Abstract
Introduction
Extensive research suggests that long-term cigarette smoking is an independent risk factor for the introduction of sexual dysfunction in men. However, results of limited data investigating this relationship in women are mixed. No studies have examined the acute effects of tobacco or nicotine on physiological sexual response in women. Controlled experimental studies examining acute effects of isolated nicotine intake on female physiological sexual responses are necessary in order to help elucidate tobacco’s potential role in the development and/or maintenance of sexual impairment in women.
Aim
To examine whether isolated nicotine intake acutely affects sexual arousal responses in nonsmoking women.
Methods
Twenty-five sexually functional women (mean age = 20 years) each with less than 100 direct exposures to nicotine completed two counterbalanced conditions in which they were randomized to received either nicotine gum (6 mg) or placebo gum, both administered double-blind and matched for appearance, taste, and consistency, approximately 40 minutes prior to viewing an erotic film.
Main Outcome Measures
Physiological (changes in vaginal pulse amplitude via vaginal photoplethysmography) and subjective (continuous self-report) sexual responses to erotic stimuli were examined, as well as changes in mood.
Results
Nicotine significantly reduced genital responses to the erotic films (P = 0.05), corresponding to a 30% attenuation in physiological sexual arousal. This occurred in 11 of 18 women with valid physiological assessments. Nicotine had no significant effect on continuous self-report ratings of sexual arousal (P = 0.45), or on mood (all Ps > 0.05).
Conclusions
Acute nicotine intake significantly attenuates physiological sexual arousal in healthy nonsmoking women. Our findings provide support to the hypothesis that nicotine may be the primary pharmacological agent responsible for genital hemodynamic disruption, thereby facilitating a cascade of biochemical and vascular events which may impair normal sexual arousal responses.
Keywords: Nicotine, Smoking, Sexual Arousal, Vaginal Photoplethysmography
Introduction
Cigarette smoking is the most preventable cause of morbidity and premature mortality worldwide [1,2]. Smoking introduces a wide range of diseases including, but not limited to, many types of cancer [3], cardiovascular diseases (e.g., coronary heart disease, peripheral vascular disease, hypertension, stroke) [4–6], and respiratory diseases [7]. Tobacco use elicits enormous consequences, with an estimated $157 billion in health-related economic losses each year within the United States alone [2] and approximately five million premature deaths annually worldwide [8].
Impairment in sexual functioning has also been reported as a sequela of long-term tobacco intake. Extensive literature indicates that cigarette smoking is an independent risk factor for introducing vasculogenic erectile impairment in men [9–11] and that these individuals are approximately 1.5 to two times as likely as nonsmokers to report erectile dysfunction [12–19]. However, limited research has investigated this link in women, and results are mixed [20–22].
The complex processes by which long-term smoking may deleteriously affect physiological mechanisms underlying sexual function is not clearly understood. Sexual arousal in men and women is a complex neurovascular event in which smooth muscle relaxation promotes arterial inflow to the genitals thereby facilitating vasocongestion [23]. Nitric oxide (NO) produced within genital endothelial cells has been identified as the principal neurotransmitter mediating these vascular events in men [24,25] and may be the primary regulator of vaginal hemodynamics in women [26]. Pathophysiological underpinnings of chronic tobacco-induced sexual impairment have been proposed in response to the wide range of research examining the effects of cigarette smoking on biochemical mechanisms underlying vascular functioning [27]. Several studies have clearly shown that smoking is associated with decreased NO in arteries [28] and veins [29]. In light of these findings, investigators have proposed that free radicals and other compounds found within cigarettes may decrease the synthesis of NO directly, or indirectly by targeting precursors, resulting in decreased genital vasoengorgement in men [30–32].
Few studies have focused on the acute effects of smoking on physiological sexual response and none have investigated these effects in female subjects. One animal study [11] reported impaired genital vasocongestion in dogs after approximately 10 minutes of acute tobacco smoke exposure. Similar results have been demonstrated in human males in response to cigarette smoking [33]. However, because chronic cigarette smoking may cause vascular degeneration [34], uncertainty arises as to whether the acute effects of tobacco smoke on sexual arousal differentially affect long-term smokers compared with nonsmokers. Additionally, nicotine dosing via tobacco smoking is difficult to control. Many factors such as number of puffs, intensity of puffing, depth of inhalation, and variation in puff volume can influence nicotine plasma concentration levels [35]. Use of cigarettes may also introduce other effects on responding because of the familiarity of the method of administration, including a participant’s expectancies of smoking effects [36]. Finally, cigarettes contain thousands of pharmacological constituents making it impossible to tease apart the primary element or group of interacting pharmacological compounds responsible for observed psychological and physiological effects.
In an attempt to address these issues, Harte and Meston [37] conducted a placebo-controlled cross-over trial examining the acute effects of isolated nicotine in nonsmoking men and revealed that nicotine significantly attenuated physiological sexual arousal responses. These findings are in accordance with those of other studies examining the deleterious acute effects of isolated nicotine on sexual arousal [38] and peripheral vasculature [29,39]. To our knowledge, there have been no published studies examining isolated nicotine’s effects on sexual functioning in women or in female animal models. Considering that the hemodynamic processes of sexual arousal in women are similar to that in men; and considering that NO isoforms have been shown to be present in genital epithelia of both men (i.e., penile [23]) and women (i.e., vaginal [40], clitoral [41]), one may speculate that smoking may affect physiological mechanisms underlying sexual arousal in men and women similarly. This may be the result of nicotine and/or particular tobacco compounds exerting their effects in the following ways: (i) centrally, by eliciting dose-dependent neurotransmitter and neuroendocrine effects [42]; (ii) peripherally, by acting as a sympathetic nervous system (SNS) agonist; or (iii) by disrupting NO synthesis directly or indirectly by targeting biochemical precursors. Complex interactions among these pathways may also exist [43].
Aim
The present study was designed to help elucidate the mechanisms that underlie sexual functioning in women by which cigarette smoking may elicit deleterious consequences. As a first step to begin to understand these potential processes, nonsmoking women were tested; this was in order to rule out aforementioned confounds that may be specific to long-term smokers. This study extends previous research by (i) isolating nicotine, which is the primary pharmacological ingredient responsible for the acute cardiovascular effects of cigarette smoking; and (ii) providing the first empirical investigation of the acute effects of isolated nicotine on sexual arousal in nonsmoking women measured both physiologically (via vaginal photoplethysmography) and subjectively (via continuous self-report).
Methods
Participants
Participants were women recruited from an undergraduate psychology subject pool, and via local community and university advertisements. During an initial telephone interview, potential participants were screened for inclusion/exclusion criteria, and were told that they would receive nicotine during one of the experimental sessions. Entry criteria included people who were between the ages of 18 and 30 years, and who reported no more than 100 direct exposures to nicotine during their lifetime. Exclusion criteria were as follows: (i) current self-reported sexual complaints within domains of sexual desire, sexual arousal, and sexual pain, and/or a history of treatment for sexual dysfunction; (ii) use of medications known or believed to affect sexual or vascular functioning, with the exception of hormonal contraceptives; (iii) medical conditions known to affect sexual functioning, or that could make nicotine administration unsafe; (iv) mandibular problems, and/or bridgework or dentures; (v) history of high or low blood pressure (vi) having a sexually transmitted disease; (vii) having a nonheterosexual orientation; and (viii) no current involvement in a heterosexual relationship. Heterosexuality was operationally defined as self-report of exclusive, or predominant opposite-gender sexual feelings and/or behaviors (i.e., scores of 0, 1, or 2) as assessed using the Kinsey Sexual Orientation Scale [44]. Menstrual cycle phase was not controlled given that both physiological and subjective sexual arousal to erotic stimuli in laboratory situations is only minimally, if at all, influenced by the menstrual cycle [45,46].
Study Design and Procedure
The design and procedure of this study were identical to our counterpart study [37] investigating the acute effects of nicotine in nonsmoking men. In brief, this study consisted of two counterbalanced experimental conditions, to which eligible participants were randomly given either nicotine (6 mg; approximately equivalent to smoking one high-yield nicotine cigarette) or placebo, both administered double-blind in gum form.1 Participants had their heart rates and systolic and diastolic blood pressures monitored prior to drug administration and approximately 30 minutes after drug administration—when nicotine reaches its peak plasma nicotine level. Participants fit the vaginal photoplethysmograph and a 5-minute adaptation recording was taken to assess baseline arousal. Participants were randomized to view one of two 12.5-minute audiovisual sequences that consisted of a 1-minute display of the word “relax” followed by a 3-minute neutral (nonsexual) film segment, and then a 8.5-minute erotic film depicting heterosexual sexual activity. Participants were instructed to continuously monitor their level of subjective sexual arousal by moving a computer mouse positioned on an adjacent table. After assessment of sexual arousal, participants removed the gum, and completed questionnaires assessing any adverse effects. All participants provided written informed consent, and either received credit toward their psychology research requirement or were financially compensated ($30). The protocol was approved by the University of Texas at Austin Institutional Review Board.
Main Self-Report Outcome Measures
Subjective arousal (CSA) was measured continuously using a hand-controlled device [52] which consisted of a computer optical mouse mounted on a track divided into seven equally spaced intervals, where 0 indicated neutral, and 1 to 7 reflected increasingly higher levels of feeling sexually aroused. The position of the pointer, with respect to the y axis of the computer’s monitor, was recorded with a software program written in MatLab (The MathWorks, Inc., Natick, MA, USA). The signal was low-pass filtered (to 0.5 Hz), and digitized (40 Hz).
To screen for absence of sexual functioning, participants completed the Female Sexual Function Index (FSFI) [53] which is comprised of six subscales: sexual interest/desire (two items); sexual arousal (four items); lubrication (four items); orgasm (three items); sexual satisfaction (three items); and sexual pain (three items). Participants were excluded from analysis if they reported a total score of less than 26. This cut-off value has been demonstrated to have sensitivity of 0.81 and specificity of 0.86 to correctly classify women with and without sexual dysfunction [54]. Additionally, women were excluded if they reported an FSFI arousal score of less than 4.1. This cut-off was determined by taking the midpoint of the mean FSFI arousal score of women diagnosed with Female Sexual Arousal Disorder (M = 3.09) and that of controls (M = 5.08) [54].
A short version of the Profile of Mood States (POMS-SF) [55] was administered to examine whether changes in mood in response to nicotine administration may mediate sexual arousal responses (e.g., increased tension and/or confusion may distract one from processing sexually relevant cues, resulting in decreased sexual arousal). Mood responses were summarized as scores reflecting six mood states: tension (six items); depression (eight items); anger (seven items); fatigue (five items); confusion (five items); and vigor (six items). Scores on the six primary mood factors were summed (with vigor weighed negatively) to yield a total mood disturbance score. The POMS-SF has demonstrated acceptable internal consistency (Cronbach’s alpha values of 0.80 and higher) [55] and has proven sensitive to short- and long-term changes in mood [56–59]. Difference scores for all six mood factor scores as well as the total mood disturbance score were computed by subtracting the baseline (before nicotine or placebo administration), from the assessment taken 30 minutes after drug administration.
In order to assess any adverse effects attributed to either placebo or nicotine administration, participants completed a 10-item questionnaire developed in our laboratory that included both bogus (blurred vision, dry eyes, fatigue, runny nose, hiccups), and rationally driven (throat irritation, headache, nausea, light headedness, dizziness) items. Participants were asked to rate each of the items on a 5-point scale according to the degree to which they experienced each sensation, ranging from 0 (not at all) to 4 (extremely), and scores were summed within the two factors.
Main Physiological Outcome Measures
Genital arousal was assessed via vaginal photoplethysmography [60] to detect changes in vaginal pulse amplitude (VPA), an indicator of vaginal vasocongestion, specific to sexual arousal [61]. The raw signal was recorded in millivolts and sampled at a rate of 80 samples/second throughout the entire 180 seconds of neutral film and 510 seconds of erotic film, low-pass filtered (0.5–30 Hz), digitized (40 Hz), and recorded using the software package AcqKnowledge III, Version 3.73 (BIOPAC Systems, Inc., Santa Barbara, CA, USA) and a Model MP100WS data acquisition unit (BIOPAC Systems, Inc., Santa Barbara, CA, USA). Artifacts caused by movement or contractions of the pelvic muscles were deleted after visual inspection of the data [61].
Heart rates and systolic and diastolic blood pressures were assessed using an Omron HEM-712C automatic inflation digital blood pressure and pulse monitor (Omron Healthcare, Inc., Ban-nockburn, IL, USA) prior to gum administration and at 30 minutes following administration of nicotine or placebo. Heart rates during the film sequence presentations were extracted from the vaginal photoplethysmography signal. Heart rates were averaged separately across the neutral and erotic films, yielding a total of four heart rate measures (one prior to drug administration, one 30 minutes after drug administration, two during the film sequence) for each participant per experimental condition.
Data Reduction
In accordance with other studies assessing physiological sexual arousal [62,63], both genital and self-report arousal measures were z-transformed across both experimental conditions within-subjects in order to attenuate the effects of idiosyncratic variation in responsiveness. Final VPA and CSA scores were then computed for both the neutral and erotic films by averaging across the neutral and erotic stimuli. Because not all participants demonstrate sufficient sexual arousal for valid assessment, their physiological and subjective data were removed from analyses if the minimum response to sexual stimuli did not exceed their response to the neutral stimulus by at least 0.5 standard deviations within the placebo condition. The exclusion criteria are similar to that used by other researchers [64] and yielded the exclusion of two participants with respect to analyses of physiological sexual arousal. All participants demonstrated reliable CSA responses. Excluding non-responders was particularly important in order to distinguish physiological attenuation attributed to nicotine administration from idiosyncratic non-responsiveness otherwise not because of nicotine intake.
Statistical Analysis
Initial Pearson product moment correlation coefficients were calculated to investigate potential confounding variables with respect to sexual arousal indices. Specifically, age and a participant’s body nicotine concentration (body weight is inversely proportional to plasma nicotine concentration level) measured in μg/kg where entered as independent variables with participants’ levels of physiological and subjective sexual arousal as dependent measures. None of the analyses were statistically significant (all Ps > 0.05; all R2s < 0.10) and therefore neither age nor body nicotine concentration was entered as covariates in subsequent analyses.
A 2 (condition: nicotine, placebo) × 2 (film: neutral, erotic) repeated measures analysis of variance (ANOVA) was used to examine the effects of nicotine in comparison with placebo on standardized VPA and CSA scores. The effects of nicotine in comparison with placebo on heart rate and systolic and diastolic blood pressure scores were examined using separate condition × time repeated measures ANOVAs. Paired samples t-tests were used on standardized VPA and CSA cores, and heart rate scores between and within the nicotine and placebo conditions during the neutral and erotic film presentations, on heart rate and systolic and diastolic blood pressure scores prior to and 30 minutes after either nicotine or placebo administration, and on subjective ratings of mood, and on both potential and bogus nicotine-induced adverse effects, between the placebo and nicotine conditions.
All analyses were performed using SPSS statistical software version 14.0 (SPSS, Inc., Chicago, IL, USA). A two-tailed α of P < 0.05 was considered statistically reliable for all analyses with the exception of analyses of self-reported mood and adverse effects in which more conservative α levels of 0.007 (P < 0.05/7), and 0.025 (P < 0.05/2) were used, respectively, by employing Bonferroni corrections. Standardized effect sizes (i.e., Cohen’s d) were reported when comparing two groups. Measures of variance, such as η2 and R2, were reported when comparing more than two groups and magnitude of association, respectively. All variances, effect sizes, and post hoc power analyses were calculated according to the guidelines proposed by Cohen [65].
Results
Sample Characteristics
Fifty-one women completed the initial telephone screening. Of these individuals, 11 reported being uninterested in participating, seven were ineligible, and eight did not show for their appointments. Twenty-five women met initial inclusion criteria and completed the two experimental sessions. Of these participants, data on five women were excluded from subsequent analyses because they did not meet the two-fold FSFI cut-off criteria. The final sample (N = 20) had a mean age of 20.2 years (SD, 2.26; range, 18–25), reported a mean of 4.9 (SD, 8.52; range, 0–30) direct exposures to nicotine during their lifetime, and all women reported no passive exposure to tobacco smoke for more than 30 minutes/day at least once per week. One participant reported a medical condition (asthma), three reported currently taking antihistamines, and one participant reported being diagnosed with anxiety, although the particular type was not specified. Of the 11 women reporting current hormonal contraceptive use, seven reported using oral contraceptives, two reported using a contraceptive vaginal ring, one participant followed a quarterly hormonal injection regimen, and one did not specify type. The mean duration of hormonal contraceptive use was 2.1 years (SD, 1.39; range 0.2–4.0). Characteristics of the participant sample are presented in Table 1.
Table 1.
Participant characteristics (N = 20)
| Characteristic | Value |
|---|---|
| Age (years) | |
| Mean (SD) | 20.2 (2.26) |
| Range | 18–25 |
| Education (years) | |
| Mean (SD) | 13.6 (1.64) |
| Range | 12–18 |
| Weight (kg) | |
| Mean (SD) | 63.0 (13.18) |
| Range | 45.8–99.8 |
| Height (m) | |
| Mean (SD) | 1.7 (0.87) |
| Range | 1.52–1.83 |
| Body mass index (kg/m2) | |
| Mean (SD) | 23.5 (4.96) |
| Range | 17.3–40.2 |
| Ethnicity, N (%) | |
| European American | 9 (45) |
| African American | 3 (15) |
| Latino | 4 (20) |
| Asian | 3 (15) |
| Other | 1 (5) |
| Current hormonal contraceptive use, N (%)* | 11 (58) |
| FSFI arousal score† | |
| Mean (SD) | 5.4 (0.60) |
| Range | 4.2–6.0 |
| FSFI total score‡ | |
| Mean (SD) | 30.6 (2.57) |
| Range | 26.4–34.2 |
| Nicotine direct§ exposures (lifetime) | |
| Mean (SD) | 4.9 (8.52) |
| Range | 0–30 |
| Nicotine body concentration (μg/kg) | |
| Mean (SD) | 98.9 (18.83) |
| Range | 60.1–131.0 |
Datum was missing for one participant.
Mean FSFI arousal score is based on a scale of 0 to 6, with 0 indicating the most severe sexual arousal difficulties and 6 indicating the least severe (or no difficulty).
Mean FSFI total score is based on a scale of 2 to 36, with 2 indicating the most severe sexual difficulties and 36 indicating the least severe (or no difficulty).
A direct exposure to nicotine was defined as ingesting nicotine pulmonarily (e.g., smoking a cigarette, cigar, or pipe), or buccally (e.g., chewing smokeless tobacco), as opposed to passive nicotine exposure which was defined as ingesting nicotine via indirect means (i.e., passive smoke exposure).
FSFI = Female Sexual Function Index.
Analyses of Physiological Sexual Arousal
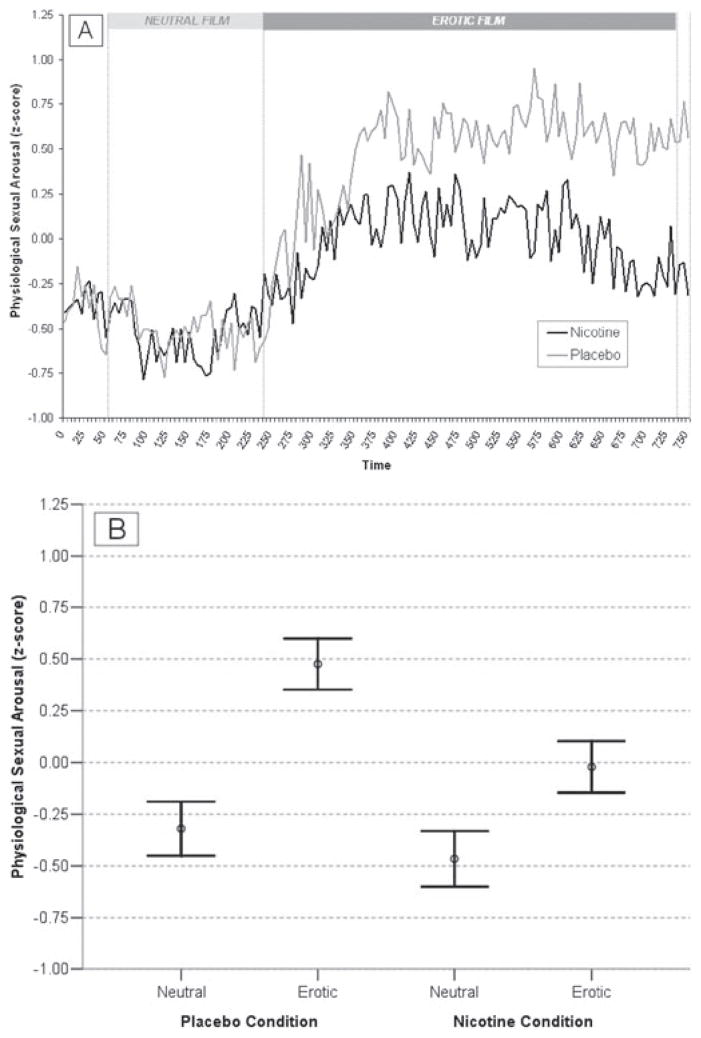
With respect to participants that produced reliable physiological sexual arousal responses (N = 18), a repeated measures ANOVA with condition (nicotine, placebo) and film type (neutral, erotic) as within-subjects factors revealed a significant main effect of the erotic films on standardized VPA scores (F1,17 = 29.79, P < 0.001, η2 = 0.64) and a significant interaction between condition and film (F1,17 = 5.61, P = 0.03, η2 = 0.25). Specifically, significant increases in standardized VPA responses to the erotic films were demonstrated in both nicotine (t17 = 2.78, P = 0.01, d = 0.65) and placebo (t17 = 7.55, P < 0.001, d = 1.78) conditions indicating that the audiovisual stimuli were effective in eliciting reliable physiological sexual responses. However, participants demonstrated significantly less physiological sexual arousal in response to nicotine administration during the erotic films compared with placebo (t17 = −2.10, P = 0.05, d = 0.49). This occurred in 11 of 18 women and corresponded to a 30% reduction in physiological sexual arousal. There was no significant difference in standardized VPA scores between nicotine and placebo conditions during the neutral films (t17 = 0.71, P = 0.49, d = 0.17). Mean standardized VPA scores for the nicotine and placebo conditions during the neutral and erotic film stimuli are presented in Figure 1.
Figure 1.
Physiological sexual arousal in response to drug administration. (A) Mean vaginal pulse amplitude in 5-second intervals across the neutral and erotic film stimuli during nicotine and placebo conditions. Data have been averaged across participants to aid in visual interpretation; however, all statistical analyses were conducted within subjects. (B) Mean vaginal pulse amplitude between the neutral stimulus and the erotic film stimulus during nicotine (N = 18) and placebo (N = 18) conditions. Open circles represent means and error bars represent standard errors of the means. Units are within-subjects standard deviations.
Analyses of Continuous Subjective Sexual Arousal
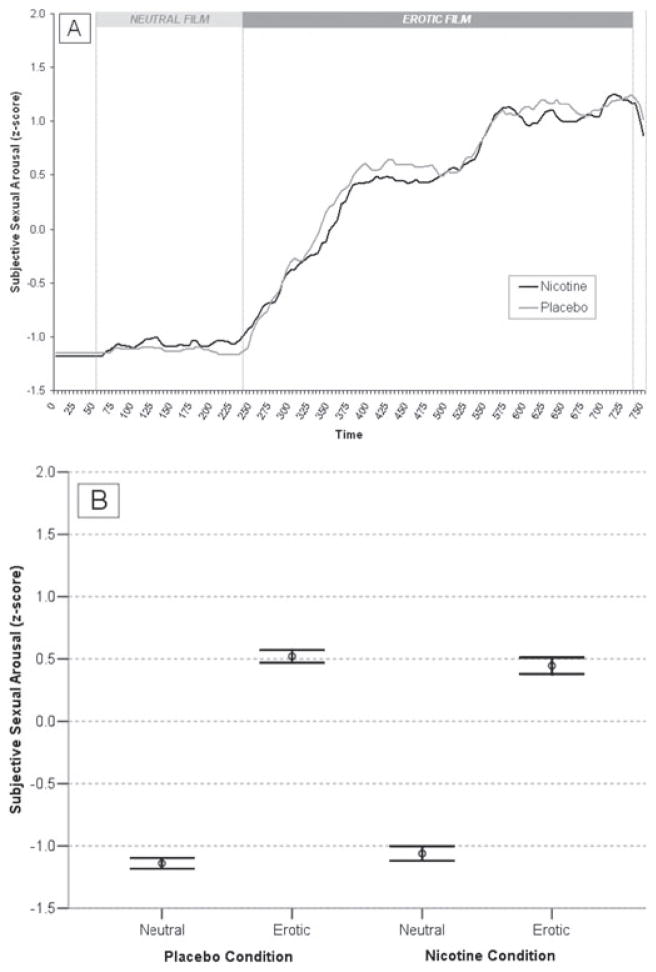
Data from four participants were not interpretable because of equipment and/or software malfunction, and therefore analyses of self-reported sexual arousal were conducted on the remaining subsample with valid assessments (N = 16). The condition (nicotine, placebo) × film (neutral, erotic) repeated measures ANOVA revealed a significant main effect of the erotic films on standardized CSA scores (F1,15 = 1,108.01, P < 0.001, η2 = 0.99), but no significant interaction between condition and film (F1,15 = 2.01, P = 0.18, η2 = 0.12). Significant increases in standardized CSA scores were demonstrated in response to the erotic films in both the nicotine (t15 = 19.19, P < 0.001, d = 4.80) and placebo (t15 = 30.48, P < 0.001, d = 7.62) conditions, indicating that the audiovisual film stimuli effectively elicited reliable subjective sexual arousal responses. However, there was no significant between-condition difference in mean standardized CSA scores during the neutral (t15 = 0.92, P = 0.37, d = 0.23) or erotic (t15 = 0.87, P = 0.45, d = 0.20) films indicating that nicotine did not differentially affect subjective sexual responding. Mean standardized CSA scores for the nicotine and placebo conditions during the neutral and erotic film stimuli are presented in Figure 2.
Figure 2.
Subjective sexual arousal in response to drug administration. (A) Mean self-report sexual arousal in 5-second intervals across the neutral and erotic film stimuli during nicotine and placebo conditions. Data have been averaged across participants to aid in visual interpretation; however, all statistical analyses were conducted within subjects. (B) Mean self-report sexual arousal between the neutral stimulus and the erotic film stimulus during nicotine (N = 16) and placebo (N = 16) conditions. Open circles represent means and error bars represent standard errors of the means. Units are within-subjects standard deviations.
Analyses of Heart Rate
The condition (nicotine, placebo) × time (four time measures: one prior to drug administration, one 30 minutes after drug administration, two during the film sequence) repeated measures ANOVA revealed a statistical trend for a main effect of condition (F1,19 = 3.51, P = 0.076, η2 = 0.16) as well as a significant condition × time interaction (F1,19 = 4.96, P = 0.01, η2 = 0.47). No significant between-condition differences in heart rate were demonstrated prior to drug administration (t19 = 0.22, P = 0.83, d = 0.05); however, participants showed significantly higher heart rates at 30 minutes after the administration of nicotine compared with placebo (t19 = 2.94, P = 0.01, d = 0.66), and during the erotic (approximately 38 minutes after nicotine administration), film presentation after nicotine administration (t19 = 2.61, P = 0.02, d = 0.58). Additionally, participants demonstrated a statistical trend for higher heart rates during the neutral (approximately 35 minutes after nicotine administration) film stimuli after nicotine administration compared with placebo (t19 = 1.95, P = 0.067, d = 0.43). These findings suggest that nicotine was demonstrating its effects on cardiovascular function during assessment of sexual arousal. Heart rates did not differ within conditions between any of the cardiovascular assessments (all Ps > 0.05). Mean heart rates in beats per minute (±SD) prior to and 30 minutes after placebo administration, as well as during both the neutral and erotic film stimuli within the placebo condition were 83.8 (±7.7), 78.9 (±8.3), 81.4 (±8.4), and 81.7 (±7.9), respectively. Mean heart rates prior to and 30 minutes after nicotine administration, as well as during both the neutral and erotic film stimuli within the nicotine condition were 83.1 (±9.4), 86.7 (±8.7), 86.0 (±8.5), and 87.1 (±8.8), respectively.
Analyses of Blood Pressure
There were no significant effects of condition or time, and no significant interaction between condition and time for either systolic or diastolic blood pressure scores (all Ps > 0.05). Mean blood pressure scores in mm Hg (±SD) prior to placebo administration, 30 minutes after placebo administration, prior to nicotine administration, and 30 minutes after nicotine administration, were 111.8 (±10.6), 112.5 (±9.0), 113.5 (±9.2), and 115.0 (±11.0), respectively.
Analyses of Mood
One participant did not give self-reported mood ratings during one experimental session and therefore this participant was excluded from analyses of mood. Data from remaining participants (N = 19) indicated that there were no significant effects of condition for any of the six mood factor scores (all Ps > 0.05) nor for the overall mood disturbance score (t18 = −1.33, P = 0.20, d = 0.31) indicating that changes in mood in response to drug administration did not change differentially between placebo and nicotine conditions.
Analyses of Adverse Effects
Two participants did not give self-reported ratings of adverse effects during one of the experimental sessions and therefore data from these participants were not included within analyses of adverse effects. Data from remaining participants (N = 18) indicated a significant increase in self-reported ratings of both bogus (t17 = 3.08, P < 0.01, d = 0.73) and potential (t17 = 5.56, P < 0.001, d = 1.31) adverse effects in response to nicotine administration.
Post Hoc Analyses
Participants reported more adverse effects during the nicotine condition compared with the placebo condition, and therefore we investigated whether subjective ratings of nicotine-induced symptomatology covaried with physiological sexual arousal. Difference scores were separately derived within subjects for both standardized VPA scores and potential adverse effects scores. Values assessed during the placebo condition were subtracted from values assessed during the nicotine condition (i.e., VPA nicotine condition minus VPA placebo condition; adverse effects nicotine condition minus adverse effects placebo condition) for women displaying reliable genital arousal and were entered into a regression model. This comprised a sub-sample of 16 participants. Results of the analysis indicated that the correlation was not statistically significant (r14 = −0.13, P = 0.64, R2 = 0.016) and the magnitude of self-reported adverse effects accounted for less than 2% of the variance in physiological sexual arousal. That is, there was no statistical relationship between increased drug symptomatology and reduced genital response.
Given that the majority of participants reported currently using hormonal contraceptives, we conducted a follow-up analysis in order to determine whether statistically significant findings with respect to nicotine’s attenuating effects on genital responses were a result of hormonal contraceptive use. Difference scores were derived within subjects by subtracting each participant’s mean standardized VPA score during the neutral stimulus from her mean standardized VPA score during the erotic stimulus for both the placebo and nicotine conditions for women displaying reliable genital arousal. This comprised a subsample of 17 participants. A 2 (condition: nicotine, placebo) × 2 (contraceptive status: current hormonal contraceptive use, no current hormonal contraceptive use) repeated measures ANOVA revealed a significant main effect of condition (F1,15 = 10.08, P < 0.01, η2 = 0.40), but no significant interaction between condition and contraceptive status (F1,15 = 1.98, P = 0.18, η2 = 0.12). This indicated that irrespective of hormonal contraceptive status, women demonstrated significantly less genital responses during the nicotine condition compared with placebo. However, visual inspection of the data suggested a trend that women taking hormonal contraceptives were less likely to demonstrate impaired physiological sexual arousal in response to nicotine administration (see Figure 3). Although a total of 12 of 17 women demonstrated less genital arousal during the nicotine condition compared with the placebo condition, a disproportionate number of women who reported no current hormonal contraceptive use (six of seven women) demonstrated nicotine-induced attenuated arousal compared with those who reported currently using hormonal contraceptives (six of 10 women).
Figure 3.
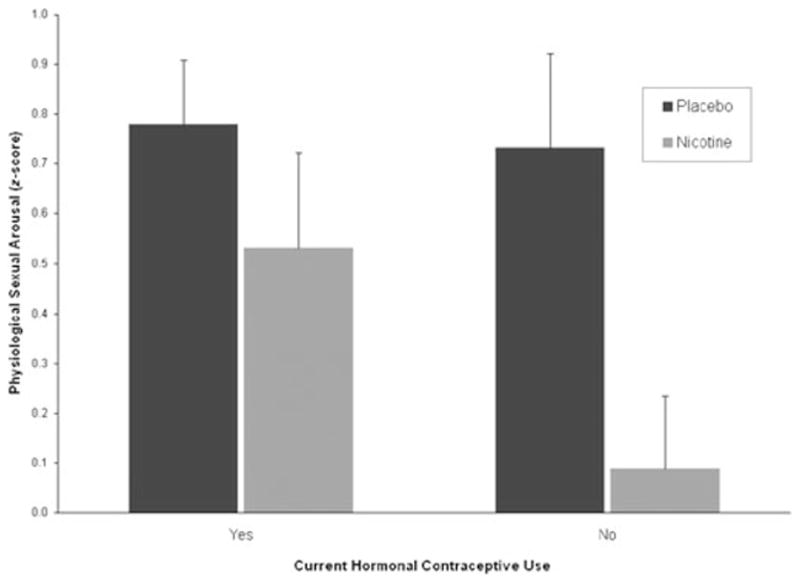
Physiological sexual arousal as a function of experimental condition and hormonal contraceptive use. Bars represent mean vaginal pulse amplitude (VPA) difference scores (mean VPA during the erotic stimulus minus mean VPA during the neutral stimulus) during the nicotine and placebo conditions for those reporting hormonal contraceptive use (N = 10) and those not reporting hormonal contraceptive use (N = 7) at time of testing. Error bars represent standard errors of the means. Units are within-subjects standard deviations.
Discussion
The current study examined the acute effects of isolated nicotine, an adrenergic agonist, on physiological and subjective sexual arousal responses in healthy nonsmoking women. Results indicated that nicotine significantly attenuated physiological sexual arousal to erotic stimuli. On one hand, these results are consistent with literature delineating nicotine’s effects on instigating cardiovascular constriction via SNS activation [66]. On the other hand, these findings are inconsistent with a growing body of literature suggesting a curvilinear relationship between SNS activity and sexual arousal, such that moderate levels facilitate, high levels inhibit, and low levels of SNS activation have less of a facilitatory effect on sexual arousal responses [67–69]. In order to examine the magnitude of nicotine-induced SNS activity, percentage of maximum heart rate was derived for each participant.2 Mean (±SD) SNS activity was 45.3% HRmax ± 4.56 during the nicotine condition which corresponded to a low to moderate level of SNS activity [71]. This is contradictory to prior research indicating that SNS activation of a similar magnitude facilitates rather than attenuates physiological sexual arousal in healthy sexually functional women. It is possible that nicotine diminished genital arousal in women via central nervous system effects or by directly targeting biochemical mechanisms underlying NO synthesis. Given there is more direct evidence substantiating the role of NO mechanisms within the clitoris compared with within vaginal epithelia [23,72], an investigation of nicotine’s effect on genital arousal using clitoral Doppler ultrasonography as opposed to vaginal photoplethysmography would be a better methodology for testing this latter hypothesis.
Nicotine did not significantly affect self-reported sexual arousal. Because nicotine may have induced a variety of undesirable effects (e.g., dizziness, throat irritation) that could have distracted women from processing sexual cues, the absence of nicotine-induced attenuation in subjective sexual arousal supports the notion that nicotine reduces genital arousal directly via physiological mechanisms, rather than indirectly by impacting cognitive processes. Similar to subjective measures of sexual arousal, experimental condition did not moderate self-reported measures of mood. Taken together, these findings suggest that diminution in genital sexual arousal in response to nicotine treatment is not likely a byproduct of nicotine’s effects on cognitive states.
More adverse effects were reported in response to nicotine administration compared with placebo which is consistent with studies investigating physical effects of nicotine replacement therapies in never-smokers [73,74]. It is essential to distinguish whether subjective ratings of adverse effects potentially confounded the relationship between the psychopharmacological effects of nicotine and attenuated physiological sexual arousal. Post hoc analyses revealed no relationship between reduced genital arousal and increased drug symptomatology. This indicates that reduction in sexual arousal in response to nicotine administration is likely to be directly attributable to underlying biochemical and physiological involvement rather than an epiphenomenon of adverse effects.
Strengths of the present investigation include: (i) administration of isolated nicotine in gum form which established relatively fast and stable plasma nicotine concentration levels; (ii) assessing only young healthy women without a history of smoking, thereby precluding potential cardiovascular consequences that may deleteriously affect sexual functioning. Additionally, no women reported any incidence of passive smoke exposure, effects of which may have vascular consequences [75]; (iii) use of a randomized, double-blind, placebo-controlled, cross-over protocol; and (iv) assessment of continuous subjective and physiological sexual responses using rigorous quantitative methods.
Several limitations of this study warrant mention. First, participants demonstrated increments in heart rates in response to nicotine administration that could often be detected by the experimenters. Although a thorough protocol was maintained in order to preserve double-blindness, it is, for the most part, infeasible to preserve experimenter blindness in studies investigating cardiovascular effects of adrenergic agents. Second, expectancies about drug content or its actions may be responsible for observable drug-like effects [76]. Eighteen of 20 women correctly identified the session during which they ingested nicotine, and it is possible that participants’ expectancies concerning nicotine’s effects on sexual arousal may have influenced the results of this study. However, if there were participant expectancies at play—whether they were with respect to nicotine’s potential facilitory or inhibitory effect on sexual functioning—they would most likely have expressed themselves within the self-report measure of sexual arousal. Because this measure did not differ between nicotine and placebo conditions, it is unlikely that expectancy effects accounted for the differential changes in physiological arousal. Another limitation is with respect to the method of nicotine delivery. Nicotine was administered via commercially manufactured set doses within gum pieces, a format which cannot be standardized for participant body weight with a reasonable degree of precision. Consequently, moderate variability in plasma nicotine concentrations would have been present among the participant sample. Although women’s body nicotine concentrations were not correlated with their magnitude of subjective or physiological sexual responses, individual differences in nicotine metabolism may exist, irrespective of nicotine dosing [77].
The majority of women who participated in this study reported using hormonal contraceptives which could be an important moderator with respect to the relationship between nicotine and sexual arousal. Although post hoc analyses indicated that there was no statistically significant interaction with respect to hormonal contraceptive status and experimental condition, a clear trend was observed suggesting that women taking hormonal contraceptives were less likely to demonstrate impaired physiological sexual arousal in response to nicotine administration. This is in line with evidence suggesting that nicotine metabolism is faster in women taking oral contraceptives compared with those who are not [78]. Future studies of this nature would benefit from including larger heterogeneous samples in order to establish what factors (e.g., formulation, duration of use), if any, pertaining to hormonal contraceptive use interact with nicotine’s acute effects on genital hemodynamic processes.
A final limitation is with respect to the overall sample size. Although this study used a cross-over protocol which increases statistical power, the sample size (N = 20) was still quite low. It was not possible to conclude with a reasonable degree of certainty (i.e., Power ≥ 0.80) that—given the observed effect sizes—nicotine was not exerting moderating effects with respect to analyses of subjective sexual arousal (Power = 0.26), as well as post hoc analyses of adverse nicotine effects (Power = 0.10) and hormonal contraceptive use (Power = 0.18).
This study was conducted in nonsmoking women in order to examine the pure effects of nicotine on physiological and psychological processes. Clearly, additional studies are needed in order to determine whether these results hold true for women who are current long-term smokers. Addressing import issues with respect to the effects of smoking on sexual arousal, such as (i) a participant’s experience with nicotine (novelty effects vs. potential physiological habituation); or (ii) duration-dependent deleterious effects of long-term smoking, would be necessary in order to generalize the results of the current study to women who smoke.
Conclusion
The results of the present study provide the first empirical evidence that isolated nicotine significantly reduces physiological sexual arousal in healthy, young, nonsmoking women. Our findings provide support to the hypothesis that nicotine may be the primary pharmacological agent responsible for genital hemodynamic disruption, thereby facilitating a cascade of biochemical and vascular events of which may impair normal sexual arousal responses. Additional studies using larger sample sizes as well as studies incorporating differing physiological assessments of sexual arousal would be beneficial in order to further elucidate the specific mechanisms by which nicotine may deleteriously affect women’s sexual functioning.
Acknowledgments
This study was presented at the annual meeting of the International Society for the Study of Women’s Sexual Health; February 23rd, 2007, Orlando, Florida; and the 33rd annual meeting of the International Academy of Sex Research; August 9th, 2007, Vancouver, British Columbia. This study was supported by Grant 5 RO1 AT00224-02 from the National Center for Complementary and Alternative Medicine to Cindy Meston. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Complementary and Alternative Medicine. The authors had no conflicts of interest with respect to financial interests, relationships, and/or affiliations relevant to the subject of this manuscript, and had full control of all data. The authors thank Muhannad Al Salayta, Ryan Adkins, Molly Rand, Elizabeth Aranda, and Yailin Ramirez for help with subject recruitment, participant testing, and data acquisition, and all study participants without whom this study would not have been possible.
Footnotes
Conflict of Interest: None declared.
Studies that have used similar nicotine preparations have reported that one 4-mg nicotine gum piece increases plasma nicotine levels by approximately 8–10 ng/mL within 30 minutes, and has a half-life of approximately 120 minutes [47–50]. Comparatively, a high-yield (0.7–1.2 mg) nicotine cigarette increases plasma nicotine levels by approximately 14 ng/mL within 10 minutes [51]. Six mg of nicotine gum was administered such that a participant’s plasma nicotine level would be comparable to smoking one cigarette.
HRmax = 206.3 – 0.711 (age) [70]. Percentage of maximum heart rate (% HRmax) was calculated with the following formula: [(χ/HRmax) × 100], where χ denotes each participant’s mean heart rate during the erotic film presentation during the nicotine condition.
Statement of Authorship
-
Conception and DesignChristopher B. Harte; Cindy M. Meston
-
Acquisition of DataChristopher B. Harte
-
Analysis and Interpretation of DataChristopher B. Harte
-
Drafting the ArticleChristopher B. Harte
-
Revising It for Intellectual ContentChristopher B. Harte; Cindy M. Meston
-
Final Approval of the Completed ArticleChristopher B. Harte; Cindy M. Meston
References
- 1.Lam TH, He Y, Li LS, Li LS, He SF, Liang BQ. Mortality attributable to cigarette smoking in China. JAMA. 1997;278:1505–8. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Annual smoking-attributable mortality, years of potential life lost, and economic costs-United States, 1995–1999. MMWR Morb Mortal Wkly Rep. 2002;51:300–3. [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services. The health consequences of smoking: A report of the surgeon general. Washington, DC: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2004 National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Google Scholar]
- 4.U.S. Department of Health and Human Services. Reducing the health consequences of smoking—25 years of progress: a report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, CDC; 1989. [Google Scholar]
- 5.U.S. Department of Health and Human Services. Tobacco use among U.S. racial/ethnic minority groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, CDC; 1998. [PubMed] [Google Scholar]
- 6.Fielding JE, Husten CG, Eriksen MP. Tobacco: Health effects and control. In: Maxcy KF, Rosenau MJ, Last JM, Wallace RB, Doebbling BN, editors. Public health and preventative medicine. New York: McGraw-Hill; 1998. pp. 817–45. [Google Scholar]
- 7.Fagerström K. The epidemiology of smoking: Health consequences and benefits of cessation. Drugs. 2002;62(suppl 2):1–9. doi: 10.2165/00003495-200262002-00001. [DOI] [PubMed] [Google Scholar]
- 8.Global Youth Tobacco Survey Collaborating Group. Differences in worldwide tobacco use by gender: Findings from the Global Youth Tobacco Survey. J Sch Health. 2003;73:207–15. doi: 10.1111/j.1746-1561.2003.tb06562.x. [DOI] [PubMed] [Google Scholar]
- 9.Condra M, Morales A, Owen JA, Surridge DH, Fenemore J. Prevalence and significance of tobacco smoking in impotence. Urology. 1986;27:495–8. doi: 10.1016/0090-4295(86)90326-2. [DOI] [PubMed] [Google Scholar]
- 10.Shabsigh R, Fishman IJ, Schum C, Dunn JK. Cigarette smoking and other vascular risk factors in vasculogenic impotence. Urology. 1991;38:227–31. doi: 10.1016/s0090-4295(91)80350-g. [DOI] [PubMed] [Google Scholar]
- 11.Juenemann KP, Lue TF, Luo JA, Benowitz NL, Abozeid M, Tanagho EA. The effect of cigarette smoking on penile erection. J Urol. 1987;138:438–41. doi: 10.1016/s0022-5347(17)43181-8. [DOI] [PubMed] [Google Scholar]
- 12.Austoni E, Mirone V, Parazzini F, Fasolo CB, Turchi P, Pescatori ES, Ricci E, Gentile V Andrology Prevention Week Centres, Italian Society of Andrology. Smoking as a risk factor for erectile dys-funtion: Data from the andrology Prevention Weeks 2001–2002 a study of the Italian Society of andrology (s.I.a.) Eur Urol. 2005;48:810–7. doi: 10.1016/j.eururo.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Feldman HA, Johannes CB, Derby CA, Kleinman KP, Mohr BA, Araujo AB, McKinlay JB. Erectile dysfunction and coronary risk factors: Prospective results from the Massachusetts male aging study. Prev Med. 2000;30:328–38. doi: 10.1006/pmed.2000.0643. [DOI] [PubMed] [Google Scholar]
- 14.Lam TH, Abdullah AS, Ho LM, Yip AW, Fan S. Smoking and sexual dysfunction in Chinese males: Findings from men’s health survey. Int J Impot Res. 2006;18:364–9. doi: 10.1038/sj.ijir.3901436. [DOI] [PubMed] [Google Scholar]
- 15.Dorey G. Is smoking a cause of erectile dysfunction? A literature review. Br J Nurs. 2001;10:455–65. doi: 10.12968/bjon.2001.10.7.5331. [DOI] [PubMed] [Google Scholar]
- 16.Jeremy JY, Mikhailidis DP. Cigarette smoking and erectile dysfunction. J R Soc Health. 1998;118:151–5. doi: 10.1177/146642409811800305. [DOI] [PubMed] [Google Scholar]
- 17.Mannino DM, Klevens RM, Flanders WD. Cigarette smoking: An independent risk factor for impotence? Am J Epidemiol. 1994;140:1003–8. doi: 10.1093/oxfordjournals.aje.a117189. [DOI] [PubMed] [Google Scholar]
- 18.Mirone V, Imbimbo C, Bortolotti A, Di Cintio E, Colli E, Landoni M, Lavezzari M, Parazzini F. Cigarette smoking as risk factor for erectile dysfunction: Results from an Italian epidemiological study. Eur Urol. 2002;41:294–7. doi: 10.1016/s0302-2838(02)00005-2. [DOI] [PubMed] [Google Scholar]
- 19.Moreira ED, Jr, Kim SC, Glasser D, Gingell C. Sexual activity, prevalence of sexual problems, and associated help-seeking patterns in men and women aged 40–80 years in Korea: Data from the Global Study of Sexual Attitudes and Behaviors (GSSAB) J Sex Med. 2006;3:201–11. doi: 10.1111/j.1743-6109.2006.00210.x. [DOI] [PubMed] [Google Scholar]
- 20.Oksuz E, Malhan S. Prevalence and risk factors for female sexual dysfunction in Turkish women. J Urol. 2006;175:654–8. doi: 10.1016/S0022-5347(05)00149-7. [DOI] [PubMed] [Google Scholar]
- 21.Safarinejad MR. Female sexual dysfunction in a population-based study in Iran: Prevalence and associated risk factors. Int J Impot Res. 2006;18:382–95. doi: 10.1038/sj.ijir.3901440. [DOI] [PubMed] [Google Scholar]
- 22.Cayan S, Akbay E, Bozlu M, Canpolat B, Acar D, Ulusoy E. The prevalence of female sexual dysfunction and potential risk factors that may impair sexual function in Turkish women. Urol Int. 2004;72:52–7. doi: 10.1159/000075273. [DOI] [PubMed] [Google Scholar]
- 23.Rosen RC, McKenna KE. PDE-5 inhibition and sexual response: Pharmacological mechanisms and clinical outcomes. Ann Rev Sex Res. 2002;13:36–88. [PubMed] [Google Scholar]
- 24.Kim N, Azadzoi KM, Goldstein I, Saenz de Tejada I. A nitric oxide-like factor mediates nonadrenergic-noncholinergic neurogenic relaxation of penile corpus cavernosum smooth muscle. J Clin Invest. 1991;88:112–8. doi: 10.1172/JCI115266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burnett AL, Lowenstein CJ, Bredt DS, Chang TS, Snyder SH. Nitric oxide: A physiologic mediator of penile erection. Science. 1992;257:401–3. doi: 10.1126/science.1378650. [DOI] [PubMed] [Google Scholar]
- 26.Kim SW, Jeong SJ, Munarriz R, Kim NN, Gold-stein I, Traish AM. Role of the nitric oxide-cyclic GMP pathway in regulation of vaginal blood flow. Int J Impot Res. 2003;15:355–61. doi: 10.1038/sj.ijir.3901038. [DOI] [PubMed] [Google Scholar]
- 27.Mazo E, Gamidov S, Anranovich S, Iremashvili V. Testing endothelial function of brachial and cavernous arteries in patients with erectile dysfunction. J Sex Med. 2005;3:323–30. doi: 10.1111/j.1743-6109.2005.00098_1.x. [DOI] [PubMed] [Google Scholar]
- 28.Zeiher AM, Schachinger V, Minners J. Long-term cigarette smoking impairs endothelium-dependent coronary arterial vasodilator function. Circulation. 1995;92:1094–100. doi: 10.1161/01.cir.92.5.1094. [DOI] [PubMed] [Google Scholar]
- 29.Chalon S, Moreno H, Benowitz NL, Hoffman BB, Blaschke TE. Nicotine impairs endothelium-dependent dilatation in human veins in vivo. Clin Pharmacol Ther. 2000;67:391–7. doi: 10.1067/mcp.2000.105153. [DOI] [PubMed] [Google Scholar]
- 30.McMahon CG, Touma K. Predictive value of patient history and correlation of nocturnal penile tumescence, colour duplex Doppler ultrasonography and dynamic cavernosometry and cavernosography in the evaluation of erectile dysfunction. Int J Impot Res. 1999;11:47–51. doi: 10.1038/sj.ijir.3900369. [DOI] [PubMed] [Google Scholar]
- 31.McVary KT, Carrier S, Wessells H. Subcommittee on smoking and erectile dysfunction socioeconomic committee sexual medicine society of North America. Smoking and erectile dysfunction: Evidence based analysis. J Urol. 2001;166:1624–32. [PubMed] [Google Scholar]
- 32.Elhanbly S, Abdel-Gaber S, Fathy H, El-Bayoumi Y, Wald M, Niederberger CS. Erectile dysfunction in smokers: A penile dynamic and vascular study. J Androl. 2004;25:991–5. doi: 10.1002/j.1939-4640.2004.tb03172.x. [DOI] [PubMed] [Google Scholar]
- 33.Gilbert DG, Hagen RL, D’Agostino JA. The effects of cigarette smoking on human sexual potency. Addict Behav. 1986;11:431–4. doi: 10.1016/0306-4603(86)90022-5. [DOI] [PubMed] [Google Scholar]
- 34.Pittilo RM, Woolf N. Cigarette smoking, endothelial cell injury and atherosclerosis. J Smok Rel Disord. 1993;4:17–25. [Google Scholar]
- 35.Herning RI, Jones RT, Benowitz NL, Mines AH. How a cigarette is smoked determines nicotine blood levels. Clin Pharmacol Ther. 1983;33:84–90. doi: 10.1038/clpt.1983.12. [DOI] [PubMed] [Google Scholar]
- 36.Brandon TH, Juliano LM, Copeland AL. Expectancies for tobacco smoking. In: Kirsch I, editor. How expectancies shape experience. Washington, DC: American Psychological Association; 1999. pp. 263–9. [Google Scholar]
- 37.Harte CB, Meston CM. Acute effects of nicotine on physiological and subjective sexual arousal in nonsmoking men: A randomized, double-blind, placebo-controlled trial. J Sex Med. 2008;5:110–21. doi: 10.1111/j.1743-6109.2007.00637.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klinge E, Alaranta A, Sjöstrand NO. Pharmacological analysis of nicotinic relaxation of bovine retractor penis muscle. J Pharmacol Exp Ther. 1988;245:280–6. [PubMed] [Google Scholar]
- 39.Mayhan WG, Patel KP. Effect of nicotine on endothelium-dependent arteriolar dilation in vivo. Am J Physiol. 1997;272:H2337–42. doi: 10.1152/ajpheart.1997.272.5.H2337. [DOI] [PubMed] [Google Scholar]
- 40.D’amati G, di Gioia CR, Bologna M, Giordano D, Giorgi M, Dolci S, Jannini EA. Type phosphodi-esterase expression in the human vagina. Urology. 2002;60:191–5. doi: 10.1016/s0090-4295(02)01663-1. [DOI] [PubMed] [Google Scholar]
- 41.Burnett AL, Calvin DC, Silver RL, Peppas DS, Docimo SG. Immunohistochemical description of nitric oxide synthase isoforms in human clitoris. J Urol. 1997;158:75–8. doi: 10.1097/00005392-199707000-00020. [DOI] [PubMed] [Google Scholar]
- 42.Pomerleau OF. Nicotine and the central nervous system: Biobehavioral effects of cigarette smoking. Am J Med. 1992;93:2S–7S. doi: 10.1016/0002-9343(92)90619-m. [DOI] [PubMed] [Google Scholar]
- 43.Sartori C, Lepori M, Scherrer U. Interaction between nitric oxide and the cholinergic and sympathetic nervous system in cardiovascular control in humans. Pharmacol Ther. 2005;106:209–20. doi: 10.1016/j.pharmthera.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 44.Kinsey AC, Pomeroy WB, Martin CE. Sexual behavior in the human male. Oxford: Saunders; 1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meuwissen I, Over R. Sexual arousal across phases of the human menstrual cycle. Arch Sex Behav. 1992;21:101–19. doi: 10.1007/BF01542588. [DOI] [PubMed] [Google Scholar]
- 46.Hoon PW, Bruce K, Kinchloe B. Does the menstrual cycle play a role in sexual arousal? Psychophysiology. 1982;19:21–7. doi: 10.1111/j.1469-8986.1982.tb02593.x. [DOI] [PubMed] [Google Scholar]
- 47.Hindmarch I, Kerr JS, Sherwood N. Effects of nicotine gum on psychomotor performance in smokers and non-smokers. Psychopharmacology (Berl) 1990;100:535–41. doi: 10.1007/BF02244008. [DOI] [PubMed] [Google Scholar]
- 48.Hurt RD, Offord KP, Croghan IT, Croghan GA, Gomez-Dahl LC, Wolter TD, Dale LC, Moyer TP. Temporal effects of nicotine nasal spray and gum on nicotine withdrawal symptoms. Psychopharmacology (Berl) 1998;140:98–104. doi: 10.1007/s002130050744. [DOI] [PubMed] [Google Scholar]
- 49.Rigotti NA. Clinical practice. Treatment of tobacco use and dependence. N Engl J Med. 2002;346:506–12. doi: 10.1056/NEJMcp012279. [DOI] [PubMed] [Google Scholar]
- 50.Tutka P, Mosiewicz J, Wielosz M. Pharmacokinetics and metabolism of nicotine. Pharmacol Rep. 2005;57:143–53. [PubMed] [Google Scholar]
- 51.Benowitz NL, Porchet H, Sheiner L, Jacob P. Nicotine absorption and cardiovascular effects with smokeless tobacco use: Comparison with cigarettes and nicotine gum. Clin Pharmacol Ther. 1988;1:23–38. doi: 10.1038/clpt.1988.107. [DOI] [PubMed] [Google Scholar]
- 52.Rellini AH, McCall KM, Randall PK, Meston CM. The relationship between women’s subjective and physiological sexual arousal. Psychophysiology. 2005;42:116–24. doi: 10.1111/j.1469-8986.2005.00259.x. [DOI] [PubMed] [Google Scholar]
- 53.Rosen RC, Brown C, Heiman J, Leiblum S, Meston CM, Shabsigh R, Ferguson D, D’Agostino R. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 54.Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): Cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31:1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 55.Shacham S. A shortened version of the Profile of Mood States. J Pers Assess. 1983;47:305–6. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- 56.Emery CF, Hsiao ET, Hill SM, Frid DJ. Short-term effects of exercise and music on cognitive performance among participants in a cardiac rehabilitation program. Heart Lung. 2003;32:368–73. doi: 10.1016/s0147-9563(03)00120-1. [DOI] [PubMed] [Google Scholar]
- 57.Berger BG, Grove JR, Prapavessis H, Butki BD. Relationship of swimming distance, expectancy, and performance to mood states of competitive athletes. Percept Mot Skills. 1997;84:1199–210. doi: 10.2466/pms.1997.84.3c.1199. [DOI] [PubMed] [Google Scholar]
- 58.Barton DL, Wender DB, Sloan JA, Dalton RJ, Balcueva EP, Atherton PJ, Bernath AM, Jr, DeKrey WL, Larson T, Bearden JD, 3rd, Carpenter PC, Loprinzi CL. Randomized controlled trial to evaluate transdermal testosterone in female cancer survivors with decreased libido; North Central Cancer Treatment Group Protocol N02C3. J Natl Cancer Inst. 2007;99:672–9. doi: 10.1093/jnci/djk149. [DOI] [PubMed] [Google Scholar]
- 59.Galantino ML, Baime M, Maguire M, Szapary PO, Farrar JT. Association of psychological and physiological measures of stress in health-care professionals during an 8-week mindfulness meditation program: Mindfulness in practice. Stress and Health. 2005;21:255–61. [Google Scholar]
- 60.Sintchak G, Geer JH. A vaginal plethysmograph system. Psychophysiology. 1975;12:113–5. doi: 10.1111/j.1469-8986.1975.tb03074.x. [DOI] [PubMed] [Google Scholar]
- 61.Laan E, Everaerd W, Evers A. Assessment of female sexual arousal: Response specificity and construct validity. Psychophysiology. 1995;32:476–85. doi: 10.1111/j.1469-8986.1995.tb02099.x. [DOI] [PubMed] [Google Scholar]
- 62.Blanchard R, Racansky IG, Steiner BW. Phallometric detection of fetishistic arousal in heterosexual male cross–dressers. J Sex Res. 1986;22:452–62. [Google Scholar]
- 63.Harris GT, Rice ME, Quinsey VL, Chaplin TC, Earls C. Maximizing the discriminant validity of phallometric assessment data. Psychological Assessment. 1992;4:502–11. [Google Scholar]
- 64.Chivers ML, Rieger G, Latty E, Bailey JM. A sex difference in the specificity of sexual arousal. Psychol Sci. 2004;15:736–44. doi: 10.1111/j.0956-7976.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- 65.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 66.Grassi G, Seravalle G, Calhoun DA, Bolla GB, Giannattasio C, Marabini M, Del Bo A, Mancia G. Mechanisms responsible for sympathetic activation by cigarette smoking. Circulation. 1994;90:248–53. doi: 10.1161/01.cir.90.1.248. [DOI] [PubMed] [Google Scholar]
- 67.Meston CM, Gorzalka BB. The effects of immediate, delayed, and residual sympathetic activation on sexual arousal in women. Behav Res Ther. 1996;34:143–8. doi: 10.1016/0005-7967(95)00050-x. [DOI] [PubMed] [Google Scholar]
- 68.Meston CM, Gorzalka BB. The effects of sympathetic activation on physiological and subjective sexual arousal in women. Behav Res Ther. 1995;33:651–64. doi: 10.1016/0005-7967(95)00006-j. [DOI] [PubMed] [Google Scholar]
- 69.Meston CM, Heiman JR. Ephedrine-activated physiological sexual arousal in women. Arch Gen Psychiatry. 1998;55:652–6. doi: 10.1001/archpsyc.55.7.652. [DOI] [PubMed] [Google Scholar]
- 70.Londeree BR, Moeschberger ML. Effect of age and other factors on maximal heart rate. Res Q Exerc Sport. 1982;53:297–304. [Google Scholar]
- 71.Fox S, Naughton J, Haskell W. Physical activity and the prevention of coronary heart disease. Ann Clin Res. 1971;3:404–32. [PubMed] [Google Scholar]
- 72.Levin RJ, Wylie K. Vaginal vasomotion—Its appearance, measurement, and usefulness in assessing the mechanisms of vasodilation. J Sex Med. 2007 doi: 10.1111/j.1743-6109.2007.00669.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 73.Heishman SJ, Snyder FR, Henningfield JE. Performance, subjective, and physiological effects of nicotine in non-smokers. Drug Alcohol Depend. 1993;34:11–8. doi: 10.1016/0376-8716(93)90041-n. [DOI] [PubMed] [Google Scholar]
- 74.Grobe JE, Perkins KA, Goettler-Good J, Wilson A. Importance of environmental distractors in the effects of nicotine on short-term memory. Exp Clin Psychopharmacol. 1998;6:209–16. doi: 10.1037//1064-1297.6.2.209. [DOI] [PubMed] [Google Scholar]
- 75.Davis JW, Shelton L, Watanabe IS, Arnold J. Passive smoking affects endothelium and platelets. Arch Int Med. 1989;149:386–9. [PubMed] [Google Scholar]
- 76.Kirsch I. Specifying nonspecifics: Psychological mechanisms of placebo effects. In: Harrington A, editor. The placebo effect: An interdisciplinary exploration. Greenwich, CT: JAI Press; 1997. pp. 159–99. [Google Scholar]
- 77.Benowitz NL, Jacob P. Individual differences in nicotine kinetics and metabolism in humans. In: Repack RS, Change N, Martin BR, editors. Pharmacokinetics, metabolism, and pharmaceutics of drugs of abuse. DHHS Publication Number 97-4141. Washington, DC: US Government Printing Office; 1997. pp. 48–64. [Google Scholar]
- 78.Benowitz NL, Lessove-Schlaggar CN, Swan GE, Jacob P., 3rd Female sex and oral contraceptive use accelerate nicotine metabolism. Clin Pharmacol Ther. 2006;79:480–8. doi: 10.1016/j.clpt.2006.01.008. [DOI] [PubMed] [Google Scholar]