Abstract
Aims
Atrial fibrillation (AF) is not always perceived as a serious health threat, but is the most common sustained arrhythmia, with a major impact on morbidity, mortality, and patient quality of life (QoL). A survey was undertaken to examine the level of understanding, perception, and attitudes of the cardiovascular risks associated with AF.
Methods and results
The AF AWARE group (an international coalition of organizations with an interest in AF) conducted an international quantitative survey in 11 countries in 2009, to investigate patients' (n = 825) and cardiologists' (n = 810) perceptions of AF, preferences for communicating information on AF and burden of AF. Both patients and physicians considered AF life-threatening (55 and 43%, respectively). Physicians were more concerned about the risk of stroke and hospitalizations than patients, whereas patients were most concerned about death risk. One in four patients felt unable to explain AF and >33% were worried or fearful about their disease. Many physicians (51%) wanted more patient information with >60% viewing available information as poor/difficult to find. Hospital specialists and GPs were identified as key information sources for patients. Most patients (83%) reported symptoms, yet 75% claimed to be satisfied with AF therapies. Atrial fibrillation patients, often with associated diseases, made an average of nine visits per year to their doctors, who consider AF difficult and time consuming to manage. Patients and physicians rated the QoL impact of AF as moderate to high.
Conclusions
A comprehensive international patient and professional information and support programme on AF is needed to improve management and consequently health outcomes.
Keywords: Atrial fibrillation, Perceptions, Patient, Physician, Survey
Introduction
Atrial fibrillation (AF) is the most common sustained heart rhythm disorder and a condition associated with high mortality and morbidity.1–5 The condition has been described as epidemic in proportion, with AF prevalence predicted to triple by 2050.6,7 The lifetime risks for development of AF are one in four for people over the age of 40 years.8
Whether silent or symptomatic, AF is typically a progressive condition, worsening over time.9 It is associated with an increased mortality risk, as well as an increased risk of developing congestive heart failure and serious thrombo-embolic events.1,5,10–12 Indeed, the mortality rate of patients with AF is approximately double that of patients with normal sinus rhythm. Atrial fibrillation has been shown to increase the risk of ischaemic stroke up to five-fold,1,11 and such strokes tend to be more severe than strokes linked with other causes.13,14 There is also a close relationship between AF and heart failure, which is associated with poor prognosis, in which AF aggravates heart failure, which in turn promotes AF.2 The presence of AF in patients with other co-morbid cardiovascular (CV) diseases worsens prognosis and contributes to the risk of sudden death.15,16 Atrial fibrillation is also associated with substantial healthcare costs, and adding to the health–economic burden posed by AF is evidence that the condition has a negative impact on patients' daily living activities and quality of life (QoL).17–20
Nonetheless, there are concerns that AF is not perceived as a serious health threat. This condition can be overlooked by the medical community, who fail to accept AF as a readily modifiable risk factor for CV morbidity and mortality.21–23 Patients also have limited awareness and poor perception of the broader risks associated with a diagnosis of AF.24,25
To better understand physicians' and patients' knowledge, perceptions, and attitudes to AF and its contribution to CV morbidity and mortality, a survey incorporating physician and patient questionnaires was conducted in association with the AF AWARE group (Atrial Fibrillation AWareness And Risk Education)—a collaborative activity between the World Heart Federation (WHF), the Stroke Alliance for Europe (SAFE), the Atrial Fibrillation Association (AFA), and the European Heart Rhythm Association (EHRA). This article reports the findings of this survey, with the aim of identifying potential gaps between the realities of AF and the perception of AF as a public health concern that may be addressed through improved educational intervention.
Methods
Members of the AF AWARE group provided input into the development of and the interpretation of results, from an international quantitative survey. The survey comprised two questionnaires; one of the questionnaires focused on obtaining responses from patients with AF, and the other addressed physicians active in the management of AF. Through parallel and complementary questionnaires, the survey sought information on respondents' (physician and patient) level of understanding of AF and AF risk, perception of AF relative to other medical conditions, practices and preferences for communicating information on AF, and the burden and QoL impact of AF. The aim of the survey was to assess the level of understanding of AF and identify differences, gaps, misconceptions, and shortcomings in both physicians' and patients' perception of AF as a serious CV disease. The survey was undertaken between February and April 2009, and the results were reviewed and interpreted by members of the AF AWARE group.
Random sampling and recruitment
The physician survey aimed to recruit a total of 810 physicians (cardiologists/electrophysiologists) under the age of 60 years. A cut-off age of 60 years was used to ensure that all physicians surveyed were below retirement age and still in clinical practice. The physician group comprised representatives from 11 countries (USA, Canada, Mexico, Brazil, UK, France, Germany, Spain, Italy, China, and Australia). These countries were chosen to provide a representative global spread of viewpoints. Recruitment aimed at about 75 physicians per country (except Australia, which aimed to recruit about 60 since the total national population and therefore the potential pool of cardiology professionals is smaller than that for other larger countries).
The majority of physicians who took part in the survey were sampled by random selection from existing physician panel databases (databases of physicians who have agreed to take part in market research) (68%) and accessed by the Taylor Nelson Sofres (TNS) Healthcare group. In order to achieve the required level of physician recruitment per country, there was a need for TNS to source a further 32% of physicians via public and private databases listing cardiologists. The panel database:public/private database share for each participating country therefore differed: Mexico 40:60%; Canada 50:50%; Brazil 80:20%; UK, USA, France, Germany, Spain, and Italy 100:0%; China and Australia 0:100%.
The AF patient sample was selected through a number of routes including patient panels (databases of patients who have agreed to be contacted for potential participation in market research studies), patient-support organizations, and via physician recommendations. Physicians could not select (only suggest) patients to take part in the survey, and the patient and physician surveys were performed entirely independently so that there was no physician influence on patient recruitment. The majority of patients were recruited from patient panels, and only 2.8% were from patient-support groups. In common with the physician survey, the patient group recruited comprised patients (825) drawn from 11 countries (75 per country; countries as per physician survey). Consent to participate was required from all patients, and some patients declined the invitation or withheld consent. Reasons given for not participating included difficulty in hearing or not feeling comfortable discussing their condition.
For both the physician and patient questionnaires, screening questions were employed to gather demographic data, to exclude patients without a confirmed diagnosis of AF, and to ensure that physicians recruited were directly involved in the management of patients with AF (a minimum of 20 patients with AF managed per month).
Data acquisition
With the exception of Brazil, where 60% of physicians completed the survey by phone and 40% used the on-line questionnaire, 100% of the physicians from the other countries completed the survey on-line. For the patient survey, 43% of patients completed the survey via the Internet as an on-line questionnaire, 40% by structured telephone interview, and 17% through face-to-face interviews. No individual patient data were reported. No direct incentive was offered to physicians or patients to take part in the survey.
Scope of the survey
The scope of the survey and its main questions were reviewed by the AF AWARE group, who subsequently appraised the survey results.
The physician survey of 24 questions (most employing an independent five-point rating scale) sought information on physicians' evaluation of the risks associated with AF and AF treatments relative to other CV diseases/treatments. Views on language used to describe AF, types of communication, and level and adequacy of information currently provided to patients with AF were collated, as well as physicians' perceptions of the level of patient familiarity with AF (risks, management, treatments). The frequency and nature of consultations provided to patients with AF and their satisfaction with AF management, as well as the physicians' perception regarding patient QoL and the health–economic impact of AF, were also part of the scope of the survey.
The patient survey of 26 questions (many employing rating scales) sought information on patients' estimate and rating of the risk of AF relative to other diseases. Level of understanding/familiarity with features of AF, as well as how patients define their preferred sources of, and satisfaction with, information on AF and AF treatments was also determined. Patient views and descriptions of how AF impacts on daily living were sought. To aid patients in comparing AF with other medical conditions, the patient survey also included simple descriptions of comparator diseases. Brief descriptions of AF were also provided for patients who might have been uncertain of the key clinical features of AF.
Statistics
The survey was carried out to gauge opinion and perceptions of AF and its treatment. Many of the questions to physicians solicited their perception of patient viewpoints and understanding. In order to apply a quantitative element to the mixture of viewpoints and perceptions revealed by the survey and to allow comparisons to be made between physician and patient answers to related questions, Student t-tests were used, employed with 95% thresholds of significance, and individual P-values are provided, where appropriate.
Results
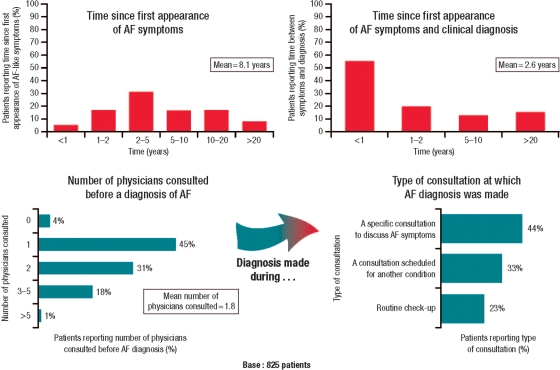
A total of 810 physicians and 825 patients from 11 countries took part in the survey. Key features of the disease profile of patients with AF, including AF diagnostic history, are provided in Figure 1. The survey screening questions on demographics identified that 83% of patients experienced symptoms of AF, with 27% reporting that they had one or more episodes of AF per week. Among the patients surveyed, 20% reported that they had AF as an on-going, long-term episode that did not terminate on medical intervention. More than half of patients described their AF symptoms as moderate (33%) or severe (11%) in answer to screening questions.
Figure 1.
Key features of the history of atrial fibrillation (AF) disease and diagnosis reported by patients.
Perceptions of atrial fibrillation risks and atrial fibrillation management
Physicians and patients had differing perceptions of the threat to health and mortality posed by AF and its relative risk in relation to other medical conditions or risk factors. Atrial fibrillation was considered life-threatening by 43% of physicians and by 55% of patients. Physicians ranked AF as posing a lower threat to life than diabetes, stroke, and heart attack. Patients rated AF as less life-threatening than heart attack, stroke, and hypertension but more life-threatening than diabetes.
Physician and patient beliefs regarding the risk associated with AF and clinical events differed. Physicians were more concerned about the risks of stroke and hospitalizations than patients, whereas patients were more concerned about the risks of death or sudden cardiac death or of a heart attack.
Atrial fibrillation management: understanding and satisfaction
Of the patients surveyed, 88% reported that they were receiving some form of treatment for their AF. Of that group, 75% were receiving anticoagulants, 61% rhythm control therapy, and 46% rate control therapy.
There was a tendency for physicians to underestimate their patients' understanding of the benefits of AF treatments and to overestimate patients' knowledge about treatment complications (Figure 2). Overall, there was a relatively high level of patient knowledge of the benefits of medication and their side effects, and of possible complications of AF. However, patients felt less familiar with more specific issues like the role for electrical cardioversion, ablation of AF, and the development of new medications.
Figure 2.
Patient knowledge about atrial fibrillation (AF) and its management. Physicians' estimates and perceptions of their patients' familiarity with aspects of treatment compared with patients' own familiarity ratings of aspects of atrial fibrillation treatments. Percentage of respondents rating aspects of atrial fibrillation treatment (perceived patient view, actual patient view) as not familiar (scores 1–2), neutral (3), and familiar (4–5), mean score rating, mean score rating difference between physicians and patients.
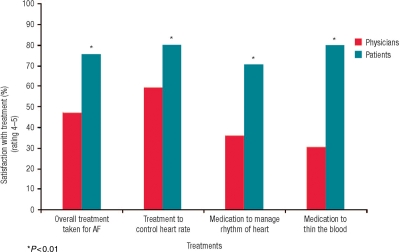
Patient satisfaction with treatment tended to be underestimated by physicians (Figure 3). Physicians' own satisfaction with AF treatments was low relative to other CV medications. In terms of AF treatments and their efficacy and safety profiles, physicians ranked AF treatments lower (at position 6) than therapies used in the management of high cholesterol, hypertension, heart attack, asthma, and diabetes (ranked 1–5, respectively), but above treatments for depression and stroke.
Figure 3.
Patient satisfaction with atrial fibrillation (AF) treatments. Physicians' estimates and perceptions of their patients' satisfaction with atrial fibrillation treatments compared with patients' own satisfaction ratings for atrial fibrillation treatments. Percentage of respondents rating aspects of atrial fibrillation treatment (perceived patient view, actual patient view) as not satisfied (scores 1–2), neutral (3), and satisfied (4–5).
Atrial fibrillation caseload
The survey found that AF patients visit a physician between 8 and 11 times a year. Recurrent episodes of AF that last more than 7 days were associated with the greatest need for physician visits (more than 10 visits per year). A total of 26% of patients said they visited the cardiologist every 6 months, 22% once every 3 months, and 17% every month.
Physicians rated AF as the third most demanding condition (after heart attack and heart failure) and the second most difficult condition (after heart attack) to manage in practice, out of a list of conditions that also included stroke, angina, diabetes, hypertension, high cholesterol, depression, asthma, and cessation of smoking. Only heart failure ranked consistently higher than AF in terms of management difficulty and demands on time. More than one in four physicians felt that AF was either too complicated to explain to patients or that they did not have enough time to fully explain AF in their consultations with patients.
Information and communication
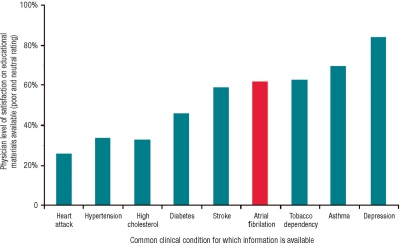
Physician opinion was that the level and quality of information about AF provided to patients compared poorly with levels of information provided on other common clinical conditions, particularly other CV diseases (Figure 4).
Figure 4.
Physician satisfaction with level of information and educational materials provided to patients with atrial fibrillation compared with information provided on other clinical conditions. Percentage of physicians rating information as poor (scores 1–2) or neutral (score 3).
When asked to score their patients' ability to explain AF, the average rating score was 2.6 (on a five-point scale). Thus, 46% of physicians rated patient ability to explain AF as poor, whereas 24% of patients rated their own ability to explain AF as poor and at least one in four patients with AF felt unable to explain their condition to another person.
Physicians considered that 51% of their patients with AF have an important need for more and improved information. Only 35% of physicians agreed that information provided by physicians to patients on AF was easy to understand, and only 20% felt there was enough educational information on AF for patients. A total of 60% of physicians believed that patients had trouble sourcing information on AF.
Patient views on the level of information provided on AF were varied, with 57% of patients agreeing that information provided by the physician was easy to understand, whereas 23% of patients reported that they did not know where to look, or whom to contact, to get information on AF. Physicians believed that 60% of patients are satisfied with the level of information provided.
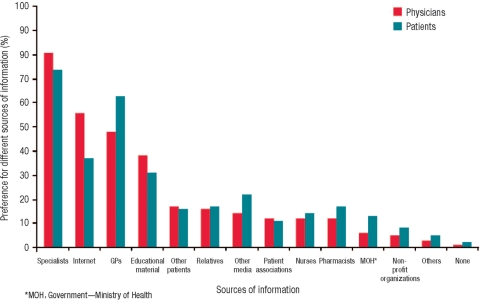
Both physicians and patients considered that specialist physicians and GPs were the core group of healthcare professionals to provide on-going patient support and information on AF (Figure 5). In addition, 46% of patients said they searched for more information on AF, or requested information on AF, in an attempt to understand their disease and its management more fully.
Figure 5.
Patients' preferred sources for receiving information on atrial fibrillation, and physicians' perceptions of their patients' preferred information sources.
Perceptions of patient concerns and quality of life
Over one-third of patients were worried or fearful about their AF (Table 1).
Table 1.
A comparison of physicians' perception of patient-worry about atrial fibrillation and actual patient-reported feelings about atrial fibrillation
| Reported or perceived feelings about AF | AF patients reporting a feeling (%) | Physician perceptions of patient feelings (%) |
|---|---|---|
| Afraid | 5 | 13 |
| Worried | 29 | 22 |
| Neither reassured nor worried | 20 | 23 |
| Quite reassured | 33 | 20 |
| Very reassured | 13 | 22 |
Values are percentage of respondents who selected each answer option.
Both physicians and patients rated AF as having an adverse impact on patient QoL. Consequences of an AF diagnosis such as hospitalization, recurrent symptoms, treatment monitoring, limitations on physical function, altered general health, limitations on social activities, and patients' altered mental health all had ‘some’ to ‘high’ impact on their patients' daily function.
Discussion
The survey findings suggest that patients' level of understanding of AF is often insufficient to allow appreciation of the risks conferred by AF and highlights that patients often have a poor understanding of AF management and treatment.
Around 25% of patients felt unable to explain their condition. These findings are in keeping with the literature on patient knowledge and perceptions of AF and its treatments. For example, in a study of 93 patients with AF, nearly half of all patients could not name their condition and did not understand the role of anticoagulant treatment for AF. However, after those patients were given literature and verbal explanations on AF and its treatment, rates of understanding improved.26 The current literature highlights that patients with risk factors (including AF) are often unable to identify their health condition as a risk factor for stroke and have low-risk perceptions about their health status.23,24
In this survey, physicians assumed that their patients would have quite low levels of understanding of the nature of AF and its management. Physicians' own perceptions of the risks associated with AF were closely aligned with the clinical facts and data regarding AF risks.1,11,12
In this survey, over 50% of patients only had their AF recognized during routine check-ups or while consulting for another condition. Better identification and appropriate treatment of AF at an earlier time point in the course of this often progressive disease could help reduce both the clinical burden and health–economic impact associated with AF.1,11,12,17,18
Physicians and patients differed in their views about, and satisfaction with, AF management and treatment. Although more than half of physicians were either neutral about or dissatisfied with treatments, patients reported that they were highly satisfied with treatments offered for AF. High levels of satisfaction with treatment were voiced despite the fact that over 80% of the patient surveys reported on-going AF symptoms.
More than one-third of patients reported that they were worried or afraid about their AF and stated that they need more reassurance and counselling on their condition. This observation seems at odds with patient reports of satisfaction with their current AF management and may indicate that patients feel resigned to their situation rather than able to affect it through their own actions or via consultations with their physician. It is known that one-third of AF patients experience persistent depression,20 and anxiety is common among newly diagnosed patients.27
Despite guidelines on AF management,5 there is some evidence in the literature that physicians may be reluctant to employ treatments for AF that could reduce AF risks because of concerns about safety. For example, a study of physicians' attitudes towards the use of antithrombotic drugs suggested uncertainties among GPs and cardiologists about the most appropriate use of these drugs,23 and similar lack of confidence in, and awareness of, treatments has been reported in other studies and reviews.22,28 Experience in other CV disease areas suggests that better adherence to guidelines and better education around the risk and benefits of treatments are needed to improve patient management.29
The apparent gaps between patient and physician understanding of AF reported in the survey could be interpreted as highlighting a need to support patients through better information provision and education. A recent study which followed a group of patients during the first 12 months after AF diagnosis noted that anxiety was the main, and a common, affective response.27 That same study concluded that addressing AF patients' anxiety should constitute a key element of patient management and should happen early in the process of establishing a good patient–physician relationship.27 These findings are reinforced by the current survey which illustrated that patients see healthcare professionals, particularly GPs, as their most important source of information. However, this observation is confounded by the fact that 60% of physicians surveyed believe that the availability of quality information is inadequate for patient counselling and that patients have trouble sourcing information. Furthermore, physicians overestimated patients' use of the Internet as an information source.
In keeping with the literature on AF, this survey found that a diagnosis of AF had considerable impact on QoL and daily living.17–20,27,30–32 In older people (aged ≥65 years) with AF, almost all studies of health-related QoL identify lower QoL outcomes in AF patients, and also identify that better control of heart rate can improve health-related QoL in these patients.32
The socio-economic burden posed by AF was also highlighted by the survey findings. Physicians ranked AF as a condition placing high demand on their time, and it was found that AF management required frequent consultations. There is evidence that early assessment and appropriate educational intervention to help improve patient's knowledge may reduce hospitalizations and potentially improve long-term health outcomes.26,33
There are limitations to patient and physician surveys inherent within the need to recruit from databases of respondents willing and able to give time to answering a set of pre-defined questions. Sampling from such databases may not provide a representative real practice cohort of either physicians treating AF or patients with AF. In the patient sample reported here, for example, 20% of patients stated they had continuous AF and more than half had moderate-to-severe AF, suggesting that this was a group of patients not representative of the population in general but representative of AF patients who are typically managed by a cardiologist. The survey used different methods of data collection—on-line and verbal interviews—which may have affected the responses obtained. However, the use of standard questions and rating scales should have ensured consistency of answers regardless of interview method. The survey sought opinion and perceptions of AF and its treatment, and many physician questions solicited physician opinions on patients' beliefs. As such, the survey responses, even those involving a rating scale, remain viewpoints and perceptions in the main and do not allow strict statistical comparisons of data points. However, the strength of this study is its contemporary and parallel assessment of patient and physician views, which offer a unique opportunity to examine gaps and differences in understanding between these groups.
In conclusion, this survey of patients with AF and physicians managing AF provides unique, international insights into levels of understanding by patients and their physicians of the risks posed by AF. A comprehensive international patient and professional information and support programme on AF is urgently needed and further clinical studies to confirm the long-term benefits of an intervention-based approach are warranted.
Funding
This work was supported by sanofi-aventis, who provided funding for the survey, editorial support, and an unrestricted educational grant to the AF AWARE group. Funding to pay the Open Access charges for this paper was provided by sanofi-aventis.
Acknowledgements
The survey was conducted by the TNS Healthcare group.
The AF AWARE Group would like to thank Dr Winnie McFadzean for her editorial support (consolidating author amends, formatting, styling) in the preparation of this manuscript.
Conflict of interest: E.A. has received consulting fees from sanofi-aventis, Cardiome, Meda Pharma, St Jude, Biotronic, Medtronic, Sorin Ela Medical. G.B. has been a member of advisory boards for sanofi-aventis, Boehringer-Ingelheim, Bayer, Boston-Scientific, and Medtronic. He has received honoraria for lectures at various meetings from such companies. He is a member of steering committees of trials sponsored by Bayer, Johnson & Johnson, Cordis, Meda Pharma Germany, and sanofi-aventis. J.C. has received consulting fees from and has been a member of the speakers' bureau for sanofi-aventis, Cardiome, Astellas, Merck, Bayer, Boehringer Ingleheim, ARYx, and Bristol Myers Squibb. G.Y.H.L. has been a member of advisory boards for sanofi-aventis, Boehringer-Ingelheim, Bayer, Astellas, and Astra Zeneca. He has received honoraria for lectures at various meetings from such companies.
References
- 1.Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98:946–52. doi: 10.1161/01.cir.98.10.946. [DOI] [PubMed] [Google Scholar]
- 2.Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003;107:2920–5. doi: 10.1161/01.CIR.0000072767.89944.6E. doi:10.1161/01.CIR.0000072767.89944.6E. [DOI] [PubMed] [Google Scholar]
- 3.Wang TJ, Massaro JM, Levy D, Vasan RS, Wolf PA, D'Agaostino RB, et al. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003;290:1049–56. doi: 10.1001/jama.290.8.1049. doi:10.1001/jama.290.8.1049. [DOI] [PubMed] [Google Scholar]
- 4.Lip GY, Agnelli G, Thach AA, Knight E, Rost D, Tangelder MJ. Oral anticoagulation in atrial fibrillation: a pan-European patient survey. Eur J Intern Med. 2007;18:202–8. doi: 10.1016/j.ejim.2006.11.005. doi:10.1016/j.ejim.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients with Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257–e354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 6.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–5. doi: 10.1001/jama.285.18.2370. doi:10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 7.Savelieva I, Camm J. Update on atrial fibrillation: part I. Clin Cardiol. 2008;31:55–62. doi: 10.1002/clc.20138. doi:10.1002/clc.20138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110:1042–6. doi: 10.1161/01.CIR.0000140263.20897.42. doi:10.1161/01.CIR.0000140263.20897.42. [DOI] [PubMed] [Google Scholar]
- 9.Kato T, Yamashita T, Sagara K, Iinuma H, Fu LT. Progressive nature of paroxysmal atrial fibrillation. Observations from a 14-year follow-up study. Circ J. 2004;68:568–72. doi: 10.1253/circj.68.568. doi:10.1253/circj.68.568. [DOI] [PubMed] [Google Scholar]
- 10.Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113:359–64. doi: 10.1016/s0002-9343(02)01236-6. doi:10.1016/S0002-9343(02)01236-6. [DOI] [PubMed] [Google Scholar]
- 11.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 12.Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22:312–8. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 13.Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, et al. Stroke severity in atrial fibrillation. The Framingham Study. Stroke. 1996;27:1760–4. doi: 10.1161/01.str.27.10.1760. [DOI] [PubMed] [Google Scholar]
- 14.Dulli DA, Stanko H, Levine RL. Atrial fibrillation is associated with severe acute ischemic stroke. Neuroepidemiology. 2003;22:118–23. doi: 10.1159/000068743. doi:10.1159/000068743. [DOI] [PubMed] [Google Scholar]
- 15.Pizzetti F, Turazza FM, Franzosi MG, Barlera S, Ledda A, Maggioni AP, et al. Incidence and prognostic significance of atrial fibrillation in acute myocardial infarction: the GISSI-3 data. Heart. 2001;86:527–32. doi: 10.1136/heart.86.5.527. doi:10.1136/heart.86.5.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pedersen OD, Abildstrom SZ, Ottesen MM, Rask-Madsen C, Bagger H, Kober L, et al. Increased risk of sudden and non-sudden cardiovascular death in patients with atrial fibrillation/flutter following acute myocardial infarction. Eur Heart J. 2006;27:290–5. doi: 10.1093/eurheartj/ehi629. doi:10.1093/eurheartj/ehi629. [DOI] [PubMed] [Google Scholar]
- 17.Wattigney WA, Mensah GA, Croft JB. Increasing trends in hospitalization for atrial fibrillation in the United States, 1985 through 1999: implications for primary prevention. Circulation. 2003;108:711–6. doi: 10.1161/01.CIR.0000083722.42033.0A. doi:10.1161/01.CIR.0000083722.42033.0A. [DOI] [PubMed] [Google Scholar]
- 18.Ringborg A, Nieuwlaat R, Lindgren P, Jonsson B, Fidan D, Maggioni AP, et al. Costs of atrial fibrillation in five European countries: results from the Euro Heart Survey on atrial fibrillation. Europace. 2008;10:403–11. doi: 10.1093/europace/eun048. doi:10.1093/europace/eun048. [DOI] [PubMed] [Google Scholar]
- 19.Thrall G, Lane D, Carroll D, Lip GY. Quality of life in patients with atrial fibrillation: a systematic review. Am J Med. 2006;119:448. doi: 10.1016/j.amjmed.2005.10.057. e1–e19. [DOI] [PubMed] [Google Scholar]
- 20.Thrall G, Lip GY, Carroll D, Lane D. Depression, anxiety, and quality of life in patients with atrial fibrillation. Chest. 2007;132:1259–64. doi: 10.1378/chest.07-0036. doi:10.1378/chest.07-0036. [DOI] [PubMed] [Google Scholar]
- 21.Murphy NF, Simpson CR, Jhund PS, Stewart S, Kirkpatrick M, Chalmers J, et al. A national survey of the prevalence, incidence, primary care burden and treatment of atrial fibrillation in Scotland. Heart. 2007;93:606–12. doi: 10.1136/hrt.2006.107573. doi:10.1136/hrt.2006.107573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deplanque D, Leys D, Parnetti L, Schmidt R, Ferro J, De Reuck J, et al. Stroke prevention and atrial fibrillation: reasons leading to an inappropriate management. Main results of the SAFE II study. Br J Clin Pharmacol. 2004;57:798–806. doi: 10.1111/j.1365-2125.2004.02086.x. doi:10.1111/j.1365-2125.2004.02086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peterson GM, Boom K, Jackson SL, Vial JH. Doctors' beliefs on the use of antithrombotic therapy in atrial fibrillation: identifying barriers to stroke prevention. Intern Med J. 2002;32:15–23. doi:10.1046/j.1445-5994.2002.00156.x. [PubMed] [Google Scholar]
- 24.Dearborn JL, McCullough LD. Perception of risk and knowledge of risk factors in women at high risk for stroke. Stroke. 2009;40:1181–6. doi: 10.1161/STROKEAHA.108.543272. doi:10.1161/STROKEAHA.108.543272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lip GY, Kamath S, Jafri M, Mohammed A, Bareford D. Ethnic differences in patient perceptions of atrial fibrillation and anticoagulation therapy: the West Birmingham Atrial Fibrillation Project. Stroke. 2002;33:238–42. doi: 10.1161/hs0102.101817. doi:10.1161/hs0102.101817. [DOI] [PubMed] [Google Scholar]
- 26.Lane DA, Ponsford J, Shelley A, Sirpal A, Lip GY. Patient knowledge and perceptions of atrial fibrillation and anticoagulant therapy: effects of an educational intervention programme. The West Birmingham Atrial Fibrillation Project. Int J Cardiol. 2006;110:354–8. doi: 10.1016/j.ijcard.2005.07.031. doi:10.1016/j.ijcard.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 27.Lane DA, Langman CM, Lip GYH, Nouwen A. Illness perceptions, affective response, and health-related quality of life in patients with atrial fibrillation. J Psychosom Res. 2009;66:203–10. doi: 10.1016/j.jpsychores.2008.10.007. doi:10.1016/j.jpsychores.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 28.Camm AJ. Safety considerations in the pharmacological management of atrial fibrillation. Int J Cardiol. 2008;127:299–306. doi: 10.1016/j.ijcard.2007.11.006. doi:10.1016/j.ijcard.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Bramlage P, Thoenes M, Kirch W, Lenfant C. Clinical practice and recent recommendations in hypertension management—reporting a gap in a global survey of 1259 primary care physicians in 17 countries. Curr Med Res Opin. 2007;23:783–91. doi: 10.1185/030079907x182077. doi:10.1185/030079907X182077. [DOI] [PubMed] [Google Scholar]
- 30.Dorian P, Jung W, Newman D, Paquette M, Wood K, Ayers GM, et al. The impairment of health-related quality of life in patients with intermittent atrial fibrillation: implications for the assessment of investigational therapy. J Am Coll Cardiol. 2000;36:1303–9. doi: 10.1016/s0735-1097(00)00886-x. doi:10.1016/S0735-1097(00)00886-X. [DOI] [PubMed] [Google Scholar]
- 31.Singh SN, Tang XC, Singh BN, Dorian P, Reda DJ, Harns CL, et al. Quality of life and exercise performance in patients in sinus rhythm versus persistent atrial fibrillation: a Veterans Affairs Cooperative Studies Program Substudy. J Am Coll Cardiol. 2006;48:721–30. doi: 10.1016/j.jacc.2006.03.051. doi:10.1016/j.jacc.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 32.Lane DA, Lip GY. Quality of life in older people with atrial fibrillation. J Interv Card Electrophysiol. 2009;25:37–42. doi: 10.1007/s10840-008-9318-y. doi:10.1007/s10840-008-9318-y. [DOI] [PubMed] [Google Scholar]
- 33.Gillis AM, Burland L, Arnburg B, Kmet C, Pollak PT, Kavanagh K, et al. Treating the right patient at the right time: an innovative approach to the management of atrial fibrillation. Can J Cardiol. 2008;24:195–8. doi: 10.1016/s0828-282x(08)70583-x. [DOI] [PMC free article] [PubMed] [Google Scholar]