Abstract
Hyperhidrosis is a disorder of perspiration in excess of the body's physiologic need and significantly impacts one's occupational, physical, emotional, and social life. The purpose of our study was to investigate the characteristics of primary hyperhidrosis in 255 patients at Ajou University Hospital Hyperhidrosis Center from March 2006, to February 2008. Information collected from the medical records was: sex, sites of hyperhidrosis, age at visit, age of onset, aggravating factors, hyperhidrosis disease severity scale (HDSS) rank, family history, occupation, and past treatment. A total of 255 patient records were reviewed; 57.6% were male. Patients with a family history (34.1%) showed a lower age of onset (13.21±5.80 yr vs. 16.04±9.83 yr in those without family history); 16.5% had previous treatment, most commonly oriental medicine. Palmar and plantar sites were the most commonly affected, and 87.9% of patients felt their sweating was intolerable and always interfered with their daily activities. Our study provides some original information on the Korean primary hyperhidrosis population. Patients who have a family history show signs of disease in early age than those without family history.
Keywords: Epidemiology, Primary Hyperhidrosis
INTRODUCTION
Hyperhidrosis is a condition characterized by excessive sweating and can be focal (primary) or generalized (secondary) (1). Secondary hyperhidrosis is caused by an underlying condition such as infection, endocrine or metabolic disorders, neoplastic diseases, neurologic conditions, spinal cord injuries, cardiovascular or respiratory disorders, anxiety, or stress (2, 3).
Primary hyperhidrosis has been associated with hyperactivity of the sympathetic nervous system and can affect the palms, soles, axillae, face, and scalp as well as other sites (2, 4). This condition occurs in otherwise healthy people and can have a deeply detrimental effect on quality of life, resulting in impairment of daily activities, social interactions and occupational activities (5, 6).
A pilot study of young Israelis reported an incidence of 1% (7), and hyperhidrosis prevalence in the United States is 2.8%, equivalent to 7.8 million people (2). Hyperhidrosis is uncommon but not rare. Despite many treatment modalities, research into the characteristics of hyperhidrosis patients is limited. Here, we retrospectively investigated the epidemiologic characteristics of primary hyperhidrosis patients visiting a hyperhidrosis center in Korea.
MATERIALS AND METHODS
We reviewed the medical records of patients visiting our hyperhidrosis center between March 2006, and February 2008, for diagnosis and treatment of hyperhidrosis. Information collected from the medical records included: sex, age at visit, age of onset, referral source, occupation, family history, past treatment, hyperhidrosis sites, aggravating factors and hyperhidrosis disease severity scale (HDSS) ranking. We analyzed the relationship between family history of hyperhidrosis and age of onset. Qualitative variables are expressed as percentages and compared using Pearson's chi-square test. Quantitative variables are expressed as mean±standard deviation and compared using Student's t-test. We analyzed the results with SPSS version 15.0 (SPSS, Chicago, IL, USA) and all P values less than 0.05 were considered statistically significant.
RESULTS
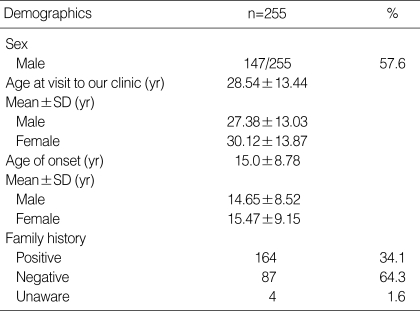
A total of 255 medical records were reviewed; 57.6% of the patients were male, the mean age was 28.54±13.44 yr old at the date of visit, with a mean age of onset of 15.0±8.78 yr old, and 34.1% of all patients had a positive family history of hyperhidrosis (Table 1). The mean age of onset in those with a positive family history was 13.21±5.80 yr, significantly lower than the age (16.04±9.83 yr) in those without family history of hyperhidrosis (P<0.006).
Table 1.
Patient demographic data
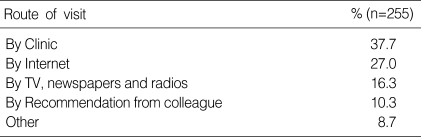
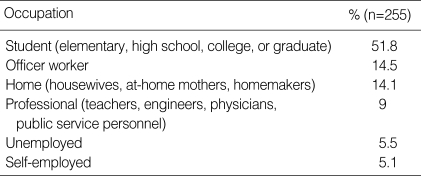
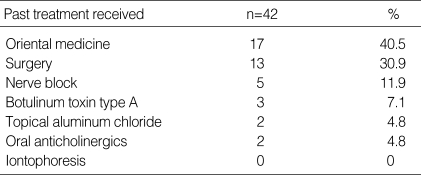
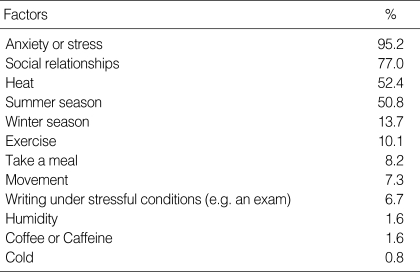
The route to visit our center and occupation of the patients are described by frequency (Tables 2, 3). The most common route of visit was "arranged by individual clinic" and the most common occupational category was "student". Previous treatment was attempted by 42 of the 255 patients (16.5%). The most common treatment modality before the visit was oriental medicine such as herbal medication and acupuncture (Table 4). The most common aggravating factors were stress or anxiety, and social relationships (Table 5).
Table 2.
Referral source
Table 3.
Patient occupation
Table 4.
Previous treatment
Table 5.
Aggravating factors
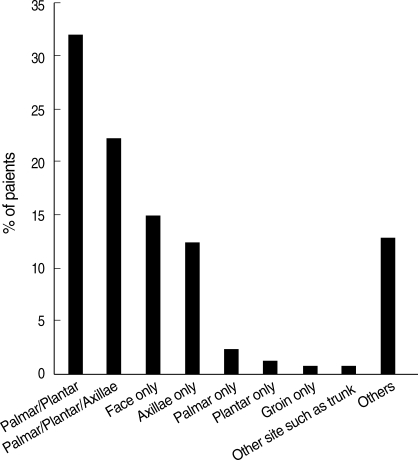
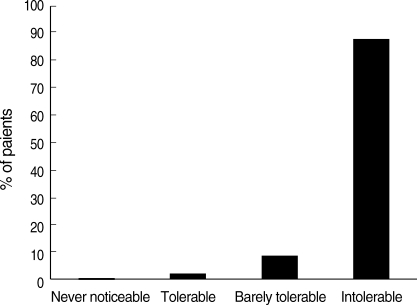
Palmar and plantar sites were the most commonly affected sites (Fig. 1). We determined how hyperhidrosis affected their life using the hyperhidrosis disease severity scale. Most (87.9%) patients felt their sweating was intolerable and always interferes with their daily activities (Fig. 2).
Fig. 1.
Sites of hyperhidrosis. Others are any combinations of excessive sweating sites except palmar/platar and palmar/plantar/axillae.
Fig. 2.
Impact of sweating on daily activities accounting by hyperhidrosis severity scale.
DISCUSSION
This research provides original information on primary hyperhidrosis and is the first descriptive study of Korean hyperhidrosis patients. The average age of onset is 15.0 yr old in our study, earlier than in a 2004 United States prevalence study (25.2 yr) (2). However, a more recent US study in 2007 showed a similar average age of onset to our study (14.05 yr) (8); the mean age at first visit for diagnosing and treatment of hyperhidrosis was 28.05 yr in our study and also in the recent US study (8), compared to 39.8 yr in the 2004 study (2). These studies showed that primary hyperhidrosis appeared in adolescence, but people seek medical treatment in early adulthood. Stolman suggested a genetic predisposition may exist, since 30-50% of patients have a family history of hyperhidrosis (9). A pedigree analysis by Kaufmann et al. (10) suggested that hyperhidrosis segregated independently as an autosomal dominant trait and was not inherited as a crosslinked trait. Ro et al. (11) reported a 65% incidence of positive family history in 49 patients with hyperhidrosis that had undergone thoracoscopic sympathectomy. The 2007 US study showed 47.3% of hyperhidrosis patients had a positive family history and patients who reported an onset age below 20 yr of age were more likely to have a positive family history of hyperhidrosis than those with a later age of onset (8). In line with these results, our study revealed a family history in 34.1% of primary hyperhidrosis cases; and positive family history patients had a younger onset age than those with a negative family history (13.21±5.80 yr old vs. 16.04±9.83 yr old).
Hyperhidrosis is present in 2.8% of the general population in the United States (2). This condition can have a deeply detrimental effect on a patient's quality of life, resulting in dramatic impairments of daily activities, social interactions and occupational activities (5, 6). But, patients rarely seek a physician because many are unaware there are many treatments for primary hyperhidrosis (1). In this study we asked patients how they were referred to our hyperhidrosis clinic or how they got information for hyperhidrosis treatment. The most common referral mode was recommendation by individual clinics, although many patients also found information from the internet or mass media.
Lear et al. (8) reported patients had some form of treatment before the consult visit, such as topical aluminum chloride or botulinum toxin type A subcutaneous injections. However, in this study the most common treatment modality before the visit was oriental medicine such as herbal medication and acupuncture.
Hyperhidrosis can be generalized, involving the whole body, but primary focal hyperhidrosis involves limited body areas, most often palms, soles, face, axillae or a combination of them. In our study, the most commonly affected sites that had excessive sweating were palmar and plantar sites simultaneously (32.2%). Other common sites were a combination of palmar, plantar and axillae (22.4%). There are many treatment modalities for hyperhidrosis such as topical aluminum chloride, iontophoresis, botulinum toxin type A injection, endoscopic thoracic sympathectomy (ETS), axillary sweat gland removal, oral anticholinergic, and chemical lumbar sympathectomy (CLS) (12-15). Most of such treatment modalities are usually effective for focal area. But our results showed many patients suffer from excessive sweating in multiple sites. In our clinic, We are performing different procedure depending on problem area. Patients who has only palmar hyperhidrosis, we perform VATS. Patients who has only plantar hyperhidrosis, we perform CLS. Patients who has only axillary hyperhidrosis, we perform axillary sweat gland removal. We use oral anticholinergic (glycopyrrolate) for the patients who has multiple sites hyperhidrosis or refuse to have invasive procedure, contraindication to have invasive treatment, recurrence after above mentioned procedure such as ETS, CLS, and axillary sweat gland removal.
Excessive sweating of primary hyperhidrosis patients is usually triggered by anxiety, embarrassment, fear, anger, excitement, or mental stress (16). Eccrine sweat glands are innervated by cholinergic fibers from the sympathetic nervous system. Their sweat secretion function is affected by emotional and gustatory stimuli. Nearly all (95%) primary hyperhidrosis patients said their sweating was intensified when they were in stressful situations or felt anxiety, and 77.0% felt their symptoms were aggravated in social situations. Another common trigger factor was heat.
The severity and impact of hyperhidrosis was assessed using the HDSS, which provides a qualitative measure allowing tailored treatment; this validated and reliable instrument has been used in other studies of hyperhidrosis (17, 18). The HDSS is used to determine the severity of sweating experienced by the respondents. A 4-point, single-item question, the HDSS asks patients to indicate which of the following best describes the impact of sweating on their daily activities: 1) never noticeable, never interferes; 2) tolerable, sometime interferes; 3) barely tolerable, frequently interferes; or 4) intolerable and always interferes. Most (87.9%) of hyperhidrosis patients have sweating that is a '4'.
In conclusion, we described the epidemiologic characteristics of primary hyperhidrosis patients in Korea for the first time. These characteristics can help physicians who treat the patients. The patients who have a family history show signs of disease in early age than those without family history. Most of hyperhidrosis patients have intolerable sweating and excessive sweating which interfered their daily activities. Since the study scope was limited to one hyperhidrosis center; a national survey should be performed to further expand the data available to assist whole Korean patients.
References
- 1.Haider A, Solish N. Focal hyperhidrosis: diagnosis and management. CMAJ. 2005;172:69–75. doi: 10.1503/cmaj.1040708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strutton DR, Kowalski JW, Glaser DA, Stang PE. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: results from a national survey. J Am Acad Dermatol. 2004;51:241–248. doi: 10.1016/j.jaad.2003.12.040. [DOI] [PubMed] [Google Scholar]
- 3.Eisenach JH, Atkinson JL, Fealey RD. Hyperhidrosis: evolving therapies for a well-established phenomenon. Mayo Clin Proc. 2005;80:657–666. doi: 10.4065/80.5.657. [DOI] [PubMed] [Google Scholar]
- 4.Hornberger J, Grimes K, Naumann M, Glaser DA, Lowe NJ, Naver H, Ahn S, Stolman LP. Recognition, diagnosis, and treatment of primary focal hyperhidrosis. J Am Acad Dermatol. 2004;51:274–286. doi: 10.1016/j.jaad.2003.12.029. [DOI] [PubMed] [Google Scholar]
- 5.Amir M, Arish A, Weinstein Y, Pfeffer M, Levy Y. Impairment in quality of life among patients seeking surgery for hyperhidrosis (excessive sweating): preliminary results. Isr J Psychiatry Relat Sci. 2000;37:25–31. [PubMed] [Google Scholar]
- 6.Lerer B, Jacobowitz J, Wahba A. Personality features in essential hyperhidrosis. Int J Psychiatry Med. 1980-1981;10:59–67. doi: 10.2190/866g-qqa9-q9ae-15nb. [DOI] [PubMed] [Google Scholar]
- 7.Connolly M, de Berker D. Management of primary hyperhidrosis: a summary of the different treatment modalities. Am J Clin Dermatol. 2003;4:681–697. doi: 10.2165/00128071-200304100-00003. [DOI] [PubMed] [Google Scholar]
- 8.Lear W, Kessler E, Solish N, Glaser DA. An epidemiological study of hyperhidrosis. Dermatol Surg. 2007;33:S69–S75. doi: 10.1111/j.1524-4725.2006.32334.x. [DOI] [PubMed] [Google Scholar]
- 9.Stolman LP. Treatment of hyperhidrosis. Dermatol Clin. 1998;16:863–869. doi: 10.1016/s0733-8635(05)70062-0. [DOI] [PubMed] [Google Scholar]
- 10.Kaufmann H, Saadia D, Polin C, Hague S, Singleton A. Primary hyperhidrosis-evidence for autosomal dominant inheritance. Clin Auton Res. 2003;13:96–98. doi: 10.1007/s10286-003-0082-x. [DOI] [PubMed] [Google Scholar]
- 11.Ro KM, Cantor RM, Lange KL, Ahn SS. Palmar hyperhidrosis: evidence of genetic transmission. J Vasc Surg. 2002;35:382–386. doi: 10.1067/mva.2002.119507. [DOI] [PubMed] [Google Scholar]
- 12.Baumgartner FJ, Bertin S, Konecny J. Superiority of thoracoscopic sympathectomy over medical management for the palmoplantar subset of severe hyperhidrosis. Ann Vasc Surg. 2009;23:1–7. doi: 10.1016/j.avsg.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Lee MR, Ryman WJ. Liposuction for axillary hyperhidrosis. Australas J Dermatol. 2005;46:76–79. doi: 10.1111/j.1440-0960.2005.00145.x. [DOI] [PubMed] [Google Scholar]
- 14.Bajaj V, Langtry JA. Use of oral glycopyrronium bromide in hyperhidrosis. Br J Dermatol. 2007;157:118–121. doi: 10.1111/j.1365-2133.2007.07884.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim WO, Yoon KB, Kil HK, Yoon DM. Chemical lumbar sympathetic block in the treatment of plantar hyperhidrosis: a study of 69 patients. Dermatol Surg. 2008;34:1340–1345. doi: 10.1111/j.1524-4725.2008.34286.x. [DOI] [PubMed] [Google Scholar]
- 16.Ellis H. Hyperhidrosis and its surgical management. Postgrad Med. 1975;58:191–196. doi: 10.1080/00325481.1975.11714151. [DOI] [PubMed] [Google Scholar]
- 17.Solish N, Bertucci V, Dansereau A, Hong HC, Lynde C, Lupin M, Smith KC, Storwick G. A comprehensive approach to the recognition, diagnosis, and severity-based treatment of focal hyperhidrosis: recommendations of the Canadian Hyperhidrosis Advisory Committee. Dermatol Surg. 2007;33:908–923. doi: 10.1111/j.1524-4725.2007.33192.x. [DOI] [PubMed] [Google Scholar]
- 18.Cetindag IB, Boley TM, Webb KN, Hazelrigg SR. Long-term results and quality-of-life measures in the management of hyperhidrosis. Thorac Surg Clin. 2008;18:217–222. doi: 10.1016/j.thorsurg.2008.01.009. [DOI] [PubMed] [Google Scholar]