Abstract
Objectives
Many suicidal patients treated and released from emergency departments (ED) fail to follow through with subsequent outpatient psychiatric appointments, often presenting back for repeat ED services. Thus, the authors sought to determine whether a mobile crisis team (MCT) intervention would be more effective than standard referral to a hospital-based clinic as a means of establishing near-term clinical contact after ED discharge. This objective was based on the premise that increased attendance at the first outpatient mental health appointment would initiate an ongoing treatment course, with subsequent differential improvements in psychiatric symptoms and functioning for patients successfully linked to care.
Methods
In a rater-blinded, randomized controlled trial, 120 participants who were evaluated for suicidal thoughts, plans, or behaviors, and who were subsequently discharged from an urban ED, were randomized to follow-up either in the community via a MCT or at an outpatient mental health clinic (OPC). Both MCTs and OPCs offered the same structured array of clinical services and referral options.
Results
Successful first clinical contact after ED discharge (here described as “linkage” to care) occurred in 39 of 56 (69.6%) participants randomized to the MCT versus 19 of 64 (29.6%) to the OPC (relative risk = 2.35, 95% CI = 1.55–3.56, p < 0.001). However, we detected no significant differences between groups using intention-to-treat analyses in symptom or functional outcome measures, at either 2 weeks or 3 months after enrollment. We also found no significant differences in outcomes between participants who did attend their first prescribed appointment via MCT or OPC versus those who did not. However divided (MCT vs. OPC, present at first appointment vs. no show), groups showed significant improvements but maintained clinically significant levels of dysfunction and continued to rely on ED services at a similar rate in the 6 months after study enrollment.
Conclusions
Community-based mobile outreach was a highly effective method of contacting suicidal patients who were discharged from the ED. However, establishing initial postdischarge contact in the community versus the clinic did not prove more effective at enhancing symptomatic or functional outcomes, nor did successful linkage with outpatient psychiatric care. Overall, participants showed some improvement shortly after ED discharge regardless of outpatient clinical contact, but nonetheless remained significantly symptomatic and at risk for repeated ED presentations.
Keywords: suicide, psychiatry, mobile crisis, health services research
Suicide is a significant public health problem,1 and the immediate site of contact with organized health care for suicidal individuals often is the emergency department (ED). The Centers for Disease Control and Prevention estimates that of the approximately 115 million U.S. ED presentations occurring in 2005, at least 4,200,000 (3.5%) were associated with symptoms of a mental disorder.2 This is likely to be a significant underestimation. Other authors estimate the proportion of ED patients who present with mental disorders to be closer to 6%.3 Additionally, the prevalence of suicidal intent in ED patients who present for other “medical” reasons approaches 11%.4 At the same time that significant psychiatric morbidity manifests in large numbers of ED patients, U.S. emergency medical services are increasingly overwhelmed and unprepared to deal with suicidal individuals. ED visits have increased dramatically during recent years while the number of EDs has declined, resulting in higher acuity, increased gridlock, and an increased concentration of patients with psychiatric disorders in the remaining EDs.5,6
As the availability of inpatient psychiatric beds has declined steadily for the past four decades, most patients expressing suicidal thoughts or less dangerous behaviors are not admitted to the hospital and instead are referred to outpatient psychiatric care. However, the clinical trajectory of patients discharged from EDs is poorly understood. Our own preliminary investigation of 100 patients referred from ED to urgent outpatient care demonstrated a “no-show” rate exceeding 90% (Currier G, Caine E, unpublished data, April 2001).
Mobile crisis teams (MCTs) serve as adjuncts or alternatives to ED psychiatric care in a majority of U.S. states.7 MCTs provide psychiatric assessment and crisis stabilization services in patients’ homes and other sites with a goal of diverting lower-intensity cases from overcrowded EDs.8 MCT services are associated with relatively high rates of consumer and provider satisfaction,9 although much of the published data concerning MCTs are more than 20 years old. We are not aware of any studies that test the efficacy of MCTs as post-ED follow-up interventions to enhance connection with ongoing outpatient care.
Several previous studies have considered patient or service factors thought to be predictive of successful referral to outpatient mental health treatment.10,11 Positive predictors of initial linkage include reduced wait time for receipt of first appointment and “bridging strategies” that improve information flow between levels of service. Positive predictors of retention in outpatient care include short wait to see a physician and receipt of psychotropic medication early in the treatment course. However, this literature generally does not reflect current barriers to timely access to psychiatric care, when wait times in many community mental health centers are protracted.
Even if barriers to access can be radically reduced, several unanswered questions remain related to the effectiveness of outpatient mental health treatment for suicidal individuals who receive ED care. The current practice of referring almost all suicidal patients from ED to outpatient psychiatric care is predicated on several untested assumptions:
All discharged ED patients who present with suicidal thoughts or behaviors are appropriate candidates for therapeutic interventions in outpatient clinical settings, typically in regularly scheduled visits of once-per-week sessions.
Thus, participation in outpatient psychiatric care is the “active ingredient” for clinical improvement among referred suicidal patients during the weeks and months after ED discharge and clinical referral.
Individual resistance to engaging in outpatient treatment is a poor decision, and clinician-driven strategies to overcome such reluctance are almost always well advised.
Based on the above assumptions, we hypothesized that MCTs would be significantly more successful at establishing contact with discharged individuals and that people who connected with a first clinical contact after ED discharge would be more likely to establish a continuing course of care, with greater associated improvements in measured symptom and functional outcomes.
METHODS
Study Design
This was a rater-blinded, randomized controlled trial to assess the relative effectiveness of using MCTs compared to expedited outpatient psychiatric appointments to link suicidal ED patients to outpatient mental health services after ED discharge. To reduce risk of coercion, at least one member of the ED clinical treatment team provided written attestation that the patient was able to understand the study and was appropriate for inclusion before any member of the research team approached potential participants. After this attestation, research staff described the project orally before obtaining written informed consent, which included a detailed description of the study. The institutional review board at the University of Rochester Medical Center reviewed and approved this study. The National Institutes of Health granted a certificate of confidentiality.
Study Setting and Population
The Department of Psychiatry of the University of Rochester Medical Center operates a regional Comprehensive Psychiatry Emergency Program (CPEP), a state-certified entity that is a component of the ED of Strong Memorial Hospital. The CPEP includes a large, urban psychiatric emergency service, with 24-hour physician coverage, mobile crisis services, 72-hour extended observation beds, and direct access to crisis residence beds in the local community. From December 2002 to November 2007, the CPEP assessed more than 7,500 admitted patients annually and also provided more than 1,500 consultations per year to patients in the general ED. The MCT provides community-based assessments and triage services to approximately 3,500 patients per year. Clinicians and staff of the CPEP have had significant experience conducting clinical drug trials, with a well-developed research infrastructure.
Potential participants included adults (ages 18 years and above) who presented voluntarily or were brought by police (“mental hygiene arrest”) to the ED. Treating attending psychiatrists who were unaffiliated with the study assessed patients’ need for hospitalization in the course of routine clinical care. All eligible participants who were present for ED evaluation Monday through Friday, 8 am–8 pm, between February 2004 and December 2005 were invited to participate. The presence of suicidal thoughts, plans, or behaviors was necessary for participation, as indicated for English- and Spanish-speaking adult patients by a rating of “1” or higher on the scale by Pfeffer et al.,12 the Spectrum of Suicidal Behavior. This five-item scale rates suicidal behavior within the previous 24 hours and includes ratings of non-suicidal, suicidal ideation, threat, mild attempts, or serious attempts. Potential participants could not already be in regular care with any public or private mental health clinician, were assessed as suitable for discharge from the ED by their treating psychiatrist, and expressed a willingness to accept outpatient follow-up care.
We excluded potential participants if they were less than 18 years old, were not rated as suicidal, were deemed incapable of providing informed consent, or already participated in outpatient mental health treatment. The only a priori diagnostic exclusions involved mental retardation or dementia, either previously diagnosed or suspected. Therefore, people with active substance abuse disorders, personality disorders, psychosis, and a variety of other disorders were included in this study.
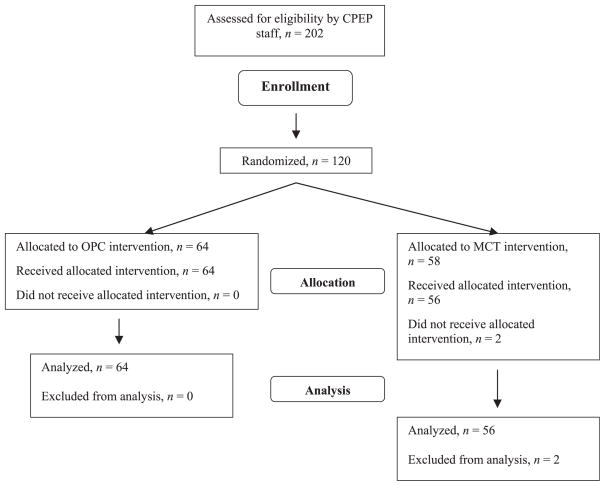
To determine symptom and functional status, participants were interviewed by research staff just prior to their discharge from the ED and subsequently in the community or in an office adjacent to the ED at 2 weeks (±1 week) following discharge and again at 3 months (±2 weeks) postdischarge. Each subject received a prepaid grocery store debit card in recognition of time spent participating in the study for each contact: $40 at enrollment, $50 at first research contact (2 weeks), and $60 at second contact (2 months). Figure 1 presents the flow of participants through the protocol.
Figure 1.
Study enrollment. CPEP = comprehensive psychiatry emergency program; MCT = mobile crisis team; OPC = outpatient psychiatry clinic.
Independent of these research assessments, ED and mental health service use data were available for study subjects even if study staff were not able to interview participants directly after ED discharge. Patient-level health service usage data in any health system within Monroe County are reported to a central data repository that was available to study investigators. A 6-month time frame was assumed to be the longest window in which a moderate intervention effect would likely be detectable.
Study Protocol
Prior to disposition, all patients in CPEP were assessed for suicide risk and appropriateness for discharge by a board-certified attending psychiatrist on service around the clock. Following the consent process and the first study evaluation, which was carried out in a private room in the ED area, participants were assigned to one of the treatment arms. The specific procedure in the CPEP used a preset series of sealed envelopes designed to assure that each subject was enrolled and consented to study participation before treatment assignment was determined. Each envelope contained instructions for outpatient psychiatric clinic (OPC) or MCT assignment, and this information was presented to the patient-subject by the clinical nurse on duty in the ED, who then provided appropriate discharge information to the subject. Research staff remained blind to each subject’s treatment assignment.
The experimental intervention consisted of community-based clinical assessment conducted by the MCT within 48 hours of discharge at a location of the subject’s choice. “Treatment as usual” consisted of referral by treating physicians to appointments in our crisis OPC, which has a mandatory requirement of offering a first clinical appointment within 5 business days of ED discharge. The content of both the first MCT and OPC appointments was the same and clinical interventions in both groups were guided by the same written manual. This consisted of a review of presenting problems, a reexamination of psychiatric symptoms and attitudes toward treatments, and an assessment of need for further mental health, medical, or chemical dependency services at that point in time. Both MCT and OPC clinicians could refer patients to other forms of continuing care if indicated.
Measures
The primary study endpoints included comparisons between groups for rate of linkage into outpatient care (defined as completion of the appointment with either MCT or OPC scheduled before ED discharge and cumulative amount of outpatient mental health clinical contact in the 6 months post–ED discharge) and changes in depression rating scores and functional assessments over 2-week and 3-month intervals subsequent to enrollment. Interviews lasted approximately 1 hour and included ratings of current suicide risk, current depression, overall psychiatric symptoms, and functional status, as well as a qualitative component exploring participants’ experience of the trial.
The Spectrum of Suicidal Behavior12 is a clinician-administered five-item screening scale for suicide rated in increasing risk severity from 0 (nonsuicidal) through 4 (serious attempt). The Hamilton Depression rating scale13 is a rater-administered scale of depression severity. This study employed the 17-item version, rated on a scale of 0 (no depression) to 54 (severe depression). The Brief Psychiatric Rating Scale14 is an 18-item rater-administered scale that assesses psychotic symptoms, affective symptoms, and overall psychopathology. The Behavior and Symptom Identification Scale (BASIS-32)15 is a self-reported measure of symptoms and functional health status. Each item is rated on a five-point scale from 0 (no difficulty) to 4 (extreme difficulty). The Scale for Suicidal Ideation16 is a 21-item rater-administered assessment of suicidal thoughts with a possible scoring range of 0–38.
Data Analysis
When designing the study, we determined that a total sample size of 120 participants (60 per group) would provide 95% power for detecting a significant difference in anticipated linkage rates between the MCT-intake group (40% anticipated linkage) and the treatment-as-usual group (10% anticipated linkage), using a two-sided alpha level of 0.05.
The study employed intention-to-treat analysis, and all participants who underwent random allocation were analyzed according to group assignment. All data analysis was carried out according to a preestablished analysis plan. Proportions were compared by using chi-square tests with continuity correction or Fisher’s exact test when appropriate. Changes in measures between groups over time were assessed using analysis of variance for repeated measures. A two-sided p-value of less than 0.05 was considered statistically significant. Given our expectation that many subjects would potentially be lost to follow-up, we chose to employ a conservative last observation carried forward methodology when analyzing intervention effects.17 Data were analyzed using the SAS 9.1 statistical package (SAS Institute, Cary, NC).
RESULTS
Subject enrollment and retention is presented in Figure 1, and baseline variables are presented in Table 1. Slightly fewer than half of participants were male, while slightly more than half of the participants were white. Diagnostically, most participants were given the diagnosis of “adjustment disorder,” suggesting to us that thresholds were not met for other DSM-IV Axis I disorders. The second most frequent diagnosis was “depression, not otherwise specified,” a common rubric used in our ED when depressive symptoms are prominently present in the context of one of several co-occurring substance use disorders. The remaining participants were diagnosed with a major mood or substance abuse disorder or an assortment of other diagnoses. A majority of subjects presented with suicidal ideation (with or without plans) or a noninjurious attempt. However, of note, almost one in 10 presented with a more serious attempt regarded as having a higher degree of potential lethality. A substantial proportion of participants had been brought to the ED involuntarily, and several participants received medications while in the ED. Three subjects had undergone physical restraint during the index episode of care. Urine toxicology screens were obtained for participants based both on clinical assessment that raised concerns about intoxication or substance use and on patient willingness to provide a sample. Over half of those tested were positive for cocaine, amphetamines, or tetrahydrocannabinol.
Table 1.
Demographic and Clinical Characteristics of Participants by Treatment Group*
| Demographics and Diagnoses | OPC (n = 64), n (%) | MCT (n = 56), n (%) | Total, N (%) | p-value |
|---|---|---|---|---|
| Male sex | 29 (45.3) | 23 (41.1) | 52 (43.3) | 0.64 |
| Age (yr), mean [range] | 30.9 [28.5–33.3] | 34.5 [31.4–37.7] | 32.7 (10.8) [18–69] | 0.06 |
| Race | 0.23 | |||
| African American or Black | 26 (40.6) | 17 (30.4) | 43 (35.8) | |
| White | 34 (53.1) | 37 (66.1) | 72 (60) | |
| Hispanic | 4 (6.3) | 1 (1.8) | 16 (13.3) | |
| Native American | 0 (0) | 1 (1.8) | 1 (0.8) | |
| Education | 0.23 | |||
| Less than eighth grade | 1 (1.6) | 4 (7.3) | 5 (4.2) | |
| Some high school or graduate | 40 (63.5) | 26 (47.9) | 66 (55.0) | |
| Some college or graduate | 22 (34.9) | 25 (45.5) | 47 (39.2) | |
| Residence | 0.25 | |||
| Homeless | 2 (4.5) | 2 (4.8) | 4 (3.3) | |
| Owns or rents home | 39 (86.7) | 31 (73.8) | 70 (58.3) | |
| Other | 4 (8.9) | 9 (21.4) | 13 (10.8) | |
| Social support (lives with) | 0.28 | |||
| Alone | 12 (30.8) | 13 (38.2) | 25 (20.8) | |
| Spouse or child | 11 (28.2) | 13 (38.2) | 24 (20.0) | |
| Others | 16 (41.0) | 8 (23.5) | 24 (20.0) | |
| Financial support | 0.97 | |||
| Unemployed/none | 19 (32.8) | 12 (38.2) | 31 (25.8) | |
| FT/PT employment | 28 (48.3) | 24 (53.3) | 52 (43.3) | |
| Family support | 6 (10.3) | 4 (8.9) | 10 (8.3) | |
| SSI/SSDI | 7 (12.1) | 5 (1.1) | 12 (10.0) | |
| ADC/welfare | 11 (19.0) | 9 (1.8) | 20 (16.7) | |
| Diagnosis | 0.92 | |||
| Adjustment disorder | 20 (31.3) | 18 (32.1) | 38 (31.7) | |
| Depression NOS | 15 (23.4) | 11 (19.6) | 26 (21.7) | |
| Major depression | 13 (20.3) | 7 (12.5) | 23 (19.2) | |
| Bipolar disorder | 3 (4.7) | 3 (5.4) | 6 (5.0) | |
| Cocaine abuse | 2 (3.1) | 2 (3.6) | 4 (3.3) | |
| Alcohol use disorders | 2 (3.1) | 3 (5.4) | 5 (4.2) | |
| Other | 9 (14.1) | 12 (21.4) | 21 (17.5) |
p-values from chi-square and Fisher’s exact as appropriate.
ADC = Aid to Dependent Children; FT/PT = full time/part time; MCT = mobile crisis team; NOS = not otherwise specified; OPC = outpatient psychiatry clinic; SSDI = Social Security Disability Insurance; SSI = Supplemental Security Income.
Most participants had significant previous mental health burden and involvement with mental health treatment of some type. A majority endorsed previous suicide attempts, past psychiatric outpatient treatment, current use of alcohol, the presence of at least one chronic medical condition, and past receipt of psychotropic medications. Forty percent had been admitted previously to a psychiatric inpatient service, while a similar number acknowledged current drug abuse, and almost 10% of female participants were pregnant when enrolled. There were no significant differences between groups in any of these variables at enrollment, and no adjustment was necessary for nominated baseline variables. Likewise, no significant differences in baseline clinical ratings were observed.
Retention in Research Follow-up
Of the 120 participants enrolled in the ED, 94 (78.3%) were successfully reevaluated in person by research staff 2 weeks postdischarge, and 76 (63.3%) were evaluated at 3 months (±2 weeks). Research retention rates did not vary by treatment group. Successful contact with the OPC group for research follow-up was 48/64 (75%) at the 2-week point and 37/64 (57.8%) at 12 weeks. For the MCT group, contact was successful in 46/56 (82.1%) at 2 weeks and 39/56 (69.6%) at 12 weeks.
Shortly after enrollment, a clinical staff member erroneously gave an OPC appointment to one subject who had been randomized to MCT. Another subject deteriorated clinically while still in the ED, requiring inpatient admission after randomization but before final ED discharge. Both subject’s initial results were carried forth in the study by assigned group in accord with our intent-to-treat analytic approach. No adverse events were reported in either treatment group.
Health Service Usage Outcomes
Significantly more MCT participants fulfilled the clinical follow-up appointment (initial “linkage”) following ED discharge (39 of 56, or 69.6%) versus participants randomized to OPC (19 of 64, or 29.6%; relative risk = 2.35, 95% CI = 1.55–3.56, p < 0.001). None of the comparisons between linked and unlinked participants shown in Table 2 were significant.
Table 2.
Characteristics of Linked Versus Unlinked Participants
| Subject Characteristic, N = 120 | Linked, n (%) | Unlinked, n (%) | Total | p-value |
|---|---|---|---|---|
| Sex | ||||
| Male | 21 (40.4) | 31 (59.6) | 52 | 0.13 |
| Female | 37 (54.4) | 31 (45.6) | 68 | |
| Race | 0.35 | |||
| White | 38 (53.5) | 33 (46.5) | 71 | |
| African American or Black | 17 (39.5) | 26 (60.5) | 43 | |
| Hispanic | 7 (43.8) | 9 (56.2) | 16 | |
| Other | 3 (50.0) | 3 (50.0) | 6 | |
| Marital status | 3.36 | |||
| Married | 17 (65.4) | 9 (34.6) | 26 | |
| Divorced | 8 (47.1) | 9 (52.9) | 17 | |
| Never married | 27 (42.2) | 37 (57.8) | 64 | |
| Education | 0.10 | |||
| College graduate | 6 (54.5) | 5 (45.5) | 11 | |
| Some college | 24 (66.7) | 12 (33.3) | 36 | |
| High school graduate | 18 (42.9) | 24 (57.1) | 42 | |
| Some high school | 8 (33.3) | 16 (66.7) | 24 | |
| Less than eighth grade | 6 (66.7) | 3 (33.3) | 9 | |
| Voluntary admission to ED | 40 (54.1) | 34 (45.9) | 74 | 0.10 |
| Receipt of meds in ED | 9 (45.0) | 11 (55.0) | 20 | 0.68 |
| Restraints in ED | 2 (66.7) | 1 (33.3) | 3 | 0.52 |
| In ED for actual suicide attempt | 13 (44.8) | 16 (55.2) | 29 | 0.84 |
| Current drug abuser | 19 (40.4) | 28 (59.6) | 47 | 0.14 |
| Current alcohol abuser | 37 (46.8) | 42 (53.2) | 79 | 0.56 |
| Cocaine positive toxicology screen | 3 (27.3) | 8 (72.7) | 11 | 0.14 |
| Past outpatient psychiatric treatment | 38 (52.8) | 35 (48.6) | 72 | 0.31 |
| Prior psychiatric admission | 23 (47.9) | 25 (52.1) | 48 | 0.94 |
| Prior suicide attempt | 33 (48.5) | 35 (51.5) | 68 | 0.96 |
| Current PCP | 42 (53.2) | 37 (46.8) | 79 | 0.17 |
PCP = primary care provider.
Postenrollment Health Service Use
Over the 6 months postenrollment, 38/58 (65.5%) of MCT subjects and 39/64 (60.1%) OPC subjects had at least one repeat ED presentation for a psychiatric complaint. Of subjects who subsequently presented at all to the ED, OPC subjects had a mean of 1.62 visits (SD = ±1.58), whereas OPC subjects had a mean of 1.68 visits (SD = ±1.38, p = 0.84). The mean number of outpatient mental health contacts in the 6 months after enrollment also did not differ significantly between OPC (5.45, SD = ±4.37) and MCT subjects (4.61, SD = ±5.48, p = 0.55).
Clinical Outcomes
As shown in Table 3, regardless of study group allocation, participants improved significantly on all measures between enrollment and 2 weeks (±1 week) and 12 weeks (±2 weeks) after ED discharge. There were no differences noted in magnitude of improvement between the MCT and OPC groups in terms of suicidal ideation, overall psychopathology, or functional status across this time period. While these represented statistically robust, clinically relevant improvements, it is important to note that many of the participants remained significantly symptomatic at the 3-month evaluation. For all measures, a statistically significant improvement in scores (p < 0.0001) was demonstrated from baseline to 3 months of follow-up; however, no difference between treatment groups was observed.
Table 3.
Comparing Participants by Treatment Group
| T0 Enrollment, Mean (SD) | T1 2 Weeks, Mean (SD) | T3 3 Months, Mean (SD) | Changes Over 3 Months’ Time, p-value | OPC vs. MCT: Between Groups, p-value | |
|---|---|---|---|---|---|
| Scale for Suicidal Ideation | <0.0001 | 0.7416 | |||
| OPC | 9.77 (8.32) | 3.77 (6.49) | 3.11 (5.95) | ||
| MCT | 9.82 (7.33) | 3.68 (6.25) | 3.91 (6.86) | ||
| Brief Psychiatric Rating Scale | <0.0001 | 0.9709 | |||
| OPC | 41.65 (9.95) | 36.71 (9.07) | 34.97 (9.19) | ||
| MCT | 40.11 (9.68) | 34.95 (9.57) | 33.53 (10.13) | ||
| Hamilton Depression Scale | <0.0001 | 0.9333 | |||
| OPC | 45.60 (7.94) | 41.10 (8.59) | 40.44 (10.34) | ||
| MCT | 43.16 (9.71) | 38.42 (8.83) | 37.49 (9.40) | ||
| BASIS-32 Functional Scale | <0.0001 | 0.6520 | |||
| OPC | 49.77 (15.78) | 40.52 (17.90) | 33.71 (18.43) | ||
| MCT | 50.05 (17.97) | 38.24 (19.47) | 33.56 (20.13) |
BASIS-32 = Behavior and Symptom Identification Scale; MCT = mobile crisis team; OPC = outpatient psychiatry clinic.
To examine the impact of successful first contact by any means, data were reexamined to compare differences in outcomes for participants who successfully linked into first contact versus those who did not, regardless of initial randomization group. As shown in Table 4, there were no statistically significant differences in rates of improvement between the linked and unlinked groups in terms of suicidal ideation, overall psychopathology, or functional status. The differences on the Hamilton Depression Rating Scale between linked and unlinked approached statistical significance (p < 0.06), but apparent differences had little clinical meaning, given the magnitude of the scores. As noted with the comparison of treatment modalities, on average both participants who were linked and who did not link tended to improve over time, although many remained notably symptomatic at the 3-month point.
Table 4.
Clinical Improvement: Linked Versus Unlinked Groups
| T0 Enrollment, Mean (SD) | T1 2 Weeks, Mean (SD) | T3 3 Months, Mean (SD) | p-value | |
|---|---|---|---|---|
| Scale for Suicidal Ideation | 0.5022 | |||
| Unlinked | 10.50 (8.64) | 2.47 (4.96) | 1.78 (4.14) | |
| Linked | 9.61 (7.88) | 2.48 (5.28) | 2.89 (6.05) | |
| Brief Psychiatric Rating Scale | 0.4055 | |||
| Unlinked | 40.50 (9.54) | 35.84 (9.13) | 33.28 (9.92) | |
| Linked | 40.50 (9.62) | 33.45 (8.91) | 31.93 (9.04) | |
| Hamilton Depression Scale | 0.0567 | |||
| Unlinked | 44.34 (8.64) | 41.20 (8.92) | 40.25 (10.42) | |
| Linked | 44.57 (9.16) | 38.45(8.47) | 37.83 (9.44) | |
| BASIS-32 Functional Scale | 0.7391 | |||
| Unlinked | 51.53(16.14) | 40.50(20.51) | 30.66 (19.65) | |
| Linked | 49.61(15.34) | 36.77(17.66) | 30.00 (18.46) |
BASIS-32 = Behavior and Symptom Identification Scale.
DISCUSSION
To our knowledge, this is the first trial to test the effectiveness of MCTs for linking discharged ED patients having suicidal ideas, plans, or attempts to outpatient psychiatric services. Mobile outreach appears to be a highly effective method of contacting suicidal patients who have been discharged from the ED. However, our data indicate that study participants experienced substantial clinical and functional improvements during the ensuing 3-month period, irrespective of treatment assignment or linkage to care. Scores on the Scale for Suicidal Ideation (SSI), in particular, were substantially and meaningfully lower at 2 weeks and did not change at 3-month assessment. Thus, while MCT succeeded beyond our initial expectation to enhance the probability of initial linkage, it apparently contributed little to improving patient outcomes versus OPC. Moreover, there was no evidence that undergoing an outpatient evaluation during the days immediately following ED discharge led to enhanced improvements in symptom or functional measures in this specific group of ED service users.
Our findings challenge several widely held assumptions upon which ED care of suicidal patients is based: 1) linkage to ED aftercare for suicidal patients is necessary for clinical improvement and 2) patients who participate in aftercare, however briefly, are likely to have better outcomes, given that ED care alone is not associated with measurable improvement. The design of the study was sufficiently sensitive to demonstrate clinical and functional improvements, and the rate of subject retention was clearly adequate to meet our assessment objectives. At the same time, many participants remained highly symptomatic, a situation that could lend itself to repeat ED visits if participants were faced with stressful life circumstances.
Our results open a new array of questions for exploration. It appeared that in many instances, the ED visit itself was sufficient to offer a basis for temporary, clinically significant improvement. This finding warrants further exploration—what happens when someone is evaluated, briefly engaged, and discharged? Are there low-cost measures that could be added to enhance such effects? Should all patients be assigned an urgent outpatient appointment, consistent with our current practice, or are there subgroups for whom this approach is unnecessary or even counterproductive? Perhaps it might be more worthwhile to offer appointments only to those who wish immediate follow-up, while providing a “ready-access” telephone contact for appointments when patients call for care. This might mitigate inappropriate reuse of the ED following index contact, and help address the challenging problem of “no-shows,” while offering expedited access to care at a time of increased distress. These findings demonstrate the need for rigorous examination of popular but untested assumptions upon which clinical management of suicidal individuals is based.
LIMITATIONS
The study subject sample was heterogeneous in terms of diagnosis and other important personal and social characteristics. This also was a subset of patients who presented for ED services with variable degrees of suicidal ideas, intent, or behavior, but who were all evaluated as sufficiently stable and safe for discharge. Our study design, sampling strategy, and questions differed from other ED based studies,18,19 making it difficult to compare results. At the same time, our findings invite careful consideration of the degree of “regression to the mean” whenever studying clinical improvement in a population as diverse, and potentially unstable, as suicidal ED patients.
Our sample was relatively small, and suicide is a rare event. Thus, the results of this study do not address the longer-term occurrence of suicide, or attempted suicide, in this group of individuals, nor can they be extrapolated to all patients treated for psychiatric disorders in the ED. Given the circumscribed scope of our evaluations, it was possible that a variety of positive or negative outcomes could have occurred that we did not measure. Finally, given the relatively high number of dropouts from care, the intention-to-treat method may bias results. To address this concern, we reanalyzed data according to actual group assignment and found no significant differences in our results (data not shown).
CONCLUSIONS
Community-based mobile outreach was a highly effective method of contacting suicidal patients who were discharged from the ED. However, establishing initial postdischarge contact in the community as opposed to at the clinic did not prove any more effective at enhancing symptomatic or functional outcomes, nor did successful linkage with outpatient psychiatric care. Overall, participants did show some improvement shortly after ED discharge regardless of outpatient clinical contact, but nonetheless remained significantly symptomatic and at risk for repeated ED presentations.
Acknowledgments
The authors express their gratitude to Paul Winters, MS, for his statistical support. Dr. Currier had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Supported, in part, by grant K23MH064517 (G. Currier, PI) from the National Institute of Mental Health and in part by grant P20 MH71897 to the NIMH/NIDA-funded Center for Public Health and Population Interventions for Preventing Suicide (E.D. Caine, PI).
Footnotes
Presented at the American Psychiatric Association, Institute on Psychiatric Services annual conference, New Orleans, LA, October 2007.
References
- 1.Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing about it? Am J Public Health. 2004;94:37–45. doi: 10.2105/ajph.94.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nawar EW, Niska RW, Xu J. [Accessed August 26, 2008];National Hospital Medical Care Survey: 2005 Emergency Department Summary. Available at: http://www.cdc.gov/nchs/data/ad/ad386.pdf. [PubMed]
- 3.Larkin GL, Claassen CA, Edmond JA, Pelletier AJ, Camargo CA., Jr Trends in U.S. emergency department visits for mental health conditions, 1992–2001. Psychiatr Serv. 2005;56:671–7. doi: 10.1176/appi.ps.56.6.671. [DOI] [PubMed] [Google Scholar]
- 4.Claassen CA, Larkin GL. Occult suicidality in an emergency department population. Br J Psychiatry. 2005;186:352–3. doi: 10.1192/bjp.186.4.352. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Hospital-based emergency care: at the breaking point. Washington, DC: National Academies Press; 2006. The future of emergency care in the United States health system. [Google Scholar]
- 6.Currier GW, Allen M. Organization and function of academic psychiatric emergency services. Gen Hosp Psychiatry. 2003;25:124–9. doi: 10.1016/s0163-8343(02)00287-6. [DOI] [PubMed] [Google Scholar]
- 7.Geller JL, Fisher WH, McDermeit M. A national survey of mobile crisis services and their evaluation. Psychiatr Serv. 1995;46:893–7. doi: 10.1176/ps.46.9.893. [DOI] [PubMed] [Google Scholar]
- 8.Scott RL. Evaluation of a mobile crisis program: effectiveness, efficiency, and consumer satisfaction. Psychiatr Serv. 2000;51:1153–6. doi: 10.1176/appi.ps.51.9.1153. [DOI] [PubMed] [Google Scholar]
- 9.Fisher WH, Geller JL, Wirth-Cauchon J. Empirically assessing the impact of mobile crisis capacity on state hospital admissions. Comm Mental Health J. 1990;26:245–53. doi: 10.1007/BF00752775. [DOI] [PubMed] [Google Scholar]
- 10.Boyer CA, McAlpine DD, Pottick KJ, Olfson M. Identifying risk factors and key strategies in linkage to outpatient psychiatric care. Am J Psychiatry. 2000;157:1592–8. doi: 10.1176/appi.ajp.157.10.1592. [DOI] [PubMed] [Google Scholar]
- 11.Van Heeringen C, Jannes S, Buylaert W, Hendrick H, De Bacquer D, Van Roomrtel J. The management of non-compliance with referral to outpatient after-care among attempted suicide patients: a controlled intervention study. Psychol Med. 1995;25:963–70. doi: 10.1017/s0033291700037454. [DOI] [PubMed] [Google Scholar]
- 12.Pfeffer C, Stokes P, Shindledecker R. Suicidal behavior and hypothalamic-pituitary-adrenocortical axis indices in child psychiatric inpatients. Biol Psychiatry. 1991;29:909–17. doi: 10.1016/0006-3223(91)90057-s. [DOI] [PubMed] [Google Scholar]
- 13.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- 15.Eisen SV, Wilcox M, Leff HS, Schaefer E, Culhane MA. Assessing behavioral health outcomes in outpatient programs: reliability and validity of the BASIS-32. J Behav Health Serv Res. 1999;26:5–17. doi: 10.1007/BF02287790. [DOI] [PubMed] [Google Scholar]
- 16.Beck AT, Kovacs M, Weissman A. Assessment of suicide intention, the scale for suicidal ideation. J Consult Clin Psychol. 1979;47:343–52. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 17.Friedman LM, Furberg CD, DeMets DL. Fundamentals of Clinical Trials. 3. New York, NY: Springer Publishing Co; 1998. p. 295. [Google Scholar]
- 18.Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294:563–70. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- 19.Guthrie E, Kapur N, Mackway-Jones K, et al. Randomised controlled trial of brief psychological intervention after deliberate self-poisoning. BMJ. 2001;323:135–7. doi: 10.1136/bmj.323.7305.135. [DOI] [PMC free article] [PubMed] [Google Scholar]