresorptive medication use: results from the 2000 Medical Expenditure Panel Survey (MEPS) Osteoporos Int. 2006;17(3):395–404. doi: 10.1007/s00198-005-2027-9. [DOI] [PubMed] [Google Scholar]
- 48.Feldstein AC, Nichols G, Orwoll E, et al. The near absence of osteoporosis treatment in older men with fractures. Osteoporos Int. 2005 Aug;16(8):953–962. doi: 10.1007/s00198-005-1950-0. [DOI] [PubMed] [Google Scholar]