Abstract
Risky sexual behavior among youth living with HIV (YLH) must be addressed to prevent the spread of the disease. The purpose of the current study was to investigate factors associated with condom use in a multi-site sample of YLH (ages 16-24). Baseline assessments were conducted with 186 YLH using a computer assisted personal interviewing (CAPI) method. Path analysis suggested that condom use was directly predicted by motivational readiness and self-efficacy for safer sex. Interventions that promote self-efficacy and motivational readiness through a variety of mechanisms may be useful in understanding and conceptualizing sexual risk behavior in YLH. However, further predictors must be studied to account for more variance.
Keywords: HIV, Adolescents, Young Adults, Condom Use, Sexual Risk
Young people between the ages of 13 to 24 are at persistent risk for HIV infection in the United States (CDC, 2006). Young adulthood is a period characterized by experimentation, including engagement in risky behaviors (e.g., substance use and sexual behavior) (Moore & Parsons, 2000). Most young adults are sexually active, with the highest rates of sexual activity reported among youth of color (Park, Mulye, Adams, Brindis, & Irwin, 2006). The prevalence of sexually transmitted infections (STIs), especially chlamydia and gonorrhea, peak in young adulthood and are highest among youth of color (CDC, 2003).
Risky sexual behavior among youth living with HIV (YLH) must be addressed to prevent the spread of the disease. Learning that one is HIV infected presents the youth with the challenge of changing their risky sexual behavior. However, this may be difficult for some youth. Research with YLH has found high rates of sexual risk behaviors (Hein, Dell, Futterman, Rotheram-Borus, & Shaffer, 1992; Murphy et al., 2001; Naar-King et al, 2006a; Rotheram-Borus et al., 1997). Specifically, Vermund and colleagues (2001) found high rates of STIs in HIV-infected adolescents in care settings in the Reaching for Excellence in Adolescent Care and Health (REACH) study (aged 12-18). However, there have only been a few multi-site studies describing sexual risk behaviors of YLH that represent the demographics of the epidemic and the adolescent clinics providing treatment to this group (minority females and men who have sex with men; adolescents and young adults) (Comulada et al., 2003; Rotheram-Borus et al., 2004).
While factors associated with sexual risk behavior among HIV-infected adults has received much attention (Heckman, Kelly, & Somiai, 1998; Kalichman, 1999; Reilly & Woo, 2001; Rosser, Gobby, & Carr, 1999), the research literature is sparse for YLH. Emotional distress has been associated with risky sexual behavior in YLH (Murphy, et al., 2001; Stiffman, Doré, Earls, & Cunningham; 1992). Stein and colleagues (2005) found that lower self-esteem predicted sexual risk behavior in HIV-infected males (ages 15-24) and several other psychosocial factors (i.e., coping style, peer norms, emotional distress, self-esteem, and social support) indirectly predicted sexual risk behavior. This study included only males, and thus, may not apply to the broader population of young men and women in adolescent HIV clinics.
Given the literature on the sexual risk behaviors of YLH is in its infancy, a theoretical framework for understanding risky behaviors in this population is necessary to guide intervention research. The Transtheoretical Model (TTM) provides an integrative approach to understanding the progression towards health behavior change (Prochaska et al., 1994). The TTM is not meant to be an all encompassing theory of behavior, but rather a framework to organize social cognitive constructs associated with behavior change (Prochaska, 2006). The framework includes a continuum of motivational readiness to change and highlights the role of self-efficacy. The TTM has received empirical support in the areas of alcohol and other drug abuse in high-risk adolescents (Migneault, Pallonen, & Velicer, 1997; Harlow et al., 1999) and substance use in YLH (Naar-King et al., 2006b). The TTM has also received empirical support in the area risky sex among YLH with hemophilia (Schultz, Butler, McKernan, Boelson, 2001).
Naar-King et al. (2006a) tested a model of TTM variables (motivational readiness and self-efficacy) and psychosocial variables (emotional distress and social support) to investigate condom use in 60 YLH (ages 16-25). Self-efficacy mediated the relationship between motivational readiness to change and condom use. General social support and emotional distress were not significantly related to condom use, motivational readiness, or self-efficacy, although social support specific to condom use was associated with condom use. It was also noted that YLH engaging in substance use (i.e., alcohol and marijuana) reported more unprotected sex acts. This study involved a single site and small sample size, and did not investigate decisional balance (weighing the pros and cons of behavior), an important factor also associated with movement in the TTM. Finally, motivational readiness was measured by a stage algorithm. Recent literature has supported arguments against discrete stages, in favor of a more continuous cognitive process (Littell & Girvin, 2002; Sutton, 2001; West, 2005).
The purpose of the current study was to investigate the social-cognitive factors associated with condom use, using the TTM as a framework, in a multi-site sample of YLH. We hypothesized that lower motivational readiness (continuous process as opposed to discrete stages), self-efficacy for safer sex, and pros for using condoms (decisional balance) would be associated with higher rates of unprotected intercourse. We also hypothesized that lower levels of these social cognitive variables would be predicted by lower social support specific for using condoms and higher levels of emotional distress. Finally, we hypothesized that lower rates of substance use would be associated with fewer unprotected sex acts.
METHOD
PARTICIPANTS
This investigation was based on baseline data from YLH who were participants in a randomized clinical trial. Youth were recruited from four Adolescent Trials Network (ATN) sites, located in Fort Lauderdale, FL, Philadelphia, PA, Baltimore, MD, and Los Angeles, CA, and one non-ATN site located in Detroit, MI. All five sites offered comprehensive, multidisciplinary care including social work and case management services and access to mental health services. Inclusion criteria included HIV+ status, ages 16 to 24, and ability to complete questionnaires in English. Because the study targeted high-risk YLH, inclusion criteria included having engaged in at least one of three behaviors (i.e., sexual risk, substance use, or currently being prescribed antiretroviral medications) and at least one of these behaviors had to be at the problem level. Problem level sexual risk behavior involved at least one unprotected sex act in the previous three months; problem level alcohol or illicit drug use was based on an adolescent medicine screener (CRAFFT: Car, Relax, Alone, Forget, Friends, and Trouble; Knight et al., 1999); and problem level medication non-adherence was based on a self-report of less than 90% adherence in the last month. Youth perceived to have an active thought disorder were excluded due to an inability to complete questionnaires.
Across all five sites, there were only 10 youths who refused to be screened for eligibility. Of the 375 participants who were screened for the study, 205 participants enrolled, 151 were not eligible (largely due to the lack of problem level behavior), 15 refused to enroll after being screened (i.e., ‘too busy, ‘not interested’), and 4 were lost to follow-up. Of the 205 participants enrolled in the study, 19 did not complete baseline data collections and were removed from this study. The current sample consisted of 186 participants.
PROCEDURES
The protocol was approved by each site’s Institutional Review Board and a certificate of confidentiality was obtained from the National Institutes of Health. At all five sites, participants were approached at the time of a regularly scheduled HIV clinic visit or at attendance during supportive activities. In addition, participants were referred to the study by primary care providers, case managers, advocates, outreach workers, and peers. Participants were required to provide written documentation of seropositivity. A general description of the study and the overall amount of time required was explained to potential participants by their clinic staff. When youth displayed an interest in the study, a research assistant obtained verbal consent prior to administering the screening interview. Upon completion of the screening interview and determination of eligibility, written informed consent was obtained prior to study enrollment; a waiver of parental consent was permitted for youth under age 18. After written consent was obtained, participants completed the baseline assessment. Youth had to complete the baseline assessment within 30 days of screener completion using a computer assisted personal interviewing (CAPI) method via an internet based application. Youth were assured that their responses would be kept confidential from members of the HIV clinic team. Responses to CAPI questions were entered into the computer by the research interviewer in a confidential manner. Once entered, all responses were anonymous and no personal identifying information was recorded during the computer session. Participants received $30 compensation for their time to complete the baseline interview. Transportation, snacks, and childcare were available to participants. Unless specified below, all measures for the present analysis asked about the youth’s status on the day of the assessment.
MEASURES
Condom use
Condom use was measured by a screener question inquiring about unprotected sexual intercourse. Youth were asked to respond “yes” or “no” to the question, “Has the participant had sexual intercourse without a condom (insertive anal, receptive anal, or vaginal) in the last 3 months?” A response of “yes” indicated sexual risk behavior.
Motivational readiness
An item from Rollnick’s Readiness Ruler (Stott, Rollnick, Rees, & Pill, 1995) was administered as a continuous measure of stage movement. Youth marked their motivational readiness to the question, “How ready are you to use condoms for sexual intercourse (anal and/or vaginal)” on a 10-point Likert scale ranging from “not ready to change” to “trying to change”. This measure has been recommended for use by clinicians to determine motivational readiness in HIV care (Cicatelli Associates, Inc. & New York/New Jersey AETC, 2003).
Self-efficacy for safer sex
Self-efficacy was measured by a combination of confidence and temptation items. Youth completed 3 items that assessed confidence to use condoms during intercourse (e.g., How sure are you that you could use condoms for sexual intercourse?) (Naar-King et al., 2006a, 2006b). Items are rated on a 5-point Likert scale ranging from “very sure I cannot” to “very sure I can.” The level of temptation to engage in sex without condom was assessed across 18 different situations (e.g., How tempted are you to have unprotected sex when you are really attracted to your partner?) (Parsons, Halkitis, Bimbi, & Borkowski, 2000; Parsons, Halkitis, Wolitski, & Gomez, 2003). Items are rated on a 5-point Likert scale ranging from “not at all” to “extremely.” A mean composite score was calculated for the 21 items and used in the analysis. Scores were reverse coded so that higher values indicate greater self-efficacy in one’s ability to resist temptation and to use condoms. Internal consistency (Cronbach’s alpha) for the 21 items was .95.
Decisional balance
The HIV and Safer Sex Decisional Balance Scale (Prochaska et al., 1994) was used to measure individuals’ perceived balance between positive and negative outcomes for using condoms. A balance composite score was used in analysis. This score is calculated by first summing the responses to five “pro” items (i.e., Importance of advantages to using condoms) and five “con” items (i.e., Importance of disadvantages to using condoms). Items are rated on a 5-point Likert scale ranging from “not important” to “extremely important.” The balance score is then computed as pros minus cons, with a higher score representing more pros for using condoms. While this measure has not previously been used with YLH, clinicians who worked with youth, including YLH, reviewed the measure for relevancy. Cronbach’s alpha for the pros and cons subscales were .92 and .90, respectively.
Social support for safer sex
Social support for condom use was measured by one item. Youth were asked to rate the following statement, “There are people in my life that are supportive about me using condoms,” on point 5-Likert scale from strongly agree to strongly disagree. This item has been previously associated with self-efficacy in YLH (Naar-King et al., 2006a).
Emotional distress
The Brief Symptom Inventory (BSI) measures nine primary symptom dimensions of physical and mental status (Derogatis & Spencer, 1982). The inventory has been used extensively in medical, psychiatric, and non-patient populations. Internal consistency for the sub-scales (dimensions) ranged from .71 to .85. The BSI is written at a 6th grade reading level. It has been widely used with adolescents, and has an adolescent normative group. The 5-point response scale ranges from “not at all” to “extremely” based on how the respondent felt in the last week. Analyses utilized the Global Symptom Index (GSI).
Substance use
Illicit drug and alcohol use was measured using the Timeline Follow-Back Procedure (TFBP) (Sobell, Brown, Leo, & Sobell, 1987). As part of this measure, participants were asked to report the number of days in the past 30 that they used substances. Alcohol and marijuana were the most commonly used substances. Substances other than alcohol or marijuana were used by only 2% of youth. The total number of days in which alcohol and marijuana were used was utilized in subsequent analyses. Substance use variables were also dichotomized (any alcohol and/or marijuana use vs. no alcohol and/or marijuana use) as this has been shown to significantly relate to unprotected sex in previous research (Naar-King, et al., 2006b).
DATA ANALYSIS
All variables used in analysis have been coded such that higher values indicate higher levels of the construct (e.g., greater motivational readiness, greater feelings of self-efficacy for safe sex). The outcome variable, condom use, is coded as 0 = did not have unprotected sex in the last three months and 1 = had unprotected sex in the last three months.
Prior to analyses, variables were screened for univariate and multivariate outliers. Six univariate outliers (> three standard deviations from the mean) were found for motivational readiness. Two univariate outliers were found for self-efficacy, and two outliers were found for decisional balance. These scores were winsorized (equated to less extreme values). In order to reduce skewness, logarithmic transformations were used on alcohol and marijuana use variables. All other variables were left untransformed to increase interpretability of findings. Scaled variable scores were missing in three cases (less than 1% of all cases for all scaled scores). Because of the limited missing data, mean imputation was used for these three scores. Univariate frequency distributions and means with standard deviations were used to describe categorical and continuous variables, respectively. Bivariate correlations were calculated to determine the associations among demographic and model variables.
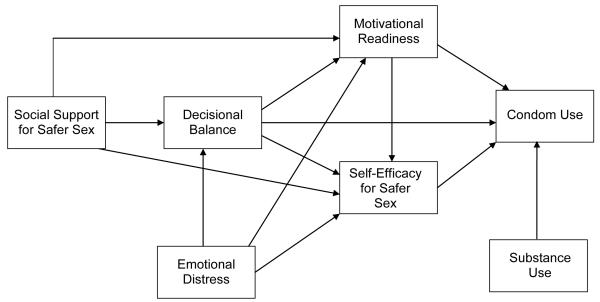
The primary analyses tested the various paths depicted in Figure 1 using path analysis and model-fitting techniques. Path analysis assesses structural relations among observed variables and is particularly appropriate when there are single indicators of each theoretical construct. The proposed path model was tested using LISREL 8.54 (Jöreskog & Sörbom, 2003). Path models were assessed by examining the statistical significance of estimated path coefficients and several statistics indicating goodness of fit for the model as a whole, such as the NFI, CFI, GFI, χ2/df, and RMSEA.
Figure 1.
Conceptual Model.
RESULTS
Descriptive Statistics and Bivariate Analyses
Ages ranged from 16 to 24 (M = 20.5 years). The sample was primarily African American (78%) and approximately half were male (52%). Over half of the sample (57%) identified themselves as heterosexual. The majority of those who did not identify as heterosexual were male (92%). Seventeen percent of youth were perinatally infected and the remainder was behaviorally infected. Table 1 displays sample demographics by site. Statistically significant differences existed between the sites with regards to ethnicity, sexual orientation, gender, and sex without a condom in the past three months.
Table 1.
Sample Demographics by Site.
| Site | N | Percent African American* |
Percent Sexual Minority*+ |
Percent Female* |
Percent Sex Without Condom Past 3 Months* |
Mean income (SD) |
|---|---|---|---|---|---|---|
| Los Angeles | 43 | 48.8 | 48.8 | 37.2 | 78.0 | $639.53 (453.73) |
| Philadelphia | 34 | 91.1 | 64.7 | 44.1 | 44.1 | $603.46 (787.94) |
| Baltimore | 36 | 100.0 | 35.3 | 55.6 | 69.4 | $416.96 (354.75) |
| Fort Lauderdale | 33 | 84.8 | 3.0 | 81.8 | 34.4 | $774.64 (970.92) |
| Detroit | 40 | 97.5 | 60.5 | 25.0 | 44.7 | $494.46 (436.12) |
| Total | 186 | 83.3 | 43.4 | 47.3 | 52.2 | $584.63(625.35) |
Significant difference across sites, p ≤ .05;
Sexual Minority refers to youth who reported their sexual orientation as “bisexual, gay/lesbian, or other.”
Fifty-four percent of the sample (n = 100) reported having unprotected intercourse in the last three months. Three percent of the sample reported that they have never had sex (n=5). Fifty-eight percent of the sample (n = 108) reported already trying to increase their use of condoms, according to the readiness ruler. Over 35% of the sample scored at or above the clinical cut-off for the global symptom index of the Brief Symptom Inventory based on published norms. Demographic characteristics were unassociated with model variables with the exception of age. Age was positively related to emotional distress (r = .38, p < .01), and negatively related to social support for safer sex (r = −.24, p < .01), motivational readiness (r = −.25, p < .01), self-efficacy for safer sex (r = −.15, p < .05), and decisional balance (r = −.15, p < .05).
Means, standard deviations, and Pearson correlations for the constructs used in the current study are presented in Table 2. The correlations with alcohol and marijuana use are based on the log transformations of alcohol and marijuana use data. However, the means and standard deviations are represented as geometric means and standard deviations for interpretability. The correlations displayed in Table 2 show initial support for the relations hypothesized in this study. Condom use was significantly correlated with motivational readiness, self-efficacy for safer sex, and decisional balance. These three variables were correlated with each other. Emotional distress and social support for safer sex (condom use) was significantly correlated with motivational readiness, self-efficacy for safer sex, and decisional balance.
Table 2.
Means, Standard Deviations (SD), and Bivariate Correlations among Model Variables.
| Model variables |
Mean (SD) | Model variables | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Condom Use |
Motivational Readiness |
Self- Efficacy for Safer Sex |
Decisional Balance |
Emotional Distress |
Social Support for Safer Sex |
Alcohol Use |
Marijuana Use |
||
| Condom Use | 0.54 (0.50) | 1.00 | |||||||
| Motivational Readiness |
8.73 (1.93) | −0.26** | 1.00 | ||||||
| Self-Efficacy for Safe Sex |
4.07 (0.90) | −0.29** | 0.34** | 1.00 | |||||
| Decisional Balance |
11.89 (7.59) | −0.20** | 0.28** | 0.47** | 1.00 | ||||
| Emotional Distress |
57.19 (14.48) | 0.08 | −0.22** | −0.39** | −0.26** | 1.00 | |||
| Social Support for Safer Sex |
4.35 (1.01) | −0.11 | 0.27** | 0.27** | 0.26** | −0.14 | 1.00 | ||
| Alcohol Use |
3.07 (4.53) | 0.01 | −0.02 | −0.07 | 0.04 | 0.16* | 0.07 | 1.00 | |
| Marijuana Use |
3.24 (5.96) | −0.004 | −0.12 | −0.12 | −0.20** | 0.26** | −0.06 | 0.20** | 1.00 |
| Any Substance Use |
0.61 (0.49) | 0.01 | −0.10 | −0.11 | −0.09 | 0.30** | −0.02 | 0.60** | 0.53** |
p < .05;
p < .01
Path Analysis
Path analysis was used to assess the relationship between the hypothesized variables and condom use. Both direct and indirect relations were evaluated. The standardized regression weights of the relevant paths were estimated. The overall fit of the model was examined based on widely used goodness of fit indices (Hu & Bentler, 1995). Because the outcome of condom use (i.e., sexual intercourse without a condom in the last three month) was dichotomous, a polychoric correlation matrix and asymptotic covariance matrix was used for analysis. This was employed to reduce any bias caused by the inclusion of an ordinal variable in LISREL (Byrne, 1998). In addition to model variables depicted in Figure 1, age was entered into the model as a covariate. For substance use, the dichotomous variable was used in the analysis (i.e., any alcohol and/or marijuana use vs. no alcohol or marijuana use). Model testing involved assessment of the hypothesized model followed by modifications to improve the overall fit and parsimony.
The hypothesized model depicted in Figure 1 was tested first. This model resulted in a fair fit, χ2(11, N = 186) = 19.78, p = .05, RMSEA = .07 (90% confidence interval = 0.1; .11). Browne and Cudeck (1993) suggest that a RMSEA of .05 indicates a close fit and that values up to .08 represent reasonable errors of approximation in the population. The comparative fit index was .96, the Normed Fit Index was .93, and the Goodness of Fit Index was .97.
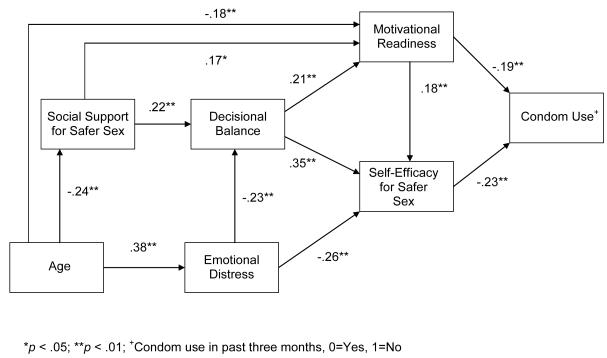
In the interest of parsimony, a final model was estimated with non-significant paths deleted from the originally proposed model. In comparison, the reduced model was significantly different from the first model, χ2diff(2, N = 186) = 12.00, p < 01. The path diagram with standardized solutions for the final, reduced model can be seen in Figure 2. Substance use was eliminated from this model because it was not a significant predictor of condom use. This model resulted in a good fit, χ2(9, N = 186) = 7.78, p = .56, RMSEA = 0.0 (90% confidence interval = 0.0; .05). The comparative fit index was 1.0, the Normed Fit Index was .97, and the Goodness of Fit Index was .99.
Figure 2.
Final Path Model for Sexual Risk
Path coefficients displayed in Figure 2 show that the hypothesized paths were significant in this sample. Condom use was directly predicted by motivational readiness and self-efficacy for safer sex, but not decisional balance. However, decisional balance significantly predicted motivational readiness and self-efficacy for safer sex. The squared multiple correlations (proportion of variance explained by the model) for the final model were as follows: .32 for self-efficacy for safer sex, .11 for decisional balance, .15 for motivational readiness, and .11 condom use. The significance of the mediating variables were evaluated using tests of indirect effects through LISREL (Sobel, 1988). There was an overall significant indirect effect from decisional balance to condom use through self-efficacy for safer sex and through motivational readiness (standardized indirect effect coefficient = −.13, p < .01). The indirect paths through self-efficacy for safer sex and through motivational readiness were each significant (p < .01, p < .05, respectively). The relationship between decisional balance and condom use was fully mediated by self-efficacy for safer sex and motivational readiness in this model. There was a significant indirect path from motivational readiness to condom use through self-efficacy for safer sex (standardized indirect effect coefficient = −.04, p < .05). Additionally, social support for safer sex significantly predicted decisional balance and motivational readiness, but not self-efficacy for safer sex. Emotional distress significantly predicted decisional balance and self-efficacy for safer sex, but not motivational readiness.
DISCUSSION
The current study suggests that several social cognitive factors are associated with condom use in YLH. Youth with greater motivational readiness and self-efficacy for safer sex were more likely to use condoms, indicating that interventions that promote self-efficacy and motivational readiness may be useful in understanding and conceptualizing sexual risk behavior in YLH. These data suggest that interventions that are formulated to increase motivation, perhaps by increasing social support for condom use, and increase self-efficacy, perhaps by increasing decisional balance (pros for condoms), may be beneficial. Motivational Interviewing (MI), a brief client-centered, yet goal-oriented method of communication designed to increase motivation and boost confidence for behavior change while addressing decisional balance concerns (Miller & Rollnick, 2002), may be an effective approach. Studies have begun to suggest that using such an approach may be successful in reducing sexual risk behavior in YLH (Naar-King et al., 2006c), and sexual risk and substance in high-risk youth (Borsari & Carey, 2000; Monti et al., 1999).
Emotional distress was related to social cognitive predictors of condom use. This finding is consistent with findings in the research literature (Murphy, et al., 2001; Stiffman et al., 1992). Knowing more about the emotional problems of YLH may assist in the development of more tailored interventions for this population. Interventions that focus on social networking and the treatment of depression may help to increase social support and reduce emotional distress for youth. It may also be helpful for such interventions to involve a therapeutic component that assists youth with HIV in living with HIV.
Surprisingly, substance use was not predictive of condom use, and thus was eliminated from the final model. The most commonly used substances in this study were alcohol and marijuana, with 43% of youth reporting alcohol use and 37% reporting marijuana use in the last 30 days. Unprotected sexual intercourse appeared to be high for youth who reported using substances and youth who did not. While Murphy and colleagues (2001) found that substance use was associated with sexual risk behavior in YLH; her cohort was younger and predominantly female. The lack of a relationship between alcohol and marijuana use, and condom use in the current study supports previous research that focuses on the types of substances used and the impact on the sexual risk behaviors of those living with HIV (Parsons & Halkitis, 2002; Parsons, Kutnick, Halkitis, Punzalan, & Carbonari, 2005; Purcell, Parsons, Halkitis, Mizuno, & Woods, 2001; Stein et al., 2005). Because of these discrepant findings, further investigation is needed to assess the association between sexual risk behavior and substance use among this population.
Although the final model was a good fit for the data and is consistent with other social cognitive theories of risky behavior (Fisher & Fisher, 2000), the model only accounted for a modest amount of variance in condom use. In contrast, similar model fit to substance use data from the same sample accounted for much more variance (Naar-King, Kolmodin, Parsons, Murphy, & Wright, in press). The model accounted for 41% of the variance in marijuana use and 28% of the variance in alcohol use. Thus, examining additional constructs may help account for more variance in risky sexual behavior. Research literature on adults with HIV and other high risk populations indicate that sensation seeking may be a predictor of sexual risk behavior. Sensation seeking is consistently associated with sexual risk behavior (Dolezal, Meyer-Bahlburg, Remien, & Petkova, 1997; Greene, Krcmar, Walters, Rubin, & Hale, 2000; Hoyle, Fejfar, & Miller, 2000; Kalichman & Cain, 2004; Kalichman, Cain, Zweben, & Swain, 2003), including among HIV+ populations (Parsons & Halkitis, 2002).
Among youth, studies have suggested that peer behaviors and attitudes are related to sexual risk behavior (Boyer et al., 2000; Hart & Peterson, 2004). Ethnic identity issues for African American young men who have sex with men (YMSM) have also been associated with sexual risk behavior (Stokes & Peterson, 1998). Young men who experience negative attitudes from members of their community due to their sexual identity may internalize such attitudes, resulting in low self-esteem, emotional distress, and thus less desire to engage in safer sex practices. Others have highlighted the need for ethnic identity in risk reduction interventions with young women (DiClemente & Wingwood, 1995). While knowledge may not be sufficient for increasing condom use, skills to avoid risk and to negotiate with partners may be lacking in persons living with HIV (Reilly & Woo, 2001). Finally, other interpersonal issues such as insecure attachments may play a role in the sexual risk behavior of persons living with HIV (Ciesla, Roberts, & Hewitt, 2004).
Limitations
YLH entered this study because of problem level risk behaviors; therefore, these participants may not be generalizable to the broader population of YLH. It is also noted that this study was conducted with a clinic-based convenience sample, and may not represent community samples. It is possible that other samples of YLH (e.g., those not in care or those with undiagnosed HIV) may have a higher percentage of youth engaging in sexual risk behavior. Such a sample may also have different substance use patterns, with regard to frequency and types of substances used. Another limitation of the current study is how sexual risk behavior was assessed. This study used self-report to assess condom use in the past three months. There were no biological measures of sexual risk (i.e., STI screens), and no inquiries regarding multiple partners and disclosure of HIV status to partners. Also, the decisional balance measure (i.e., pros and cons for condom use) had never been utilized with YLH. However, clinicians who work with youth, including YLH, reviewed the measure. There were site differences in demographic characteristics, suggesting that single site studies may not generalize to other geographical locations. Multi-site intervention studies will need to control for the effect of site. Finally, these data are cross-sectional, and any directionality of relationships must be examined with longitudinal data. While the current study provides some insight into sexual risk behavior for YLH, more formative research is still needed to understand predictors of sexual risk behavior and to inform interventions for YLH.
ACKNOWLEGEMENT
The Adolescent Trials Network for HIV/AIDS Interventions (ATN) supported this work [U01-HD040533 and U01-HD040474 from the National Institutes of Health through the National Institute of Child Health and Human Development (B. Kapogiannis, S. Lee), with supplemental funding from the National Institutes on Drug Abuse (N. Borek) and Mental Health (P. Brouwers, S. Allison)]. The study was scientifically reviewed by the ATN’s Behavioral Leadership Group. Network, scientific, and logistical support was provided by the ATN Coordinating Center (C. Wilson, C. Partlow) at the University of Alabama at Birmingham. Network operations and data management support was provided by the ATN Data and Operations Center at Westat, Inc. (J. Korelitz, J. Davidson, D. R. Harris). We acknowledge the contribution of the investigators and staff at the following ATN 004 sites that participated in this study: Children’s Diagnostic and Treatment Center (Ana Puga, MD, Esmine Leonard, BSN, Zulma Eysallenne, RN); Children’s Hospital of Los Angeles (Marvin Belzer, MD, Cathy Salata, RN, Diane Tucker, RN, MSN); University of Maryland (Ligia Peralta, MD, Leonel Flores, MD, Esther Collinetti, BA); University of Pennsylvania and the Children’s Hospital of Philadelphia (Bret Rudy, MD, Mary Tanney, MPH, MSN, CPNP, Naini Seth, BSN, Kelly Lannutti, BA); University of Southern California (Andrea Kovacs, M.D.), and Wayne State University Horizons Project (K. Wright, DO, P. Lam, MA, V. Conners, BA). We sincerely thank the youth who participated in this project.
REFERENCES
- Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology. 2000;68:728–733. [PubMed] [Google Scholar]
- Boyer CB, Shafer M, Wibbelsman CJ, Seeberg D, Teitle E, Lovell N. Associations of sociodemographic, psychosocial, and behavioral factors with sexual risk and sexually transmitted diseases in teen clinic patients. The Journal of Adolescent Health. 2000;27(2):102–111. doi: 10.1016/s1054-139x(99)00113-5. [DOI] [PubMed] [Google Scholar]
- Browne MW, Crudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Byrne BM. Structural equation modeling with LISREL, PRELIS, and SIMPLIS: Basic concepts, applications, and programming. Lawrence Erlbaum Associates, Publishers; Mahwah, NJ: 1998. [Google Scholar]
- Center for Disease Control and Prevention (CDC) [Retrieved January 31, 2008];HIV/AIDS among youth. CDC HIV/AIDS Fact Sheet. 2006 June; 2006. from http://www.cdc.gov/hiv/resources/factsheets/youth.htm.
- Center for Disease Control and Prevention (CDC) Youth Risk Behavior Surveillance—United States, 2003. Morbidity and Mortality Weekly Report 2004. 2003;53(SS-2):1–29. [PubMed] [Google Scholar]
- Cicatelli Associates, Inc. New York/New Jersey AETC [Retrieved January 31, 2007];Behavior management in clinical HIV care: Part II secondary prevention of HIV. 2003 from http://www.aids-ed.org.
- Ciesla JA, Roberts JE, Hewitt RG. Adult attachment and high-risk sexual behavior among HIV-positive patients. Journal of Applied Social Psychology. 2004;34(1):108–124. [Google Scholar]
- Comulada WS, Swendeman DT, Rotheram-Borus MJ, Mattes KM, Weiss RE. Use of HAART among young people living with HIV. American Journal of Health Behavior. 2003;27(4):389–400. doi: 10.5993/ajhb.27.4.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L, Spencer P. Brief Symptom Inventory: Administration, scoring, and procedures manual-I. Clinical Psychometric Research; Baltimore, MD: 1982. [Google Scholar]
- DiClemente RJ, Wingwood G. A randomized controlled trial of an HIV sexual risk reduction intervention for young African-American women. Journal of the American Medical Association. 1995;274(16):1271–1276. [PubMed] [Google Scholar]
- Dolezal C, Meyer-Bahlburg HF, Remien RH, Petkova E. Substance use during sex and sensation seeking as predictors of sexual risk behavior among HIV+ and HIV− gay men. AIDS and Behavior. 1997;1(1):19–28. [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention (AIDS prevention and mental health) Kluwer Academic/Plenum Publishers; New York: 2000. pp. 3–48. [Google Scholar]
- Greene K, Krcmar M, Walters LH, Rubin DL, Hale J. and L. Targeting adolescent risk-taking behaviors: The contributions of egocentrism and sensation-seeking. Journal of Adolescence. 2000;23:439–461. doi: 10.1006/jado.2000.0330. [DOI] [PubMed] [Google Scholar]
- Harlow LL, Prochaska JO, Redding CA, Rossi JS, Velicer W, Snow MG. Stages of condom use in a high HIV-risk sample. Psychology & Health. 1999;14:143–157. [Google Scholar]
- Hart T, Peterson JL. Predictors of risky sexual behavior among young African American men who have sex with men. American Journal of Public Health. 2004;94(7):1122–1124. doi: 10.2105/ajph.94.7.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman T, Kelly J, Somiai A. Predictors of continued high-risk sexual behavior in a community sample of persons living with HIV/AIDS. AIDS and Behavior. 1998;2:127–135. [Google Scholar]
- Hein K, Dell R, Futterman D, Rotheram-Borus MJ, Shaffer N. Comparison of HIV+ and HIV− adolescents: Risk factors and psychosocial determinants (1995) Pediatrics. 1992;95(1):96–104. [PubMed] [Google Scholar]
- Hoyle RH, Fejfar MC, Miller JD. Personality and sexual risk taking: A quantitative review. Journal of Personality. 2000;68(6):1204–1231. doi: 10.1111/1467-6494.00132. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural Equation modeling: Concepts, issues, and applications. Sage Publications, Inc.; Thousand Oaks, CA: 1995. pp. 76–99. [Google Scholar]
- Jöreskog K, Sörbom D. LISREL 8.54. Scientific Software International; Chicago, IL: 2003. [Google Scholar]
- Kalichman SC, Cain D. A prospective study of sensation seeking and alcohol use as predictors of sexual risk behaviors among men and women receiving sexually transmitted infection clinic services. Psychology of Addictive Behaviors. 2004;18(4):367–373. doi: 10.1037/0893-164X.18.4.367. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Cain D, Zweben A, Swain G. Sensation seeking, alcohol use, and sexual risk behavior among men receiving services at a clinic for sexually transmitted infections. Journal of Studies on Alcohol. 2003;64(4):564–569. doi: 10.15288/jsa.2003.64.564. [DOI] [PubMed] [Google Scholar]
- Kalichman S. Psychological and social correlates of high-risk sexual behavior among men and women living with HIV/AIDS. AIDS Care. 1999;11(4):415–428. doi: 10.1080/09540129947794. [DOI] [PubMed] [Google Scholar]
- Knight JR, Shrier LA, Bravender TD, Farrell M, Vander Bilt J, Shafer HJ. A new brief screen for adolescent substance abuse. Archives of Pediatric and Adolescent Medicine. 1999;153:591–596. doi: 10.1001/archpedi.153.6.591. [DOI] [PubMed] [Google Scholar]
- Littell JH, Girvin H. Stages of change: A critique. Behavior Modification. 2002;26(2):223–273. doi: 10.1177/0145445502026002006. [DOI] [PubMed] [Google Scholar]
- Migneault JP, Pallonen UE, Velicer WF. Decisional balance and stage of change for adolescent drinking. Addictive Behaviors. 1997;22:339–351. doi: 10.1016/s0306-4603(96)00252-3. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. Guilford; New York: 2002. [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Moore S, Parsons JT. A research agenda for adolescent risk-taking: Where do we go from here? Journal of Adolescence. 2000;23(4):371–376. doi: 10.1006/jado.2000.0325. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Durako SJ, Moscicki A, Vermund SH, Ma Y, Schwarz DF, et al. No change in health risk behaviors over time among HIV infected adolescents in care: Role of psychological distress. Journal of Adolescent Health. 2001;29(S):57–63. doi: 10.1016/s1054-139x(01)00287-7. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Kolmodin K, Parsons J, Murphy D, Wright K. Predictors of substance use in high risk youth living with HIV: Adaptation of the transtheoretical model. AIDS Care. 2009 in press. [Google Scholar]
- Naar-King S, Wright K, Parsons J, Frey M, Templin T, Ondersma S. Transtheoretical Model and condom use in HIV+ youth. Health Psychology. 2006a;25:648–652. doi: 10.1037/0278-6133.25.5.648. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Wright K, Parsons J, Frey M, Templin T, Ondersma S. Transtheoretical model and substance use in HIV+ youth. AIDS Care. 2006b;18:839–845. doi: 10.1080/09540120500467075. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Wright K, Parsons J, Frey M, Templin T, Lam P, Murphy D. Healthy choices: Motivational enhancement therapy for high risk behaviors in HIV-positive youth. AIDS Education and Prevention. 2006c;18(1):1–11. doi: 10.1521/aeap.2006.18.1.1. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Wright K, Parsons J, Frey M, Templin T, Lam P, Murphy D. Healthy choices: Motivational enhancement therapy for high risk behaviors in HIV-positive youth. AIDS Education and Prevention. 2006c;18(1):1–11. doi: 10.1521/aeap.2006.18.1.1. [DOI] [PubMed] [Google Scholar]
- Park MP, Mulye TP, Adams S, Brindis C, Irwin C. The health status of young adults in the United States. Journal of Adolescent Health. 2006;39:305–317. doi: 10.1016/j.jadohealth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Kutnick A, Halkitis PN, Punzalan JC, Carbonari JP. Sexual risk behaviors and substance use among alcohol abusing HIV+ men who have sex with men. Journal of Psychoactive Drugs. 2005;37(1):11–26. doi: 10.1080/02791072.2005.10399746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN, Wolitski RJ, Gomez CA. Correlates of sexual risk behaviors among HIV+ men who have sex with men. AIDS Education and Prevention. 2003;15(5):383–400. doi: 10.1521/aeap.15.6.383.24043. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN. Sexual and drug using practices of HIV+ men who frequent commercial and public sex environments. AIDS Care. 2002;14(6):815–826. doi: 10.1080/0954012021000031886. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN, Bimbi DS, Borkowski T. Perceptions of the benefits and costs associated with condom se and unprotected sex among late adolescent college students. Journal of Adolescence. 2000;23:377–391. doi: 10.1006/jado.2000.0326. [DOI] [PubMed] [Google Scholar]
- Prochaska JO. Moving beyond the transtheoretical model. Addiction. 2006;101:768–778. doi: 10.1111/j.1360-0443.2006.01404.x. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychology. 1994;13:39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Parsons JT, Halkitis PN, Mizuno Y, Woods W. Relationship of substance use by HIV-seropositive men who have sex with men and unprotected anal intercourse with HIV-negative and unknown serostatus partners. Journal of Substance Abuse. 2001;13(1-2):185–200. doi: 10.1016/s0899-3289(01)00072-4. [DOI] [PubMed] [Google Scholar]
- Reilly T, Woo G. Predictors of high-risk sexual behavior among people living with HIV/AIDS. AIDS and Behavior. 2001;5(3):205–217. [Google Scholar]
- Rosser B, Gobby J, Carr W. The unsafe sexual behavior of persons living with HIV/AIDS: An empirical approach to developing new HIV prevention intervention targeting HIV-positive persons. Journal of Sex Education and Therapy. 1999;27(167):18–28. [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, Comulada WS, Weiss RE, Lee M, Lightfoot M. Prevention for substance-using HIV-positive young people: Telephone and in-person delivery. Journal of Acquired Immune Deficiency Syndromes. 2004;37:S68–77. doi: 10.1097/01.qai.0000140604.57478.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Murphy DA, Coleman CL, Kennedy M, Reid HM, Cline TR, et al. Risk acts, health care, and medical adherence among HIV+ youths in care over time. AIDS and Behavior. 1997;1(1):43–52. [Google Scholar]
- Schultz JR, Butler RB, McKernan L, Boelson R. Developing theory-based risk reduction interventions for HIV-positive young people with hemophilia. Hemophilia. 2001;7:64–71. doi: 10.1046/j.1365-2516.2001.00458.x. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Direct and indirect effect in linear structural equation models. In: Long JS, editor. Common problems/proper solutions: Avoiding error in quantitative research. Sage; Beverly Hills, CA: 1988. pp. 46–64. [Google Scholar]
- Sobell LC, Brown J, Leo GI, Sobell MB. The reliability of the Alcohol Timeline Followback when administered by telephone and computer. Drug and Alcohol Dependence. 1987;42:49–54. doi: 10.1016/0376-8716(96)01263-x. [DOI] [PubMed] [Google Scholar]
- Stein JA, Rotheram-Borus MJ, Swendeman D, Milburn NG. Predictors of sexual transmission risk behaviors among HIV-positive young men. AIDS Care. 2005;17(4):433–442. doi: 10.1080/09540120412331291724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiffman AR, Doré P, Earls F, Cunningham R. The influence of mental health problems on AIDS-related risk behaviors in young adults. The Journal of Nervous and Mental Disease. 1992;180(5):314–20. doi: 10.1097/00005053-199205000-00005. [DOI] [PubMed] [Google Scholar]
- Stokes JP, Peterson JL. Homophobia, self-esteem and risk for HIV among African American men who have sex with men. AIDS Education and Prevention. 1998;10(3):278–292. [PubMed] [Google Scholar]
- Stott NC, Rollnick S, Rees MR, Pill RM. Innovation in clinical method: diabetes care and negotiating skills. Family Practice. 1995;12:413–418. doi: 10.1093/fampra/12.4.413. [DOI] [PubMed] [Google Scholar]
- Sutton S. Back to the drawing board? A review of applications of the transtheoretical model to substance use. Addiction. 2001;96:175–186. doi: 10.1046/j.1360-0443.2001.96117513.x. [DOI] [PubMed] [Google Scholar]
- Vermund SH, Wilson CM, Rogers A, Partlow C, Moscicki AB. Sexually transmitted infections among HIV infected and HIV uninfected high-risk youth in the REACH study. Journal of Adolescent Health. 2001;29S:49–56. doi: 10.1016/s1054-139x(01)00296-8. [DOI] [PubMed] [Google Scholar]
- West R. Time for a change: putting the transtheoretical (stages of change) model to rest. Addiction. 2005;100:1036–1039. doi: 10.1111/j.1360-0443.2005.01139.x. [DOI] [PubMed] [Google Scholar]