Abstract
The goal of the present study was to assess how reduced SERCA2a expression affects in vivo myocardial ischemia/reperfusion (I/R) injury. We specifically wanted to determine to what extent hearts with reduced SERCA2a levels are susceptible to in vivo I/R injury. Therefore, we examined the effects of different ischemic periods on post-ischemic myocardial injury in wild-type (WT) and SERCA2a heterozygous knockout (SERCA2a+/−) mice expressing lower levels of SERCA2a pump in vivo. Following 20-min ischemia and 48-hour reperfusion, SERCA2a+/− mice developed significant myocardial infarction (MI) compared to negligible infarction in WT mice (14 ± 3% vs. 3 ± 1%, P<0.01); whereas following 30-min ischemia, the infarction was significantly larger in SERCA2a+/− mice compared to WT mice (49 ± 5% vs. 37 ± 3%, P<0.05). Further, echocardiographic analysis revealed worsened postischemic contractile function in SERCA2a+/− mice compared to WT mice. Thus, these findings demonstrate that maintaining optimal SERCA2a function is critical for myocardial protection from I/R injury and postischemic functional recovery.
Keywords: Sarcoplasmic reticulum, Ca2+-ATPase (SERCA), Ischemia, Reperfusion, Myocardial infarction, Contractile function
1. Introduction
Myocardial infarction (MI) is the single largest cause of cardiac death worldwide. Acute myocardial ischemia/reperfusion (I/R) injury is associated with contractile dysfunction, MI, and sudden death [1]. Patients may die from progressive hemodynamic deterioration due to heart failure (HF) or as a result of a new ischemic event such as recurrent angina or MI [2]. Ventricular remodeling and wall thinning are critically dependent on the infarct size, and thus, the MI size is a major determinant of mortality [3]. Therefore, preventing acute MI or limiting infarct size is critical to improve immediate and long-term outcome of patients with acute coronary syndrome and to avoid the development of HF. Recently, we have demonstrated in isolated hearts that reduced SERCA2a levels worsen postischemic myocardial recovery with increased intracellular Ca2+ (Ca2+i) overload and infarction [4]. Also it has been documented that mice with reduced SERCA2a exhibited an accelerated onset of HF when subjected to pressure overload [5]. Thus, mice with reduced functional SERCA2a are more prone to stress conditions.
While SERCA2a expression is reduced in the failing heart [2,6], the effect of this on susceptibility to further ischemic injury is unknown. Therefore, it is important to determine the effect of reduced SERCA2a on susceptibility to in vivo myocardial I/R.
A major goal of this study was to translate our recent in vitro findings [4] under in vivo conditions to further validate the role of SERCA2a in myocardial I/R. The present study was, thus, designed to determine the effects of both shorter and longer durations of in vivo regional ischemia on subsequent MI size and contractile function in both WT and SERCA2a+/− mice.
2. Methods
2.1. Mice
Generation and characterization of heterozygous SERCA2a knockout (SERCA2a+/−) mice have been described previously [7].
2.2. Western blot analysis
Western blotting with cardiac homogenates was performed as described previously [7,8].
2.3. in vivo myocardial ischemia/reperfusion (I/R)
in vivo myocardial I/R was performed in male littermates (16–20 weeks) as described [8].Briefly, mice were anesthetized with intraperitoneal ketamine and xylazine, intubated, ventilated, and chest was opened. The left anterior descending (LAD) coronary artery was ligated by a 7-0 silk ligature. After 20- or 30-min LAD artery occlusion, the knot was released to start reperfusion.
2.4. Echocardiography
In vivo cardiac function was determined 4 days before and 48 hours after reperfusion by M-mode echocardiography as described [4].Briefly, two-dimensional short-axis view was used, and LV fractional shortening (FS) was calculated as FS (%)= (LVEDD−LVESD)/LVEDD×100.
2.5. Myocardial infarct size measurement
MI was measured after 48 hours reperfusion as described previously with slight modification [8]. Each myocardial slice was photographed, and area at risk (AAR), infarct area (IA) and non risk area were determined by computerized planimetry.
2.6. Data analysis
All results are expressed as the mean ± SEM. Data were analyzed either by two-tailed Student's t-test for paired data from the same experiment or unpaired data from different experiments. Values of P<0.05 were considered statistically significant.
3. Results and discussion
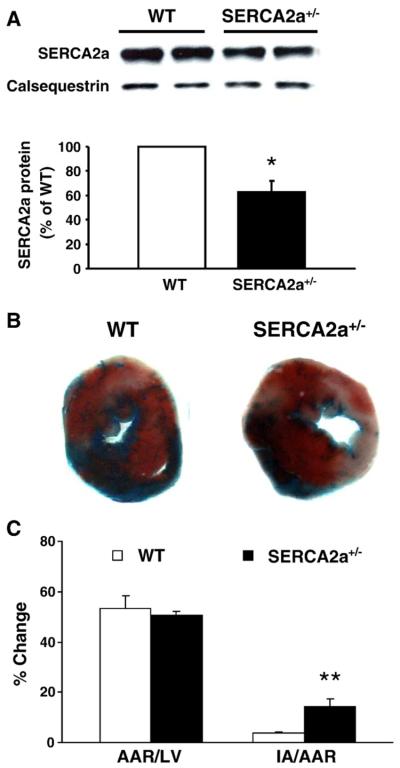
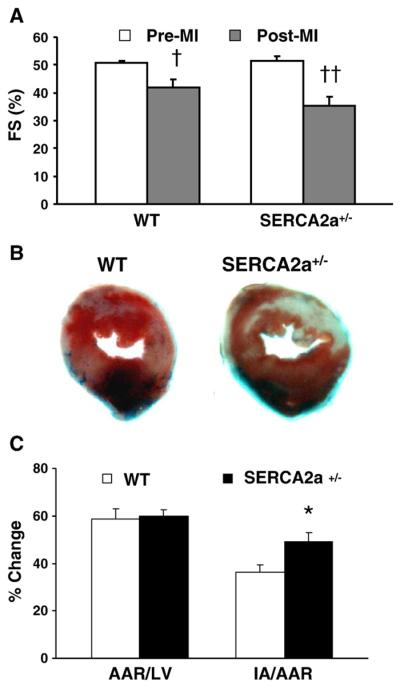
In this study, we test the hypothesis that hearts with reduced SERCA2a (Fig. 1A) are more susceptible to I/R injury in vivo. In order to examine this question, we used SERCA2a+/− mice [7] in which expression was ~35% lower than wild type hearts (Fig. 1A). The most striking finding is that when SERCA2a+/− mice were subjected to a sub-lethal I/R, the hearts developed significant MI compared to negligible infarction in WT (Figs. 1B, C). In addition, SERCA2a+/− hearts exhibited significantly larger MI following lethal I/R compared to WT mice (Figs. 2B, C). Importantly, in contrast to WT, echocardiography revealed markedly reduced post-MI fractional shortening in SERCA2a+/− mice from respective pre-MI value (Fig. 2A). These results further confirm our published results with in vitro I/R [4]. It has been reported that Ca2+i overload with reduced expression and/or activity of SERCA2a plays a pivotal role in I/R injury [9], and thus, SERCA2a mediated Ca2+ transport is of crucial importance in the transition from reversible to irreversible injury during I/R. We reported that SERCA2a+/− hearts had markedly higher Ca2+i at baseline, after ischemia and during early reperfusion [4]. This Ca2+ overload was likely due to decreased cytosolic Ca2+ removal by SR, because SERCA2a+/− hearts have a lower Ca2+ uptake activity than WT hearts [7]. Consistent with a Ca2+ overload mechanism, we also observed that isolated SERCA2a+/− hearts had higher incidence of persistent arrhythmias during reperfusion than WT hearts (5/6 vs. 3/6 hearts). In contrast, SERCA overexpression with its attendant efficient Ca2+ removal strongly protected the heart against I/R injury, reperfusion arrhythmias and improved diastolic function [8]. Thus, the present in vivo study demonstrates for the first time that decreased SERCA2a pump activity could exacerbate a sublethal injury into a lethal injury, and further increase MI following an acute lethal I/R.
Fig. 1.
Myocardial infarction and function in hearts subjected to 20-min LAD ligation and 48-hour reperfusion. (A) Immunoblots and bar graphs for SERCA2a protein levels in WT and SERCA2a+/− hearts, calsequestrin as internal control (N = 3/group). (B) Representative sections of hearts stained with phthalo blue and 2,3,5-triphenyltetrazolium chloride after I/R. (C) Percentage of area at risk (AAR) over left ventricle (LV) and infarct area (IA) over AAR. All values are means ± SEM. N =5–6/group; *P<0.05 vs. WT; **P<0.01 vs. WT.
Fig. 2.
Myocardial function and infarction in hearts subjected to 30-min LAD ligation and 48-hour reperfusion. (A) FS (%) before (pre-MI) and after MI (post-MI). (B, C) Please see Fig. 1 for description. N =5–7/group.†P<0.05 vs. Pre-MI; ††P<0.01 vs. Pre-MI; *P<0.05 vs. WT.
These findings have important clinical implications because SERCA2a+/− mice [7] are an ideal model to explore how decreased SERCA2a pump expression can compromise cardiac function during disease states. It was previously shown that SERCA2a+/− mice exhibit accelerated HF when subjected to pressure overload [5]. In the clinical setting of I/R, reduced SERCA2a would be expected to lead to HF with greater morbidity and mortality [2]. Importantly, 1 in 5 patients experiences recurrent angina within a year of hospitalization for CABG surgery, baseline angina, and cardiac revascularization [10]. Thus, patients with prior MI are at greater risk of recurrent MI and exacerbated HF [2,10]. There is now growing evidence that reduced Ca2+ transients and contractile dysfunction in human HF and in animal models are due to depressed SR function [2,6,11,12]. Reduced SR Ca2+ uptake has also been reported in human myocardium following reversible I/R [13]. Recently, we [8] and others [14,15] have shown that increasing SR Ca2+ uptake function by SERCA overexpression strongly protects the heart against I/R injury with efficient Ca2+ removal, improved contractile function, and reduced arrhythmias and myocardial infarction. Of note, efficient SR Ca2+ uptake and subsequent improved postischemic myocardial function might impede the consequences of Ca2+ overload-induced cellular and molecular changes. Recently, DNA micro-array data in rat MI showed that SERCA2 gene transfer increases cardioprotective gene expression and lowers the expression of genes that are known to exacerbate heart failure [15]. Therefore, future studies incorporating DNA microarray, biochemical, morphological and functional data in clinically relevant models will be able to verify these findings and establish the mechanisms of SERCA2a-induced cardioprotection.
In conclusion, the present study provides convincing data to suggest that reduced myocardial SERCA2a activity renders the heart more susceptible to I/R injury, and further reaffirms the critical role and need of optimal SERCA2a function in MI.
Acknowledgments
This work was supported by NIH grants HL63744, HL65608, HL38324, and HL64140 to JLZ, and HL64140 and HL088555 to MP.
Footnotes
There are no conflicts-of-interest.
References
- 1.Bolli R, Becker L, Gross G, Mentzer R, Jr, Balshaw D, Lathrop DA. Myocardial protection at a crossroads: the need for translation into clinical therapy. Circ Res. 2004;95:125–34. doi: 10.1161/01.RES.0000137171.97172.d7. [DOI] [PubMed] [Google Scholar]
- 2.Smith G. Matters of the heart: the physiology of cardiac function and failure. Exp Physiol. 2007;92:973–86. doi: 10.1113/expphysiol.2007.034314. [DOI] [PubMed] [Google Scholar]
- 3.Burns RJ, Gibbons RJ, Yi Q, Roberts RS, Miller TD, Schaer GL, et al. The relationships of left ventricular ejection fraction, end-diastolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis. J Am Coll Cardiol. 2002;39:30–6. doi: 10.1016/s0735-1097(01)01711-9. [DOI] [PubMed] [Google Scholar]
- 4.Talukder MA, Kalyanasundaram A, Zuo L, Velayutham M, Nishijima Y, Periasamy M, et al. Is reduced SERCA2a expression detrimental or beneficial to postischemic cardiac function and injury? Evidence from heterozygous SERCA2a knockout mice. Am J Physiol Heart Circ Physiol. 2008;294:H1426–34. doi: 10.1152/ajpheart.01016.2007. [DOI] [PubMed] [Google Scholar]
- 5.Schultz JEJ, Glascock BJ, Witt SA, Nieman ML, Nattamai KJ, Liu LH, et al. Accelerated onset of heart failure in mice during pressure overload with chronically decreased SERCA2 calcium pump activity. Am J Physiol Heart Circ Physiol. 2004;286:H1146–53. doi: 10.1152/ajpheart.00720.2003. [DOI] [PubMed] [Google Scholar]
- 6.Lehnart SE, Schillinger W, Pieske B, Prestle J, Just H, Hasenfuss G. Sarcoplasmic reticulum proteins in heart failure. Ann NY Acad Sci. 1998;853:220–30. doi: 10.1111/j.1749-6632.1998.tb08270.x. [DOI] [PubMed] [Google Scholar]
- 7.Ji Y, Lalli MJ, Babu GJ, Xu Y, Kirkpatrick DL, Liu LH, et al. Disruption of single copy of the SERCA2a gene results in altered Ca2+ homeostasis and cardiomyocytes function. J Biol Chem. 2000;275:38073–80. doi: 10.1074/jbc.M004804200. [DOI] [PubMed] [Google Scholar]
- 8.Talukder MA, Kalyanasundaram A, Zhao X, Zuo L, Bhupathy P, Babu GJ, et al. Expression of SERCA isoform with faster Ca2+ transport properties improves postischemic cardiac function, Ca2+ handling, and decreases myocardial infarction. Am J Physiol Heart Circ Physiol. 2007;293:H2418–28. doi: 10.1152/ajpheart.00663.2007. [DOI] [PubMed] [Google Scholar]
- 9.Mubagwa K. Sarcoplasmic reticulum function during myocardial ischemia and reperfusion. Cardiovasc Res. 1995;30:166–75. [PubMed] [Google Scholar]
- 10.Maddox TM, Reid KJ, Spertus JA, Mittleman M, Krumholz HM, Parashar S, et al. Angina at 1 year after myocardial infarction: prevalence and associated findings. Arch Intern Med. 2008;168:1310–6. doi: 10.1001/archinte.168.12.1310. [DOI] [PubMed] [Google Scholar]
- 11.Armoundas AA, Rose J, Aggarwal R, Stuyvers BD, O, Rourke B, Kass DA, et al. Cellular and molecular determinants of altered Ca2+ handling in the failing rabbit heart: primary defects in SR Ca2+ uptake and release mechanisms. Am J Physiol Heart Circ Physiol. 2007;292:H1607–18. doi: 10.1152/ajpheart.00525.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zucchi R, Ronca F, Ronca-Testoni S. Modulation of sarcoplasmic reticulum function: a new strategy in cardioprotection? Pharmacol Ther. 2001;89:47–65. doi: 10.1016/s0163-7258(00)00103-0. [DOI] [PubMed] [Google Scholar]
- 13.Nef HM, Möllmann H, Skwara W, Bölck B, Schwinger RH, Hamm Ch, et al. Reduced sarcoplasmic reticulum Ca2+-ATPase activity and dephosphorylated phospholamban contribute to contractile dysfunction in human hibernating myocardium. Mol Cell Biochem. 2006;282:53–63. doi: 10.1007/s11010-006-1171-7. [DOI] [PubMed] [Google Scholar]
- 14.Gianni D, Chan J, Gwathmey JK, del Monte F, Hajjar RJ. SERCA2a in heart failure: role and therapeutic prospects. J Bioenerg Biomembr. 2005;37:375–80. doi: 10.1007/s10863-005-9474-z. [DOI] [PubMed] [Google Scholar]
- 15.Niwano K, Arai M, Koitabashi N, Watanabe A, Ikeda Y, Miyoshi H, et al. Lentiviral vector-mediated SERCA2 gene transfer protects against heart failure and left ventricular remodeling after myocardial infarction in rats. Mol Ther. 2008;16:1026–32. doi: 10.1038/mt.2008.61. [DOI] [PubMed] [Google Scholar]