Abstract
Please cite this paper as: Beaudoin et al. (2010) Serologic survey of swine workers for exposure to H2N3 swine influenza A. Influenza and Other Respiratory Viruses 4(3), 163–170.
Background Of the 16 influenza A hemagglutinin (H) subtypes, only H1, H2 and H3 viruses have been shown to cause sustained human infection. Whereas H1 and H3 viruses currently circulate seasonally in humans, H2 viruses have not been identified in humans since 1968. In 2006, an H2N3 influenza virus was isolated from ill swine in the United States.
Objective To assess the potential for zoonotic influenza transmission, the current study looked for serologic evidence of H2 influenza infection among workers at two swine facilities, some exposed and some unexposed to H2N3‐positive pigs.
Methods The sera were assessed for antibodies to swine H2 influenza and currently circulating seasonal human influenza A subtypes H1N1 and H3N2. Workers were interviewed to obtain details such as age, influenza vaccination history, experiences of influenza‐like‐illness, and use of personal protective equipment and hygiene when working with pigs. Exposure and risk factors for positive antibody titers were compared for exposed and unexposed individuals as well as for H2 antibody‐positive and H2 antibody‐negative individuals.
Results Blood was taken from 27 swine workers, of whom four had positive H2 antibody titers (≥1:40). Three of the positive employees were born before 1968 and one had an unknown birth date. Only one of these workers had been exposed to H2N3‐positive pigs, and he was born in 1949.
Conclusions These data do not support the hypothesis that swine workers were infected with the emergent swine H2N3 influenza A virus.
Keywords: Influenza, occupational exposure, seroepidemiologic studies, swine influenza, zoonoses
Background
As it had been several decades since the last major influenza pandemic, many influenza experts believed another such event was imminent. The world has been on high alert since the 1997 emergence of highly pathogenic avian influenza H5N1 in Asia. This heightened awareness has resulted in enhanced influenza surveillance, and in the spring of 2009, the first cases of a novel influenza virus were identified in Southern California. 1 The Centers for Disease Control and Prevention (CDC) identified the virus as an influenza A H1N1 virus of swine influenza virus lineage (A/California/2009/H1N1). On June 11, 2009, influenza experts were proven correct when the World Health Organization declared the presence of an H1N1 influenza pandemic.
Since the influenza pandemic of 1918–1919 (Spanish influenza), there have been reports of influenza viruses common to both pigs and people circulating simultaneously and causing disease in both animal and human populations. 2 In the 91 years that have passed since the 1918 pandemic, type A influenza virus infections have become endemic in swine and are a cause of significant respiratory morbidity. During that same period, there have now been three influenza pandemics in humans and continuous circulation of seasonal influenza viruses of H1 and H3 subtypes across the globe.
Although seasonal influenza viruses are very common infections in humans, there are also cases of animal influenza viruses infecting humans every year. According to the CDC, there were 12 reported human cases of swine influenza in the United States between December 2005 and February 2009. 3 One review of human cases of swine influenza described a total of 50 reported cases in the literature from 1958 to 2005, drawing the conclusion that there are no clinical features that distinguish human infection with swine influenza from infection with seasonal human influenza. 4 In addition, several studies have shown that swine workers are at increased risk of infection with swine influenza. 5 , 6 , 7
There are 16 influenza A hemagglutinin (H) subtypes, of which H1, H2 and H3 have been frequent causes of infection among humans. Whereas H1 and H3 are currently circulating seasonally, H2 viruses have not been identified in humans since 1968 and have only been circulating in wild bird populations. 8 , 9 , 10 , 11 In 2006, an H2N3 virus was isolated from ill pigs at a commercial swine nursery in the United States. 12 The virus was found to belong to the American avian influenza lineage and shared only 84·5% similarity with the H2N2 viruses of the 1957 influenza pandemic. The virus was shown through laboratory analysis to have undergone adaptation to mammalian hosts. This finding initiated interest into the zoonotic potential of this virus, as the majority of persons in the United States (individuals born after 1968) would have no pre‐existing antibodies to H2 influenza, and transmission of this virus to humans could result in sustained spread and potential human illness. The objective of the current study was to assess the potential for transmission of the H2N3 virus from pigs to humans, by evaluating demographic and behavioral information as well as conducting serology for evidence of exposure to H2 influenza.
Methods
Study population
In early 2008, 27 participants were recruited from two large swine farms in the United States – Farm 1 and Farm 2. Field veterinarians had routinely submitted samples from each farm to the University of Minnesota Veterinary Diagnostic Laboratory, and thus the swine influenza histories were known for the preceding 6 years. There had been no evidence of H2 swine influenza in Farm 1 prior to September 2006. Sixteen of the participants were recruited from Farm 1, where H2N3 swine influenza A virus was isolated from pigs. Farm 2, and its eleven participants, had no known exposure to pigs with H2 influenza, and H2 influenza A virus had not been isolated from pigs at that farm. Farm 1 was visited in February, and Farm 2 was visited in May of 2008. Both farms were large, multi‐site commercial swine facilities with similar biosecurity protocols. The study was conducted after institutional review board approval (University of Minnesota Institutional review board reviews 0701M01041 and 0706M10503) and signed informed consent of each participant.
Workers were asked a set of questions to obtain details such as age, influenza vaccination history, experiences of influenza‐like illness and use of hygiene practices and personal protective equipment (PPE) when working with pigs (Figure 1). To determine exposure status, workers on Farm 1 were asked if they were employed by the farm between August and December 2006, a time‐span which includes the period during which H2‐positive pigs were present. Serum samples were obtained for antibody evaluation by hemagglutination inhibition and microneutralization serology assays.
Figure 1.
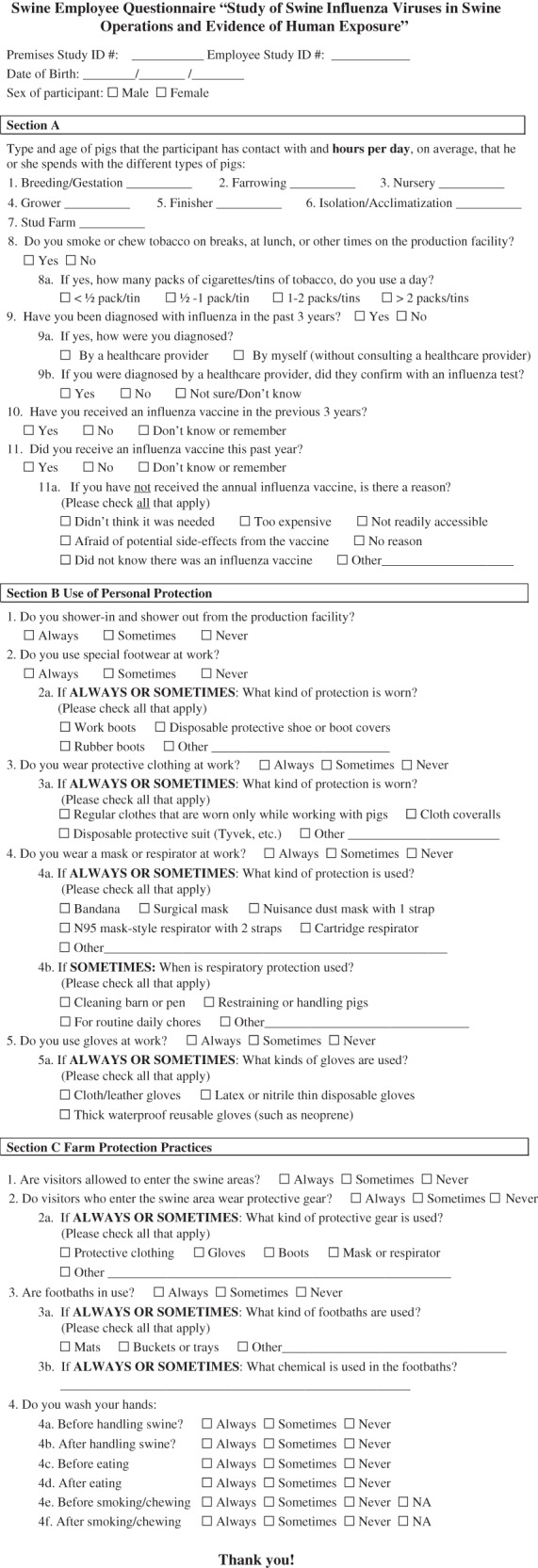
Swine worker questionnaire.
Laboratory procedures
Serum samples were tested using a hemagglutination inhibition (HI) assay and a microneutralization (MNT) assay against H2N3 influenza A/Sw/MO/4296424/2006 (H2), the virus identified in September 2006 on Farm 1. The sera were also assessed by HI for antibodies to two recently circulating human influenza A subtypes: H1N1 Influenza A/New Caledonia/20/99 (H1) and H3N2 influenza A/Panama/2007/99 (H3). Eight control sera, from persons without pig exposure and born after 1968, were also analyzed for antibodies to the H2, H1 and H3 subtypes.
Hemagglutination inhibition
The CDC’s HI serologic protocol was used for analysis of the serum. This protocol is described in detail elsewhere. 6 , 7 The viruses used in the H1 and H3 human influenza HI assays were propagated in embryonated chicken eggs. The virus used in the H2 swine influenza HI assay was grown in MDCK cells, and, as there was sufficient virus obtained from this method, egg culture was not utilized. Hemagglutination inhibition titers were reported as the reciprocal of the highest dilution of serum that inhibited virus‐induced hemagglutination of 0·50% turkey (swine H2 assays) or 0·65% guinea pig (human H1 and H3 assays) erythrocyte solution. To assess the protocol for cross‐reactivity, control samples provided by the CDC were run in addition to study samples. The control sera included H1 antiserum A/New Caledonia/20/99 and H3 antiserum A/Panama/2007/99, as well as influenza B antisera and negative control antisera.
Microneutralization
The microneutralization protocol was modified from a previously described procedure. 13 Following heat inactivation for 30 minutes at 56°C, the serum samples underwent twofold serial dilutions in a 50 μl volume of Dulbecco’s modified Eagle’s medium containing 1% bovine serum albumin and antibiotics (V diluent) in immunoassay plates. The sera were then mixed with an equal volume of V diluent containing influenza virus at 100 TCID50 per 50 μl. Four control wells of virus plus V diluent (VC) or V diluent alone (CC) were included on each plate. After incubation for 2 hours at 37°C in a 5% CO2 humidified atmosphere, 100 μl of MDCK cells at 2 × 105/ml was added to each well. The plates were again incubated for 24 hours at 37°C and 5% CO2. The monolayers were washed with phosphate‐buffered saline (PBS) and fixed in cold 80% acetone for 10 minutes. Indirect ELISA, with a mouse monoclonal antibody to the influenza A nucleoprotein (Millipore, Billerica, MA, USA), and polyclonal goat‐anti‐mouse IgG – horseradish peroxidase conjugate was used to detect the presence of influenza adsorbed to the MDCK monolayer.
At room temperature, the fixed plates were washed three times with PBS containing 0·05% Tween 20 (wash buffer). The anti‐NP antibody, diluted 1/4000 in PBS containing 5% evaporated nonfat milk, was added to each well. After incubation at room temperature for one hour, plates were washed eight times in wash buffer, and 100 μl of horseradish peroxidase‐labeled goat anti‐mouse immunoglobulin G (Kirkegaard & Perry, Gaithersburg, MD, USA) diluted 1/2000 in PBS containing 5% evaporated nonfat milk was added to each well. The plates were incubated for one hour at room temperature and then washed eight times with wash buffer. One hundred microliters of 3,3′,5,5′‐tetramethylbenzidine two‐component microwell peroxidase substrate kit (Kirkegaard & Perry) were added to each well, and the plates were incubated at room temperature for 10 minutes. The reaction was stopped with an equal volume of 1 N sulfuric acid. The absorbance was measured at 490 nm (A 490) with a Versa Max microplate plate reader (Molecular Devices, Sunnyvale, CA, USA) and analyzed with SoftMax Pro 4.7.1 software (Molecular Devices, Sunnyvale, CA, USA). The average A 490 was determined for quadruplicate wells of virus‐infected (VC) and ‐uninfected (CC) control wells, and a neutralizing endpoint was determined by using a 50% specific signal calculation. The endpoint titer was expressed as the reciprocal of the highest dilution of serum with A 490 value less than X, where X = [(average A 490 of VC wells) − (average A 490 of CC wells)]/2 + (average A 490 of CC wells).
Statistical analysis
Using the software SPSS Statistics version 17.0 (SPSS Inc., Chicago, IL, USA), we evaluated a number of demographic parameters and risk factors for association with positive H2 antibody titers. Risk factors included smoking status, self‐reported influenza‐like‐illness over the past 3 years, vaccination against seasonal influenza, use of PPE and hand washing practices. These factors were compared among exposed and unexposed workers as well as among H2‐positive and H2‐negative individuals. The participants who worked with H2‐positive pigs between September and December 2006 on Farm 1 were grouped as “exposed”, and the remaining participants from both Farms 1 and 2 were grouped as “unexposed”. Continuous variables were compared using an independent samples two‐tailed t‐test, and ordinal outcomes were compared using either Fisher’s exact test (for binomial outcomes) or Pearson’s chi‐square (for polynomial outcomes). Antibody titers were evaluated as a dichotomous outcome, with HI and MNT titers ≥1:40 or higher considered to be positive, showing evidence of previous infection. The measure of a 1:30–1:40 HI antibody titer has been associated with a 50% protective level of antibody with human influenza infection. 14 , 15
Results
A total of 27 swine workers were willing to participate from the two farms. Participant demographics can be seen in Table 1. Eight of the 27 participants were born prior to 1968, and one participant had an unknown birth date. Sixteen employees (of 40 total) consented to participate from Farm 1, where H2‐positive pigs had been identified in 2006. Of these participants, 69% (11 of 16) had been employed by Farm 1 between August and December 2006. At Farm 2, where there had been no history of H2 influenza infection in pigs, 11 swine workers (of 14 total) were willing to participate.
Table 1.
Demographic characteristics of all 27 study participants and exposed and unexposed groups
| All participants (%) | Exposed participants | Unexposed participants | P‐value | |
|---|---|---|---|---|
| Age in years (mean, range)* | 35, 19–58 | 36, 24–58 | 34, 19–51 | 0·611 |
| Number of persons born prior to 1968* | 8 | 4 | 4 | 0·683 |
| Gender | ||||
| Male | 23 | 10 | 13 | 0·488 |
| Female | 4 | 1 | 3 | – |
| Smoke or chew tobacco | 12 (44) | 6 | 6 | 0·452 |
| Currently vaccinated for seasonal influenza (2007–2008) | 7 (26) | 1 | 6 | 0·183 |
| Vaccinated for seasonal influenza in last 3 years | 10 (37) | 4 | 6 | 0·687 |
| Reported influenza in last 3 years | 9 (33) | 4 | 5 | 1·0 |
| Exposed to H2‐positive pigs in 2006 | 11 (41) | 11 | 0 | – |
*One participant did not provide an age.
Comparison of exposed and unexposed participants
The exposed and unexposed groups were not significantly different with regard to mean age, proportion of persons born prior to 1968, gender distribution, incidence of vaccination for seasonal influenza (both current and in the last 3 years), incidence of doctor‐diagnosed and self‐reported influenza in the last 3 years, and use of tobacco. The groups also did not differ in their time spent in various pig housing units (breeding, farrowing, nursery, finisher or isolation), use of PPE, or most hand washing practices (data not shown). Both the exposed and unexposed groups were statistically similar with regard to positive H1 or H3 serum antibody titer (data not shown).
Comparison of H2 antibody‐positive and negative participants
Four participants were found to have an antibody titer of greater than 1:40 to H2 influenza by either HI or MNT (Table 2). Three of the four persons were born prior to 1968, and the fourth person had an unknown birth date. Only one of these persons was exposed to H2‐positive pigs, and he was born in 1949. Of the eight participants who are known to have been born prior to 1968, three of them (38%) were positive for H2 antibodies. None of the eight control sera had a positive H2 antibody titer. The study population did not differ significantly from the controls with regard to overall prevalence of positive H2 antibody titer (Fisher’s exact test, P = 0·55).
Table 2.
Summary of serologic response in H2 antibody‐positive participants
| Age (years) | HI assay result | MNT assay result | Exposed to H2N3‐positive pigs? |
|---|---|---|---|
| 51 | 1:80 | 1:40 | No |
| 51 | 1:40 | 1:20 | No |
| 58 | 1:80 | 1:40 | No |
| Unknown | 1:40 | 1:80 | Yes |
HI, hemagglutination inhibition.
Comparison of the H2‐positive and negative participants differed significantly only with regard to mean age [t = 4·74, P = 0·00, 95%CI (11·8, 29·9)] and proportion of births before 1968 (Fisher’s exact test, P = 0·02) (Table 3). The groups were statistically similar with regard to gender, though no women had a positive H2 titer. The H2‐positive and negative groups were also statistically equivalent with regard to incidence of vaccination for seasonal influenza (both current and in the last 3 years), incidence of doctor‐diagnosed and self‐reported influenza in the last 3 years, use of tobacco, time spent in various pig housing units, use of PPE, and hand washing practices (data not shown). All H2‐positive workers were born prior to 1968 except for one person with an unknown date of birth. Only one of these individuals was exposed to H2‐positive pigs.
Table 3.
Comparison of H2 antibody‐positive and negative participants
| Seropositive participants | Seronegative participants | P‐value | |
|---|---|---|---|
| No. participants | 4 | 23 | – |
| Smoke or chew tobacco | 0 | 12 | 0·106 |
| Currently vaccinated for seasonal influenza (2007–2008) | 0 | 7 | 0·545 |
| Vaccinated for seasonal influenza in last 3 years | 1 | 9 | 0·758 |
| Reported influenza in last 3 years | 2 | 7 | 0·582 |
| Exposed to H2‐positive pigs in 2006 | 1 | 10 | 1·0 |
| Mean age*a (years) | 53 | 33 | 0 |
| Percentage of persons born prior to 1968b (%) | 75 | 22 | 0·022 |
| Gender ratio (male:female) | 4:0 | 19:4 | 1·0 |
*One participant did not provide an age.
aStatistically significant: t = 4·74, P = 0·00, 95%CI (11·8, 29·9).
bStatistically significant: Fisher’s exact test P = 0·022.
Use of personal protective equipment
All workers reported use of some form of PPE. Use of all types of PPE was statistically similar in exposed and unexposed workers, as well as between H2‐seropositive and seronegative workers. Use of PPE was not significantly related to seropositivity when looked at as a trinomial response (“sometimes”, “always”, “never”) or as a binomial response (“sometimes or always”, “never”). Boots were worn by 100% of employees on both farms. Mask‐use was reported “always” by 4% of workers, “sometimes” by 26%, and “never” by 70% of workers. Glove‐use was reported “always” by 37% of workers, “sometimes” by 48%, and “never” by 15% of workers. Special clothing used only when working with pigs was worn by all participants, with 96% reporting use at all times.
Seasonal influenza illness and vaccination
Vaccination in the 2007–2008 season was not statistically associated with a positive H3 or H2 antibody titer, though it was associated with a positive H1 titer (Fisher’s exact test, P = 0·01). Neither H1 nor H3 titers were statistically associated with vaccination in the last 3 years, reported influenza in the last 3 years, or influenza diagnosed by a doctor in the last 3 years. Two of the control sera were positive for H1 antibodies and three for H3 antibodies. The study population did not statistically differ from the controls with regard to prevalence of positive H1 and/or H3 antibody titers.
Discussion
H2 antibody assays
It is likely that the four individuals with H2 antibodies were exposed to the H2N2 virus circulating in humans in the 1950s–1960s. All of the H2 antibody‐positive workers with a known birth date were born prior to 1968, and only one of the individuals was exposed to the H2N3‐positive pigs. Differentiating the antibody titer response of this individual to the human pandemic strain of H2 versus the 2006 H2 swine strain cannot be done with the serologic tests performed in this study, because significant cross‐reaction exists between the human H2 strain and the swine H2 strain (Richard Webby, personal communication). Further laboratory tests, such as hemabsorption assays, would be required to confirm that these four individuals seroconverted to the swine H2N3 influenza virus in 2006 rather than the human H2N2 virus earlier in life.
The window for exposure of our study population to H2 influenza‐infected pigs is well‐defined by repeated diagnostic sampling and clinical examinations of the pigs. As it is the only time period during which the virus was isolated from swine nasopharyngeal swabs, it is unlikely that any of the employees were exposed to H2N3‐positive pigs before or after the window of August through December 2006. In February 2008, serology of the swine herd showed that older seropositive sows were still present in the herd, but they were housed with new gilts that remained seronegative (data not shown).
The antibody titer cutoff used for both HI and MNT in this study was 1:40, though it has not been documented that both tests are equally sensitive to detection of influenza antibodies, including antibodies to H2 viruses. In 2009, one group used a regression model to identify the correlation of HI and MNT titers to 2009 pandemic H1N1 in stored serum. 16 They identified that a 1:40 HI titer corresponded to a 1:40 MNT titer in children and to a titer of 1:160 and 1:80 in adult and older populations, respectively. To date, no such correlation has been made for H2 virus antibodies, but in the particular case of this study, the use of a 1:80 MNT cutoff would have statistically yielded the same results as the 1:40 cutoff.
Personal protective equipment
There are few studies that investigate the use of PPE by swine workers in tandem with serological measurements. In the current study, no statistical difference in PPE‐use was seen between the H2‐seropositive and seronegative groups, however, the sample size of only 27 workers may have decreased our ability to recognize such an association. As influenza is known to be spread via inoculation of mucous membranes by contaminated hands, droplet transmission, and likely by aerosolized virus particles, it is logical that gloves, masks (N95 or better), boots and protective clothing would be protective. Such equipment is recommended for use by persons undergoing known or expected exposure to other sources of influenza, including birds with highly pathogenic avian influenzas and pigs with swine influenza. 17 , 18 , 19 The actual benefit of PPE and the subsequent alleviation of risk to those occupationally exposed to swine influenza viruses are yet unquantified, and this subject requires more attention and investigational research.
Seasonal influenza vaccination
Seasonal influenza vaccination is recommended by the National Pork Board for all workers at swine facilities to prevent co‐infection with swine and human influenza viruses. 19 Numerous manuscripts have highlighted the importance of influenza vaccination for swine workers. 6 , 7 , 20 In our study, 26% of the participating workers reported current vaccination (for the 2007–2008 season) for seasonal influenza. Most unvaccinated individuals could not give a reason for forgoing vaccination. Among other concerns, some workers felt that it was not needed, inconvenient or could cause side‐effects. Current vaccination was associated with a positive H1 antibody titer but not a positive H3 antibody titer. The association with H1 antibody identification is most likely due to effective cross‐reaction between the antigen used in the MNT and HI tests and the H1 subtype included in the seasonal vaccine.
Conclusion
This study did not show evidence of swine‐to‐human transmission of H2N3, as seroconversion to H2 influenza was only associated with age and birth before 1968. There was no relationship between positive H2 titers and seasonal influenza vaccination, reported illness over the past 3 years, PPE‐use or hand‐washing.
The small sample size in this study is certainly one of its limitations, though it was unavoidable due to the small number of employees present at the time of the H2N3 infection in the pigs, and to the fact that the identification of H2N3 was a rare event. The virus was only known to be present at two farms in the United States, one of which declined to participate in this study. In addition, at the time of testing, turnover of employees limited the number of individuals available who had been exposed to the pigs eighteen months before.
Further investigations into the H2 antibody seroprevalence of the general population would be informative, especially with regard to groups born before and after 1968, the last time H2 influenza was identified in human circulation. In addition, it is unknown whether there is a higher prevalence of seroconversion in swine workers than in the general population, a finding which was not identified in this analysis. This concern could have been better addressed with a larger number of controls who were matched for age.
The delayed collection of employee blood samples after swine infection was not optimal. It is possible that the 18‐month period after exposure of the Farm 1 workers to the H2N3 influenza‐positive pigs allowed waning antibody titers to obscure our serology interpretation. There is evidence, however, that people and pigs can remain seropositive for a period longer than 18 months. 21 , 22
The results of this study indicate that continued research of influenza transmission, both from pigs to people and vice versa, is needed. We showed no evidence of human infection with the H2N3 swine influenza, despite continued employee contact with ill pigs throughout the period of virus shedding. This indicates that there is more involved in interspecies influenza transmission than mere proximity and contact. Although it is important to remember that protecting swine workers from potential infection is important (including the use of PPE and seasonal influenza vaccination), there are likely many host, pathogen and environmental factors that interact to allow or prevent interspecies transmission. Further research into the risk factors, both behavioral and immunological, that play a role in human and swine influenza infection is necessary in order to better define the existing gateways that facilitate, and the barriers that prevent, such transmission. The emergence of the novel H1N1 influenza A virus in the spring of 2009 will hopefully spur on further research regarding the transmissibility and spread of influenza viruses between populations of humans and animals.
Funding
Partial funding supported by Centers for Disease Control and Prevention (Cooperative Agreement Number U19 C1000407) and by the National Institute of Allergy and Infectious Diseases (R01 AI068803‐01A1).
Conflict of Interest
Marie Gramer acted as paid consultant to Pfizer Animal Health and Novartis Animal Health. Amanda Beaudoin has received funding from the National Pork Board and Pfizer Animal Health for research in the past five years but that funding was not related to this work. She has also received fees for speaking at various pork producer and swine veterinary meetings.
Acknowledgements
Jim Lowe, Carthage Veterinary Services, Illinois.
References
- 1. Centers for Disease Control and Prevention . Swine influenza A (H1N1) infection in two children – Southern California, March–April 2009. Morb Mortal Wkly Rep 2009; 58:1–3. Available at http://www.cdc.gov/mmwr/preview/mmwrhtml/mm58d0421a1.htm (Accessed 21 May 2009). [PubMed] [Google Scholar]
- 2. Olsen CW, Brown IH, Easterday BC, Van Reeth K. Swine Influenza; in Straw BE, Zimmerman JJ, D’Allaire S, Taylor DJ. (eds): Diseases of Swine, 9th edn Ames, Iowa: Blackwell Publishing, 2006; 469–482. [Google Scholar]
- 3. Centers for Disease Control and Prevention . Key facts about swine influenza. 2009. Available at http://www.cdc.gov/flu/swineflu/key_facts.htm (Accessed 7 May 2009).
- 4. Myers KP, Olsen CW, Gray GC. Cases of swine influenza in humans: a review of the literature. Clin Infect Dis 2007; 44:1084–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Olsen CW, Brammer L, Easterday BC et al. Serologic evidence of H1 swine influenza virus infection in swine farm residents and employees. Emerg Infect Dis 2002; 8:814–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gray GC, McCarthy T, Capuano AW, Setterquist SF, Olsen CW, Alavanja MC. Swine workers and swine influenza virus infections. Emerg Infect Dis 2007; 13:1871–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Myers KP, Olsen CW, Setterquist SF et al. Are swine workers in the United States at increased risk of infection with zoonotic influenza virus? Clin Infect Dis 2006; 42:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Krauss S, Walker D, Pryor SP et al. Influenza A viruses of migrating wild aquatic birds in North America. Vector Borne Zoonotic Dis 2004; 4:177–189. [DOI] [PubMed] [Google Scholar]
- 9. Liu JH, Okazaki K, Bai GR, Shi WM, Mweene A, Kida H. Interregional transmission of the internal protein genes of H2 influenza virus in migratory ducks from North America to Eurasia. Virus Genes 2004; 29:81–86. [DOI] [PubMed] [Google Scholar]
- 10. Munster VJ, Baas C, Lexmond P et al. Spatial, temporal, and species variation in prevalence of influenza A viruses in wild migratory birds. PLoS Pathog 2007; 3:e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schafer JR, Kawaoka Y, Bean WJ, Suss J, Senne D, Webster RG. Origin of the pandemic 1957 H2 influenza A virus and the persistence of its possible progenitors in the avian reservoir. Virology 1993; 194:781–788. [DOI] [PubMed] [Google Scholar]
- 12. Ma W, Vincent AL, Gramer MR et al. Identification of H2N3 influenza A viruses from swine in the United States. Proc Natl Acad Sci USA 2007; 104:20949–20954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rowe T, Abernathy RA, Hu‐Primmer J et al. Detection of antibody to avian influenza A (H5N1) virus in human serum by using a combination of serologic assays. J Clin Microbiol 1999; 37:937–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hobson D, Curry RL, Beare AS, Ward‐Gardner A. The role of serum haemagglutination‐inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. J Hygiene 1972; 70:167–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Potter CW, Jennings R, Nicholson K, Tyrrell DAJ, Dickinson KG. Immunity to attenuated influenza virus WRL 105 infection induced by heterologous, inactivated influenza A virus vaccines. J Hygiene 1977; 79:321–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hancock K, Veguilla V, Lu X et al. Cross‐reactive antibody responses to the 2009 pandemic H1N1 influenza virus. Supplementary appendix. N Engl J Med 2009; 361:1945–1952. [DOI] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention . Influenza (flu) | Interim guidance for protection of persons involved in U.S. avian influenza outbreak disease control and eradication activities. Available at http://www.cdc.gov/flu/avian/professional/protect‐guid.htm (Accessed 13 May 2009).
- 18. Centers for Disease Control and Prevention . H1N1 flu | Interim guidance for people who have close contact with pigs in non‐commercial settings: preventing the spread of influenza A viruses, including the novel influenza A (H1N1) virus. Available at http://www.cdc.gov/H1N1flu/guidelines_pig_workers.htm (Accessed 8 September 2009).
- 19. National Pork Board . Worker safety – zoonoses. Available at http://www.pork.org/WorkerSafety/Default/safety‐topics/zoonoses.aspx (Accessed 13 May 2009).
- 20. Gray GC, Baker WS. The importance of including swine and poultry workers in influenza vaccination programs. Clin Pharmacol Ther 2007; 82:638–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yu X, Tsibane T, McGraw PA et al. Neutralizing antibodies derived from the B cells of 1918 influenza pandemic survivors. Nature 2008; 455:532–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Desrosiers R, Boutin R, Broes A. Persistence of antibodies after natural infection with swine influenza virus and epidemiology of the infection in a herd previously considered influenza‐negative. J Swine Health Prod 2004; 12:78–81. [Google Scholar]


