Abstract
Open radical prostatectomy (ORP) is the reference standard for the surgical management of localized prostate cancer. With wider availability of minimally invasive radical prostatectomy techniques, there is a debate regarding the standard treatment of the management of localized prostate cancer. Therefore, we reviewed the current status of laparoscopic radical prostatectomy (LRP) and robotic-assisted laparoscopic radical prostatectomy (RALRP) as compared with ORP. Because no prospective, randomized trials comparing the different techniques have been performed, outcomes must be assessed from published series by centers that focus on ORP, LRP, and RALRP. Aside from reducing the amount of blood loss, current data suggest that the most significant outcomes (cure, continence, and potency) are no better with LRP or RALRP than with conventional ORP. Therefore, in experienced hands, ORP remains the gold standard procedure. However, there is a trend toward consistently better outcomes following RALRP in comparison with LRP. In the end, individual patient outcomes can be maximized by choosing the best modality based on the patient’s comorbid medical conditions, cancer characteristics, and surgeon experience. Future studies are needed to further investigate long-term cancer control as well as functional outcomes for RALRP series.
Key words: Laparoscopy, Prostatectomy, Prostatic neoplasms, Robotics
In the United States, prostate cancer accounts for approximately one-third of cancer in men and, as of 2004, 86% of diagnosed prostate cancer was localized.1 It has been estimated that the annual incidence of prostate cancer in the United States will rise from 192,280 in 2009 to 384,000 in the year 2025 and to 452,000 in the year 2045.2 Men with clinically localized prostate cancer confront a variety of treatment choices that include but are not limited to watchful waiting; active surveillance with deferred treatment if the cancer shows signs of local growth; brachytherapy, external beam irradiation therapy, or both, with or without hormonal therapy; cryotherapy; high-intensity focused ultrasound; and radical prostatectomy (RP). Open radical prostatectomy (ORP) has been considered the gold standard for the surgical treatment of localized prostate cancer; however, laparoscopic and robotic-assisted prostatectomies have become standards of care at many centers worldwide.
Realizing the need for a systematic analysis of the literature regarding available methods of treatment of locally confined tumors, the American Urological Association (AUA) assembled the Prostate Cancer Clinical Guidelines Panel in 1989. The AUA convened this panel again in 1995 to explore the literature regarding available methods for treating locally confined prostate cancer, as well as to make practice policy recommendations based on the treatment outcomes data.3 The panel found the outcomes data inadequate for valid comparisons of treatments. As a result, in making its recommendations, the panel presented treatment alternatives as options, identifying the advantages and disadvantages of each, and recommended as a standard “that patients with newly diagnosed, clinically localized prostate cancer should be informed of all commonly accepted treatment options.”3
Although there have been several modifications and improvements in technique, the mainstay for the surgical treatment of prostate cancer has been RP since Hugh Hampton Young performed the first perineal prostatectomy in 1905.4 However, the inconsistency in ORP outcomes, the establishment of laparoscopy in the urological armamentarium, and the growing success of less invasive treatment alternatives (such as brachytherapy in prostate cancer), accelerated the development of laparoscopic radical prostatectomy (LRP) in 1991.1 In addition to the conventional advantages of minimally invasive surgery, the LRP technique was believed to reduce blood loss and shorten operating room times and hospital stays, while attaining oncologic and functional outcomes similar to ORP. Despite these advantages, LRP proved to be a complex procedure constrained by 2-dimensional visualization, a counterintuitive nature that led to a steep learning curve in addition to limited ergonomics.5 Moreover, LRP requires advanced laparoscopic skills to maneuver rigid laparoscopic instruments that are fixed at the skin level by trocars, resulting in an overall reduction in degrees of freedom for dissection and suturing as compared with open surgery.
To overcome some of these limitations, a robotic system was introduced to facilitate a laparoscopic approach to radical prostatectomy. In early 2000, the first robot-assisted laparoscopic radical prostatectomy (RALRP) was performed using the da Vinci® Surgical System (Intuitive Surgical, Sunnyvale, CA).1 Because this technology provides a 3-dimensional view of the operative field and jointed laparoscopic instruments that mimic the movements and dexterity of the human wrist and hand, it was hoped that it would achieve further reductions in operating time and length of hospital stay. Notably, the emergence of RALRP made laparoscopic dissection technically easier, shortening operator learning curves and creating widespread patient and surgeon interest in minimally invasive prostatectomy. In accordance, robot-assisted surgery rapidly gained popularity among urologists. Lee6 states that approximately 60% of all RPs performed in the United States in 2007 were performed using robotic assistance. Each year a greater number of urologists in both academic and private practice settings seek to obtain robotic training.
Regardless of these advances, there remains minimal consensus regarding the optimal treatment of men with localized prostate cancer. This review summarizes the prominent features of each surgical approach to RP with the hope of better defining the management of localized prostate cancer for both patient- and surgeon-specific care.
Operative Outcomes
There is general agreement that the goals of RP are, in order of importance, to cure cancer, maintain urinary continence, maintain erectile function, and minimize complications and perioperative suffering.2 The indications for ORP, LRP, and RALRP are identical: localized disease (stage cT2 or less) without evidence of clinical or radiographic metastatic disease. In particular, contraindications to minimally invasive laparoscopic prostatectomy include uncorrectable bleeding diatheses or the inability to undergo general anesthesia due to severe cardiopulmonary compromise.4
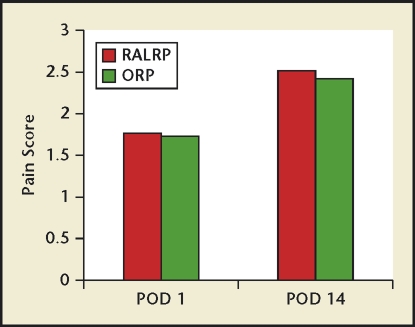
For many procedures, an advantage of a laparoscopic approach is its less invasive aspect when compared with an open surgical incision. With laparoscopy, minimally invasive incisions may create less postoperative pain and may decrease the analgesic requirement. Importantly, minimizing the amount of perioperative narcotic use can significantly impact several measures of postoperative morbidity, such as pulmonary function and ileus duration.7 However, because of the involvement of the upper abdomen with respiration, upper abdominal incisions are generally more painful than those in the lower abdomen. Thus, unlike nephrectomy (in which a generous upper abdominal incision is required for an open surgical approach), there is less opportunity for considerable improvement in postoperative pain with LRP.7 In line, a prospective study conducted at Vanderbilt University (Nashville, TN) by Smith and colleagues8 did not find a significant difference in postoperative pain in the first 14 days after surgery when comparing open and robotic RP. Moreover, Webster and coworkers7 evaluated 314 patients who underwent open RP and 154 men who underwent RALRP by the same surgeon. This study revealed that perioperative narcotic use and patient-reported pain were similar regardless of surgical approach (Figure 1).
Figure 1.
Mean pain scores after robotic-assisted laparoscopic radical prostatectomy (RALRP) and open radical prostatectomy (ORP) performed at Vanderbilt University (Nashville, TN).7 POD, postoperative day.
It is now apparent that the small abdominal incision involved in all surgical approaches to RP translates to low pain scores. ORP is performed through an 8- to 10-cm lower abdominal incision. This relatively small incision is usually sufficient to expose the preperitoneal space and allow access to the prostate and to the pelvic sidewalls for lymphadenectomy. Both LRP and RALRP make use of small incisions. For RALRP, the cumulative size of the incisions is approximately 5 to 6 cm after specimen removal, which is slightly smaller than the standard ORP incision.7 In addition, the largest incision is generally at the periumbilical site, where the incision is extended enough to allow for extraction of the prostate and is often hidden by the umbilical crease.
Other advantages of the laparoscopic approach to prostatectomy include improved visualization and the positive pressure created by the carbon dioxide pneumoperitoneum used for insufflation. Pneumoperitoneum reduces the pressure gradient between the blood vessels and the remainder of the operative field, resulting in less venous and capillary bleeding during the operation.4 Appropriately, the potential for blood loss is consistently reduced in the LRP and RALRP series (Table 1). The meta-analysis by Parsons and Bennett9 exposed 5 studies (N = 672 patients) that evaluated operative blood loss. Compared with the ORP group, the LRP and RALRP groups were associated with significantly less operative blood loss.
Table 1.
Operative Outcomes of Open Radical Prostatectomy, Laparoscopic Radical Prostatectomy, and Robotic-Assisted Laparoscopic Radical Prostatectomy from Selected Single Institution Series
| Reference | Institution | Technique | Patients (N) | OR Time (min) | EBL (mL) | LOS (d) | Length of Catheterization (d) | Complication Rate (%) |
| Schroeck et al.20 | University of Florida College of Medicine (Gainesville, FL) | ORP | 500 | 143 | 820 | 2.11 | 8 | 0.2 |
| Palisaar et al.29 | Ruhr-Universität Bochum (Bochum, Germany) | ORP | 62 | 161 | 790 | 11 | 10 | N/A |
| Gregori et al.11 | Ospedale Luigi Sacco (Milan, Italy) | LRP | 80 | 218 | 376 | 4.5 | 10 | 22.5 |
| Hakimi et al.23 | Montefiore Medical Center (Bronx, NY) | LRP | 75 | 232 | 311 | 3.4 | N/A | 14.7 |
| Guillonneau et al.30 | L’Institut Mutualiste Montsouris (Paris, France) | LRP | 350 | 170 | 290 | 5 | 4.2 | N/A |
| Badani et al.15 | Vattikuti Urology Institute (Detroit, MI) | RALRP | 2766 | 154 | 142 | 1.14 | 10 | 12.2 |
| Hakimi et al.23 | Montefiore Medical Center | RALRP | 75 | 199 | 230 | 1.95 | N/A | 10.7 |
EBL, estimated blood loss; LOS, length of stay; LRP, laparoscopic radical prostatectomy; OR, operating room; ORP, open radical prostatectomy; RALRP, robotic-assisted laparoscopic radical prostatectomy.
Beyond reducing blood loss, minimally invasive surgery has been shown to decrease postoperative morbidity and length of stay for a number of surgical procedures. Patel and colleagues10 studied 374 patients who underwent RRP and 629 patients who underwent RALRP. They reported the mean length of stay (LOS) in ORP patients to be 1.23 days, and 94.3% of these patients were discharged on or before postoperative day 1. On the other hand, the mean LOS was 1.17 days in RALRP patients and 97.5% of these patients were discharged on or before postoperative day 1. In line with several reported series, this prospective study confirmed that RALRP allowed for early patient discharge, with the majority of patients being ready for hospital discharge on postoperative day 1. Nevertheless, this study demonstrates that comparable results can be achieved with ORP. However, unlike these 2 comparable techniques, Gregori and associates11 report a mean hospital stay of 4.5 days in their LRP series.
Finally, another factor supporting the benefit of the intuitive nature of the robotic technique is the rate of conversion to open surgery. When surgeons performing LRP and RALRP are in trouble, they may need to convert emergently to an open procedure to control life-threatening bleeding. Most studies report conversion rates for LRP of 2% to 8%, compared with 0% to 1% for RALRP.5 Likewise, overall major complications appear to be marginally lower after LRP and RALRP, generally once the learning curve is completed, as opposed to after ORP.1,12
Oncologic Outcomes
The primary goal of prostate cancer surgery is to provide satisfactory oncologic outcomes. Biochemical progression and margin positivity are the 2 commonly used indices to assess oncologic outcomes following RP.1 An increasing prostate-specific antigen (PSA) level is an early sign of biochemical progression and prostate cancer recurrence. Furthermore, a positive surgical margin, meaning cancer cells at the inked margin of resection, has been associated with up to a 4-fold increased risk of biochemical recurrence after adjusting for other known risk factors.13 Although ORP provides long-term oncologic control for up to 15 years, limited follow- up data are available for the minimally invasive approaches.
Overall, Nelson2 reports that the 5-year freedom from PSA failure rates are 80%, roughly 75%, and 91.6% for open, laparoscopic, and robotic approaches, respectively. Similarly, Touijer and colleagues14 showed that LRP effectively controlled the disease in 78% of men with prostate cancer at 5 years after surgery at Memorial Sloan-Kettering Cancer Center (MSKCC; New York, NY). At MSKCC, the agreed-upon definition of biochemical recurrence is 0.1 ng/mL confirmed by a subsequent rising PSA level. Another MSKCC group that used the open surgical approach experienced 82% freedom from progression at 5 years after surgery. In line, surgeons who prefer an open technique argue that favoring their oncologic approach is the ability to alter surgical technique in real-time based on intraoperative visual and tactile assessment of tumor stage.2 Badani and colleagues15 reported on one of the largest RALRP series at a median follow-up of 22 months. There was a 7.2% PSA recurrence rate with a 5-year actuarial biochemical-free survival of 84% in this series.2 Despite these differences, given the relatively short-term follow-up for the minimally invasive techniques and varying definitions of biochemical recurrence, it is difficult to state which approach has superior outcomes.
Margin status is an important independent predictor of disease recurrence after radical prostatectomy and, therefore, a measure of treatment efficacy. The positive surgical margin rate was 20% for ORP versus 16.7% for RALRP in a study by Ahlering and coworkers.16 Smith and colleagues8 retrospectively reviewed 200 procedures from each approach. The overall incidence of positive surgical margins was significantly lower among the RALRP cohort compared with ORP cases (15% vs 35%, P < .001). In particular, RALRP had a statistically lower positive margin rate in the specimen groups with a T2 stage and Gleason score of 6 or less. Menon and associates17 reported an 11% positive surgical margin rate in their RALRP series; comparatively, Lepor and coworkers18 report an 8% positive surgical margin rate in their ORP experience with 500 patients. Surgeons reporting more than 100 LRPs showed positive surgical margin rates that ranged from 16% to 27%.2 Based on such published results, LRP may be perceived to compromise the oncologic goals of RP.19 Meanwhile, the generally similar risks of a positive surgical margin in ORP and RALRP indicate analogous cancer-specific survival rates across these approaches to surgery.9 Still, more definitive conclusions will require the accumulation of long-term survival for LRP and RALRP.
Functional Outcomes
The often indolent nature of prostate cancer makes health-related quality of life (HRQoL) and satisfaction with treatment increasingly important for both patients and providers.20 Schroeck and colleagues20 explain that treatment satisfaction is mainly derived from perceived differences between expectations and experience. Urinary incontinence and erectile dysfunction are the 2 major concerns for patients after radical prostatectomy. In fact, poor general health, in addition to bother due to urinary dysfunction and sexual dysfunction, has been found to be an independent predictor for regret after primary treatment.20
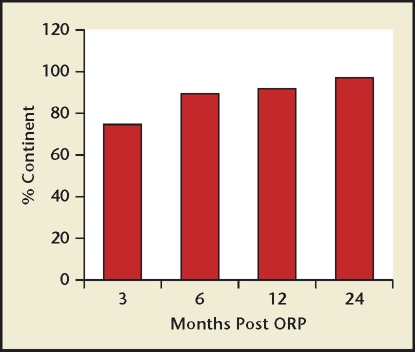
Continence rate, commonly defined as requiring 1 or no pads per day, is reported to be between 90% to 92% after ORP, 82% to 96% after LRP, and 95% to 96% after RALRP.1 In the Prostate Cancer Outcomes Study, Penson and colleagues21 demonstrated continence rates of 90% at 24-month follow-up and 86% at 60-month follow-up in 1288 men who underwent ORP. In the world’s largest reported ORP series of 3477 patients, Frota and coauthors1 report an overall 93% continence rate. Similarly, in a series of 621 patients who underwent ORP, Lepor and colleagues18 report that 74.4%, 89.6%, 92.4%, and 97.1% of men considered themselves continent at 3, 6, 12, and 24 months, respectively (Figure 2). Stolzenburg and Coworkers22 demonstrated a continence rate of 84% at 6-month follow-up and a 92% continence rate at 1-year follow up in 700 extraperitoneal LRPs.
Figure 2.
Patient assessment of urinary continence after open radical prostatectomy (ORP).25
At the Montefiore Medical Center (Bronx, NY), Hakimi and colleagues23 experience a continence rate of 89.3% in LRP patients and 93.3% in RALRP patients at 12 months. Although they do not note a significant difference between LRP and RALRP, a trend toward a faster return of continence and potency was experienced in favor of RALRP at 3, 6, and 12 months postoperatively.23 With RALRP, Ahlering and associates16 reported a 98% continence rate at 12-month follow-up in their initial series of 200 patients. In addition, Menon and coauthors17 reported a continence rate of 96% in a series of more than 1100 RALRP procedures. At Vanderbilt University, Smith and colleagues8 reported continence at 12 months (defined as 1 or no pads) as 97% for RALRP and 94% for ORP. Guillonneau and associates24 presented a single-institution nonrandomized study from MSKCC measuring recovery of continence following ORP and LRP. Using the definition of continence as no use of pads, 257 patients who underwent LRP were compared with 298 patients who underwent ORP. At every measured time point ORP had better recovery of continence and was significantly better than LRP across the study. Finally, at last reported follow-up, 97% of ORP patients were free of pads compared with 69% of LRP patients. Evidently, ORP has superior results to LRP and comparable results to RALRP in regard to urinary continence.
It is difficult based on the current literature to determine if one approach is superior to the other for the preservation of the neurovascular bundles and sexual function. Data indicate that 95% of men in their 40s who undergo traditional nerve sparing in an ORP will regain sexual function adequate for intercourse, whereas only 50% of men in their 70s will regain the same function, still maintaining single-digit rates of positive margins.4 Using a robotic approach, Menon25 began to dissect a plane on the anterior-lateral portion of the prostate largely ignored during standard open or laparoscopic RP, preserving the “veil of Aphrodite” of periprostatic fascia. Histologic analysis of this tissue plane demonstrated nerves coursing through. In a report on 154 consecutive patients in whom this tissue was preserved, along with the more widely recognized neurovascular bundles, Menon25 reported a 96% intercourse rate and a 69% normal erection rate at 12 months after surgery. Moreover, using 2 studies included in the meta-analysis by Parsons and Bennett,9 there was a nonsignificant trend toward increased potency for the laparoscopic and robotic-assisted group. At the Montefiore Medical Center, among the patients who underwent a bilateral nerve-sparing procedure, 71% of LRP patients and 76.5% of RALRP patients were potent at 12 months postoperatively.23 Although these data may suggest that RALRP has some advantages in recovery of potency, the data do not clearly support one technique as superior to the others.
When Hara and colleagues26 compared quality of life in patients who underwent LRP and ORP, no significant differences were found in any of the items of general health before or after surgery. They observed no significant differences in functional status, urological symptoms, physical comfort, psychologic distress, and social activity before and after surgery. Sexual life was significantly impaired by surgery with no difference between the LRP and ORP groups. This result was confirmed by the International Index of Erectile Function (IIEF) data, with the IIEF score significantly decreasing after surgery. Following surgery, quality of life due to incontinence symptoms deteriorated, whereas quality of life due to voiding symptoms was improved by surgery.26 With regard to satisfaction with urination, a slight but not significant improvement was reported after surgery. Interestingly, these measures were comparable between the LRP and ORP groups.
However, in a comparison of RALRP and ORP completed by Schroeck and colleagues,20 it was found that undergoing RALRP is independently associated with more frequent dissatisfaction and regret after RP. Specifically, after adjusting for multiple sociodemographic variables and Expanded Prostate Cancer Index Composite domain scores, patients who underwent RALRP were approximately 3 to 4 times as likely to be dissatisfied and regretful as those who underwent ORP.20 Schroeck and colleagues20 postulate that patients who chose the innovative, less invasive RALRP may have higher expectations for their postoperative HRQoL as compared with patients who chose more traditional surgery. Consequently, even though RALRP patients achieved similar function and bother scores compared with patients who underwent ORP, those patients still experienced a higher level of dissatisfaction and regret.20
Learning Curve
It is known that LRP and RALRP are technically demanding, requiring a significant operator learning curve. Various authors have concluded that to become proficient at LRP or RALRP, defined as achieving outcomes comparable with their open surgical experience, a surgeon must perform anywhere from 8 to 12 cases to as many as 200 cases.1 Patel and coauthors10 advocate that, for a laparoscopically naive yet experienced open surgeon, open surgical skills can be successfully transferred to a laparoscopic environment in 8 to 12 cases using a robotic interface. In addition, several programs have reported that surgeons with minimal or no laparoscopic experience mastered the learning curve using the da Vinci Surgical System after 10 to 20 cases.5 On the other hand, Guillonneau and associates24 have noted that it takes 40 to 60 cases for experienced laparoscopists to master the learning curve, mainly attributed to the counterintuitive nature of dissection and the difficult urethrovesical anastomosis. What’s more, both Patel and coworkers10 and Guillonneau and coworkers24 note that, for the laparoscopically naive surgeon, 80 to 100 cases are probably required to attain proficiency.5,10,24 Thus, the development of a robotic interface significantly shortens the LRP learning curve for an experienced open yet naive laparoscopic surgeon.
While a surgeon is learning a new technique, numerous patients may achieve outcomes inferior to what they might otherwise have obtained with an experienced surgeon. Klein and associates12 reveal that cancer control after RP improves with increasing surgeon experience regardless of preoperative risk group. This study’s overall cohort experienced an absolute decrease in the risk of recurrence at 5 years in a patient seeing an experienced rather than an inexperienced surgeon between 6.6% and 12%, depending on risk group. Also, Badani and colleagues15 demonstrate that with continuous quality improvement and technical refinement during their RALRP series, they improved outcomes well after the initial learning curve, which they stated to be approximately 18 cases. In fact, the mean console time decreased by 19% between the first 200 and last 200 patients.
In addition, some surgeons do not have the patient volume to ever complete their learning curve.13 To investigate the impact of variations in patient volume, Eastham and colleagues evaluated health-related outcomes after RP using the Surveillance, Epidemiology, and End Results Medicare database. Postoperative morbidity was lower in very high-volume hospitals than in low-volume hospitals (27% vs 32%; P = .03).13 Also, morbidity was lower when the RP was performed by very high-volume surgeons as opposed to low-volume surgeons (26% vs 32%; P < .001). A similar pattern was found in the rate of late urinary complications. These findings suggest that the incidence of early postoperative morbidity and urinary complications is lower among surgeons who perform a high volume of RP.13 The variability in outcome among surgeons with the highest volume of RP strongly suggests that variations in surgical proficiency have a significant effect on results.
Moreover, in a greater detailed analysis, clinical outcomes were examined among the 159 surgeons who performed a high or very high volume of procedures. This evaluation revealed wide surgeon-to-surgeon variation, greatly exceeding any that could be predicted based on chance or variations in the case mix.13 It follows that the success of RP and the incidence of complications fluctuate not only among surgeons with distinct levels of experience, but also among the subset of highly experienced surgeons. Few surgeons are proficient in more than one surgical approach to RP, let alone are they willing to randomly offer 2 different options.19 Therefore, inherent limitations are present in studies because individual surgeon experiences and training have varied for both the minimally invasive and the open radical prostatectomy groups.
Cost
Cost is a relevant issue when comparing the different approaches with RP. It is apparent that start-up costs for the da Vinci robot are significantly greater than those for standard laparoscopy.5 Even when considering the possible shorter hospital stay associated with RALRP, RALRP is far more expensive than traditional ORP.27 Lotan and colleagues28 reported that ORP had a cost advantage of $487 over LRP and $1726 over RALRP. According to Lotan and colleagues, LRP has proved to be almost as cost competitive as ORP, whereas RALRP is the most expensive to the hospital due to purchase of the robot, maintenance, and cost of operative equipment. At the cost of $1.2 million per robot, a yearly maintenance fee of $100,000 and a $1500 perpatient cost in disposable robotic instruments per operation, the financial responsibilities for starting and maintaining a robotic practice can be intimidating.4
Recent cost-effective analyses of RALRP have indicated that cost equivalence between standard ORP and RALRP may be achieved at high-volume prostatectomy centers where RALRP is performed on the order of 10 or more cases per week.10 Therefore, in the upcoming years and decades, as experience with LRP and RALRP increases, the early training of new generations of surgeons involves robotics, and costs of robotic technologies decrease, cost equivalence between open, laparoscopic, and robotic surgeries may be achieved.
Conclusions
When confronted with the diagnosis of localized prostate cancer, patients have to opt for one treatment over another in the absence of solid scientific evidence favoring a specific treatment. In this setting, pretreatment patient education and counseling are crucial parts of the decision-making process. The results of this analysis should be helpful in counseling patients about therapy decisions for newly diagnosed, localized prostate cancer. Urologists must carefully depict the risks and benefits of recent technologies during preoperative counseling to minimize regret and maximize satisfaction.21
The surgical removal of localized prostate cancer continues to be the most definitive treatment of the disease.2 In the hands of an experienced surgeon, the standard represented by ORP is very high. Aside from reductions in blood loss, many results of LRP and RALRP at centers of excellence are comparable with those after ORP; however, overall they have not proved to be superior to ORP outcomes or resulted in anticipated benefits to patients.13 Therefore, considering the lack of superiority of the other techniques, the shorter learning curves, and the available long-term outcome data, the open technique remains the gold standard.
However, there is a trend toward consistently better outcomes following RALRP as opposed to LRP. RALRP can successfully diminish the learning curve that surgeons face when beginning to perform LRP. RALRP also offers quicker and superior return to continence, and decreases in operative time as well as length of hospital stay. Moreover, with the robotic approach, the surgeon regains much of the degree of freedom for dissection that is lacking with LRP.4 Consequently, the use of LRP is confined to centers that have historically and exclusively used this technique, and is disappearing from the armamentarium of minimally invasive prostatic surgery at other centers. Although economic considerations are vital, the advantages provided by robotic technology have the potential to minimize patient morbidity while improving both functional and oncologic outcomes. The short-term data are expanding and are encouraging when compared with the current gold standard of ORP. As robotic technology evolves and becomes more prevalent, there is likely to be continued innovation and improved surgical outcomes. Ultimately, RALRP is a new technology that deserves our attention and needs further evaluation.
Despite this trend, current data suggest that results ultimately depend more on surgical technique than on surgical approach. Dissimilarity in outcomes among high-volume surgeons points toward distinctions in quality of care that are probably related to variations in surgical technique. Furthermore, rates of blood loss, positive surgical margins, incontinence, and erectile dysfunction vary widely from surgeon to surgeon.13 It has become clear that the best chance for cure rests in the most experienced hands in patients in all risk groups.12 Nelson2 eloquently states, “the difference between Tiger Woods and the local club champion is not in the putter, the irons, or the woods, it is in skill and consistency.”
Main Points.
Open radical prostatectomy (ORP) has been considered the gold standard for the surgical treatment of localized prostate cancer; however, laparoscopic (LRP) and robotic-assisted prostatectomy (RALRP) have become standards of care at many centers worldwide.
The emergence of RALRP made laparoscopic dissection technically easier. Minimally invasive incisions create less postoperative pain, reduce blood loss, and decrease hospital length of stay.
ORP provides long-term oncologic control for up to 15 years. Surgeons who prefer an open technique claim the ability to alter surgical technique in real-time based on intraoperative visual and tactile assessment of tumor stage.
Urinary incontinence and erectile dysfunction are the 2 major concerns for patients after radical prostatectomy. Continence rate is reported to be between 90% and 92% after ORP, 82% to 96% after LRP, and 95% to 96% after RALRP. Data may suggest that RALRP has some advantages in recovery of potency over other RP techniques.
LRP and RALRP are technically demanding, and both have a significant operator learning curve.
RALRP is the most expensive to the hospital due to purchase of the robot, maintenance, and cost of operative equipment. As a result, the financial responsibilities for starting and maintaining a robotic practice can be intimidating. Although economic considerations are vital, the advantages provided by robotic technology have the potential to minimize patient morbidity while improving both functional and oncologic outcomes.
References
- 1.Frota R, Turna B, Barros R, Gill IS. Comparison of radical prostatectomy techniques: open, laparoscopic and robotic assisted. Int Braz J Urol. 2008;34:259–269. doi: 10.1590/s1677-55382008000300002. [DOI] [PubMed] [Google Scholar]
- 2.Nelson JB. Debate: open radical prostatectomy vs. laparoscopic vs. robotic. Urol Oncol. 2007;25:490–493. doi: 10.1016/j.urolonc.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 3.Middleton RG, Thompson IM, Austenfeld MS, et al. Prostate cancer clinical guidelines panel summary: report on the management of clinically localized prostate cancer. J Urol. 1995;154:2144–2148. [PubMed] [Google Scholar]
- 4.Bivalacqua TJ, Pierorazio PM, Su LM. Open, laparoscopic and robotic radical prostatectomy: optimizing the surgical approach. Surg Oncol. 2009;18:233–241. doi: 10.1016/j.suronc.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Ahlering TE. Robotic versus laparoscopic radical prostatectomy. Nat Clin Pract Urol. 2004;1:58–59. doi: 10.1038/ncpuro0040. [DOI] [PubMed] [Google Scholar]
- 6.Lee DI. Robotic prostatectomy: what we have learned and where we are going. Yonsei Med J. 2009;50:177–181. doi: 10.3349/ymj.2009.50.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Webster TM, Herrell SD, Chang SS, et al. Robotic assisted laparoscopic radical prostatectomy versus retropubic radical prostatectomy: a prospective assessment of postoperative pain. J Urol. 2005;174:912–914. doi: 10.1097/01.ju.0000169455.25510.ff. [DOI] [PubMed] [Google Scholar]
- 8.Smith JA , Jr, Chan RC, Chang SS, et al. A comparison of the incidence and location of positive surgical margins in robotic assisted laparoscopic radical prostatectomy and open retropubic radical prostatectomy. J Urol. 2007;178:2385–2390. doi: 10.1016/j.juro.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Parsons JK, Bennett JL. Outcomes of retropubic, laparoscopic, and robotic-assisted prostatectomy. Urology. 2008;72:412–416. doi: 10.1016/j.urology.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 10.Patel HR, Linares A, Joseph JV. Robotic and laparoscopic surgery: cost and training. Surg Oncol. 2009;18:242–246. doi: 10.1016/j.suronc.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Gregori A, Simonato A, Lissiani A, et al. Laparoscopic radical prostatectomy: perioperative complications in an initial and consecutive series of 80 cases. Eur Urol. 2003;44:190–194. doi: 10.1016/s0302-2838(03)00261-6. [DOI] [PubMed] [Google Scholar]
- 12.Klein EA, Bianco FJ, Serio AM, et al. Surgeon experience is strongly associated with biochemical recurrence after prostatectomy for all preoperative risk categories. J Urol. 2008;179:2212–2217. doi: 10.1016/j.juro.2008.01.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eastham J, Tokuda Y, Scardino P. Trends in radical prostatectomy. Int J Urol. 2009;16:151–160. doi: 10.1111/j.1442-2042.2008.02178.x. [DOI] [PubMed] [Google Scholar]
- 14.Touijer K, Secin FP, Cronin AM, et al. Oncologic outcome after laparoscopic radical prostatectomy: 10 years of experience. Eur Urol. 2009;55:1014–1019. doi: 10.1016/j.eururo.2008.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Badani KK, Kaul A, Menon M. Evolution of robotic radical prostatectomy: assessment after 2766 procedures. Cancer. 2007;110:1951–1958. doi: 10.1002/cncr.23027. [DOI] [PubMed] [Google Scholar]
- 16.Ahlering TE, Woo D, Eichel L, et al. Robotassisted versus open radical prostatectomy: a comparison of one surgeon’s outcomes. Urology. 2004;63:819–822. doi: 10.1016/j.urology.2004.01.038. [DOI] [PubMed] [Google Scholar]
- 17.Menon M, Shrivastava A, Kaul S, et al. Vattikuti Institute prostatectomy: contemporary technique and analysis of results. Eur Urol. 2007;51 (suppl 1):15–21. doi: 10.1016/j.eururo.2006.10.055. [DOI] [PubMed] [Google Scholar]
- 18.Lepor H, Kaci L, Xue X. Continence following radical retropubic prostatectomy using self-reporting instruments. J Urol. 2004;171:1212–1215. doi: 10.1097/01.ju.0000110631.81774.9c. [DOI] [PubMed] [Google Scholar]
- 19.Touijer K, Eastham JA, Secin FP, et al. Comprehensive prospective comparative analysis of outcomes between open and laparoscopic radical prostatectomy conducted in 2003 to 2005. J Urol. 2008;179:1811–1817. doi: 10.1016/j.juro.2008.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schroeck FR, Krupski TL, Sun L, et al. Satisfaction and regret after open retropubic or robotassisted laparoscopic radical prostatectomy. Eur Urol. 2008;54:785–793. doi: 10.1016/j.eururo.2008.06.063. [DOI] [PubMed] [Google Scholar]
- 21.Penson DF, McLerran D, Feng Z, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005;173:1701–1705. doi: 10.1097/01.ju.0000154637.38262.3a. [DOI] [PubMed] [Google Scholar]
- 22.Stolzenburg JU, Rabenalt R, Do M, et al. Endoscopic extraperitoneal radical prostatectomy: the University of Leipzig experience of 1,300 cases. World J Urol. 2007;25:45–51. doi: 10.1007/s00345-007-0156-9. [DOI] [PubMed] [Google Scholar]
- 23.Hakimi AA, Blitstein J, Feder M, et al. Direct comparison of surgical and functional outcomes of robotic-assisted versus pure laparoscopic radical prostatectomy: single-surgeon experience. Urology. 2009;73:119–123. doi: 10.1016/j.urology.2008.08.491. [DOI] [PubMed] [Google Scholar]
- 24.Guillonneau B, el-Fettouh H, Baumert H, et al. Laparoscopic radical prostatectomy: oncologic evaluation after 1,000 cases at Montsouris Institute. J Urol. 2003;169:1261–1266. doi: 10.1097/01.ju.0000055141.36916.be. [DOI] [PubMed] [Google Scholar]
- 25.Menon M. Robotic radical retropubic prostatectomy. BJU Int. 2003;91:175–176. doi: 10.1046/j.1464-410x.2003.04070.x. [DOI] [PubMed] [Google Scholar]
- 26.Hara I, Kawabata G, Miyake H, et al. Comparison of quality of life following laparoscopic and open prostatectomy for prostate cancer. J Urol. 2003;169:2045–2048. doi: 10.1097/01.ju.0000063961.99940.6c. [DOI] [PubMed] [Google Scholar]
- 27.Djavan B, Ravery V, Rocco B, et al. European study of radical prostatectomy: time trends in Europe, 1993–2005. BJU Int. 2007;100(suppl 2):22–25. doi: 10.1111/j.1464-410X.2007.06948.x. [DOI] [PubMed] [Google Scholar]
- 28.Lotan Y, Cadeddu JA, Gettman MT. The new economics of radical prostatectomy: cost comparison of open, laparoscopic and robot assisted techniques. J Urol. 2004;172:1431–1435. doi: 10.1097/01.ju.0000139714.09832.47. [DOI] [PubMed] [Google Scholar]
- 29.Palisaar JR, Wenske S, Sommerer F, et al. Open radical retropubic prostatectomy gives favourable surgical and functional outcomes after transurethral resection of the prostate. BJU Int. 2009;104:611–614. doi: 10.1111/j.1464-410X.2009.08474.x. [DOI] [PubMed] [Google Scholar]
- 30.Guillonneau B, Cathelineau X, Doublet JD, et al. Laparoscopic prostatectomy: assessment after 550 procedures. Crit Rev Oncol Hematol. 2002;43:123–133. doi: 10.1016/s1040-8428(02)00024-0. [DOI] [PubMed] [Google Scholar]