Abstract
Neurofibromatosis type 1 (NF1) is one of the most commonly inherited autosomal dominant disorders. In order to determine whether genomic alterations and/or chromosomal aberrations involved in the malignant progression of NF1 were present in a Korean patient with NF1, molecular and cytogenetic analyses were performed on the pathologically normal, benign, and malignant tissues and primary cells cultured from those tissues of the patient. The comparative genomic hybridization (CGH) array revealed a Y chromosome loss in the malignant peripheral nerve sheet tumor (MPNST) tissue. G-banding analysis of 50 metaphase cells showed normal chromosomal patterns in the histopathologically normal and benign cultured cells, but a mosaic Y chromosome loss in the malignant cells. The final karyotype for the malignant cells from MPNST tissue was 45,X,-Y[28]/46,XY[22]. The data suggest that the somatic Y chromosome loss may be involved in the transformation of benign tumors to MPNSTs.
Keywords: CGH Array; Chromosome Loss; G-banding; Nerve Sheath Neoplasms; Neurofibromatosis 1, Y chromosome
INTRODUCTION
Neurofibromatosis type 1 (NF1) is a common autosomal dominant genetic disorder with an incidence of approximately 1 in 3,000-3,500 individuals worldwide (1). NF1 is clinically characterized by the presence of well established phenotypic features, including café-au-lait (CAL) spots, neurofibromas, freckling of the axillary or inguinal region, Lisch nodules, optic nerve gliomas, and bone dysplasias (1). Nearly all NF1 patients have benign dermal neurofibromas, and approximately 30% of NF1 patients have benign plexiform neurofibromas which can undergo malignant transformation to malignant peripheral nerve sheet tumors (MPNSTs) (2). Malignant transformation into MPNSTs was observed in 2-13% of NF1 patients with plexiform neurofibromas (3) and represents a major cause of mortality in NF1 patients (1).
Haploinsufficiency for neurofibromin has been suggested as the molecular basis of the disease (1, 2). NF1 is caused by mutations in 1 of the 2 alleles of the NF1 gene, located at chromosome 17q11.2, encoding neurofibromin, a GTPase activating protein (GAP). Approximately 5-20% of all NF1 patients have been reported to carry a heterozygous large ~1.5 Mb deletion at chromosome 17q11, where the entirety of the NF1 gene and several neighboring genes exist, mediated by homologous recombination between the NF1 repetitive sequences (4). It has been reported that a bi-allelic inactivation of NF1, with one allele constitutionally inactivated and the other somatically mutated, is required for neurofibroma and MPNST formation (5), indicating that the tumor progression of NF1 is most likely triggered by the complete loss of the NF1 gene in somatic cells. Somatic loss of heterozygosity (LOH) at the NF1 locus has been described for neurofibromas and MPNSTs in previous studies (5).
In a previous study, we reported the case of a 24-yr old male NF1 patient with benign plexiform neurfiboromas and MPNSTs (6). A whole gene expression comparison study was carried out using tissue samples obtained by surgical resection and skin biopsy from the patient. Because frequent genomic imbalances in chromosomes 17, 19, and 22q in the neurofibromas and MPNSTs have been reported in the patients with NF1 (7), we also tested for genomic alterations and/or chromosomal aberrations in the same patient in this study. Comparison study among normal, benign and malignant tissues and cells was carried out on the chromosomal level. Here, we report a Korean patient with NF1 who had a mosaic Y chromosome loss involved in malignant progression.
CASE REPORT
A 24-yr old male patient was diagnosed to have NF1 based on standard diagnostic criteria at the Genetic Clinic in Ajou University Hospital. The patient, having a NF1 nonsense mutation (Y2264X) in the NF1 gene, preFsented the clinical features of NF1 with café-au-Lait spots, plexiform neurofibromas, cutaneous neurofibromas, subcutaneous neurofibromas, scoliosis, and neurofibrosarcomas (MPNSTs) (6). After surgical resection of tumors in the patient died at age of 25. Tumor specimens containing benign and malignant tumors and histopathologically normal tissues were obtained by surgical resection and skin biopsy, respectively. Three types of tissues, normal skin fibroblasts, benign plexiform neurofibromas, and MPNSTs were prepared and histopathologically evaluated by routine light microscopy after staining with hematoxylin and eosin (H&E) as previously described (6).
To determine whether genomic alterations, including microdeletions and gene copy number changes, existed in this male patient, we performed a comparative genomic hybridization (CGH) array with high resolution CGH array slides containing 1440 clones, including 356 cancer related genes from BAC libraries at a resolution of 2.3 Mb. Three types of tissues were used; normal skin fibroblasts, benign plexiform neurofibromas, and malignant neurofibrosarcomas (MPNST), all bearing an identical germ line mutation of the Y2264X (c.6792C>G) nonsense mutation on the NF1 gene (6).
DNA was extracted from the tissue samples and used for a CGH array, performed as previously described (8). Commercially available CGH array slides (Genomarray; Macrogen Inc., Korea) were analyzed using the chromofluor image analysis system (Arrayscanner, Array analysis; Macrogen Inc., Korea). The slides contained 1440 clones from BAC libraries. Each cloned BAC clone DNA was arrayed on the slide in three spots. Non-NF1 male DNA was used as a reference. The slides were scanned into two 16-bit TIFF image files using GenePix4200A two-color fluorescent scanner (MDS Inc., Canada) and quantitated using GenePix software (MDS Inc., Canada). Green (reference) to red (test) (G/R) ratios were automatically determined for each sample, and the normalized G/R ratio was taken to represent the relative average number of copies of the sequence for those spots that were selected as controls. Spots with G/R ratios more than the mean plus 2.5 standard deviations (1.25) were considered as amplifications or gains of the indicated copy number; less than the mean minus 2.5 deviations (-0.75) were considered as losses of the copy number.
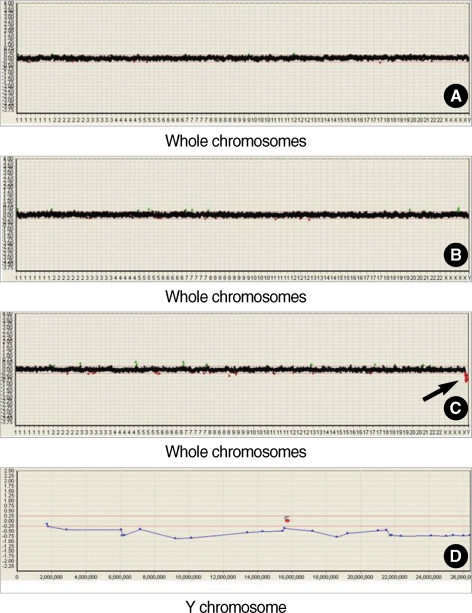
Control hybridization of non-NF1 male DNA was performed in four independent experiments and resulted in a mean log2 fluorescence ratio of 0.0±0.125 S.D., reflecting the equal copy number in test and reference DNAs (data not shown). Hybridization of non-NF1 male DNA (reference) vs. DNA from normal tissue of the NF1 patient and further hybridizations of DNA from normal tissue and from benign or malignant tissues from the NF1 patient were performed and their results shown in Fig. 1. Multiple tests were performed to further narrow down the significant clones discussed in this paper. No genetic alteration, including DNA copy number change across whole chromosomes, was detected in the hybridizations of reference DNA vs. DNA from either normal tissue (Fig. 1A) or benign tissue (Fig. 1B). However, the loss of the whole Y chromosome was detected in the hybridization of the DNA from normal tissue vs. the DNA from MPNST tissue (Fig. 1C). The detailed CGH array profile of the Y chromosome for NPNST tissue showed Y chromosome-specific genomic loss across the whole region of the Y chromosome (Fig. 1D). Therefore, we focused our study on the Y chromosome aberrations in the MPNST tissue.
Fig. 1.
CGH array profiles of the normal, benign and malignant tissues of a patient with NF1. Graphics from the Macrogen's Mac-Viewer array CGH software show that CGH array profiles for whole chromosomes by (A) hybridization of non-NF1 male DNA (reference) versus test DNA from normal tissue of the NF1 patient, (B) hybridization of DNA from normal tissue versus DNA from benign tissue of the NF1 patient, and (C) hybridization of DNA from normal tissue vs. DNA from MPNST tissue of the NF1 patient. Arrow indicates where loss occurred in the Y chromosome. (D) Graphic shows detailed CGH array profile for the whole region of Y chromosome in the hybridization of DNAs from normal tissues vs. MPNST tissues of the NF1 patient. Two markers with a letter 'C' indicate the position of centromere.
To confirm the CGH array findings, G-banding analysis was performed on primary tissue cultured cells. First, primary tissue culture was performed by primary explant technique from the pathologically normal, benign, and MPNST tissue fragments. The dissected tissues were finely chopped, rinsed with PBS, and the pieces were seeded onto the surface of a culture T24 flask in a small volume (1 mL) of Dulbecco's modified Eagle's complete medium (DMEM) supplemented with a high concentration (40%) of heat-treated fetal bovine serum (FBS), 2 mM glutamine, non-essential amino acids, 2.5 mm sodium pyruvate, 100 U/mL penicillin and 100 mg/mL streptomycin. After an overnight incubation at 37℃, the medium volume was made up to 5 mL and then changed weekly until a substantial outgrowth of cells was observed. Cells were then grown in DMEM media supplemented with 10% heat-treated FBS.
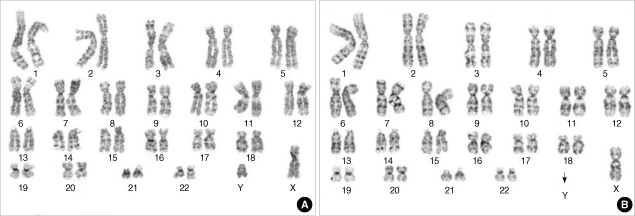
Metaphase cells were harvested and G-banding analyses were carried out using the cultured cells of 5 passages. Cytogenetic analyses were performed on GTG-banded metaphase spreads prepared from three types of fibroblast cells from the NF1 patient. The karyotypes were described in accordance with ISCN (2009). Chromosome analyses were done in 50 metaphases for each sample with a resolution of 450 bands. Representative GTG-banded karyotypes of 50 metaphases are shown in Fig. 2. Normal karyotypes were observed in both normal and benign tissue cultured cells (Fig. 2A), but abnormal karyotype with a mosaic loss of the Y chromosome was detected in the malignant tissue cultured cells (Fig. 2B). This type of Y chromosome loss was detected in approximately 56% of the counted cells (28/50). These G-banding study results in primary tissue cultured cells reproduced the CGH array findings in the same tissues. The karyotype for the malignant cells from MPNST tissue revealed 45,X, -Y[28]/46, XY[22].
Fig. 2.
GTG-banded karyotypes of the benign and malignant fibroblast cells from a NF1 patient. (A) Normal karyotype, 46,XY, was detected in metaphases of the benign cells. (B) Abnormal karyotype of loss of Y chromosome, 45,X,-Y, was detected in metaphases of the malignant cells. Arrow indicates where loss occurred in the Y chromosome.
DISCUSSION
NF1 is notable for the malignant transformation of normal and/or benign tumor tissues to malignant peripheral nerve sheet tumors (MPNSTs) (3). Three different pathological phenotypes of tissues, normal, benign and malignant, may exist within one individual despite of an identical germ line mutation in the NF1 gene, supporting the two-hit hypothesis that an additional NF1 loss is an independent, somatic event (9). Studies on the somatic loss of heterozygosity (LOH) in NF1 showed that about 20% of dermal neurofibromas, 40% of plexiform neurofibromas, and 60% of MPNSTs have a LOH either at the NF1 locus or at 17q (5, 10).
The molecular mechanisms potentially required for the full transformation of benign neurofibromas into MPNSTs are poorly understood. Loss of neurofibromin function by bi-allelic inactivation of NF1 may be necessary for benign neurofibroma formation, but is not sufficient for the transformation of neurofibromas to MPNSTs, suggesting that other genetic alterations or epigenetic events must occur in benign tumors for the malignant transformations in NF1 patients. At the gene level, alterations like mutations and/or gene expression changes in other genes including CDKN2A/p14ARF/p15INK4b/p16INK4a, CDKN1B/p27KI11, RB, TP53, PTEN, EGFR, FRAP1 (mTOR), TSC2, TGF-β, HGF-α, TNXB, and TNC, have been identified in MPNSTs (6, 11). In the chromosomal level, several CGH studies of NF1-associated and sporadic MPNSTs reported the existence of gains and/or losses of genetic materials in chromosomes, 4q, 7, 8q, 15q, 17p, 17q, 19, 22q, and X (7, 12, 13). Although no previous studies have reported common patterns of chromosomal aberrations in NF1, the most frequent genomic imbalances in NF-1 associated MPNSTs were detected in chromosome 17q (7).
In our previous study, we reported the results of a gene expression comparison study of a 24-yr old patient with NF1 (6). A whole gene expression comparison study was carried out in normal, benign and malignant tissues and a total of 20 genes were identified showing clear differences in expression patterns among those tissues. Recent studies regarding chromosomal aberrations in NF1 led to this study in the chromosomal level of the same patient. Here, we performed molecular cytogenetic analysis using samples of the same normal, benign and malignant tissues from the patient and also performed cytogenetic analysis using the primary cultured cells from those tissues. Initially, a comparison study was carried out between tissue types using a CGH array. High-resolution CGH arrays are a powerful tool for the detection of genomic alterations, including gene copy number changes and chromosome deletions and duplications (8). Recent studies have identified a gain of a 550 kb segment at 7q, loss of 2.5 Mb at 17q11.2, and duplications in the NF1 locus at 17q11 through CGH array analysis (14). Using a CGH array, we identified the loss of the Y chromosome in the malignant tissue of a patient with NF1. No genetic alterations were detected at the NF1 locus on 17q. This result was supported by G-banding analysis of cultured cells. Karyotype results showed a mosaic loss in the Y chromosome of the malignant cells, but not in the normal and benign cells, suggesting that the somatic loss of the Y chromosome in this patient may be associated with the malignant transformation of benign neurofibromas to MPNSTs. In this study, Y chromosome loss was first detected through CGH array in MPNST tissue and confirmed by cytogenetic analysis in cultured cells from MPNST tissue. This ruled out the possibility that the Y chromosome loss occurred during cell culture by chance.
Multiple studies have reported that loss of the Y chromosome is a normal age-related phenomenon (15). The likelihood of Y chromosome loss increased significantly in normal males after the age of 70. In our case study, the normal age-related Y chromosome loss is less relevant as the NF1 patient is in his mid-twenties. In addition, Y chromosome loss is frequently observed in some types of tumors such as prostate cancer, pancreatic cancer, squamous cell carcinoma of the head and neck, acute leukemia, hepatocellular carcinoma, and kaposi's sarcoma (16, 17). A study regarding the significance of Y chromosome loss in hematologic diseases reported that the institutional incidence of Y chromosome loss was ~10% of hematologic disease groups and the Y loss is frequently seen as mosaicism with a normal (46,XY) clone (18). Our case had a Y chromosome loss with mosaicism in 56% of the counted cells. The molecular mechanisms of the loss of Y chromosome in these tumors remain unclear. Several cancer related genes have been found to be located on the Y chromosome at Yp, TSPY (Y-encoded testis-specific gene), Yq, XKRY (XK-related protein on Y chromosome), PRY (PTPBL-related protein on Y), RRM (RNA recognition motif), YRRM2 (Y chromosome RNA recognition motif 2), and CDY1 (Chromodomain on Y chromosome) (19). Although male predominance has been reported in the NF1 patients with tibial pseudarthrosis (20), it is not clear whether these genes are associated with malignant transformation of benign neurofibromas to MPNSTs in this case. Further studies are necessary to elucidate the relationship between Y chromosome-specific cancer related genes and tumor progression of NF1.
To elucidate the mechanisms for the malignant transformation of NF1, we previously performed a comparison study at the gene level in histopathologically different tissues of a Korean patient with NF1 (6), and in the present study we carried out comparison study on the genomic and chromosomal levels in the same patient. As a result, we have found the mosaic loss of the Y chromosome in MPNST tissues and cells of the patient. This is the first reported case of Y chromosome loss in NF1. Considering Y chromosome loss has been associated with some types of tumors (16, 17), this result strongly suggests that the somatic loss of the Y chromosome may have caused the transformation of benign tumors to MPNSTs in this patient. Although we are reporting on one case, our data may provide insight into improving the understanding the underlying mechanisms of somatic tumor progression of NF1 on the chromosomal level.
Footnotes
This work was supported by a grant (KRF-2006-331-E00029) from the Korea Research Foundation (MOEHRD, Basic Research Promotion Fund) and a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (A050234).
References
- 1.Savar A, Cestari DM. Neurofibromatosis type I: genetics and clinical manifestations. Semin Ophthalmol. 2008;23:45–51. doi: 10.1080/08820530701745223. [DOI] [PubMed] [Google Scholar]
- 2.Huson SM. Neurofibromatosis 1: a clinical and genetic overview. In: Huson SM, Hughes RAC, editors. The neurofibromatosis. London: Chapman and Hall Medical; 1994. pp. 160–203. [Google Scholar]
- 3.Evans DG, Baser ME, McGaughran J, Sharif S, Howard E, Moran A. Malignant peripheral nerve sheath tumours in neurofibromatosis 1. J Med Genet. 2002;39:311–314. doi: 10.1136/jmg.39.5.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brunetti-Pierri N, Grange DK, Ou Z, Peiffer DA, Peacock SK, Cooper ML, Eng PA, Lalani SR, Chinault AC, Gunderson KL, Craigen WJ, Cheung SW. Characterization of de novo microdeletions involving 17q11.2q12 identified through chromosomal comparative genomic hybridization. Clin Genet. 2007;72:411–419. doi: 10.1111/j.1399-0004.2007.00896.x. [DOI] [PubMed] [Google Scholar]
- 5.Legius E, Marchuk DA, Collins FS, Glover TW. Somatic deletion of the neurofibromatosis type 1 gene in a neurofibrosarcoma supports a tumour suppressor gene hypothesis. Nat Genet. 1993;3:122–126. doi: 10.1038/ng0293-122. [DOI] [PubMed] [Google Scholar]
- 6.Jeong SY, Han JH, Park YY, Kim HJ. Identification of differentially expressed genes related to NF1-associated malignant transformation from a patient with neurofibromatosis type 1. Genes and Genomics. 2008;30:407–418. [Google Scholar]
- 7.Koga T, Iwasaki H, Ishiguro M, Matsuzaki A, Kikuchi M. Frequent genomic imbalances in chromosomes 17, 19, and 22q in peripheral nerve sheath tumours detected by comparative genomic hybridization analysis. J Pathol. 2002;197:98–107. doi: 10.1002/path.1101. [DOI] [PubMed] [Google Scholar]
- 8.Yano S, Matsuyama H, Matsuda K, Matsumoto H, Yoshihiro S, Naito K. Accuracy of an array comparative genomic hybridization (CGH) technique in detecting DNA copy number aberrations: comparison with conventional CGH and loss of heterozygosity analysis in prostate cancer. Cancer Genet Cytogenet. 2004;150:122–127. doi: 10.1016/j.cancergencyto.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Serra E, Puig S, Otero D, Gaona A, Kruyer H, Ars E, Estivill X, Lázaro C. Confirmation of a double-hit model for the NF1 gene in benign neurofibromas. Am J Hum Genet. 1997;61:512–519. doi: 10.1086/515504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Upadhyaya M, Kluwe L, Spurlock G, Monem B, Majounie E, Mantripragada K, Ruggieri M, Chuzhanova N, Evans DG, Ferner R, Thomas N, Guha A, Mautner V. Germline and somatic NF1 gene mutation spectrum in NF1-associated malignant peripheral nerve sheath tumors (MPNSTs) Hum Mutat. 2008;29:74–82. doi: 10.1002/humu.20601. [DOI] [PubMed] [Google Scholar]
- 11.Carroll SL, Ratner N. How does the Schwann cell lineage form tumors in NF1? Glia. 2008;56:1590–1605. doi: 10.1002/glia.20776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lothe RA, Karhu R, Mandahl N, Mertens F, Sauter G, Heim S, Borresen-Dale AL, Kallioneimi OP. Gain of 17q24-qter detected by comparative genomic hybridization in malignant tumors from patients with von Recklinghausen's neurofibromatosis. Cancer Res. 1996;56:4778–4781. [PubMed] [Google Scholar]
- 13.Schmidt H, Taubert H, Meye A, Würl P, Bache M, Bartel F, Holzhausen HJ, Hinze R. Gains in chromosomes 7, 8q, 15q and 17q are characteristic changes in malignant but not in benign peripheral nerve sheath tumors from patients with Recklinghausen's disease. Cancer Lett. 2000;155:181–190. doi: 10.1016/s0304-3835(00)00426-2. [DOI] [PubMed] [Google Scholar]
- 14.Bartsch O, Vlcková Z, Erdogan F, Ullmann R, Novotná D, Spiegel M, Beyer V, Haaf T, Zechner U, Seemanová E. Two independent chromosomal rearrangements, a very small (550 kb) duplication of the 7q subtelomeric region and an atypical 17q11.2 (NF1) microdeletion, in a girl with neurofibromatosis. Cytogenet Genome Res. 2007;119:158–164. doi: 10.1159/000109634. [DOI] [PubMed] [Google Scholar]
- 15.Wong AK, Fang B, Zhang L, Guo X, Lee S, Schreck R. Loss of the Y chromosome: an age-related or clonal phenomenon in acute myelogenous leukemia/myelodysplastic syndrome? Arch Pathol Lab Med. 2008;132:1329–1332. doi: 10.5858/2008-132-1329-LOTYCA. [DOI] [PubMed] [Google Scholar]
- 16.Wallrapp C, Hahnel S, Boeck W, Soder A, Mincheva A, Lichter P, Leder G, Gansauge F, Sorio C, Scarpa A, Gress TM. Loss of the Y chromosome is a frequent chromosomal imbalance in pancreatic cancer and allows differentiation to chronic pancreatitis. Int J Cancer. 2001;91:340–344. doi: 10.1002/1097-0215(200002)9999:9999<::aid-ijc1014>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 17.Kujawski M, Jarmuz M, Rydzanicz M, Szukala K, Wierzbicka M, Grenman R, Golusinski W, Szyfter K. Frequent chromosome Y loss in primary, second primary and metastatic squamous cell carcinomas of the head and neck region. Cancer Lett. 2004;208:95–101. doi: 10.1016/j.canlet.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Wiktor A, Rybicki BA, Piao ZS, Shurafa M, Barthel B, Maeda K, Van Dyke DL. Clinical significance of Y chromosome loss in hematologic disease. Genes Chromosomes Cancer. 2000;27:11–16. [PubMed] [Google Scholar]
- 19.Park SJ, Jeong SY, Kim HJ. Y chromosome loss and other genomic alterations in hepatocellular carcinoma cell lines analyzed by CGH and CGH array. Cancer Genet Cytogenet. 2006;166:56–64. doi: 10.1016/j.cancergencyto.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 20.Stevenson DA, Birch PH, Friedman JM, Viskochil DH, Balestrazzi P, Boni S, Buske A, Korf BR, Niimura M, Pivnick EK, Schorry EK, Short MP, Tenconi R, Tonsgard JH, Carey JC. Descriptive analysis of tibial pseudarthrosis in patients with neurofibromatosis 1. Am J Med Genet. 1999;84:413–419. doi: 10.1002/(sici)1096-8628(19990611)84:5<413::aid-ajmg5>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]