Abstract
The number of health-related websites has proliferated over the past few years. Health information consumers confront a myriad of health related resources on the internet that have varying levels of quality and are not always easy to comprehend. There is thus a need to help health information consumers to bridge the gap between access to information and information understanding—i.e. to help consumers understand health related web-based resources so that they can act upon it. At the same time health information consumers are becoming not only more involved in their own health care but also more information technology minded. One way to address this issue is to provide consumers with tailored information that is contextualized and personalized e.g. directly relevant and easily comprehensible to the person’s own health situation. This paper presents a current trend in Consumer Health Informatics which focuses on theory-based design and development of contextualized and personalized tools to allow the evolving consumer with varying backgrounds and interests to use online health information efficiently. The proposed approach uses a theoretical framework of communication in order to support the consumer’s capacity to understand health-related web-based resources.
Keywords: consumer health information, internet, contextualization of information, personalization
Introduction
As government agencies (e.g. the National Institutes of Health, Medicare/Medicaid), non-profit organizations (e.g. medical associations), and for-profit companies are increasingly providing health information and services online, the internet is becoming an important source of health information for the general public.1–3 However, consumers of health information on the internet are increasingly being confronted with a myriad of health related resources that have varying levels of quality and are not always easy to comprehend. There is thus a need to help these consumers to bridge the gap between access to information and information understanding—i.e. to help consumers understand health related web-based resources so that they can act upon it. One way to address this issue is to provide consumers with tailored information which is contextualized and personalized e.g. directly relevant and easily comprehensible to the person’s own health situation.
This necessarily requires a deep understanding of the backgrounds, needs, and preferences of health information consumers, particularly because the profile of e-health information consumers is changing. Indeed, health information consumers are becoming not only more involved in their own health care but also more information technology minded. Furthermore, the profile of these evolving consumers is shaped by an increase in the aging population, who are prone to chronic conditions and are in need of more involvement in self-management of their chronic illnesses.
The field of Consumer Health Informatics (CHI) aims at supporting consumers of health information to address their needs and changes by developing web-based applications with which consumers can efficiently obtain information, digest, and act upon the information they have found online. Furthermore, CHI focuses on analyzing consumers’ needs for health related information; studying and implementing methods for making information accessible to consumers; and modeling and integrating consumers’ preferences into web-based applications.4,5
This paper presents a current trend in CHI, which focuses on theory-based design and development of contextualized and personalized tools to allow the evolving consumer with varying backgrounds and interests to use online health information efficiently. There is lack of research in this particular area, and the approach we advocate here is based upon our own research projects. This paper first describes the multi-facets of the emerging e-health information consumer. Issues in the field of CHI directly affecting consumers are presented in the second section. The proposed approach using a theoretical framework of communication in order to support the consumer’s capacity to understand health-related web-based resources is then discussed in the third section. Directions for further research are discussed in the final section.
The Changing Facets of Health Information Consumers
Behaviors of the consumer of health information
Patients have become active consumers of health related information. At the same time, they are now encouraged—and in many cases, expected—to be well informed and responsible. In particular, they are expected to play a more active role in seeking medical information, managing their health and medical care, and participating in health and medical decision-making.6–8
However, what patients need, want, or prefer may be very different from what medical professionals think they would need, want, or prefer.9–12 Furthermore, health information consumers are heterogeneous individuals who have diverse needs and preferences for health information and display diverse behavioral patterns.13 Data from a large scale mail panel survey14 have suggested that there are significant differences in how health information consumers value, understand, and seek health-related information content and sources. Specifically, along the two dimensions of “degree of engagement in health enhancement” and “degree of independence in health decision making,” distinct groups were identified: independent actives and independent passives, doctor-dependent actives and doctor-dependent passives. Independent actives more easily understand health information and are more likely to seek health information from multiple sources such as physicians, the internet, books and magazines. In comparison, doctor-dependent actives have more difficulty understanding health information and are more likely to primarily rely on their doctors for health information and decisions. Compared with these two “active” groups, the independent passives and doctor-dependent passives groups are both less engaged in health enhancement, suggesting that both groups value health information less. Not surprisingly, these two passive groups are less likely to seek health information from any source, including doctors (more so for independent passives than for doctor-dependent passives).
Other predictors of consumers’ online health information seeking behaviors include age, gender, education, race/ethnicities, and computer/internet experiences.14–18 Furthermore, individuals who have chronic illnesses or face significant barriers in accessing health care through healthcare providers (e.g. uninsured, greater physical distance/time travel to provider) are more likely to seek health information online.2,16
The older adult as consumer of health information
Overall, older adults are less likely than their younger counterparts to seek health-related information online or offline.14,17,19 A survey study reported that older and less educated African-Americans were more likely than their younger and more educated counterparts to lack necessary skills to use the internet for health information.20 Nevertheless, some older adults have already begun to take advantage of the internet’s potential in helping to meet their health information needs.12,21,22
There is an increasing awareness amongst the older population that, although they may have health problems, they can take action to live healthily. As the aging population is rising and health costs become more expensive, health professionals and policy makers are often stimulating this attitude and the need for more prevention and self-management. People with long term illness such as diabetes or asthma will tend to have specific information needs with regards to, for example, the prevention, management and treatments of their health problems which can change overtime.2
Self-management for the consumer of health information
Self-management of most chronic conditions is characterized by extensive responsibility that patients have to take. Whether self-management means taking medication, making life-style changes or undertaking preventive actions, patients make the day-to-day decisions.23 Self-management entails learning about the illness and treatment options, finding out practical information on healthcare services, and understanding medical jargons.24 Patients seek online information which is comprehensible and tailored to their health situation. 25 They need skills and tools to be empowered to manage their health.26,27 These requirements for “Personalized Information” and “Involvement and Empowerment” are closely tied to, for example, the Dutch e-Citizen Charter,28 an e-Government standard for digital contacts with the citizens.
CHI Challenges to Reach the Multi-Facet Consumers
It is a challenge to the field of Consumer Health Informatics to support the consumer of health information not only to find and assess relevant information on the internet (contextualized and personalized), but also to understand it and act upon it.
Helping consumers to obtain relevant e-health information
Information seeking underpins the person’s motivations and focus, and what has been referred to as the “information journey”.29 This information journey often starts with online searching at a commercial search engine.18,30,31 However, in attempting to obtain health information on the internet from these commercial websites, consumers generally have ineffective search strategies, as indicated by their tendency of using short, overly general queries when conducting online searches.31–34 Zeng and colleagues35 developed the Health Information Query Assistant (HIQuA) system, aiming at facilitating consumer health information retrieval on the internet. Their evaluation results showed that the use of query recommendations enabled by the HIQuA system led to statistically significant higher rates of successful queries.
Another strategy is the use of theoretical models of information seeking in order to drive the development of web-based health applications. For example, the cognitive model of information retrieval (IR) proposed by Sutcliffe and Ennis36 was used in the design of the health website SeniorGezond37 dedicated to older adults in the area of fall prevention.
Helping consumers to assess quality health related websites
With the number of health-related websites growing exponentially in recent years, it has become increasingly more difficult for consumers to assess the quality of health information on the internet, including which websites they can trust. Earlier research suggests that much health information available on many health-related websites was of poor quality and inconsistent with established medical professional guidelines.38,39 Yet, few consumers actually check the origin or date of the information they have found online.2,18,40 Efforts have been made to assess and control the quality of online consumer health information.40–44
A number of organizations and individual researchers have devised new ways (such as user guidance tools, accreditation labels and filtering tools) aiming to help internet users find quality health information. These include: the Centre for Health Information Quality and the DISCERN project in the U.K., the Comprehensive Health Enhancement Support System (CHESS), the MedPICS Certification and Rating of Trustworthy Health Information on the Net, eEurope Quality Criteria for Health related Websites, and Code of the American Medical Association. Despite these efforts, the access to and assessment of quality health information continues to be a challenging task for most consumers. We have reported45 on how difficult it can be for a layperson to assess the quality of information on health-related websites. It appears that these existing tools/guidelines for evaluating the quality of information are not adequately being used by consumers. Moreover, the quality of information is determined not only by the quality of single pieces of information but also how the various pieces of information are organized in a meaningful way for the user.
Helping consumers to understand e-health information
Finding relevant information and assessing its quality are the first building blocks to the empowerment of consumers. An increasingly bigger challenge for CHI is to help consumers understand the health information they have retrieved and assessed so that they can act upon it and make informed decisions. At the same time, people increasingly tend to seek on the internet, tailored and more customized information that can fit their own personal circumstances, including health situation.25,46,47 Some efforts have been made to accommodate consumers’ needs and preferences. For instance, survey data suggest that an important reason that patients and their families turn to the internet to look for genetics-related information is that they hope the internet would provide information in a layperson’s language.48 Recognizing the need to develop online health information resources that are easily accessible and understandable to the lay public, the National Library of Medicine of the National Institutes of Health in the United States designed the Genetics Home Reference site that is “sensitive” to lay people.49
Information understanding can be cognitively demanding for the users, especially elderly users, and it is dependent in part on the context in which the information is given. Durnell Cramton50 has shown that the lack of contextualization (see Table 1) is a common problem in communication under dispersed and technology mediated conditions such as healthcare communication. Contextualization is about providing supportive information to explain a core message (in this case a health message). Contextualization of information can help improving the user’s understanding and sustain an effective human-machine communication. In particular, contextualization of information can help to reduce the user’s cognitive distance (i.e. the difference in knowledge between the user and the website as the information provider). An added dimension to contextualization is that of personalization (see Table 1) which when coupled together provides a form of individualization necessary to understand the health message.
Table 1.
Construct and definitions of the theoretical model.
| Construct | Definition |
|---|---|
| Physician-patient gap | The differences in knowledge and situation between the physician and patient |
| Mutual understanding | Communication is judged to be comprehensible and true |
| Communication complexity | The communicators’ perception of the effort needed to ensure mutual understanding |
| Contextualization | Provision of explicit background information that explains the core message |
| Personalization | Adapting the message to the consumer’s situation and attitude |
Tailoring in the form of contextualization and personalization provides a form of individualization conveying, explicitly or implicitly, that the message is specifically for “you” and make the content more relevant and meaningful to the recipient.51 Furthermore, tailoring means creating two-way communication between the information provider and the user in which information about a given user is used by the provider to determine what specific content the user should receive, the context by which the content will be presented, and through which channels the content will be delivered.51
Bridging the Gap Between Consumer’s Access to Information and Consumer’s Understanding
It has become of prime importance to develop Information and Communication Technology (ICT) based tools that can provide tailored information (contextualized and personalized) in order to support the consumer’s capacity to understand health-related web-based resources. Evidence from the literature indicates that tailored web-based applications are promising (e.g. for dietary behaviors).52,53 However, more research is needed with regards to the consumers’ cognitive abilities in understanding the health information they receive. There is a need to bridge the gap between the provider’s perspective and the patient’s perspective. Perspective taking is a necessary step for patient’s understanding and needs to be supported by ICT.54
To address this problem, an approach using a theoretical framework of communication is proposed54 and the use of dedicated instruments to measure the user’s understanding and the user’s personal cognitive ability. The research that is carried out55,56 serves as an illustration to this approach.
Theoretical Framework: Te’eni Model of Communication
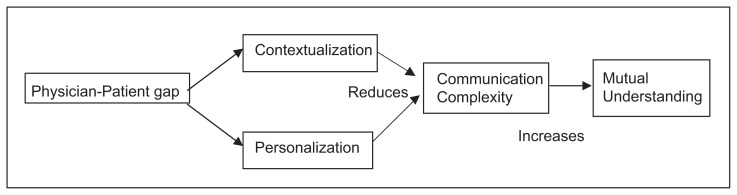
As pointed out in Hawkins et al.51 there is a need to better understand how and why tailoring of health information works. In order to investigate tailoring, specifically with a focus on the user’s understanding within the setting of ICT-based healthcare communication, we are guided by the model of communication proposed by Te’eni.54 Te’eni introduces the notion of communication complexity as the communicator’s perception of the cognitive effort needed to ensure effective communication. Effective communication results from the use of cognitive resources to overcome the difficulties in understanding and uncertainties about the message. Another construct of this model is that of mutual understanding (MU) which requires that the communication be comprehensible according to the sender’s intended meaning and the user’s cognitive capacity (see Fig. 1 and Table 1).
Figure 1.
Te’eni model of communication.
Effective contextualization and personalization reduces communication complexity and makes it easier for the consumer to understand and trust information.54 Contextualization is the provision of background information that explains the message (e.g. explanations of medical terms and statements). However, contextualization is effective only when needed57 and can be counterproductive for consumers who already understand and trust the information. Similarly, personalization (i.e. fitting the information to the person’s situation) reduces communication complexity and makes it easier for the consumer to understand and assimilate the message.54 Tailoring the information to the consumer’s specific situation means that there is less demand on the consumer to transform and translate the information. Consequently the communication complexity is reduced and this leads to easier and less erroneous communication.
Te’eni found that communication complexity is due to the intensity of information, the diversity of views, and the incompatibility between representations and use of information. The differences in knowledge and terminology between physicians and patients create a high level of communication complexity because the perspectives held by both parties are very different and the transformation needed from the physician’s representation to that of the patient is substantial. The initial communication complexity inherent in the communication between these two parties is high and must be reduced in order to increase mutual understanding. The provision of contextual information such as explanations and demonstrations of concrete solutions to causes of relevant problems is necessary to create a common ground between the communicators.58 Similarly, personalizing the information communicated so that it applies directly to the characteristics of the patient or of the situation the patient faces (e.g. the specific situation the patient is experiencing) reduces complexity by requiring less transformations or adaptations.54 When users need to select, translate or adapt information before applying it to their needs, the chances of error, misunderstanding and frustration grow.59
Measurement Instrument for Information Understanding
Alongside the theoretical framework, instruments are needed to be able to measure the user’s level of understanding given the presence (or lack) of contextualization and personalization; in other words, to measure what Te’eni defines as mutual understanding (MU). Within the theoretical framework of Te’eni, MU is about person-to-person understanding (one user understanding another user). In our setting, it is about person-to-system understanding.56 In other words, it is about the user’s understanding or comprehension of the information he or she has found; Specifically, MU as the outcome parameter was developed based on Bloom’s taxonomy of learning outcomes.60 This taxonomy includes six hierarchical levels for learning outcomes: knowledge, comprehension, application, analysis, synthesis, and evaluation.
Level 1 knowledge: recalling factual information.
Level 2 comprehension: explaining the meaning of information, association of concepts, differentiation.
Level 3 application: using information in concrete situations. Application involves the recall of knowledge in combination with comprehension to describe a new situation.
Level 4 analysis: breaking down a whole into its constituting components. Analysis involves analyzing data at hand. It involves for example recognizing unstated assumptions and error in reasoning, making inferences, evaluating relevance of the data.
Level 5 synthesis: putting parts together to form a new and integrated whole. Synthesis involves higher skills of information formation and processing. Synthesis typically involves creating a new product or a combination of ideas to form a new whole.
Level 6 evaluation: making judgments. Typically evaluation is concerned, for example, with making value decision about issues, resolving controversies or differences of opinion, and developing opinions and judgments.
This taxonomy provides a useful structure to categorize and prepare test questions in the MU instrument we developed. This instrument, measures the first four levels of the taxonomy with a total of seven problems: two at level 1 (knowledge); two at level 2 (comprehension); two at level 3 (application) and one at level 4 (analysis). The MU instrument took the form of open questions, statements measured on a Likert Scale for agreement/disagreement, and open questions based on a case description. The last two levels are not included since they are more relevant for testing professionals (or trainees) in the field rather than lay people (this study’s targeted group). The MU instrument was reviewed by two professionals from the rheumatology department at LUMC. They insured the accuracy of the problems presented to the participants and the appropriate level of difficulty of the task. The total score of the questions for all the categories makes up the MU score which is scaled with three levels: Low (0–15), Medium (16–31), and High (32–42).
While using a website to obtain needed health information, users are in a learning situation in that they are acquiring knowledge about, for instance, a specific condition or treatment. Thus, it was chosen to measure MU from a learning perspective and draw from the literature on lifelong learning, distance education and teaching. To our knowledge, this is an innovative and unexplored way to apply this taxonomy.
Measurement Instrument for User’s Profile: The Case of Cognitive Style
Tailoring of health information needs to take into account more personal aspects of the users, for example, the user’s unique cognitive style. Cognitive styles refer to the preferred way an individual organizes, filters, transforms, and processes information. Findings from research suggest that users with different cognitive styles develop different strategies and tactics when seeking information on the Web.61
A person’s cognitive style can be identified using the Group Embedded Figure Test (GEFT).62 This test determines whether a person is field dependent (i.e. approaches a problem in a holistic, global way) or field independent (i.e. approaches a problem in an analytical, deterministic way). Although information seeking is dependent on the operation of the same basic cognitive processes, not every person exhibits the same information seeking tactics. Information seeking behavior is highly variable because it is associated with elements or characteristics that are significantly different from one individual to the other. The validity of the GEFT instrument was established and reported by62 based on its parent test, the Embedded Figures Test. Moreover, the GEFT is a standardized instrument with a reliability estimate of 0.82.
The Seniorgezond Website: An Example of ICT-Based Contextualization
Based on the theoretical framework of Te’eni, and using the measurement instruments above mentioned, a study was carried out in order to gain better insights on how tailoring works.56 A randomized controlled experimental design was chosen, using the SeniorGezond websitea we had previously developed as a test-bed.63 The study consisted of a pre-test, the intervention with the website, and a post-test. Participants (n = 40) were randomly assigned to exposure or no exposure to contextualization with the website. This study demonstrates only one of the two strategies that is proposed, namely contextualization.
The information structure of the website was used as the starting point to manipulate contextualization of information within the website. The information within the website is structured around problems of ‘fall’ incidences, and contains four levels of information. The top level ‘Causes of falls’ include frequently occurring problems in the domain of fall incidences (e.g. dizziness). The second level ‘Solutions’ focuses on possible interventions and advices associated with the causes of falling e.g. use of a walking aid. Solutions are supported by the third level ‘Products and Services’ e.g. walking aids, fitness programs. From the Products and Services level, users can access the ‘Supportive Facts’ which makes up the fourth and lowest level of the information trees. Supportive Facts contain addresses about where to purchase products and services, as well as insurance information. The four levels take the user from general to specific information. Manipulation of the contextualization was achieved by removing the Solutions level (second level) as well as cross-links to the other levels from the navigation. The Solutions level embeds relevant contextualization since it acts as a buffer between the Causes (background information) level and the Products and Services level. The Products and Services level only provides descriptions about products such as walking-aid and services such as sport and physical exercises. Without the Solutions level, there is no information about the reasons that one should select one of these products or services.
Results from this study provide empirical evidence that contextualization significantly increases understanding for non-knowledgeable users. Furthermore, participant’s cognitive style was found to be a significant factor on understanding. We also found that participants bring their own contexts such as social context and psychological context to support their understanding.
Discussion and Directions for Further Research
Challenges for the design of CHI web applications
Designing web-based healthcare applications with functionalities of contextualization and personalization can strengthen the already existing informative functions of the Web and is a step further towards better understanding of the user’s personal situations and preferences. There has been an extensive growth of health research on supporting consumers and patients at home (e.g. see the International Conferences on Pervasive Computing Technologies for Healthcare), and on persuading individuals to adhere to “healthy” behavior (e.g. see the International Conferences “Persuasive”). However, there is not yet a coherent, theoretically and empirically sound set of models, methods and guidelines for contextualization and personalization, specifically for self-management systems to accommodate various types of patients with chronic conditions. There is therefore a strong need to develop guidelines for ICT-based tools for contextualization and personalization which will be part of the design requirements for health-related websites.
Within the setting of the study that was carried out with the SeniorGezond website, one whole level of interventions was chosen (the Solutions level) as context. However, it is not the unique possibility. More research needs to be done in this area. In particular, needs assessment and requirements should be carried out not only for contextualization but also for personalization in order to design and develop ICT-based tailored applications. This new research area needs to take into account the variety of existing health portals and the different groups of patients with chronic conditions.
As we strive to define these guidelines of contextualization and personalization, we also should take into account the users’ own personal contexts. Results from our study56 indicate that there is a gap between the informational contexts proposed to the website visitors (such as the level of possible solutions) and the user’s personal contexts. This problem should be addressed in order to insure that both, top-down (from the expert to the user) and bottom-up (from the user to the expert) approaches to contexts can be coupled in order to develop coherent contextualization and personalization guidelines.
Benefits for consumers and patients
Bridging the gap between access to information and information understanding can empower consumers (in particular those with chronic conditions) by enhancing their comprehension of information and, subsequently, act upon the information. Patient empowerment efforts should be targeted to where there is a significant potential for improving patients’ control and autonomy. Changes in health condition can better be understood and decisions can be better made by the patient on the basis of informed choices and education. ICT-based contextualization and personalization of health information provide a new research avenue to support this process of patient empowerment.64 Being an informed patient requires a good level of information literacy and health literacy65 and is a lifelong learning process. A better comprehension of the terminology employed through contextualization can raise health literacy level. Components of contextualization and personalization of information in self-management systems have a role to play as a pre-requisite in raising the website visitor’s health literacy and eventually his lifelong learning development.
Benefits for the healthcare professionals
The healthcare professionals who will in the near future decrease in number and who currently handle more and more chronically ill patients have to manage increasing workload.66 Healthcare services therefore need to be more efficient and effective. In addition, stimulating self-management of patients with chronic conditions can have a positive influence on the use of healthcare services. A transfer of care activities from the healthcare providers to the patients could be achieved by equipping patients with adequate tailored tools (in particular, dedicated for self-management). In this way, patients become real partners in the care process, and healthcare professionals can treat more serious patient cases.
Conclusion
Consumers of health information on the internet are evolving. They surf the internet more often to find health related information, are more active in their own healthcare, and are more information technology minded. Furthermore, the profile of health information consumers is changing due to an increase in the aging population who often have to manage chronic conditions. Consumers have access to a large number of health-related websites, whose contents are not always easy to comprehend. Efforts have been in made in the past to help consumers find relevant information, assess the information quality and increase their e-health literacy. The issue of information understanding is now coming to the forefront. While it has been acknowledged that health information should be tailored to reach more consumers, limited research has been carried out to enable the emerging consumers of health information to bridge the gap between access to information and information understanding. From our point of view it is important to focus not only on contextualization but also on personalization and how they are intertwined. This paper has reported on a theory-driven approach to address this issue, advocating, 1) the development of measurement instruments for evaluation of these dedicated tools, and 2) the development of guidelines, driven by theory, for designing ICT-based contextualization and personalization of information tools.
Acknowledgements
The authors would like to thank J.W. Schoones (Walaeus Library, LUMC), our colleagues Regina Overberg and Herman Lodder from the Clinical Informatics Group, and Ton Rövekamp (TNO Quality of Life, Leiden). Bo Xie has been funded in part with federal funds from the National Library of Medicine, National Institutes of Health, under Contract No NO1-LM-6–3502.
Footnotes
Disclosure
The authors report no conflicts of interest.
References
- 1.Bylund CL, Sabee CM, Imes RS, Sanford AA. Exploration of the construct of reliance among patients who talk with their providers about internet information. Journal of Health Communication. 2007;12:17–28. doi: 10.1080/10810730601091318. [DOI] [PubMed] [Google Scholar]
- 2.Fox S. E-patients with a disability or chronic disease. Washington, DC: PEW internet and American Life; 2007. (available at: http://www.pewinternet.org/pdfs/EPatients_Chronic_Conditions_2007.pdf) [Google Scholar]
- 3.Huntington P, Nicholas D, Jamali HR, Russell C. Health information for the consumer: NHS vs. the BBC. Aslib Proceedings. 2007;59:46–67. [Google Scholar]
- 4.Eysenbach Recent advances: Consumer Health Informatics. BMJ. 2000;320:1713–1716. doi: 10.1136/bmj.320.7251.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eysenbach Design and evaluation of consumer health information web sites. Lewis, et al., editors. Consumer Health Informatics. 2005:34–60. [Google Scholar]
- 6.Ballard-Reisch DS. A model of participative decision making for physician-patient interaction. Health Communication. 1990;2:91–104. [Google Scholar]
- 7.Mcnutt RA. Shared medical decision making: problems, process, progress. JAMA. 2004;292:2516–8. doi: 10.1001/jama.292.20.2516. [DOI] [PubMed] [Google Scholar]
- 8.Evans S, Tritter J, Barley V, et al. User involvement in U.K. cancer services: bridging the policy gap. European Journal of Cancer Care (Engl) 2003;12(4):331–8. doi: 10.1046/j.1365-2354.2003.00431.x. [DOI] [PubMed] [Google Scholar]
- 9.Hassol A, Walker JM, Kidder D, et al. Patient experiences and attitudes about access to a patient electronic health care record and linked Web messaging. Journal of American Medical Informatics Association. 2004;11:505–513. doi: 10.1197/jamia.M1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Masys D, Baker D, Butros A, Cowles KE. Giving patients access to their medical records via the internet: the PCASSO experience. Journal of American Medical Informatics Association. 2002;9:181–91. doi: 10.1197/jamia.M1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winkelman WJ, Leonard KJ, Rossos PG. Patient-perceived usefulness of online electronic medical records: employing grounded theory in the development of information and communication technologies for use by patients living with chronic illness. Journal of American Medical Informatics Association. 2005;12:306–14. doi: 10.1197/jamia.M1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xie B. (In press) Older adults’ health information wants in the internet age: Implications for patient-provider relationships. Journal of Health Communication. doi: 10.1080/10810730903089614. [DOI] [PubMed] [Google Scholar]
- 13.Morahan-Martin JM. How internet users find, evaluate, and use online health information: A cross-cultural review. CyberPsychology and Behavior. 2004;7:497–510. doi: 10.1089/cpb.2004.7.497. [DOI] [PubMed] [Google Scholar]
- 14.Maibach EW, Weber D, Massett H, Hancock GR, Price S. Understanding consumers’ health information preferences: development and validation of a brief screening instrument. Journal of Health Communication. 2006;11:717–36. doi: 10.1080/10810730600934633. [DOI] [PubMed] [Google Scholar]
- 15.Dickerson S, Reinhart AM, Feeley TH, et al. Patient internet use for health information at three urban primary care clinics. Journal of American Medical Informatics Association. 2004;11:499–504. doi: 10.1197/jamia.M1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bundorf MK, Wagner TH, Singer SJ, Baker LC. Who searches the internet for health information? Health Services Research. 2006;41:819–36. doi: 10.1111/j.1475-6773.2006.00510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fox S. Health Information Online. Washington, DC: Pew internet and American Life Project; Retrieved March 16, 2007, from http://www.pewinternet.org/pdfs/PIP_Healthtopics_May05.pdf.2005. [Google Scholar]
- 18.Fox S. Online Health Search. Washington, DC: PEW internet and American Life; 2006. (available at: http://www.pewinternet.org/pdfs/PIP_Online_Health_2006.pdf) [Google Scholar]
- 19.Hill SA, Laugharne R. Decision making and information seeking preferences among psychiatric patients. Journal of Mental Health. 2006;15:75–84. [Google Scholar]
- 20.Carlson BA, Neal D, Magwood G, Jenkins G, King MG, Hossler CL. A community-based participatory health information needs assessment to help eliminate diabetes information disparities. Health Promotion Practice. 2006;7:213S–22S. doi: 10.1177/1524839906288694. [DOI] [PubMed] [Google Scholar]
- 21.Kaiser Family Foundation. e-Health and the elderly: how seniors use the internet for health information. 2005. Retrieved March 12, 2008 from http://www.kff.org/entmedia/upload/e-Health-and-the-Elderly-How-Seniors-Use-the-internet-for-Health-Information-Key-Findings-From-a-National-Survey-of-Older-Americans-Survey-Report.pdf.
- 22.Hardt JH. Older adults seeking healthcare information on the internet. Educational Gerontology. 2007;3:561–72. [Google Scholar]
- 23.Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. The Lancet. 2004;364:1523–37. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- 24.Barlow J, Wright C, Sheasby J, Turner A, Hainswirth J. Self-management approaches for people with chronic conditions: a review. Patient Education and Counseling. 2002;48:177–87. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 25.Keselman A, Logan R, Smith CA, Leroy G, Zeng-treitler Q. Developing Informatics Tools and Strategies for Consumer-centered Health Communication. Journal of the American Medical Informatics Association. 2008;15(4):473–783. doi: 10.1197/jamia.M2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lorig K, Ritter PL, Laurent DD, Plant K. Internet-based chronic disease self-management: A randomized trial. Medical Care. 2006;44(13):964–71. doi: 10.1097/01.mlr.0000233678.80203.c1. [DOI] [PubMed] [Google Scholar]
- 27.Aujoulat I, d’Hoore W, Deccache A. Patient empowerment in theory and practice: Polysemy or cacophony? Patient Education and Counseling. 2007;66:13–20. doi: 10.1016/j.pec.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 28.BurgerServiceCode. available at http://www.burger.overheid.nl/files/workbook_ecc_english.pdf.2006.
- 29.Attfield S, Adams A, Blandford A. Patient information needs: pre and post consultations. Health Informatics Journal. 2006;12:165–77. doi: 10.1177/1460458206063811. [DOI] [PubMed] [Google Scholar]
- 30.Peterson G, Aslani P, AWK How Do Consumers Search For And Appraise Information On Medicines On The Internet? A qualitative study using focus groups. Journal of Medical Internet Research. 5 doi: 10.2196/jmir.5.4.e33. Retrieved January 23, 2007 from http://www.jmir.org/2003/4/e33/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eysenbach G, Köhler C. How do consumers search for and appraise health information on the world wide web? Qualitative study using focus groups, usability tests, and in-depth interviews. BMJ. 2002;324:573–77. doi: 10.1136/bmj.324.7337.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeng QT, Kogan S, Polvnick RM, Crowell J, Lacroix EM, Greenes RA. Positive Attitudes And Failed Queries: An Exploration Of The Conundrums Of Consumer Health information retrieval. International Journal of Medical Informatics. 2004;73:45–55. doi: 10.1016/j.ijmedinf.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 33.Zeng QT, Kogan S, Ash N, Greenes RA, Boxwala AA. Characteristics of consumer terminology for health information retrieval. Methods of information in medicine. 2002;41:289–98. a http://www.seniorgezond.nl. [PubMed] [Google Scholar]
- 34.Xie B. Older adults, health information, and the internet. ACM Interactions. 2008;15:44–6. [Google Scholar]
- 35.Zeng QT, Crowell J, Plovnick RM, Kim E, Ngo L, Dibble E. Assisting consumer health information retrieval with query recommendations. Journal of American Medical Informatics Association. 2006;13:80–90. doi: 10.1197/jamia.M1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sutcliffe A, Ennis M. Towards a cognitive theory of information retrieval. Interact Comput. 1998;10:321–51. [Google Scholar]
- 37.Alpay LL, Toussaint PJ, Ezendam NPM, Rovekamp T, Graafmans W, Westendorp R. Easing internet access of health information for the elderly users: design considerations and usability. Health Informatics Journal. 2004;10(3):185–94. [Google Scholar]
- 38.Berland GK, Elliott MN, Morales LS, Algazy JI, Kravitz RL, Broder MS. Health information on the internet: accessibility, quality, and readability in English and Spanish. Journal of the American Medical Association. 2001;285:2612–21. doi: 10.1001/jama.285.20.2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Griffiths KM, Christensen H. Quality of web based information on the treatment of depression: cross sectional survey. British Medical Journal. 2000;321:1511–15. doi: 10.1136/bmj.321.7275.1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eysenback G, Powell J, Kuss O. Empirical studies assessing the quality of health information for consumers on the World Wide Web: a systematic review. Journal of the American Medical Association. 2002;287 doi: 10.1001/jama.287.20.2691. [DOI] [PubMed] [Google Scholar]
- 41.Childs S. Judging the quality of internet-based health information. Performance Measurement and Metrics. 2005;6:80–96. [Google Scholar]
- 42.Kunst H, Groot D, Latthe P. Accuracy of information on apparently credible websites: survey of common health topics. British Journal of Medicine. 2002;324:581–82. doi: 10.1136/bmj.324.7337.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fallis D, Fricke M. Indicators of accuracy of consumer health information on the internet: a study of indicators relating to information for managing fever in children in the home. Journal of American Medical Informatics Association. 2002;9:73–9. doi: 10.1136/jamia.2002.0090073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morahan-Martin JM, Anderson C. Information and misinformation online: recommendations for facilitating accurate mental health information retrieval and evaluation. CyberPsychology and Behavior. 2000;3:731–42. [Google Scholar]
- 45.Alpay LL, Overberg RI, Zwetsloot-Schonk JHM. Empowering citizens in assessing health related websites: a driving force for healthcare governance. International Journal of Healthcare Technology and Management (IJHTM) 2007a;8(1/2):141–160. doi: 10.1504/IJHTM.2007.012103. Special issue: Governing ICT in healthcare and governing healthcare with ICT. [DOI] [Google Scholar]
- 46.Cobb NK, Graham AL. Characterizing Internet Searchers of Smoking Cessation Information. [last accessed October 2008];J Med internet Res. 2006 8(3):e17. doi: 10.2196/jmir.8.3.e17. http://www.jmir.org/2006/3/e17/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smilde-van den Doel DA. Personalisatie en contextualisatie van informatie op internet vanuit het perspectief van patiënten: Een korte inventarisatie via een focusgroep tijdens de voorbereiding van een subsidieaanvraag. Pallas Report (Pallas Health Research and Consultancy) 2008 May; (in Dutch) [Google Scholar]
- 48.Taylor MR, Alman A, Manchester DK. Use Of the internet by patients and their families to obtain genetics-related information. Mayo Clinic Proceedings. 2001;76:772–6. doi: 10.1016/S0025-6196(11)63219-9. [DOI] [PubMed] [Google Scholar]
- 49.Mitchell JA, Fun J, Mccray AT. Design Of genetics homw reference: a new NLM consumer health resource. Journal of American Medical Informatics Association. 2004;11:439–47. doi: 10.1197/jamia.M1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Durnell Cramton C. The Mutual Knowledge Problem and Its Consequences for Dispersed Collaboration. Organiz Sci. 2001;12(3):346–371. [Google Scholar]
- 51.Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Education Research. 2008;23(3):454–66. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oenema A, Brug J, Lechner L. Web-based tailored nutrition education: results of a randomized controlled trial. Health Education Research. 2001;16(6):647–60. doi: 10.1093/her/16.6.647. [DOI] [PubMed] [Google Scholar]
- 53.Kroeze W, Werkman A, Brug J. A Systematic Review of Randomized Trials on the Effectiveness of Computer-Tailored Education on Physical Activity and Dietary Behaviors. Annals of Behavioral Medicine. 2006;31(3):205–223. doi: 10.1207/s15324796abm3103_2. [DOI] [PubMed] [Google Scholar]
- 54.Te’eni D. Review: A cognitive-affective model of organizational communication for designing IT. MIS Quarterly. 2001;25(2):251–312. [Google Scholar]
- 55.Alpay LL, Verhoef J, Toussaint PJ, Zwetsloot-Schonk JHM. What makes an “informed patient”? The impact of contextualization on the search for health information on the internet. In: Hasman, et al., editors. Ubiquity: Technologies for better health in aging societies; Proceedings of Medical Informatics Europe (MIE); Maastricht, The Netherlands. 2006. pp. 913–19. [PubMed] [Google Scholar]
- 56.Alpay LL, Verhoef J, Te’eni D, Putter H, Toussaint PJ, Zwetsloot-Schonk JHM. Can Contextualization Increase Understanding During Man-Machine Communication? A Theory-Driven Study. The Open Medical Informatics Journal. 2008;2:82–91. doi: 10.2174/1874431100802010082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Katz A, Te’eni D. The Contingent Impact of Contextualization on Computer-Mediated Collaboration. Organization Science. 2007;18(2):261–279. doi: 10.1287/orsc.1060.0237.. [DOI] [Google Scholar]
- 58.Gumperz JJ. Discourse Strategies. Cambridge University Press; Cambridge: 1982. [Google Scholar]
- 59.Te’eni D, Feldman R. Performance and satisfaction in adaptive websites: a laboratory experiment on search tasks within a task-adapted website. Journal of AIS. 2001;2(3):1–28. [Google Scholar]
- 60.Bloom B. Taxonomy of educational objectives: the classification of educational goals: Handbook 1, Cognitive Domain. Longmans; New York: 1956. [Google Scholar]
- 61.Kim P, Eng TR, Deering MJ, Maxfield A. Published criteria for evaluating healthrelated websites: review. BMJ. 1999;318(7184):647–49. doi: 10.1136/bmj.318.7184.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Witkin HA, Ottman PK, Raskin E, Karp SA. A manual for the embedded figures tests. Consulting Psychologists Press; Palo Alto, CA: 1971. [Google Scholar]
- 63.Alpay LL, Toussaint PJ, Ezendam NPM, et al. The Dutch website “SeniorGezond”: An illustration of a road map for the informed patient. Managed Care (Swiss Revue) 2007b. Available online www.tellmed.ch Fachliteratur, Managed Care Nr.2 2007. 2007b.
- 64.Kivits J. Researching the ‘Informed Patient’: the case of online information seekers. Information, Communication and Society. 2004;4:510–530. [Google Scholar]
- 65.McCray AT. Promoting Health Literacy. Journal of the American Medical Informatics Association. 2005;12(2):152–63. doi: 10.1197/jamia.M1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Baker L, Rideout J, Gertler P, Raube K. Effect of an internet-based system for doctor-patient communication on health care spending. Journal of American Medical Informatics Association. 2005;12:530–36. doi: 10.1197/jamia.M1778. [DOI] [PMC free article] [PubMed] [Google Scholar]