Abstract
Objectives: To determine the demands on healthcare resources caused by different types of illnesses and variation with age and sex.
Design: Information on healthcare use was obtained from all 22 healthcare sectors in the Netherlands. Most important sectors (hospitals, nursing homes, inpatient psychiatric care, institutions for mentally disabled people) have national registries. Total expenditures for each sector were subdivided into 21 age groups, sex, and 34 diagnostic groups.
Setting: Netherlands, 1994.
Main outcome measures: Proportion of healthcare budget spent on each category of disease and cost of health care per person at various ages.
Results: After the first year of life, costs per person for children were lowest. Costs rose slowly throughout adult life and increased exponentially from age 50 onwards till the oldest age group (⩾95). The top five areas of healthcare costs were mental retardation, musculoskeletal disease (predominantly joint disease and dorsopathy), dementia, a heterogeneous group of other mental disorders, and ill defined conditions. Stroke, all cancers combined, and coronary heart disease ranked 7, 8, and 10, respectively.
Conclusions: The main determinants of healthcare use in the Netherlands are old age and disabling conditions, particularly mental disability. A large share of the healthcare budget is spent on long term nursing care, and this cost will inevitably increase further in an ageing population. Non-specific cost containment measures may endanger the quality of care for old and mentally disabled people.
Key messages
Little is known about demands for health care outside acute sectors
In the Netherlands health costs are strongly age dependent, increasing exponentially after age 50
The five highest healthcare costs are for mental retardation, musculoskeletal disease, dementia, other mental disorders, and ill defined conditions
Coronary heart disease, all cancers, and stroke accounted for only 9% of costs
The main healthcare costs are for care not cure and costs are likely to increase rapidly in an ageing society
Introduction
The debate on containing the cost of health care is mainly focused on the supply side and the financing of health care.1 Little attention is given to changes in population health, which is another important determinant of costs. This may be because the relation between disease and costs is not straightforward and relevant data are often lacking. We therefore subdivided total healthcare costs in the Netherlands by healthcare sector, diagnosis, age, and sex to determine which illnesses and age groups have the greatest demand for care. The Dutch healthcare budget is ideal for this type of analysis since the country is small, more than 99% of its population has full health insurance cover, and because of a longstanding administrative tradition most healthcare sectors have excellent registries, of which the most important are national. The completeness of Dutch healthcare data has allowed us to include not only the acute care sectors but also those sectors which deliver long term care to disabled people. Long term care is rarely included in other studies,2–5 which consequently underestimate the high costs of disabling disease.
Methods
We used data on healthcare costs for each care sector from the Ministry of Health for 1994 (table 1).6 Additional personal expenditures, such as over the counter medicines and spectacles (6% of all costs), were not included.
Table 1.
Percentage of healthcare budget spent on different sectors of care in Netherlands, 1994
| Healthcare sector | % of total* |
|---|---|
| Hospital care | 32.1 |
| Nursing homes | 8.9 |
| Old people’s homes: | |
| Medical costs | 3.7 |
| Living costs | 5.4 |
| Psychiatric care | 7.1 |
| Institutions for mentally and physically disabled people | 8.6 |
| Primary medical and paramedical services (excluding dental care) | 5.7 |
| Dental care | 4.0 |
| Pharmaceutical care | 8.8 |
| Home care and other small sectors | 10.4 |
| Healthcare administration | 5.3 |
Healthcare spending in 1994 was 59.5 bn guilders (£21.3bn, $32.7 bn), 9.7% of gross national product.
We clustered the diagnoses of the international classification of diseases (ICD, 9th revision)7 into 34 diagnostic groups, which can be regrouped into the 17 chapters of the ICD (table 2). We defined groups of diagnoses to minimise misclassification between diagnostic groups and so that each group would be large enough to describe a sufficiently large proportion of healthcare costs. Conditions that could not be related to a specific diagnostic group but that are unambiguously related to a specific functional system (cardiovascular, respiratory, mental, etc) were assigned to the remainder group of that specific ICD chapter. Ill defined conditions which could not be related to a specific ICD chapter were classified as “symptoms and ill defined conditions” (ICD chapter 16). This is particularly relevant in primary health care, where patients present with problems not diagnoses. To avoid double counting we have considered only primary diagnoses.
Table 2.
Diagnostic groups used in study and corresponding ICD 9 code7
| ICD chapter | Diagnostic group | ICD codes | |
|---|---|---|---|
| I | Infectious and parasitic diseases | Infection | 1-139 |
| II | Neoplasms | Cancer | 140-208 |
| Benign neoplasms | 210-239 | ||
| III | Endocrine, metabolic, and nutritional diseases | Diabetes | 250 |
| Other endocrine diseases | 240-279 | ||
| IV | Blood and blood forming organs | Blood diseases | 280-289 |
| V | Mental disorders | Dementia | 290 |
| Schizophrenia | 295 | ||
| Depression and anxiety | 296, 300 | ||
| Alcohol and drugs | 291-292, 303-305 | ||
| Mental retardation, Down’s syndrome* | 317-319, 758.0 | ||
| Other mental disorders | Remainder 290-316 | ||
| VIa | Nervous system | Neurological disorders | 320-359 |
| VIb | Sense organs | Eye disorders | 360-379 |
| Ear disorders | 380-389 | ||
| VII | Circulatory system | Hypertension | 401-405 |
| Coronary heart diseases | 410-414 | ||
| Heart failure | 428-429 | ||
| Stroke | 430-438 | ||
| Other circulatory diseases | Remainder 390-459 | ||
| VIII | Respiratory system | Asthma and chronic obstructive airways disease | 490-496 |
| Other respiratory diseases | 460-489, 497-519 | ||
| IX | Digestive system | Dental diseases | 520-529 |
| Gastrointestinal diseases | 531-569 | ||
| Liver, gall, pancreatic diseases | 570-579 | ||
| Xa | Urinary system | Urinary disorders | 580-599 |
| Xb | Genital organs | Genital disorders | 600-629 |
| XI | Pregnancy and childbirth† | Pregnancy | 630-676 |
| XII | Skin diseases | Skin diseases | 680-709 |
| XIII | Musculoskeletal system | Musculoskeletal diseases | 710-739 |
| XIV/XV | Perinatal/congenital conditions† | Perinatal/congenital conditions | 740-779 |
| XVI | Symptoms, signs, and ill defined conditions | Ill defined conditions | 780-899 |
| XVII | Accidents | Falls | E880-888 |
| Other accidents | E800-879, E890-999 | ||
| Not allocated | |||
| Non-specific‡ | |||
Down’s syndrome is classified in ICD chapter XV, code 758.0. †Hospital costs of healthy babies (boys and girls) after childbirth were assigned to pregnancy and childbirth (women). ‡Costs of healthcare administration and living costs in old people’s homes.
Of all healthcare costs, 8.1% could not be allocated to any diagnostic group because of insufficient information from some smaller healthcare sectors and 5.3% are for healthcare administration and are not related to specific health problems. Together with the living costs in old people’s homes, these costs were assigned to non-specific healthcare costs.
For each healthcare sector we identified key variables that are representative of healthcare use in that sector, such as days of stay for nursing costs in hospitals and nursing homes or outpatient visits for costs of outpatient hospital care. We divided each sector by sex, 21 age groups (0, 1-4, 5-9, 10-14, ...⩾95 years), and 34 diagnostic clusters to give 1428 cells (2 × 21× 34). We considered the distribution of the costs to be the same as the distribution of the key variable for that sector. Thus, for each healthcare sector costs for each combination of age, sex, and diagnostic group were calculated as the proportion of the key variable in the relevant cell times the total costs for the sector.
The probability distribution of key variables was derived from sector specific registries and sample surveys. Detailed information about the registries and the key variables used is available in a report8 and on our web page: http://www.eur.nl/fgg/mgz/.
Results
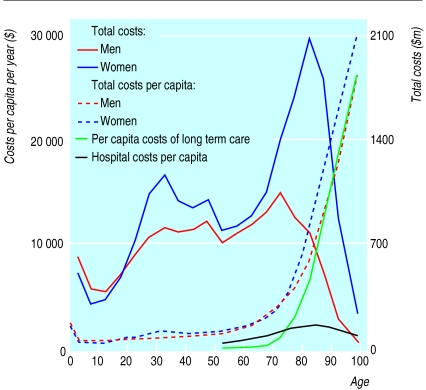
Total healthcare costs, representing 9.7% of the Dutch gross national product, were £1381 ($2124) per capita in 1994, £1613 ($2481) for women and £1144 ($1760) for men. The distribution is strongly age dependent (figure). Costs are relatively high in the first year of life, reflecting the high costs of perinatal and infant care, but then drop to the lowest levels in childhood. During adulthood costs increase slowly, and after age 50 they start to increase exponentially up to the highest age group (⩾95). The higher share in total costs of women (59%) is predominantly caused by their longer life expectancy, the higher prevalence of women in nursing homes and homes for elderly people, and the high costs of reproduction (including contraception and diseases of the genital organs).
Table 3 shows the share in total costs of diagnostic groups by sex (table 3). A high proportion of healthcare costs are for mental disorders. Mental retardation ranks 1, dementia ranks 3, depression and anxiety ranks 15, schizophrenia 23, alcohol and drug misuse 31, and the heterogeneous remainder group of mental disorders ranks 4. All mental disorders together cover 28.4% of the healthcare budget that could be allocated to diagnostic groups. Ill defined conditions, which include many psychosomatic problems, rank 5. Musculoskeletal diseases (predominantly all types of arthritis) rank 2. Dental diseases (predominantly dentists’ costs) rank 6. The main causes of death—that is, stroke, all cancers combined, and coronary heart disease—rank 7, 8, and 10, respectively. Among women, costs of reproduction rank 6.
Table 3.
Healthcare costs by diagnostic group and sex, Netherlands 1994, ranked by share (in % of total healthcare costs)
| Rank | Diagnostic group* | Men | Women | Total |
|---|---|---|---|---|
| 1 | Mental retardation, Down’s syndrome | 11.0 | 6.0 | 8.1 |
| 2 | Musculoskeletal diseases | 5.4 | 6.4 | 6.0 |
| 3 | Dementia | 2.9 | 7.4 | 5.6 |
| 4 | Other mental disorders | 5.4 | 4.7 | 5.0 |
| 5 | Ill defined conditions | 4.6 | 5.0 | 4.8 |
| 6 | Dental diseases | 4.9 | 3.8 | 4.2 |
| 7 | Stroke | 3.0 | 3.4 | 3.2 |
| 8 | Cancer | 3.7 | 2.8 | 3.2 |
| 9 | Pregnancy | 0.0 | 4.3 | 2.6 |
| 10 | Coronary heart diseases | 3.9 | 1.5 | 2.5 |
| 11 | Neurological disorders | 2.6 | 2.3 | 2.4 |
| 12 | Other circulatory diseases | 2.8 | 2.1 | 2.4 |
| 13 | Other respiratory diseases | 2.9 | 1.9 | 2.3 |
| 14 | Other accidents | 2.8 | 1.9 | 2.3 |
| 15 | Depression and anxiety | 1.8 | 2.6 | 2.3 |
| 16 | Falls | 1.3 | 2.4 | 2.0 |
| 17 | Gastrointestinal diseases | 2.4 | 1.6 | 1.9 |
| 18 | Asthma and chronic obstructive airways disease | 2.4 | 1.2 | 1.7 |
| 19 | Eye disorders | 1.7 | 1.7 | 1.7 |
| 20 | Liver, gall, and pancreatic diseases | 1.7 | 1.6 | 1.7 |
| 21 | Skin diseases | 1.7 | 1.6 | 1.6 |
| 22 | Genital disorders | 0.9 | 1.9 | 1.5 |
| 23 | Schizophrenia | 2.1 | 1.0 | 1.4 |
| 24 | Urinary disorders | 1.3 | 1.3 | 1.3 |
| 25 | Infection | 1.5 | 1.2 | 1.3 |
| 26 | Hypertension | 1.3 | 1.3 | 1.3 |
| 27 | Diabetes | 1.1 | 1.4 | 1.2 |
| 28 | Ear disorders | 1.4 | 0.9 | 1.1 |
| 29 | Heart failure | 1.1 | 1.1 | 1.1 |
| 30 | Perinatal/congenital conditions | 1.4 | 0.9 | 1.1 |
| 31 | Alcohol and drugs | 1.4 | 0.4 | 0.8 |
| 32 | Benign neoplasms | 0.5 | 0.9 | 0.7 |
| 33 | Other endocrine diseases | 0.4 | 0.8 | 0.6 |
| 34 | Blood diseases | 0.3 | 0.3 | 0.3 |
| Not allocated | 7.2 | 8.8 | 8.1 | |
| Non-specific† | 9.1 | 11.7 | 10.7 | |
| Share in total costs (%) | 41.0 | 59.0 | 100.0 | |
See table 2 for ICD codes of all diagnostic groups.
Costs of healthcare administration and living costs in old people’s homes.
Table 4 shows the 15 diagnostic categories with the highest healthcare expenditure for five age groups. In all age groups either mental retardation or dementia is the main healthcare cost. In children cognitive disability ranks second but congenital diseases also cover many mentally disabling conditions. Among younger adults (age 15-44) the heterogeneous remainder group of mental disorders is second and schizophrenia, depression, and alcohol and drug related problems all rank among the top 15. Musculoskeletal diseases rank among the top five in all age groups after age 14, and ill defined conditions rank among the top six in all age groups. In the oldest age group (⩾85) stroke is second and accidental falls (predominantly hip fractures) third. All cancers reach the top five only in the 65-84 age group and coronary heart disease only in middle age (age 45-64).
Table 4.
Fifteen diagnostic groups* accounting for highest percentage of healthcare costs for five age groups, Netherlands 1994
| Age 0-14
|
Age 15-44
|
Age 45-64
|
Age 65-84
|
Age ⩾85
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rank | Diagnostic group | % of costs | Diagnostic group | % of costs | Diagnostic group | % of costs | Diagnostic group | % of costs | Diagnostic group | % of costs | ||||
| 1 | Perinatal/congenital condition | 10.2 | Mental retardation, Down’s syndrome | 16.5 | Mental retardation, Down’s syndrome | 9.4 | Dementia | 9.5 | Dementia | 22.2 | ||||
| 2 | Mental retardation, Down’s syndrome | 9.7 | Other mental disorders | 8.6 | Musculoskeletal diseases | 8.3 | Stroke | 6.7 | Stroke | 6.6 | ||||
| 3 | Other respiratory diseases | 6.3 | Pregnancy | 8.5 | Dental diseases | 6.3 | Musculoskeletal diseases | 5.8 | Falls | 5.9 | ||||
| 4 | Other mental disorders | 6.0 | Dental diseases | 6.6 | Ill defined conditions | 5.8 | Cancer | 5.6 | Musculoskeletal diseases | 4.3 | ||||
| 5 | Ill defined conditions | 5.5 | Musculoskeletal diseases | 6.3 | Coronary heart diseases | 5.0 | Ill defined conditions | 4.6 | Ill defined conditions | 3.7 | ||||
| 6 | Ear disorders | 5.2 | Ill defined conditions | 4.7 | Other mental disorders | 4.9 | Coronary heart diseases | 4.0 | Heart failure | 2.9 | ||||
| 7 | Dental disorders | 4.6 | Schizophrenia | 3.5 | Cancer | 4.6 | Other circulatory diseases | 3.9 | Cancer | 2.1 | ||||
| 8 | Infection | 4.0 | Depression/anxiety | 3.4 | Depression/anxiety | 3.4 | Neurological disorders | 2.9 | Other respiratory diseases | 2.1 | ||||
| 9 | Neurological disorders | 2.8 | Other accidents | 3.1 | Other circulatory diseases | 3.3 | Other mental disorders | 2.6 | Neurological disorders | 2.0 | ||||
| 10 | Other accidents | 2.3 | Genital disorders | 2.3 | Gastrointestinal diseases | 2.7 | Falls | 2.5 | Other circulatory diseases | 1.7 | ||||
| 11 | Eye disorders | 2.2 | Skin diseases | 2.2 | Neurological disorders | 2.7 | Asthma and chronic obstructive airways disease | 2.5 | Other mental disorders | 1.5 | ||||
| 12 | Asthma and chronic obstructive airways disease | 2.3 | Other respiratory diseases | 2.0 | Liver, gall, and pancreatic diseases | 2.5 | Eye disorders | 2.3 | Liver, gall, and pancreatic diseases | 1.3 | ||||
| 13 | Musculoskeletal diseases | 1.9 | Neurological disorders | 2.0 | Hypertension | 2.5 | Diabetes | 2.2 | Eye disorders | 1.2 | ||||
| 14 | Gastrointestinal diseases | 1.6 | Alcohol/drugs | 1.6 | Asthma and chronic obstructive airways disease | 2.2 | Gastrointestinal diseases | 2.2 | Urinary disorders | 1.2 | ||||
| 15 | Skin diseases | 1.6 | Gastrointestinal diseases | 1.6 | Other accidents | 2.2 | Heart failure | 2.1 | Other accidents | 1.1 | ||||
| % share of age groups in total costs | 7.9 | 29.3 | 20.7 | 30.6 | 11.6 | |||||||||
| % share of age groups in population | 18.4 | 46.0 | 22.5 | 11.8 | 1.3 | |||||||||
See table 2 for ICD codes of all diagnostic groups.
Discussion
In the Netherlands healthcare costs are dominated by old age and by disability, particularly mental disability and musculoskeletal diseases. The amount of the healthcare budget spent on the main fatal diseases is relatively modest: all cardiovascular diseases and all cancers, which together cause 67% of all deaths, accounted for only 17% of all healthcare costs that could be allocated to a diagnostic group.
These results have to be interpreted with caution. Less attention should be paid to the exact share of costs spent on each diagnostic group than to the patterns of distribution which emerge from these data. Firstly, the key variables used to break down costs are generally not collected for epidemiological purposes, but in the Netherlands there is no financial incentive to register one diagnosis rather than another. We considered only primary diagnoses. It is beyond the limits of the method used to assign costs appropriately to the primary as well as each secondary diagnosis. Valid information about secondary diagnoses is generally lacking or incomplete. As a result, costs of diagnoses that are more often registered as secondary or tertiary, such as diabetes, are slightly underestimated. However, the registered primary diagnosis is generally the more important diagnosis for the healthcare sector concerned and the main reason why health care is needed—for example, what the internist calls osteoporosis is for the surgeon a hip fracture, for the ambulance service an accidental fall, and for the nursing home a demented patient. The advantage of our method is that each guilder is allocated to only one combination of age, sex, and diagnostic group, avoiding double counting.
Secondly, the key variables used to break down costs for each healthcare sector do not represent exactly equal amounts of resources. Not all days of stay in hospitals or nursing homes are equally expensive, some hours of care are more labour intensive than others, and outpatient visits or primary care consultations can vary in length. As a result, costs of some diagnoses may be biased. For example, because hospital nursing costs are broken down by bed days without any differentiation, costs of diagnoses for which relatively more days are spent in intensive care will be slightly underestimated and vice versa. These limitations, however, will not affect our main findings, such as the exponential increase in per capita costs by age or the heavy burden of mental disorders.
Comparability
Our study’s biggest strength is its comprehensiveness. This explains why our results seem at variance with an American (Medicare) study that shows decreasing costs at the oldest ages.2 The American study did not include long term home care for elderly people or care in nursing and old people’s homes. It is these costs which cause the exponential increase in costs in old age. Like the American study we found that costs for acute admissions in hospital decrease at the oldest ages (figure 1). Most of these patients are already admitted to a nursing home or are too old or too ill to consider hospital admission useful. A Swedish study, which is older and less complete, showed the same results.9
Our findings correspond largely with those of our earlier study in 1988.10,11 Studies that are more or less comparable have been published in England,3 Australia,4 and Canada.5 These studies show basically similar cost patterns but with lower shares, particularly for mental retardation and dementia. However, they either did not consider all health care, particularly long term psychiatric care,3,4 or could not assign these costs to diagnoses.5 Apart from the degree of comprehensiveness, many other methodological and country specific issues may cause differences in cost distributions. A serious international comparison of distribution of cost of illness would require specifically designed cross national studies.
Our study considered only medical costs and not costs of informal care. It has been estimated that if informal care in the Netherlands was entirely substituted by professional care it would double the current costs of professional home care.12 Informal care mainly substitutes for simple forms of professional care. If these costs had been included the total costs of chronic, disabling conditions such as dementia and musculoskeletal disease would have been even more dominant, thus strengthening our conclusions.
The share of costs accounted for by fatal diseases is relatively small because care stops at death. Disability is the main reason why people use health care. The pattern of epidemiological causes of costs that we found is remarkably consistent with Murray and Lopez’s estimates of the main causes of disability in the developed world.13,14 In 1990 they estimated that mental disorders (including dementia and hereditary disorders of the central nervous system) accounted for 35.5% of life years lived with disability. In our study, the same disorders, including congenital anomalies, accounted for 28.4% of all healthcare costs that could be allocated to diagnostic groups. Musculoskeletal diseases, including arthritis and dorsopathy, caused 7.3% of the allocated healthcare costs, while Murray and Lopez estimated that osteoarthritis covered 6.1% of the life years lived with disability.
The costs presented here are grouped cross sectional figures. Each age group contains people with low or no costs and those with high costs due to costly interventions, severe disability, or impending death. In higher age groups more people have high costs, causing costs per person to rise. The cost distribution by age is informative, especially for societies that face a further ageing of the population. Since the distribution of costs is determined by the current prevalence of disease and disability, future healthcare costs will depend (among other things) on the evolution of the risk of disability and death by age.
We conclude that healthcare costs in the Netherlands are strongly determined by old age and disability. In future the ageing of society will undoubtedly increase healthcare needs. When talking about cost containment in health care we should not forget that large shares of the budgets are not spent on cure but on care. Long term care of old, frail, and mentally disabled people will always be labour intensive and expensive but is the hallmark of a civilized society.
Figure.
Total and per capita healthcare costs by age and sex for hospital and long term care in Netherlands, 1994. Long term care includes nursing homes, old people’s homes, institutional care for disabled people, and appliances to assist disabled people. In 1994 $1=£0.65
Footnotes
Funding: Dutch Ministry of Health, Welfare, and Sports and Health Care Information Centre (SIG).
Conflict of interest: None.
References
- 1.Aaron H, Schwartz WB. Rationing health care: the choice before us. Science. 1990;247:418–422. doi: 10.1126/science.2300804. [DOI] [PubMed] [Google Scholar]
- 2.Lubitz J, Beebe J, Baker C. Longevity and Medicare expenditures. N Engl J Med. 1995;332:999–1003. doi: 10.1056/NEJM199504133321506. [DOI] [PubMed] [Google Scholar]
- 3.Executive NHS. Burdens of disease: a discussion document. London: Department of Health; 1996. [Google Scholar]
- 4.Australian Institute of Health and Welfare. Australia’s health 1996. Canberra: AIHW; 1996. , 1996. [Google Scholar]
- 5.Moore R, Mao Y, Zhang J, Clarke K. Economic burden of illness in Canada, 1993. Ottowa: Minister of Public Works and Government Services; 1997. [PubMed] [Google Scholar]
- 6.Ministry of Health. Annual overview of health care, 1997. The Hague: SDU; 1996. [Google Scholar]
- 7.World Health Organisation. International Classification of Diseases. 9th ed. Geneva: WHO; 1977. [Google Scholar]
- 8.Polder JJ, Meerding WJ, Koopmanschap MA, Bonneux L, van der Maas PJ. Costs of diseases in the Netherlands, 1994. Rotterdam: Erasmus University, Department of Public Health, Institute of Medical Technology Assessment; 1997. [Google Scholar]
- 9.Lindgren B. The economic impact of illness. In: Abshagen U, Munnich FE, editors. Cost of illness and benefits of drug treatment. Munich: Zuckschwerdt Verlag; 1990. pp. 12–20. [Google Scholar]
- 10.Koopmanschap MA, van Roijen L, Bonneux L. Costs of diseases in the Netherlands, 1988. Rotterdam: Erasmus University, Department of Public Health, Institute of Medical Technology Assessment; 1991. [Google Scholar]
- 11.Koopmanschap MA, van Roijen L, Bonneux L, Bonsel GJ, Rutten FFH, van der Maas PJ. Costs of diseases in an international perspective. Eur J Public Health. 1994;4:258–264. [Google Scholar]
- 12.Groenenboom GKC, Huijsman R. Elderly care in economic perspective: cost scenarios. Utrecht: De Tijdstroom Steering Committee on Future Health Scenarios; 1995. [Google Scholar]
- 13.Murray CJL, Lopez AD. Global and regional descriptive epidemiology of disability. In: Murray CJL, Lopez AD, editors. The global burden of disease and injury series. Harvard: Harvard University Press; 1996. pp. 201–246. [Google Scholar]
- 14.Murray CJL, Lopez AD. Global mortality, disability and the contribution of risk factors. The global burden of disease study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]