Abstract
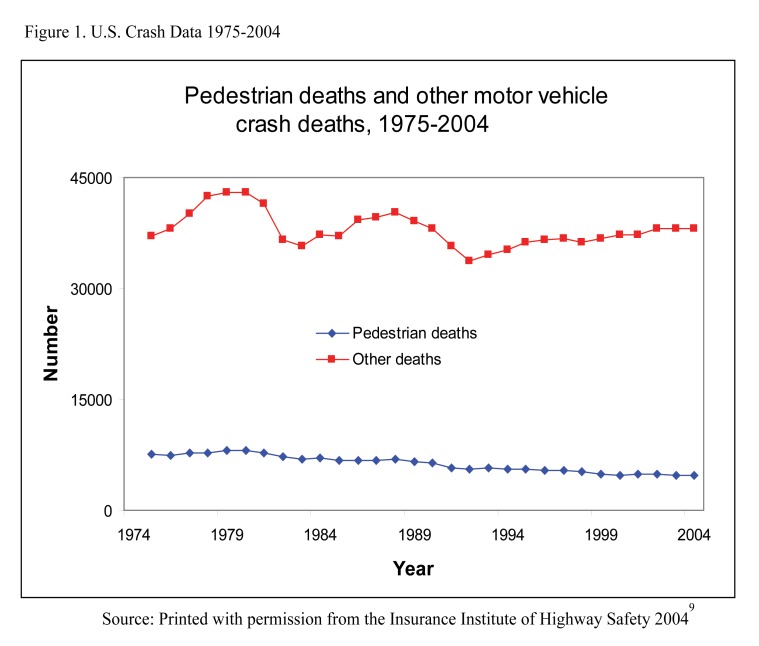
Traffic-related pedestrian injuries are a growing public health threat worldwide. The global economic burden of motor vehicle collisions and pedestrian injuries totals $500 billion.1 In 2004, there were 4,641 pedestrian deaths and over 70,000 injuries in the United States.2 Injury patterns vary depending on the age, gender and socioeconomic status of the individual. Children, older adults, and those of lower socioeconomic status are most affected. The burden of injury upon the individual, families and society is frequently overwhelming. Although pedestrian injuries and deaths are relatively on the decline in the United States, this is not universally true throughout the world. It requires particular attention by emergency medicine physicians, public health experts and policy makers.
Keywords: pedestrian injury, motor vehicle, public health
INTRODUCTION
All-Too-Common Fatal Scenarios
A hurried mother backs out of her suburban neighborhood driveway in an effort to get to work on time but fails to realize that her three-year-old son slipped out of the front door and stands directly behind her car in an innocent game of hide-and-seek. An elderly gentleman using a cane at the crosswalk cannot avoid the oncoming speeding vehicle. A college student pulls away from the curb after having a few drinks and overlooks the pizza delivery girl on her bicycle. In developing nations, villagers transporting food and water on foot to their homes share a narrow causeway with large trucks. These are but a few of the common examples of why pedestrian motor-vehicle collisions are prevalent in the United States and the world.
Pedestrian injuries are a growing concern for public health care professionals and the health care industry in the United States (U.S.) and worldwide. In 2004 the National Highway Traffic Safety Administration (NHTSA) reported over 70,000 pedestrian injuries and 4,641 pedestrian deaths due to traffic-related injuries.2 It is estimated that a pedestrian is killed in a traffic crash every 113 minutes and injured every eight minutes. Among those particularly vulnerable are children, the elderly, and those of lower socioeconomic status. From a global perspective, this public health concern is more evident in developing nations. The World Health Organization (WHO) reports that road-traffic injuries are a major but neglected public health threat, with an estimated 1.2 million killed and 50 million people injured worldwide.1 Not surprisingly, a substantial percentage of these road-traffic injuries and deaths are pedestrians, in some countries accounting for 40% of the fatalities.3
U.S. BURDEN OF INJURY
The annual global economic burden of motor vehicle collisions and pedestrian injuries is enormous, totaling 500 billion dollars.4 In the year 2000, the total cost of all motor vehicle collisions in the United States was 230.6 billion dollars. Lost productivity, medical costs, legal and court costs, emergency services, insurance administration, travel delay, property damage and workplace losses are all included in these costs.5 Travel delay costs and property damage costs from pedestrian collisions are a smaller fraction of the total attributable burden in pedestrian- related collisions. Losses in workplace and household productivity accounted for over one-third of the total costs in the U.S. The implications for such difficult-to-measure consequences as pain, suffering, disability and family cohesiveness are perhaps more important in determining the net cost of pedestrian injuries and mortality on society. These may include such chronic psychiatric conditions as post-traumatic stress disorder and major depressive episode.6,7
RISK FACTORS FOR PEDESTRIAN COLLISIONS
It is important to analyze the risk factors of pedestrian injuries so that successful targeting and interventional programs can be implemented. Two primary factors are when and where pedestrian collisions occur. National data indicate that most fatalities occur between the hours of 6 pm and midnight.2 Impaired vision among drivers due to the lack of daylight, coupled with pedestrian traffic and alcohol consumption by either the driver or the pedestrian, are plausible explanations for the higher incidence of pedestrian collisions after dark. Nearly 40% of all pedestrian fatalities involve pedestrian intoxication. In 18% of fatal pedestrian collisions, the drivers had consumed alcohol.2 As this is a preventable risk factor, it lends further support to the strict enforcement of laws designed to regulate a driver’s alcohol and drug consumption,. Two-thirds of pedestrian fatalities occur in urban areas and three-fourths occur in non-intersections.8 Urban areas have a higher rate of pedestrian and motor vehicle traffic. Drivers non-compliant with speed limitations, pedestrian lack of safety awareness, poor city planning and other variables all lead to a higher incidence of pedestrian collisions in urban centers. Rural areas pose their own unique, significant risks. Although the overall number of collisions is fewer than in urban centers, pedestrian injuries are more severe and are fatal a greater percentage of times in rural settings.8 Higher vehicle speeds, lack of proper pedestrian walkways and larger distances to a trauma center likely contribute to a higher mortality rate.
AGE AS A RISK FACTOR
Children, older adults and those of lower socioeconomic status are most vulnerable to being struck by a motor vehicle. Children, impulsive in nature and without the integrated sensory and cognitive skills, may lack the judgment to avoid oncoming traffic. At the same time, adults tending to children are likely to over-estimate the child’s ambulatory ability. Risky driving behaviors, such as driving while intoxicated or speeding, childhood impulsivity and poor parental supervision frequently occur simultaneously when there is a pediatric pedestrian collision.
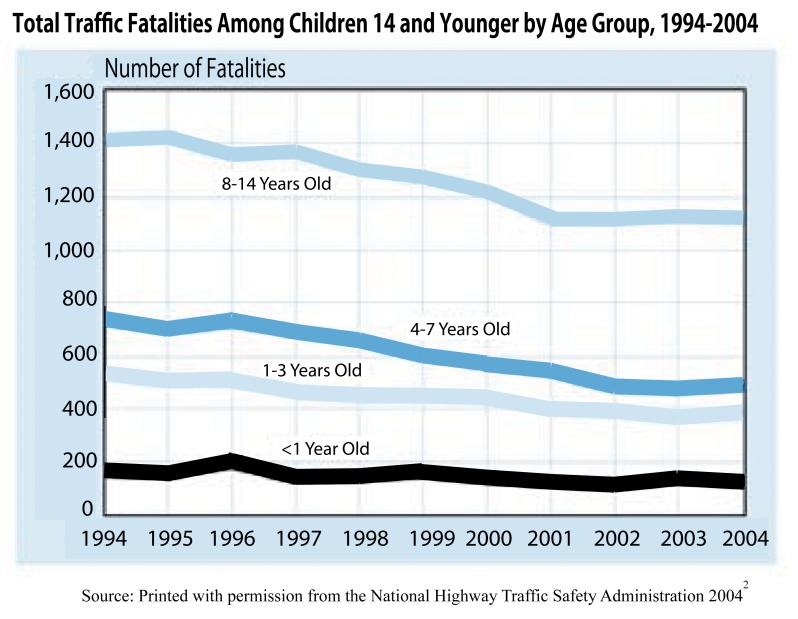
Children younger than 16 are most likely to be struck by motor vehicles. Pedestrians in the 10–15 age group have the highest non-fatal injury rates in the United States. Children under the age of 15 account for 30% of a l l pedestrian injuries in the U.S.; of those injured, 17,000 were age 14 and younger, with males accounting for 58% (10,000).2 Pedestrian collisions remain the second leading cause of unintentional, injury-related death among children in the 5–14 age group.10 Children under the age of 15 account for 8% of all pedestrian deaths; 63% of these pediatric fatalities in children less than 14 years of age are males.
Older adult pedestrians, those 65 years and older, have their own limitations that make them susceptible to collisions. As adults age, gradual losses in hearing, vision, reflexes and flexibility put them at risk for pedestrian collisions. Furthermore, once the older adult pedestrian is struck, their co-morbid conditions and limited physical reserves contribute to a higher percentage of death and disability when compared to the rest of the population. Older adults make up 12% of the U.S. population, yet they account for 23% of all hospitalizations for traumatic injuries.11 Compared to younger patients, older adults for any given injury experience longer hospitalization, more complications, and higher mortality rates.12,13 The same results hold true for older-adult pedestrian injuries, accounting for over a 20% overall mortality rate and an increased incidence of both severe and critical trauma.14,15 Risky behaviors are noticeably absent in older adult pedestrians who are injured. Senior pedestrian collisions occur more often during daylight hours, at the end of blocks rather than mid-block, and rarely involve pedestrian intoxication.8 While older adults account for a lower number of pedestrian injuries (7%), they account for a greater percentage of pedestrian casualties (16%), despite their commendable safety practices.2 Because of more limited biophysical reserves, older adults are more frequently severely injured or killed.
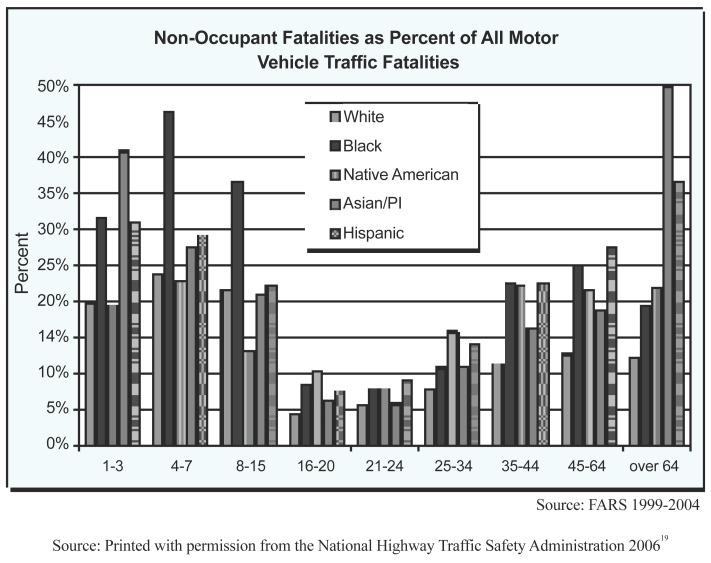
SOCIAL STATUS
Pedestrian injuries affect all people, but they have a greater negative impact on those of lower socioeconomic standing (SES). While it is notably difficult to comprehensively define SES, several studies commonly utilize proxies for SES, such as economically disadvantaged, limited education and social support. Several studies have shown that people from these backgrounds are affected a greater percentage of times, have fewer social supports in place, and use emergency services less frequently.16–18 They are also most likely to be the main income providers in their families, and their death or disability creates a greater financial burden on an already economically strained situation. Race and ethnicity also play a large role in pedestrian injuries and fatalities. Recent national data indicate that all minorities of all age groups are more likely to be involved in a fatal non-occupant collision than the non-Hispanic Caucasian population. This comparison holds true for all minorities, except for Native American children less than 15 years old.19 African-American children in the 4–7 age group accounted for 47% of pedestrian traffic fatalities and 37% in the 8–15 age group.19 Regardless of an urban or rural location, African-American children were killed in disproportionate numbers in these two age groups.
The over-representation in pedestrian injuries among those from lower SES is not completely understood. Many experts suggest that individuals from a lower SES may engage in more risky behavior and be less likely to be aware of public safety issues. Lower-income families are also likely to have less supervision for their children as they may not have the resources to provide adequate daycare while at work. Cultural-related attitudes and perceptions concerning safety and public health, access to health care, and limitations in their exposure to health promotion also may also prove to be important reasons for the increased incidence of pedestrian injuries in the United States. While pedestrians of low SES from developing countries experience the same limitations as their U.S. counterparts, they encounter the added danger of sharing the roadway with large vehicles whose drivers have few or no motor-vehicle regulations imposed on them.20,21
INJURY PATTERNS
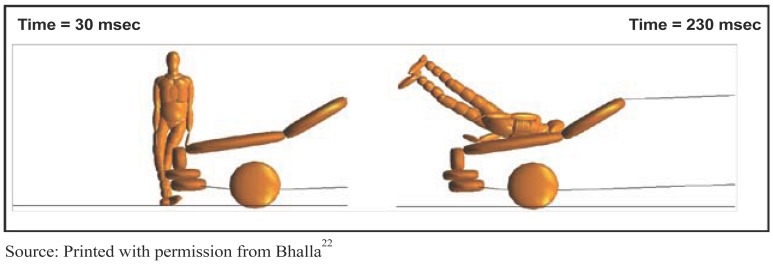
Frontal collisions are categorized by the height of the impact relative to the location of the pedestrian’s center of gravity. Most adult vehicle collisions occur when the center of gravity is above the upper front edge (bumper) of the oncoming vehicle, whereas in pediatric pedestrian collisions the center of gravity is often below the bumper. In adult collisions, the front bumper strikes the lower leg region. The legs are accelerated in the direction of vehicle travel, while the upper body and head are brought into contact with the hood and/or windshield. Therefore, there are three distinct impacts. The first is between the lower leg and the bumper. This is immediately followed by contact between the thigh area and the upper edge of the hood. These impacts cause rotation of the upper body, resulting in another impact between the head/shoulders and the hood/windshield region. At low speeds, the pedestrian remains on the hood. At higher speeds, the increased momentum causes the legs to rotate above the head before falling back onto the hood. At even higher impact speeds, the pedestrian somersaults onto the windshield/roof after head impact. Further increases in impact speed can cause the pedestrian to pass fully over the vehicle. This leads to subsequent impacts with the ground and other roadway objects as the pedestrian slides/rolls/bounces to rest.
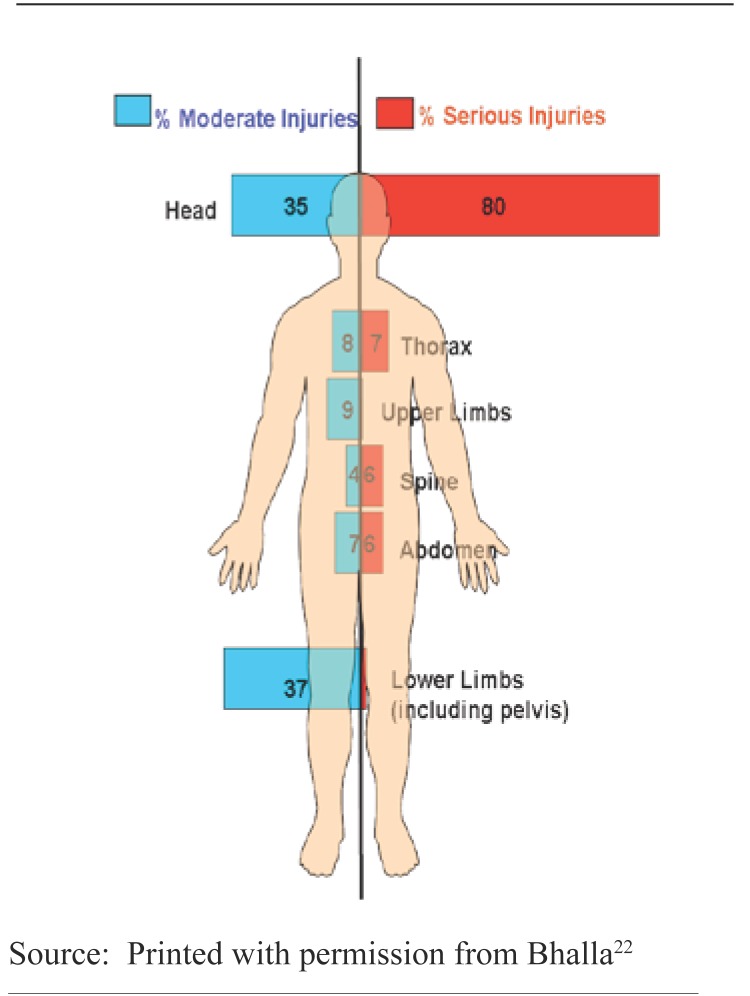
The severity of the injuries is related to many factors, including vehicle speed, the angle of impact of the vehicle upon the pedestrian, the center of gravity of the pedestrian, the part of the body that first comes into contact with the vehicle, the part of the vehicle the pedestrian impacts first, and the vehicle design. Most injuries arising from these vehicle and ground impacts in adults are trauma to the head, legs and pelvis., tibial plateau fractures and ligamentous injuries of the knee, as well as traumatic brain injuries, are all common.23 One study showed that the most common injuries seen in children, aside from superficial injuries, involved the head and neck (34.6%), with musculoskeletal injuries the second most common (22.2%). In contrast, the same study found that among adults, musculoskeletal injuries (41.4%) were more common than head and neck injuries (26.7%). The statistical trend of musculoskeletal injuries being more common than head and neck injuries also remained consistent in a sub-analysis in older-adult pedestrian collision victims.24 Most pediatric pedestrian collisions that involved traumatic brain injury did not involve cervical injuries. Regardless of this fact, a review of one database showed that pediatric C-spine dislocations most commonly result from pedestrian collisions.25 The most common injuries seen in pediatric pedestrian collisions tend to be traumatic brain injuries and musculoskeletal injuries, followed by chest and abdominal injuries. In musculoskeletal injuries the upper and lower legs and knees are most frequently injured, which can lead to long-term disabilities. Head injuries are generally more life threatening.
EMERGENCY CARE CONSIDERATIONS
The post-crash emergency medicine implication of the collision begins in the pre-hospital phase. The geographic distance of the collision from a designated trauma center is crucial to the overall success of the evaluation and resuscitation of the pedestrian victim. The farther the collision is from a trauma center the worse the outcome will be for the pedestrian. Access to Emergency Medical Services (EMS) varies in the U.S. and to a much greater degree in developing nations. Those who live in a rural setting and suffer severe injuries are more likely to succumb from them before arriving at a hospital. Most deaths from road-traffic injuries occur prior to hospital arrival regardless of the socioeconomic level of the nation. Those countries with a lower SES had higher pre-hospital death rates – 51% in a developing nation compared to 21% in the U.S., which Mock et al attributed to the increased time to arrival to a designated trauma center.26 Decreased transit times and improvements in prehospital EMS systems, with incorporated protocols, can improve outcomes.27
Timely arrival at a trauma center is crucial, as is the initial stabilization and rapid evaluation of the injured pedestrian. The unique injury patterns manifested in pedestrian collisions require a level of expertise available only in a trauma center. Several studies in industrialized nations show that direct transport to a Level I trauma center in moderate and severe injuries, using the Injury Severity Index (ISS), helped reduce mortality rates.28–30 Furthermore, transferring severely injured trauma patients at a Level III trauma center to a Level I trauma center also reduced mortality rates.31
The importance of the implementation and standardization of the American College of Surgeons’ Advanced Trauma Life Support (ATLS) guidelines is germane to improving the morbidity and mortality of these victims. Implementing these guidelines has proven effective in improving survival.32 While ATLS guidelines were developed so that a single caregiver could sequentially care for the multi-trauma victim, ideally the guidelines should be used with a horizontal organization, with each member of the trauma team designated to specific tasks done in a simultaneous manner. This organization is shown to lead to significant reductions in resuscitation times.33 The aim of the trauma team is to provide a safe and efficient evaluation of the patient, identify all injuries, and instigate definitive management of such injuries. Major pedestrian trauma resuscitations should accomplish stabilization and diagnosis of life-threatening injuries within 30 minutes of arrival to the hospital. Because most hospitals cannot afford this costly level of coverage, appropriate pre-hospital triage systems become invaluable in distributing patients to the appropriate level of care.
As with any trauma resuscitation, the team should begin with the ABCs. Assessing the patient’s airway, breathing and circulation is always included in the primary survey of the multi-trauma victim. Since pedestrian injuries often involve traumatic brain injuries and the potential for cervical spine trauma, careful consideration must be taken when manipulating the patient with regard to airway management. In-line cervical stabilization is required when intubating patients, and an evaluation for pneumothorax and hemothorax should take place simultaneously. Even slow to moderate-speed pedestrian collisions can cause intra-thoracic, intra-abdominal, pelvic and long bone injuries. All of these can be major sources of hemorrhage, requiring immediate assessment and intervention. Life-saving measures such as endotracheal intubations, thoracostomies and blood administration may be necessary for the initial stabilization of the patient. The Focused Assessment with Sonography for Trauma (FAST) exam, with or without other modalities such as DPL and CT scan, is essential in evaluating abdominal injuries. A low threshold for the use of diagnostic modalities, such as CT, should be kept in mind when evaluating pedestrian traumas. Often, surgical intervention is required and should not be delayed. If time allows, a thorough secondary survey should include a head-to-toe evaluation for serious and subtle injuries. Any signs of tachycardia, tachypnea and hypotension should not be disregarded.
Pedestrian traumas are usually multi-trauma victims who can pose significant challenges. More often than not, the pedestrian patient is unable to recall the events leading up to the collision, and witnesses are either unavailable or grossly misrepresent the speed and direction of the collision. The trauma team should err on the side of caution in the disposition of these complicated patients.
INTERVENTION AND INJURY PREVENTION PROGRAMS
Recognition and rapid treatment of life-threatening injuries is not sufficient. A holistic approach to the epidemic of trauma should look beyond the post-crash event and include both the pre-crash and crash events in an effort to minimize the disease burden to society.
Interventions can be applied to the established Haddon matrix for motor vehicle collisions.34 Three intertwined factors – human, vehicle and environment – are subject to three distinct phases of the event: pre-crash, crash and post-crash. Each of these individual elements allows opportunities for intervention to reduce road-crash injury. Haddon, with his systematic approach to motor vehicle collisions, sought to identify and rectify the major sources of error or design weakness that contribute to fatal and severe injury crashes, as well as to mitigate the severity and consequences of injury. By reducing exposure to risk, preventing road traffic crashes from occurring, reducing the severity of injury in the event of a crash and reducing the consequences of injury through improved post-collision care, Haddon thought to decrease the disease burden of pedestrian collisions. While evidence from highly motorized countries shows that Haddon’s integrated approach to road safety produces a marked decline in road deaths and serious injuries,35, 36 the practical realization of this systems approach remains the most important challenge for road-safety policy makers and professionals.
Pedestrian educational measures and programs play an integral part in reducing the incidence of this preventable death. Numerous studies and programs are in place to curtail pedestrian injuries, but few are well implemented or survive the scrutiny of evidence-based medicine. A 2002 Cochrane review looked at thousands of studies but selected only15 randomized control trials to review, 14 of which were pediatric interventions. In all of these studies the methodological quality of the data is in question and most had large number of patients lost to follow-up. The poor quality of the data aside, the reviewers surmised that while educational intervention programs are helpful and that periodic re-education is necessary to elicit improvements in observed behavior, improvement in observed behavior alone has not been proven to reduce the risk of pedestrian injuries.37 Another possible intervention is to provide safer, more direct routes for pedestrian traffic. Pedestrians are twice as likely to be struck by a motor vehicle when the pedestrian route is not separated from the vehicular route. Providing safe routes for pedestrians can limit their exposure to motor-vehicle traffic.38 Incentives for safe and affordable use of public transportation, such as railway and bus routes, can limit risk exposure. Disincentives, such as levying taxes on gasoline, although highly unpopular, could incline drivers to make fewer trips and to use public transportation more often.
In conjunction with programs that intervene in pedestrian behavioral patterns, ones that affect both driver attitudes and local environmental conditions play a significant role in reducing the risk posed to pedestrians. Stricter laws on driving under the influence of alcohol and drugs have proven effective in reducing both motor-vehicle collisions and collisions involving pedestrians. Traffic-calming measures that incorporate speed limitations, color displays and signs of pedestrian traffic, as well as visual displays of crosswalks (“zebra-ing” x-walks), have also been successful in reducing the incidence of pedestrian injuries and fatalities in specific locations.
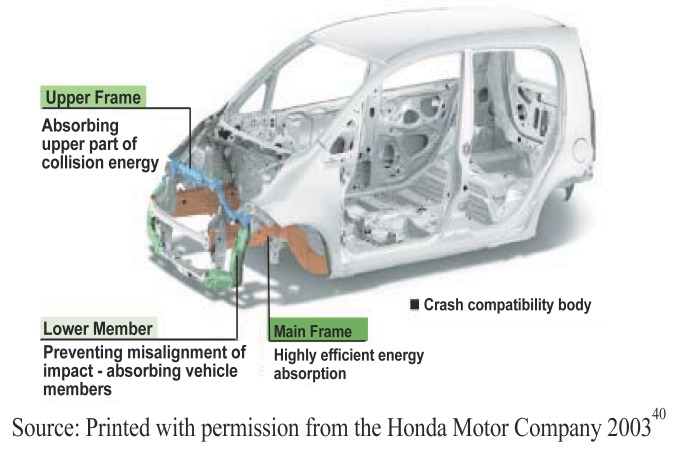
Technological advances by car manufacturers continue to help reduce the severity of injuries sustained during the crash. In an effort to reduce the impact energy transmitted to the pedestrian, car manufacturers have begun to implement pedestrian-safe technologies, such as more compliant front bumpers, greater clearance from the top of the hood to the underlying engine block, crumple zones of the main frame of the vehicle, and breakaway windshield wipers. The focus now is to make crashes more survivable by dispersing the mechanical energy of the crash over time and space, which in turn reduces the impact of the collision on the pedestrian. In the past vehicles in the U.S. commonly used metal or chrome front bumpers that had little or no malleability and transmitted all the energy of the vehicle onto the pedestrian in a collision, causing fatal injuries. Currently in the U.S. front bumpers are made of synthetic materials. Ongoing automotive research holds the promise of even safer technology. Increasing the visibility of both pedestrians and motor vehicles by the use of already established technologies, such as daytime traffic lights and reflective pedestrian clothing, can further reduce the disease burden of pedestrian collisions.39 Future pedestrian-friendly automotive technology may include night vision or infrared systems to minimize collisions in non-daylight hours. Although the automotive industry is aware of the burden of disease that collisions represent, it has been slow in implementing change that would be beneficial to the pedestrians and public health.
CONCLUSIONS
Road-traffic pedestrian injuries are a significant public health concern, annually killing over 4,000 people in the U.S. and almost 1.2 million worldwide. The magnitude of non-fatal injuries is staggering, with over 60,000 people injured in the U.S. and between 20 million and 50 million worldwide.1,2 Data indicate that these injuries will rise dramatically by the year 2020, particularly in countries that are rapidly motorizing.
Health-care providers in emergency medicine are in a unique position in that they witness daily the tragic outcomes of trauma and injury sustained by patients. The injury patterns manifested in pedestrian collisions are unique and require a level of expertise seen only in a trauma center. It is the responsibility of emergency medicine physicians to be hypervigilant with regard to occult, life-threatening injuries where a rapid assessment and diagnosis can prevent severe morbidity and death. The emergency physician’s responsibility should go beyond immediate patient treatment to focus as well on a holistic approach to this growing epidemic. Because pedestrian motor-vehicle collisions are predictable they can be prevented. Future research and implementation of strategic education and technological programs can reduce the risk exposure to those populations most at risk: children, older adults, and those of lower socio-economic status. Advocacy for pedestrian safety can involve health-policy issues at the local, regional or legislative level. No one is better suited to provide health-policy reform than the emergency medicine physician, through personal testimony and expert opinion supported by research. A multi-pronged approach to this major public health issue would do much to minimize the effects of pedestrian motor vehicle injuries.
Figure 1.
U.S. Crash Data 1975–2004
Figure 2.
Pediatric Pedestrian Fatalities 1994–2004
Figure 3.
Ethnic Make-up of Non-Occupant Fatalities 1999–2004
Figure 4.
Impact Sequence of Adult Pedestrian Collision
Figure 5.
Adult Pedestrian Injury Profile
Figure 6.
Vehicle Technology Reducing Pedestrian Injuries
TABLE 1.
Change in rank order of DALYs for the 10 leading causes of the global burden of disease
| Rank | 1990 Disease or injury | Rank | 2020 Disease or injury |
|---|---|---|---|
| 1 | Lower respiratory infections | 1 | Ischaemic heart disease |
| 2 | Diarrhoeal diseases | 2 | Unipolar major depression |
| 3 | Perinatal conditions | 3 | Road traffic injuries |
| 4 | Unipolar major depression | 4 | Cerebrovascular disease |
| 5 | Ischaemic heart disease | 5 | Chronic obstructive pulmonary disease |
| 6 | Cerebrovascular disease | 6 | Lower respiratory infections |
| 7 | Tuberculosis | 7 | Tuberculosis |
| 8 | Measles | 8 | War |
| 9 | Road traffic injuries | 9 | Diarrhoeal diseases |
| 10 | Congenital abnormalities | 10 | HIV |
DALY: Disability-adjusted life year. A health-gap measure that combines information on the number of years lost from premature death with the loss of health from disability.
Source: Printed with permission from the World Health Organization 20041
REFERENCES
- 1.Peden M. World Report on Road Traffic Injury Prevention: Summary. World Health Organization. 2004 [Google Scholar]
- 2.Traffic Safety Facts 2004:Pedestrians. National Highway and Transportation Safety Administration. 2004 [Google Scholar]
- 3.Mohan D. Traffic safety and health in Indian cities. Journal of Transport and Infrastructure. 2002;9:79–92. [Google Scholar]
- 4.Koppits E, Cropper M. Traffic Fatalities and Economic Growth. The World Bank. 2003 doi: 10.1016/j.aap.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Blincoe L, Seay A, Zaloshnja E. The Economic Impact of Motor Vehicle Crashes, 2000. National Highway Traffic Safety Administration. 2002 [Google Scholar]
- 6.Holbrook TL, Hoyt DB, Coimbra R, Potenza B, Sise M, Anderson JP.Long-term posttraumatic stress disorder persists after major trauma in adolescents: New data on risk factors and functional outcome Journal of Trauma 2005584764–9.discussion 9–71. [DOI] [PubMed] [Google Scholar]
- 7.Frommberger UH, Stieglitz RD, Nyberg E, Schlickewei W, Kuner E, Berger M. Prediction of posttraumatic stress disorder by immediate reactions to trauma:A prospective study in road traffic accident victims. European Arch Psychiatry Clinical Neuroscience. 1998;248(6):316–21. doi: 10.1007/s004060050057. [DOI] [PubMed] [Google Scholar]
- 8.Shankar U. Pedestrian Roadway Fatalities. National Highway Traffic Safety Administration. 2003 [Google Scholar]
- 9.Fatality Facts 2004:Pedestrians. Insurance Institute for Highway Safety. 2004 [Google Scholar]
- 10.Web-based Injury Statistics Query and Reporting System (WISQARS) Centers for Disease Control; National Center for Injury Prevention and Control. 2003.
- 11.MacKenzie EJ, Morris JA, Jr, Smith GS, Fahey M.Acute hospital costs of trauma in the United States: Implications for regionalized systems of care Journal of Trauma 19903091096–101.discussion 101–3. [DOI] [PubMed] [Google Scholar]
- 12.McKevitt EC, Calvert E, Ng A, et al. Geriatric trauma: Resource use and patient outcomes. Canadian Journal of Surgery. 2003;46(3):211–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. Journal of Trauma. 1998;45(4):805–10. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 14.Small TJ, Sheedy JM, Grabs AJ. Cost, demographics and injury profile of adult pedestrian trauma in inner Sydney. ANZ Journal of Surgery. 2006;76(1–2):43–7. doi: 10.1111/j.1445-2197.2006.03646.x. [DOI] [PubMed] [Google Scholar]
- 15.Demetriades D, Gkiokas G, Velmahos GC, Brown C, Murray J, Noguchi T. Alcohol and illicit drugs in traumatic deaths: prevalence and association with type and severity of injuries. Journal of the American College of Surgery. 2004;199(5):687–92. doi: 10.1016/j.jamcollsurg.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 16.Nantulya VM, Reich MR. Equity dimensions of road traffic injuries in low- and middle-income countries. Injury Control Safety Promotion. 2003;10(1–2):13–20. doi: 10.1076/icsp.10.1.13.14116. [DOI] [PubMed] [Google Scholar]
- 17.Laflamme L, Diderichsen F. Social differences in traffic injury risks in childhood and youth--a literature review and a research agenda. Injury Prevention. 2000;6(4):293–8. doi: 10.1136/ip.6.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mock CN, nii-Amon-Kotei D, Maier RV.Low utilization of formal medical services by injured persons in a developing nation: Health service data underestimate the importance of trauma Journal of Trauma 1997423504–11.discussion 11–3. [DOI] [PubMed] [Google Scholar]
- 19.Hilton J. Race and Ethnicity Factors in Fatal Motor Vehicle Traffic Crashes 1999–2004. National Highway Traffic Safety Administration. 2006.
- 20.Evans T, Brown H. Road traffic crashes: Operationalizing equity in the context of health sector reform. Injury Control Safety Promotion. 2003;10(1–2):11–2. doi: 10.1076/icsp.10.1.11.14117. [DOI] [PubMed] [Google Scholar]
- 21.Odero W, Khayesi M, Heda PM. Road traffic injuries in Kenya: Magnitude, causes and status of intervention. Injury Control Safety Promotion. 2003;10(1–2):53–61. doi: 10.1076/icsp.10.1.53.14103. [DOI] [PubMed] [Google Scholar]
- 22.Bhalla K. Pedestrian Safety Through Vehicle Design. Wikipedia. 2006 [Google Scholar]
- 23.Grande CM, Stene JK, Barton CR. The trauma anesthesiologist. Md Med J. 1988;37(7):531–6. [PubMed] [Google Scholar]
- 24.Peng RY, Bongard FS. Pedestrian versus motor vehicle accidents: An analysis of 5,000 patients. Journal of the American College of Surgery. 1999;189(4):343–8. doi: 10.1016/s1072-7515(99)00166-0. [DOI] [PubMed] [Google Scholar]
- 25.Brown RL, Brunn MA, Garcia VF. Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg. 2001;36(8):1107–14. doi: 10.1053/jpsu.2001.25665. [DOI] [PubMed] [Google Scholar]
- 26.Mock CN, Jurkovich GJ, nii-Amon-Kotei D, Arreola-Risa C, Maier RV.Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development J Trauma 1998445804–12.discussion 12–4. [DOI] [PubMed] [Google Scholar]
- 27.Husum H, Gilbert M, Wisborg T, Van Heng Y, Murad M. Rural prehospital trauma systems improve trauma outcome in low-income countries: a prospective study from North Iraq and Cambodia. J Trauma. 2003;54(6):1188–96. doi: 10.1097/01.TA.0000073609.12530.19. [DOI] [PubMed] [Google Scholar]
- 28.Hartl R, Gerber LM, Iacono L, Ni Q, Lyons K, Ghajar J.Direct transport within an organized state trauma system reduces mortality in patients with severe traumatic brain injury J Trauma 20066061250–6.discussion 6. [DOI] [PubMed] [Google Scholar]
- 29.Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process-outcome evaluation J Trauma 1999464565–79.discussion 79–81. [DOI] [PubMed] [Google Scholar]
- 30.Sampalis JS, Denis R, Frechette P, Brown R, Fleiszer D, Mulder D.Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma J Trauma 1997432288–95.discussion 95–6. [DOI] [PubMed] [Google Scholar]
- 31.Hedges JR, Adams AL, Gunnels MD. ATLS practices and survival at rural level III trauma hospitals, 1995–1999. Prehosp Emerg Care. 2002;6(3):299–305. doi: 10.1080/10903120290938337. [DOI] [PubMed] [Google Scholar]
- 32.Ali J, Adam R, Butler AK, et al. Trauma outcome improves following the advanced trauma life support program in a developing country J Trauma 1993346890–8.discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 33.Collicott PE, Hughes I. Training in advanced trauma life support. JAMA. 1980;243(11):1156–9. [PubMed] [Google Scholar]
- 34.Haddon W., Jr The changing approach to the epidemiology, prevention, and amelioration of trauma: the transition to approaches etiologically rather than descriptively based. Am J Public Health Nations Health. 1968;58(8):1431–8. doi: 10.2105/ajph.58.8.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Motor-vehicle safety: a 20th century public health achievement. MMWR Morb Mortal Wkly Rep. 1999;48(18):369–74. [PubMed] [Google Scholar]
- 36.Trinca GW. Road trauma prevention: perspectives. World J Surg. 1992;16(3):370–3. doi: 10.1007/BF02104433. [DOI] [PubMed] [Google Scholar]
- 37.Duperrex O, Roberts I, Bunn F. Safety education of pedestrians for injury prevention. Cochrane Database Syst Rev. 2002;(2):CD001531. doi: 10.1002/14651858.CD001531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ossenbruggen PJ, Pendharkar J, Ivan J. Roadway safety in rural and small urbanized areas. Accid Anal Prev. 2001;33(4):485–98. doi: 10.1016/s0001-4575(00)00062-2. [DOI] [PubMed] [Google Scholar]
- 39.Elvik R. A meta-analysis of studies concerning the safety effects of daytime running lights on cars. Accid Anal Prev. 1996;28(6):685–94. doi: 10.1016/s0001-4575(96)00041-3. [DOI] [PubMed] [Google Scholar]
- 40.Fact Book: Safety Technologies. Honda Motor Company, 2003. (Accessed at http://world.honda.com/factbook/auto/motorshow/200310/10.html.)