Abstract
Objective
To test the hypothesis that among hazardously drinking incarcerated women who are returning to the community, a brief alcohol intervention will result in less alcohol use at follow-up relative to standard of care.
Methods
Eligible participants endorsed hazardous alcohol consumption--four or more drinks at a time on at least three separate days in the previous three months or a score of 8 or above on the AUDIT. Participants were randomized to either an assessment-only condition or to two brief motivationally-focused sessions, the first delivered during incarceration, the second one month later after community re-entry. Participants recalled drinking behaviors at three and six months after the baseline interview using a 90-day Timeline Followback method.
Results
The 245 female participants averaged 34 years of age, and were 71% Caucasian. Participants were abstinent only 47% of days in the three months prior to incarceration. On most days (85%) that they drank, women consumed four or more drinks. Intervention effects on abstinent days were statistically significant at 3-months (OR = 1.96, 95% CI 1.17, 3.30); the percent of days abstinent was 68% for those randomized to intervention and 57% for controls. At 6-months the effect of the intervention was attenuated and no longer statistically significant.
Conclusions
Among incarcerated women who reported hazardous drinking, a two-session brief alcohol intervention increased abstinent days at three-months, but this effect decayed by six months. Study participants continued to drink heavily after return to the community. More intensive intervention pre-release and after re-entry may benefit hazardously-drinking incarcerated women.
Keywords: Alcohol, Incarceration, Women
INTRODUCTION
There are approximately 200,000 female inmates in prisons and jails in the United States, and since 1995 the number of women in prisons has increased 53%, far surpassing increases in the rate of incarceration of men [1]. Often returning to communities with few resources, the first weeks after release represent a time of vulnerability as released inmates encounter social and economic challenges related to housing, employment, and family. Criminal activity, substance abuse and high risk behaviors frequently recur in the days to weeks following release from jail and prison [2,3]. Alcohol use plays a significant, negative role in the lives of women who become incarcerated, and a return to hazardous drinking has been associated with recidivism and health consequences [4]. Alcohol-associated sexual risk-taking leads to high rates of sexually transmitted infections, including HIV in this population [5,6].
Estimates of the prevalence of hazardous drinking among the incarcerated depend on the type of correctional sample, and measure of alcohol use. A lifetime history of alcohol abuse has been reported in approximately one-third of female offenders [7–9]. This rate is approximately five times that in a national sample of community-dwelling women [10]. Estimates of women under the influence of alcohol at the time of arrest suggest even higher rates [11–13].
Imprisonment is an enforced period of abstinence and could potentially lead to a persistent reduction in alcohol and other drug use. This period of abstinence may provide a “teachable moment,” as women recognize the possible link between drinking and incarceration, but it is not clear that incarcerated women want to change their drinking or are motivated to persist in reductions. Maintenance of abstinence may be difficult for incarcerated women returning to the communities where hazardous drinking began, and researchers have not attempted interventions to reduce alcohol consumption in this population. Brief interventions for alcohol use disorders have become popular over the past fifteen years not only because they may be acceptable to non-treatment seeking populations, but also because they can be administered by a wide variety of providers in a range of clinical settings, and offered less expensively than extended treatments.
Brief interventions have proven efficacy for decreasing alcohol consumption and alcohol related problems when applied in outpatient clinical settings to hazardous and unhealthy drinkers [14,15]. In a meta-analytic review examining brief motivational interviewing (MI) interventions specifically, MI was found to be effective in reducing alcohol use among heavy drinkers. [16] In the few studies that include dependent drinkers, the magnitude of the MI effect size increases when drinkers are treatment-seeking [16]. In medical populations who are not voluntarily seeking help to reduce drinking, brief interventions for alcohol dependent persons have generally not had success [17,18].
Incarcerated women who drink hazardously represent one population that can be identified opportunistically by screening and who may benefit from a brief intervention initiated during incarceration and reinforced after community re-entry [19]. Incarcerated women who drink hazardously are accessible and, despite the rapid turnover of most jails, often have time for an intervention. An intervention that begins during incarceration and is reinforced soon after return to the community where alcohol is once again available, offers women two time points to consider their alcohol consumption [20].
The unmet need for alcohol screening and the opportunity for intervention among incarcerated women underscore the importance of determining the efficacy of brief interventions for this population. Therefore we conducted a randomized trial to compare an assessment-only control condition to a two-session brief motivational intervention to reduce drinking frequency. The study design is such that interventionists provide the first session during incarceration, and the second session takes place in the community when participants are re-exposed to the availability of alcohol. Our alcohol use outcomes are related to the combined impact of these two sessions. We also wanted to determine if our intervention impacted alcohol-related problems, mental health scores, and alcohol treatment entry in women returning to the community after incarceration.
METHODS
Study Site
In Rhode Island, all incarcerated persons are housed on a single campus that operates as a unified, centralized and comprehensive state correctional system, the Rhode Island Department of Correction (RI DOC), encompassing jail, prison, rehabilitative services, and community corrections (probation/parole).
Study Design and Procedure
All detained women over a 40-month period from February 2004 to June 2007 were eligible for screening for a randomized clinical trial of a brief intervention to reduce alcohol use and HIV risk. The trial protocol was approved by the Miriam Hospital Institutional Review Board, the Office for Human Research Protection, and the RI DOC’s Medical Research Advisory Group. The full details regarding the logistical planning for this trial have been published elsewhere [21].
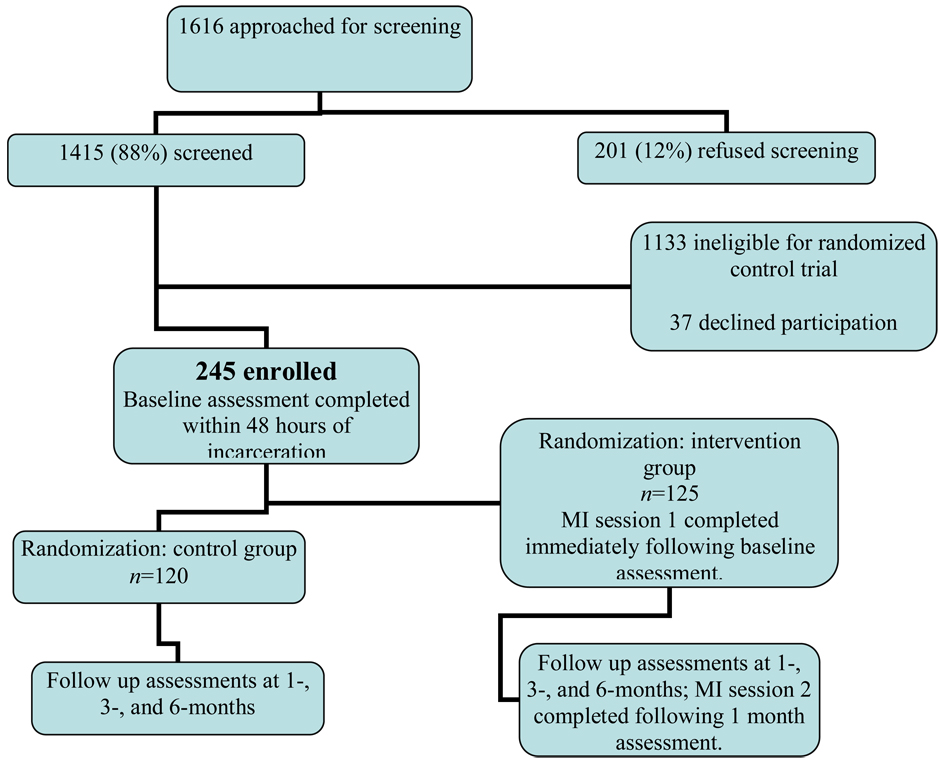
Participants were eligible for the clinical trial of interest if they spoke English, had reliable contact information, and endorsed having risky sexual behavior (unprotected sex on at least three separate days in the three months prior to incarceration) and hazardous alcohol consumption (four or more drinks at a time on at least three separate days in the previous three months or a score of 8 or above on the AUDIT [22], which was framed to the past year) [13]. As shown in Figure 1, during the enrollment period, on their first day of incarceration 1616 women were approached for screening and 201 refused. Of the 1415 women screened, 1133 were ineligible; 37 eligible women refused participation leaving a final sample of 245 women (see [19] for details).
Figure 1.
Study Enrollment and Protocol.
Schedule of the intervention
Following the baseline assessment which was completed on the first or second day of incarceration, participants were randomized to an intervention group receiving the motivational intervention or a control condition. Randomization and concealment were overseen by the study methodologist (BJA) and research staff performing the assessments were blinded to the participant’s assigned condition. All women were scheduled for follow-up assessment at 1-, 3-, and 6-months following the baseline assessment, regardless of whether the participant was incarcerated.
For each intervention group participant, two individual intervention sessions were scheduled, each lasting 30–45 minutes. The initial MI session was conducted at the time of the baseline interview while the participant was incarcerated, immediately following the baseline assessment. The second MI session was scheduled for one-month later, after the participant had been released, at a hospital-based research site in the community; the intervention session immediately followed the one-month assessment. If the participant was still incarcerated at the time of the scheduled 1-month follow-up assessment, the interview was completed, but the second MI session was delayed until she was 1) either released (and it was completed in the community within weeks, but prior to the 3-month assessment), or 2) if she had a prolonged incarceration, the second MI session was completed several days prior to the 3-month assessment.
Participants assigned to the control condition completed baseline, one-, three-, and six-month assessment visits only. At the completion of the one-month research assessment, participants in both conditions received the names and phone numbers of local drug and alcohol treatment facilities, as well as their next interview date.
Manual Development and Therapist Training
The manual for this study was adapted from the MI approach of Miller and Rollnick [23] and the Brief Alcohol Intervention in Needle Exchangers study [24]. Training consisted of reviewing the five basic principles of motivational interviewing including, a) expressing empathy, b) developing discrepancy, c) avoiding argumentation, d) rolling with resistance, and e) support self-efficacy [23]. All intervention sessions were audiotaped and tapes were reviewed in biweekly supervision sessions.
Initial MI Session (during incarceration)
The goal of this first session was for the interventionist, using motivational interviewing techniques, to set goals regarding making a change in alcohol use behavior, and to explore strategies to deal with internal or external obstacles/barriers in achieving these goals. During this session interventionists discussed: the participant’s values and goals, pros and cons of alcohol use (using a decisional balance handout), thoughts about alcohol use and cutting back/quitting, feedback from the research assessment (highlighting cost of alcohol, reasons for drinking and negative consequences), thoughts about the usefulness of alcohol treatment, state of readiness to make changes, and generation of a change plan. Due to RIDOC regulations, participants were not allowed to keep any materials from the intervention session. Upon release, the feedback report and change plan handouts were enclosed in a mailing including payment for the baseline interview, community resources, condoms and the next appointment date.
Follow-Up MI Session
The follow-up session was based on the participant’s goal(s) and change plan from the initial MI session. For those participants with an alcohol change goal, follow-up sessions focused on progress, assessment of barriers, and developing concrete strategies for meeting new goals. Recovery strategies were also discussed, with an emphasis on identifying high-risk situations for relapse, and developing effective strategies for coping in high risk situations.
If the participant set a non-alcohol related goal, sessions focused on progress towards goals and barriers in achieving these goals. MI techniques were used to review the information from the first session in order to reevaluate the possibility for setting an alcohol goal. Interventionists offered suggestions about interim steps which participants might consider prior to setting an abstinence goal.
Therapist Integrity
The Motivational Interviewing Treatment Integrity Code Version 2.0 (MITI) [25,26] was used both to train the four female study interventionists (three clinical psychologists, one masters level counselor) and to monitor the MI skills of the interventionists during biweekly supervision. The MITI 2.0 allows for an assessment of threshold competence for individual therapists and a measure of integrity of MI interventions, has two global scores (“empathy” and “spirit;” score range 1–7) and seven behavior counts (e.g. “giving information”, “MI adherent”). Three raters trained in MI (inter-rater reliability >0.60) coded a random sample of 15% of the treatment sessions, coding 20-minute segments of each session. These segments were selected from the full sessions to evenly reflect each portion of the intervention. Sessions were double-coded frequently to prevent rater drift. Mean scores across the 2 global scales for the intervention sessions were 5.1 (SD .81; Empathy) and 4.6 (SD .85; Spirit)
Measures
At the baseline assessment, research staff, blinded to treatment group assignment, asked participants to recall 90 days prior to their incarceration using the Timeline Followback (TLFB) method [27]. Staff asked respondents to recall days they consumed alcohol and how many drinks on each day. They were then asked about vaginal or anal sex on each of these 90 days. Other measures included the Short-Index of Problems (SIP) [28], and a dichotomous indicator of treatment entry, coded 1 if the participant attended an AA meeting, entered a medically supervised detoxification program, entered residential treatment, or attended outpatient alcohol treatment in the last 90 days. Lifetime diagnosis of DSM IV alcohol dependence was measured using the SCID [29].
Statistical Analysis
We present means, medians, and percentages to describe the background characteristics and pre-baseline alcohol use behaviors in this cohort. Pearson χ2 tests and t-tests for differences in means were used to test the equivalence of intervention groups at baseline.
We use zero-inflated count regression models to test the effect of intervention on drinking outcomes [30]. These models simultaneously estimate two equations. The inflation part of the model uses a logit or probit response to estimate the probability of a zero response (that is, an abstinent day). The count part of the model uses a Poisson response, or a negative binomial, to estimate the quantity of alcohol use (drinks per drinking day). All models were estimated using Mplus 5.1 [31]. The default standard errors are the robust sandwich estimators; here adjusted for within subject clustering.
Our primary outcomes were 1) the probability of an abstinent day and 2) drinks per drinking day as reported using TLFB methodology on the baseline, and 1-, 3-, and 6-month follow-up interviews. We restricted our analyses to days when the participant was not incarcerated. Our analysis proceeded in three steps. We first examined the overdispersion parameter for the constant only zero-inflated negative-binomial (ZINB). We then used the difference scaled χ2 test to compare two models with alternative parameterizations of time [32]. One operationalized the effect of time as linear (coded 0, 1, 3, 6); the second treated time as unconstrained with dummy indicators representing each of the three follow-up periods. Intervention effects were then estimated as the first-order treatment by time interaction for the best fitting zero-inflated count mode and time parameterization.
We report exponentiated coefficients giving the expected factor change on the odds of not drinking alcohol on a given day and the expected factor change on the expected number of drinks per drinking day; the later coefficients are sometimes referred to as incidence rate ratios (IRR). To facilitate interpretation we also present the model estimated probabilities of not drinking alcohol (zero count) and the expected number of drinks per drinking day.
We conducted a secondary analysis to determine if the intervention had an effect on functional outcomes at the 3- and 6-month follow-up assessments. Models estimating the effect on the SIP assumed normally distributed error; the effect on treatment entry was estimated as a logistic response with binomial error. Intervention effects were estimated as the first-order treatment by time interaction effect using GEE models.
RESULTS
Participants averaged 34.1 (±8.9) years of age, and 71% were Caucasian (Table 1). On average, participants reported their alcohol consumption on 87.5 (± 7.6; Mdn = 90) days prior to baseline. The mean percent days using any alcohol and heavy (≥ 4 drinks) amounts of alcohol were 51.7 (± 33.6) and 43.9 (± 33.7), respectively. Participants averaged 12.4 (± 10.0) drinks per drinking day, their mean AUDIT score was 20.6 (±10.1) and 220 (90%) met SCID criteria for a lifetime diagnosis of alcohol dependence. Demographic characteristics and baseline alcohol use behaviors did not differ significantly between the intervention groups (Table 1).
Table 1.
Baseline Characteristics by Intervention (n = 245).
| Total (n = 245) |
Treatment (n = 125) |
Control (n = 120) |
t (p=) | |
|---|---|---|---|---|
| Mean Age (Yrs) | 34.1 (±8.9) | 33.3 (±9.4) | 34.9 (±8.3) | 1.40 (.162) |
| Mean Education (Yrs) | 10.4 (±1.6) | 10.3 (±1.6) | 10.5 (±1.6) | 1.18 (.240) |
| Mean % Alc. Days | 51.7 (±33.6) | 54.2 (±33.2) | 49.3 (±32.0) | −1.17 (.243) |
| Mean % Heavy Days | 43.9 (±33.7) | 44.9 (±34.3) | 42.7 (±33.2) | −0.50 (.615) |
| Mean Drks / DrinkDay | 12.4 (±10.0) | 12.5 (±10.3) | 12.4 (±9.8) | 0.04 (.970) |
| Mean AUDIT | 20.6 (±10.1) | 20.8 (±10.2) | 20.4 (±10.0) | −0.33 (.738) |
|
χ2 (p =) |
||||
| n (%) Ethnicity | ||||
| Caucasian | 175 (71.4%) | 89 (71.2%) | 86 (71.7%) | 1.21 (.751) |
| African-American | 47 (19.2%) | 26 (20.8%) | 21 (17.5%) | |
| Hispanic | 17 (6.9%) | 8 (6.4%) | 9 (7.5%) | |
| Other | 6(2.5%) | 2 (1.6%) | 4 (3.3%) | |
| n (%) 1-Mo. Assessment | 186 (75.9%) | 96 (76.8%) | 90 (75.0%) | 0.11 (.742) |
| n (%) 3-Mo. Assessment | 194 (79.2%) | 99 (79.2%) | 95 (79.2%) | 0.00 (.995) |
| n (%) 6-Mo. Assessment | 193 (78.8%) | 99 (79.2%) | 94 (78.3%) | 0.03 (.868) |
| n (%) At Least 1 FU | 224 (91.4%) | 114 (91.2%) | 110 (91.7%) | 0.02 (.896) |
| n (%) At Risk 1-Mo. | 132 (53.9%) | 67 (53.6%) | 65 (54.2%) | 0.01 (.929) |
| n (%) At Risk 3-Mo. | 174 (71.0%) | 86 (71.7%) | 88 (70.4%) | 0.05 (.827) |
| n (%) At Risk 6-Mo. | 180 (73.5%) | 92 (76.7%) | 88 (70..%) | 1.23 (.267) |
| n (%) Any At Risk | 210 (85.7%) | 107 (85.6%) | 103 (85.8%) | 0.00 (.958) |
One hundred eighty six (76%), 194 (79%), and 193 (79%) of the participants were located and completed assessments at the 1-, 3,-, and 6-month follow-ups, respectively; 224 (91%) completed at least one follow-up (Table 1). Of those who completed assessments, 132, 174, and 180 participants had 1 or more days during which they were not incarcerated during the intervals assessed at the 1-, 3-, and 6-month follow-ups. Follow-up rates were very similar in both intervention arms and there was no evidence of differential attrition.
Model Selection and Aggregate Changes in Alcohol Use Behaviors Over Time
The overdispersion parameter estimated for a constant-only negative binomial model was statistically significant (z = −10.19, p < .001) indicating the ZINB is preferred to the ZIP. The model in which time was unconstrained fit the data significantly better than the linear time model (Difference Scaled χ2 = 10.89, df = 2, p < .05). Coefficients indicated the expected odds of not using any alcohol were 1.48 (95% CI 1.11, 1.98), 1.84 (95% CI 1.41, 2.39), and 1.96 (95% CI 1.49, 2.56) times lower on days observed at 1-month, 3-months, and 6-months, respectively, than on days observed prior to baseline. Additionally, the expected number of drinks per drinking day was significantly lower at 3-months (p < .05) and 6-months (p < .01) than at baseline. Compared to baseline the expected number of drinks per day decreased by a factor of 0.81 (95% CI 0.67, 0.97) at 3-months and by a factor of 0.79 (95% CI 0.66, 0.95) at 6-months. Drinks per drinking day did not differ significantly between baseline and 1-month (IRR = 0.91, 95% CI 0.73, 1.10) among non-incarcerated women. Based on these analyses, the ZINB was used to test the effects of intervention with separate effects estimated for each of the 3 follow-up periods. Baseline assessment is the reference category in all estimated models.
Estimated Intervention Effects
One hundred twenty five women were assigned to the treatment arm. Of these, 70 (56%) received their second intervention session in the community, 23 (18%) received it while at the RIDOC due to prolonged incarceration, and 32 (26%) did not receive a second intervention session. Table 2 gives the estimated effect of a brief intervention on alcohol use at each follow-up. A test of the treatment by time interaction effect on the inflation part of the model indicates statistically significant between group differences (Difference Scaled χ2 = 8.20, df = 3, p < .05) in abstinent days. At 1-month, between group differences are small and not statistically significant. Intervention effects on abstinent days are substantively larger and statistically significant at 3-months (OR = 1.96, 95% CI 1.17, 3.30). By 6-months the effect of intervention was somewhat attenuated and no longer statistically significant.
Table 2.
Zero-Inflated Negative Binomial Model Estimating the Effect of Brief Intervention on Alcohol Abstinence and Number of Drinks per Drinking Day (210 Participants Assessed for a Total of 48,723 Non-Incarcerated Person-Days).
| Inflation Model OR (95% CI)a |
Negative Binomial IRR (95% CI)a |
|
|---|---|---|
| Intervention | 0.79 (0.54, 1.15) | 1.00 (0.78, 1.29) |
| Month 1 | 1.34 (0.89, 2.02) | 1.01 (0.78, 1.31) |
| Month 3 | 1.33 (0.92, 1.91) | 0.81 (0.63, 1.04) |
| Month 6 | 1.63*(1.84, 2.72) | 0.78 (0.61, 1.00) |
| Intervention by Month 1 | 1.22 (0.69, 2.17) | 0.80 (0.53, 1.19) |
| Intervention by Month 3 | 1.96*(1.17, 3.30) | 1.01 (0.70, 1.45) |
| Intervention by Month 6 | 1.44 (0.84, 2.49) | 1.03 (0.72, 1.47) |
p < .05,
p < .01
Estimated effect on the odds of not using alcohol. Confidence interval estimates and tests of significance were based on robust variance estimators adjusted for within subject clustering.
There was no evidence that the intervention significantly reduced the number of drinks on days when drinking was initiated. A test of the treatment by time interaction effect on the count part of the model was not statistically significant (Difference Scaled χ2 = 0.98, df = 3, p > .10) and an examination of the individual coefficients indicated the effects of intervention on the expected number of drinks on drinking days were trivially small at baseline, 3-, and 6-months (Table 2). The effect at 1-month was substantively stronger (IRR = 0.81, 95% CI 0.63, 1.04) though not statistically significant (p > .05).
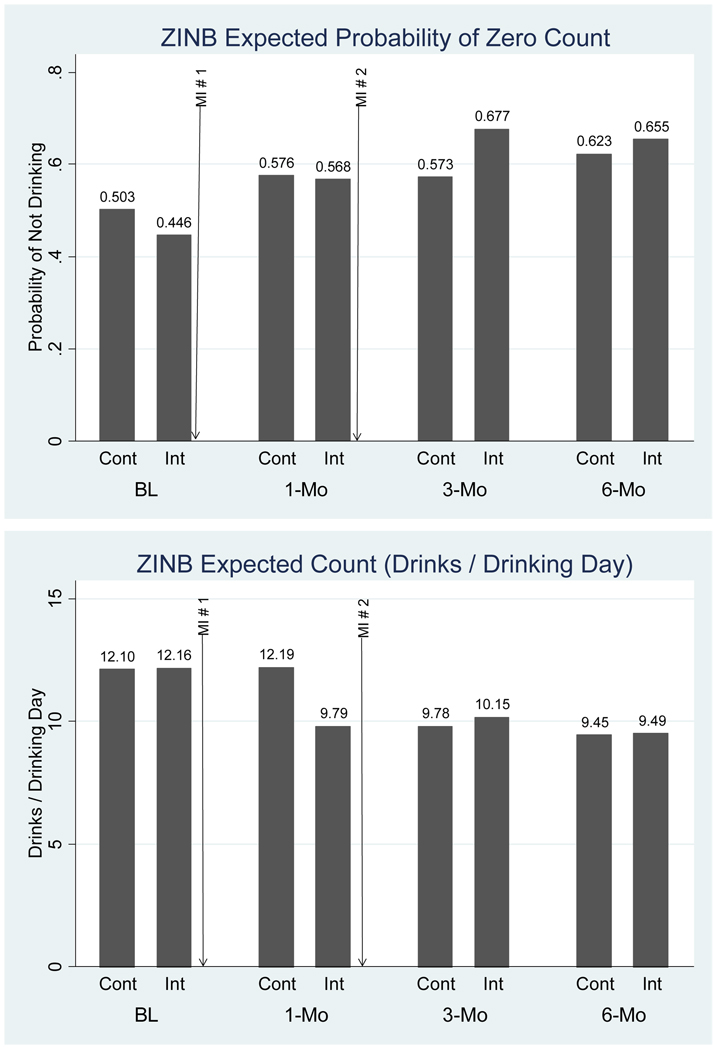
The probability of abstinence and the number of drinks per drinking day are presented in Figure 2. Figure 2 highlights that the first session of MI immediately following the baseline assessment, and the second session of MI was conducted following the 1-month assessment. The panels in Figure 2 directly parallel the inflation and count parts of the ZINB model given in Table 2. At baseline, those randomized to intervention had a slightly lower probability of drinking on days in the prior three months, at 1-month the probability of an abstinent day in the two groups was nearly equal, and at 3-months the probability of an abstinent day was .68 for those randomized to intervention and .57 for controls. At 6-months, the significant intervention group effect was no longer present.
Figure 2.
Expected Probability of a Zero-Count and the Expected Drinks per Drinking Day by Treatment Group and Assessment Period Estimated by ZINB.
The first intervention session followed the baseline assessment. The second intervention session followed the 1-month assessment.
The second panel of Figure 2 gives the expected number of drinks per drinking day for the ZINB model presented in Table 2. At 1-month participants randomized to intervention consumed 9.8 drinks per drinking day while controls were estimated to drink 12.2 drinks per drinking day (p> .10) At all other time points between group differences in the number of drinks per drinking day were very small.
We performed two additional exploratory analyses. First, we found that neither site of the second MI session nor time between MI sessions one and two were significantly associated with either drinking outcome. Second, we tested intervention effects comparing women who were and were not alcohol dependent. At 3- months, the observed intervention effect was stronger among the 22 women who did not meet dependence criteria (IRR = 7.55; 95% CI 0.9–37.8) than among the 188 who did (IRR 1.69; 95% CI 1.0–2.9). At 1- and 6-months, the intervention effects were non-significant.
Functional Outcomes
Intervention effects on alcohol treatment entry were small and not statistically significant at either the 3- or 6-month assessments (Table 3). Paralleling the primary outcome analysis, participants randomized to intervention reported fewer adverse alcohol consequences than controls on the Short-Inventory of Problems observed at 3-months (b = −4.96, 95%CI −8.91, −1.02, p < .05), but not at 6-months (b = −2.30, 95%CI −6.26,1.65).
Table 3.
Generalized Estimating Equation Models Estimating the Effect of Brief Intervention on the Short Inventory of Problems (SIP), the Mental Functioning Component of the SF-12, and Treatment Entry.
| SIPa | Mental Func. SF-12a |
Treatment Entryb |
|
|---|---|---|---|
| b (95%CI)c |
b (95%CI) |
OR (95%CI) |
|
| Intervention | 2.83 (−0.64,6.31) |
0.97 (−1.84,3.78) |
0.67 (0.35,1.28) |
| Month 3 | −5.10* (−7.87,−2.32) |
6.05** (3.09,9.02) |
3.02** (1.82,5,00) |
| Month 6 | −7.46* (−10.18,−4.74) |
7.97** (5.25,10.70) |
3.84** (2.42, 6.07) |
| Intervention by Month 3 | −4.96* (−8.91,−1.02) |
−0.64 (−4.73,3.24) |
1.23 (0.59,2.56) |
| Intervention by Month 6 | −2.30 (−6.26,1.65) |
−1.63 (−5.49,2.23) |
1.37 (0.67,2.81) |
| Intercept | 21.46 | 30.30 | |
p < .05,
p < .01
The effects on the Short-Inventory of Problems and the Mental Functioning Component of the SF-12 were estimated with an identity link and normally distributed error.
The effects on treatment entry were estimated with a logit link and binomial error distribution.
Tests of significance and confidence interval estimates were based on robust standard errors adjusted for within subject clustering.
DISCUSSION
In this randomized clinical trial of incarcerated women who reported hazardous drinking prior to incarceration, we found that a two-session brief alcohol intervention increased abstinent days during the three-months after the baseline assessment. The 24% decline in drinking days in the intervention group was associated with decreased SIP scores, suggesting the clinical meaningfulness of these findings.
Using AUDIT and binge-drinking screeners to determine study eligibility, we were surprised to find that 90% of our “hazardous drinkers” were alcohol dependent. These women drank extremely heavily, consuming on average 12 drinks on their drinking days. Many brief intervention studies exclude individuals with severe drinking problems. Indeed brief intervention has proven efficacy in decreasing alcohol consumption and related consequence only in hazardous drinkers without alcohol dependence [14,17]. In one meta-analysis, brief interventions were no more effective than control conditions when persons with severe alcohol problems were included, except for those persons seeking treatment [15]. On hospital inpatient services where patients also undergo enforced abstinence, several studies have demonstrated the efficacy of brief interventions on alcohol consumption [33,34], although not all have shown this effect [18]. A systematic review of controlled studies enrolling hospital inpatients reported an association between brief intervention and decreased alcohol-related problems, but not alcohol consumption [17]. Our treatment effect is particularly promising given that most of these women were alcohol dependent (effects were superior among the non-dependent), were not treatment-seeking, and had not self-identified as problem drinkers.
As expected, both treatment arms decreased their drinking days and drinks per drinking day during the follow-up period. The period of enforced abstinence during incarceration, and the research assessment itself could have motivated participants contemplating change to decrease alcohol consumption in both randomized groups. We found a significant intervention effect in days abstinent only at the three-month assessment. We did not find an intervention effect at the one-month follow-up, which would have represented the effect of only the single intervention session performed during incarceration. The three-month follow-up period represents the resultant change after two sessions, suggesting the importance of the second, post-release contact with participants. The significant treatment effect faded between the three and the six-month assessments, a finding which is consistent with the results of meta-analyses [16,35]. The optimal timing and number of community-based booster sessions remains open to further study, but at least suggest that to enhance the effectiveness of brief alcohol interventions for this population, ongoing monitoring of participants’ drinking will be important, particularly as most hazardously drinking women, including all those enrolled in this study, are not mandated to alcohol treatment programs upon community re-entry. We should note that the intervention group effect at three months was achieved mainly through moderation of ongoing alcohol use rather than cessation; only 18 (8.6%) women maintained abstinence during the entire follow-up period. Rates of complete abstinence among those randomized to intervention (9.4%) did not differ significantly (χ2 = 0.17, df = 1, p > .10) from controls (7.8%). In addition, there was no significant intervention effect on drinks per drinking day at any follow-up assessment. This suggests that while the intervention influenced initiation of drinking, once drinking began women were unable to constrain their consumption.
Our study had several strengths. We developed a screening and intervention protocol that was feasible and replicable across correctional settings. Furthermore we did not restrict our eligibility criteria based on mental health disorders or other drug use, and few eligible women refused to participate. Our study also had limitations. Participants could not be blinded, although they were generally interviewed at follow-up by research staff they had not met. Primary outcomes were self-reported but were assessed by trained staff using validated, standardized procedures and techniques to aid recall and minimize bias. There was likely an assessment effect, reducing drinking generally, which may have limited group differences. Interventionists were trained clinicians; jails and prisons will need to have staff with expertise in health behavior change dedicated to improving the drinking outcomes of women to apply these findings but this intervention has broad potential applicability across US prison systems. Finally, this study included only incarcerated women who drank hazardously and met heterosexual sex-risk criteria. Thus the generalizability of our findings to other populations of women, or to men, may be limited. Future analyses will examine the relationship of reduction in alcohol use to sexual risk-taking.
Although the proportion of abstinent days increased when compared to the period prior to incarceration, study participants continued to drink, and drink heavily after their return to the community. Brief intervention was inadequate to produce consistent or prolonged abstinence and future studies must link released women with additional assistance to reduce consumption and related problems. Future interventions may also include the provision of other known efficacious therapies such as medications for dependent drinkers.
Among incarcerated women there is a high prevalence of health problems including substance use, mental health disorders and HIV. Socioeconomic and psychological factors affect drinking behavior and access to treatment. The high prevalence of hazardous drinking among incarcerated women and the absence of previous intervention studies drove the development and design of this brief intervention clinical trial. Our findings have important implications for the long-term reintegration and rehabilitation of this population. A brief intervention during incarceration, supplemented by a booster visit after return to the community may catalyze change. Continued and more intensive interventions pre-release and after re-entry could benefit these women.
ACKNOWLEDGEMENTS
This study was funded by the National Institute on Alcoholism and Alcohol Abuse AA 014495. Dr. Stein is a recipient of a NIDA Mid-Career Award DA 000512
Footnotes
Trial registered at clinicaltrials.gov; Clinical Trial #NCT00237003
No author on this manuscript has any personal or financial interest that would influence the results.
REFERENCES
- 1.Harrison PM, Beck AJ. Prison and jail inmates at midyear 2004. U.S. Department of Justice; 2005. (Bureau of Justice Statistics, NCJ 208801) [Google Scholar]
- 2.Richie BE, Freudenberg N, Page J. Reintegrating women leaving jail into urban communities: a description of a model program. J. Urban Health. 2001;78:290–303. doi: 10.1093/jurban/78.2.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, et al. Release from prison—a high risk of death for former inmates. N Eng J Med. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henderson DJ. Drug abuse and incarcerated women—a research review. J Subst Abuse Treat. 1998;15:579–587. doi: 10.1016/s0740-5472(97)00319-x. [DOI] [PubMed] [Google Scholar]
- 5.Stein MD, Anderson BJ, Caviness CM, Rosengard C, Kiene S, Friedmann P, Clarke JG. The relationship of alcohol use and sexual risk-taking among hazardously-drinking incarcerated women: an event level analysis. J Stud Alcohol Drugs. 2009;70:508–515. doi: 10.15288/jsad.2009.70.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Willers DM, Peiper JF, Allsworth JE, Stein MD, Rose JS, Clarke JG. Prevalence and predictors of sexually transmitted infections among newly incarcerated females. Sex Trans Dis. 2008;35:68–72. doi: 10.1097/OLQ.0b013e318154bdb2. [DOI] [PubMed] [Google Scholar]
- 7.Grella CE, Greenwell L. Treatment needs and completion of community-based aftercare among substance-abusing women offenders. Women’s Health Issues. 2007;17:244–255. doi: 10.1016/j.whi.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Jordan BK, Schlenger WE, Fairbank JA, Caddell JM. Prevalence of psychiatric disorders among incarcerated women. II. Convicted felons entering prison. Arch Gen Psychiatry. 1996;53:513–519. doi: 10.1001/archpsyc.1996.01830060057008. [DOI] [PubMed] [Google Scholar]
- 9.Teplin LA, Abram KM, McClelland GM. Prevalence of psychiatric disorders among incarcerated women. I. Pretrial jail detainees. Arch Gen Psychiatry. 1996;53:505–512. doi: 10.1001/archpsyc.1996.01830060047007. 1996. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Chui WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Bassel N, Ivanoff A, Schilling RF, Gilbert L, Chen DR. Correlates of problem drinking among drug-using incarcerated women. Addict Behav. 1995;20:359–369. doi: 10.1016/0306-4603(94)00075-a. [DOI] [PubMed] [Google Scholar]
- 12.Greenfeld LA. Women Offenders. U.S. Department of Justice; 1999. (Bureau of Justice Statistics, NCJ 175688) [Google Scholar]
- 13.Paasche-Orlow MK, Clarke JG, Hebert MR, Ray MK, Stein MD. Educational attainment but not literacy is associated with HIV risk behavior among incarcerated women. J Women’s Health. 2005;14:852–859. doi: 10.1089/jwh.2005.14.852. [DOI] [PubMed] [Google Scholar]
- 14.Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Int Med. 1997;12:274–283. doi: 10.1046/j.1525-1497.1997.012005274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 16.Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol. 2006;41:328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- 17.Emmen MJ, Schippers GM, Bleijenberg G, Wollersheim H. Effectiveness of opportunistic brief interventions for problem drinking in a general hospital setting: systematic review. BMJ. 2004;328:318. doi: 10.1136/bmj.37956.562130.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saitz R, Palfai TP, Cheng DM, Horton NJ, Freedner N, Dukes K, et al. Brief intervention for medical inpatients with unhealthy alcohol use: a randomized controlled trial. Ann Intern Med. 2007;146:167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- 19.Caviness CM, Hatgis C, Anderson BJ, Rosengard C, Kiene SM, Friedmann PD, et al. Three brief alcohol screens for detecting hazardous drinking in incarcerated women. J Stud Alcohol Drugs. 2009;70:50–54. doi: 10.15288/jsad.2009.70.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system. Improving public health and safety. JAMA. 2009;301:183–190. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hebert MR, Clarke JG, Caviness CM, Ray MK, Friedmann PD, Stein MD. Feasability of gaining access to women in jail for interventions. Women Health. 2008;47:79–93. doi: 10.1080/03630240802134159. [DOI] [PubMed] [Google Scholar]
- 22.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption – II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 23.Miller WR, Rollnick S. Motivational Interviewing: preparing people for change. New York: Guilford Press; 2002. [Google Scholar]
- 24.Stein M, Charuvastra A, Maksad J, Anderson B. A Randomized Trial of a Brief Alcohol Intervention for Needle Exchangers. Addiction. 2002;97:691–700. doi: 10.1046/j.1360-0443.2002.00102.x. [DOI] [PubMed] [Google Scholar]
- 25.Moyers T, Martin T, Manual J, Miller W. The Motivational Interviewing Treatment Integrity (MITI) Code: Version 2.0. 2005 Available from http://casaa.unm.edu/codinginst.html.
- 26.Moyers T, Martin T, Manual J, Hendrickson S, Miller W. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Sobell LC, Sobell MB. Timeline Followback user’s guide: a calendar method for assessing alcohol and drug use. Toronto, Ontario, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- 28.Miller WR, Tonigan JS, Longabaugh R. Project MATCH Monograph Series. Vol. 4. Rockville, MD: NIAA; 1995. The Drinker Invventory of Consequences (DrInC): An Instrument for Assessing Adverse Consequences of Alcohol Abuse. [Google Scholar]
- 29.Spitzer RL, Williams JBW, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID): I. History, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 30.Long JS, Freeze J. Regression Models for Categorical Dependent Variables Using Stata. 2nd Ed. College Station, TX: Stata Press; 2006. [Google Scholar]
- 31.Muthén LK, Muthén BO. MPlus Users Guide. 5th Edition. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- 32.Satorra A, Bentler PM. A Scaled Difference Chi-square Test Statistic for Moment Structure Analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blondell RD, Looney SW, Northington AP, Lasch ME, Rhodes SB, McDaniels RL. Can recovering alcoholics help hospitalized patients with alcohol problems? J Fam Pract. 2001;50:447. [PubMed] [Google Scholar]
- 34.Hulse GK, Tait RJ. Six-month outcomes associated with a brief alcohol intervention for adult in-patients with psychiatric disorders. Drug Alcohol Rev. 2002;21:105–112. doi: 10.1080/09595230220138993a. [DOI] [PubMed] [Google Scholar]
- 35.Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]