Abstract
We report a case of transitional cell carcinoma (TCC) discovered within a calyceal diverticulum at the time of percutaneous nephrolithotomy. The stones and tumor were endoscopically removed and the diverticular cavity fulgurated. Pathologic analysis demonstrated low-grade TCC. A subsequent laparoscopic radical nephroureterectomy was performed and high-grade TCC invading the parenchyma was found. This case demonstrates the potential for TCC to develop in stone-containing calyceal diverticula and also the potential for coexistence of different grades of TCC within the involved renal unit.
Key words: Transitional cell carcinoma, Calyceal diverticulum, Urolithiasis, Stone, Urinary tract infection, Percutaneous nephrolithotomy
Urothelial malignancy of the upper urinary tract is relatively uncommon when compared with all urothelial cancer, comprising only about 5% of tumors.1 Many factors are known to be associated with increased risk for developing upper tract cancer. Men are twice as likely as women and whites twice as likely as blacks to develop urothelial malignancy. The highest rate of upper tract disease is found in the Balkan states, a phenomenon that likely results from a higher prevalence of degenerative interstitial nephropathy in this region, termed Balkan nephropathy.
Among modifiable risk factors for developing upper urinary tract cancer, tobacco smoking is perhaps the most influential, contributing a dose-dependent relative risk (RR).2 Long-term smoking (> 25 years) is associated with a RR of 4.5 for developing upper tract malignancy compared with nonsmokers. Active smokers (RR = 5.2) have more risk than former smokers; however, even former smokers have more than double the risk of a person who has never smoked. Other modifiable risk factors for developing upper tract cancer include heavy coffee consumption (> 7 cups/d) and chronic analgesic use.2 Family history, occupational exposures to aromatic amines such as aniline, β-naphthylamine, and benzidine, as well as radiation exposure, have also been suggested as risk factors.
Upper urinary tract stones, with or without recurrent urinary tract infection (UTI), are a known risk factor for upper tract cancers including squamous cell carcinoma (SCC), transitional cell carcinoma (TCC), and adenocarcinoma (AC). The mechanism is thought to be mediated through chronic inflammation leading to urothelial proliferation and eventual malignant transformation. Using data from the national Swedish inpatient registry and the national Swedish cancer registry, Chow and associates found significantly increased rates of renal pelvis and ureter cancer (standardized incidence ratio [SIR] = 2.5) among patients admitted for upper urinary tract stones.3 They also found that distal ureteral tumors occurred more frequently than proximal tumors, although proximal stones were associated with a higher risk of malignancy than distal stones.3 This association may be due to downstream tumor seeding within the urinary tract.
Calyceal diverticula are often found to contain stones. Carcinoma within a calyceal diverticulum, however, is exceedingly uncommon. Only 3 such cases have been reported in the literature, none of them within the United States and none found during a procedure for stone removal.4–6 Herein, we report a case of TCC within a calyceal diverticulum that was discovered during percutaneous nephrolithotomy (PCNL).
Case History
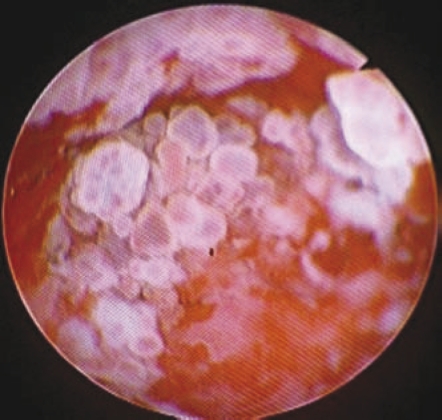
A 68-year-old white man had intermittent gross hematuria and right flank pain for 1 year. Comorbidities included tobacco abuse, coronary artery disease, bilateral carotid artery stenosis, diabetes mellitus, and a remote history of renal trauma. Physical examination results were normal. Serum creatinine, urine cytology, and culture were normal. He was evaluated with abdominal and pelvic magnetic resonance imaging (MRI), computed tomography (CT) cystoscopy, and retrograde pyelography. The MRI and CT demonstrated a 3 cm × 3 cm right posterior calyceal diverticulum containing multiple dependent stones which was also highlighted on the retrograde study (Figures 1–3). Cystoscopy demonstrated no mucosal lesions. The patient elected to undergo PCNL, which was performed under general anesthesia. An 18-gauge needle was placed in the diverticular cavity under fluoroscopic guidance after which a guide wire was curled in the diverticular cavity. The tract was balloon dilated to 30 Fr and a similar sized working sheath was positioned at the edge of the diverticular cavity. Multiple stones and papillary lesions were seen on rigid endoscopy. The stones and lesions were completely removed and the diverticular cavity was fulgurated. A 24 Fr Malecot catheter was inserted and removed 72 hours later.
Figure 1.
Computed tomography of the abdomen supine (top) and prone (bottom) demonstrating a 3 cm × 3 cm calyceal diverticulum containing stones.
Figure 3.
Endoscopy image captured during percutaneous nephrolithotomy of papillary lesions within the calyceal diverticulum.
Pathologic analysis demonstrated low-grade TCC and the stone composition was calcium oxalate and uric acid. It was decided to proceed with laparoscopic right radical nephroureterectomy as it would not be possible to adequately follow this patient’s upper urinary tract endoscopically. This was performed uneventfully. Pathologic analysis demonstrated high-grade TCC with parenchymal invasion. Regional lymph nodes were not involved (T3N0M0). The patient elected to receive adjuvant systemic chemotherapy with carboplatin and gemcitabine. He subsequently developed a pulmonary nodule, which was biopsied percutaneously and demonstrated SCC. It could not be determined whether this was a metastatic lesion or a primary lung tumor. A follow-up cystoscopy did not reveal any bladder or urethral lesions and results of saline wash cytology were negative. He did not tolerate continued systemic chemotherapy and elected to pursue supportive care.
Discussion
Stones within the upper urinary tract are a known risk factor for malignancy of the renal collecting system, ureter, and bladder.3 To our knowledge, there are no prior reported cases of a calyceal diverticular TCC found during PCNL. There have been 3 cases of TCC in calyceal diverticular cavities where this diagnosis was confirmed after radical nephroureterectomy or simple nephrectomy.4–6 The diagnosis was suspected in each case based on preoperative imaging. Imaging, however, is not always reliable, as a significant number of patients who undergo nephrectomy for removal of a poorly functioning stone-laden kidney may have unexpected cancer in the removed renal unit. In 2007, Yeh and colleagues reported a series of 47 patients who underwent nephrectomy to treat a stone disease in a nonfunctioning kidney.7 They found malignancy in 24 of the 47 patients (51%) who underwent nephrectomy, but the lesion was seen on preoperative imaging in only 7 of those 24 patients (29%).
The exact mechanism for stone-related urothelial malignancy has not been proven, but many consider chronic inflammation and mucosal irritation caused by the stone to be a causative factor. Additionally, stone formers with frequent UTIs have twice the risk of developing an upper tract malignancy compared with patients without this problem.3 Although, SCC and AC of upper tracts are strongly associated with upper urinary tract stone disease,8,9 TCC remains the most common histology in this cohort.3,7
Renal stones, especially staghorn calculi, may result in a limited ability to visualize concomitant neoplasms within the renal pelvis, ureter, or, as in this case, a calyceal diverticulum. Large stone burden may obscure an underlying mucosal lesion radiographically. In patients with longstanding upper urinary tract stones, especially associated with infection, such lesions may be even more difficult to diagnose given the related inflammation and fibrosis normally present in such cases. Infected patients and patients with chronic mucosal irritation from stones may also make interpretation of urine cytology difficult. In our patient, extensive radiographic imaging was obtained to evaluate his hematuria and characterize the diverticulum. The initial retrograde pyelogram and subsequent CT and MRI studies did not reveal an associated soft tissue mass.
Difficulty with diagnosing urothelial malignancy in these patients has led some to advocate for routine random biopsy of the collecting system during PCNL performed for stone disease.10–12 Although we do not advocate this practice, we recommend that any lesions of the collecting system seen during PCNL should be biopsied or removed endoscopically in total. This may permit an earlier diagnosis of an underlying malignancy of the collecting system, giving the patient a better chance of survival.
Main Points.
Urothelial malignancy of the upper urinary tract is relatively uncommon when compared with all urothelial cancer, comprising about 5% of tumors. Men are twice as likely as women, and whites twice as likely as blacks, to develop this kind of malignancy.
Modifiable risk factors include tobacco smoking, heavy coffee consumption (>7 cups/d), and chronic analgesic use. Family history, occupational exposures, and radiation exposure may also be contributing risk factors.
Preoperative imaging is not always reliable regarding malignancy detection because a significant number of patients who undergo nephrectomy for removal of a poorly functioning stone-laden kidney have been found to have unexpected cancer in the removed renal unit.
Stone formers with frequent urinary tract infections have twice the risk of developing an upper tract malignancy compared with those patients without this problem, and although squamous cell carcinoma and adenocarcinoma of the upper tracts are strongly associated with this kind of malignancy, transitional cell carcinoma remains the most common histology in this cohort.
Difficulty in diagnosis of urothelial malignancies has prompted some to advocate routine random biopsy of the collecting system during percutaneous nephrolithotomy (PCNL) performed for stone disease. Although this practice is not recommended, what is suggested is that any lesions seen during PCNL be biopsied or removed endoscopically in total. This may permit an earlier diagnosis of underlying malignancy, providing patients with better chance for survival.
Figure 2.
Retrograde pyelogram.
References
- 1.Campbell MF, Wein AJ, Kavoussi LR. Campbell-Walsh Urology. 9th ed. Philadelphia, PA: W.B. Saunders; 2007. [Google Scholar]
- 2.Ross RK, Paganini-Hill A, Landolph J, et al. Analgesics, cigarette smoking, and other risk factors for cancer of the renal pelvis and ureter. Cancer Res. 1989;49:1045–1048. [PubMed] [Google Scholar]
- 3.Chow WH, Lindblad P, Gridley G, et al. Risk of urinary tract cancers following kidney or ureter stones. J Natl Cancer Inst. 1997;89:1453–1457. doi: 10.1093/jnci/89.19.1453. [DOI] [PubMed] [Google Scholar]
- 4.Adachi T, Ezaki K, Funai K. A case of transitional cell carcinoma in a pyelocaliceal diverticulum [in Japanese] Hinyokika Kiyo. 1989;35:1383–1386. [PubMed] [Google Scholar]
- 5.Hayashi S, Iwai Y, Yasumoto R, et al. Milk of calcium renal stone in a patient with ureteral tumor: a case report [in Japanese] Hinyokika Kiyo. 1993;39:1035–1038. [PubMed] [Google Scholar]
- 6.Yoshimura K, Yoshida H, Kawase N, Taki Y. A case of transitional cell carcinoma and milk of calcium in a pyelocalyceal diverticulum [in Japanese] Hinyokika Kiyo. 1998;44:649–652. [PubMed] [Google Scholar]
- 7.Yeh CC, Lin TH, Wu HC, et al. A high association of upper urinary tract transitional cell carcinoma with nonfunctioning kidney caused by stone disease in Taiwan. Urol Int. 2007;79:19–23. doi: 10.1159/000102907. [DOI] [PubMed] [Google Scholar]
- 8.Raghavendran M, Rastogi A, Dubey D, et al. Stones associated with renal pelvic malignancies. Indian J Cancer. 2003;40:108–112. [PubMed] [Google Scholar]
- 9.Li MK, Cheung WL. Squamous cell carcinoma of the renal pelvis. J Urol. 1987;138:269–271. doi: 10.1016/s0022-5347(17)43116-8. [DOI] [PubMed] [Google Scholar]
- 10.Ozdamar AS, Ozkürkcügil C, Gültekin Y, Gökalp A. Should we get routine urothelial biopsies in every stone surgery? Int Urol Nephrol. 1997;29:415–420. doi: 10.1007/BF02551106. [DOI] [PubMed] [Google Scholar]
- 11.Gökalp A, Günes HA, Gültekin EY, et al. Renal pelvic biopsies of renal calculi patients. Br J Clin Pract. 1989;43:297–299. [PubMed] [Google Scholar]
- 12.Katz R, Gofrit ON, Golijanin D, et al. Urothelial cancer of the renal pelvis in percutaneous nephrolithotomy patients. Urol Int. 2005;75:17–20. doi: 10.1159/000085921. [DOI] [PubMed] [Google Scholar]