Abstract
Purpose
The purpose of this study was to explore mothers’ perspectives about reproductive health (RH) discussions with their adolescent daughters with diabetes.
Methods
This study of mothers used a sequential explanatory mixed method design with 2 phases. Phase 2, the focus of this report, was a qualitative descriptive study using open-ended semi-structured telephone interviews. Ten mothers from a larger study sample were selected by purposeful sampling. Qualitative content analysis techniques were used to analyze the interview transcripts.
Results
The following 4 themes describing mothers’ perspectives about RH discussions with their adolescent daughters with diabetes were identified: 1) maternal awareness; 2) maternal knowledge; 3) triggers for initiating RH discussions; and, 4) maternal fears/concerns. Several mothers were aware of their daughters’ sexual activity and were aware that their daughters should preplan a pregnancy. They knew that an unplanned pregnancy may have detrimental effects on their daughters’ health and feared that their daughters would have an unplanned pregnancy. A major trigger for mothers to initiate RH discussions was when a daughter had a steady boyfriend. Mothers’ fears and concerns were focused around their daughters having an unplanned pregnancy. Overall, mothers reported they were not comfortable with RH conversations.
Conclusions
Mothers fear unplanned pregnancies for their daughters with diabetes and want to discuss RH issues with them, but are uncomfortable doing so. Diabetes educators could be instrumental in educating and providing communication skills to mothers to help foster RH communication with their adolescent daughters with diabetes.
Adolescence is a time when sexual risk-taking behaviors emerge.1,2 It has been reported that 43% of high school white females have been sexually active.3 Almost half of those reporting to be sexually active had an onset of sexual debut by the tenth grade. Similar patterns of sexual activity have been reported in adolescents with type 1 diabetes.4,5 In a multi-site phone survey of 87 adolescent girls with diabetes with a mean age of 17.86 years (SD=1.26, range 16–22) it was found that 43% had been sexually active.5 These adolescents with diabetes had their sexual debut at a mean age of 15.8 years (SD=1.2, range 14–18). Seventy-three percent reported use of a condom at each sexual encounter. However, only 30% reported the use of combination methods for birth control (i.e., condom with another method). In another report of 47 adolescent girls with diabetes with a mean age of 17.4 years (range 16–19) 32% reported being sexually active.4 In summary, from these studies, adolescents with diabetes have similar sexual risk-taking behaviors as adolescents in the general population.
Risk-taking sexual behaviors may result in negative consequences, such as an unplanned pregnancy and complications.6 Approximately 400,000 American teens in the general population become pregnant each year,7,8 with approximately 80% being unplanned.9 Pregnancy rates for teens with diabetes are consistent with those of the general population. In the previously reported multi-site phone survey,5 11% of the adolescent girls with diabetes who had been sexually active reported having at least one unplanned pregnancy. Pregnancy during adolescence is considered to be high risk,10 and diabetes presents added risks for maternal and fetal complications.
According to the American Diabetes Association (ADA),11 all women with diabetes of child-bearing age, starting at puberty, must receive preconception counseling and be educated about the risks of an unplanned pregnancy so that they may be empowered to be in control of their own reproductive health (RH). It has been reported that adolescent girls with diabetes have limited awareness of how diabetes can affect their RH, and of the risks of unplanned pregnancies to maternal and fetal complications.12,13 However, mothers can be key figures in the dissemination of this very important RH information to their adolescent daughters. Fortunately, parental involvement, such as mother-daughter sexual communication has shown to decrease the risk of negative developmental outcomes and prevent high-risk behaviors, such as, unprotected sex, in adolescents.14–16
Although many studies have investigated RH communication between mothers and daughters in the general population no studies have examined RH communication between a mother and her daughter with diabetes. Moreover, no studies have examined what mothers think about discussing these very important issues with their daughters with diabetes. Therefore, the purpose of this study was to explore mothers’ perspectives about initiating RH discussions with their adolescent daughters with diabetes.
Methods
Research Design
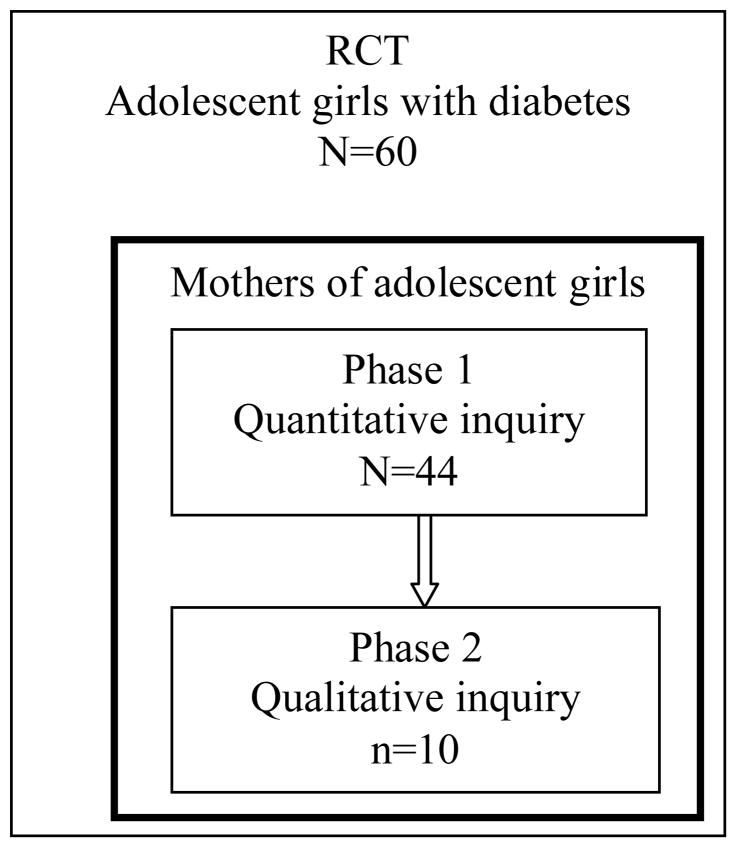
This qualitative descriptive study used semi-structured telephone interviews to explore mothers’ perspectives of RH discussions with their adolescent daughters with diabetes. As the second phase in a sequential explanatory mixed method design,17 this study’s sample (n=10) was purposively selected from the primary quantitative correlational and repeated measures study (N=44).
The sequential explanatory mixed method design is a two-phase model, where quantitative data is collected in the first phase and qualitative data is collected in the second phase.17 The qualitative phase is designed to be linked with and help to explain the quantitative results of the first phase. However, in this report we are focusing only on the qualitative interview data. Qualitative description is a naturalistic research approach that focuses on describing a phenomenon (i.e., mothers thoughts and experiences of talking with their daughters about RH issues) in a way that is not highly abstract or interpretive.18 It provides an overall review or summary of the events that is descriptive with low inference.18 The open-ended questions posed to mothers during the interviews allowed mothers to further describe, in their own words, their thoughts and experiences about talking with their daughters about RH issues17 This information could not be obtained with closed-ended questions as used in the quantitative phase of the study. This type of design provides the researcher with a deeper understanding of the phenomenon.17
This study of mothers was nested within a larger randomized, controlled clinical trial (RCT) that examined the effects of a newly developed CD-ROM preconception counseling educational program entitled “Reproductive Health Awareness for Teens with Diabetes (READY-Girls)”.19 Adolescent girls with type 1 diabetes between the ages of 13 to 19 years of age participated in the RCT while their mothers participated in the current study. See Figure 1.
Figure 1.
Sequential explanatory mixed method design
Sample
Mothers were recruited for the current study when their daughters’ were recruited to participate in the RCT. Mothers did not receive an intervention, however, they were labeled as intervention group (IG) or standard care control group (CG) based on their daughters’ randomization in the larger RCT. Mothers were required to be English speaking and living with their daughters, who could be natural, adoptive or step. We used criterion-related purposeful sampling20 to select a subset of 10 mothers from the total sample (N=44). Participants were selected for variation on the following parameters: baseline knowledge (modified Family Planning Behavior and Diabetes Study Questionnaire) and intention scores (modified Initiating Discussion questionnaire), daughters’ group assignment (IG or CG), and daughters’ age group (≤16 or ≥17 years) at the time of recruitment. Data from questionnaires administered in Phase 1 were used for criterion-related sampling.20 Table 1 presents the breakdown of sampling parameters. Table 2 presents a sampling matrix.
Table 1.
Sampling parameters (n=10)
| Daughter’s group assignment | |
| Intervention | 5 (50) |
| Control | 5 (50) |
| Daughter’s age group | |
| 13–16 years | 6 (60) |
| 17–20 years | 4 (40) |
| Mother’s knowledge | |
| Low ≤ 60% correct | 6 (60) |
| High > 60% correct | 4 (40) |
| Mother’s intention to initiate discussion | |
| Low ≤ 13 | 7 (70) |
| High > 13 | 3 (30) |
Data n (%).
Table 2.
Sampling Matrix
| Intervention group | Control group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Daughter’s age group 13–16 years | Daughter’s age group 17–19 years | Daughter’s age group 13–16 years | Daughter’s age group 17–19 years | ||||||
| Maternal history of diabetes | Maternal history of diabetes | Maternal history of diabetes | Maternal history of diabetes | Total | |||||
| Yes | No | Yes | No | Yes | No | Yes | No | ||
| Low knowledge/Low intention | 1 | 1 | 1 | 1 | 4 | ||||
| Low knowledge/High intention | 1 | 1 | 2 | ||||||
| High knowledge/Low intention | 1 | 1 | 1 | 3 | |||||
| High knowledge/High intention | 1 | 1 | |||||||
| Total | 1 | 3 | 0 | 1 | 0 | 2 | 1 | 2 | 10 |
The following 2 paragraphs describe the measures used for sample selection. The Family Planning Behavior and Diabetes Study Questionnaire,13,21 which was used with the adolescent girls in the RCT, was modified for mothers. This questionnaire measured mothers’ demographic characteristics and RH knowledge. Four subscales measured knowledge of diabetes and pregnancy, birth control, and sexuality, and general family planning. Summation of these 4 subscales comprised total knowledge, which is represented by percent correct (0–100%). Baseline scores of knowledge were dichotomized, using the median score of 60 as the cut point, into low and high for sampling purposes. The median score was chosen as it represents the 50th percentile of a distribution of scores, the point where an equal number of scores will fall above and below the median score.22
Intention to initiate RH discussion was measured using an adapted version of the larger RCT study’s “Initiating Discussion” questionnaire.23 Mothers self-reported their intention to initiate discussion with their daughters regarding RH issues. The measure contained 2 items with a 7-point Likert-type response scale with a score range of 2–14. The items were summed and the higher scores indicated greater intention to initiate discussion. Baseline scores of intention were dichotomized, using the median score of 13, into low and high for sampling purposes.
This study was approved by the University of Pittsburgh Institutional Review Board. Informed consent was obtained from mothers. To maintain confidentiality, transcripts were identified by the assigned subject identification number. Mothers were compensated $20 for their time.
Data Collection
The principal investigator (PI) conducted interviews via the telephone using a semi-structured interview guide that began with a “grand tour” question (e.g., “I’d like for you to tell me about discussing RH issues, such as monthly periods, sex, birth control or pregnancy with your daughter”). Additional questions probed the mother’s perceptions of who initiated discussions, timing of discussions, barriers and facilitators to discussions, and her comfort with initiation of discussion. There was no time limit to the interviews which generally lasted 20–30 minutes. Interviews were digitally recorded, transferred to a secure laptop, transcribed verbatim, and reviewed for accuracy. The interviews were conducted over a 1-year period of time, which began 2 years after mothers’ completion of the quantitative portion of this study.
Data Management and Statistical analysis
Qualitative content analysis techniques were used to analyze the interview data.18,24 The unit of analysis was sentences or paragraphs. A qualitative database program, ATLAS.ti v5.2 was used to facilitate organization and maintenance of the data. Analyses began with dual review of the first two transcripts with the PI (MH) and an experienced qualitative researcher (MBH). Initial codes were labeled and defined by consensus agreement among coders. For each of the next two interviews, these investigators coded the data separately, and then reviewed each coded transcript together. The last 6 interviews were coded by the PI and then reviewed by the methodological expert. Each interview was reviewed, discussed and consensus was reached on all coded data during analytic meetings. The code list and definitions were developed and refined with the coding of each interview. Comparisons were made within and across participant interviews during coding. Theoretical and methodological memoing24 techniques were also employed.
The following techniques were used to establish trustworthiness as described by Lincoln and Guba.25 Member checks were conducted by having two certified diabetes educators review and comment on the overall adequacy of this report. In addition, an audit trail that includes the digitally recorded interviews, verbatim transcripts, coding template, data analysis notes, and analytic memos was developed to establish credibility. Transferability was addressed with the use of purposive sampling and a thorough description of the context in which the interviews were carried out. Analysis by a second reviewer with expertise in qualitative analysis (MBH) enhanced rigor of the process and confirmability of findings.
Results
Ten mothers participated in interviews. Demographic characteristics of the mothers are presented in Table 3.
Table 3.
Demographic characteristics of mothers (n=10)
| Age (years) | 46.2 ± 3.2 |
| Ethnicity | |
| African-American | 1 (10) |
| Caucasian | 7 (70) |
| Missing | 2 (20) |
| Marital status | |
| Married | 9 (90) |
| Separated/divorced | 1 (10) |
| Education | |
| High school grad | 3 (30) |
| Attend some college | 1 (10) |
| College grad | 6 (60) |
| Employment | |
| Professional | 3 (30) |
| Skilled | 4 (40) |
| Unskilled | 2 (20) |
| Unemployed | 1 (10) |
| Religion | |
| Protestant | 4 (40) |
| Roman Catholic | 6 (60) |
| Mothers with Diabetes (n=2) | |
| Pregestational diabetes using insulin | 0 (0) |
| Post-gestational diabetes not using insulin | 1 (10) |
| Gestational diabetes only | 1 (10) |
Data are means ± SD and n (%).
The researchers identified the following 4 themes describing mothers’ perspectives of speaking with their adolescent daughters with diabetes about RH issues: 1) maternal awareness; 2) maternal knowledge; 3) triggers for initiating RH discussions; and, 4) maternal fears/concerns. Included is the number of respondents for which each theme applied to illustrate the thematic patterns and representativeness of the themes in the data.
Maternal Awareness
Maternal awareness refers to a mother’s awareness of her daughter’s sexual behavior and/or health risk with regard to diabetes and RH, such as experiencing an unplanned pregnancy. A recurrent pattern of awareness involved a daughter’s sexual activity or the possibility of her becoming sexually active (n=9). “She was growing up and I knew it was going to happen sooner or later.” “I don’t want to act like I’m stupid and that this girl is never going to have sex.” “I don’t believe she is sexually active, though you are never 100% sure.”
Mothers (n=8) were also aware of the risks of unplanned pregnancies in women with diabetes and verbalized support for the use of birth control by their daughters. “I think it is appropriate to tell people in this situation birth control is available and you’ve got to be using it.” “Since this study (larger RCT) she has been put on birth control because she was open enough with me to make me aware she was sexually active.” However, some mothers verbalized displeasure with their daughter’s decision to be sexually active. “She’s very open and honest with me so I can appreciate that, but you don’t like it.” “I was very disappointed it (sexual activity) did come.” Even if mothers were not pleased with the decisions of their daughters to be sexually active, they understood the need for protection. “I made her aware that even though she is on the pill she still needs to wear condoms because you still need to be cautious.” “I didn’t want to support it or promote that she have sex by putting her on the pill, but I didn’t want to be a stupid parent and act like just because I tell her don’t do that (have sex) she won’t do it.”
Maternal Knowledge
Maternal knowledge refers to a mother’s knowledge of diabetes and RH. Although specific complications were not mentioned, most mothers (n=8) seemed to have some general knowledge about the effects of diabetes on an unplanned pregnancy and that a pregnancy should be planned. “I don’t approve of her getting, having children right away because of the effects of diabetes and pregnancy.” “They (RCT intervention) told her that she had to get her sugar regulated, make sure it’s always in check months in advance and make sure her A1C level is steady months in advance.” “There’s example after example, of people we know who have had successful pregnancies because they were careful, they took care of themselves, they did the right thing in getting ready for it.” One mother mentioned abortion as an option to preserve her daughter’s health in the event of an unplanned pregnancy, “if it came to her health or terminating a pregnancy, I would have to say terminate the pregnancy as a recommendation, and I don’t want to ever have to do that.” On the other hand, one mother felt she did not have the correct knowledge and stated that the RCT intervention “explained it much better than I would of”.
Triggers to Initiating Reproductive Health Discussion
Triggers for initiating RH discussions are those instances that prompt mothers to talk with their daughters about these important issues. All 10 of the mothers used one or more types of triggers as prompts to begin talking with their daughters about RH. Some mothers (n=4) initiated discussion when their daughters were younger, others (n=6) when they were older.
One mother reported using her daughter’s questioning about why her adopted brother looked different as a starting point for talking about sex with her daughter, who was 3 years of age at the time of the discussion. Several (n=5) mothers reported using school or formal sex education classes as a trigger to begin RH discussions. “We attended a basic class together when she was probably in 5th or 6th grade … and that opened up the opportunity for us to just give her some basic information.”
They do have … sex education at school…I think the first year they do that is … the 6th grade … they discuss general body function of the reproductive organs, menstrual periods and things like that with the girls and that was always a big help to be a start for conversations at home.
Television programs were also used as triggers to begin discussions. One mother reported, “if there was something on TV … that generally would be one that would trigger conversations.”
We always watched television with them … so anytime something on television … one of those sitcoms or something that had innuendos we would always discuss, we could always say well do you have any thoughts on that?
Mother participation in phase 1 of this study and the daughters’ participation in the RCT triggered discussions between mothers and daughters. One mother reported “right after she took it (RCT questionnaires) we talked more about the questions that were on it … the questions sure sparked conversations.” Another mother reported using the one-on-one time in the car after participating in the study to talk with her daughter. “I think basically a lot of our conversations were on the way home … after she had answered questions or I had answered questions.” Mothers used ‘alone time,’ whether it was a long walk or a long car ride, or an evening out to dinner as an opportunity to talk with their daughters about their RH concerns.
Mothers reported using different triggers for older daughters. The most frequently reported impetus for mothers (n=5) to initiate discussions about preventing a pregnancy was a ‘steady boyfriend’. A steady boyfriend in their daughters’ lives triggered mothers to talk with their daughters about the risks that are involved with an unplanned pregnancy. One mother talked with her daughter and boyfriend together, “I actually sat down with both of them and so that he was totally aware of how the consequences of an unplanned pregnancy would be for her.” “We’ve talked a lot more about it since then (the RCT) because she’s had her first kind of boyfriend, sexual experience situation.” “Any time she’s had a boyfriend or anything like that we talk about those things.” Other mothers predicted that when a steady boyfriend comes “on the scene” or their daughters go to college they will talk with them at that time about the importance of preventing an unplanned pregnancy.
If she was graduating and/or there was someone significant on the scene, then I think that would be the time when I would do that. But right now her being on the pill I think it’s really sufficient.
I feel like we need to have a conversation before she goes off to college about what … how she is going to handle this … would she go to the college clinic for birth control or would she just not get herself into situations where she might you know, might be tempted.
Maternal fears
Mothers had many fears and concerns.
I think with diabetes, it’s something a mother never forgets..... her diabetes has been shall I say, a cross, that not only that I bear, but probably every parent of a child with diabetes carries the same cross, it’s something that never leaves you and something you have a fear about because even when your child gets a certain age you still have a fear that they are doing the right thing.
Maternal fears/concerns encompassed general health, diabetes associated complications and reproductive ability as well as unplanned pregnancies. Some of the teens are now attending college and mothers voiced concerns about college life. “I think I worry more about actually the drinking and maintaining control and diabetes.” Others verbalized concerns about their daughters smoking and about the ill effects of smoking with diabetes.
However, the majority of fears/concerns verbalized were those associated with RH issues, which was the focus of the study. One mother’s fear was that of the unknown, whether her daughter would be able to have children. She asked the doctor about childbearing when the diagnosis of diabetes was made, “even though she was only 10 years old, …I asked the doctor I said if [sic] she was going to be able to have a baby?”.
As the girls have grown older mothers have more fears and concerns about their daughters experiencing an unplanned pregnancy, as these mothers seem to know that women with diabetes should plan their pregnancies. Fears and concerns about unplanned pregnancies were expressed by 8 of the 10 mothers. “Right now we’re worried because she can’t be on the pill and we’re kind of grappling with what that might mean.” “I still worry that even though she’s still on the pill and using condoms that there could always still be that chance that she could get pregnant.”
Conclusion
This study is the first to explore mothers’ perspectives about RH of their adolescent girls with diabetes and their communication practices regarding these issues. From the 10 interviews conducted with mothers of adolescent girls with diabetes, the following themes were identified: maternal awareness, maternal knowledge, triggers for initiating RH discussion, and maternal fears/concerns. Overall, these mothers had initiated some discussion with their daughters about RH issues. Most of these mothers claimed to have been aware of their daughters’ sexual behavior or aware that they were at an age when they may become sexually active. Mothers also seemed to know that their daughters should plan a pregnancy and that preventing an unplanned pregnancy is very important for their daughters’ health. This coincides with the recommendations from the ADA 11 that women with diabetes need to plan their pregnancies.
There were many triggers that prompted mothers to talk with their daughters about RH issues. In early adolescence, sex education classes or something seen on television prompted a discussion. In later adolescence, a steady boyfriend was consistently reported as a trigger for mothers to begin discussing issues of RH. Specifically, mothers began to talk about birth control and the importance of preventing an unplanned pregnancy. They felt their daughters were susceptible to unplanned pregnancies. This is similar to findings of other studies conducted in the general population where it has been reported that mothers talked more with their adolescents about sex when they had greater perceived risks of their adolescents being exposed to the AIDS virus.26,27
Mothers, naturally, have many fears and concerns for the overall health and welfare of their children. During the interviews, mothers expressed fears and concerns for their daughters’ health. Most were associated with their daughters having an unplanned pregnancy. Mothers recognized that a higher risk for detrimental health effects is associated with an unplanned pregnancy in their daughters with diabetes. They reported that it was, however, sometimes difficult to discuss these issues with their daughters.
No studies have examined, from a mother’s perspective, RH communication between mothers and their adolescent daughters with or without diabetes. The majority of studies had examined whether sexual communication had taken place and whether there was agreement between parents and their adolescents as to what was discussed. No studies were found that reported on what triggers prompt mothers to discuss sexual information with their daughters. However, one study examined videotaped conversations between a mother and her daughter about AIDS.28 It was reported in this study of 21 dyads that the content of the AIDS conversations were focused around preventive measures and AIDS education and mothers were dominant in these conversations.
Limitations
Conducting the interviews via the telephone was a limitation due to the inability to capture the nonverbal language of the participant. However, to minimize this effect, the interviews were digitally recorded and tone deflections were noted as memos in the analyses. Another limitation was that the sample was from a small convenience sample embedded within a larger RCT study. However, criterion-related purposive sampling was used to enhance transferability of the findings. The last limitation to mention was that there was a 2 year time delay between participation in phase 1 of the mothers’ study and the interviews, which may have limited mothers’ recall. To minimize this potential threat to credibility, mothers were asked to think about conversations with their daughters at the age they were during study participation.
Implications
This study is unique in that it raises awareness of the importance of maternal involvement in RH discussions with adolescent daughters with diabetes. Diabetes nurse educators need to include mothers when discussing these very important issues with adolescents. Diabetes nurse educators can assist mothers in their RH discussions with their daughters by making sure that mothers have accurate RH information and effective communication skills. Mothers can be taught how to capitalize on ‘everyday triggers’ to initiate or resume conversations with their daughters. Nurse educators should recognize that despite available information and media references to sexual activity in popular culture, discussions between mothers and adolescent daughters are still difficult.
Future studies need to evaluate actual RH discussions between mothers and their adolescent daughters with diabetes. Intervention studies should include prospective description and evaluation of intervention effects on mother-daughter RH discussions and on the daughters’ RH behaviors, specifically those steps taken to prevent an unplanned pregnancy.
Acknowledgments
Financial Support: Sigma Theta Tau/American Association of Diabetes Educators Foundation Grant, Corinne M. Barnes Scholarship for Doctoral Studies in Nursing Care of Children, and American Diabetes Association Clinical Research Award
A special thank you to the 10 mothers who shared their thoughts and experiences of discussing some very sensitive issues with their daughters, and to Jean Roemer, RN, MSN, MN, CPNP, CDE and Maryilyn Clougherty, RN, MSN, CDE for their thoughtful reviews of this manuscript.
Contributor Information
Margaret Hannan, University of Pittsburgh, School of Nursing, Department of Health Promotion and Development, Pittsburgh, PA.
Mary Beth Happ, University of Pittsburgh, School of Nursing, Department of Acute/Tertiary Care, Pittsburgh, PA.
Denise Charron-Prochownik, University of Pittsburgh, School of Nursing, Department of Health Promotion and Development, Pittsburgh, PA.
References
- 1.Feldman SS, Elliott GR. At The Threshold: The Developing Adolescent. Cambridge, Massachusetts: Harvard University Press; 1997. [Google Scholar]
- 2.Wiener DE, Cohen MI. Challenges of delivering health care to adolescents. In: Hoekelman RA, editor. Primary Pediatric Care. 3. St. Louis: Mosby; 1997. [Google Scholar]
- 3.Grunbaum JA, Kann L, Kinchen S, et al. Youth Risk Behavior Surveillance -United States, 2003. MMWR Surveillance Summaries. 2004 May 21;53(No SS-2) [PubMed] [Google Scholar]
- 4.Charron-Prochownik D, Becker D, Sereika S, Ferons M, Reddinger J. Impact of a newly developed CD-ROM Reproductive Health Education Program on Teen Women with DM: 3-month f/u [Abstract] Diabetes. 2002;51(S2):A436. [Google Scholar]
- 5.Falsetti D, Charron-Prochownik D, Sereika SM, et al. Condom use, pregnancy, and STDs in adolescent females with and without type 1 diabetes. Diabetes Educator. 2003;29(1):135–143. doi: 10.1177/014572170302900118. [DOI] [PubMed] [Google Scholar]
- 6.Burns CE, Barber N, Brady M, Dunn A. Pediatric Primary Care: A Handbook for Nurse Practitioners. 1. Philadelphia: W.B. Saunders Company; 1996. [Google Scholar]
- 7.Abma JC, Martinez GM, Mosher WD, Dawson BS. Teenagers in the United States: Sexual activity, contraceptive use, and childbearing, 2002. National Center for Health Statistics. Vital Health Statistics. 2004;23(24) [PubMed] [Google Scholar]
- 8.Hamilton BE, Martin JA, Ventura SJ, Sutton PD, Menacker F. Births: Preliminary data for 2004. National vital statistics reports. 8. Vol. 54. Hyattsville, Maryland: National Center for Health Statistics; 2005. [PubMed] [Google Scholar]
- 9.Henshaw SK. Unintended pregnancy in the United States. Family Planning Perspectives. 1998;30(1):24, 29–46. [PubMed] [Google Scholar]
- 10.Porter L. Reducing teenage & unintended pregnancies through client centered & family focused school-based family planning programs. Journal of Pediatric Nursing. 1988;13:158–163. doi: 10.1016/S0882-5963(98)80074-2. [DOI] [PubMed] [Google Scholar]
- 11.American Diabetes Association. Standards of medical care in Diabetes - 2007. Diabetes Care. 2007;30(Supplement 1):S26–27. [Google Scholar]
- 12.Charron-Prochownik D, Becker D, Sereika S, Ferons M, Lockhart D, Cohen B. The impact of a newly developed CD-ROM reproductive health education program on teens with diabetes [Abstract] Diabetes. 2001;50(S2):A25. [Google Scholar]
- 13.Charron-Prochownik D, Sereika S, Becker D, et al. Reproductive health beliefs and behaviors in teens with diabetes: Application of the Expanded Health Belief Model. Pediatric Diabetes. 2001;2:30–39. doi: 10.1046/j.1399-543x.2001.00000.x. [DOI] [PubMed] [Google Scholar]
- 14.Anderson BJ, Brackett J, Ho J, Laffel LMB. An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Diabetes Care May. 1999;22(5):713–721. doi: 10.2337/diacare.22.5.713. [DOI] [PubMed] [Google Scholar]
- 15.Resnick MD, Bearman PS, Blum RW, et al. Protecting adolescents from harm: Findings from the National Longitudinal Study on adolescent health. JAMA. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 16.Whitaker DJ, Miller KS. Parent-adolescent discussions about sex and condoms: Impact on peer influences of sexual risk behavior. Journal of Adolescent Research. 2000;15(2):251–273. [Google Scholar]
- 17.Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications, Inc; 2007. [Google Scholar]
- 18.Sandelowski M. Focus on research methods: Whatever happened to qualitative description? Research in Nursing & Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 19.Charron-Prochownik D, Sereika SM, Hannan M, et al. Reproductive health education for adolescent girls with diabetes (READY-Girls): Sustaining long-range outcomes [Abstract] Diabetes. 2006;55(S1):1800-P. [Google Scholar]
- 20.Sandelowski M. Focus on research methods: Combining qualitative and quantitative sampling, data collection, and analysis techniques in mixed-methods studies. Research in Nursing and Health. 2000;23:246–255. doi: 10.1002/1098-240x(200006)23:3<246::aid-nur9>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 21.Wang S-L, Charron-Prochownik D, Sereika SM, Siminerio L, Kim Y. Comparing three theories in predicting reproductive health behavioral intention in adolescent women with diabetes. Pediatric Diabetes. 2006;7:108–115. doi: 10.1111/j.1399-543X.2006.00154.x. [DOI] [PubMed] [Google Scholar]
- 22.Glass GV, Hopkins KD. Statistical Methods in Education and Psychology. Boston: Allyn and Bacon; 1996. [Google Scholar]
- 23.Charron-Prochownik D, Wang S-L, Sereika SM, Kim Y, Janz NK. A theory-based reproductive health and diabetes instrument. American Journal of Health Behavior. 2006;30(2):208–220. doi: 10.5555/ajhb.2006.30.2.208. [DOI] [PubMed] [Google Scholar]
- 24.Miles MB, Huberman AM. Qualitative Data Analysis. 2. Thousand Oaks: Sage; 1994. [Google Scholar]
- 25.Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park: Sage Publications; 1985. [Google Scholar]
- 26.Miller KS, Whitaker DJ. Predictors of mother-adolescent discussions about condoms: Implications for providers who serve youth. Pediatrics. 2001;108:e28. doi: 10.1542/peds.108.2.e28. [DOI] [PubMed] [Google Scholar]
- 27.Romo LF, Lefkowitz ES, Sigman M, Au TK. Determinants of mother-adolescent communication about sex in Latino families. Adolescent & Family Health. 2001;2(2):72–82. [Google Scholar]
- 28.Lefkowitz ES, Kahlbaugh P, Kit-fong Au T, Sigman M. A longitudinal study of aids conversations between mothers and adolescents. AIDS Education and Prevention. 1998;10(4):351–365. [PubMed] [Google Scholar]