Summary
Various forms of pemphigus have been reported to occur with myasthenia gravis (MG), with and without thymoma. We described two cases of pemphigus vulgaris associated with MG without thymoma.
Case 1. A 44 year-old woman presented with 3 years history of pemphigus vulgaris. Three years later, she developed myasthenic symptoms with elevated level of anti-acetylcholine receptor (AChR) antibodies - 5.2 nmol/L. She was thymectomised and we revealed only hyperplastic thymus.
Case 2. A 64-year-old woman had a general fatigue and intermittent double vision. She was diagnosed as MG three years later. Two months before she diagnosed as MG, she had pruritic erythematous, erosive and bullous lesions on her body and extremities.
Oral prednisolon, pyridostigmine bromide and azathioprine or cyclophosphamide didn`t adequately control MG and pemphigus in our patients, so they received intravenous immunoglobulins of 0.4 g/kg for 5 consecutive days. After that therapy, our patients markedly improved.
Conclusion: The precise pathological mechanisms of the association between pemphigus and MG are not fully understood. The thymus has been suggested to be a possible common origin of autoimmune response in these disorders.
Keywords: Myasthenia gravis, pemphigus vulgaris, intravenous immunoglobulins
Case report
Case 1. A 44 year-old woman presented with 3 years history of pemphigus vulgaris (Fig. 1 A). She was treated with corticosteroids and cyclophosphamid without adequate control of the pemphigus. She developed a general fatigue and difficulty in climbing stairs, extraocular muscles weakness with intermittent blurred vision, and deterioration of symptoms with daily activity (Fig. 1 B). Serologic studies showed positive antinuclear antibody (1:40) and antibodies to acetylcholine receptor (AChR) (5.2 nmol/L, normal value < 0,2 nmol/L). The patient underwent thymectomy and the pathology revealed thymus hyperplasia. She was treated with pyridostigmine bromide (120-180 mg/daily), cyclophosphamide (100 mg/daily) and with intravenous immunoglobulin (IVIG). IVIG was administered at a dose of 0.4 g/kg/day for 5 consecutive days followed with long term IVIG with a single doses of 0.4 g/kg every 6 weeks for one year. This therapeutic approach resulted in a stable remission of both diseases.
Figure 1.
A - Skin lesions typical for pemphigus vulgaris were observed on the skin of the leg. B - A mild weakness of the facial muscles was present at voluntary contraction.
Case 2. A 61-year-old woman developed general fatigue and intermittent double vision. Her MG was recognized three years later when she was 64, and two months before she experienced pruritic erythematous, erosive and bullous lesions of the skin over her body and extremities. Neurological and dermatological examination confirmed generalized MG and pemphigus vulgaris (Fig. 2 A-B). At the admission her MG worsened dramatically and she had to be admitted in an intensive care unit. Anti-AChR antibodies were positive in a high concentration (12.4 nmol/L). A chest computerized tomography scan revealed no significant thymus pathology and it did not require thymectomy. Oral prednisolon (60 mg/daily), pyridostigmine (240-360 mg/daily), and azathioprine (150 mg/daily) were not sufficient to control MG and pemphigus. Additional therapy included IVIG of 0.4 g/kg/day for 5 consecutive days followed with long term IVIG with a single dose of 0.4 g/kg every 6 weeks for six months. After the last IVIG infusion the patient reached the stable clinical remission of both diseases.
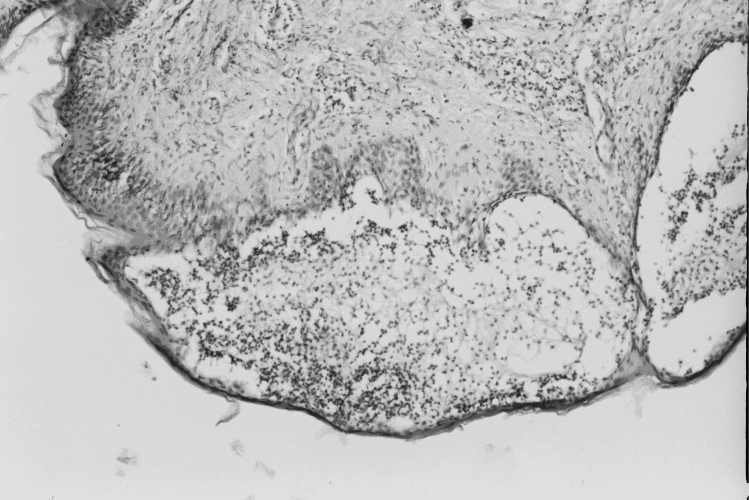
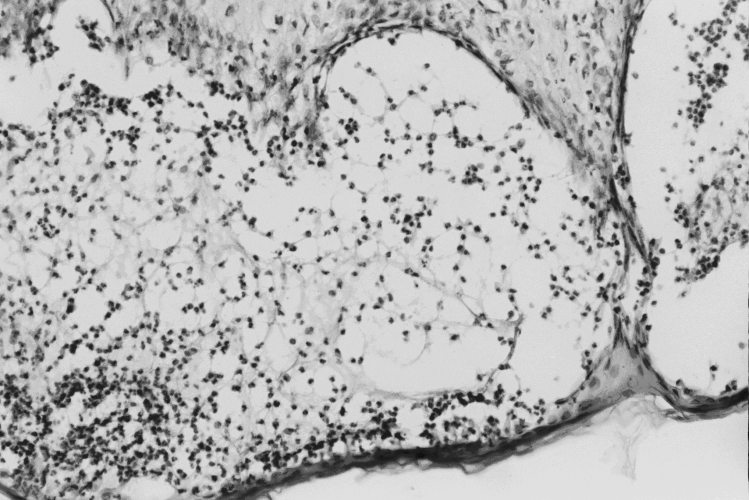
Figure 2.
A-B. Histopathology findings of pemphigus vulgaris.
Suprabasal intraepidermal blister, subtle spongiosis with no marked evidence of acantholysis, at the edge of the blister is focal collections of eosinophils and lymphocytes. In the papillary dermis scattered lymphocytes and eosinophils are present. This appearance is known as eosinophilic spongiosis.
Discussion
MG is an autoimmune disease characterized by an abnormal fatiguability and weakness of the skeletal muscles. The majority of patients have anti-AChR antibodies which cause the postsynaptic block of the neuromuscular transmission. Various autoimmune diseases have been reported to be associated with MG, such as dysfunction of a thyroid gland, rheumatoid arthritis, systemic lupus erythematosus (SLE), Sjogren`s syndrome and several other disorders. It has been reported that vitiligo, alopecia totalis or areata, pemphigus vulgaris or pemphigus foliaceus may occasionally be associated with MG (1–3). In the first of our two patients, MG started first while in the second patient pemphigus developed 3 years before MG. In both patients the diagnosis of the both disease was done at the same time. The precise pathological mechanism of the association between pemphigus and MG is not fully understood. The thymus has been suggested to be a possible common origin of an autoimmune response to different antigens. The thymus contains myoid cells and Hassall`s corpuscles, composed of epithelial cells which are also the constituent of the skin. It could explain the possible autoimmune reaction to the cross-reactive antigens of both tissues (4).
Oral prednisolon, pyridostigmine bromide and azathioprine or cyclophosphamide were not sufficient in the treatment of MG and pemphigus in our patients (5). That was the reason for administration of IVIG therapy.
Our experience with IVIG therapy in two patients with MG associated with pemphigus vulgaris was positive and suggest that this combination of diseases could not be effectively treated by standard immunosuppressive therapy but deserves long term IVIG treatment.
References
- 1. Huh WK, Tada J, Fujimoto W, et al. Thyroid gland tumor, pemphigus foliaceus and myasthenia gravis in the daughter of a woman with myasthenia gravis. Clinical & Experimental Dermatology 2001;26:504-7. [DOI] [PubMed] [Google Scholar]
- 2. Maize JC, Dobson RL, Ptovost TT. Pemphigus and myasthenia gravis. Arch Dermatol 1975;111:1334-9. [PubMed] [Google Scholar]
- 3. Shere Y, Bar-Dayan Y, Shoenfeld Y. Thymoma thymic hyperplasia, thymectomy and autoimmune diseases. Int J Oncol 1997;10:939-43. [DOI] [PubMed] [Google Scholar]
- 4. Patten SF, Dijkstra JWE. Review associations of pemphigus and autoimmune disease with malignancy or thymoma. Int J Dermatol 1994;33:836-42. [DOI] [PubMed] [Google Scholar]
- 5. Grando SA. New approaches to the treatment of pemphigus. J Investig Dermatol Symp Proc 2004;9:84-91. [DOI] [PubMed] [Google Scholar]