Abstract
Participants’ personal condom use measures and those of their last sex partner’s were examined in five stages of change for consistent condom use among 449 urban sexually active, heterosexual, African–American crack smokers. The measures included participants’ personal and their last sex partner’s perceived responsibility, personal and perceived negative attitudes, and participants’ self-efficacy to use condoms. The relationships between the measures and the stages were examined using analyses of variance and multivariate logistic regression. Over 90% of participants did not use condoms, consistently. Two-thirds of the inconsistent users were in the precontemplation stage. The rest were equally divided between the contemplation and preparation stages. Personal responsibility outperformed other measures in initial intention to become a regular condom user; partner’s perceived responsibility dominated continued intention and actual consistent condom use. Negative attitudes and self-efficacies had strong relationships to the stages of consistent condom use in univariate analyses but these relationships became substantially weaker when the responsibility, attitude, and self-efficacy concepts were entered simultaneously into multivariate analyses.
The prevalence of HIV and AIDS remains high, particularly among heterosexual, non-Hispanic, black men and women (CDC, 2006; Dean et al., 2005). Less than half of heterosexuals who have multiple sex partners are regular condom users (Anderson, 2003; Anderson et al., 1999; Celentano, 2004). Crack cocaine (powder cocaine transformed into a sold form) smokers are at a particularly high risk because crack smoking is associated with a number of social and behavioural HIV infection risk factors. Many crack smokers also reside in poor, bounded inner city neighbourhoods, in which the prevalence of sexually transmitted infections is high (Adimora et al., 2003; Baseman et al., 1999). Crack smokers are less likely than other drug users to use condoms (Booth et al., 2000; Timpson et al., 2003) but engage more in unprotected vaginal sex with multiple partners (Brunswick & Flory, 1998; Riehmann et al., 1998; Ross et al., 1999; Wingood & DiClemente, 1998).
Numerous cognitive-behavioural theories and models have been applied to explain condom use in at-risk populations, including the theory of planned behaviour (TPB; Ajzen, 1991), social cognitive theory (SCT; Bandura, 2004, 1998, 1986), and the transtheoretical model (TTM; Prochaska & DiClemente, 1984). These frameworks share many constructs, such as attitude, self-efficacy and behavioural intention (Kasprzyk et al., 1998), but also have their own unique constructs. For example, condom use subjective norms are included in the TPB, but there are no equivalents in the TTM which, unlike the TPB or SCT, stipulate that a behaviour change takes place in discrete ‘stages’ of change, from resistance to change to intention to change which results in an overt behaviour change (Prochaska & DiClemente, 1984).
Adding new or alternative constructs is one way to improve the explanatory power of existing theories and models. According to Ajzen (1991), one of these constructs is personal norms which, to date, have received little attention in HIV-prevention research. Personal norms are an individual’s perception of the ethical correctness of performing a behaviour. Unlike different forms of social norms, personal norms are based on self-standards and are used to identify internalized cognitive processes that are based on a personal sense of right and wrong. Manstead (2000) claims that personal norms operate independently from social consequences and have strong anticipated affective outcomes on a behaviour. An example of a statement reflecting a personal norm is, ‘The responsible thing to do is …’ which was clearly the most commonly endorsed response when heterosexual men who have multiple partners have been asked about positive outcomes of condom use (Fishbein et al., 2001). A part of personal norms is personal responsibility to perform (or not to perform) a behavior (Ajzen, 1991; Cialdini et al., 1991; Conner & Armitage, 1998).
In addition to introducing the condom use responsibility construct, this study also addressed the dyadic nature of condom use. This is often a neglected feature in current predominant behaviour change models. Condom use is not enacted in isolation but, it is influenced by the sex partner (Catania et al., 1990).
The first aim of this paper was to describe and explain, with using univariate analyses, how African–American crack cocaine smokers’ and their partners’ condom use attitudes and responsibilities, as well as, participants’ self-efficacy, were related to stages of change for consistent condom use. The second aim was to assess, simultaneously, how the selected constructs were related to each other, across the stages of change.
Methods
Recruitment
Participants were heterosexual African–American crack cocaine users from two inner-city neighbourhoods in Houston, Texas. All data collection procedures and instruments for the study were reviewed and approved by the university committee for the protection of human subjects. Recruitment, between February 2003 and March 2005, involved a combination of targeted sampling and participant referrals (Booth et al., 1993; Watters & Biernacki, 1989). Recruiters briefly described the study, provided condoms, and study-related printed materials. Interested respondents were asked to visit one of two neighbourhood offices, which were manned by trained, research assistants who also were experienced in collecting data from crack smokers.
Prior to obtaining interested respondents verbal consent for an initial screening, the purpose and voluntary nature of the study were explained. Consenting respondents completed a brief questionnaire about their eligibility. Only 18 to 40 year old, African–Americans who reported having smoked crack in the past 48 hours, had vaginal sex in the past seven days, resided in one of the neighbourhoods targeted for recruitment, and who provided sufficient contact information for follow-up interviews, were recruited. If an individual met eligibility criteria, they were asked to provide a urine specimen to test for cocaine metabolites. Those who were not cocaine users, according to OnTrack TesTstik® test (Varian, Inc., Lake Forest, CA), were asked to defer participation until a later time. Individuals, for whom the test categorized them as current cocaine users, were provided a detailed explanation of the study, in writing, and asked for written informed consent. Consenting individuals were scheduled for a private computer-aided interview at the same office. At the end of the interview, participants received a compensation of $25.
Participant characteristics
All 496 recruited participants were heterosexual, African–Americans whose mean age was 33 years (sd = 5.8). Most were men (63%), single (81%), and less than a fifth (18%) were married or lived with a partner of the opposite sex. The average number of years of schooling was 11 years (sd = 1.7). Almost half of the participants (48%) were unemployed. The three most common sources of income, among those who earned money, were a full-time job (28%), trading sex for money (17%), and working at odd jobs (15%). Participants’ median income, in the last 30 days, was between $200 and $400. A quarter (26%) regarded themselves as homeless and 2% lived on the streets. A full 54% of participants had smoked crack cocaine, at least daily, during the past 30 days and the majority (58%) reported having been in drug treatment, at least once. The two most commonly reported sexual relationships were having a main and casual partner (47%) and having only a causal partner (41%). In the past 30 days, the mean of sex encounters was 22.7 times (sd = 18.6). The average number of different sex partners was 7.9 (sd = 8.6).
Condom use measures
Measurement of condom use was limited to the use of male condoms, during vaginal sex, with last partner. Only 2% of participants reported ever using a female condom with their last partner, in the seven days before the interview. To aid participants to recall their sexual events, the last partner was chosen as a reference (Brewer et al., 1999). Interviewers elicited information about him/her by first asking the participant to provide the partner’s first name and then referred to the partner by name for all subsequent questions.
Stages of consistent condom use with the last partner
As in previous studies (Brown-Peterside et al., 2000; Noar et al., 2002; Ross et al., 2003; Schnell et al., 1996), a stage of change algorithm for condom use stages was based on three questions about intentions, and current and past condom use frequency during vaginal sex. 1) Intentions to start using condoms, in the next six months, or in the next 30 days, were measured on a 10-point Likert scale, varying from 1 (strongly disagree) to 10 (strongly agree). Values 1 to 5 indicated lack of intention and values 6 to 10 indicated intention. 2) Response alternatives about the current frequency of condom use varied from 0 (never) to 4 (always). 3) A question about the length of past consistent condom use had four categories (0 = <1 month, 1 = 1–3 months, 2 = 3–5, and 3 = ≥6 months). The algorithm based on the three questions produced five stages of consistent condom use.
In the precontemplation (PC) stage, respondents did not always use condoms and had no intention to do so, in the next six months. The contemplation (C) stage included those who intended to always use condoms, in the next six months, but not in the next 30 days. In the preparation (P) stage, respondents intended to always use condoms, in the next 30 days. However, if participants only intended, but had not used condoms, previously, at least some of the time with the last partner, they were classified into the C stage. The action (A) stage was defined as always using condoms, for less than six months. The maintenance (M) stage was defined as always using condoms for six months or more. Additionally, participants in the A and M stages had used a condom during their last sexual intercourse with their last partner.
Independent constructs
Questions assessed each of the six multi-item, independent, theoretical constructs on the 10-point Likert scale. These were first examined using a principal axis factor analysis with direct oblique rotation and a principal component analysis, with Varimax rotation (Gorsuch, 1980). The scree test (Gorsuch, 1980) showed that both factoring methods extracted an identical number of factors for each construct. Items, which reduced the internal consistency (Cronbach’s coefficient α) of a scale, were eliminated. The independence of the final six measures was confirmed by entering their items, simultaneously, into the principal axis factor and the principal component analyses. Both analyses produced six stable and independent factors. Their items were identical to those obtained in separate construct-by-construct analyses.
Personal responsibility for condom use
Three similar questions (range: 1 = strongly disagree, 10 = strongly agree) were used to assess both participants’ personal responsibility and their perceptions about the level of their last sex partners’ responsibility to use condoms. Questions in the respondents’ personal condom use responsibility measure (M = 5.5, α = .86) were: ‘I think we should use a condom when we have sex’, ‘I think it is my responsibility to be sure that we use condoms’, and “I think we should use a condom every time we have sex.’
The items for the perceived partner condom use responsibility measure (M = 3.7, α = 0.89) included: ‘My last partner thinks we should use a condom when we have sex’, ‘My last partner thinks it is his/her responsibility to be sure we use condoms’, and ‘My last partner thinks we should use a condom every time we have sex.’
Condom use attitudes
Eight questions (range: 1 = strongly disagree, 10 = strongly agree) were used to assess the participants’ negative attitude (M = 6.2; α = .93) and their perceived partner’s negative attitude (M = 6.2; α = 0.97). All items measured negative attitude towards condoms, such as, ‘Condoms are a lot of trouble’, ‘Condoms interrupt the flow of sex’, and ‘Condoms make sex less exciting.’ The stems of questions that elicited the respondents’ perceptions of the partner’s attitude were phrased as ‘How much do you think [partner’s name] agrees or disagrees that …’
Condom use self-efficacies
The participants’ self-efficacy constructs covered both efficacy and outcome expectations (Bandura, 2004). Five questions (range: 1 = not at all confident, 10 = very confident) of the personal performance self-efficacy measure (M = 6.9; α = 0.91) focused on the respondent’s confidence in their ability to make sex with a condom intimate, exciting, fun, romantic, and to communicate about condom use.
Personal situational self-efficacy measure
Situational self-efficacy measure (M = 4.7, α = 0.96) included 15 questions which assessed respondents’ confidence (range: 1 = not at all confident, 10 = very confident) to use condoms in various partner situations (cf. Velicer et al., 1990). Situations included alcohol use (e.g. ‘When you have had a couple of drinks’), emotional involvement with last partner (e.g. ‘When you feel really close to him/her’), and sexual arousal (e.g. ‘When you are really turned on’).
Analysis
Co-variation between the stages of consistent condom use or their combinations, and the responsibility, attitude and self-efficacy measures were first examined in univariate two-way analyses of variance. In addition to stage, gender was entered as another fixed effect because of reported sex differences in condom use (Timpson et al., 2001; Wingood & DiClemente, 1998). If an overall stage effect was significant (p < .05), mean differences between stage and its adjacent stage were tested with Scheffé’s a posterior test (p < .05). The proportion of the variance explained was quantified with Nagelkerke’s R2.
The simultaneous effects of independent participant and partner measures on stage, (or their combinations), differences were assessed with a series of unadjusted multivariate logistic analyses. Stage-related differences in independent measures were assessed with odds ratios, (OR), their 95% confidence intervals (95% CI), and the Wald test. The proportion of the variance the stages explained was estimated using Nagelkerke’s R2. Independent measures were converted into T-scores (M = 50, sd = 10) to make the measures comparable. The main comparisons took place: 1) between inconsistent and consistent condom users; 2): between condom use non-intenders, intenders and consistent users; and 3) between the four stages (PC, C, P, and A + M). Only variables with significant ORs were considered. The A and M stages were merged to maintain an adequate sample size and because univariate analyses revealed, only minimal differences between these two stages.
Results
Stages of change for consistent condom use
The stages of consistent condom use were defined for 449 respondents or 91% of all 496 participants and formed the final study population of this paper. The majority, or 66% of the participants, was in the PC stage for consistent condom use. Thirteen percent was in the C stage and 14% in the P stage. Less than 10% was consistent condom users; 3% was in the A and 5% in the M stage. No significant sex differences emerged, χ2(4, N = 449) = 3.0, p = .57.
We examined differences between the 449 participants and 47 excluded participants whose stages of consistent condom use could not be defined. The groups were similar in sociodemographic characteristics and frequency of vaginal sex. The excluded were, however, significantly less likely to have a main sex partner than the retained (28% vs. 58%, p < .001).
Condon use responsibility by stage
The means of the participants’ personal responsibility [F(4, 439) = 62.2, p < .001)] (Figure 1) and their perceived partner responsibility [(F(4, 438) = 51.2, p < .001)] (Figure 2) for condom use increased significantly across the stages in both sexes. The stages explained 39% of the variance of the participants’ responsibility and 33% of the partner responsibility measures.
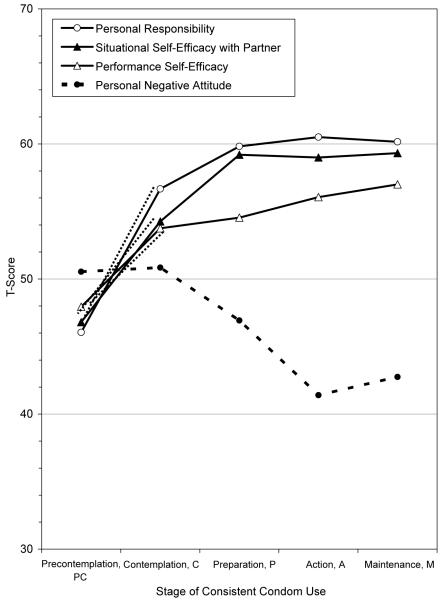
Figure 1.
T-score means of the personal negative attitude, personal situational self-efficacy, personal performance self-efficacy, and personal responsibility about condom use measures in five stages of consistent condom use.
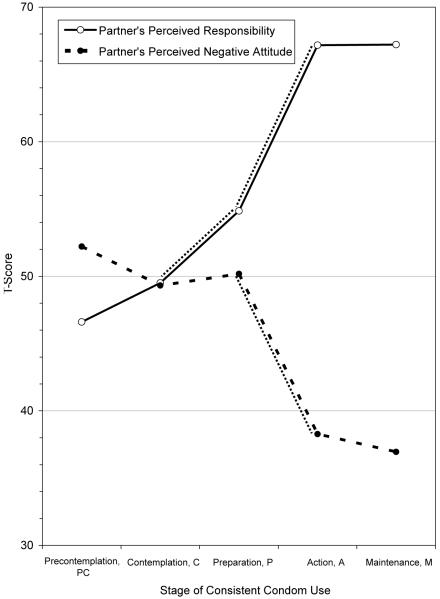
Figure 2.
T-score means of the perceived partner negative attitude and responsibility about condom use measures in five stages of consistent condom use.
A broken add-on line in Figure 1 indicated significant differences in means between the PC and C stages of the personal responsibility measure in a stage to adjacent stage comparison. A broken add-on line in Figure 2 specified significant mean differences between the C and P stages and between the P and A stages.
Negative attitudes by stage
Both participants’ personal negative attitude (Figure 1) [(F(4, 439) = 6.9, p < .001)] and their partner’s perceived negative attitude (Figure 2) [(F(4, 439) = 18.7, p < .001)] towards condom use significantly decreased with stage progression. Stages explained 10% of the variance of participant attitude and 15% of the variance in partner attitude. The reduction was similar for males and females. The only significant stage to adjacent stage difference emerged in partner’s negative attitude between the P and A stages (Figure 2).
Participants’ self-efficacies by stage
Both participants’ personal performance self-efficacy [(F(4, 439) = 14.0, p < .001] and personal situational self-efficacy with partner measures [(F(4, 439) = 37.6, p < .001] demonstrated in Figure 1 similar significant stage to adjacent stage relationships. The only significant increases in stage means occurred between the PC and C stages. Stages accounted twice as much for the situational self-efficacy variance (28%) than for the performance self-efficacy variance (12%).
Group comparisons
Inconsistent vs. consistent condom users
In a comparison of inconsistent with consistent condom users (i.e., PC, C, or P stages vs. the A or M stages) in Table I, independent participant and last partner variables together accounted for 65% of the contrast variance.
Table I.
Odds ratios (OR) and their 95% confidence intervals (CI) for the significant cognitive measures by the Wald test ranking between inconsistent and consistent condom users
| Inconsistent Condom Users (PC, C, or P Stages, N = 415) |
⇨ | Consistent Condom Users (A or M Stages, N = 33) |
|---|---|---|
| OR (95% CI) | ||
| Partner’s Responsibility | 1.20 (1.11–1.30) | |
| Partner’s Negative Attitude | .89 (.82–.96) | |
Two partner measures, his/her perceived condom use responsibility, increased 20% of consistent condom use (OR = 1.20) and his/her perceived negative condom use attitude decreased consistent condom use by 12% (OR = .88).
Non-intenders vs. intenders
In a contrast between those inconsistent condom users who did not intend to use condoms consistently (the PC stage) and intenders who were planning to start using condoms consistently (the C or P stages) (see the left side of Table II), independent variables accounted for 52% of the variance in condom use intentions. Only participant measures emerged significant. Intenders reported 16% higher personal condom use responsibility, 8% higher personal situational self-efficacy, and 5% higher personal negative attitude than non-intenders.
Table II.
Odds ratios (OR) and their 95% confidence intervals (CI) for the significant cognitive measures by the Wald test ranking between (1) non-intenders and intenders of consistent condom users and between (2) intenders and consistent condom users
| Non-Intenders (PC Stage, N = 294) |
⇨ | Intenders (C or P Stages, N = 121) |
Intenders (C or P Stages, N = 121) |
⇨ | Consistent Users (A or M Stages, N = 33) |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | ||||
| Personal Responsibility | 1.16 (1.12–1.22) | Partner’s Responsibility | 1.20 (1.10–1.31) | ||
| Personal Situational Self-Efficacy | 1.08 (1.04–1.12) | Partner’s Negative Attitude | .90 (.83–.98) | ||
| Personal Negative Attitude | 1.05 (1.01–1.08) | ||||
The second contrast (the right side of Table II) compared the condom use intenders (the C or P stages) with consistent condom users (A or M stages) and explained 63% of the variance. At this time, partner measures alone were significant discriminators. Consistent condom users reported 20% higher perceived partner responsibility and experienced 11% lower negative partner attitude than the intenders.
Stage-by-stage comparison
Table III compared differences between the PC, C, P, and the merged A or M stages.
Table III.
Odds ratios (OR) and their 95% confidence intervals (CI) for the significant cognitive measures by the Wald test ranking between the four stages of consistent condom use
| Precontemplation PC (N = 294) |
⇨ | Contemplation C (N = 58) |
Contemplation C (N = 58) |
⇨ | Preparation P (N = 63) |
Preparation P (N = 63) |
⇨ | Action or Maintenance A or M (N = 33) |
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | ||||||
| Personal Responsibility |
1.15 (1.10–1.20) | Partner’s Responsibility |
1.08 (1.02–1.13) | Partner’s Responsibility |
1.21 (1.08–1.35) | |||
| Personal Negative Attitude |
1.06 (1.02–1.10) | Personal Negative Attitude |
.93 (.88–.99) | Partner’s Negative Attitude |
.88 (.80–.97) | |||
| Personal Situational Self-Efficacy |
1.06 (1.02–1.10) | |||||||
In the PC vs. C stage comparison, the independent measures explained 37% of the stage change variance. Only a participant’s personal measures discriminated the stages. Respondents in the C stage reported 15% higher personal responsibility, 6% higher personal negative attitude, and 6% higher personal situational self-efficacy.
In the C vs. P stage comparison, the independent measures accounted for 26% of the variance. One participant and one partner measure were equally important. Those in the P stage reported 8% higher perceived partner responsibility and 8% lower personal negative attitude related to consistent condom use.
The final P vs. A or M stages comparison explained 64% of the variance and involved two partner measures. Partner responsibility in the A or M stages was 21% higher and partner’s negative attitude were 13% lower than in the P stage.
Discussion
Less than one-tenth of the 449 African–American crack cocaine smokers in our study used condoms consistently with their last sex partner; two-thirds had no intention to do so. To shine a light on this important public health problem, we examined what role responsibility played between condom non-users and users in different stages of change for consistent condom use, in addition to well-established attitudes and self-efficacy concepts. Dyadic influences associated with condom use were measured by comparing respondents’ personal attitude, self-efficacies and responsibilities to use condoms with respondents’ perceptions about their partner’s attitude and responsibilities. Reliance on partner perception information eliminated a tedious process of tracking down each respondent’s partner for an interview or survey in our hard-to-reach study population. Another advantage of the indirect data collection was that perceptions are based on both verbal and non-verbal communication which is likely to assess more accurately the nature of the condom use decisions, especially when communication between sex partners is limited.
Personal responsibility
Personal responsibility to use condoms best explained early intentions for consistent condom use while perceived partner responsibility dominated the rest of stage-to-stage transitions. This finding lends support to a suggested distinction between different types of responsibilities. For instance, Wolitski et al. (2003) separated respondent, partner, and mutual responsibilities. The observed high significance of responsibility also, could be due to its multi-item assessment to circumvent a previously reported problem of relying on a single-item measure which may have marred previous studies (Armitage & Conner, 2001; Conner & Armitage, 1998). Additional research, on the role of responsibility in determining condom use (Boyd & Wandersman, 1991; Conner & Armitage, 1998; Godin et al., 1996; Morrison-Beedy et al., 2002; Raats et al., 1995; Sagrestano et al., 2005) is much warranted, especially because the concept explained most condom use variance both in univariate and multivariate analyses. However, the examined responsibility concept accounted for no more than 20% of the variance. This calls for more refined conceptual research, which distinguishes, as suggested (Conner & Armitage, 1998; Manstead, 2000; Parker et al., 1995; Raats et al., 1995) social, normative, personal, and moral aspects of responsibility.
Attitude and self-efficacy concepts
Multivariate analyses on negative attitudes and self-efficacy explained a modest amount of condom use variance compared to the responsibility measure. Most of our observations parallel earlier findings about the importance of reduced negative partner attitude concerning achieving consistent condom use (Ross et al., 2003), with one exception. Participants, who contemplated consistent condom use in the C stage, reported somewhat greater negative attitude about regular condom use than precontemplators. We speculate that this finding reflects inconveniences related to starting using condoms during every sex act.
Both efficacy expectations (personal situational self-efficacy with last partner) and outcome expectations (personal performance self-efficacy) are pivotal parts of the SCT (Bandura, 1986). The concepts, especially situational self-efficacy, had strong positive relationships with stages, but only in univariate analyses. One explanation for the lack of similar effects in multivariate analyses was a shared variance between the self-efficacy and responsibility measures as indicated by their high intercorrelations.
Limitations
A major caveat in interpreting these findings is their reliance on cross-sectional data which excluded examination of causal inferences and potential variation in the assessed variables over time. Use of targeted sampling and participant referral sampling methods prohibited accurate estimates on how well these results generalized to other populations. On the other hand, these sampling methods are often the only feasible methods of collecting a representative sample with hidden and elusive populations, for which there are no a priori information. The relatively small number of consistent condom users in the sample made comparisons between the short- and long-term condom uses unstable. Some researchers have also questioned the accuracy of self-reported condom use (de Visser & Smith, 2000; Turner & Miller, 1997; Weir et al., 1999) while others (Ajzen & Fishbein, 2004; Jaccard et al., 2002) have found self-reports reasonably accurate. Furthermore, in most cases, self-reports remain one of a few feasible data collection method alternatives for direct assessments (e.g. observing) of intimate sexual behaviours.
Conclusions
Consistent condom use was rare and most participants were not planning to become consistent condom users. The most apparent pattern emerging from this cross-sectional study on the relationships, between the consistent condom use stages and their cognitive covariates, was a shift in influence in both sexes, from the respondent measures, at the very beginning of the stage continuum when respondents started to think about the possibility of using condoms consistently, to partner measures when consistent condom use became a firm decision. If these findings replicate in longitudinal studies, condom use promotion interventions need increasingly to emphasize dyadic aspects of condom use.
Acknowledgements
Research reported in this manuscript was supported by a grant from the National Institute on Drug Abuse, R01 DA14519 (PI: Mark L Williams).
References
- Adimora A, Schoenbach V, Martinson F, Donaldson K, Stancil T, Fullilove R. Concurrent partnerships among rural African Americans with recently reported heterosexually transmitted HIV infection. Journal of Acquired Immune Deficiency Syndromes. 2003;34:423–29. doi: 10.1097/00126334-200312010-00010. [DOI] [PubMed] [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Ajzen I, Fishbein M. Questions raised by a reasoned action approach: Comments on Ogden (2003) Health Psychology. 2004;23:431–34. doi: 10.1037/0278-6133.23.4.431. [DOI] [PubMed] [Google Scholar]
- Anderson JE. Condom use and HIV risk among US Adults. American Journal of Public Health. 2003;93:912–14. doi: 10.2105/ajph.93.6.912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson JE, Wilson R, Doll L, Jones S, Baker P. Condom use and HIV risk behaviors among U.S. adults: Data from a national survey. Family Planning Perspective. 1999;31:24–28. [PubMed] [Google Scholar]
- Armitage C, Conner M. Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology. 2001;40:471–99. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology and Health. 1998;13:623–49. [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. 1st ed. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Baseman J, Ross M, Williams M. Sale of sex for drugs and drugs for sex: An economic context of sexual risk behavior for STDs. Sexually Transmitted Diseases. 1999;26:444–49. doi: 10.1097/00007435-199909000-00005. [DOI] [PubMed] [Google Scholar]
- Booth RE, Kwiatkowski CF, Chitwood DD. Sex related HIV risk behaviors: Differential risks among injection drug users, crack smokers, and injection drug users who smoke crack. Drug and Alcohol Dependence. 2000;58:219–26. doi: 10.1016/s0376-8716(99)00094-0. [DOI] [PubMed] [Google Scholar]
- Booth R, Watters J, Chitwood D. HIV risk-related sex behaviors among injection drug users, crack smokers, and injection drug users who smoke crack. American Journal of Public Health. 1993;83:1144–48. doi: 10.2105/ajph.83.8.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd B, Wandersman A. Predicting undergraduate condom use with the Fishbein and Ajzen and the Triandis attitude-behavior models: Implications for public health interventions. Journal of Applied Psychology. 1991;21:1810–30. [Google Scholar]
- Brewer D, Garrett S, Kulasingam S. Forgetting as a cause of incomplete reporting of sexual and drug injection partners. Sexually Transmitted Diseases. 1999;26:166–76. doi: 10.1097/00007435-199903000-00008. [DOI] [PubMed] [Google Scholar]
- Brown-Peterside P, Redding C, Ren R, Koblin B. Acceptability of a stage-matched expert system intervention to increase condom use among women at high risk of HIV infection in New York City. AIDS Education and Prevention. 2000;12:171–81. [PubMed] [Google Scholar]
- Brunswick AF, Flory MJ. Changing HIV infection rates and risk in an African-American community cohort. AIDS CARE. 1998;10:267–81. doi: 10.1080/713612411. [DOI] [PubMed] [Google Scholar]
- Celentano DD. It’s all in the measurement: Consistent condom use is effective in preventing sexually transmitted infections. Sexually Transmitted Diseases. 2004;31:161–62. doi: 10.1097/01.olq.0000117589.12564.1b. [DOI] [PubMed] [Google Scholar]
- Catania J, Kegeles S, Coates T. Towards an understanding of risk behavior: An AIDS risk reduction model (ARRM) Health Education Quarterly. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention) HIV/AIDS surveillance report: Cases of HIV infection and AIDS in the United States and dependent areas, 2005. Vol. 17. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta: 2006. [Google Scholar]
- Cialdini R, Kallgren C, Reno R. A focus theory of normative conduct: A theoretical refinement and reevaluation of the role of norms in human behavior. Advances in Experimental Social Psychology. 1991;24:201–34. [Google Scholar]
- Conner M, Armitage C. Extending the theory of planned behavior: A review and avenues for further research. Journal of Applied Social Psychology. 1998;28:1429–64. [Google Scholar]
- Dean HD, Steele CB, Satcher AJ, Nakashima AK. HIV/AIDS among minority races and ethnicities in the United States, 1999–2003. Journal of the National Medical Association. 2005;97:5S–12S. [PMC free article] [PubMed] [Google Scholar]
- de Visser R, Smith M. When always isn’t enough: Implications of the late application of condom for the validity and reliability of self-reported condom use. AIDS Care. 2000;12:221–24. doi: 10.1080/09540120050001904. [DOI] [PubMed] [Google Scholar]
- Fishbein M, von Haeften I, Appleyard J. The role of theory in developing effective interventions: Implications from project SAFER. Psychology. Health & Medicine. 2001;6:223–38. [Google Scholar]
- Godin G, Maticka-Tyndale E, Adrien A, Manson-Singer S, Williams D, Cappon P. Cross-cultural testing of three social cognitive theories: An application to condom use. Journal of Applied Social Psychology. 1996;26:1556–86. [Google Scholar]
- Gorsuch RL. Factor analysis. 2nd ed. Lawrence Erlbaum; Hillsdale, NJ: 1980. [Google Scholar]
- Jaccard J, McDonald R, Wan CK, Dittus PJ, Quinlan S. The accuracy of self-reports of condom use and sexual behavior. Journal of Applied Psychology. 2002;32:1863–1905. [Google Scholar]
- Kasprzyk D, Montano DE, Fishbein M. Application of an integrated behavioral model to predict condom use: A prospective study among high HIV risk groups. Journal of Applied Social Psychology. 1998;28:1557–83. [Google Scholar]
- Manstead A. The role of moral norm in the attitude-behavior relation. In: Terry D, Hogg M, editors. Attitudes, behavior, and social context: The role of norms and group membership. Lawrence Erlbaum Associates, Publishers; Mahwah, N.J: 2000. pp. 11–30. [Google Scholar]
- Morrison-Beedy D, Carey M, Lewis B. Modeling condom-use stage of change in low-income, single, urban women. Research in Nursing & Health. 2002;25:122–34. doi: 10.1002/nur.10026. [DOI] [PubMed] [Google Scholar]
- Noar S, Morokoff P, Redding C. Sexual assertiveness in heterosexually active men: A test of three samples. AIDS Education and Prevention. 2002;14:330–42. doi: 10.1521/aeap.14.5.330.23872. [DOI] [PubMed] [Google Scholar]
- Parker D, Manstead A, Stradling S. Extending the theory of planned behaviour: The role of personal norm. British Journal of Social Psychology. 1995;34:127–37. [Google Scholar]
- Prochaska J, DiClemente C. The transtheoretical approach. Dow-Jones-Irwin; Homewood, Il: 1984. [Google Scholar]
- Raats M, Shephard R, Sparks P. Including moral dimensions of choice with the structure of the theory of planned behavior. Journal of Applied Social Psychology. 1995;25:484–94. [Google Scholar]
- Riehmann K, Sly D, Soler H, Eberstein I, Quadagno D, Harrison D. Dual-methods use among an ethnically diverse group of women at risk of HIV infection. Family Planning Perspectives. 1998;30:212–16. [PubMed] [Google Scholar]
- Ross L, Kohler C, Grimley D, Bellis J. Intention to use condoms among three low-income, urban African American subgroups: cocaine users, noncocaine drug users, and nondrug users. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2003;80:147–60. doi: 10.1093/jurban/jtg147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross M, Hwang L, Leonard L, Teng M, Duncan L. Sexual behavior, STDs, and crack cocaine use in a crack house population. International Journal of STD and AIDS. 1999;10:224–30. doi: 10.1258/0956462991913989. [DOI] [PubMed] [Google Scholar]
- Ross M, Timpson S, Williams M, Bowen A. Situational correlates of condom use in a sample of African American drug users who are primarily crack cocaine users. AIDS and Behavior. 2003;7:55–60. doi: 10.1023/a:1022561423599. [DOI] [PubMed] [Google Scholar]
- Sagrestano LM, Rogers A, Kittleson MJ, Sarvela PD. Does efficacy mediate stage of change and condom use in injected-drug users? American Journal of Health Behavior. 2005;29:12–24. doi: 10.5993/ajhb.29.1.2. [DOI] [PubMed] [Google Scholar]
- Schnell D, Galavotti C, Fishbein M, Chan D, AIDS Community Demonstration Projects Measuring the adoption of consistent use of condoms using the stage of change model. Public Health Reports. 1996;111(Supp. 1):59–68. [PMC free article] [PubMed] [Google Scholar]
- Timpson S, Pollack K, Bowen A, Williams M, Ross M, McCoy C, McCoy H. Gender differences in processes of change for condom use: Patterns across stages of change in crack cocaine users. Health Education Research. 2001;16:541–53. doi: 10.1093/her/16.5.541. [DOI] [PubMed] [Google Scholar]
- Timpson SC, Williams ML, Bowen AM, Keel KB. Condom use behavior in HIV-infected African crack cocaine users. Substance Abuse. 2003;24:211–20. doi: 10.1023/a:1026043529583. [DOI] [PubMed] [Google Scholar]
- Turner C, Miller H. Zenilman’s anomaly reconsidered: Fallible reports, ceteris paribus, and other hypotheses. Sexually Transmitted Diseases. 1997;24:522–27. doi: 10.1097/00007435-199710000-00005. [DOI] [PubMed] [Google Scholar]
- Velicer WF, DiClemente CC, Rossi JS, Prochaska JO. Relapse situations and self-efficacy: An integrative model. Addictive Behaviors. 1990;15:271–83. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- Watters J, Biernacki P. Targeted sampling: Options for the study of hidden populations. Social Problems. 1989;36:416–30. [Google Scholar]
- Weir SS, Roddy RE, Zekeng L, Ryan KA. Associations between condom use and HIV infection: A randomized study of self reported condom use measures. Journal of Epidemiological Community Health. 1999;53:417–22. doi: 10.1136/jech.53.7.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood G, DiClemente R. Partner influences and gender-related factors associated with noncondom use among young adult African American women. American Journal of Community Psychology. 1998;26:29–51. doi: 10.1023/a:1021830023545. [DOI] [PubMed] [Google Scholar]
- Wolitski RJ, Bailey CJ, O’Leary A, Gomez C, Parsons JT. Self-perceived responsibility of HIV-seropositive men who have sex with men for preventing HIV transmission. AIDS and Behavior. 2003;7:363–72. doi: 10.1023/b:aibe.0000004728.73443.32. [DOI] [PubMed] [Google Scholar]