Abstract
This article reports findings from a randomized controlled trial of massage and guided meditation with patients at the end of life. Using data from 167 randomized patients, the authors consider patient outcomes through 10 weeks post-enrollment, as well as next-of-kin ratings of the quality of the final week of life for 106 patients who died during study participation. Multiple regression models demonstrated no significant treatment effects of either massage or guided meditation, delivered up to twice a week, when compared with outcomes of an active control group that received visits from hospice-trained volunteers on a schedule similar to that of the active treatment arms. The authors discuss the implications of their findings for integration of these complementary and alternative medicine therapies into standard hospice care.
Introduction
Since the mid-1990s, improving the quality of care at the end of life has become a national priority in the United States (US). Influential reports from the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment,1 the Institute of Medicine,2 and the Robert Wood Johnson Foundation3,4 have all called for improvements in end-of-life care, including use of a broad range of palliative therapies to meet the special physical, psychosocial, and spiritual needs of terminally ill patients.3
Concurrent with the rising interest in improving the quality of end-of-life care, there has been increased interest in, and receptivity to, complementary and alternative medicine (CAM). CAM use in the US increased during the latter half of the 20th century and has remained stable during the initial years of the current century.5-7 Researchers have estimated that half of the baby boom generation had used some form of CAM by age 33 years, suggesting widespread acceptance of CAM in the cohort now on the threshold of the end-of-life period.5 Because several CAM techniques had shown promise as palliative therapies by early in this century, the integration of CAM into end-of-life care became a topic of interest.8-10
Few scientifically rigorous studies have examined the impact of CAM on dying patients’ outcomes. In a 2006 review of randomized controlled trials of massage and meditation among patients with life-threatening illness,11 we found only four studies12-15 that specifically tested these therapies in hospice or palliative care environments. All of the studies based their findings on small samples (n=28 to 56) and tested interventions delivered over a very brief time period (2 to 4 weeks). In its final report,16 the 2004 State of the Science Conference on End-of-Life Care, noting the dramatic increase in the number of older adults facing the need for end-of-life care, stated that the current design of the Medicare hospice benefit restricts the availability of interventions that might help many persons at end of life and indicated the need for research to validate untested interventions. In a statement specifically addressing CAM therapies, the report indicated that research to date investigating potential benefits of CAM in this population had suffered from “insufficient numbers of studies, small samples, and weak study designs.”16
Individuals from a variety of perspectives have emphasized the importance of being free from pain, experiencing human touch, and maintaining good overall quality of life as important quality-of-care indicators for patients approaching death.17-19 In the current article we report results from a recently completed randomized controlled trial with a sample of patients at the end of life, investigating the effects of two CAM therapies (massage and guided meditation) on participants’ overall quality of life and pain distress. We then discuss the implications of our findings for integration of these therapies into standard care of terminally ill patients, given the limited pool of financial resources available for end-of-life care.
Methods
Data for this article came from a randomized controlled trial that tested the effects of two active interventions (therapeutic massage and guided meditation) on the quality of patients’ end-of-life experience, when compared to the effects of an attention control condition (friendly visits) that served as a proxy for a service that has been implemented as part of standard care in hospice (the hospice volunteer). The University of Washington administered the study, recruited participants, and collected research data. Bastyr University, a private institution specializing in science-based natural medicine, developed the clinical protocols, oversaw all clinical service provision, and collected clinical data.
Participants
Patient participants included hospice or palliative care patients living in the Seattle, Washington, metropolitan area, who spoke English, were at least 18 years old, were mentally capable of providing reliable responses during a 60-90 minute baseline interview, were expected to survive for at least 3 weeks after enrollment, and agreed to accept assignment to any of the three treatment conditions. Persons who met all other study requirements, but who were not receiving hospice or palliative care, could also qualify, provided they had been diagnosed with AIDS or stage IV cancer.
When the study was initially designed, we had no quality-of-life data from a population of dying persons on which to base power calculations. However, observed correlations between depression and quality of life20 suggested powering the study on depression data from older adults nearing the end of life. The resulting analyses led to a recruitment goal of 100 persons per treatment group as adequate for detecting clinically meaningful differences in depression and, by extension, quality of life.
Patient recruitment efforts centered on Seattle-area hospice organizations, cancer and AIDS clinics, physicians’ offices, and cancer support groups. Members of the research group met weekly with hospice care teams to monitor their case loads for patients appropriate for study participation. Each patient who enrolled in the study nominated a study partner who could provide collateral information at baseline and proxy information at a follow-up interview that covered the final week of the patient’s life. Although a family member or close friend typically fulfilled the study partner role, socially isolated patients could nominate a member of their healthcare team for this purpose.
Baseline Data Collection
Study interviewers conducted face-to-face structured, computer-assisted baseline interviews with the patient and study partner at locations of the participants’ choice. Most patient baseline interviews occurred in patients’ places of residence, with a few completed in medical care settings where patients were receiving chemotherapy or other treatments. Study partner interviews occurred in the residence of the patient or study partner, at work sites, or in quiet public settings such as coffee houses. Patients provided demographic data, information about past use of CAM services, prospective ratings of the services offered in the study’s three treatment arms, and their perceptions about symptom distress and quality of life during the 7 days before the interview. Study partners answered parallel questions about the patient’s condition during the previous 7 days, and both patients and study partners provided information about priorities for the patient’s final week of life. Study partner and patient interviews did not always occur on the same day, and the ordering of the two was at the discretion of the participants. We abandoned attempts to complete baseline interviews with study partners if they had not occurred within 1 week after the patient’s first treatment visit; when this occurred, there was no penalty to the patient.
We completed most baseline interviews in a single session. However, when patients needed to interrupt the baseline session (e.g., because of fatigue or other symptoms), we scheduled additional sessions to continue and complete the interview. Random assignment to one of the three treatment groups occurred immediately after completion of the patient baseline interview.
Clinical Protocol
The study established strict eligibility requirements for clinical service providers. Meditation instructors were Washington-State-licensed naturopathic physicians, and massage providers were Washington-state-licensed massage therapists. We required both provider categories to have been licensed for at least 2 years and to have had at least 1 year’s experience working with seriously ill patients. Friendly visitors had completed volunteer training courses from accredited hospice programs and had served as hospice volunteers for at least 1 year before joining the study. All providers underwent 7 hours of study-related training, participated in monthly group telephone consultation and supervision, and received compensation from the study for each patient visit.
Patients determined the location of clinical sessions. Most occurred in the patient’s residence, but could be moved to hospitals or other healthcare settings as need arose. The protocol for treatment visits in all three study arms stipulated that treatment would last for 35 minutes, but that the visit could include up to 10 additional minutes for introductions, information exchange, and paperwork. Massage therapists were to provide a light back-and- neck massage in a position of the patient’s choosing, followed by effleurage and goodbye holding. Depending on need, they could spend some time focusing on areas of particular tension or stress. Meditation providers were to lead the patient in progressive muscle relaxation, mindfulness-based meditation, and guided imagery/visualization. We have included the script and instructions for the meditation sessions as an appendix to this article. Friendly visitors could spend the allotted time with the patient (e.g., reading to them, engaging in conversation, writing letters, doing light chores, running errands, or just spending time with them); alternatively, they could provide respite or other assistance to caregivers without directly interacting with the patient. Although the protocol specified the default treatment routine for each treatment arm, providers were allowed to tailor the intervention to meet specific needs and requests of patients.
The Bastyr University study staff made initial assignments of treatment providers to patients, guided by scheduling requirements and geographic considerations. However, if patients were unhappy with the provider assigned or specific features of the treatment provided, they could request modifications. Follow-up interviews with UW staff included a routine way for making such requests that prevented patients from having to voice discontent directly to treatment providers. The protocol did not allow for changes in treatment group assignment, nor did it permit withdrawal from the study and reentry with the possibility of random assignment to a different treatment condition.
After randomization, patients could receive up to two treatment visits per week until death (or the end of the study), although they could elect less frequent visits if they so desired. Participants could drop out of the study permanently at any point or could take extended vacations from treatment as their needs dictated. They were free to take advantage of any treatments offered outside the study, even if that treatment matched one offered in an arm of the study to which they had not been assigned.
Follow-up Data Collection
After every two treatment visits, patients completed a short follow-up interview with UW staff, either in person or by telephone, according to their preference. Each series of two treatment visits and a follow-up interview constituted a “treatment block,” and – unless the patient had been flagged as no longer able to provide follow-up data – a new treatment block could not begin until the patient completed the interview for the preceding block. The follow-up interview could not occur until the next day after the second treatment visit for the block, but could be delayed for several days, provided that it occurred prior to the first treatment of the succeeding block. At each interview, the patient indicated whether changes were needed in their treatment schedule, provider, or details of treatment; whether they had received comfort care services outside the study since their last interview; and their quality of life and symptom distress during the 7-day period prior to the interview.
In addition to patients’ regular follow-up interviews, study partners of patients who died during participation provided follow-up data about the final week of the patient’s life. These interviews occurred within 6 months after the patient’s death.
Measures and Analysis
Outcomes reported in this article were based on participants’ ratings of quality of life (ranging from 0 [no quality of life] to 10 [perfect quality of life]) and pain distress (0 [no pain] or 1 [pain with no accompanying distress] through 5 [pain with much accompanying distress]). Reported quality of life was a single-item rating, similar to one used to validate the Quality of Dying and Death instrument.21 Pain distress was drawn from the Memorial Symptom Assessment scale.22 We used four measures derived from these ratings: (a) the mean value of patients’ quality-of-life ratings over the baseline interview and all follow-up interviews within 10 weeks after baseline; (b) the expected number of weeks of good-quality life over the 10-week period, where ratings of 7-10 constituted good-quality life; (c) the expected number of weeks with low pain distress over the 10-week period, where ratings of 1.5 or less constituted low pain distress; and (d) study partners’ reports of the quality of life experienced by 106 deceased patients during their final 7 days before death. To compute the expected weeks of good-quality life and low pain distress, we transformed the quality-of-life and pain-distress measures to account for persons who died, and also imputed data for weeks when patients were not interviewed, as described elsewhere.23 The transformed variable represented the proportion of the sample expected to report good quality of life (or low pain distress) at an interview occurring the following week. For example, a quality-of-life rating of 10 was transformed to 0.93 because persons with that value had a 93% chance of reporting quality of life at 7 or higher the following week; a quality-of-life rating of 1 was transformed to 0.03; and a person who was dead at the time of a planned measurement received 0.00 (i.e., no probability of having good quality of life one week later). For reasons of simplicity we have dropped the word “expected” in summarizing our findings. Quality-of-life ratings that were missing for reasons other than death were imputed from a regression of quality-of-life ratings on time from death (or last available measure, if the person survived). Sensitivity analyses, reported elsewhere,23 indicated that the findings were not sensitive to the type of imputation. We calculated weeks of good-quality life and weeks with low pain distress from the transformed, imputed measures. We based all analyses on intention to treat.
The primary predictors of interest were two dichotomous variables representing the patient’s assignment to either the meditation or massage treatment group. The reference group consisted of patients assigned to friendly visits.
In addition to the outcomes and predictors of interest, we used several variables provided by patients at the baseline interview to describe the sample and as covariates in regression models testing intervention efficacy. Among these were six dichotomous measures: gender, white race (including mixed-white), receipt of a 4-year college degree, average income greater than $2,000 per month during the 3 years prior to study enrollment, referral to the study by a hospice program, and primary diagnosis of cancer. We also used four ordinal variables from the baseline interview: patient age, perceived overall health status (0 = worst health imaginable … 10= as near perfect health as imaginable), and the baseline values for quality of life and pain distress (the latter two variables also contributing to the outcomes of interest). Finally, to provide a description of the amount of contact between study personnel and patients during the 10-week period following baseline interview, we computed for each patient the number of treatment visits and the number of follow-up data-collection interviews.
We used least squares linear regression to test for differences between the randomization groups on each of the four outcomes (the mean value of the patient’s quality-of-life ratings, weeks of good-quality life, weeks with low pain distress, and study partners’ reports of the quality of deceased patients’ final week of life). Each regression model included adjustment for gender, white race (yes/no), college graduate (yes/no), cancer diagnosis (yes/no), baseline health rating (0-10), baseline quality-of-life rating (0-10), and baseline pain distress rating (0-5). We also adjusted for patient age, log age, gender by age interaction, and gender by log age interaction, which permitted the outcome to vary non-linearly with age and differently for men and women.
In addition to analysis of the outcomes based on data provided by patients and study partners at follow-up interviews, we used data from the full sample of randomized patients to test for differences in survival at 10 weeks (Pearson χ2) and over the entire course of the study (Kaplan-Meier survival analysis with the Breslow generalized Wilcoxon test). We also used the full sample to compare the treatment groups with regard to the number of contacts patients had with study personnel (Kruskal-Wallis χ2).
Results
We randomized 167 patients to the three treatment groups – 56 to each of the active interventions and 55 to the attention control group (Table 1). Average age at enrollment was 69 years (ranging from 34 to 98 years). A majority of the participants were female, white race, cancer patients, and referred to the study from hospice programs. About 60% had monthly household incomes in excess of $2,000. Almost 42% had graduated from college. Mean baseline ratings of health (5.60, on a 0-10 scale with 10 indicating perfect health), quality of life (6.08, on a 0-10 scale with 10 indicating perfect quality of life), and pain distress (2.46, on a 0-5 scale with 5 indicating maximum distress) all tipped slightly toward the positive end of each scale (Table 1). Although there were substantial differences between treatment groups on gender and primary diagnosis, analysis of variance showed no significant differences between treatment groups on any of the baseline measures.
Table 1. Sample Description, 167 Patients Randomized to Treatment.
| Meditation | Massage | Friendly Visit | Total | |
|---|---|---|---|---|
| Number of Patients | 56 | 56 | 55 | 167 |
| Mean (SD) Agea | 72.09 (15.36) | 68.09 (15.96) | 69.46 (17.67) | 69.88 (16.34) |
| Number (%) Female | 36 (64) | 39 (70) | 31 (56) | 106 (63) |
| Number (%) Whiteb | 51 (91) | 54 (96) | 51 (93) | 156 (93) |
| Number (%) College Graduate | 22 (39) | 21 (38) | 27 (49) | 70 (42) |
| Number (%) with Monthly Household Income > $2,000c | 29 (60) | 30 (58) | 32 (62) | 91 (60) |
| Number (%) Referred by Hospice | 45 (80) | 43 (77) | 40 (73) | 128 (77) |
| Number (%) with Cancer | 33 (59) | 41 (73) | 41 (75) | 115 (69) |
| Mean (SD) Health Rating, Baselined | 5.87 (2.20) | 5.51 (2.55) | 5.42 (1.96) | 5.60 (2.24) |
| Mean (SD) Quality of Life, Baselinee | 6.04 (2.43) | 6.38 (2.53) | 5.84 (2.48) | 6.08 (2.48) |
| Mean (SD) Pain Distress, Baselinef | 2.38 (1.81) | 2.50 (1.66) | 2.51 (1.55) | 2.46 (1.67) |
| Number (%) Alive at End of Study | 9 (16) | 13 (23) | 8 (15) | 30 (18) |
| Number (%) Alive 10 Weeks after Baseline | 38 (68) | 46 (82) | 36 (65) | 120 (72) |
| Median (IQR) # Treatment Visits per Patient | 10.00 (11.00) | 13.00 (10.00) | 9.00 (11.00) | 11.00 (11.00) |
| Median (IQR) # Follow-up Data Collection Visits per Patient | 4.50 (6.00) | 6.00 (5.00) | 4.00 (6.00) | 5.00 (5.00) |
| Median Estimated Survival (days)g | 149 | 165 | 127 | 149 |
Age at time of baseline interview.
Patients were counted as white if they endorsed white race, even if they also endorsed another race or indicated Hispanic ethnicity.
Based on 152 responses (48 meditation, 52 massage, 52 friendly visit)
Based on 0-10 self-report rating (0 = worst imaginable and still be alive … 10 = as near perfect as imaginable); 165 responses (55 per randomization group).
Based on 0-10 self-report rating (0 = no quality of life … 10 = perfect quality of life)
Based on 0-5 self-report rating (0 = no pain, 1=had pain, but it didn’t cause distress … 5 = had pain, and it caused very much distress)
Estimated with Kaplan-Meier curve.
Survival Rates
Almost 72% of the patients lived for 10 weeks or more after enrollment, and about 18% lived until the end of the study. The estimated median survival time for all patients was 149 days after study enrollment. Differences between treatment groups were not statistically significant on any of the survival-related outcomes: 66-day survival (p = 0.106), survival to end of study (p = 0.445), and median survival time after enrollment (p = 0.637).
Amount of Contact between Patients and Study Personnel
During the 10 weeks following baseline interview, patients had a median of 11 treatment visits and 5 data collection interviews (Table 1). Patients assigned to the massage group had significantly more contact with study personnel during this period than did patients assigned to the other groups (p = 0.021 for treatment visits; p = 0.019 for interviews).
Much of the between-group difference resulted from dropout immediately after random assignment among patients assigned to meditation and friendly visits (four dropouts from each group, compared with none from the massage group). When we excluded these eight patients, between-group differences in number of study contacts became non-significant. Even with the exclusions, however, massage patients had somewhat more contact with the study during the first 10 weeks after enrollment (median = 13 treatment visits) than did those in the meditation (median = 10.5) and friendly visit (median = 10) groups, owing to fewer early deaths (10 in the massage group, compared with 17 in the meditation and 16 in the friendly visit group) and fewer dropouts after starting treatment (3 each for the meditation and friendly visit groups, compared with 1 for the massage group). Average elapsed times between visits for patients who received two or more treatments during the 69-day period were similar for the three groups (mean = 6.2 days for the massage and meditation groups, and 7.3 days for friendly visit patients).
Primary Outcomes
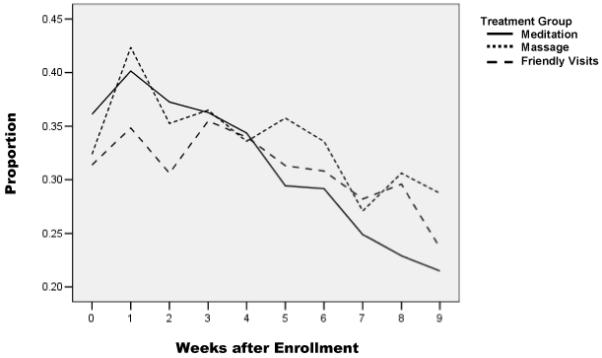
In the sample as a whole, quality of life declined over the 10-week analysis period, as patients died and fewer of those who were still alive reported good-quality life (Figure 1). Each of the treatment groups, considered individually, experienced overall decline in the proportion with good-quality life (Figure 2) and low pain distress (Figure 3), although each of the samples had periods with stabilization or even slight improvement in these outcomes before resuming the decline. The massage group experienced generally higher quality of life over the 10-week period, owing primarily to their slightly higher quality of life at enrollment.
Figure 1. Reported Quality of Life, Baseline Week and First 9 Follow-up Weeks.
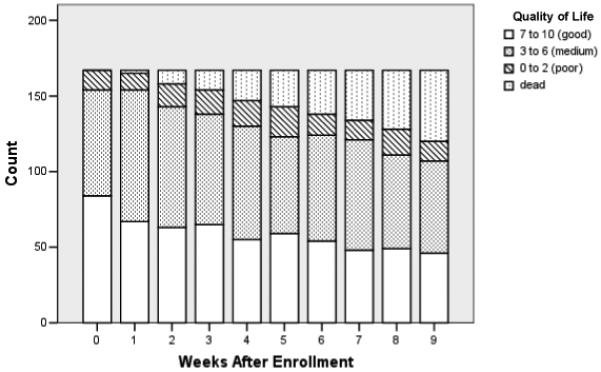
Figure 2. Proportion with Expected Good-Quality Life over Time.
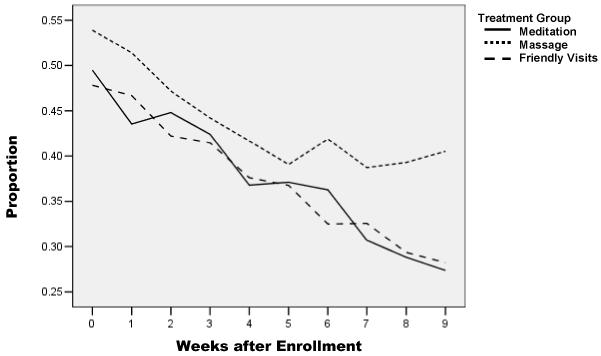
Figure 3. Proportion with Expected Low Pain Distress over Time.
Linear regression models with adjustment for covariates showed no significant effects of either massage or meditation, when compared with friendly visits (Table 2). Histograms of regression residuals showed reasonably normal distributions, each having a central node and no noticeable heavy or light tails. Parameter estimates for each of the two active treatments were non-significant for patients’ average quality-of-life ratings over time, weeks of good quality life, and weeks with low pain distress. Study partner reports of the quality of patients’ final 7 days of life also showed no association with treatment group.
Table 2. Study Outcomes.
| Unadjusted Sample Means (s.e.) |
Adjusted Differences from Friendly Visita |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Meditation | Massage | Friendly Visit | Meditation | Massage | |||||
| Baseline through Follow-up Week #9 | Mean | s.e. | p b | Mean | s.e. | p b | |||
| Patient’s Mean Actual Quality-of-Life Ratingc | 5.649 (0.284) | 5.977 (0.276) | 5.772 (0.298) | −0.269 | 0.238 | .261 | −0.146 | 0.239 | .542 |
| Patient’s Expected Weeks of Good-Quality Lifed | 3.389 (0.296) | 3.907 (0.321) | 3.372 (0.329) | −0.135 | 0.348 | .698 | +0.120 | 0.349 | .731 |
| Patient’s Expected Weeks with Low Pain Distresse | 2.832 (0.292) | 3.053 (0.277) | 2.823 (0.308) | −0.036 | 0.316 | .910 | +0.179 | 0.317 | .573 |
| Quality of Last 7 Days of Lifef | 5.240 (0.585) | 5.690 (0.545) | 5.050 (0.460) | +0.515 | 0.757 | .499 | +0.546 | 0.739 | .462 |
We adjusted regression models for gender, age, ln(age), gender*age interaction, gender* ln(age) interaction, cancer (yes/no), baseline health rating, baseline quality-of-life rating, baseline pain rating, white race, college graduate. (For two patients who were missing a value for the baseline health rating, we estimated the value from a regression equation in which baseline health rating was regressed on age, gender, cancer, baseline quality-of-life rating, and baseline pain rating.)
Statistical significance of the treatment group assignment.
The mean value of the actual quality-of-life ratings the patient provided within 65 days of baseline (0 = no quality of life … 10 = perfect quality of life).
We considered quality-of-life ratings between 7 and 10 to reflect good-quality life.
We considered pain-distress ratings <1.5 to reflect low pain distress.
Based on the 0-10 quality-of-life ratings provided by 106 study partners interviewed after patients’ deaths (0 = no quality of life, 10 = perfect quality of life).
Discussion
Several reports from the US healthcare community have called for improvements in the care of the dying, and private citizens frequently mention good quality of life and freedom from pain as goals for the end-of-life period. With rising acceptance of CAM therapies in the American population and some evidence from pilot studies that these therapies hold promise for palliation of seriously ill patients, interest has grown in their possible application to end-of-life care.
Our study focused on massage and guided meditation, two CAM therapies having potential for relief of pain, depression, anxiety, and other symptoms of terminal illness, without the toxicity and negative side effects often produced by medications for symptom amelioration at end of life.24,25 Trained and experienced professionals delivered the massage and meditation interventions to patients on a schedule of the patient’s choosing and at a rate of up to two sessions per week. Results for the first 10 weeks after enrollment showed no significant massage or meditation effect on patients’ actual quality-of-life ratings, or on weeks of good quality life or low pain distress, when compared with outcomes for patients receiving friendly visits from persons trained as hospice volunteers. Nor were there significant differences between the three treatment groups in the quality of patients’ final week of life, as measured by ratings provided by study partners of deceased patients. Receiving attention from persons trained to provide psychosocial support to patients and their families at the end of life, a service that hospices offer as part of standard care, appeared to convey benefit equal to that received from massage or guided meditation, when benefit was evaluated with measures derived from ratings of overall quality of life and pain distress.
This study makes important contributions to the science of end-of-life care. The 2004 State of the Science Conference on End-of-Life Care indicated the need for research to validate (or invalidate) untested interventions and suggested in particular that studies investigating the use of CAM with terminally ill patients had been too few, too small, and insufficiently rigorous from a design perspective. Our study adds to the very small group of published randomized controlled trials of these two CAM interventions with patients at end of life; its sample of 167 randomized patients is a substantial increase over sample sizes used in the previous studies; and its strict clinical and research protocols and use of highly-trained clinicians provides scientific rigor. Our finding that neither of these treatments produced significantly better results than visits by trained hospice volunteers will be disappointing to persons advocating integration of CAM therapies into standard care in hospice and palliative care programs. However, it is important that therapies show sufficient positive impact to justify investment of limited resources.
The Medicare per diem rate for a hospice patient in Seattle is currently $155.80.26 Our CAM provider charges ranged from $40 to $65 per visit, plus transportation costs. This study provides no evidence that requiring integration of professional massage therapists or meditation instructors as uniformly provided treatments in end-of-life care would be a good investment, compared with the continued use of trained hospice volunteers. Although this begs the question of whether integration of massage and meditation as elective treatments in hospice care would result in better quality of life for hospice patients, our study also failed to provide evidence supporting that alternative. In addition to examining differences between assigned treatment groups on the outcomes reported in this article, we investigated whether participants’ enthusiasm for their assigned treatment (assessed before assignment) or the ratio of that enthusiasm level to their mean enthusiasm for the three treatments had a significant association with outcome. Neither variable was significantly associated with any of the four outcomes presented herein (data not shown).
Limitations
This study has several limitations. First, despite the improvement in sample size compared with samples reported in previous studies with similar populations, the findings are nonetheless based on a relatively small sample of terminally ill patients. Although it could be argued that the observed between-group differences would have been statistically significant with a larger sample, the differences were small enough that only a sample much larger than the 300 patients targeted in recruitment efforts would have sufficed. Moreover, the observed differences were so weak as to have been arguably non-meaningful from a clinical perspective. More important for generalizability is the fact that participants came from a restricted geographic area, and only those patients who were reasonably intact mentally and who had an anticipated prognosis of at least 3 weeks’ survival were eligible for participation. Moreover, our sample over-represented white and female groups, compared with all US decedents in 2002,27 and had a considerably higher percentage of college-educated persons than obtained for the US population as a whole in 200028 – all of which further compromise our ability to generalize.
Second, the study focuses on two very general outcomes – overall quality of life and pain distress. It may be unreasonable to expect two brief intervention visits each week, even over an extended period, to have a measurable impact on quality of life, given the potential contributions of so many concurrent and intervening factors. Examination of more limited outcomes, such as patients’ satisfaction with the treatment or their attributions of the specific impact of the treatment on their quality of life, might have pointed to differences between treatment groups.
Third, although our control condition was an attempt to replicate services provided as part of standard care in hospice, our friendly visitors may have been somewhat more skilled in providing these services than the typical hospice volunteer, inasmuch as they had all served as hospice volunteers for at least 1 year prior to joining the study. Furthermore, in addition to their hospice training and experience, they participated in study-specific training and supervision as part of the study intervention team.
Fourth, it is not clear that the randomized controlled trial is the best research model for testing interventions provided to terminally ill patients. Randomization of dying patients to non-preferred treatment groups, with the expectation that they will devote a portion of their limited remaining time and energy to these treatments without hope for subsequent enjoyment of a preferred treatment, has serious ethical implications. In our study, patients gave considerably higher prospective ratings to the two active interventions (mean = 9.4 on a 0-10 scale) than to friendly visits (mean = 8.2), and despite the fact that meditation received an average prospective rating equivalent to that of massage, it joined friendly visits as an intervention that motivated withdrawal from the study before any treatment had occurred. Other research designs may be more appropriate for patients at the end of life, among them crossover trials in which each participant rotates between two treatment conditions for month-long periods for the duration of their study involvement. Particularly when interventions require considerable active participation, as is the case with guided meditation, a design that involves randomizing only those persons who have no treatment preference and assigning all other participants to their treatment of choice may be appropriate,29 thus allowing a test of treatment efficacy (using the randomized sample), plus additional tests for the impact of motivation.
Fifth, outcome measures that penalize for death, as do our measures of weeks of good-quality life and weeks of low pain distress, may not be the best choice in testing the effects of interventions on quality, rather than duration, of life. (In at least one study30 substantial numbers of persons indicated they would elect a therapy that improves quality of life, even if it might hasten death.) However, our test of patients’ mean actual quality-of-life ratings, in which there was no penalty for death, also showed no effect of treatment, and an analysis of quality-of-life trajectories over patients’ time in the study, based on multilevel modeling of patients’ actual quality-of-life ratings, similarly failed to find significant differences by treatment group (data not shown).
Conclusions and Recommendations
Although this study failed to provide evidence sufficient to support integration of either massage or guided meditation into standard care at end of life, we believe that further studies that test these interventions while addressing some of the limitations in our study are warranted – for example, a crossover trial in which patients alternate months between massage and friendly visits and participate in very brief targeted follow-up interviews, specifically addressing the patient’s perception of the impact of the treatments on their quality of life, rather than simply asking them for a global rating of their quality of life. A study comparing massage with friendly visits provided to patients suffering from dementia could also yield useful information if caregivers were enlisted to evaluate the specific effects of treatment on patients’ mood or overall quality of life. Besides studies with terminally ill patients, trials might test CAM interventions with primary caregivers of the dying. Each of these proposed studies could measure the effects of identified treatments on outcomes of interest, as well as the effects of matching treatments to participants’ treatment preferences. We believe that our experience in this study will assist in designing better studies to assess the value of integrating a range of CAM therapies into care of both the dying and their significant others.
Acknowledgments
The authors are grateful for the following contributions to this work:
Financial support from the National Institutes of Health / National Cancer Institute (grant #5R01-CA106204) and the Lotte & John Hecht Memorial Foundation.
Research assistance from Yuki Durham, Department of Health Services, University of Washington
The time, energy, and good will provided by the participating patients, their family and friends, and their hospice and palliative care providers.
Appendix. Scripted Protocol for Meditation Session
Patient may be positioned supine, prone, side lying or sitting depending upon comfort levels
1. Establish therapeutic alliance / didactic introduction to meditation (1st session, 10 min)
Hello, _________. I’m ____________. I am a naturopathic physician who will be teaching you and guiding you in meditation. We’ll be spending about 45 minutes with each other about twice a week here in your room, if that’s OK with you.
Before we begin I wanted to first ask if you have any experience practicing relaxation and abdominal breathing. Have you ever practiced meditation?
LISTEN.
The purpose of meditation is to both focus and relax the mind and the body. Meditation techniques have existed in all cultures of the world for thousands of years. In our modern world, meditation is practiced by patients at home and in hospitals to calm the mind and decrease pain. Many studies have shown that people feel calmer and less stressed when they practice meditation regularly. There are many types of meditation techniques. However, most techniques use the same principle: breathing deeply into your belly and watching your own breathing. The beginning student of meditation is instructed to simply watch the breath go in and out. We do this because the breath is the bridge between the mind and the body. Meditation is a tool every one of us can use to ease pain if we have pain, reduce fear if we are scared, and clear the mind if the mind is thinking non stop. By calming the mind, people who practice meditation find that it is easier to change the way they feel about things that can’t be changed. For example, people who meditate say they were able to find forgiveness when they were angry. When we meditate we are able to feel acceptance for situations that we fear and that we can’t change. Through meditation we can learn to let go of worries. We can feel more loving towards ourselves and those around us. Meditation is also a way to bring a sense of connectedness to our inner selves.
You and I will meet about two times a week. During each session we’ll do a series of things together. First, I will spend 5 minutes talking to you and seeing how you’re doing. I will answer any questions you may have since my last visit. Then in the next 15 minutes I will guide you through a relaxation exercise that will help you relax parts of your body that may feel tense. Then I will teach you what is called “abdominal breathing” (breathing deeply into your belly). After that, we will spend 10 minutes or so guiding you through what is called ‘mindfulness meditation.’ Mindfulness meditation is a technique for clearing, calming, and focusing the mind. During this part of the meditation we will just pay attention to breathing. You may experience sleepiness, or even fall asleep. It’s OK if you do. You may feel distracted or bored or restless. That’s normal, too. Don’t worry. You may feel sad. You may feel love. Simply notice what comes up for you as we proceed.
After practicing these techniques, we will spend 5 minutes in silent meditation. I will use this small chime to start and end this last part of our session together. At the end we’ll spend a few minutes talking about how the session went for you, any thoughts or comments you have, and how you’re feeling.
So before we begin I’d like to get a sense of how you’re doing today. How are you feeling physically and emotionally? LISTEN
2. Guided progressive relaxation (Modified from Kabat-Zinn) 15 minutes
During this process of guided relaxation it will be best if you close your eyes and try to stay awake. However, if you fall asleep, do not worry. Sometimes people fall asleep during the first sessions. It is important to remember not to try too hard to relax. This will just create tension. I will be telling you to focus your attention in one part of your body at a time. When you hear me naming a part of the body, simply become aware of that part of your body as I mention it.
While focusing on a part of your body, let’s say for example your legs, you may feel your legs are tense or in pain. You may want to make the tension or the pain disappear. When this happens, just become aware of the tension and “watch it” – as you would watch a movie. If you become upset, angry, bored, or feel any other disturbing thought or emotion, don’t try to change it. Just watch the emotion or the thought. Simply notice what you are feeling. If a critical thought appears, just notice the thought, observe it. Be aware of how you are feeling, aware of what’s happening right now. Remember there is no one right way to feel while doing this. The way you are feeling right now is the only “right way.”
Allow your eyes to close gently. Let your arms lie calmly at your sides, the palms open towards the ceiling if that feels comfortable for you, allowing your feet to fall away from each other. Slowly bring your attention to the fact that you are breathing. Simply experience the air moving in and out of your body. Now direct your attention to your belly. Feel the sensations in the belly as the breath comes into your body and the abdomen expands gently. Feel the breath moving out of the body and the belly deflating. Just follow the rhythmic movements of your belly with each breath. Imagine that you are watching yourself breathing in and out, your belly expanding when the air goes in, and deflating when the air goes out.
Now take a deep breath and as you let the air out, feel your body becoming heavy, sinking into the bed/chair. As you breathe in, your belly expands with the air. As you breathe out, your body becomes heavier and heavier, sinking deeper and deeper into the bed/chair.
Now we will start moving our attention through different parts of the body to help the body relax. We will go from the feet to the head. First let’s focus the attention on the feet. Take your mind away from your belly, and move your attention down to your legs. Become aware of whatever sensations may be coming from your feet. Perhaps your feet are tingling; perhaps you feel moisture, warmth. Whatever you feel, just become aware of that feeling. Nothing matters, except feeling your feet as they are. As you breathe in imagine that the air is moving right down through the lungs, down into your belly, down into your feet. As you breathe out imagine that the breath is moving back from your feet up through your body and out your nose. Imagine breathing into your toes, then breathing out from your toes.
Now become aware of the lower legs, the front and the back of the legs. Become aware of any sensations in your lower legs. Try not to move them. How do the legs feel? Accept the feelings as you feel them. As you feel the air going in, expanding your belly, let that air run down into your lower legs. As you breathe out, imagine the air running up your legs, up through your upper body and out the nose. Feel your body becoming heavier, more relaxed with each breath, sinking deeper and deeper into the bed/chair.
Let the focus now move up to your knees. Feel your knees, the front, the sides and back of the knees. Breathe into your belly, in and out, deeply and slowly.
Let’s now move the attention into the thighs, all the way up to the groin. Feel your thighs, the back of your thighs sinking into the bed/chair. As you breathe in, feel the air expanding your belly and going down into your legs. Breathe into your thighs.
Become aware of your hips and your pelvis. Experience your pelvis, the entire area below your belly button. Breathe deeply into your pelvis and hips. Become aware of your hips in contact with the bed/chair. Feel the sensations of contact, or weight. As you breathe in, feel your hips sinking even deeper into the bed/chair, letting go of any tension as you sink even deeper and deeper. Totally present in each moment. Just being right here as you are right now.
Now let’s direct our attention to the lower back. Feel the sensations in your lower back. Let the breath move into every part of your lower back. When you breathe in, feel the belly expanding and the lower back sinking even deeper into the bed/chair. When you breathe out, feel the lower back relaxing, letting go of all tension.
Moving your attention now up into the upper back. Just feel the sensations in this part of the body. Breathing in you may feel your rib cage expanding in front and let go of any tension or discomfort in the upper back, just let it dissolve. Feel the belly expanding when breathing in. When breathing out, feel the lower back sinking even deeper into the bed/chair. Feeling very relaxed. Allowing your attention to shift to the belly again and to watch the rising and falling of your belly as you breathe. Just allowing the awareness to expand from the belly to the chest as well. Feeling the movements of your chest and ribs. Breathe into the center of your chest, into your heart. Breathe out tension.
Allow your attention to move now to your fingertips. Become aware of the sensations in the tips of your fingers and the thumbs in both hands. You may feel some pulsations. You may feel dampness. Just feel your fingers. Feel the front and the back of the fingers. Breathe into your fingertips and breathe out from your fingertips.
Allow your awareness to include the palms of your hands, the backs of your hands and your wrists. Perhaps you may feel the pulse of the blood moving to and from your hands. Become aware of the forearms and elbows as well. Become aware of any sensations, any discomfort, any tension.
Allow your awareness now to include your upper arms. Right up to the armpits and shoulders. The shoulders may feel tension or pain. Perhaps the neck feels tense. For a moment now just experience your shoulders and your neck just as they are. And feel the air going into your shoulders with the in breath and upper arms and out from your shoulder and upper arms during the out breath. Let that tension dissolve as you breathe out.
Now become aware of the face, the jaw and the chin. Just experiencing it as it is. Breathe into your face and out from your face. Let any tension in the face, jaw and chin dissolve.
Become aware of your lips and your mouth, your teeth, your gums, your tongue, the roof of your mouth. Notice your forehead, your scalp. Be aware of your eyes and the eyebrows and the space between the eyebrows and the entire region around your eyes. Become aware of your eyelids. Breathe into your eyes and out from your eyes. Allowing the sides of your head to relax as you experience the sensations on the side of your head. Breathe into your ears and breathing out from your ears and letting them relax as well. Breathing into your forehead and out from your forehead, letting it soften. Just being aware that you’re nourishing your face by breathing in, letting your forehead relax, letting tension and worries dissolve in relaxation and stillness.
Now become aware of the back of the head and the top of the head. Breathing in and breathing out from this part of the head. Imagine the air going in and out from the top of your head and right back down into it. Now you see yourself breathing into the top of the head and out from the top of your head. Just watching and allowing your breath to move in this way. Along the entire length of your body all of your muscles in a deep state of relaxation and your mind simply aware of this flow of the breath, experiencing your entire body breathing.
Feel your whole body breathing. Lying here in a state of stillness and deep relaxation. Sinking deeper and deeper into a state of well being as you come in touch with feeling complete, feeling whole, feeling at peace. Open to things just as they are in each moment. You are in a state of peace and healing, allowing the world to be as it is, beyond personal fears and concerns. Beyond the tendencies of the mind to want things a certain way. See yourself as complete right now, just as you are. Experience the fullness of the moment, experience the fullness of your ability to love and be whole – just are you are, right now.
Silence for 30 seconds.
3. Breathing meditation (based on Sharon Salzberg) 5 min
Now that the body and the mind are very relaxed, we will spend a few minutes just watching the breath. Bring a quality of relaxed, open, spacious awareness to feeling your breath. Take three deep, easy breaths and release them.
3 breaths
Allow the breath to become natural, so you’re not trying to force or control it in any way.
Notice the place where you feel the breath most clearly. It may be the in-and-out movement of the air at the nostrils. You may feel tingling or vibration, or changes in temperature. You may feel the breath most distinctly with the rising and falling of the chest or the abdomen: stretching … pressure … tension … release.
As you feel the breath, say to yourself “in” as you feel the breath going in; “out” as you feel the breath leave your body. Very gently, very quietly in your mind, become aware of the actual sensations … just note “in” and “out”…“rising” and “falling.” 10 sec
You don’t need to make the breath special. It doesn’t have to be deep or long or different from however it is and however it changes. It’s happening anyway, so simply be aware of it … one breath at a time. 10 sec
You may find your attention wandering. You may realize that you’ve been lost in thought, planning, remembering, whatever. Perhaps it’s been quite some time since you last felt the breath consciously. It doesn’t matter. You don’t have to judge or analyze how you got there. Don’t worry. See if you can gently let go of whatever the distraction has been and simply begin again. Gently let go, and return the attention to the actual feeling of the breath.
This act of beginning again is the essential art of meditation practice … over and over and over, we begin again. You may find your attention wandering again and again. It doesn’t matter. The mind has been trained to be distracted. In a very patient manner, just let go … reconnect … come back to the feeling of the breath in this very moment … the natural, normal breath. 15 sec
Simply feel your breath ....
If you find your attention has wandered, that’s fine. See if you can practice being patient, being gentle, and beginning again. You may discover that there’s a pause or a gap between the in breath and the out breath, or between the out breath and the next in breath. If you find such a pause, you can allow the attention to settle there, in the space between breaths. Simply feel your body lying/sitting here. Then allow the next breath to come naturally.
Notice the difference between feeling the breath and observing the breath from some distance. You’re not struggling to see the breath or visualize it, but simply feeling it. Feel the tingling or the heat or the coolness at the nostrils … or the stretching, the pressure, the movement in the chest or abdomen.
There’s nothing you need to do about it. You don’t need to change it; you don’t need to force it or perfect it. Focus your mind on each breath. We’re simply here. This is our life, right in this moment, this one breath. Many, many distractions will arise. A torrent of thoughts and plans and images and aches and pains – it doesn’t matter. Just watch your breath.
If you’ve lost touch with an awareness of the breath … just recognize it and simply come back to the breath. If you start to feel sleepy, just notice it and return your mind to the breath. Take a few deep breaths consciously … and then again, allow the breath to become natural. If you have to begin again and again and again in the course of one sitting, that’s the practice. That’s what meditation is. 10 sec
Focus your attention on the breath that’s appearing right now. See if you can sustain attention through the course of one entire breath. 10 sec
4. Counting breaths meditation (Based on Marsha Linehan’s Walking like Buffalo) 10 min
For the last part of today’s session I want to teach you another simple method of meditation that involves counting your breaths. Counting your breaths is another method of mindfulness meditation.
Place your hands on your chest or your belly. Notice the air coming in filling up your lungs; just notice whatever happens – without expectation. First we will learn to focus the mind. The way to practice focusing the mind is to practice an activity. The activity we will practice is counting the breath. Let me go over the instructions first before we try this method together.
You will count your in breath and count your out breath. One in, two out, three in, four out, and so on. When you get to 10 you start over. If you find that you’ve gotten lost on the way, simply start over. Sometimes people don’t stop at 10 and keep going and then notice that they’ve counted beyond 10. If you notice that, simply return to one – just start over. Focus on the breath in and the breath out. Count one, two, three, four.
When you are counting “one” try to count as if every part of your body is saying “one” – your mind and your body – your whole self is saying one and nothing else. When you say two – everything about you is saying two and nothing else – as if your whole body and mind is saying two. Your whole self is saying two – and nothing else. Every time a thought comes through, try to notice it, and gently return your mind to counting. Gently always returning the mind to counting your breaths. If an urge to move comes in just notice it. Just keep counting. If an itch or urge to blow your nose – just notice it. See what happens if you don’t follow your impulse to move. Notice the natural movements of the body as you breathe. If it is a strain not to move, then move mindfully. Then bring your attention back to counting your breaths – in and out.
You may want to move because you have a pain in your hips or back – just notice it. Sometimes the body will move when tension is released. That’s OK. You may notice you’re in an uncomfortable position – just notice it. Just observe your impulses. Just notice. Simply count your breaths. One in, two out, three in … until you reach 10 and start again.
I’ll start our counting meditation with a sound of the chime. When the time is over, you will hear the chime again. Between the chimes we will practice counting breaths silently. It won’t be too long and it won’t be too short.
Silent counting meditation for 5 minutes. Start by ringing chime softly. End with a soft ringing of the chime.
When you’re ready, wiggle your fingers and your toes. When you’re ready, gently open your eyes and come back to the room and to me. When you’re ready, I’d like you to tell me your experiences during our meditation session today.
LISTEN
After each session, ask the patient how s/he is feeling, if s/he has questions or comments s/he would like to share with you. Also, ask for feedback about what worked and did not work, what the patient was able or not able to follow, and what s/he was comfortable with. Use this feedback to tailor subsequent sessions to meet the patient’s needs. Modifications are allowed as long as they are consistent with the techniques used in the protocol: for example, if the guided relaxation is not appropriate for a patient, increase the time used for silent meditation or other portions of the protocol.
When patient has finished reporting to you, end the session by saying; “See you on _______ at ______. Good bye. Be well.”
Appendix References
- Kabat-Zinn J. Full Catastrophe of Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Delta; 1991. [Google Scholar]
- Kabat-Zinn J. Mindfulness Meditation Practice Series One [audio cassette] Nightingale-Conant Corporation; 1995. [Google Scholar]
- Kabat-Zinn J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life. Hyperion; 1994. [Google Scholar]
- Linehan MM. Walking like Buffalo [compact disc] Behavioral Tech, LLC; 2003. [Google Scholar]
- Salzberg S, Goldstein J. Insight Meditation: An In-Depth Correspondence Course [Book and Cassette edition] Sounds True; 1998. [Google Scholar]
References
- 1.SUPPORT Principal Investigators A controlled trial to improve care for seriously ill hospitalized patients: the study to understand prognoses and preferences for outcomes and risks of treatment (SUPPORT) JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 2.Field MJ, Cassel CK, editors. Approaching death: improving care at the end of life. National Academies Press; Washington, DC: 1997. [PubMed] [Google Scholar]
- 3.Task Force on Palliative Care. Last Acts Campaign. Robert Wood Johnson Foundation Precepts of palliative care. J Palliat Med. 1998;1:109–112. doi: 10.1089/jpm.1998.1.109. [DOI] [PubMed] [Google Scholar]
- 4.The Robert Wood Johnson Foundation [accessed September 9, 2008];Means to a better end: a report on dying in America today. 2002 Available from: http://www.rwjf.org/files/publications/other/meansbetterend.pdf.
- 5.Kessler RC, Davis RB, Foster DF, Van Rompay MI, Walters EE, Wilkey SA, Kaptchuk TJ, Eisenberg DM. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med. 2001;135:262–268. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 7.Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in the use of complementary and alternative medicine by US adults: 1997-2002. Altern Ther Health Med. 2005;11:42–49. [PubMed] [Google Scholar]
- 8.Pan CX, Morrison RS, Ness J, Fugh-Berman A, Leipzig RM. Complementary and alternative medicine in the management of pain, dyspnea, and nausea and vomiting near the end of life: a systematic review. J Pain Symptom Manage. 2000;20:374–387. doi: 10.1016/s0885-3924(00)00190-1. [DOI] [PubMed] [Google Scholar]
- 9.Demmer C, Sauer J. Assessing complementary therapy services in a hospice program. Am J Hosp Palliat Care. 2002;19:306–314. doi: 10.1177/104990910201900506. [DOI] [PubMed] [Google Scholar]
- 10.Lewis CR, de Vedia A, Reuer B, Schwan R, Tourin C. Integrating complementary and alternative medicine (CAM) into standard hospice and palliative care. Am J Hosp Palliat Care. 2003;20:221–228. doi: 10.1177/104990910302000312. [DOI] [PubMed] [Google Scholar]
- 11.Lafferty WE, Downey L, McCarty RL, Standish LJ, Patrick DL. Evaluating CAM treatment at the end of life: a review of clinical trials for massage and meditation. Complement Ther Med. 2006;14:100–112. doi: 10.1016/j.ctim.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Soden K, Vincent K, Craske S, Lucas C, Ashley S. A randomized controlled trial of aromatherapy massage in a hospice setting. Palliat Med. 2004;18:87–92. doi: 10.1191/0269216304pm874oa. [DOI] [PubMed] [Google Scholar]
- 13.Wilcock A, Manderson C, Weller R, Walker G, Carr D, Carey A-M. Does aromatherapy massage benefit patients with cancer attending a specialist palliative care day centre? Palliat Med. 2004;18:287–90. doi: 10.1191/0269216304pm895oa. [DOI] [PubMed] [Google Scholar]
- 14.Wilkie DJ, Kampbell J, Cutshall S, Halabisky H, Harmon H, Johnson LP, Weinacht L, Rake-Marona M. Effects of massage on pain intensity, analgesics and quality of life in patients with cancer pain: a pilot study of a randomized clinical trial conducted within hospice care delivery. Hosp J. 2000;15(3):31–53. [PubMed] [Google Scholar]
- 15.Sloman R. Relaxation and imagery for anxiety and depression control in community patients with advanced cancer. Cancer Nurs. 2002;25:432–435. doi: 10.1097/00002820-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed September 9, 2008];Improving End-of-Life Care. NIH Consensus and State-of-the-Science Statements. 2004 21(3):1–28. Available from: http://consensus.nih.gov/2004/2004EndOfLifeCareSOS024PDF.pdf. [PubMed]
- 17.Lynn J. Measuring quality of care at the end of life: a statement of principles. J Am Geriatr Soc. 1997;45:526–527. doi: 10.1111/j.1532-5415.1997.tb05184.x. [DOI] [PubMed] [Google Scholar]
- 18.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2482. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 19.Downey L, Engelberg RA, Curtis JR, Lafferty WE, Patrick DL. Shared priorities for the end-of-life period. J Pain Symptom Manage. 2009;37:175–188. doi: 10.1016/j.jpainsymman.2008.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diehr PH, Derleth AM, McKenna SP, Martin ML, Bushnell DM, Simon G, Patrick DL. Synchrony of change in depressive symptoms, health status, and quality of life in persons with clinical depression. Health Qual Life Outcomes. 2006;4:27. doi: 10.1186/1477-7525-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Curtis JR, Patrick DL, Engelberg RA, Norris K, Asp C, Byock I. A measure of the quality of dying and death: initial validation using after-death interviews with family members. J Pain Symptom Manage. 2002;24:17–31. doi: 10.1016/s0885-3924(02)00419-0. [DOI] [PubMed] [Google Scholar]
- 22.Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Kiyasu E, Sobel K, Coyle N, Kemeny N, Norton L, Scher H. The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer. 1994;30A:1826–1336. doi: 10.1016/0959-8049(94)90182-1. [DOI] [PubMed] [Google Scholar]
- 23.Diehr P, Lafferty WE, Patrick DL, Downey L, Devlin SM, Standish LJ. Quality of life at the end of life. Health Qual Life Outcomes. 2007 Aug 3;5:51. doi: 10.1186/1477-7525-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernard SA, Bruera E. Drug interactions in palliative care. J Clin Oncol. 2000;18:1780–1799. doi: 10.1200/JCO.2000.18.8.1780. [DOI] [PubMed] [Google Scholar]
- 25.AGS Panel on Persistent Pain in Older Persons The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50:S205–S224. doi: 10.1046/j.1532-5415.50.6s.1.x. [DOI] [PubMed] [Google Scholar]
- 26.Providence Hospice of Seattle . personal communication. Sep 9, 2008. [Google Scholar]
- 27.National Center for Health Statistics [Accessed September 9, 2008];Deaths by place of death, age, race, and sex: United States. 2002 Available from: http://www.cdc.gov/nchs/data/dvs/mortfinal2002_work309.pdf.
- 28.US Census Bureau [Accessed September 9, 2008];Educational attainment of people 18 years and over, by metropolitan and nonmetropolitan residence, age, sex, race and Hispanic origin: March 2002. Available from: http://www.census.gov/population/socdemo/education/ppl-169/tab11.pdf.
- 29.Brewin CR, Bradley C. Patient preferences and randomized clinical trials. Br Med J. 1989;299:313–315. doi: 10.1136/bmj.299.6694.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rector TS, Txchumperlin LK, Kubo SH, Bank AJ, Francis GS, McDonald KM, Keeler CA, Silver MA. Use of the Living with Heart Failure questionnaire to ascertain patients’ perspectives on improvement in quality of life versus risk of drug-induced death. J Card Fail. 1995;1:201–206. doi: 10.1016/1071-9164(95)90025-x. [DOI] [PubMed] [Google Scholar]


