Abstract
Purpose
Interventions targeting multiple risk behaviors are needed for youth living with HIV (YLH). A randomized clinical trial compared Healthy Choices, a 4 session motivational intervention targeting two of three risk behaviors (HIV medication adherence, sexual risk behavior and substance use) to multidisciplinary specialty care alone. This paper presents intermediary outcomes available at 3-month follow-up, variables proposed to be precursors to behavior change (motivation, self-efficacy and depression).
Methods
YLH (N = 186) with at least one of the three problem behaviors were recruited from four sites in the Adolescent Trials Network (ATN) and one non-ATN site and were assessed at baseline and 3 months.
Results
Of the 94 youth randomly assigned to the treatment condition, 84% received at least one session, 67% received at least two sessions, 56% received at least 3 sessions, and 49% completed all four sessions. In intent-to-treat analysis, only depression was significantly improved in the treatment group compared to controls. However, in per-protocol analysis, youth receiving at least two sessions of the intervention also showed significant improvements in motivational readiness to change compared to youth in the control condition.
Conclusion
Results suggest the potential benefits of clinic-based motivational interventions for YLH who access these interventions. Delivering interventions in the community using an outreach model may improve access. Analysis of subsequent time points will determine effects on actual behavior change.
Introduction
Youth living with HIV (YLH) struggle with multiple risk behaviors that have implications for their own health and for that of the public. Studies have reported high rates of sexual risk behaviors1,2 and substance use 1,3, and poor adherence to antiretroviral medication4,5. Moreover, risk behaviors are likely to cluster 6–8 because different risk behaviors may serve the same developmental functions (e.g., striving for autonomy, identifying with peers, attempting to attain adult status) 9. The covariance of risk behaviors suggests the need for interventions targeting multiple risk behaviors to reduce HIV transmission and improve health outcomes in YLH10. However, randomized controlled intervention trials with YLH are rare. Retention of YLH in interventions is a concern as the only multi-site randomized behavioral intervention trial found that 41% were fully retained in an 18 session intervention11.
A briefer intervention may be more easily implemented in clinic settings to serve a broader range of youth and could promote motivation to utilize the array of services offered by clinics that typically serve YLH. As a foundation for the current study, Naar-King and colleagues 12 piloted a briefer intervention, titled Healthy Choices, which focused on boosting motivational readiness for change and building self-efficacy for multiple risk behaviors. To assist with brevity, youth only focused on 2 of the 3 most problematic risk behaviors (sexual risk, substance use, or medication adherence/general health behaviors) based on their baseline assessment. It was a four-session intervention delivered over 10 weeks based on Motivational Interviewing (MI)13 and showed preliminary evidence of reductions in multiple risk behaviors12.
MI is a method of communication designed to increase motivational readiness to change by exploring ambivalence about behavior change, eliciting discrepancies between behaviors and goals, and building self-efficacy. At the foundation of MI are client-centered techniques, such as expressing empathy and positive regard, which are thought to assist in developing rapport and in reducing emotional distress14. These three proposed mechanisms of change (motivational readiness, self-efficacy, and reduced psychological distress) have been found to be associated with actual risk behaviors in YLH1–4, 15. MI is often used as a brief preparatory intervention to increase engagement in more intensive treatments16.
This paper presents the methods of a multi-site study of the Adolescent Trials Network (ATN) testing the Healthy Choices intervention along with outcomes available immediately post-treatment (3-month follow-up). These intermediary outcomes (motivational readiness, self-efficacy, and depression as an indicator of emotional distress) are not only the proposed mediators of behavior change for Healthy Choices as described above, but also studies have suggested that MI interventions often have short-term effects on these variables before actual behavior change is documented17. We hypothesized that youth in the intervention condition would have greater improvements in motivation, self-efficacy, and depression than youth in the control condition immediately post-treatment. Data analysis procedures were included to address issues related to flexibly targeting multiple risk behaviors in an intervention study.
Methods
YLH were recruited from four ATN sites located in Fort Lauderdale, Philadelphia, Baltimore, and Los Angeles, and one non-ATN site in Detroit. Inclusion criteria included HIV-positive status, ages 16 to 24, and ability to complete questionnaires in English. Inclusion criteria included having a problem in at least one of three HIV risk behaviors (substance use, sexual risk, medication non-adherence). YLH were screened for problem level substance use behavior with the CRAFFT (Car, Relax, Alone, Forget, Friends, and Trouble)16, a 6-item adolescent screener. In the original CRAFFT, two or more yes responses indicated problem level substance use. To ensure that substance problems were current, 3 items were changed from “ever used” to used in the last 3 months: used substances to relax, used substances by yourself, and forgetting while using. A single item determined current sexual risk behavior where YLH endorsed the presence or absence of an unprotected intercourse act in the previous three months. A single item determined screening for a medication adherence problem where YLH endorsed whether or not they were less than 90% adherent in the last month. If they were prescribed medications but had refused them, this was considered less than 90% adherent. Because the intervention focused on multiple risk behaviors, youth had to have at least engaged in a second behavior so that a second behavior could be discussed in the intervention, even if the focus was on maintenance or preventing escalation to a problem level. Exclusion criteria were having a history of any psychiatric thought disorder that might lead to an inability to complete questionnaires (e.g., schizophrenia, schizoaffective disorder), being currently involved in behavioral research targeting adherence, sexual risk, or substance use, and being currently involved in a formal substance abuse treatment program.
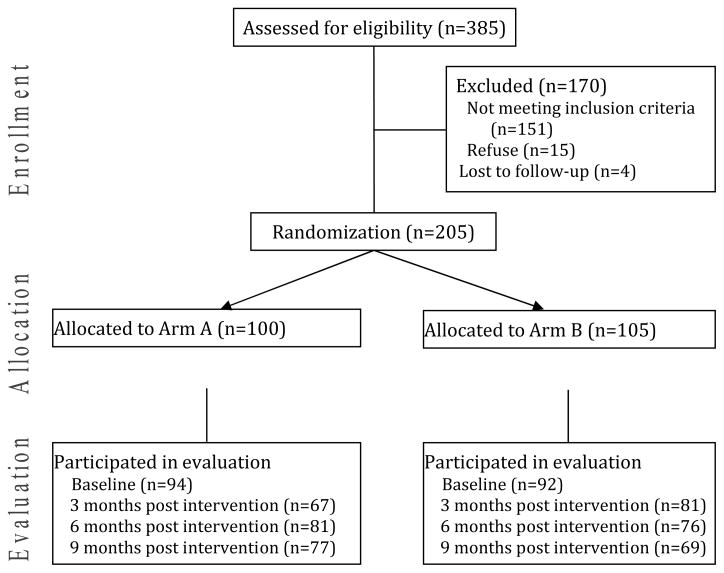
Figure 1 describes recruitment and retention. Of the 205 enrolled, 19 did not complete baseline data collections and could not be analyzed for a final sample size of 186. Because of the brevity of the intervention and the comprehensive support services available in the clinic setting, YLH were randomized to the intervention plus HIV specialty care (N = 94) or HIV specialty care alone (N = 92).
Figure 1.
Consolidated Standards of Reporting Trial Diagram of the Health Choice Intervention Trial: Arm A = Healthy Choices plus specialty care, Arm B = Special care alone.
Procedures
The protocol was approved by each site’s Institutional Review Board and a certificate of confidentiality was obtained from the National Institutes of Health. Upon determination of eligibility, written informed consent was obtained, and a waiver of parental consent was permitted for youth under age 18. Participants were then randomized so that intervention sessions could be scheduled immediately after the baseline assessment to promote intervention retention. Randomization was carried out using a permuted block design with randomly determined block sizes of 4 and 6. Randomization was stratified by site and targeted problem behavior. An automated clinical trial management tool, based on telephone interactive voice response (IVR) technology, was used to randomize subjects to treatment arm. This tool allows users to send and receive randomization information from any telephone.
Following the screener, youth completed the baseline assessment within 30 days. All measures were collected using computer assisted personal interviewing (CAPI) where the researcher conducts a face-to-face interview but enters responses directly into the computer. Participants received $30 compensation for the baseline visit, and $35 for the 3-month follow-up visit. Transportation, snacks and childcare were available. All assessments and intervention sessions occurred at the clinic sites. Retention strategies included reminder calls and collaboration with clinic staff and outreach staff to contact hard-to-reach youth. Preliminary outcomes at 3 months are presented, while data analyses for subsequent follow-ups are underway.
Multidisciplinary HIV specialty care
All sites provided HIV primary care with an adolescent medicine specialist and provided the following onsite services: adherence, mental health, and risk reduction counseling, case management, HIV support groups, home visits, peer advocacy and outreach, and transportation. At baseline, YLH reported mean utilization of 9.8 support services over the previous 3 months with no differences between those assigned to treatment and those assigned to control (p = .58).
Healthy Choices
The four sixty-minute sessions have been previously described 11,18 and were adapted from Motivational Enhancement Therapy (MET)19. Youth could work on two of three possible problem behaviors based on their entry screening: substance use, sexual risk, or medication adherence. If they had problems in all three behaviors (N = 18 of 186), a random selection of two of the three behaviors determined the intervention targets. If the participant had only one problem level behavior, the second targeted behavior would be the one that the subject had engaged in. If in addition to one problem behavior, there were two behaviors that were engaged in but not at a problem level, then one of the two was chosen as the second possible target for the intervention using a random selection process (includes 28 participants). Although control condition participants did not receive the intervention, a similar process served to identify the two risk behaviors that would be examined for changes over time in assessing the potential efficacy of the intervention.
Therapists were doctoral students in psychology or trained mental health clinicians. Therapists participated in a 2-day MI training by members of the Motivational Interviewing Network of Trainers. Therapists received weekly phone supervision and case feedback from one of the supervising trainers. Therapists submitted videotaped recordings of each therapy session to the research team both for supervisor review and for coding with the Motivational Interviewing Treatment Integrity codes (MITI 2.0)20. The MITI produces specific feedback to the supervisor and therapist on use of MI techniques. A twenty minute portion of each tape was selected at random and coded by a member of the MITI coding team, a group of seven trained raters whose reliability was assessed using the Intra-Class Correlation (ICC) statistic. To ensure reliability, each rater coded the same 20 minute portion of a taped therapy session. The ICC for this coded segment was shown to be highly reliable, with a Cronbach’s alpha = .967; ICC average measures = .97 α <.01. Average MITI global therapist ratings were above the “Beginner Competency” level20.
Measures
All measures for the present analysis asked about the youth’s status the day of the assessment (baseline and 3-month follow-up), with the exception of the Brief Symptom Inventory, which asks about the previous week. Thus, these intermediary outcomes did not overlap with the intervention period (10 weeks). Rollnick’s Readiness Ruler 21 was administered with two items for each of the three behaviors: avoiding alcohol use and avoiding illicit drug use, condom use for intercourse and disclosure to sexual partners, taking HIV medications as prescribed and attending HIV primary care appointments. Youth marked their readiness for these behaviors on a 10 point scale from 1 (not ready) to 10 (completely ready). These measures have been found to be correlated with actual condom use 2, substance use 3, and medication adherence 15 suggesting validity. For self-efficacy, YLH completed the Temptation scales, which have shown good reliability and validity in adults with HIV 22, 23. Each item described a situation, and youth rated how tempted they would be to use drugs, have unprotected sex or miss medications in that situation, from 1 (not at all tempted) to 5 (extremely tempted). Forty items addressed substance use (20 items for alcohol use and 20 items for illicit drug use), 18 items addressed condom use, and 14 items addressed taking medications. Additional items rated on a 5-point scale asked about general confidence to avoid risk (6 items per behavior); however, the increased missing data for the sexual risk items on this scale precluded inclusion in the analysis. The self-efficacy items did not include missing appointments or disclosing to sexual partners due to concerns about instrument burden. Cronbach’s alpha was .95 for the substance use temptation scale, .94 for the medication adherence temptation scale, and .94 for the condom use items. The temptation items were reverse scored so that higher scores indicated greater self-efficacy ranging from 1 to 5 for each behavior. The depression scale of the Brief Symptom Inventory measured symptom patterns of depression. The BSI has shown evidence of reliability and validity in many studies of medical, psychiatric, and non-patient populations 24, as well as in YLH 2,3. The BSI yields t-scores where scores greater than 65 indicate clinical distress.
Data Analytic Plan
The hypothesis that the intervention group would have improved motivation, self-efficacy and depression, relative to the control group, was first tested with an intent-to-treat (ITT) approach. Missing data were replaced with the mean of that measure for each group. Repeated measures analysis of variance was used to test for group (treatment vs. standard care) by time (baseline vs. 3-month follow-up) effects. In addition to ITT, per protocol analysis is recommended to completely present the profile of results and understand differential outcomes for high risk populations who have been retained in interventions25. Thus, following the ITT analysis, a per protocol analysis (on-treatment analysis) utilized the same repeated measures analysis of variance but excluding youth (N=31) in the intervention condition who did not complete at least two intervention sessions (one per behavior) 11, 26, 27.
In order to analyze outcomes specifically related to intervention targets, making sure to include all participants to increase power, measures were combined based on the relevant two behaviors consistent with the work of leaders in the field of multiple risk behaviors28. The behavior-specific outcome measures (i.e., motivational readiness and self-efficacy) included those items targeted by the intervention. Thus, for example, for participants whose target behaviors were adherence and substance use, the motivational readiness variable included four items, two addressing medication adherence and two targeting substance use. Total scores for motivational readiness ranged from 4 to 40, and total scores for self-efficacy ranged from 2 to 10. Effect sizes using Cohen’s d 29 are also reported, with the mean difference in change scores divided by the pooled standard deviation across the pre-test and post-test means for each group (4 measures)30.
Results
Of the 186 participants, 122 (65.6%) had reached a problem level for substance use, 82 (44.1%) for HIV medication adherence, and 100 (53.8%) for sexual risk. Of the 186 participants, 86 (46.2%) had one of these problem behaviors, 82 (44.1%) had two problem behaviors, and 18 (9.7%) had all three problem behaviors. Table 1 shows baseline characteristics, with more males in the control condition at baseline (not controlled for in randomization). Retention at 3-month follow-up was 80.6% (73.4% of treatment group and 88.0% of controls). Participants retained at 3 months did not differ significantly from those who were not in any demographic variable or baseline risk behavior. There were no significant differences at baseline between the intervention and control groups in the three outcomes: motivational readiness, self-efficacy, or depression. Of the 94 youth randomly assigned to the treatment condition, 83.9% received at least one session, 66.9% received at least two sessions, 56.3% received at least 3 sessions, and 48.9% completed all four sessions. There were no differences between those completing the minimum dose of two sessions and those who did not in demographics, presence of a particular problem behavior or number of problem behaviors, or for the current outcomes of motivational readiness, self-efficacy and depression. There were also no differences between those completing the maximum dose of four sessions and those completing fewer sessions in any of these variables.
Table 1.
Sample Characteristics
| Item | Total | Intervention | Control | Comparison X2 or t-test (p) |
|---|---|---|---|---|
| Mean age (SD) | 20.5 (2.3) | 20.5 (2.4) | 20.5 (2.3) | 0.06 (.95) |
| Race/ethnicity | ||||
| AA/Black (%) | 155 (83.3) | 80 (85.1) | 75 (81.5) | 0.43(.51) |
| Others (%) | 31(16.7) | 14 (14.9) | 17 (18.5) | |
| Biological sex | ||||
| Male (%) | 98 (52.7) | 42 (44.7) | 56 (60.9) | 4.89 (0.03)* |
| Sexual orientation | ||||
| Straight/hetero (%) | 103 (56.6) | 56 (61.5) | 47 (51.6) | 1.81 (.18) |
| Perinatally Infected (%) | 14 (15.9) | 17 (18.4) | .43 (.32) |
Note: p<.05
Means and standard deviations of the summary motivational readiness and self-efficacy measures and BSI depression for the intervention and control groups at baseline and 3-month follow-up are shown in Table 2. Results of intent-to-treat analysis suggest a significant effect for depression (F (1, 184) = 4.56, p = .03) with an effect size of .3. There was not a significant effect for motivational readiness (F (1, 184) = 1.75, p = .19), though there was a small effect size of .2. The effect on self-efficacy was also not significant (F (1, 184) = 1.14, p = .29) with an effect size of .01. Per protocol analysis compared those who received at least 2 sessions of the intervention (N = 63) with those in the control condition (N = 92). There were still significant improvements in depression in the group who received treatment compared to the control group (F (1, 153) = 4.60, p = .03) with an effect size of .3. YLH who received the intervention also improved motivational readiness compared to controls (F (1, 153) = 5.82, p =.02) with an effect size of .4. The effect on self-efficacy was borderline significant (F (1,153) = 3.54, p = .06), and the effect size was .2.
Table 2.
Descriptive statistics for treatment and control groups at baseline and 3-month follow-up
| Baseline | 3-months | Baseline | 3-months | |||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| INTENT TO TREAT | Treatment N=94 | Control N=92 | ||||||
| BSI – Depression* | 55.57 | 11.81 | 51.51 | 10.43 | 55.85 | 13.22 | 55.28 | 12.50 |
| Motivational Readiness | 31.38 | 8.24 | 32.81 | 6.20 | 30.27 | 7.65 | 30.20 | 7.80 |
| Self-efficacy | 7.96 | 1.32 | 8.48 | 1.21 | 7.42 | 1.59 | 7.81 | 1.40 |
| PER PROTOCOL | Treatment N=63 | Control N=92 | ||||||
| BSI – Depression* | 55.21 | 11.77 | 50.72 | 11.52 | 55.85 | 13.22 | 55.28 | 12.50 |
| Motivational Readiness* | 30.51 | 7.50 | 33.45 | 5.54 | 30.27 | 7.65 | 30.20 | 7.80 |
| Self-efficacy | 8.02 | 1.30 | 8.66 | 1.18 | 7.52 | 1.59 | 7.81 | 1.40 |
Significant group × time intervention effect (p < .05)
Discussion
Rates of the multiple risk behaviors in this sample indicate a strong need for treatment intervention in this population. This multi-site study tested the effect of a clinic-based brief intervention targeting multiple risk behaviors simultaneously in high-risk youth living with HIV. YLH received the intervention in the real-world setting of adolescent medicine clinics instead of a research venue. Results suggest that a brief MI intervention improved depression and also improved motivation for changing risk behaviors for those who attended at least two MI sessions. This is the first study of a brief intervention to test these important precursors to behavior change in YLH. The intervention effect was strongest for depression, as it was significant both in intent-to-treat and per protocol analysis. It is possible that the new therapists in the study were able to master the client-centered components of MI to effect change in emotional distress, but that greater shifts in motivation required more therapist skill in the goal-directed components of MI. Alternatively, the measurement of motivation may have been weaker than the standardized measure of depression. The motivational readiness measure included only single items for each behavior with relatively high scores at baseline (7.5 out of 10). Furthermore, multiple behaviors were summed into a single score so that larger changes in motivation for one behavior could be masked by lack of change in another behavior.
Self-efficacy, as defined by belief in the ability to avoid risky behaviors in the face of temptation, approached significance for those who received the intervention. It is possible that while MI supports self-efficacy through affirmation of client strengths, confidence to avoid risk in very specific tempting situations may require a more intensive skills-building intervention.
Two-thirds of the sample assigned to the treatment condition received at least two intervention sessions. These youth could not be distinguished from the remaining high-risk youth on any of the baseline variables measured. Increasing access by offering the intervention in the home or community and by including an outreach component may improve intervention retention, as has been suggested in one study of youth perinatally infected with HIV 32. Certainly, an outreach approach has been recommended to engage high-risk youth in HIV counseling and testing 33 and HIV primary care 34. Rotheram-Borus indicated that their intervention was offered at community agencies but could also be offered in the home or a location convenient for the youth11. However, the authors do not report specific outreach strategies or the percentage of youth receiving intervention outside of study sites. Incorporating outreach strategies within behavior change interventions could not only increase access by providing services in flexible locations, but also by including case finding approaches such as those utilized by health departments for the delivery of HIV test results and partner notification. Further studies of factors influencing appointment attendance (e.g., motivation and self-efficacy for attending treatment sessions) may elucidate strategies to improve intervention retention.
A limitation of the study is the lack of an attention control. However, standard care in these clinics included significant support services with an average of over 9 visits over 3 months, more than twice what was offered in Healthy Choices. YLH in the intervention condition appeared to be less likely to complete the 3 month follow-up. Yet there were no significant differences in baseline characteristics between youth retained and those not retained, suggesting that this attrition did not likely bias the results. Further analysis of subsequent time points will determine if differential attrition dissipates over the course of the study. Additional limitations of this study include the recruitment of youth in clinic settings only and the reliance on self-report measures with limited evidence of reliability and validity in YLH. Also, we randomly selected two of three target behaviors when all three problem behaviors were present. In an MI approach, the participant would choose which two behaviors to target, and this may improve intervention outcomes.
Results suggest the utility of brief MI delivered in adolescent medicine clinics to improve depression and motivational readiness among youth who access the intervention. Brief MI interventions may be helpful to boost motivation to engage in services offered by multidisciplinary adolescent clinics serving YLH. Interventions that utilize MI as a precursor to more intensive interventions such as cognitive-behavioral treatment 24–25 are worth further exploration in YLH.
Acknowledgments
This work was supported by The Adolescent Trials Network for HIV/AIDS Interventions (ATN) [U01-HD040533 from the National Institutes of Health through the National Institute of Child Health and Human Development (B. Kapogiannis, S. Lee)], with supplemental funding from the National Institutes on Drug Abuse (N. Borek) and Mental Health (P. Brouwers, S. Allison). The study was scientifically reviewed by the ATN’s Behavioral Leadership Group. Network, scientific and logistical support was provided by the ATN Coordinating Center (C Wilson, C. Partlow) at The University of Alabama at Birmingham Network operations and data management support was provided by the ATN Data and Operations Center at Westat, Inc. (J. Korelitz, J. Davidson, B. Harris). We acknowledge the contribution of the investigators and staff at the following ATN 004 sites that participated in this study: Children’s Diagnostic and Treatment Center (Ana Puga, MD, Esmine Leonard, BSN, Zulma Eysallenne, RN); Childrens Hospital of Los Angeles (Marvin Belzer, MD, Cathy Salata, RN, Diane Tucker, RN, MSN); University of Maryland (Ligia Peralta, MD, Leonel Flores, Esther Collinetti, BA); University of Pennsylvania and the Children’s Hospital of Philadelphia (Bret Rudy, MD, Mary Tanney, MPH, MSN, CPNP, Adrienne DiBenedetto, BSN); University of Southern California (Andrea Kovacs, M.D.,), and Wayne State University Horizons Project (K. Wright, D.O., P. Lam, M.A., V. Conners, B.A.). We sincerely thank the youth who participated in this project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sylvie Naar-King, Wayne State University Jeffrey
Jeffrey T. Parsons, Hunter College and the Graduate Center of the City University of New York
Debra Murphy, University of California – Los Angeles
Karen Kolmodin, Wayne State University
D. Robert Harris, Westat, ATN 004 Protocol Team, Adolescent Trials Network for HIV/AIDS Interventions
References
- 1.Murphy DA, Durako SJ, Moscicki AB, et al. No Change in health risk behaviors over time among HIV infected adolescents in care: role of psychological distress. J Adolesc Health. 2001;29(3 Suppl):57–63. doi: 10.1016/s1054-139x(01)00287-7. [DOI] [PubMed] [Google Scholar]
- 2.Naar-King S, Wright K, Parsons JT, Frey M, Templin T, Ondersma S. Transtheoretical model and condom use in HIV-positive youths. Health Psychol. 2006b;25(5):648–652. doi: 10.1037/0278-6133.25.5.648. [DOI] [PubMed] [Google Scholar]
- 3.Naar-King S, Wright K, Parsons JT, Frey M, Templin T, Ondersma S. Transtheoretical model and substance use in HIV-positive youth. AIDS Care. 2006c;18(7):839–845. doi: 10.1080/09540120500467075. [DOI] [PubMed] [Google Scholar]
- 4.Hosek SG, Harper GW, Domanico R. Predictors of medication adherence among HIV-infected youth. Psychol Health Med. 2005;10(2):166–179. doi: 10.1080/1354350042000326584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy DA, Wilson CM, Durako SJ, Muenz LR, Belzer M, Network HAR. Antiretroviral medication adherence among REACH HIV-infected adolescent cohort in the USA. AIDS Care. 2001;13:27–40. doi: 10.1080/09540120020018161. [DOI] [PubMed] [Google Scholar]
- 6.Dryfoos JG. Preventing high-risk behavior. Am J Public Health. 1991;81(2):157–158. doi: 10.2105/ajph.81.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jessor R, Bos JVD, Vanderryn J, Costa FM, Turbin MS. Protective factors in adolescent probelm behavior: Moderator effects and developmental change. Dev Psychol. 1995;31(6):923–933. [Google Scholar]
- 8.Park MP, Mulye TP, Adams S, Brindis C, Irwin C. The health status of young adults in the United States. J Adolesc Health. 2006;39:305–317. doi: 10.1016/j.jadohealth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 9.Jessor R. Risk behavior in adolescence: A psychosocial framework for understanding and action. Dev Rev. 1992;12(4):374–390. doi: 10.1016/1054-139x(91)90007-k. [DOI] [PubMed] [Google Scholar]
- 10.Wu Y, Burns JJ, Stanton BF, Li X, Harris CV, Galbraith J, Lang W. Influence of prior sexual risk experience on response to intervention targeting multiple risk behaviors among adolescents. J Adolesc Health. 2005;36:56–63. doi: 10.1016/j.jadohealth.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 11.Rotheram-Borus MJ, Lee M, Lin YY, Lester P. Six-year intervention outcomes for adolescent children of parents with the human immunodeficiency virus. Arch Pediatr Adolesc Med. 2004;158:742–748. doi: 10.1001/archpedi.158.8.742. [DOI] [PubMed] [Google Scholar]
- 12.Naar-King S, Wright K, Parsons J, et al. Healthy Choices: Motivational enhancement therapy for health risk behaviors in HIV+ Youth. AIDS Educ Prev. 2006a;18(1):1–11. doi: 10.1521/aeap.2006.18.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Miller WR, Rollnick S. The atmosphere of change. In: Miller WR, Rollnick S, editors. Motivational interviewing: Preparing people to change addictive behavior. New York, NY: The Guilford Press; 2002. [Google Scholar]
- 14.Rogers C. The necessary and sufficient conditions of therapeutic personality change. Journal Consult Clin Psychol. 1957;21(2):95–103. doi: 10.1037/h0045357. [DOI] [PubMed] [Google Scholar]
- 15.Kolmodin K, Naar-King S, Murphy D, Parson J, Harper G. Predictors of Medication Adherence in High Risk Youth Living with HIV. J Pediatr Psychol. Under Review. [Google Scholar]
- 16.Hettema J, Steele J, Miller WR. Motivational Interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 17.Knight JR, Shrier LA, Bravender TD, Farrell M, Vander J, Shaffer HJ. A new brief screen for adolescent substance aduse. Arch Pediatr Adolesc Med. 1999;153:591–596. doi: 10.1001/archpedi.153.6.591. [DOI] [PubMed] [Google Scholar]
- 18.Naar-King S, Lam P, Wang B, Wright K, Parsons JT, Frey MA. Brief report: maintenance of effects of motivational enhancement therapy to improve risk behaviors and HIV-related Health in a randomized controlled trial of youth living with HIV. J Pediatr Psychol. 2008;33(4):441–445. doi: 10.1093/jpepsy/jsm087. [DOI] [PubMed] [Google Scholar]
- 19.Miller W, Zweben A, DiClemente C, Rychtarik R. Motivational enhancement therapy manual. Rockville MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- 20.Moyers TB, Martin T, Manuel JK, Miller WR. The motivational interviewing treatment integrity (MITI) code: version 2.0. 2004:1–19. [Google Scholar]
- 21.Stott NCH, Rollnick S, Pill RM. Innovation in clinical method: Diabetes care and negotiating skills. Fam Pract. 1995;12:413–418. doi: 10.1093/fampra/12.4.413. [DOI] [PubMed] [Google Scholar]
- 22.Parsons JT, Halkitis PN, Wolitski RJ, Gomez CA. The seropositive urban men’s study (SUMS) team. Correlates of sexual risk behaviors among HIV-positive men who have sex with men. AIDS Educ Prev. 2003;15:383–400. doi: 10.1521/aeap.15.6.383.24043. [DOI] [PubMed] [Google Scholar]
- 23.Parsons JT, Rosof E, Punzalan JC, Dimaria L. Intergration of motivational interviewing and cognitive behavioral therapy to improve HIV medication adherence and reduce substance use among HIV-positive men and women: results of a pilot project. Aids Patient Care STDS. 2005;19:31–39. doi: 10.1089/apc.2005.19.31. [DOI] [PubMed] [Google Scholar]
- 24.Derogatis L, Spencer P. Brief Symptom Inventory: Administration, Scoring, and Procedures Manual-I. Baltimore: Clinical Psychometric Research INC; 1982. [Google Scholar]
- 25.Amico KR, Harman JJ, O’Grady MA. Attrition and related trends in scientific rigor: A score card for ART adherence intervention research and recommendations for future directions. Curr HIV/AIDS Rep. 2008;5:172–185. doi: 10.1007/s11904-008-0026-0. [DOI] [PubMed] [Google Scholar]
- 26.Dennis M, Godley SH, Diamond G, et al. The cannibis youth treatment (CYT) study: Main findings from two randomized trials. J Subst Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 27.Parsons JT, Golub SA, Rosof E, Holder C. Motivational interviewing and cognitive- behavioral intervention to improve HIV medication adherence among hazardous drinkers: A randomized controlled trial. J Acqui Immune Defic Syndr. 2007;46(4):443–450. doi: 10.1097/qai.0b013e318158a461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jessor R, Turbin MS, Costa FM. Risk and protection in successful outcomes among disadvantage adolescents. Appl Dev Sci. 1998;2(4):194–208. [Google Scholar]
- 29.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 30.Olejnik S, Algina J. Measures of effect size for comparitive studies: applications, interpretations, and limitations. Contemp Educ Psychol. 2000;25(3):241–286. doi: 10.1006/ceps.2000.1040. [DOI] [PubMed] [Google Scholar]
- 31.Ashman JJ, Conviser R, Pounds MB. Association between HIV- positive individuals’ receipt of ancillary services and medical care receipt and retention. AIDS Care. 2002;14:S109–118. doi: 10.1080/09540120220149993a. [DOI] [PubMed] [Google Scholar]
- 32.Ellis DA, Naar-King S, Cunningham PB, Secord E. Use of multisystemic therapy to improve antiretroviral adherence and health outcomes in HIV-infected pediatric patients: Evaluation of a pilot program. AIDS Patient Care STDS. 2006 Feb;20(2):112–121. doi: 10.1089/apc.2006.20.112. [DOI] [PubMed] [Google Scholar]
- 33.Johnson RL, Stanford PD, Douglas W, Botwinick G, Marino E. High risk sexual behaviors among adolescents engaged through a street-based peer outreach program ( the adolescent HIV project) J Natl Med Assoc. 2001;93:170–177. [PMC free article] [PubMed] [Google Scholar]
- 34.Schneir A, Kipke MD, Melchior LA, Huba GJ. A model of integrated care for HIV-positive and very high-risk youth. J Adolesc Health. 1998;23S:59–70. doi: 10.1016/s1054-139x(98)00054-8. [DOI] [PubMed] [Google Scholar]