Abstract
Noonan syndrome (NS) is a relatively common, clinically variable and genetically heterogeneous developmental disorder characterized by postnatally reduced growth, distinctive facial dysmorphism, cardiac defects and variable cognitive deficits. Other associated features include ectodermal and skeletal defects, cryptorchidism, lymphatic dysplasias, bleeding tendency, and, rarely, predisposition to hematologic malignancies during childhood. NS is caused by mutations in the PTPN11, SOS1, KRAS, RAF1, BRAF and MEK1 (MAP2K1) genes, accounting for approximately 70% of affected individuals. SHP2 (encoded by PTPN11), SOS1, BRAF, RAF1 and MEK1 positively contribute to RAS-MAPK signaling, and possess complex autoinhibitory mechanisms that are impaired by mutations. Similarly, reduced GTPase activity or increased guanine nucleotide release underlie the aberrant signal flow through the MAPK cascade promoted by most KRAS mutations. More recently, a single missense mutation in SHOC2, which encodes a cytoplasmic scaffold positively controlling RAF1 activation, has been discovered to cause a closely related phenotype previously termed Noonan-like syndrome with loose anagen hair. This mutation promotes aberrantly acquired N-myristoylation of the protein, resulting in its constitutive targeting to the plasma membrane and dysregulated function. PTPN11, BRAF and RAF1 mutations also account for approximately 95% of LEOPARD syndrome, a condition which resembles NS phenotypically but is characterized by multiple lentigines dispersed throughout the body, café-au-lait spots, and a higher prevalence of electrocardiographic conduction abnormalities, obstructive cardiomyopathy and sensorineural hearing deficits. These recent discoveries demonstrate that the substantial phenotypic variation characterizing NS and related conditions can be ascribed, in part, to the gene mutated and even the specific molecular lesion involved.
Key Words: Cardiofaciocutaneous syndrome, Costello syndrome, Genotype-phenotype correlations, LEOPARD syndrome, Molecular basis of disease, Molecular epidemiology, Mutation analysis, Neurocardiofacialcutaneous syndrome family, Noonan syndrome, RAS signaling
Introduction
Noonan syndrome (NS, OMIM 163950) is the eponymous name for the disorder described by the pediatric cardiologist Jacqueline Noonan more than 40 years ago [Noonan, 1968]. She based the description of this putatively novel syndrome on observations made in 9 patients with pulmonic stenosis, a distinctive dysmorphic facial appearance with hypertelorism, ptosis and low-set ears, webbed neck, and chest deformities. Several male patients also had cryptorchidism. NS is thought to be relatively common, although its prevalence has not been determined accurately to date. Most authors cite the figure of 1 in 1,000–2,500 live births firstly reported by Nora et al. [1974], but that estimate is not based on a population study.
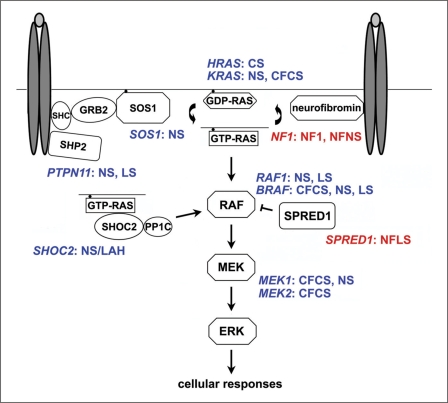
NS is a Mendelian trait transmitted in an autosomal dominant manner. Rare cases with parental consanguinity have been described [van der Burgt and Brunner, 2000], but it is not clear whether these represent true instances of autosomal recessive inheritance. A significant, but not precisely determined percentage of cases is due to de novo mutations. NS is genetically heterogeneous, and, based upon the recent discoveries of the underlying disease genes, it can now be regarded as a disorder of upregulated RAS-MAPK signaling (fig. 1). Depending on the cellular context, this pathway mediates diverse biological functions such as proliferation, migration, survival, cell fate determination, differentiation and senescence, predominantly through the regulation of transcription, cytoskeletal rearrangement and metabolism. The RAS-MAPK cascade is activated in response to cytokine, hormone and growth factor stimulation, and is a major mediator of early and late developmental processes, including morphology determination, organogenesis, synaptic plasticity processes and growth. Due to its nodal role in signal transduction, signal traffic through this pathway is tightly controlled, and its enhanced activation has been established to contribute significantly to oncogenesis (see below) [Bos, 1989; Davies et al., 2002; Rajalingam et al., 2007].
Fig. 1.
Schematic diagram showing the RAS-MAPK signal transduction pathway and affected disease genes in disorders of the neurocardiofacialcutaneous syndrome family. The double ovals in dark grey and the light grey ovals represent generic dimerized cell-surface receptors binding to their ligand. Abbreviations: CFCS, cardiofaciocutaneous syndrome; CS: Costello syndrome; LS, LEOPARD syndrome; NF1, neurofibromatosis type 1; NFLS, neurofibromatosis type 1-like syndrome (also termed Legius syndrome); NFNS, neurofibromatosis-Noonan syndrome; NS, Noonan syndrome; NS/LAH, Noonan-like syndrome with loose anagen hair.
Thus far, 7 genes (PTPN11, SOS1, KRAS, RAF1, BRAF, SHOC2 and MEK1, alias MAP2K1) have been causally related to NS or closely related conditions, including LEOPARD syndrome and Noonan-like syndrome with loose anagen hair. Germline mutations in a subgroup of those genes as well as in genes encoding signal transducers participating in the same pathway (HRAS, KRAS, NF1, SPRED1, BRAF, MEK1 and MEK2, alias MAP2K2) have been identified to be implicated in other clinically related disorders (Costello syndrome, cardiofaciocutaneous syndrome, neurofibromatosis type 1 and Legius syndrome) (fig. 1) [Schubbert et al., 2007b]. This shared pathogenetic mechanism and clinical overlap justify the grouping of these developmental diseases in a single family of disorders, which has been termed the neurocardiofacialcutaneous syndrome (NCFCS) family. In this review, we outline the clinical aspects and molecular genetics of NS and associated phenotypes.
Clinical Features
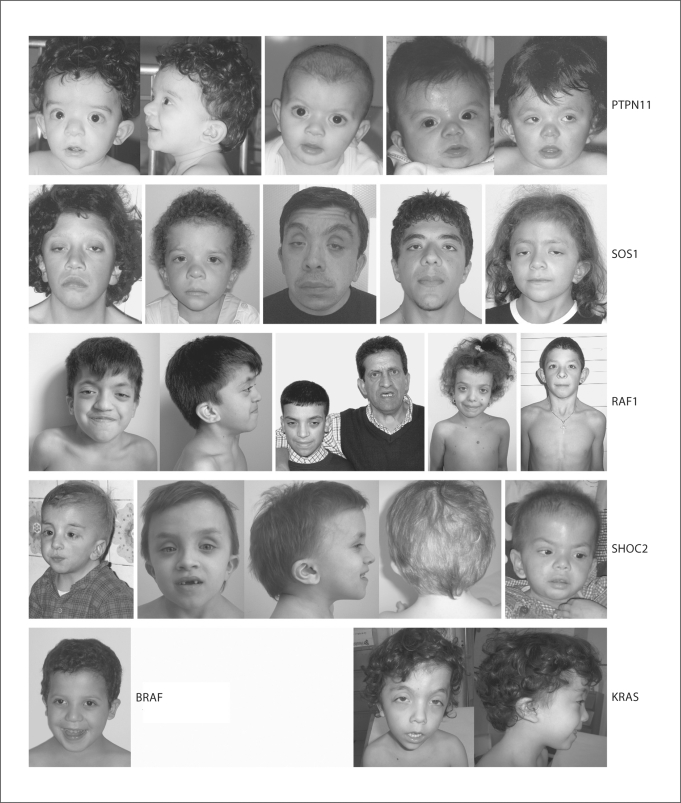
Clinical manifestations of NS include a typical dysmorphic appearance, congenital heart defects (CHD) or hypertrophic cardiomyopathy (HCM), webbing of the neck, postnatal reduced growth, cryptorchidism, eye abnormalities, and skeletal anomalies such as pectus deformities, cubitus valgus, and vertebral defects. Other relatively common features are bleeding diathesis, ectodermal anomalies, lymphatic dysplasias, and variable cognitive deficits. Diagnosis is made by clinical examination [Noonan, 1994; Allanson, 2007; van der Burgt, 2007]. While a comprehensive scoring system has been developed to aid in clinical diagnosis [Duncan et al., 1981; van der Burgt et al., 1994], most clinicians continue to use a more subjective assessment. NS is characterized by marked variability (fig. 2), and the phenotype becomes less pronounced with age [Allanson et al., 1985a]. For these reasons and because of the clinical overlap with other related disorders (see below), establishing the diagnosis can be very difficult, especially in adulthood. Genetic testing is now available and is capable of confirm diagnosis in a large percentage of cases (approx. 70%, in our experience), which, however, is strictly dependent on the diagnostic criteria used to make diagnosis.
Fig. 2.
Dysmorphic facial features in Noonan syndrome. Series of affected individuals heterozygous for mutations in different disease genes are shown.
NS facial features and signs include high forehead, hypertelorism, downslanting palpebral fissures, epicantal folds, ptosis, low-set and/or posteriorly rotated ears (fig. 2). A short and/or webbed neck and a low posterior hairline commonly occur.
The type and severity of the cardiac disease can vary from trivial to life-threatening [Burch et al., 1993; Marino et al., 1999; Bertola et al., 2000]. Pulmonic stenosis and HCM are the most common forms of cardiac disease, but a wide range of other lesions, including atrioventricular septal defects and aortic coarctation, are also observed. Newborns, infants and children suspected of having NS need a careful cardiac evaluation, including an echocardiogram. Evaluation of the heart in early infancy does not exclude the possibility that an affected child will develop more severe HCM later in childhood. This suggests that serial evaluations during this period are indicated.
Feeding problems are noted in the majority of affected infants and can cause failure to thrive [Shah et al., 1999]. For some patients, the inadequacy in oral intake may be severe enough to necessitate placement of gastrostomy tubes, although occupational/feeding therapy is an adequate intervention for most. In most patients, feeding difficulties resolve by around age 18 months.
Developmental delay and learning problems are quite common in NS, perhaps affecting one-third of patients [Sharland et al., 1992a]. Some motor delay can be attributed to the hypotonia often observed in affected infants. However, increased prevalence of attention deficit/hyperactivity disorder and frank mental retardation are also observed. More significant neurological problems, such as epilepsy, are noted in a small minority of patients. Available data indicate that the heterogeneity in cognitive abilities observed in NS is at least partially to be ascribed to the individual affected genes and type of mutation involved [Cesarini et al., 2009; Pierpont et al., 2009]. Specifically, mutations affecting transducers upstream of RAS appear to be less frequently associated with mental retardation. In contrast, mutations in downstream components of the pathway are generally associated with a more severe cognitive impairment. Of note, moderately impaired social cognition in terms of emotion recognition and alexithymia in adult subjects with NS has also been reported [Verhoeven et al., 2008].
Visual problems commonly occur in NS [Lee et al., 1992; Alfieri et al., 2008]. Ophthalmological and orthoptic evaluation of a relatively large cohort of patients who were also assessed for behavioral visual tests (crowding acuity and stereopsis) and visuo-motor integration (VMI) test documented that more than 80% of subjects exhibit abnormalities in visual function and one-third of individuals has abnormalities on VMI [Alfieri et al., 2008]. Abnormal ocular movements and weak or absent stereopsis occur most commonly. Similarly, hearing loss has been described in about 40% of patients [Cremers and van der Burgt, 1992; Qiu et al., 1998]. Auditory problems have been correlated with the abnormal craniofacial anatomy, particularly of the temporal bone [Naficy et al., 1997].
One of the salient features of NS is short stature, with median heights of less than the 3rd centile in affected children [Witt et al., 1986; Ranke et al., 1988]. In an attempt to increase adult stature, efforts have been undertaken to study the effects of growth hormone (GH) therapy during childhood [for a recent review of surveys, see Padidela et al., 2008]. There appears to be a scientific basis for this since studies of GH secretion in this disorder have documented some quantitative and qualitative abnormalities [Ahmed et al., 1991; Tanaka et al., 1992; Noordam et al., 2002]. In addition, some of the proteins altered in NS have been linked directly with the intracellular signaling pathway controlling the cellular response to GH. While initial studies reporting results from a single year of therapy demonstrated significant acceleration in linear growth, reports of longer courses have been less encouraging, possibly due to the effect of long-term GH therapy on bone maturation. A recent prospective survey on the effect of long-term GH treatment on adult height in NS, however, documented a significant mean height gain, and did not confirm occurrence of bone age acceleration during the first years of GH treatment [Noordam et al., 2008]. Similarly, an unrelated study indicated that GH might significantly improve height in children with NS with earlier initiation of therapy [Romano et al., 2009]. There are studies indicating that affected subjects with PTPN11 gene mutations (see below) tend to exhibit mild GH resistance and relatively poor response to GH treatment [Binder et al., 2005; Ferreira et al., 2005], but this association has not been confirmed in a recent long-term survey [Noordam et al., 2008]. One additional concern have been the potential adverse effects of GH on the heart in NS patients with HCM, while reports have emphasized the fact that cardiac phenotypes other than HCM (considered by some to be a contraindication for GH therapy) were unaffected after therapy [Cotterill et al., 1996; MacFarlane et al., 2001; Noordam et al., 2001; Brown et al., 2002].
Orthopedic problems are common in NS [Sharland et al., 1992a]. For instance, pectus deformities are observed in the vast majority, but are rarely severe enough to warrant surgical intervention. Scoliosis occurs in approximately 10% of patients. Other bony defects, such as vertebral anomalies, occur at low frequency.
Bleeding diathesis frequently occurs in patients with NS. The most common abnormalities include von Willebrand disease, deficiencies of factors XI and XII, and thrombocytopenia [Sharland et al., 1992b; Massarano et al., 1996; Singer et al., 1997]. Since many affected children will require interventional procedures such as balloon pulmonary valvuloplasty and orchidopexy, this is important to bear in mind to prevent significant hemorrhagic complications. Two childhood leukemias, juvenile myelomonocytic leukemia (JMML, OMIM 607785) and acute lymphoblastic leukemia (ALL), are at increased prevalence in NS, although they affect only a small percentage of patients. The myeloproliferative disorder in children with NS (NS/JMML) may regress without treatment, follow an aggressive clinical course or evolve to acute myeloid leukemia [Bader-Meunier et al., 1997; Fukuda et al., 1997; Choong et al., 1999]. PTPN11 mutation screening in patients with NS/JMML demonstrated association with specific mutations that are rare among patients with NS, demonstrating genotype-phenotype correlation (see below) [Tartaglia et al., 2003; Kratz et al., 2005]. According to this evidence, hematologic examination should be periodically performed during infancy and childhood in patients carrying NS/JMML-associated PTPN11 mutations.
The lymphatic system develops abnormally in NS, although the persistence of lymphedema at birth occurs less frequently than observed in Turner syndrome. Lymphangiectasia affecting the gastrointestinal tract and lungs has presented in infants and children with this disorder [Baltaxe et al., 1975; Herzog et al., 1976; Hernandez et al., 1980; Fisher et al., 1982; Ozturk et al., 2000]. The former complication may lead to protein-losing enteropathy and the latter to spontaneous chylothorax, both being difficult to manage. Some older patients might develop peripheral lymphedema, usually most pronounced in the legs, that is treated with compressive bandages [Lanning et al., 1978].
Renal abnormalities are found in a minority of affected children, but warrant a screening with an abdominal ultrasound [George et al., 1993]. Regarding gonadal development and function, unilateral/bilateral cryptorchidism is frequently observed in affected boys. Of note, Marcus et al. [2008] documented Sertoli cell dysfunction in men with normal testicular descent, suggesting that cryptorchidism is not the sole contributing factor to impairment of testicular function in NS. Consistent with this observation, abnormal levels of follicle-stimulating hormone and inhibin B have been documented, suggesting different mechanisms of disturbance in male gonadal function [Marcus et al., 2008].
Prenatal diagnosis of NS may be suspected in the presence of ultrasonographic findings such as cystic hygroma, increased nuchal translucency and hydrops fetalis. Among fetuses with normal chromosomes, the diagnosis of NS will be made in approximately 1–3% of cases with nuchal edema in the first trimester [Reynders et al., 1997; Adekunle et al., 1999; Nisbet et al., 1999; Hiippala et al., 2001]. Since height and weight are usually normal in newborns with NS, parameters of fetal growth are not helpful in making the diagnosis. A recent retrospective review performed to assess the utility of PTPN11 testing based on prenatal sonographic findings indicated that heterozygous missense mutations of PTPN11 are relatively common in fetuses with cystic hygroma and normal karyotype (16%), including those in whom it was an isolated feature (11%) [Lee et al., 2009]. These data indicate that prenatal PTPN11 testing has diagnostic relevance and can aid in risk assessment and genetic counseling. As NS is genetically heterogeneous, negative PTPN11 testing cannot exclude the diagnosis, but further study is required to establish the roles of the other NS genes in prenatally detected features of the trait.
Disorders Clinically Related to Noonan Syndrome
LEOPARD Syndrome
LEOPARD syndrome (LS, OMIM 151100) is an autosomal dominant trait that overlaps phenotypically with NS. It is also allelic with NS, with a restricted spectrum of mutations in PTPN11 accounting for the majority of affected individuals [Digilio et al., 2002; Legius et al., 2002] (see below). The acronymic name refers to the major features: Lentigines, ECG conduction abnormalities, Ocular hypertelorism, Pulmonic stenosis, Abnormal genitalia, Retardation of growth, and sensorineural Deafness [Gorlin et al., 1971]. Similar to NS, there are age-dependent aspects of the phenotype. Facial dysmorphism is similar to that of NS but is usually milder [Digilio et al., 2006], and the neck is short but not webbed. Multiple lentigines present as dispersed flat, black-brown macules, mostly on the face, neck, and upper part of the trunk, but sparing the mucosae. In general, lentigines appear at the age of 4–5 years and increase until puberty into the thousands. Café-au-lait spots are also observed, alone or in association with lentigines, in up to 70–80% of the patients [Digilio et al., 2006], and usually precede the appearance of lentigines, being present from the first months of life. Growth retardation (height below the 3rd centile) is observed in 25% of affected individuals, and final height in 85% of subjects is below the 25th centile [Voron et al., 1976; Gorlin et al., 1990]. Approximately half of the affected individuals have heart defects, which are similar to those in NS but occur with different frequencies. ECG anomalies, progressive conduction defects and HCM are the most frequent features. Of note, HCM is detected in up to 80% of LS patients with heart defects, most commonly appearing during infancy. It is progressive and paralleled by the appearance of lentigines [Somerville and Bonham-Carter, 1972]. Diagnostic criteria for LS have been outlined by Voron and colleagues [1976]. A clinical diagnosis is not always feasible, particularly in young patients with no lentigines, due to the overlap with NS and neurofibromatosis-Noonan syndrome (see below). In these patients, the clinical differentiation from NS might be difficult during infancy and early childhood. The occurrence of distinctive association of signs, including HCM, sensorineural deafness, and café-au-lait spots represents an important diagnostic handle in these young patients [Digilio et al., 2006]. Sarkozy et al. [2009a] provide an updated review of the clinical and molecular genetics aspects of this disorder.
Cardiofaciocutaneous Syndrome
Cardiofaciocutaneous syndrome (CFCS, OMIM 115150) is a rare, sporadic multiple congenital anomalies/mental retardation syndrome characterized by failure to thrive, severe feeding problems, developmental delay, reduced growth, distinctive dysmorphic face, abnormalities of the skin, gastrointestinal tract and central nervous system, and cardiac defects [Reynolds et al., 1986; Roberts et al., 2006]. CFCS has a considerable clinical overlap with NS, and ‘borderline’ cases are commonly observed, which justified the long debated question of whether it was a separate nosologic entity or an extreme phenotype/variant of NS [Fryer et al., 1991; Neri et al., 1991; Wieczorek et al., 1997].
Recurrent facial/head features include relative/absolute macrocephaly, which is usually associated with high forehead, bitemporal narrowing and facial dysmorphism that appears more ‘coarse’ compared to NS. The cutaneous involvement includes dry and hyperkeratotic skin (face, arms and legs), ichthyosis, eczema, sparse, friable and curly hair, absent/sparse eyebrows and eyelashes, pigmentary changes (such as café-au-lait spots, naevi or lentigines) and hemangiomata. Heart defects occur in the majority of affected individuals and most commonly consist of pulmonic stenosis, HCM and septal defects [Roberts et al., 2006]. The cognitive deficits are usually moderate to severe. Hypotonia results in marked motor delay. Structural brain abnormalities include cerebral atrophy, frontal lobe, corpus callosum or cerebellar vermis hypoplasia, and hydrocephalus [Roberts et al., 2006]. Seizures are also frequently observed. As for Costello syndrome (see below), life expectancy is shortened on average due to the early death of affected individuals with severe cardiac involvement.
CFCS is genetically heterogeneous, with mutations in the KRAS, BRAF, MEK1 and MEK2 genes occurring in approximately 60–90% of affected individuals [Niihori et al., 2006; Rodriguez-Viciana et al., 2006b; Narumi et al., 2007; Nava et al., 2007; Schulz et al., 2008].
Costello Syndrome
Costello syndrome (CS, OMIM 218040) is the eponymous name for the disorder originally described in 1971, and further delineated by the same author in 1977, as a condition characterized by prenatal overgrowth followed by postnatal feeding difficulties and severe failure to thrive, distinctive ‘coarse’ facial features, mental retardation, short stature, cardiac defects (most commonly HCM, septal defects, valve thickening and/or dysplasia, and arrhythmias), and musculoskeletal and skin abnormalities [Costello, 1971, 1977; Zampino et al., 1993; Hennekam, 2003]. Children and young adults with CS are predisposed to malignancies [Gripp, 2005]. Solid tumors, including rhabdomyosarcoma and less frequently neuroblastoma and bladder carcinoma, have been estimated to occur in approximately 15% of affected individuals throughout childhood, while benign cutaneous papillomata in the perinasal or/and perianal region(s) represent a distinctive and common feature associated with the disorder.
CS is caused by germline missense mutations in the HRAS proto-oncogene (OMIM 190020) [Aoki et al., 2005]. Data from published surveys indicate that HRAS mutations account for 83–100% of subjects with a confirmed diagnosis of CS [Aoki et al., 2005; Estep et al., 2006; Gripp et al., 2006; Kerr et al., 2006; Zampino et al., 2007]. This finding has been explained as either locus heterogeneity or by the difficulties of diagnosis in cases exhibiting overlapping features with clinically related disorders or a phenotype that evolves with time. In our opinion, CS should be used only for those subjects who are heterozygous for an HRAS mutation. The absence of a mutation in the gene in a subject with a phenotype apparently fitting CS might be predictive of a clinically related but nosologically distinct condition. Clinical re-evaluation of these cases would help considerably to confirm or reject the diagnosis.
Neurofibromatosis-Noonan Syndrome
The so-called neurofibromatosis-Noonan syndrome (NFNS, OMIM 601321) is a peculiar clinical trait, first noted in 1985 by Allanson et al. [1985b], who described subjects with features of both neurofibromatosis type 1 (NF1, OMIM 162200) and NS. It has been long speculated whether NFNS is a variant of either NF1 or NS, a chance association, or a distinct disorder [Opitz and Weaver, 1985; Carey, 1998]. Recent reports have provided some insights but have not completely resolved the issues. NF1 mutation analysis performed in 3 independent cohorts of patients with features fitting NFNS documented occurrence of heterozygous NF1 mutations in 23 of 28 subjects [Baralle et al., 2003; De Luca et al., 2005; Hüffmeier et al., 2006]. Lesions included nonsense mutations, out-of-frame deletions, missense changes (mostly affecting the GAP domain), and small in-frame deletions. Those groups also searched for PTPN11 mutations in their subjects but failed to find any. In contrast, 2 cases of NFNS with NF1 and PTPN11 mutations have been reported [Bertola et al., 2005; Thiel et al., 2009]. Finally, NF1 mutations have co-segregated with the NFNS trait in a few kindreds large enough to make second mutations highly unlikely. Taken together, the current evidence indicates that most individuals with NFNS harbor an NF1 mutation and that a single mutation can be sufficient to engender the trait. Double heterozygosity for NF1 and PTPN11 mutations rarely cause NFNS, and it is not yet clear how frequently mutations in other NS disease genes co-occur with NF1 defects in the disorder. These findings support the view that NFNS is genetically distinct from NS and emphasize the extreme phenotypic variability associated with lesions in the NF1 gene. The identification of specific NF1 alleles recurring in NFNS, the evidence that these alleles cosegregate with the condition in families, and the observation of a peculiar mutational spectrum strongly suggest that the term ‘NFNS’ does characterize a phenotypic variant of NF1, which manifests with a lower incidence of plexiform neurofibromas, skeletal anomalies, and internal tumors, in association with hypertelorism, ptosis, low-set ears, and CHDs [Carey, 1998; Baralle et al., 2003; De Luca et al., 2005; Hüffmeier et al., 2006; Nyström et al., 2009]. It should be noted, however, that some of the mutations identified in patients with NFNS have also been reported in NF1 without any feature suggestive of NS.
Legius Syndrome
Legius syndrome (OMIM 611431), previously termed neurofibromatosis type 1-like syndrome, is an autosomal dominant condition characterized by multiple axillary freckling, café-au-lait spots, macrocephaly, and an NS-like facial dysmorphism in some individuals [Brems et al., 2007; Pasmant et al., 2009; Spurlock et al., 2009]. Some patients have learning difficulties and/or hyperactive behavior. Despite the clinical overlap with NF1, affected individuals do not have Lisch nodules, neurofibromas or central nervous system tumors, while lipomas represent a relatively common feature. Additional studies are required to establish susceptibility of affected individuals to cancer. Legius syndrome is caused by loss-of-function mutations of the SPRED1 gene, which encodes a negative modulator of RAS-MAPK signaling [Brems et al., 2007]. SPRED1 mutational analysis of sporadic or familial cases with a diagnosis of NF1 or with a phenotype suggestive of the disorder indicates that mutations account for approximately 0.5–1% of NF1 mutation-negative cases.
Molecular Pathogenesis
PTPN11
The PTPN11 gene (OMIM 176876) encodes SHP2, a widely expressed cytoplasmic Src homology 2 (SH2) domain-containing protein tyrosine phosphatase functioning as an intracellular signal transducer [Neel et al., 2003; Tartaglia et al., 2004b]. SHP2 is required during development and regulates cell migration, proliferation, survival and differentiation through multiple signaling pathways, including the RAS-MAPK cascade. It contains 2 tandemly arranged N-terminal SH2 domains (N-SH2 and C-SH2), a single catalytic domain (PTP) and a C-terminal tail containing 2 tyrosyl phosphorylation sites and a proline-rich stretch whose function is not well characterized (fig. 3A). The SH2 domains selectively bind to short amino acid motifs containing a phosphotyrosyl residue and promote SHP2's association with cell surface receptors, cell adhesion molecules and scaffolding adapters. Crystallographic data indicate that the N-SH2 domain functions as an intramolecular switch controlling SHP2's catalytic activation [Hof et al., 1998]. Specifically, it interacts intramolecularly with the PTP domain basally, blocking the access of the substrate to the catalytic site. Upon engagement of the N-SH2 phosphopeptide, a conformational change of the domain weakens the autoinhibiting interaction, activating the phosphatase. Although it has been demonstrated that SHP2 can either positively or negatively modulate signal flow depending upon its binding partner and interactions with downstream signaling networks, it is now established that SHP2 positively controls the activation of the RAS-MAPK cascade induced by a number of growth factors and cytokines [Neel et al., 2003; Dance et al., 2008; Xu and Qu, 2008]. In most cases, SHP2's function in intracellular signaling appears to be upstream of RAS.
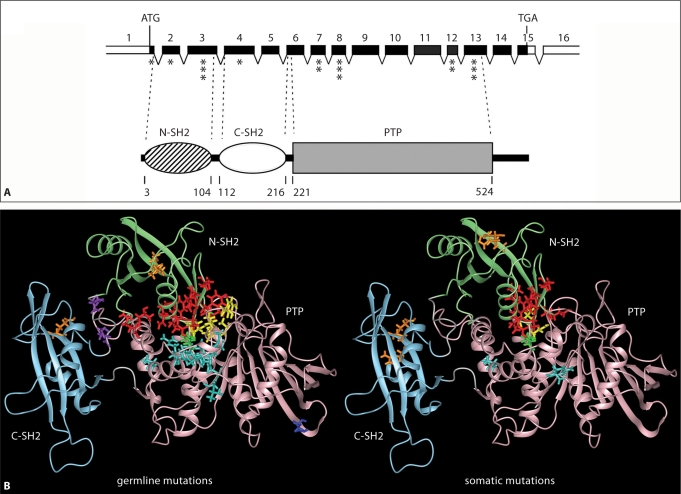
Fig. 3.
PTPN11 gene organization, SHP2 domain structure and location of affected residues in human disease. A The PTPN11 gene and its encoded protein. The numbered, filled boxes at the top indicate the coding exons; the positions of the ATG and TGA codons are shown. Exon location of disease-associated mutations is indicated (the number of asterisks is an index of the relative prevalence of mutations within each exon). SHP2's functional domains, consisting of 2 tandemly arranged SH2 domains at the N-terminus (N-SH2 and C-SH2) followed by a protein tyrosine phosphatase (PTP) domain, are shown below. The numbers below that cartoon indicate the amino acid boundaries of those domains. B Location of mutated residues in the 3-dimensional structure of SHP2 in its catalytically inactive conformation. Residues affected by germline (left) or somatically acquired (right) mutations are shown with their lateral chains colored according to the classification proposed by Tartaglia et al. [2006] (red, mutations affecting the N-SH2/PTP interaction; yellow, mutations affecting the N-SH2/PTP interaction and possibly catalysis; green, mutations affecting the N-SH2/PTP interaction and possibly substrate specificity; cyan, mutations affecting the N-SH2/PTP interaction and/or catalysis; orange, mutations promoting increased SH2 phosphopeptide-binding affinity or affecting specificity; violet, mutations affecting SH2 orientation or mobility; blue, unclassified).
PTPN11 was discovered as a major NS disease gene by using a positional candidacy approach in 2001 [Tartaglia et al., 2001]. Subsequent studies performed with large, clinically well-characterized cohorts have provided an estimate of the relevance of PTPN11 mutations in the epidemiology of NS, and explored genotype-phenotype correlations [Tartaglia et al., 2002; Zenker et al., 2004; Jongmans et al., 2005]. Based on those efforts, it has now been established that PTPN11 mutations account for approximately 50% of NS, and are more prevalent among subjects with pulmonary valve stenosis and short stature, and less common in individuals with HCM and/or severe cognitive deficits. Available records based on more than 500 germline defects indicate that NS-causing PTPN11 mutations are almost always missense changes and are not randomly distributed throughout the gene [Tartaglia et al., 2006]. Biochemical and functional characterization of disease-associated mutations support the view that they can perturb SHP2 function by distinct mechanisms [Keilhack et al., 2005; Tartaglia et al., 2006; Martinelli et al., 2008]. Most of the mutations affect residues involved in the N-SH2/PTP interdomain binding network that stabilizes SHP2 in its catalytically inactive conformation or are in close spatial proximity to them (fig. 3B). These mutations are predicted to up-regulate SHP2's physiological activation by impairing the switch between the active and inactive conformation, favoring a shift in the equilibrium toward the former, without consequences on SHP2's catalytic capability. A number of mutations, however, affect residues contributing to the stability of the catalytically inactive conformation but also participating in catalysis or controlling substrate specificity. For some of these defects, the individual substitution does not markedly perturb substrate affinity and/or catalysis, but rather protein activation by N-SH2 dissociation prevails. A few mutations affect residues located outside of the interacting regions of the N-SH2 and PTP domains (fig. 3B). A few changes involve residues located in the linker stretch connecting the N-SH2 and C-SH2 domains and are likely to alter the flexibility of the N-SH2 domain, inhibiting the N-SH2/PTP interaction. Two recurrent mutations affect residues Thr42 (N-SH2) and Glu139 (C-SH2) that are part of the phosphopeptide-binding pocket of each SH2 domain. Experimental evidence supports the idea that these amino acid substitutions promote SHP2 gain-of-function by either increasing the binding affinity or altering the binding specificity of the protein for the phosphorylated signaling partners.
A distinct class of PTPN11 mutations has been identified to underlie LEOPARD syndrome (LS; OMIM 151100) [Digilio et al., 2002; Legius et al., 2002]. Analysis of several unrelated individuals with a phenotype fitting or suggestive of LS has confirmed the presence of a heterozygous PTPN11 mutation in the vast majority of cases. Tyr279Cys and Thr468Met represent the most common defects, even though additional mutations have been documented [Sarkozy et al., 2009b]. While an impaired catalytic activity has been established as biochemical behavior shared by these SHP2 mutants [Hanna et al., 2006; Kontaridis et al., 2006; Tartaglia et al., 2006], they do not appear to perturb intracellular signaling by a merely dominant negative effect [Hanna et al., 2006; Martinelli et al., 2008; Oishi et al., 2009], as supposed in the past [Kontaridis et al., 2006].
PTPN11 mutation-positive NS/LS are rarely accompanied by multiple giant cell lesions of the jaw and/or other bone/soft tissues [Tartaglia et al., 2002; Sarkozy et al., 2004; Jafarov et al., 2005; Lee et al., 2005; Beneteau et al., 2009]. This association, which was originally introduced as a distinct nosologic entity and denominated Noonan-like/multiple giant cell lesion syndrome (NL/MGCLS, OMIM 163955) [Cohen and Gorlin, 1991], is now considered as part of the NS/LS/CFCS phenotypic spectrum. NL/MGCLS-associated PTPN11 mutations have been observed in individuals with NS, LS or CFCS, including families segregating the trait without any bony involvement. Consistent with this view, this trait is genetically heterogeneous with documented germline mutations affecting other NS/CFCS disease genes coding for transducers participating in the RAS-MAPK signaling pathway (see below) [Beneteau et al., 2009; Hanna et al., 2009; Neumann et al., 2009].
Children with NS are predisposed to a spectrum of hematologic abnormalities and malignancies, including juvenile myelomonocytic leukemia (JMML), a clonal myeloproliferative disorder of childhood characterized by a hypersensitive pattern of myeloid progenitor colony growth in response to GM-CSF, which is due to a selective inability to down-regulate RAS function [Niemeyer and Kratz, 2008]. PTPN11 mutation screening on a relatively large number of children with NS and JMML has demonstrated the presence of germline mutations in the majority of cases, with one mutation rarely observed in NS, c.218C>T (Thr73Ile), occurring in a large percentage of children [Tartaglia et al., 2003; Loh et al., 2004b; Kratz et al., 2005]. The association between this specific amino acid change and JMML in NS and the key-role of SHP2 in RAS signaling and hematopoiesis suggested that a distinct class of lesions in the gene, possibly acquired as a somatic event, might play a role in leukemogenesis. Indeed, somatic missense PTPN11 mutations have been demonstrated to occur in approximately one-third of isolated JMML as well as in variable proportions of other myeloid and lymphoid malignancies of childhood [Tartaglia et al., 2003, 2004a, 2005; Loh et al., 2004a, b; Kratz et al., 2005]. The prevalence of PTPN11 mutations among adult patients with myeloid or lymphoid disorders appears to be considerably lower than observed among pediatric cases [Hugues et al., 2005; Loh et al., 2005; Tartaglia et al., 2006], even though SHP2 overexpression has been documented in adult human leukemia [Xu et al., 2005]. Similarly, PTPN11 is only rarely mutated in non-hematologic cancers [Bentires-Alj et al., 2004; Chen et al., 2006; Martinelli et al., 2006, 2009]. As observed in NS, the vast majority of PTPN11 lesions identified in this heterogeneous group of hematologic malignancies are missense changes that alter residues located at the interface between the N-SH2 and PTP domains (fig. 3B). Remarkably, comparison of the molecular spectra observed with NS and leukemias indicates a clear-cut genotype-phenotype correlation, strongly supporting the idea that the germline-transmitted PTPN11 mutations have different effects on development and hematopoiesis than those acquired somatically. Consistent with this, the biochemical behavior of SHP2 mutants associated with malignancies tends to be more activating than observed with the NS-associated mutant proteins [Keilhack et al., 2005; Tartaglia et al., 2006]. Moreover, the leukemia-associated PTPN11 mutations up-regulate RAS signaling and induce cell hypersensitivity to growth factors and cytokines more than the NS defects do [Loh et al., 2004b; Chan et al., 2005; Schubbert et al., 2005]. Overall, the available genetic, modeling, biochemical and functional data support a model in which distinct gain-of-function thresholds for SHP2 activity are required to induce cell-, tissue- or developmental-specific phenotypes, each depending on the transduction network context involved in the phenotype. According to this model, SHP2 mutants associated with NS have relatively milder gain-of-function effects, which are sufficient to perturb development processes but inadequate to deregulate hematopoietic precursor cell proliferation. The PTPN11 mutations observed in isolated JMML and other hematologic malignancies produce mutant SHP2 proteins with higher gains in function. Since these molecular lesions are observed almost exclusively as somatic defects, it is likely that they affect embryonic development and/or fetal survival. The PTPN11 mutations observed in NS with JMML produce SHP2 with intermediate activity, which would explain the relatively benign clinical course of the leukemia compared to that observed in isolated JMML.
It should be mentioned that de novo duplications of the chromosomal region encompassing PTPN11 (12q24) have been documented in 2 subjects with clinical features suggestive of NS without mutations in any known NS genes [Shchelochkov et al., 2008; Graham et al., 2009]. While these consistent observations suggest that increased dosage of SHP2 may have dysregulating effects on intracellular signaling and consequences on developmental processes, the screening of a relatively large cohort of NS cases negative for mutations in previously identified genes indicate that PTPN11 gene duplication represents an uncommon cause of NS.
SOS1
Cell surface tyrosine kinase receptors activate RAS proteins by recruiting guanine nucleotide exchange factors (GEFs) to the cytoplasmic side of the plasma membrane. These proteins catalyze the release of guanosine diphosphate (GDP) from RAS, facilitating the conversion of the inactive GDP-bound form to active guanosine triphosphate (GTP)-bound RAS [Quilliam et al., 1995]. Among the GEFs, 2 members of the son of sevenless (SOS) family, SOS1 and SOS2, promote guanine nucleotide exchange on RAS proteins, but not on RAS-related family members, such as the RAP and RHO proteins [Nimnual and Bar-Sagi, 2002; Quilliam et al., 2002]. SOS proteins are constitutively bound to the Src homology 3 (SH3) domain of growth factor receptor-bound protein 2 (GRB2), and following growth factor stimulation, the GRB2-SOS complex binds directly to specific tyrosyl-phosphorylated motifs of the activated receptor or to an adaptor protein through the SH2 domain of GRB2 [Nimnual and Bar-Sagi, 2002].
Based on their modulatory role in RAS signaling, 2 groups considered SOS1 and SOS2 as excellent candidate genes, and independently discovered that SOS1 is mutated in a relatively large percentage of subjects with NS [Roberts et al., 2007; Tartaglia et al., 2007]. The SOS1 gene (OMIM 182530) encodes a large multidomain protein (fig. 4A) [Chardin et al., 1993]. The N-terminal portion of the protein contains a histone domain (HD) that is characterized by 2 tandemly arranged histone folds, and is followed by a Dbl homology (DH) domain and a pleckstrin homology (PH) domain, which are implicated in the activation of RAC, a small GTPase of the RHO/CDC42 family [Nimnual et al., 1998]. The C-terminal half of the protein contains the RAS exchanger motif (Rem) domain and the Cdc25 domain, which are required for the RAS-specific nucleotide exchange activity of SOS1. Finally, the region at the C-terminus contains recognition sites for SH3 domains and mediates interaction of SOS1 with SH3 domain-containing adaptor proteins that deliver SOS1 to the membrane upon receptor activation. Additional anchorage sites on the membrane are provided by the phosphatidylinositol phosphate-binding site within the PH domain [Chen et al., 1997] and an extended positively charged surface of the HD domain [Sondermann et al., 2005]. Sos1is widely expressed, and as opposed to Sos2, which is dispensable for mouse development, loss of Sos1 function results in a range of embryonic defects, including cardiovascular abnormalities, causing mid-gestational lethality [Wang et al., 1997].
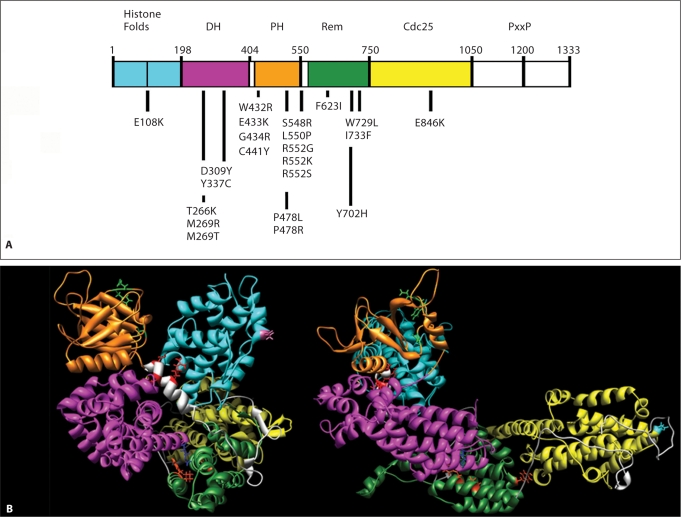
Fig. 4.
SOS1 domain structure and location of affected residues in NS. A SOS1 missense mutations are positioned below the cartoon of the SOS1 protein with its functional domains indicated above. Abbreviations: DH, Dbl homology domain; PH, plekstrin homology domain; Rem, RAS exchanger motif; PxxP, proline-rich motif. B Location of the mutated residues on the 3-dimensional structure of SOS1. The functional domains are color-coded as follows: cyan, histone folds; magenta, DH; orange, PH; green, Rem; yellow, Cdc25. Residues affected by mutations are indicated with their lateral chains (violet, histone folds; blue, DH; green, PH; red, helical linker; orange, Rem; cyan, Cdc25). Based on Sondermann et al. [2005], who utilized structural data and computational modeling.
The available data indicate that SOS1 is the second most frequently mutated NS disease gene, accounting for approximately 20% of subjects without a defect in PTPN11 or KRAS [Roberts et al., 2007; Tartaglia et al., 2007; Zenker et al., 2007a]. The vast majority of the mutations identified are missense and affect multiple domains, clustering in specific regions of the protein (fig. 4). Approximately half of SOS1 defects affect residues located in the short helical linker connecting the PH and REM domains, with substitutions of residue Arg552 accounting for approximately 30% of total mutations. A second mutation cluster is located within the PH domain (residues 432 to 434), while a third functional cluster resides at the interacting regions of the DH (Thr266 and Met269) and Rem (Trp729 and Ile733) domains. A single amino acid change (Glu846Lys) within the Cdc25 domain accounts for more than 10% of defects.
Subjects heterozygous for a mutated SOS1 allele tend to exhibit a distinctive phenotype which is characterized by ectodermal abnormalities (keratosis pilaris/hyperkeratotic skin, sparse eyebrows), generally associated with absence of cognitive deficits [Tartaglia et al., 2007; Zenker et al., 2007a]. In these patients, height is less frequently below the 3rd centile compared with the general population of individuals with NS. Based on the high prevalence of ectodermal involvement in SOS1 mutation-positive NS subjects, mutational screening has been performed on a clinically well-characterized CFCS cohort that revealed that SOS1 is not a major disease gene for this disorder [Zenker et al., 2007a]. A few individuals with ectodermal manifestations and distinctive facial dysmorphism which might be suggestive of CFCS, however, have been reported [Narumi et al., 2008; Nyström et al., 2008]. In these subjects, cognitive deficits are generally absent or minor, but at least 1 case with mental retardation was reported [Narumi et al., 2008]. Recently, SOS1 mutations have been identified in 9 individuals with NS associated with MGCL of jaws or joints (pigmented villonodular synovitis) [Mascheroni et al., 2008; Beneteau et al., 2009; Hanna et al., 2009; Neumann et al., 2009]. All of the mutations had previously been documented in subjects with NS without MGCL, confirming the view that MGCL represent a feature of NS, and that the use of NL/MGCLS should be avoided.
The GEF activity of SOS1 is controlled by 2 regulatory determinants: the RAS catalytic site and an allosteric site that stimulates exchange activity through the binding of nucleotide-bound RAS [Margarit et al., 2003]. Whereas the former is located entirely within the Cdc25 domain, the allosteric site is bracketed by the Cdc25 and Rem domains. The mechanism of activation of the protein is complex: basally, the interaction between the DH and Rem domain stabilizes SOS1 in its catalytically inactive conformation by masking the allosteric binding site for RAS. Following SOS1 translocation to the membrane, the inhibitory effect of the DH domain is relieved by still undefined events allowing RAS binding to the allosteric site, which in turn promotes a conformational change of the Rem and Cdc25 domains, and RAS binding to the catalytic site [Sondermann et al., 2004]. Remarkably, most NS-causing SOS1 mutations reside in regions within the molecule that are predicted to contribute structurally to the maintenance of the catalytically autoinhibited conformation (fig. 4B). Biochemical data confirmed such predictions and demonstrated that NS-causing SOS1 mutations promote gain of function. Roberts et al. [2007] demonstrated that transient expression of 4 mutants (Met269Arg, Asp309Tyr, Arg552Gly and Glu846Lys) in 293T cells induced sustained ligand-dependent ERK activation as well as enhanced and prolonged RAS activation. Consistent with those findings, Tartaglia et al. [2007] observed a prolonged EGF-stimulated RAS activation in Cos-1 cells transiently expressing the Arg552Gly mutant and an essentially constitutive RAS activation in cells expressing the Trp728Leu SOS1 protein. Since many of the SOS1 mutations alter residues related to SOS autoinhibition, either through interaction of the histone folds with the PH-Rem linker or interaction of the DH domain at the allosteric RAS binding site, the predominant pathogenetic mechanism appears to be increased availability of the allosteric RAS binding site enhancing GEF activity and, as a consequence, increased RAS-GTP levels. It should be noted that the DH-PH module of SOS has also been implicated in the activation of the Rho GTPase RAC [Nimnual et al., 1998]. The extent to which SOS1 gain-of-function mutations affect different RAS-dependent or RAC-dependent signals remains to be determined.
Based on the activating role of NS-causing SOS1 mutations, a possible contribution of gain-of-function mutations in this gene in cancer was evaluated [Kratz et al., 2007; Swanson et al., 2008; our unpublished data]. Mutational analyses performed on genomic DNA from more than 1,000 solid tumors (pancreatic, lung, breast, colon, thyroid cancers) and hematological malignancies (myeloproliferative disorders and acute myeloid and lymphoblastic leukemias) indicate that SOS1 mutations do not contribute significantly to oncogenesis in most cancers, suggesting that NS patients heterozygous for a SOS1 mutation are not at increased risk of developing cancer.
KRAS
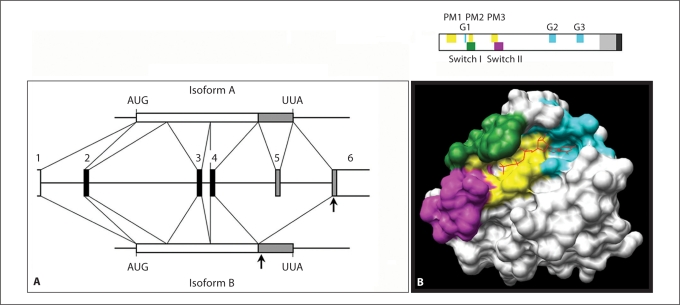
The KRAS gene (OMIM 190070) produces 2 transcripts through alternative splicing, resulting in 2 proteins called KRASA and KRASB (fig. 5A) [Friday and Adjei, 2005]. For the KRASA transcript, exon 5 contains the stop codon and a portion of the 3′ untranslated region (3′UTR), of which the remainder resides in exon 6. For the KRASB transcript, exon 5 is skipped, so exon 6 comprises a portion of the coding region, the stop codon and the entire 3′UTR. As with the other members of the RAS family, KRAS isoforms use GDP/GTP-regulated molecular switching to control intracellular signal flow [Mitin et al., 2005; Wennerberg et al., 2005]. They exhibit high affinity for both GDP and GTP, low GTPase activity, and cycle from a GDP-bound inactive state to a GTP-bound active state, the latter allowing signal flow by protein interaction with multiple downstream transducers (fig. 1). GDP/GTP cycling is controlled by GAPs, which accelerate the intrinsic GTPase activity, and GEFs, as SOS1, which promote release of GDP. RAS proteins share a structure that includes a conserved domain (residues 1 to 165), known as the G domain, which is required for its signaling function, and a less conserved C-terminal tail, called the hypervariable region, that guides post-translational processing and plasma membrane anchoring (fig. 5B). Within this region, conserved sequence elements direct the GTP/GDP binding and exchange, and GTP hydrolysis. Furthermore, 2 tracts, denoted as Switch I and Switch II, undergo major conformational changes upon GTP/GDP exchange and mediate binding to effectors, GAPs and GEFs [Barbacid, 1987; Mitin et al., 2005].
Fig. 5.
KRAS gene organization, protein domain structure and location of affected residues specifically affecting the KRASB isoform. A KRAS gene organization and transcript processing to produce the alternative KRAS isoforms A and B. The numbered black and grey boxes indicate the invariant coding exons and exons undergoing alternative splicing, respectively. KRASB mRNA results from exon 5 skipping. In KRASA mRNA, exon 6 encodes the 3′-UTR. The arrows indicate location of mutations affecting codons 152, 153 and 156. B Schematic diagram (above) and tridimensional representation (below) of the structural and functional domains defined within RAS proteins. The motifs required for signaling function (PM1 to PM3 indicate residues involved in binding to the phosphate groups, while G1 to G3 are those involved in binding to the guanine base) are indicated. The hypervariable region is shown in grey, together with the C-terminal motifs that direct post-translational processing and plasma membrane anchoring (dark grey). The GTP/GDP binding pocket is shown in cyan (guanine ring-binding surface) and yellow (triphosphate group binding surface) together with the Switch I (green) and Switch II (magenta) domains, according to the GTP-bound RAS conformation.
Based on the link between the functions of SHP2 and RAS, 2 groups independently used a candidate gene approach to discover that KRAS mutations can cause NS [Carta et al., 2006; Schubbert et al., 2006]. Four missense heterozygous mutations in the KRAS gene were identified in 7 individuals among 212 PTPN11 mutation-negative subjects with NS. A generally more severe NS phenotype appeared to be associated with KRAS mutations, which included JMML and craniosynostosis in 1 subject and a phenotype at the interface with CFCS/CS in 2 individuals. Consistent with this, KRAS mutations were also identified in a small percentage of individuals diagnosed as having CFCS [Niihori et al., 2006; Schubbert et al., 2006]. The diversity of mutations associated with these developmental disorders as well as their phenotypic spectrum have been investigated further, refining the picture of a clustered distribution of germline disease-associated KRAS defects, and confirming the high clinical variability [Nava et al., 2007; Zenker et al., 2007b; Kratz et al., 2009]. On the whole, available data indicate that NS-causing KRAS mutations are missense, do not generally occur as somatically acquired changes contributing to oncogenesis, and account for less than 3% of affected individuals with NS. Most mutations cluster in the first and second coding exons of the gene, which are shared by the 2 KRAS isoforms. Mutations affecting exon 6, however, have been documented in one-third of NS or CFCS subjects with a KRAS germline mutation. This exon codes for residues at the C-terminus of KRASB but not KRASA (fig. 5A). Of note, the C-termini of RAS proteins are subjected to post-translational modifications, which have important implications for their functions [Silvius, 2002]. Similar to the other RAS family members, KRASA is palmitoylated at cysteine residues upstream of the conserved CAAX motif, which is replaced with a polylysine stretch in KRASB. This differential processing of the 2 KRAS isoforms leads to alternative trafficking pathways to the plasma membrane and distinct membrane localization [Friday and Adjei, 2005]. Moreover, recent evidence demonstrates that the 2 KRAS isoforms play distinct roles in development. While the B isoform is ubiquitously expressed in embryonic and adult tissues in mice, KrasA expression is restricted temporally and spatially and is not expressed in the adult heart [Plowman et al., 2003]. Consistent with these data, loss of both the Kras isoforms is embryonic lethal in mice [Johnson et al., 1997; Koera et al., 1997], while absence of only KrasA does not perturb development [Plowman et al., 2003]. Although KRAS mutations affecting domains shared by the 2 isoforms can cause NS and CFCS, the identification of exon 6 mutations documented that isolated KRASB gain-of-function is sufficient for disease pathogenesis, further evidence that isoform B plays the major role in development.
As observed for the somatically acquired oncogenic NRAS, KRAS and HRAS mutations, the NS-causing KRAS defects were found to up-regulate protein function by impairing the switch between the active and inactive conformation [Schubbert et al., 2006, 2007a]. Of note, functional KRAS upregulation can be promoted by multiple mechanisms. In particular, biochemical characterization of the Val14Ile and Thr58Ile KRAS mutants documented an impaired intrinsic and GAP-stimulated GTPase activity compared to the wild-type protein, which was, however, higher than that of the oncogenic Gly12Asp mutant that has negligible GTPase activity. Interestingly, the Val14Ile and Thr58Ile KRAS proteins were partially responsive to neurofibromin and p120 GAP, although to different extents [Schubbert et al., 2006]. In contrast, Pro34Arg and Asp153Val KRAS mutants were found to exhibit normal intrinsic rates of GTP hydrolysis, while a fifth mutant, Phe156Leu, had impaired GTPase activity that was similar to that observed for the cancer-associated Gly12Asp KRAS mutant. While Pro34Arg KRAS was insensitive to neurofibromin or p120 GAP stimulation, the Phe156Leu mutant had an intermediate level of responsiveness and the Asp153Val KRAS protein exhibited a response to GAPs that was comparable to that observed for the wild-type protein. These mutants also differed in their capability to bind guanine nucleotides with the Asp153Val protein exhibiting a normal GTP/GDP dissociation rate while Phe156Leu KRAS showed a dramatically increased rate of guanine nucleotide dissociation. Although these studies documented a complex pattern of intrinsic biochemical properties, expression of these mutants in COS-7 cells promoted higher levels of phosphorylated MEK and ERK proteins, indicating hyperactivation of the MAPK cascade. Consistent with these findings, expression of these mutants in murine fetal liver cells conferred variable hyper-responsive behavior to GM-CSF. It should be noted that proliferation in these cells remained dependent on growth factor stimulation, different from what was observed for cells expressing the cancer-associated Gly12Asp mutant.
A small number of germline missense mutations in HRAS underlie CS, which is clinically related to NS [Aoki et al., 2005]. The vast majority of defects affect residues Gly12 and Gly13, which also represent the hot spots of oncogenic somatic mutations [Adjei, 2001]. As documented for NS/CFCS-causing KRAS mutations, defects affecting those residues render the protein insensitive to GAP-promoted GTP hydrolysis, resulting in a constitutively GTP-bound, active state [Colby et al., 1986; Bos, 1989; Adjei, 2001], while other less common amino acid substitutions involving residues placed in the purine ring binding pocket of the protein (His117 and Ala146) [Kerr et al., 2006; Zampino et al., 2007] are predicted to affect the stability of HRAS binding to GDP/GTP, favoring a shift in the equilibrium towards the GTP-bound, active form of RAS, bypassing the requirement for a GEF [Clanton et al., 1986; Der et al., 1986; Feig et al., 1986; Walter et al., 1986; Denayer et al., 2008].
Available data indicate that the Gly12Ser amino acid substitution is the most recurrent mutation in CS, accounting for approximately 85% of affected individuals with mutated HRAS. This change recurs with considerably lower prevalence in human cancers (approx. 5% of total HRAS amino acid substitutions) (COSMIC; http://www.sanger.ac.uk/genetics/CGP/cosmic/). Experimental data indicate that Gly12Ser has a lower transformation potential than the Gly12Val mutant [Seeburg et al., 1984], which is the most common somatic HRAS defect in human tumors (about 45% of total somatic HRAS mutations). The latter has been documented in 2 individuals with CS who exhibited a relatively severe phenotype (approx. 2% of cases with an HRAS mutation) [Aoki et al., 2005; van der Burgt et al., 2007]. Consistent with this, no mutation affecting residue Gln61, which constitute approx. 33% of total HRAS lesions in human cancer, has been documented in individuals with CS to date. Such a striking difference in prevalence and spectrum of HRAS amino acid substitutions suggests that CS-causative mutations have less potency for deregulating protein function than cancer-contributing ones and that the latter might exert a stronger perturbing effect on development when inherited.
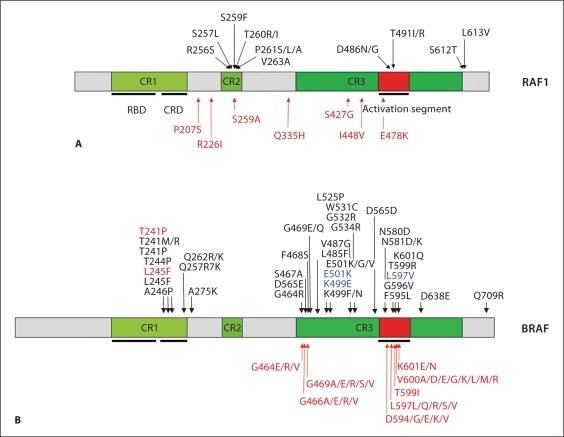
RAF1 and BRAF
The RAF1, BRAF and ARAF proteins are members of a small family of serine-threonine kinases that function as RAS effectors [Wellbrock et al., 2004; Schreck and Rapp, 2006; Leicht et al., 2007]. These kinases phosphorylate and activate the dual specificity kinases MEK1 and MEK2, which in turn promote the activation of the MAPKs, ERK1 and ERK2. The 3 members of the RAF family are likely to play different roles in the activation of the RAS-MAPK signaling cascade. Indeed, BRAF has a considerably higher MEK kinase activity compared to RAF1 and ARAF, and these proteins also differ in their expression profiles as well as in the regulatory mechanisms controlling their function. Furthermore, based on the murine knock-out models, they appear to have unique roles during development [Pritchard et al., 1996; Wojnowski et al., 1997; Mikula et al., 2001].
The RAF1 gene (OMIM 164760) encodes a protein with 3 functional domains, known as conserved regions 1 to 3 (CR1–3) (fig. 6A). The N-terminal CR1 contains the region involved in GTP-RAS binding and a cysteine-rich sequence that mediates RAF1's interaction with the cytosolic surface of the cell membrane. CR2 contains a negative regulatory domain controlling protein translocation to the membrane and its catalytic activation, while the C-terminal CR3 comprises the kinase domain of the protein [Wellbrock et al., 2004]. Differently from BRAF, for which mutations recur in colon, ovary and thyroid cancers and melanoma, RAF1 missense changes are observed rarely in malignancies [Emuss et al., 2005; COSMIC database, http://www.sanger.ac.uk/genetics/CGP/cosmic/].
Fig. 6.
RAF1 and BRAF domain structures and location of affected residues in human disease. The domains of the RAF1 (A) and BRAF (B) proteins are indicated (CR, conserved region; RBD, RAS-binding domain; CRD, cysteine-rich domain). Germline (RAF1: NS and LS; BRAF: NS, LS and CFCS) and somatic (associated with cancer) mutations are reported above and below each cartoon, respectively. Only somatic BRAF mutations with prevalence ≥1.5%, according the COSMIC database (http://www.sanger.ac.uk/genetics/CGP/cosmic/) are reported. The BRAF T599I substitution, which rarely occurs in cancer and is homologous to the NS-causing RAF1 T491I change, is also reported. BRAF missense changes associated with a phenotype fitting NS or LS are colored blue and orange, respectively.
Two studies identified missense mutations in RAF1 in subjects with NS who were negative for a mutation in PTPN11, KRAS and SOS1 [Pandit et al., 2007; Razzaque et al., 2007], with a frequency of mutations ranging between 10 and 30%. Mutations in the same gene were also identified in 2 of 6 subjects with LS without a mutation in PTPN11 [Pandit et al., 2007]. RAF1 mutations affect residues clustering in 3 regions of the protein (fig. 6A). The first cluster involves the N-terminal consensus 14-3-3 recognition sequence (Arg256-Ser257-Thr258-pSer259-Thr260-Pro261) or adjacent residues within the CR2 region. Of note, Arg256, Ser257, Ser259 and Pro261, which are the invariant residues within this motif, were all found to be mutated. Mutations resulting in amino acid substitutions within this region account for approximately 70% of total RAF1 defects. The second group includes mutations affecting residues within the activation segment region of the kinase domain (Asp486 and Thr491), and constitute approximately 15% of NS- or LS-causing RAF1 amino acid changes. Of note, several BRAF missense mutations detected in solid tumors alter the activation segment, including some (Asp594Gly and Thr599Ile) homologous to those of RAF1 identified in subjects with NS. Finally, the third cluster (15% of RAF1 mutations) affects 2 adjacent residues (Ser612 and Leu613) located at the C-terminus in proximity of Ser621, a residue that undergoes phosphorylation and is important for the regulation of RAF1's catalytic activation. Nearly none of the RAF1 residues mutated in NS and LS is altered in cancer.
The catalytic activation of RAF1 is complex. In its inactive conformation, the N-terminal portion of the protein is thought to interact with and inactivate the kinase domain at the C-terminus. This autoinhibited conformation is stabilized by 14-3-3 protein dimers that bind to phosphorylated Ser259 and Ser621 [Wellbrock et al., 2004; Schreck and Rapp, 2006; Leicht et al., 2007]. Dephosphorylation of Ser259, which is possibly mediated by protein phosphatase 1C (PP1C) or protein phosphatase 2A (PP2A), is required for stable interaction with GTP-RAS, allowing protein translocation to the plasma membrane and further interaction with other still uncharacterized proteins. Among them are serine/threonine kinases that phosphorylate regulatory residues that, in their unphosphorylated state, contribute to stabilizing the catalytically inactive conformation of the protein. Functional characterization of a selected panel of RAF1 mutants supports the idea that mutations can differentially perturb protein function and intracellular signaling. In particular, Ser257Leu, Pro261Ser, Pro261Ala, Val263Ala and Leu613Val amino acid changes, which affect the 14-3-3 binding motif or the C-terminus of the protein, promote enhanced kinase activity and increased activation of the MAPK cascade compared to wild-type protein [Pandit et al., 2007; Razzaque et al., 2007]. In contrast, Asp486Asn and Thr491Ile, representing the mutation cluster in the activation segment, were observed to be kinase impaired. Of note, while the expression of the Asp486Asn mutant was found to cause a reduced activation of the pathway, expression of Thr491Ile did not, suggesting that (1) a different mechanism not requiring RAF1 catalytic activation promotes upregulation of the MAPK cascade, and (2) additional pathway(s) might be involved in signaling dysregulation driven by RAF1 mutations. Pandit et al. [2007] provided evidence supporting the model that the increased activation promoted by the amino acid substitutions affecting the N-terminal 14-3-3 binding site results from a loss of 14-3-3-mediated inactivation, while the mechanism through which mutations at the C-terminus activate RAF1's kinase activity remains to be explained.
Phenotype analysis of the NS and LS subjects with RAF1 mutations is notable for the observation that a large percentage of cases (75%) exhibit HCM, which is significantly different from the HCM prevalence of 18% in the general NS population. Moreover, this genotype-phenotype correlation seems to be allele-specific as HCM appears to be associated with mutations affecting the N-terminal 14-3-3 consensus site or the C-terminus. In addition to the 2 cases with LS, multiple nevi, lentigines and/or café-au-lait spots were detectable in one-third of NS patients with RAF1 mutations, suggesting a predisposition to hyperpigmented cutaneous lesions.
Recent studies reported that missense mutations in BRAF, which are known to account for a large fraction (50–75%) of CFCS [Niihori et al., 2006; Rodriguez-Viciana et al., 2006b], occur in a small percentage (less than 2%) of subjects with phenotype fitting or suggestive of NS or LS (fig. 6B) [Razzaque et al., 2007; Nyström et al., 2008; Sarkozy et al., 2009a]. Of note, NS-associated mutations largely do not overlap with those occurring in CFCS, suggesting a genotype-phenotype correlation. The detection of the recurrence of the Trp531Cys amino acid substitution as well as the clustering of mutations at Thr241, further supports the idea that the phenotype resulting from germline BRAF defects might be allele-specific. Available clinical data indicate that these subjects share neonatal growth failure and feeding difficulties, mild-to-moderate cognitive deficits, and hypotonia, and have a higher prevalence of multiple nevi and dark-colored lentigines [Sarkozy et al., 2009a]. As adults, they display the full-blown phenotype of NS, which however appears more severe compared to that associated with PTPN11 and SOS1 mutations. In these individuals, however, polyhydramnios, HCM, and CFCS-related skin features [Roberts et al., 2006; Armour and Allanson, 2008] are uncommon or absent, and cardiac defects, neurological impairment and feeding problems appear to be less severe compared to what is generally observed in CFCS [Sarkozy et al., 2009a]. Similarly, the individual with LS who was heterozygous for the Thr241Pro change displayed a phenotype overlapping that of PTPN11 or RAF1 mutation-positive LS cases, although cognitive difficulties were more severe and the cardiac involvement milder [Sarkozy et al., 2009a]. While the occurrence of distinct BRAF gene mutations in subjects with a phenotype fitting NS would indicate that some features might be allele-specific, the observation that a subgroup of BRAF mutation-positive subjects exhibit an ‘intermediate’ phenotype [Sarkozy et al., 2009a] suggests that a clinical continuum characterized by a differential combination and severity of features is associated with defects in the BRAF gene. These findings emphasize the difficulty in identifying efficient clinical criteria to define CFCS, LS or NS nosologically, and make evident the usefulness of a molecular-based definition of these clinically overlapping conditions that might direct clinicians toward a more appropriate management of patients. These findings also indicate that molecular screening of this gene would be worthwhile in individuals with clinical features fitting NS or LS with moderate to severe cognitive deficits. More recently, Koudova et al. [2009] reported on a patient with LS and normal intelligence who was found to carry a novel sequence change in BRAF, which further illustrates that the phenotypic spectrum caused by BRAF mutations is broader than previously assumed and that mental retardation does not necessarily represent an associated feature.
To date, more than 40 germline BRAF mutations have been identified (fig. 6B). All are missense defects that are not randomly distributed, clustering in the cysteine-rich domain and in the amino-terminal portion and activation segment of the kinase domain. Most mutations are recurrent, with substitutions of residues Gln257 and Glu501 accounting for approximately 40% of all defects. Different from the other 2 members of the family, RAF1 and ARAF, which are only occasionally mutated in human cancers, somatic BRAF mutations frequently occur in malignant melanomas and in thyroid, colorectal and ovarian cancers. Consistent with the observation that cancers are uncommon among subjects carrying a BRAF mutation, however, germline BRAF mutations are rarely observed as somatic mutations contributing to oncogenesis. NIH-3T3 cell colony focus formation assay data indicate that CFCS-associated BRAF mutants have a reduced transforming capability compared with the recurrent oncogenic Val600Glu BRAF protein, and that the NS- and LS-associated BRAF mutants do not confer enhanced transformation to cells [Sarkozy et al., 2009a]. While these results support the view that the mutations transmitted through the germline have less potency in deregulating BRAF's function, they also suggest that NS- and LS-associated mutations are less activating compared to those associated with CFCS, which parallels the observations indicating that phenotypes arising from germline BRAF defects might be allele specific. Of note, in vitro functional studies indicate that both germline and somatic amino acid changes can confer either increased or decreased activity upon the mutant protein as compared to the wild-type protein [Rodriguez-Viciana et al., 2006b; Dhomen and Marais, 2007; Sarkozy et al., 2009a], suggesting that multiple alternative mechanisms are likely to be involved in the functional dysregulation of the kinase.
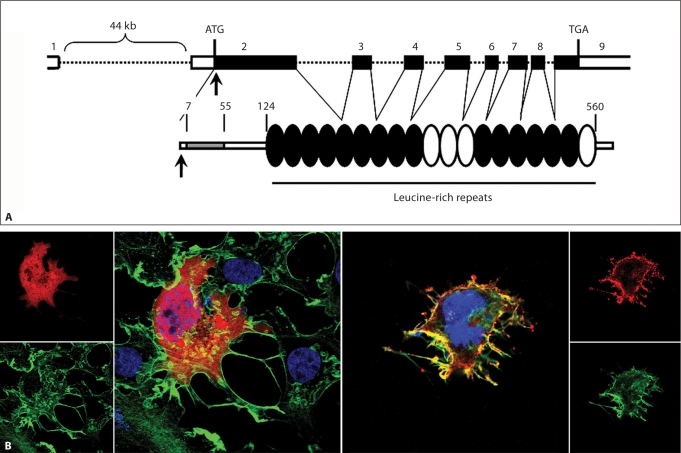
SHOC2
N-myristoylation is an irreversible form of protein fatty acylation occurring co-translationally, e.g. during protein synthesis, in which myristate, a 14-carbon saturated fatty acid, is covalently added to an N-terminal glycine residue after excision of the initiator methionine residue by methionylaminopeptidase [Boutin, 1997; Farazi et al., 2001; Resh, 2006]. It is a relatively common lipid modification of many signal transducers, and contributes to direct protein anchoring to cellular membranes, which is required for their proper function. Cordeddu et al. [2009] recently discovered that aberrantly acquired N-myristoylation of SHOC2, a cytoplasmic leucine-rich repeat-containing protein that positively modulates RAS-MAPK signal flow, underlies a clinically distinctive condition previously termed Noonan-like syndrome with loose anagen hair (NS/LAH, OMIM 607721) [Mazzanti et al., 2003]. In this condition, features are at first view reminiscent of NS. The phenotype of these subjects, however, is notable for the observation that they exhibit reduced growth associated with proven GH deficiency, cognitive deficits, distinctive hyperactive behavior, and hair anomalies including easily pluckable, sparse, thin, slow growing hair. In a subgroup of these subjects, a diagnosis of loose anagen hair (LAH) was confirmed by microscopic examination of pulled hairs, many of which were in the anagen phase but lacked an inner and outer root sheath. Most of them exhibited hairless and darkly pigmented skin with eczema or ichthyosis, and tendency to pruritus. Ectodermal anomalies also included sparse eyebrows and dystrophic or thin nails. Voice was characteristically hoarse or hypernasal, the latter documented in 1 subject and caused by velopharyngeal insufficiency. Cardiac anomalies are observed in the majority of the cases, with dysplasia of the mitral valve and septal defects significantly overrepresented compared with the general NS population [Cordeddu et al., 2009]. All of the patients with NS/LAH screened so far share a c.4A>G change in SHOC2, which predicts the substitution of Ser2 by Gly. This amino acid change promotes N-myristoylation of the protein, and causes aberrant targeting of SHOC2 to the plasma membrane and impaired translocation to the nucleus upon growth factor stimulation (fig. 7) [Cordeddu et al., 2009].
Fig. 7.
The disease-causing c.4A>G change in SHOC2 promotes protein myristoylation and cell membrane targeting. A SHOC2 genomic organization and protein structure. The coding exons are shown at the top as numbered filled boxes. Intronic regions are reported as dotted lines. SHOC2 motifs comprise an N-terminal lysine-rich region (grey colored) followed by 19 leucine-rich repeats. Numbers above the domain structure indicate the amino acid boundaries of those domains. B Confocal laser scanning microscopy analysis documents that SHOC2wt (red) is uniformly distributed in the cytoplasm and nucleus in starved cells (left), while SHOC2S2G (red) is specifically targeted to the cell membrane. Actin cytoskeleton (green) and nuclei (blue) are also shown.
SHOC2 is a widely expressed protein composed almost entirely of leucine-rich repeats (LRR) and has a lysine-rich sequence at the N-terminus (fig. 7). In C. elegans, where SHOC2/SUR-8 was discovered, the protein acts as a positive modulator of signal transduction elicited by EGL-15 and LET-23, and mediated by LET-60, homologues of vertebrate FGFR, EGFR and RAS family members, respectively [Selfors et al., 1998; Sieburth et al., 1998]. Since LRRs can provide a structural framework for protein-protein interactions, SHOC2 is believed to function as a scaffold linking RAS to downstream signal transducers. It has recently been reported that SHOC2 functions as a regulatory subunit of the catalytic subunit of protein phosphatase 1 (PP1C) [Rodriguez-Viciana et al., 2006a]. By binding GTP-MRAS, SHOC2 promotes PP1C translocation to the membrane, allowing PP1C-mediated RAF1 dephosphorylation at residue Ser259, which is required for stable RAF1 translocation to the plasma membrane and catalytic activation. According to this model, constitutive membrane translocation of the disease-causing SHOC2S2G is expected to promote prolonged PP1C-mediated RAF1 dephosphorylation at Ser259 and, consequently, sustained RAF1-stimulated MAPK activation. Initial functional characterization of the mutant protein indicates that the expression of SHOC2S2G enhances ERK activation in a cell type-specific fashion [Cordeddu et al., 2009]. The observations that subcellular localization of SHOC2 is restricted to the nucleus following EGF stimulation and that SHOC2S2G ectopic expression in Caenorhabditis elegans engenders protruding vulva, a neomorphic phenotype previously associated with aberrant signaling, suggest that the disease-causing mutant might exert a wider perturbing effect on intracellular signaling. Of note, this discovery documents the first example of an acquired co-translational modification causing human disease.
MEK1
One germline mutation in MEK1, predicting the Asp67Asn amino acid substitution, has recently been documented in 2 unrelated subjects exhibiting a phenotype fitting NS [Nava et al., 2007]. Mutations in MEK1 and MEK2 had been reported to account for approximately 20% of CFCS [Rodriguez-Viciana et al., 2006b; Narumi et al., 2007; Nava et al., 2007; Nyström et al., 2008; Schulz et al., 2008; Dentici et al., 2009], including 1 subject with MGCL as an associated feature [Neumann et al., 2009]. These findings would be suggestive of phenotypic heterogeneity. One additional previously unreported variant (Glu44Gly), which was identified in a third sporadic case and her apparently clinically unaffected mother but not in 200 population-matching controls, is likely to represent a private polymorphism [Nava et al., 2007]. According to this study, MEK1 gene mutations would account for approximately 3% of PTPN11- and SOS1-mutation negative NS cases. In both NS and CFCS, MEK gene mutations are mostly missense changes affecting residues located in the regulatory region and the N-terminal portion of the catalytic domain. A few in-frame deletions affecting those domains have also been reported in CFCS.
MEK1 (OMIM 176872) and the functionally related MEK2 belong to a family of dual specificity kinases that phosphorylate ERK proteins at tyrosine and serine/threonine residues [Zheng and Guan, 1993]. The MEK proteins share a conserved structure including a negative regulatory domain at the N-terminus and a single protein kinase domain. MEK1 and MEK2 are both effectors of RAF proteins, but appear to play non-redundant roles. In particular, genetic evidence from mouse models indicates that MEK1 function is required during embryonic development [Giroux et al., 1999], while MEK2 is dispensable [Bélanger et al., 2003]. Of note, even though MEK kinase activity is necessary for cell transformation via the MAPK cascade [Cowley et al., 1994], and constitutively active MEK mutants promote transformation [Mansour et al., 1994], mutations in these genes have not been reported in human cancers so far (COSMIC database, http://www.sanger.ac.uk/genetics/CGP/cosmic/). Functional characterization of the 3 CFCS-causing mutants documented that their transient expression in 293T cells is more active than the wild-type protein in stimulating ERK phosphorylation basally [Rodriguez-Viciana et al., 2006b]. No data on the effect of the Asp67Asn change on MEK1 function and MAPK signaling is currently available.
Concluding Remarks
From a genetic point of view, NS was a poorly understood condition until recently. Following the discovery of PTPN11 as a major disease gene for the disorder in 2001, six additional disease genes have been identified subsequently. It is now established that NS is caused by hyperactivation of the RAS-MAPK transduction pathway. Mutations in identified disease genes are estimated to account for at least 70% of affected individuals, indicating that other disease genes responsible for a substantial portion of NS remain to be identified. Screening efforts and genotype-phenotype correlation analyses have documented that mutations in identified disease genes are associated with distinct phenotypes, explaining, in part, the wide clinical diversity characterizing this relatively common developmental disorder.
It should be considered that the overlapping features observed among NS and related disorders of the NCFCS family, the wide breadth of phenotypes within each trait, and absence of clinical features with pathognomonic value and consensus on specific and routinely used diagnostic criteria make diagnosis of these diseases challenging, particularly during early infancy and in adulthood. Such a failure has direct impact on patient management because of the prognostic relevance of diagnosis (prevalence and extent of cardiac disease, degree of cognitive and growth impairment, cancer predisposition). Molecular diagnosis now offers the opportunity to overcome the weakness of subjective clinical criteria and represents a highly informative prognostic tool, with direct impact on counseling and appropriate patient management.
Acknowledgements
The authors apologize to colleagues whose work was not cited due to limited space. Research in the authors’ laboratories is supported in part by grants from Telethon-Italy (GGP07115) and ERARE 2009 (NSEuroNet) to M.T., from ‘Associazione Italiana Sindromi di Costello e Cardiofaciocutanea’ to M.T. and G.Z., and from the National Institutes of Health (HL71207) and March of Dimes (06-1047) to B.D.G.
References
- Adekunle O, Gopee A, el-Sayed M, Thilaganathan B. Increased first trimester nuchal translucency: Pregnancy and infant outcomes after routine screening for Down's syndrome in an unselected antenatal population. Br J Radiol. 1999;72:457–460. doi: 10.1259/bjr.72.857.10505009. [DOI] [PubMed] [Google Scholar]
- Adjei AA. Blocking oncogenic Ras signaling for cancer therapy. J Natl Cancer Inst. 2001;93:1062–1074. doi: 10.1093/jnci/93.14.1062. [DOI] [PubMed] [Google Scholar]
- Ahmed ML, Foot AB, Edge JA, Lamkin VA, Savage MO, Dunger DB. Noonan's syndrome: Abnormalities of the growth hormone/IGF axis and the response to treatment with human biosynthetic growth hormone. Acta Paediatr Scand. 1991;80:446–450. doi: 10.1111/j.1651-2227.1991.tb11880.x. [DOI] [PubMed] [Google Scholar]
- Alfieri P, Cesarini L, Zampino G, Pantaleoni F, Selicorni A, et al. Visual function in Noonan and LEOPARD syndrome. Neuropediatrics. 2008;39:335–340. doi: 10.1055/s-0029-1216354. [DOI] [PubMed] [Google Scholar]
- Allanson JE. Noonan syndrome. Am J Med Genet C Semin Med Genet. 2007;145C:274–279. doi: 10.1002/ajmg.c.30138. [DOI] [PubMed] [Google Scholar]
- Allanson JE, Hall JG, Hughes HE, Preus M, Witt RD. Noonan syndrome: The changing phenotype. Am J Med Genet. 1985a;21:507–514. doi: 10.1002/ajmg.1320210313. [DOI] [PubMed] [Google Scholar]
- Allanson JE, Hall JG, Van Allen MI. Noonan phenotype associated with neurofibromatosis. Am J Med Genet. 1985b;21:457–462. doi: 10.1002/ajmg.1320210307. [DOI] [PubMed] [Google Scholar]
- Aoki Y, Niihori T, Kawame H, Kurosawa K, Ohashi H, et al. Germline mutations in HRAS proto-oncogene cause Costello syndrome. Nat Genet. 2005;37:1038–1040. doi: 10.1038/ng1641. [DOI] [PubMed] [Google Scholar]
- Armour CM, Allanson JE. Further delineation of cardio-facio-cutaneous syndrome: clinical features of 38 individuals with proven mutations. J Med Genet. 2008;45:249–254. doi: 10.1136/jmg.2007.054460. [DOI] [PubMed] [Google Scholar]
- Bader-Meunier B, Tchernia G, Mielot F, Fontaine JL, Thomas C, et al. Occurrence of myeloproliferative disorder in patients with Noonan syndrome. J Pediatr. 1997;130:885–889. doi: 10.1016/s0022-3476(97)70273-7. [DOI] [PubMed] [Google Scholar]
- Baltaxe HA, Lee JG, Ehlers KH, Engle MA. Pulmonary lymphangiectasia demonstrated by lymphangiography in 2 patients with Noonan's syndrome. Radiology. 1975;115:149–153. doi: 10.1148/115.1.149. [DOI] [PubMed] [Google Scholar]
- Baralle D, Mattocks C, Kalidas K, Elmslie F, Whittaker J, et al. Different mutations in the NF1 gene are associated with neurofibromatosis-Noonan syndrome (NFNS) Am J Med Genet. 2003;119A:1–8. doi: 10.1002/ajmg.a.20023. [DOI] [PubMed] [Google Scholar]
- Barbacid M. Ras genes. Annu Rev Biochem. 1987;56:779–827. doi: 10.1146/annurev.bi.56.070187.004023. [DOI] [PubMed] [Google Scholar]
- Bélanger LF, Roy S, Tremblay M, Brott B, Steff AM, et al. Mek2 is dispensable for mouse growth and development. Mol Cell Biol. 2003;23:4778–4787. doi: 10.1128/MCB.23.14.4778-4787.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beneteau C, Cavé H, Moncla A, Dorison N, Munnich A, et al. SOS1 and PTPN11 mutations in five cases of Noonan syndrome with multiple giant cell lesions. Eur J Hum Genet. 2009;17:1216–1221. doi: 10.1038/ejhg.2009.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentires-Alj M, Paez JG, David FS, Keilhack H, Halmos B, et al. Activating mutations of the Noonan syndrome-associated SHP2/PTPN11 gene in human solid tumors and adult acute myelogenous leukemia. Cancer Res. 2004;64:8816–8820. doi: 10.1158/0008-5472.CAN-04-1923. [DOI] [PubMed] [Google Scholar]
- Bertola DR, Kim CA, Sugayama SM, Albano LM, Wagenfuhr J, et al. Cardiac findings in 31 patients with Noonan's syndrome. Arq Bras Cardiol. 2000;75:409–412. doi: 10.1590/s0066-782x2000001100005. [DOI] [PubMed] [Google Scholar]
- Bertola DR, Pereira AC, Passetti F, de Oliveira PS, Messiaen L, et al. Neurofibromatosis-Noonan syndrome: Molecular evidence of the concurrence of both disorders in a patient. Am J Med Genet A. 2005;136:242–245. doi: 10.1002/ajmg.a.30813. [DOI] [PubMed] [Google Scholar]
- Binder G, Neuer K, Ranke MB, Wittekindt NE. PTPN11 mutations are associated with mild growth hormone resistance in individuals with Noonan syndrome. J Clin Endocrinol Metab. 2005;90:5377–5381. doi: 10.1210/jc.2005-0995. [DOI] [PubMed] [Google Scholar]
- Bos JL. Ras oncogenes in human cancer: a review. Cancer Res. 1989;49:4682–4689. [PubMed] [Google Scholar]
- Boutin JA. Myristoylation. Cell Signal. 1997;9:15–35. doi: 10.1016/s0898-6568(96)00100-3. [DOI] [PubMed] [Google Scholar]
- Brems H, Chmara M, Sahbatou M, Denayer E, Taniguchi K, et al. Germline loss-of-function mutations in SPRED1 cause a neurofibromatosis 1-like phenotype. Nat Genet. 2007;39:1120–1126. doi: 10.1038/ng2113. [DOI] [PubMed] [Google Scholar]
- Brown DC, Macfarlane CE, McKenna WJ, Patton MA, Dunger DB, et al. Growth hormone therapy in Noonan's syndrome: Non-cardiomyopathic congenital heart disease does not adversely affect growth improvement. J Pediatr Endocrinol Metab. 2002;15:851–852. doi: 10.1515/jpem.2002.15.6.851. [DOI] [PubMed] [Google Scholar]
- Burch M, Sharland M, Shinebourne E, Smith G, Patton M, McKenna W. Cardiologic abnormalities in Noonan syndrome: Phenotypic diagnosis and echocardiographic assessment of 118 patients. J Am Coll Cardiol. 1993;22:1189–1192. doi: 10.1016/0735-1097(93)90436-5. [DOI] [PubMed] [Google Scholar]
- Carey JC. Neurofibromatosis-Noonan syndrome. Am J Med Genet. 1998;75:263–264. doi: 10.1002/(sici)1096-8628(19980123)75:3<263::aid-ajmg7>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Carta C, Pantaleoni F, Bocchinfuso G, Stella L, Vasta I, et al. Germline missense mutations affecting KRAS isoform b are associated with a severe Noonan syndrome phenotype. Am J Hum Genet. 2006;79:129–135. doi: 10.1086/504394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesarini L, Alfieri P, Pantaleoni F, Vasta I, Cerutti M, et al. Cognitive profile of disorders associated with dysregulation of the RAS/MAPK signaling cascade. Am J Med Genet. 2009;149A:140–146. doi: 10.1002/ajmg.a.32488. [DOI] [PubMed] [Google Scholar]
- Chan RJ, Leedy MB, Munugalavadla V, Voorhorst CS, Li Y, et al. Human somatic PTPN11 mutations induce hematopoietic-cell hypersensitivity to granulocyte-macrophage colony-stimulating factor. Blood. 2005;105:3737–3742. doi: 10.1182/blood-2004-10-4002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chardin P, Camonis JH, Gale NW, van Aelst L, Schlessinger J, et al. Human Sos1: a guanine nucleotide exchange factor for Ras that binds to GRB2. Science. 1993;260:1338–1343. doi: 10.1126/science.8493579. [DOI] [PubMed] [Google Scholar]
- Chen RH, Corbalan-Garcia S, Bar-Sagi D. The role of the PH domain in the signal-dependent membrane targeting of Sos. EMBO J. 1997;16:1351–1359. doi: 10.1093/emboj/16.6.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Takita J, Hiwatari M, Igarashi T, Hanada R, et al. Mutations of the PTPN11 and RAS genes in rhabdomyosarcoma and pediatric hematological malignancies. Genes Chromosomes Cancer. 2006;45:583–591. doi: 10.1002/gcc.20322. [DOI] [PubMed] [Google Scholar]
- Choong K, Freedman MH, Chitayat D, Kelly EN, Taylor G, Zipursky A. Juvenile myelomonocytic leukemia and Noonan syndrome. J Pediatr Hematol Oncol. 1999;21:523–527. [PubMed] [Google Scholar]
- Clanton DJ, Hattori S, Shih TY. Mutations of the Ras gene product p21 that abolish guanine nucleotide binding. Proc Natl Acad Sci USA. 1986;83:5076–5080. doi: 10.1073/pnas.83.14.5076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MM, Jr, Gorlin RJ. Noonan-like/multiple giant cell lesion syndrome. Am J Med Genet. 1991;40:159–166. doi: 10.1002/ajmg.1320400208. [DOI] [PubMed] [Google Scholar]
- Colby WW, Hayflick JS, Clark SG, Levinson AD. Biochemical characterization of polypeptides encoded by mutated human Ha-ras1 genes. Mol Cell Biol. 1986;6:730–734. doi: 10.1128/mcb.6.2.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordeddu V, Di Schiavi E, Pennacchio LA, Ma'ayan A, Sarkozy A, et al. Mutation of SHOC2 promotes aberrant protein N-myristoylation and causes Noonan-like syndrome with loose anagen hair. Nat Genet. 2009;41:1022–1026. doi: 10.1038/ng.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello JM. A new syndrome. NZ Med J. 1971;74:397. [Google Scholar]
- Costello JM. A new syndrome: mental subnormality and nasal papillomata. Aust Paediatr J. 1977;13:114–118. doi: 10.1111/j.1440-1754.1977.tb01135.x. [DOI] [PubMed] [Google Scholar]
- Cotterill AM, McKenna WJ, Brady AF, Sharland M, Elsawi M, et al. The short-term effects of growth hormone therapy on height velocity and cardiac ventricular wall thickness in children with Noonan's syndrome. J Clin Endocrinol Metab. 1996;81:2291–2297. doi: 10.1210/jcem.81.6.8964866. [DOI] [PubMed] [Google Scholar]
- Cowley S, Paterson H, Kemp P, Marshall CJ. Activation of MAP kinase kinase is necessary and sufficient for PC12 differentiation and for transformation of NIH 3T3 cells. Cell. 1994;77:841–852. doi: 10.1016/0092-8674(94)90133-3. [DOI] [PubMed] [Google Scholar]
- Cremers CW, van der Burgt CJ. Hearing loss in Noonan syndrome. Int J Pediatr Otorhinolaryngol. 1992;23:81–84. doi: 10.1016/0165-5876(92)90082-z. [DOI] [PubMed] [Google Scholar]
- Dance M, Montagner A, Salles JP, Yart A, Raynal P. The molecular functions of Shp2 in the Ras/Mitogen-activated protein kinase (ERK1/2) pathway. Cell Signal. 2008;20:453–459. doi: 10.1016/j.cellsig.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Davies H, Bignell GR, Cox C, Stephens P, Edkins S, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417:949–954. doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- De Luca A, Bottillo I, Sarkozy A, Carta C, Neri C, et al. NF1 gene mutations represent the major molecular event underlying neurofibromatosis-Noonan syndrome. Am J Hum Genet. 2005;77:1092–1101. doi: 10.1086/498454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denayer E, Parret A, Chmara M, Schubbert S, Vogels A, et al. Mutation analysis in Costello syndrome: functional and structural characterization of the HRAS p.Lys117Arg mutation. Hum Mutat. 2008;29:232–239. doi: 10.1002/humu.20616. [DOI] [PubMed] [Google Scholar]
- Dentici ML, Sarkozy A, Pantaleoni F, Carta C, Lepri F, et al. Spectrum of MEK1 and MEK2 gene mutations in cardio-facio-cutaneous syndrome and genotype-phenotype correlations. Eur J Hum Genet. 2009;17:733–740. doi: 10.1038/ejhg.2008.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Der CJ, Pan BT, Cooper GM. RasH mutants deficient in GTP binding. Mol Cell Biol. 1986;6:3291–3294. doi: 10.1128/mcb.6.9.3291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhomen N, Marais R. New insight into BRAF mutations in cancer. Curr Opin Genet Dev. 2007;17:31–39. doi: 10.1016/j.gde.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Digilio MC, Conti E, Sarkozy A, Mingarelli R, Dottorini T, et al. Grouping of multiple-lentigines/LEOPARD and Noonan syndromes on the PTPN11 gene. Am J Hum Genet. 2002;71:389–394. doi: 10.1086/341528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digilio MC, Sarkozy A, de Zorzi A, Pacileo G, Limongelli G, et al. LEOPARD syndrome: clinical diagnosis in the first year of life. Am J Med Genet A. 2006;140A:740–674. doi: 10.1002/ajmg.a.31156. [DOI] [PubMed] [Google Scholar]
- Duncan WJ, Fowler RS, Farkas LG, Ross RB, Wright AW, et al. A comprehensive scoring system for evaluating Noonan syndrome. Am J Med Genet. 1981;10:37–50. doi: 10.1002/ajmg.1320100106. [DOI] [PubMed] [Google Scholar]
- Emuss V, Garnett M, Mason C, Marais R. Mutations of C-RAF are rare in human cancer because C-RAF has a low basal kinase activity compared with B-RAF. Cancer Res. 2005;65:9719–9726. doi: 10.1158/0008-5472.CAN-05-1683. [DOI] [PubMed] [Google Scholar]
- Estep AL, Tidyman WE, Teitell MA, Cotter PD, Rauen KA. HRAS mutations in Costello syndrome: detection of constitutional activating mutations in codon 12 and 13 and loss of wild-type allele in malignancy. Am J Med Genet A. 2006;140:8–16. doi: 10.1002/ajmg.a.31078. [DOI] [PubMed] [Google Scholar]
- Farazi TA, Waksman G, Gordon JI. The biology and enzymology of protein N-myristoylation. J Biol Chem. 2001;276:39501–39504. doi: 10.1074/jbc.R100042200. [DOI] [PubMed] [Google Scholar]
- Feig LA, Pan BT, Roberts TM, Cooper GM. Isolation of Ras GTP-binding mutants using an in situ colony-binding assay. Proc Natl Acad Sci USA. 1986;83:4607–4611. doi: 10.1073/pnas.83.13.4607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira LV, Souza SA, Arnhold IJ, Mendonca BB, Jorge AA. PTPN11 (protein tyrosine phosphatase, nonreceptor type 11) mutations and response to growth hormone therapy in children with Noonan syndrome. J Clin Endocrinol Metab. 2005;90:5156–5160. doi: 10.1210/jc.2004-2559. [DOI] [PubMed] [Google Scholar]
- Fisher E, Weiss EB, Michals K, DuBrow IW, Hastrieter AR, Matalon R. Spontaneous chylothorax in Noonan's syndrome. Eur J Pediatr. 1982;138:282–284. doi: 10.1007/BF00441221. [DOI] [PubMed] [Google Scholar]
- Friday BB, Adjei AA. K-ras as a target for cancer therapy. Biochim Biophys Acta. 2005;1756:127–144. doi: 10.1016/j.bbcan.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Fryer AE, Holt PJ, Hughes HE. The cardio-facio-cutaneous (CFC) syndrome and Noonan syndrome: Are they the same? Am J Med Genet. 1991;38:548–551. doi: 10.1002/ajmg.1320380410. [DOI] [PubMed] [Google Scholar]
- Fukuda M, Horibe K, Miyajima Y, Matsumoto K, Nagashima M. Spontaneous remission of juvenile chronic myelomonocytic leukemia in an infant with Noonan syndrome. J Pediatr Hematol Oncol. 1997;19:177–179. doi: 10.1097/00043426-199703000-00019. [DOI] [PubMed] [Google Scholar]
- George CD, Patton MA, el Sawi M, Sharland M, Adam EJ. Abdominal ultrasound in Noonan syndrome: A study of 44 patients. Pediatr Radiol. 1993;23:316–318. doi: 10.1007/BF02010926. [DOI] [PubMed] [Google Scholar]
- Giroux S, Tremblay M, Bernard D, Cardin-Girard JF, Aubry S, et al. Embryonic death of Mek1-deficient mice reveals a role for this kinase in angiogenesis in the labyrinthine region of the placenta. Curr Biol. 1999;9:369–372. doi: 10.1016/s0960-9822(99)80164-x. [DOI] [PubMed] [Google Scholar]
- Gorlin RJ, Anderson RC, Moller JH. The leopard (multiple lentigines) syndrome revisited. Birth Defects Orig Artic Ser. 1971;7:110–115. [PubMed] [Google Scholar]
- Gorlin JR, Cohen MM, Levin LS. Leopard syndrome. In: Gorlin JR, Cohen MM, Levin LS, editors. Syndromes of the Head and Neck. New York: Oxford University Press; 1990. pp. 461–464. [Google Scholar]
- Graham JM, Jr, Kramer N, Bejjani BA, Thiel CT, Carta C, et al. Genomic duplication of PTPN11 is an uncommon cause of Noonan syndrome. Am J Med Genet A. 2009;149A:2122–2128. doi: 10.1002/ajmg.a.32992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gripp KW. Tumor predisposition in Costello syndrome. Am J Med Genet C Semin Med Genet. 2005;137C:72–77. doi: 10.1002/ajmg.c.30065. [DOI] [PubMed] [Google Scholar]
- Gripp KW, Lin AE, Stabley DL, Nicholson L, Scott CI, Jr, et al. HRAS mutation analysis in Costello syndrome: genotype and phenotype correlation. Am J Med Genet A. 2006;140A:1–7. doi: 10.1002/ajmg.a.31047. [DOI] [PubMed] [Google Scholar]
- Hanna N, Montagner A, Lee WH, Miteva M, Vidal M, et al. Reduced phosphatase activity of SHP-2 in LEOPARD syndrome: consequences for PI3K binding on Gab1. FEBS Lett. 2006;580:2477–2482. doi: 10.1016/j.febslet.2006.03.088. [DOI] [PubMed] [Google Scholar]
- Hanna N, Parfait B, Talaat IM, Vidaud M, Elsedfy HH. SOS1: a new player in the Noonan-like/multiple giant cell lesion syndrome. Clin Genet. 2009;75:568–571. doi: 10.1111/j.1399-0004.2009.01149.x. [DOI] [PubMed] [Google Scholar]
- Hennekam RC. Costello syndrome: an overview. Am J Med Genet C Semin Med Genet. 2003;117C:42–48. doi: 10.1002/ajmg.c.10019. [DOI] [PubMed] [Google Scholar]
- Hernandez RJ, Stern AM, Rosenthal A. Pulmonary lymphangiectasis in Noonan syndrome. AJR Am J Roentgenol. 1980;134:75–80. doi: 10.2214/ajr.134.1.75. [DOI] [PubMed] [Google Scholar]
- Herzog DB, Logan R, Kooistra JB. The Noonan syndrome with intestinal lymphangiectasia. J Pediatr. 1976;88:270–272. doi: 10.1016/s0022-3476(76)80998-5. [DOI] [PubMed] [Google Scholar]
- Hiippala A, Eronen M, Taipale P, Salonen R, Hiilesmaa V. Fetal nuchal translucency and normal chromosomes: A long-term follow-up study. Ultrasound Obstet Gynecol. 2001;18:18–22. doi: 10.1046/j.1469-0705.2001.00481.x. [DOI] [PubMed] [Google Scholar]
- Hof P, Pluskey S, Dhe-Paganon S, Eck MJ, Shoelson SE. Crystal structure of the tyrosine phosphatase SHP-2. Cell. 1998;92:441–450. doi: 10.1016/s0092-8674(00)80938-1. [DOI] [PubMed] [Google Scholar]
- Hüffmeier U, Zenker M, Hoyer J, Fahsold R, Rauch A. A variable combination of features of Noonan syndrome and neurofibromatosis type I are caused by mutations in the NF1 gene. Am J Med Genet A. 2006;140A:2749–2756. doi: 10.1002/ajmg.a.31547. [DOI] [PubMed] [Google Scholar]
- Hugues L, Cavé H, Philippe N, Pereira S, Fenaux P, Preudhomme C. Mutations of PTPN11 are rare in adult myeloid malignancies. Haematologica. 2005;90:853–854. [PubMed] [Google Scholar]
- Jafarov T, Ferimazova N, Reichenberger E. Noonan-like syndrome mutations in PTPN11 in patients diagnosed with cherubism. Clin Genet. 2005;68:190–191. doi: 10.1111/j.1399-0004.2005.00475.x. [DOI] [PubMed] [Google Scholar]
- Johnson L, Greenbaum D, Cichowski K, Mercer K, Murphy E, et al. K-ras is an essential gene in the mouse with partial functional overlap with N-ras. Genes Dev. 1997;11:2468–2481. doi: 10.1101/gad.11.19.2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongmans M, Sistermans EA, Rikken A, Nillesen WM, Tamminga R, et al. Genotypic and phenotypic characterization of Noonan syndrome: New data and review of the literature. Am J Med Genet. 2005;A 134A:165–170. doi: 10.1002/ajmg.a.30598. [DOI] [PubMed] [Google Scholar]
- Keilhack H, David FS, McGregor M, Cantley LC, Neel BG. Diverse biochemical properties of Shp2 mutants. Implications for disease phenotypes. J Biol Chem. 2005;280:30984–30993. doi: 10.1074/jbc.M504699200. [DOI] [PubMed] [Google Scholar]
- Kerr B, Delrue MA, Sigaudy S, Perveen R, Marche M, et al. Genotype-phenotype correlation in Costello syndrome: HRAS mutation analysis in 43 cases. J Med Genet. 2006;43:401–405. doi: 10.1136/jmg.2005.040352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koera K, Nakamura K, Nakao K, Miyoshi J, Toyoshima K, et al. K-ras is essential for the development of the mouse embryo. Oncogene. 1997;15:1151–1159. doi: 10.1038/sj.onc.1201284. [DOI] [PubMed] [Google Scholar]
- Kontaridis MI, Swanson KD, David FS, Barford D, Neel BG. PTPN11 (Shp2) mutations in LEOPARD syndrome have dominant negative, not activating, effects. J Biol Chem. 2006;281:6785–6792. doi: 10.1074/jbc.M513068200. [DOI] [PubMed] [Google Scholar]
- Koudova M, Seemanova E, Zenker M. Novel BRAF mutation in a patient with LEOPARD syndrome and normal intelligence. Eur J Med Genet. 2009;52:337–340. doi: 10.1016/j.ejmg.2009.04.006. [DOI] [PubMed] [Google Scholar]
- Kratz CP, Niemeyer CM, Castleberry RP, Cetin M, Bergsträsser E, et al. The mutational spectrum of PTPN11 in juvenile myelomonocytic leukemia and Noonan syndrome/myeloproliferative disease. Blood. 2005;106:2183–2185. doi: 10.1182/blood-2005-02-0531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kratz CP, Niemeyer CM, Thomas C, Bauhuber S, Matejas V, et al. Mutation analysis of Son of Sevenless in juvenile myelomonocytic leukemia. Leukemia. 2007;21:1108–1109. doi: 10.1038/sj.leu.2404620. [DOI] [PubMed] [Google Scholar]
- Kratz CP, Zampino G, Kriek M, Kant SG, Leoni C, et al. Craniosynostosis in patients with Noonan syndrome caused by germline KRAS mutations. Am J Med Genet A. 2009;149A:1036–1040. doi: 10.1002/ajmg.a.32786. [DOI] [PubMed] [Google Scholar]
- Lanning P, Simila S, Suramo I, Paavilainen T. Lymphatic abnormalities in Noonan's syndrome. Pediatr Radiol. 1978;7:106–109. doi: 10.1007/BF00975679. [DOI] [PubMed] [Google Scholar]
- Lee JC, Tartaglia M, Gelb BD, Fridrich K, Sachs S, et al. Phenotypic and genotypic characterization of Noonan-like/multiple giant cell lesion syndrome. J Med Genet. 2005;42:e11. doi: 10.1136/jmg.2004.024091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KA, Williams B, Roza K, Ferguson H, David K, et al. PTPN11 analysis for the prenatal diagnosis of Noonan syndrome in fetuses with abnormal ultrasound findings. Clin Genet. 2009;75:190–194. doi: 10.1111/j.1399-0004.2008.01085.x. [DOI] [PubMed] [Google Scholar]
- Lee NB, Kelly L, Sharland M. Ocular manifestations of Noonan syndrome. Eye. 1992;6:328–334. doi: 10.1038/eye.1992.66. [DOI] [PubMed] [Google Scholar]
- Legius E, Schrander-Stumpel C, Schollen E, Pulles-Heintzberger C, Gewillig M, Fryns JP. PTPN11 mutations in LEOPARD syndrome. J Med Genet. 2002;39:571–574. doi: 10.1136/jmg.39.8.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leicht DT, Balan V, Kaplun A, Singh-Gupta V, Kaplun L, et al. Raf kinases: function, regulation and role in human cancer. Biochim Biophys Acta. 2007;1773:1196–1212. doi: 10.1016/j.bbamcr.2007.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loh ML, Reynolds MG, Vattikuti S, Gerbing RB, Alonzo TA, et al. PTPN11 mutations in pediatric patients with acute myeloid leukemia: Results from the children's cancer group. Leukemia. 2004a;18:1831–1834. doi: 10.1038/sj.leu.2403492. [DOI] [PubMed] [Google Scholar]
- Loh ML, Vattikuti S, Schubbert S, Reynolds MG, Carlson E, et al. Mutations in PTPN11 implicate the SHP-2 phosphatase in leukemogenesis. Blood. 2004b;103:2325–2331. doi: 10.1182/blood-2003-09-3287. [DOI] [PubMed] [Google Scholar]
- Loh ML, Martinelli S, Cordeddu V, Reynolds MG, Vattikuti S, et al. Acquired PTPN11 mutations occur rarely in adult patients with myelodysplastic syndromes and chronic myelomonocytic leukemia. Leuk Res. 2005;29:459–462. doi: 10.1016/j.leukres.2004.10.001. [DOI] [PubMed] [Google Scholar]
- MacFarlane CE, Brown DC, Johnston LB, Patton MA, Dunger DB, et al. Growth hormone therapy and growth in children with Noonan's syndrome: Results of 3 years' follow-up. J Clin Endocrinol Metab. 2001;86:1953–1956. doi: 10.1210/jcem.86.5.7468. [DOI] [PubMed] [Google Scholar]
- Mansour SJ, Matten WT, Hermann AS, Candia JM, Rong S, et al. Transformation of mammalian cells by constitutively active MAP kinase kinase. Science. 1994;265:966–970. doi: 10.1126/science.8052857. [DOI] [PubMed] [Google Scholar]
- Marcus KA, Sweep CG, van der Burgt I, Noordam C. Impaired Sertoli cell function in males diagnosed with Noonan syndrome. J Pediatr Endocrinol Metab. 2008;21:1079–1084. doi: 10.1515/jpem.2008.21.11.1079. [DOI] [PubMed] [Google Scholar]
- Margarit SM, Sondermann H, Hall BE, Nagar B, Hoelz A, et al. Structural evidence for feedback activation by Ras.GTP of the Ras-specific nucleotide exchange factor SOS. Cell. 2003;112:685–695. doi: 10.1016/s0092-8674(03)00149-1. [DOI] [PubMed] [Google Scholar]
- Marino B, Digilio MC, Toscano A, Giannotti A, Dallapiccola B. Congenital heart diseases in children with Noonan syndrome: An expanded cardiac spectrum with high prevalence of atrioventricular canal. J Pediatr. 1999;135:703–706. doi: 10.1016/s0022-3476(99)70088-0. [DOI] [PubMed] [Google Scholar]
- Martinelli S, Carta C, Flex E, Binni F, Cordisco EL, et al. Activating PTPN11 mutations play a minor role in pediatric and adult solid tumors. Cancer Genet Cytogenet. 2006;166:124–129. doi: 10.1016/j.cancergencyto.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Martinelli S, Torreri P, Tinti M, Stella L, Bocchinfuso G, et al. Diverse driving forces underlie the invariant occurrence of the T42A, E139D, I282V and T468M SHP2 amino acid substitutions causing Noonan and LEOPARD syndromes. Hum Mol Genet. 2008;17:2018–2029. doi: 10.1093/hmg/ddn099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinelli S, McDowell HP, Vigne SD, Kokai G, Uccini S, et al. RAS signaling dysregulation in human embryonal rhabdomyosarcoma. Genes Chromosomes Cancer. 2009;48:975–982. doi: 10.1002/gcc.20702. [DOI] [PubMed] [Google Scholar]
- Mascheroni E, Digilio MC, Cortis E, Devito R, Sarkozy A, et al. Pigmented villonodular synovitis in a patient with Noonan syndrome and SOS1 gene mutation. Am J Med Genet A. 2008;146A:2966–2967. doi: 10.1002/ajmg.a.32538. [DOI] [PubMed] [Google Scholar]
- Massarano AA, Wood A, Tait RC, Stevens R, Super M. Noonan syndrome: Coagulation and clinical aspects. Acta Paediatr. 1996;85:1181–1185. doi: 10.1111/j.1651-2227.1996.tb18225.x. [DOI] [PubMed] [Google Scholar]
- Mazzanti L, Cacciari E, Cicognani A, Bergamaschi R, Scarano E, Forabosco A. Noonan-like syndrome with loose anagen hair: a new syndrome? Am J Med Genet A. 2003;118A:279–286. doi: 10.1002/ajmg.a.10923. [DOI] [PubMed] [Google Scholar]
- Mikula M, Schreiber M, Husak Z, Kucerova L, Rüth J, et al. Embryonic lethality and fetal liver apoptosis in mice lacking the c-raf-1 gene. EMBO J. 2001;20:1952–1962. doi: 10.1093/emboj/20.8.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitin N, Rossman KL, Der CJ. Signaling interplay in Ras superfamily function. Curr Biol. 2005;15:R563–R574. doi: 10.1016/j.cub.2005.07.010. [DOI] [PubMed] [Google Scholar]
- Naficy S, Shepard NT, Telian SA. Multiple temporal bone anomalies associated with Noonan syndrome. Otolaryngol Head Neck Surg. 1997;116:265–267. doi: 10.1016/S0194-59989770339-5. [DOI] [PubMed] [Google Scholar]
- Narumi Y, Aoki Y, Niihori T, Neri G, Cavé H, et al. Molecular and clinical characterization of cardio-facio-cutaneous (CFC) syndrome: overlapping clinical manifestations with Costello syndrome. Am J Med Genet A. 2007;143A:799–807. doi: 10.1002/ajmg.a.31658. [DOI] [PubMed] [Google Scholar]
- Nava C, Hanna N, Michot C, Pereira S, Pouvreau N, et al. Cardio-facio-cutaneous and Noonan syndromes due to mutations in the RAS/MAPK signalling pathway: genotype-phenotype relationships and overlap with Costello syndrome. J Med Genet. 2007;44:763–771. doi: 10.1136/jmg.2007.050450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neel BG, Gu H, Pao L. The ‘Shp’ing news: SH2 domain-containing tyrosine phosphatases in cell signaling. Trends Biochem Sci. 2003;28:284–293. doi: 10.1016/S0968-0004(03)00091-4. [DOI] [PubMed] [Google Scholar]
- Neri G, Zollino M, Reynolds JF. The Noonan-CFC controversy. Am J Med Genet. 1991;39:367–370. doi: 10.1002/ajmg.1320390323. [DOI] [PubMed] [Google Scholar]
- Neumann TE, Allanson J, Kavamura I, Kerr B, Neri G, et al. Multiple giant cell lesions in patients with Noonan syndrome and cardio-facio-cutaneous syndrome. Eur J Hum Genet. 2009;17:420–425. doi: 10.1038/ejhg.2008.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemeyer CM, Kratz CP. Paediatric myelodysplastic syndromes and juvenile myelomonocytic leukaemia: molecular classification and treatment options. Br J Haematol. 2008;140:610–624. doi: 10.1111/j.1365-2141.2007.06958.x. [DOI] [PubMed] [Google Scholar]
- Niihori T, Aoki Y, Narumi Y, Neri G, Cavé H, et al. Germline KRAS and BRAF mutations in cardio-facio-cutaneous syndrome. Nat Genet. 2006;38:294–296. doi: 10.1038/ng1749. [DOI] [PubMed] [Google Scholar]
- Nimnual A, Bar-Sagi D. The two hats of SOS. Sci STKE. 2002;145:PE36. doi: 10.1126/stke.2002.145.pe36. [DOI] [PubMed] [Google Scholar]
- Nimnual AS, Yatsula BA, Bar-Sagi D. Coupling of Ras and Rac guanosine triphosphatases through the Ras exchanger Sos. Science. 1998;279:560–563. doi: 10.1126/science.279.5350.560. [DOI] [PubMed] [Google Scholar]
- Nisbet DL, Griffin DR, Chitty LS. Prenatal features of Noonan syndrome. Prenat Diagn. 1999;19:642–647. doi: 10.1002/(sici)1097-0223(199907)19:7<642::aid-pd610>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Noonan JA. Hypertelorism with Turner phenotype. A new syndrome with associated congenital heart disease. Am J Dis Child. 1968;116:373–380. doi: 10.1001/archpedi.1968.02100020377005. [DOI] [PubMed] [Google Scholar]
- Noonan JA. Noonan syndrome. An update and review for the primary pediatrician. Clin Pediatr (Phila) 1994;33:548–555. doi: 10.1177/000992289403300907. [DOI] [PubMed] [Google Scholar]
- Noordam C, Draaisma JM, van den Nieuwenhof J, van der Burgt I, Otten BJ, Daniels O. Effects of growth hormone treatment on left ventricular dimensions in children with Noonan's syndrome. Horm Res. 2001;56:110–113. doi: 10.1159/000048101. [DOI] [PubMed] [Google Scholar]
- Noordam C, Peer PG, Francois I, De Schepper J, van den Burgt I, Otten BJ. Long-term GH treatment improves adult height in children with Noonan syndrome with and without mutations in protein tyrosine phosphatase, non-receptor-type 11. Eur J Endocrinol. 2008;159:203–208. doi: 10.1530/EJE-08-0413. [DOI] [PubMed] [Google Scholar]
- Noordam K, van der Burgt I, Brunner HG, Otten BJ. The relationship between clinical severity of Noonan's syndrome and growth, growth hormone (GH) secretion and response to GH treatment. JPediatr Endocrinol Metab. 2002;15:175–180. doi: 10.1515/jpem.2002.15.2.175. [DOI] [PubMed] [Google Scholar]
- Nora JJ, Nora AH, Sinha AK, Spangler RD, Lubs HA. The Ullrich-Noonan syndrome (Turner phenotype) Am J Dis Child. 1974;127:48–55. doi: 10.1001/archpedi.1974.02110200050007. [DOI] [PubMed] [Google Scholar]
- Nyström AM, Ekvall S, Berglund E, Björkqvist M, Braathen G, et al. Noonan and cardio-facio-cutaneous syndromes: two clinically and genetically overlapping disorders. J Med Genet. 2008;45:500–506. doi: 10.1136/jmg.2008.057653. [DOI] [PubMed] [Google Scholar]
- Nyström AM, Ekvall S, Allanson J, Edeby C, Elinder M, et al. Noonan syndrome and neurofibromatosis type I in a family with a novel mutation in NF1. Clin Genet. 2009;76:524–534. doi: 10.1111/j.1399-0004.2009.01233.x. [DOI] [PubMed] [Google Scholar]
- Oishi K, Zhang H, Gault WJ, Wang CJ, Tan CC, et al. Phosphatase-defective LEOPARD syndrome mutations in PTPN11 gene have gain-of-function effects during Drosophila development. Hum Mol Genet. 2009;18:193–201. doi: 10.1093/hmg/ddn336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opitz JM, Weaver DD. The neurofibromatosis-Noonan syndrome. Am J Med Genet. 1985;21:477–490. doi: 10.1002/ajmg.1320210310. [DOI] [PubMed] [Google Scholar]
- Ozturk S, Cefle K, Palanduz S, Erten NB, Karan MA, et al. A case of Noonan syndrome with pulmonary and abdominal lymphangiectasia. Int J Clin Pract. 2000;54:274–276. [PubMed] [Google Scholar]
- Padidela R, Camacho-Hübner C, Attie KM, Savage MO. Abnormal growth in Noonan syndrome: genetic and endocrine features and optimal treatment. Horm Res. 2008;70:129–136. doi: 10.1159/000145016. [DOI] [PubMed] [Google Scholar]
- Pandit B, Sarkozy A, Pennacchio LA, Carta C, Oishi K, et al. Gain-of-function RAF1 mutations cause Noonan and LEOPARD syndromes with hypertrophic cardiomyopathy. Nat Genet. 2007;39:1007–1012. doi: 10.1038/ng2073. [DOI] [PubMed] [Google Scholar]
- Pasmant E, Sabbagh A, Hanna N, Masliah-Planchon J, Jolly E, et al. SPRED1 germline mutations caused a neurofibromatosis type 1 overlapping phenotype. J Med Genet. 2009;46:425–430. doi: 10.1136/jmg.2008.065243. [DOI] [PubMed] [Google Scholar]
- Pierpont EI, Pierpont ME, Mendelsohn NJ, Roberts AE, Tworog-Dube E, Seidenberg MS. Genotype differences in cognitive functioning in Noonan syndrome. Genes Brain Behav. 2009;8:275–282. doi: 10.1111/j.1601-183X.2008.00469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plowman SJ, Williamson DJ, O'Sullivan MJ, Doig J, Ritchie AM, et al. While K-ras is essential for mouse development, expression of the K-ras 4a splice variant is dispensable. Mol Cell Biol. 2003;23:9245–9250. doi: 10.1128/MCB.23.24.9245-9250.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pritchard CA, Bolin L, Slattery R, Murray R, McMahon M. Post-natal lethality and neurological and gastrointestinal defects in mice with targeted disruption of the A-Raf protein kinase gene. Curr Biol. 1996;6:614–617. doi: 10.1016/s0960-9822(02)00548-1. [DOI] [PubMed] [Google Scholar]
- Qiu WW, Yin SS, Stucker FJ. Audiologic manifestations of Noonan syndrome. Otolaryngol Head Neck Surg. 1998;118:319–323. doi: 10.1016/S0194-59989870308-0. [DOI] [PubMed] [Google Scholar]
- Quilliam LA, Khosravi-Far R, Huff SY, Der CJ. Guanine nucleotide exchange factors: activators of the Ras superfamily of proteins. Bioessays. 1995;17:395–404. doi: 10.1002/bies.950170507. [DOI] [PubMed] [Google Scholar]
- Quilliam LA, Rebhun JF, Castro AF. A growing family of guanine nucleotide exchange factors is responsible for activation of Ras-family GTPases. Prog Nucleic Acid Res Mol Biol. 2002;71:391–444. doi: 10.1016/s0079-6603(02)71047-7. [DOI] [PubMed] [Google Scholar]
- Rajalingam K, Schreck R, Rapp UR, Albert S. Ras oncogenes and their downstream targets. Bioch Biophys Acta. 2007;1773:1177–1195. doi: 10.1016/j.bbamcr.2007.01.012. [DOI] [PubMed] [Google Scholar]
- Ranke MB, Heidemann P, Knupfer C, Enders H, Schmaltz AA, Bierich JR. Noonan syndrome: Growth and clinical manifestations in 144 cases. Eur J Pediatr. 1988;148:220–227. doi: 10.1007/BF00441408. [DOI] [PubMed] [Google Scholar]
- Razzaque MA, Nishizawa T, Komoike Y, Yagi H, Furutani M, et al. Germline gain-of-function mutations in RAF1 cause Noonan syndrome. Nat Genet. 2007;39:1013–1017. doi: 10.1038/ng2078. [DOI] [PubMed] [Google Scholar]
- Resh MD. Trafficking and signaling by fatty-acylated and prenylated proteins. Nat Chem Biol. 2006;2:584–590. doi: 10.1038/nchembio834. [DOI] [PubMed] [Google Scholar]
- Reynders CS, Pauker SP, Benacerraf BR. First trimester isolated fetal nuchal lucency: Significance and outcome. J Ultrasound Med. 1997;16:101–105. doi: 10.7863/jum.1997.16.2.101. [DOI] [PubMed] [Google Scholar]
- Reynolds JF, Neri G, Herrmann JP, Blumberg B, Coldwell JG, et al. New multiple congenital anomalies/mental retardation syndrome with cardio-facio-cutaneous involvement – the CFC syndrome. Am J Med Genet. 1986;25:413–427. doi: 10.1002/ajmg.1320250303. [DOI] [PubMed] [Google Scholar]
- Roberts A, Allanson J, Jadico SK, Kavamura MI, Noonan J, et al. The cardiofaciocutaneous syndrome. J Med Genet. 2006;43:833–842. doi: 10.1136/jmg.2006.042796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AE, Araki T, Swanson KD, Montgomery KT, Schiripo TA, et al. Germline gain-of-function mutations in SOS1 cause Noonan syndrome. Nat Genet. 2007;39:70–74. doi: 10.1038/ng1926. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Viciana P, Oses-Prieto J, Burlinqame A, Fried M, McCormick F. A phosphatase holoenzyme comprised of Shoc2/Sur8 and the catalytic subunit of PP1 functions as an M-Ras effector to modulate Raf activity. Mol Cell. 2006a;22:217–230. doi: 10.1016/j.molcel.2006.03.027. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Viciana P, Tetsu O, Tidyman WE, Estep AL, Conger BA, et al. Germline mutations in genes within the MAPK pathway cause cardio-facio-cutaneous syndrome. Science. 2006b;311:1287–1290. doi: 10.1126/science.1124642. [DOI] [PubMed] [Google Scholar]
- Romano AA, Dana K, Bakker B, Davis DA, Hunold JJ, et al. Growth response, near-adult height, and patterns of growth and puberty in patients with Noonan syndrome treated with growth hormone. J Clin Endocrinol Metab. 2009;94:2338–2344. doi: 10.1210/jc.2008-2094. [DOI] [PubMed] [Google Scholar]
- Sarkozy A, Obregon MG, Conti E, Esposito G, Mingarelli R, et al. A novel PTPN11 gene mutation bridges Noonan syndrome, multiple lentigines/LEOPARD syndrome and Noonan-like/multiple giant cell lesion syndrome. Eur J Hum Genet. 2004;12:1069–1072. doi: 10.1038/sj.ejhg.5201290. [DOI] [PubMed] [Google Scholar]
- Sarkozy A, Carta C, Moretti S, Zampino G, Digilio MC, et al. Germline BRAF mutations in Noonan, LEOPARD, and cardiofaciocutaneous syndromes: molecular diversity and associated phenotypic spectrum. Hum Mutat. 2009a;30:695–702. doi: 10.1002/humu.20955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkozy A, Digilio MC, Zampino G, Dallapiccola D, Tartaglia M, Gelb BD. LEOPARD syndrome: clinical aspects and molecular pathogenesis; in Zenker M (ed): Noonan Syndrome and Related Disorders. Monogr Hum Genet Karger, Basel. 2009b;17:55–65. [Google Scholar]
- Schreck R, Rapp UR. Raf kinases: oncogenesis and drug discovery. Int J Cancer. 2006;119:2261–2271. doi: 10.1002/ijc.22144. [DOI] [PubMed] [Google Scholar]
- Schubbert S, Lieuw K, Rowe SL, Lee CM, Li X, et al. Functional analysis of leukemia-associated PTPN11 mutations in primary hematopoietic cells. Blood. 2005;106:311–317. doi: 10.1182/blood-2004-11-4207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubbert S, Zenker M, Rowe SL, Böll S, Klein C, et al. Germline KRAS mutations cause Noonan syndrome. Nat Genet. 2006;38:331–336. doi: 10.1038/ng1748. [DOI] [PubMed] [Google Scholar]
- Schubbert S, Bollag G, Lyubynska N, Nguyen H, Kratz CP, et al. Biochemical and functional characterization of germ line KRAS mutations. Mol Cell Biol. 2007a;27:7765–7770. doi: 10.1128/MCB.00965-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubbert S, Shannon K, Bollag G. Hyperactive Ras in developmental disorders and cancer. Nat Rev Cancer. 2007b;7:295–308. doi: 10.1038/nrc2109. [DOI] [PubMed] [Google Scholar]
- Schulz AL, Albrecht B, Arici C, van der Burgt I, Buske A, et al. Mutation and phenotypic spectrum in patients with cardio-facio-cutaneous and Costello syndrome. Clin Genet. 2008;73:62–70. doi: 10.1111/j.1399-0004.2007.00931.x. [DOI] [PubMed] [Google Scholar]
- Seeburg PH, Colby WW, Capon DJ, Goeddel DV, Levinson AD. Biological properties of human c-Ha-ras1 genes mutated at codon 12. Nature. 1984;312:71–75. doi: 10.1038/312071a0. [DOI] [PubMed] [Google Scholar]
- Selfors LM, Schutzman JL, Borland CZ, Stern MJ. Soc-2 encodes a leucine-rich repeat protein implicated in fibroblast growth factor receptor signaling. Proc Natl Acad Sci USA. 1998;95:6903–6908. doi: 10.1073/pnas.95.12.6903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah N, Rodriguez M, Louis DS, Lindley K, Milla PJ. Feeding difficulties and foregut dysmotility in Noonan's syndrome. Arch Dis Child. 1999;81:28–31. doi: 10.1136/adc.81.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharland M, Burch M, McKenna WM, Patton MA. A clinical study of Noonan syndrome. Arch Dis Child. 1992a;67:178–183. doi: 10.1136/adc.67.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharland M, Patton MA, Talbot S, Chitolie A, Bevan DH. Coagulation-factor deficiencies and abnormal bleeding in Noonan's syndrome. Lancet. 1992b;339:19–21. doi: 10.1016/0140-6736(92)90141-o. [DOI] [PubMed] [Google Scholar]
- Shchelochkov OA, Patel A, Weissenberger GM, Chinault AC, Wiszniewska J, et al. Duplication of chromosome band 12q24.11q24.23 results in apparent Noonan syndrome. Am J Med Genet A. 2008;146A:1042–1048. doi: 10.1002/ajmg.a.32215. [DOI] [PubMed] [Google Scholar]
- Sieburth DS, Sun Q, Han M. SUR-8, a conserved Ras-binding protein with leucine-rich repeats, positively regulates Ras-mediated signaling in C. elegans. Cel1. 1998;94:119–130. doi: 10.1016/s0092-8674(00)81227-1. [DOI] [PubMed] [Google Scholar]
- Silvius JR. Mechanisms of Ras protein targeting in mammalian cells. J Membr Biol. 2002;190:83–92. doi: 10.1007/s00232-002-1026-4. [DOI] [PubMed] [Google Scholar]
- Singer ST, Hurst D, Addiego JE., Jr Bleeding disorders in Noonan syndrome: Three case reports and review of the literature. J Pediatr Hematol Oncol. 1997;19:130–134. doi: 10.1097/00043426-199703000-00006. [DOI] [PubMed] [Google Scholar]
- Somerville J, Bonham-Carter RE. The heart in lentiginosis. Br Heart J. 1972;34:58–66. doi: 10.1136/hrt.34.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sondermann H, Soisson SM, Boykevisch S, Yang SS, Bar-Sagi D, Kuriyan J. Structural analysis of autoinhibition in the Ras activator Son of sevenless. Cell. 2004;119:393–405. doi: 10.1016/j.cell.2004.10.005. [DOI] [PubMed] [Google Scholar]
- Sondermann H, Nagar B, Bar-Sagi D, Kuriyan J. Computational docking and solution X-ray scattering predict a membrane-interacting role for the histone domain of the Ras activator Son of sevenless. Proc Natl Acad Sci USA. 2005;102:16632–16637. doi: 10.1073/pnas.0508315102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spurlock G, Bennett E, Chuzhanova N, Thomas N, Jim HP, et al. SPRED1 mutations (Legius syndrome): another clinically useful genotype for dissecting the neurofibromatosis type 1 phenotype. J Med Genet. 2009;46:431–437. doi: 10.1136/jmg.2008.065474. [DOI] [PubMed] [Google Scholar]
- Swanson KD, Winter JM, Reis M, Bentires-Alj M, Greulich H, et al. SOS1 mutations are rare in human malignancies: implications for Noonan syndrome patients. Genes Chromosomes Cancer. 2008;47:253–259. doi: 10.1002/gcc.20527. [DOI] [PubMed] [Google Scholar]
- Tanaka K, Sato A, Naito T, Kuramochi K, Itabashi H, Takemura Y. Noonan syndrome presenting growth hormone neurosecretory dysfunction. Intern Med. 1992;31:908–911. doi: 10.2169/internalmedicine.31.908. [DOI] [PubMed] [Google Scholar]
- Tartaglia M, Mehler EL, Goldberg R, Zampino G, Brunner HG, et al. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat Genet. 2001;29:465–468. doi: 10.1038/ng772. [DOI] [PubMed] [Google Scholar]
- Tartaglia M, Kalidas K, Shaw A, Song X, Musat DL, et al. PTPN11 mutations in Noonan syndrome: molecular spectrum, genotype-phenotype correlation, and phenotypic heterogeneity. Am J Hum Genet. 2002;70:1555–1563. doi: 10.1086/340847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tartaglia M, Niemeyer CM, Fragale A, Song X, Buechner J, et al. Somatic mutations in PTPN11 in juvenile myelomonocytic leukemia, myelodysplastic syndromes and acute myeloid leukemia. Nat Genet. 2003;34:148–150. doi: 10.1038/ng1156. [DOI] [PubMed] [Google Scholar]
- Tartaglia M, Martinelli S, Cazzaniga G, Cordeddu V, Iavarone I, et al. Genetic evidence for lineage- and differentiation stage-related contribution of somatic PTPN11 mutations to leukemogenesis in childhood acute leukemia. Blood. 2004a;104:307–313. doi: 10.1182/blood-2003-11-3876. [DOI] [PubMed] [Google Scholar]
- Tartaglia M, Niemeyer CM, Shannon KM, Loh ML. SHP-2 and myeloid malignancies. Curr Opin Hematol. 2004b;11:44–50. doi: 10.1097/00062752-200401000-00007. [DOI] [PubMed] [Google Scholar]
- Tartaglia M, Martinelli S, Iavarone I, Cazzaniga G, Spinelli M, et al. Somatic PTPN11 mutations in childhood acute myeloid leukaemia. Br J Haematol. 2005;129:333–339. doi: 10.1111/j.1365-2141.2005.05457.x. [DOI] [PubMed] [Google Scholar]
- Tartaglia M, Martinelli S, Stella L, Bocchinfuso G, Flex E, et al. Diversity and functional consequences of germline and somatic PTPN11 mutations in human disease. Am J Hum Genet. 2006;78:279–290. doi: 10.1086/499925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tartaglia M, Pennacchio LA, Zhao C, Yadav KK, Fodale V, et al. Gain-of-function SOS1 mutations cause a distinctive form of Noonan syndrome. Nat Genet. 2007;39:75–79. doi: 10.1038/ng1939. [DOI] [PubMed] [Google Scholar]
- Thiel C, Wilken M, Zenker M, Sticht H, Fahsold R, et al. Independent NF1 and PTPN11 mutations in a family with neurofibromatosis-Noonan syndrome. Am J Med Genet A. 2009;149A:1263–1267. doi: 10.1002/ajmg.a.32837. [DOI] [PubMed] [Google Scholar]
- van der Burgt I. Noonan syndrome. Orphanet J Rare Dis. 2007;2:4. doi: 10.1186/1750-1172-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Burgt I, Brunner H. Genetic heterogeneity in Noonan syndrome: evidence for an autosomal recessive form. Am J Med Genet. 2000;94:46–51. doi: 10.1002/1096-8628(20000904)94:1<46::aid-ajmg10>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- van der Burgt I, Berends E, Lommen E, van Beersum S, Hamel B, Mariman E. Clinical and molecular studies in a large Dutch family with Noonan syndrome. Am J Med Genet. 1994;53:187–191. doi: 10.1002/ajmg.1320530213. [DOI] [PubMed] [Google Scholar]
- van der Burgt I, Kupsky W, Stassou S, Nadroo A, Barroso C, et al. Myopathy caused by HRAS germline mutations: implications for disturbed myogenic differentiation in the presence of constitutive HRas activation. J Med Genet. 2007;44:459–462. doi: 10.1136/jmg.2007.049270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhoeven W, Wingbermühle E, Egger J, Van der Burgt I, Tuinier S. Noonan syndrome: psychological and psychiatric aspects. Am J Med Genet A. 2008;146A:191–196. doi: 10.1002/ajmg.a.32115. [DOI] [PubMed] [Google Scholar]
- Voron DA, Hatfield HH, Kalkhoff MD. Multiple lentigines syndrome: case report and review of the literature. Am J Med. 1976;60:447–456. doi: 10.1016/0002-9343(76)90764-6. [DOI] [PubMed] [Google Scholar]
- Walter M, Clark SG, Levinson AD. The oncogenic activation of human p21ras by a novel mechanism. Science. 1986;233:649–652. doi: 10.1126/science.3487832. [DOI] [PubMed] [Google Scholar]
- Wang DZ, Hammond VE, Abud HE, Bertoncello I, McAvoy JW, Bowtell DD. Mutation in Sos1 dominantly enhances a weak allele of the EGFR, demonstrating a requirement for Sos1 in EGFR signaling and development. Genes Dev. 1997;11:309–320. doi: 10.1101/gad.11.3.309. [DOI] [PubMed] [Google Scholar]
- Wellbrock C, Karasarides M, Marais R. The RAF proteins take centre stage. Nat Rev Mol Cell Biol. 2004;5:875–885. doi: 10.1038/nrm1498. [DOI] [PubMed] [Google Scholar]
- Wennerberg K, Rossman KL, Der CJ. The Ras superfamily at a glance. J Cell Sci. 2005;118:843–846. doi: 10.1242/jcs.01660. [DOI] [PubMed] [Google Scholar]
- Wieczorek D, Majewski F, Gillessen-Kaesbach G. Cardio-facio-cutaneous (CFC) syndrome – a distinct entity? Report of three patients demonstrating the diagnostic difficulties in delineation of CFC syndrome. Clin Genet. 1997;52:37–46. doi: 10.1111/j.1399-0004.1997.tb02512.x. [DOI] [PubMed] [Google Scholar]
- Witt DR, Keena BA, Hall JG, Allanson JE. Growth curves for height in Noonan syndrome. Clin Genet. 1986;30:150–153. doi: 10.1111/j.1399-0004.1986.tb00587.x. [DOI] [PubMed] [Google Scholar]
- Wojnowski L, Zimmer AM, Beck TW, Hahn H, Bernal R, et al. Endothelial apoptosis in Braf-deficient mice. Nat Genet. 1997;16:293–297. doi: 10.1038/ng0797-293. [DOI] [PubMed] [Google Scholar]
- Xu D, Qu CK. Protein tyrosine phosphatases in the JAK/STAT pathway. Front Biosci. 2008;13:4925–4932. doi: 10.2741/3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R, Yu Y, Zheng S, Zhao X, Dong Q, et al. Overexpression of Shp2 tyrosine phosphatase is implicated in leukemogenesis in adult human leukemia. Blood. 2005;106:3142–3149. doi: 10.1182/blood-2004-10-4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zampino G, Mastroiacovo P, Ricci R, Zollino M, Segni G, et al. Costello syndrome: further clinical delineation, natural history, genetic definition, and nosology. Am J Med Genet. 1993;47:176–183. doi: 10.1002/ajmg.1320470210. [DOI] [PubMed] [Google Scholar]
- Zampino G, Pantaleoni F, Carta C, Cobellis G, Vasta I, et al. Diversity, parental germline origin, and phenotypic spectrum of de novo HRAS missense changes in Costello syndrome. Hum Mutat. 2007;28:265–272. doi: 10.1002/humu.20431. [DOI] [PubMed] [Google Scholar]
- Zenker M, Buheitel G, Rauch R, Koenig R, Bosse K, et al. Genotype-phenotype correlations in Noonan syndrome. J Pediatr. 2004;144:368–374. doi: 10.1016/j.jpeds.2003.11.032. [DOI] [PubMed] [Google Scholar]
- Zenker M, Horn D, Wieczorek D, Allanson J, Pauli S, et al. SOS1 is the second most common Noonan gene but plays no major role in cardio-facio-cutaneous syndrome. J Med Genet. 2007a;44:651–656. doi: 10.1136/jmg.2007.051276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenker M, Lehmann K, Schulz AL, Barth H, Hansmann D, et al. Expansion of the genotypic and phenotypic spectrum in patients with KRAS germline mutations. J Med Genet. 2007b;44:131–135. doi: 10.1136/jmg.2006.046300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng CF, Guan KL. Properties of MEKs: the kinases that phosphorylate and activate the extracellular signal-regulated kinases. J Biol Chem. 1993;268:23933–23939. [PubMed] [Google Scholar]