Abstract
The purpose of this study was to investigate the unique contribution of a personal norm of condom-use responsibility to the formation of intentions to use male condoms during vaginal sex. Data were collected from 402 male and 157 female heterosexual African American crack cocaine smokers in Houston, Texas, US. Two structural equation models of the intention to use a condom with the last sex partner were estimated. One model included measures of condom-use attitudes, subjective norms and condom-use self-efficacy. A second model included these three measures and a fourth measure of a personal norm of condom-use responsibility. Separate models were estimated for men and women. The addition of a personal norm of condom-use responsibility provided a significantly better fit to the data than did models including only outcome expectations, subjective norms and self-efficacy. Results also showed distinctly different underlying cognitive structures of condom-use intention for men and women. A personal norm of condom-use responsibility had a strong direct effect on men’s intentions to use condoms with the last sex partner. Other variables appeared to have no direct effect on men’s intentions. Women’s intentions were strongly influenced by a personal norm and social subjective norms. Situational self-efficacy and outcome expectations had weaker, yet significant, effects on women’s intentions. Given the strong effect of personal norms on men’s intentions to use condoms, further research should be undertaken.
Introduction
Behavioural science theory has been used to guide the development and research of interventions to increase condom use by persons a high risk of HIV infection. While various theories propose slightly different underlying cognitive structures, an integrated behavioural model illustrated by Fishbein (2000) includes those factors generally accepted as influencing condom use (Albarracin et al., 1998, 2001, 2004; Crepaz & Marks, 2002; Terry, 1993). This model holds that three cognitive factors: condom-use attitudes, normative beliefs and self-efficacy, indirectly influence condom-use behaviour through the intention to use condoms. Studies indicate a large amount of variance is unaccounted for by these factors in the integrated model, leading to suggestions that other cognitive factors may be important (Kok et al., 2006; Logan et al., 2002; Sutton et al., 1999; Zimmerman & Vernberg, 1994). A personal norm of condom-use responsibility may be one such factor (Bowen et al., 2006; Conner & Armitage, 1998; Gold et al., 1994; Marks et al., 1999; Robinson et al., 2002; Wolitski et al., 2004). Narrowly defined, a personal norm of condom-use responsibility is a personal belief that it is one’s responsibility to use a condom during sex (Boyd & Wandersman, 1991; Godin et al., 1996; Manstead, 2000). This definition is consistent with an understanding of personal norms as defined by Triandis (1994) and Ajzen (1991).
HIV-prevention interventions developed early in the epidemic stressed an individual’s need to be responsible for his/her protection against infection (Bayer, 1997). It could be argued that the responsibility stressed in the early interventions was a personal norm of condom-use responsibility. Studies conducted with adolescents (Ben-Zur et al., 2003; Ford & Norris, 1995; Moore & Rosenthal, 1991; Nguyen et al., 1994) and adults (Bernard et al., 1989; Boyd & Wandersman, 1991; Fazekas et al., 2001; van Empelen et al., 2001; Varga, 2001) found that stronger personal norms were associated with greater intention to use condoms. Unfortunately, operationalizing and measuring the concept was difficult and infrequent, and design and measurement flaws limit the utility of these studies. Not all studies measured or assessed condom-use responsibility as a personal norm, making it difficult to assess exactly what was being measured (Bernard et al., 1989; Fazekas et al., 2001; Moore & Rosenthal, 1991; Nguyen et al., 1994; van Empelen et al., 2001) or did not include a measure of a personal norm of condom-use responsibility as part of a multivariate analyses, limiting conclusions that might be drawn about the role of the personal norms in relationship to other factors (Ben-Zur et al., 2000; Ford & Norris, 1995). When condom-use responsibility was examined for its effects on condom use or condom-use intention, models were not estimated separately for men and women, limiting the ability to draw inferences about gender differences (Boyd & Wandersman, 1991). There is little doubt that men and women do form condom-use intentions and are able to act on those intentions (Sheeran & Orbell, 1998). However, accounting for gender differences is important as there is strong evidence that factors affecting men’s and women’s condom-use decisions are significantly different (Amaro, 1995; Kusseling et al., 1996; Morrison et al., 1995; Pulerwitz et al., 2002; von Haeften & Kenski, 2001).
The purpose of this study was to investigate the unique contribution of a personal norm of condom-use responsibility on the intention to use male condoms during vaginal sex. Specifically, we were interested in assessing whether and how a personal norm of condom-use responsibility might increase the explanatory value of a model that included condom-use attitudes, perceived norms and self-efficacy. In addition, if condom-use responsibility did prove useful, we were interested in whether the variable affected intention to use condoms directly or indirectly through one of the other cognitive variables preceding condom-use intention. To test these possibilities, two structural equation models of the intention to use condoms were estimated. One model estimated the effect of factors included in Fishbein’s integrated model on the intention to use condoms. The second model included a personal norm of condom-use responsibility as an exogenous variable. Models were estimated separately for men and women.
Methods
Sample
Data were provided by a sample of heterosexual African American crack cocaine users. Crack cocaine smokers are at high risk for HIV transmission (Ross et al., 2003; van Empelen et al., 2001), as smoking crack lowers sexual inhibitions in some users (Wingood & DiClemente, 1998) and creates a socioeconomic environment in which trading sex for money or crack is common (Baseman et al., 1999). Furthermore, crack smokers have multiple sex partners (Inciardi et al., 1993; Lansky et al., 2000), many of whom overlap in time (Adimora et al., 2003) and inconsistently use condoms with all partners (Ford & Norris, 1995; McNair et al., 1998; Wingood & DiClemente, 1998).
Inclusion criteria for the study were: African American; between 18 and 40 years old; had smoked crack cocaine in the 48 hours before screening; had had vaginal sex at least once in the seven days before screening; resided in one of two neighbourhoods targeted for recruitment; and had provided sufficient information that there was a reasonable chance of relocation for follow-up interviews. Study procedures and data collection forms were reviewed and approved by the University of Texas Health Science Center at Houston’s Committee for the Protection of Human Subjects and the University of Wyoming’s Institutional Review Board.
Of 1,110 individuals screened, 625 (41%) met eligibility criteria. Reasons for being ineligible were: not having had sex in the seven days before screening (38%); not having had vaginal sex (26%); having a negative urine screen for cocaine (12%); and other reasons such as failing to be within the specified age range, living outside the target neighbourhoods or being too high or too incoherent to respond to screening questions (24%). There were no significant differences in gender, age or reported frequency of drug use between those who did not pass screening and those who met eligibility requirements.
Procedures
Data were collected between May 2002 and March 2004 in Houston, Texas as part of a study on the efficacy of an intervention designed to increase condom use during vaginal sex by adult African American heterosexual crack smokers.
Individuals were recruited using a combination of targeted sampling and participant referral. A targeted sampling plan was developed to identify neighbourhoods having high rates of drug use, and drug use was confirmed through interviews with local key informants knowledgeable about patterns of illicit drug-use in the city (Booth et al., 1993; Watters & Biernacki, 1989). Key informants were also asked to identify public places in the targeted neighbourhoods where crack smokers were likely to congregate and to provide introductions for outreach workers before the outreach workers approached recruits to ask them to participate. During encounters with recruits, outreach workers briefly described the research project, provided interested individuals with a risk-reduction packet that included condoms and asked if they were interested in taking part in a health-related study. If a recruit showed interest in participating in the study, the outreach worker gave him/her a business card and asked him/her to go to the nearby office for screening. Once individuals had participated in the study, they were asked to recruit others who they thought might be eligible to participate.
Individuals presenting for screening were informed: of the intent of the study; that participation was voluntary; that responding to any question could be refused; that they would be asked to present a picture identification card and that personal identifying information would be kept on file at the office; that all personal identifying information would be confidential and would not be linked to other data; and that screening was necessary to determine if an individual was eligible. If these conditions were understood and acceptable, consent to be screened was elicited. If an individual met basic screening criteria, (s)he was asked to provide a urine sample to validate a self-report of recent crack cocaine use. Samples were tested for cocaine metabolites using ONTRACK test kits. The results of the urine screen were immediately available. If a urine sample was negative, the individual was informed that they could return for screening at a later time. If a urine sample was positive, the individual was asked to be in the study and to provide written informed consent. Once written informed consent was obtained, participants were immediately interviewed.
Measures
Trained research assistant collected data for this study using the Peer Outreach Questionnaire (POQ). Interviews were conducted in private at a community-based office located close to the neighbourhoods targeted for recruiting. The POQ was developed by the investigators and has been used in previous studies of drug-using populations. Studies using measures similar to those in the POQ (Darke, 1998; Dowling-Guyer et al., 1994; Needle et al., 1995) have found that drug users can reliably report their behaviours and that data are valid. Forty-eight-hour test-retest data generated by a sample of 50 individuals matching study criteria also showed that the POQ produces reliable and valid data (available from the authors).
Demographics and drug use
The characteristics of participants were measured by responses to questions about gender, age, employment status, average monthly income and living arrangements. Lifetime and current drug use were measured for crack cocaine, alcohol, marijuana, methamphetamines, fry (marijuana cigarettes dipped in formaldehyde) and heroin. Risk of HIV infection related to needle use was measured by a history of drug injection and the frequency of drug injection and sharing needles or paraphernalia in the 30 days prior to the interview.
Sexual behaviours and condom use
Sexual behaviours and condom use were measured by asking a participant to think about the last time they had sex with their most recent or ‘last’ sex partner. The most recent sex partner was defined as the person with whom a participant had had vaginal sex in the seven days before the interview. Referencing responses to the last sex partner was used to take subjective differences among sex partners into account (Fishbein, 2000) and to improve respondent recall of sexual events and behaviours (Brewer et al., 1999). To aid in eliciting responses to questions about the last sex partner, the interviewer first asking the participant to provide the partner’s first name. All questions were then referenced by name.
Intention to use condoms
Intention to use condoms during vaginal sex was measured using a single item. Respondents were asked if s/he intended to use a male condom the next time s/he had vaginal sex with the named partner. Responses were recorded using a ten-point Likert scale that ranged from ‘definitely do not intend’ to ‘definitely do intend’ to use a condom the next time they had sex with the named partner. Intention was measured only as the intention to use male condoms. Previous research suggests that drug users are unfamiliar with the female condom and responded to questions about it as if they are responding to questions about male condoms (Timpson et al., 2005).
Predictors of intention to use condoms
All measures of the cognitive attitudes and beliefs about condom use included in the study are multi-item scales. Scale composition was confirmed by principal component factor analysis (PCA) using a Varimax rotation. Only items having a factor loading greater than 0.60 were included in a scale. Items were scored by a respondent using a ten-point Likert-type scale that ranged from 0–10. Scale scores are the means of item scores included in the scale.
Principal component factor analysis of the condom-use attitudes measures revealed a single factor composed of nine items (α = 0.92; M = 5.9). Among the items included in the measure were statements that using condoms would be ‘a lot of trouble,’ ‘would interrupt the flow of sex’ and ‘would make sex less sensual, fun or romantic’. As most of the items reflected negative condom-use attitudes, higher scores reflect more negative attitudes.
Principal component factor analysis revealed two independent condom-use self-efficacy beliefs. Emotional self-efficacy included seven items (α = 0.88; M = 6.9) and measured the belief that the respondent could make using condoms during vaginal sex exciting and emotionally satisfying. Situational self-efficacy included 15 items (α = 0.96; M = 6.9) and measured the belief that the respondent could use condoms in a variety of situations, such as when drunk, high, sexually aroused, lonely or feeling a need to be emotionally close to the partner.
Condom-use subjective norms were measured by two items using the partner as the referent other (α = 0.89; M = 4.2). Previous research with drug users has shown that they generally do not know or care what others, except the sex partner, think about their personal condom use (Williams et al., 2000).
Personal norm of condom use responsibility
Principal component factor analysis resulted in a condom-use responsibility scale composed of three items. Items were statements about a feeling of condom-use responsibility, ‘I think it is my responsibility to use a condom when I have vaginal sex with (partner’s name)’ and beliefs about whether condoms should be used. The measure had good internal reliability (α = 0.88) and a mean near the midpoint (M = 5.9).
Analyses
Data from 51 participants whose last partner was a ‘new’ partner were excluded from the analysis because it was felt that they might lack sufficient experience with that partner to have formed beliefs about the partner’s condom-use expectations. Four were excluded because their last sexual partner was a person of the same gender. Eleven were excluded because they reported that sex with their most recent partner exceeded the past seven days or because the number of times they reported having had sex with the last partner in the seven-day timeframe was unreliable. Data used for the analyses were from 402 men and 157 women.
Pearson’s two-tailed correlation coefficients were computed to assess relationships among variables and to assess collinearity (Tabachnick & Fidell, 1996). Bivariate correlations, estimated separately for men and women, showed that condom-use attitudes, subjective norms, emotional self-efficacy, situational self-efficacy and a personal norm of condom-use responsibility were significantly correlated, but sufficiently independent to be used to construct structural equation models. Correlational analysis also showed that all variables were significantly correlated with the intention to use condoms.
Two structural equation models were estimated separately for men and women. The first model estimated included only attitudes; emotional self-efficacy; situational self efficacy; and subjective norms. The second or expanded model included these measures and the measure of a personal norm of condom-use responsibility, which was entered in the model as an exogenous variable. The models estimated were recursive; that is the effects of variables in the models were hypothesized to flow in one direction only. Full models estimating all paths available were calculated using AMOS (Byrne, 2001). Trimmed models, eliminating paths that were not significant, are presented.
Several measures of the goodness-of-model-fit are available and each has benefits and limitations (Kline, 1998). For this analysis, three were used. The Bentler-Bonett normed fit index (NFI) ranges from 0.00–1.00. An NFI score greater than 0.90 indicates a good fit of the model to the data. A second measure used was the comparative fit index (CFI). A CFI score great than 0.90 and close to 0.95 indicates a good fit. A third measure, the incremental fit index (IFI) evaluates goodness-of-fit and model parsimony. The measure ranges from 0.00–1.00, with values over 0.90 indicating good model fit and parsimony.
To compare the fit of the first and expanded models to the data, a chi-squared difference test was used (Kline, 1998). The test is conducted by calculating the difference in chi-squared statistics and degrees of freedoms between the first and second models. If the difference in chi-squared statistics, using the difference in degrees of freedoms, is significant, the second model is assumed to be the better fit. If the difference is not significant, the first model is assumed to fit the data better.
Results
Participants
No significant gender differences were found by age, education, living status or income. The age of participants ranged from 18–40 years and the average was 32.9 (median = 34). The average education was 11.4 years (median = 11). The majority of participants were single or living as single (82%) and most were living in tenuous housing, someone else’s home (63%), a shelter, boarding house or hotel (13%) or on the streets (6%). Most considered themselves homeless (61%) and about three-quarters (72%) earned less than $600 in the month prior to the interview. Almost half of the participants were employed in full- or part-time jobs (47%). There was a significant difference in source of income by gender. A job was the major source of income for men (57%). Slightly less than a fifth of women (18%) reported earning income from some type of job. Trading sex for money was the major source of income for more than a third of women (38%), compared to less than 10% of men.
Eighty-eight percent of the participants smoked crack cocaine more than once a day, with an average of 73.3 times (median = 30) in the 30 days before the interview. Other drugs used included marijuana (59%), codeine syrup (7%), fry (4%) and methamphetamine (2%). Less than 1% were injecting drugs at the time of the interview. The average number of sex partners in the seven days before the interview was significantly greater for women (M = 6.17; SD = 11.03) than for men (M = 3.92; SD = 4.37). However, there were no gender differences in the median number of partners (median = 3). Significantly more women (61%) had a lifetime history of trading sex for money than did men (11%). There was no significant difference in condom use by gender, with approximately half of men (49%) and women (57%) reporting ‘never using condoms’.
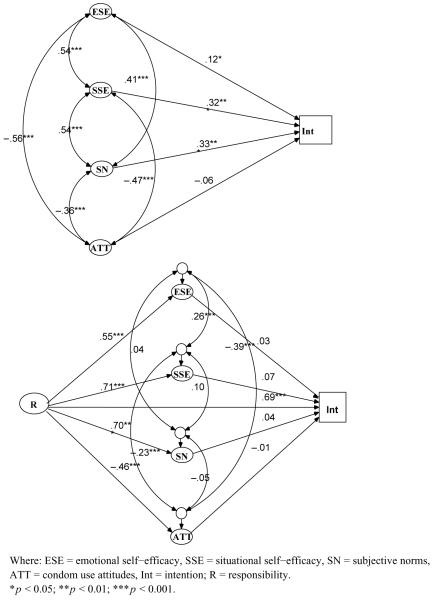
Men’s intention to use condoms
As shown in Figure 1, the model including only condom-use attitudes, subjective norms, emotional self-efficacy and situational self-efficacy was significant (χ2 = 977.98; df = 425; p < 0.000) and fit the data fairly well (NFI = 0.90; CFI = 0.94; IFI = 0.94). Paths from situational self-efficacy and subjective norms to intention were significant and moderately strong. The path from emotionalself-efficacy to intention was significant but weak. The path from condom-use attitudes to intention was not significant.
Figure 1.
Structural equation models of men’s intention to use condoms.
The expanded model, which included the condom-use responsibility variable, was significant (χ2 = 1508.98; df = 516; p < 0.000) and produced a significant improvement over the first model estimated (Δχ2 = 320.35; Δdf = 91; p < 0.000). Again, the model provided an acceptable fit to the data (NFI = 0.88; CFI = 0.91; IFI = 0.91). All direct paths from the condom-use responsibility variable to other variables included in the expanded model were significant and strong. However, only the direct path from condom-use responsibility to intention was significant.
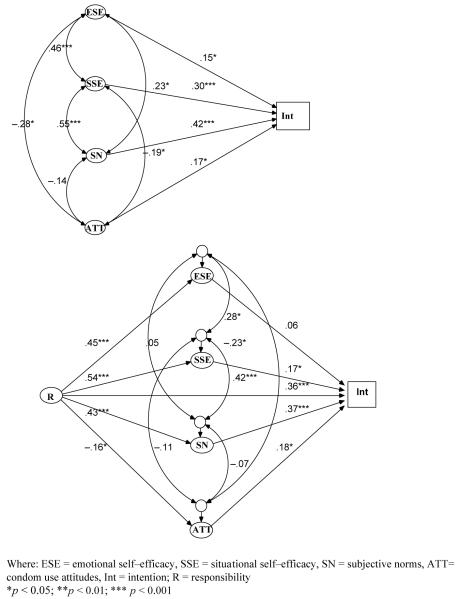
Women’s intention to use condoms
The model estimated for women using condom-use attitudes, subjective norms, emotional self-efficacy and situational self-efficacy, as shown in Figure 2, was significant (χ2 = 783.60; df = 425; p < 0.000) and provided a moderately acceptable fit to the data (NFI = 0.82; CFI = 0.90; IFI = 0.90). All paths from the variables to intention were significant. The strongest path was from subjective norms to intention. The path from situational self-efficacy to intention was moderately strong. The paths from emotional self-efficacy and condom-use attitudes were significant but weak.
Figure 2.
Structural equation models of women’s intentions to use condoms.
Adding the ‘personal norm of condom-use responsibility’ variable as an exogenous variable produced a model that was significant (χ2 = 1103.95; df = 516; p < 0.000) and provided a significant improvement over the first model estimated (Δχ2 = 360.04; Δdf = 91; p < 0.000). The fit of the expanded model was acceptable, although moderate (NFI = 0.77; CFI = 0.86; IFI = 0.86). All paths from condom-use responsibility to condom-use attitudes, subjective norms, emotional self-efficacy and situational self-efficacy variables were significant. Three paths to intention-to-use-condoms were significant. The direct paths from condom-use responsibility and subjective norms to intention were positive and strong. The paths from situational self-efficacy and condom-use attitudes to intention were significant but weak.
Discussion
The goal of this study was to examine the utility of adding a ‘personal norm of condom responsibility’ to the integrated model of condom use (Fishbein, 2000) and to examine its differential utility for men and women. Data were provided by a sample of African American crack cocaine smokers. Crack cocaine smokers are at high risk for HIV infection and infection with other sexually transmitted diseases because of a large number of sex partners and involvement in trading sex for money or drugs. The high risk of this population is supported by the characteristics of this sample. Participants in the study were smoking crack frequently, using an average of twice daily in the 30 days before they were interviewed. Participants also had high numbers of sex partners, and women had greater numbers of partners than men. The higher number of sex partners for women is due to the greater number of women who support themselves by trading sex for money. A high level of risk is also reflected in the infrequency of condom use. About half of the men the study and more than half of the women never used condoms during vaginal sex.
Results of the structural equation modeling indicate that the addition of a ‘personal norm of condom responsibility’ increases the predictive validity of the models of intention to use condoms and that that there are significant differences between the models estimated for men and women. Condom-use poses very different issues for men and women. More specifically, if a man decides to use a condom, in many respects the decision is his alone. For women, using a male condom may mean convincing a male partner to do so. The need to convince a male partner to use a condom may interact with a woman’s communication skills and be dependent upon the power structure in the relationship. A woman’s desire to insist that a male partner wear a condom may depend on her strategy to form a bond with a particular partner or the number of times she has had sex with a man. Although demonstrating different dynamic structures in the expanded models, a personal norm of condom-use responsibility was strongly related to condom-use intention in models for both men and women.
The results of modelling men’s intentions suggest that a personal norm of condom-use responsibility may be the only variable directly influencing the formation of men’s condom-use intentions. The failure of any of the direct paths from condom-use attitudes, subjective norms, emotional self-efficacy and situational self-efficacy to intention to achieve significance supports this conclusion. This result strongly suggests that men may make their condom-use decisions based largely on their personal feelings of condom-use responsibility. This may be true because men feel that condom use is such a personal behaviour that only their personal norms are relevant to their decision. As suggested by the expanded model, men’s feelings of condom-use responsibility may affect condom-use attitudes, self-efficacy, and subjective norms, but that these may play no role in making condom-use decisions. As men’s feelings of condom-use responsibility increase, their attitudes about using condoms may become more favorable, they may come to believe that they can make sex with a condom more enjoyable and exciting and that they can do so in difficult situations, such as when they are high or drunk. Men may also believe, as a result of their feelings of condom-use responsibility, that their partners also believe that condoms should be used during vaginal sex.
The addition of a personal norm of condom-use responsibility to the women’s model of condom-use intention provided a significant improvement over the model that included only condom-use attitudes, subjective norms and self-efficacy variables. The expanded model suggests that, unlike men, women’s feelings of personal responsibility for condom use and the belief that their partners think they should use condoms are both important in the formation of women’s condom use intentions. As suggested above, this may be because women do not actually use condoms and may base their intentions at least partially on what they believe their partners want. The expanded model also suggests that, while situational self-efficacy and condom-use attitudes may influence women’s condom-use intentions, their effect on intention is much weaker than either condom-use responsibility or the belief that their partners think condoms should be used. As in the men’s expanded model, the strong direct paths from condom-use responsibility to emotional self-efficacy, situational self-efficacy, and subject norms suggest that women’s belief that they are responsible for using condoms influences these other factors.
The strong direct paths in both men’s and women’s models from a personal norm of condom-use responsibility to condom-use self-efficacy beliefs, subjective norms and condom-use attitudes suggests that both men and women may need to develop personal norms of condom-use responsibility before they assess whether they can make sex while using condoms emotionally satisfying or believe that they can use condoms in difficult personal situations, such as when they are high, drunk, sexually aroused, or when a partner does not want to use condoms. Developing a personal norm of condom use, therefore, may be a first and perhaps necessary process before condom-use attitudes, feelings of self-efficacy, or subjective norms begin to change. Both men and women’s models also suggest that the perception of the partner’s desire to use condoms is strongly influenced by personal feelings of condom-use responsibility. Both men and women may assume that their partner’s condom-use beliefs are consistent with their own, even if they do not know what the beliefs of the partner truly are. It is also plausible that men and women select partners who share their feelings of condom-use responsibility.
Limitations
Like any research involving hidden populations, the sample from which data were generated is not random, limiting the degree to which results can be generalized to other groups of heterosexual adult drug users. Generalization is also limited because the sample consisted of only African American crack cocaine smokers. While limiting the sample to African American crack cocaine smokers controlled for the effects of race/ethnicity and drug use on the estimated models, it also limits the ability to draw conclusions about heterosexuals who may use other drugs or about crack cocaine smokers in other racial/ethnic groups.
Study results are also limited because data were self-reported. While self-reported data about recent sexual behaviour are reliable, estimating the true accuracy of the data is virtually impossible (Catania et al., 1990a,b). Self-reported sexual behaviour tends to be biased toward more recent behaviour with more recent partners. Self-reported sexual behaviour also tends to be biased toward events that are out of the ordinary. Routine or habitual behaviour is often clustered. To limit these sources of error, only sexual behaviour with the last partner in the seven days before participants were interviewed were used. However, to what extent recall was improved is unknown. In addition to error associated with recall, the subjective context of the sex partner is known to influence measurement of condom use (Fishbein, 2000). To limit the effect of subjective context, measurement of cognitive factors influencing condom use was referenced to a sex partner by name or identifier. Data may also be limited because models were not estimated by partner type. The intention to use condoms during vaginal sex is known to vary by partner type. However, there is evidence suggesting that condom use with specific partners varies by factors unrelated to the partner’s type, such as frequency of sex (Fortenberry et al., 2002; Williams et al., 2001).
Despite these limitations, the findings of this study suggest that interventions to increase condom use developed for heterosexual drug users should target increasing personal norms of condom-use responsibility. However, from the perspective of crack cocaine smokers, precisely what crack smokers mean when they say that they feel a personal responsibility for using condoms is unknown. Iterative studies that carefully and fully explore drug users’ sense of condom-use responsibility and its meaning are needed. Most importantly, formative studies that investigate how personal norms of condom use are formed, their strength once formed, and if they vary as sexual partners and situations change are needed before interventions targeting personal norms can be developed and implemented. Furthermore, as the expanded models suggest, gender differences must receive additional study and results should be applied when interventions are developed. In particular, additional research is needed on how drug users, particularly women, form perceptions about their partner’s condom-use beliefs and how these interact with their personal feelings of condom-use responsibility.
The findings of this study also suggest that models of condom-use intentions and condom-use behaviour need further thought and testing. The findings produced by the men’s model in particular suggest that variables other than condom-use attitudes, subjective norms, or self-efficacy co-vary with condom-use intentions. The relative strength of the personal norm variable in both the men’ and women’s model of condom-use intentions suggests that the assumption that all variables exogenous to most models of condom use operate through endogenous variables, even when endogenous variables have an apparent effect on intention, may need modification. At the very least, variables and concepts that take the interpersonal nature of sexual behaviour and its moral overtones into account deserve further development.
Acknowledgements
This research was supported by a grant from the National Institute on Drug Abuse. All work and opinions herein are solely those of the authors.
References
- Adimora A, Schoenbach V, Martinson F, Donaldson K, Stancil T, Fullilove R. Concurrent partnerships among rural African Americans with recently reported heterosexually transmitted HIV Infection. Epidemiology and Social Science. 2003;34:423–429. doi: 10.1097/00126334-200312010-00010. [DOI] [PubMed] [Google Scholar]
- Ajzen I. The theory of planned behaviour. Organizational Behaviour and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Albarracin D, Fishbein M, Middlestadt S. Generalizing behavioural findings across times, samples and measures: A study of condom use. Journal of Applied Social Psychology. 1998;28:657–674. [Google Scholar]
- Albarracin D, Johnson B, Fishbein M, Muellerleile P. Theories of reasoned action and planned behaviour as models of condom use: A meta-analysis. Psychological Bulletin. 2001;127:142–151. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracin D, Kumkale G, Johnson B. Influences of social power and normative support on condom use decisions: A research synthesis. AID Care. 2004;16:700–723. doi: 10.1080/09540120412331269558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaro H. Love, sex and power. Considering women’s realities in HIV prevention. American Psychologist. 1995;50:437–447. doi: 10.1037//0003-066x.50.6.437. [DOI] [PubMed] [Google Scholar]
- Baseman J, Ross M, Williams M. Sale of sex for drugs and drugs for sex: An economic context of sexual risk behaviour for STDs. Sexually Transmitted Diseases. 1999;26:444–449. doi: 10.1097/00007435-199909000-00005. [DOI] [PubMed] [Google Scholar]
- Bayer R. Responsibility and intimacy in the AIDS epidemic. The Responsive Community. 1997;7:45–55. [PubMed] [Google Scholar]
- Ben-Zur H, Breznitz S, Wardi N, Berzon Y. Denial of HIV/AIDS and preventive behaviour among Israeli adolescents. Journal of Adolescence. 2000;23:157–174. doi: 10.1006/jado.2000.0305. [DOI] [PubMed] [Google Scholar]
- Bernard J, Hébert Y, de Man A, Farrar D. Attitudes of French-Canadian university students toward use of condoms: A structural analysis. Psychological Reports. 1989;65:851–854. doi: 10.2466/pr0.1989.65.3.851. [DOI] [PubMed] [Google Scholar]
- Booth R, Watters J, Chitwood D. HIV risk-related sex behaviours among injection drug users, crack smokers, and injection drug users who smoke crack. American Journal of Public Health. 1993;83:1144–1148. doi: 10.2105/ajph.83.8.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd B, Wandersman A. Predicting undergraduate condom use with the Fishbein and Ajzen and the Triandis attitude-behaviour models: Implications for public health interventions. Journal of Applied Psychology. 1991;21:1810–1830. [Google Scholar]
- Bowen A, Williams M, Dearing E, Timpson S, Ross M. Male heterosexual crack smokers with multiple sex partners: Between and within person predictors of condom intention. Health Education Research. 2006;21:549–559. doi: 10.1093/her/cyl009. [DOI] [PubMed] [Google Scholar]
- Brewer D, Garrett S, Kulasingam S. Forgetting as a cause of incomplete reporting of sexual and drug injection partners. Sexually Transmitted Diseases. 1999;26:166–176. doi: 10.1097/00007435-199903000-00008. [DOI] [PubMed] [Google Scholar]
- Byrne B. Structural equation modeling with AMOS: Basic concepts, applications, and programming. Lawrence Erlbaum Associates, Inc.; Mahwah, NJ: 2001. [Google Scholar]
- Catania J, Gibson D, Marin B, Coates T, Greenblatt R. Response bias in assessing sexual behaviours relevant to HIV transmission. Evaluation and Program Planning. 1990a;13:19–29. [Google Scholar]
- Catania J, Gibson D, Chitwood D, Coates T. Methodological problems in AIDS behavioural research: Influences on measurement error and participation bias in studies of sexual behaviour. Psychological Bulletin. 1990b;108:339–362. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]
- Conner M, Armitage C. Extending the theory of planned behaviour: A review and avenues for further research. Journal of Applied Social Psychology. 1998;28:1429–1464. [Google Scholar]
- Crepaz N, Marks G. Towards an understanding of sexual risk behaviour in people living with HIV: A review of social, psychological, and medical findings. AIDS. 2002;16:135–149. doi: 10.1097/00002030-200201250-00002. [DOI] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: A review. Drug and Alcohol Dependence. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Dowling-Guyer S, Johnson M, Fisher D, Needle R, Watters J, Andersen M, et al. Reliability of drug users’ self-reported HIV risk behaviours and validity of self-reported recent drug use. Assessment. 1994;1:383–392. [Google Scholar]
- Fishbein M. The role of theory in HIV prevention. AIDS Care. 2000;12:273–278. doi: 10.1080/09540120050042918. [DOI] [PubMed] [Google Scholar]
- Ford K, Norris A. Factors related to condom use with casual partners among urban African-American and Hispanic males. AIDS Education and Prevention. 1995;7:494–503. [PubMed] [Google Scholar]
- Fortenberry J, Tu W, Harezlak J, Katz B, Orr D. Condom use as a function of time in new and established adolescent sexual relationships. American Journal of Public Health. 2002;92:211–213. doi: 10.2105/ajph.92.2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazekas A, Senn C, Ledgerwood D. Predictors of intention to use condoms among university women: An application and extension of the theory of planned behaviour. Canadian Journal of Behavioural Science. 2001;33:103–117. [Google Scholar]
- Godin G, Maticka-Tyndale E, Adrien A, Manson-Singer S, Willms D, Cappon P. Cross-cultural testing of three social cognitive theories: An application to condom use. Journal of Applied Social Psychology. 1996;26:1556–1586. [Google Scholar]
- Gold R, Skinner M, Ross M. Unprotected anal intercourse in HIV-infected and non-infected gay men. Journal of Sex Research. 1994;31:59–77. [Google Scholar]
- Inciardi J, Lockwood D, Pottieger A. Women and crack-cocaine. Macmillan Publishing Company; New York: 1993. pp. 91–106. [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. Guilford Press; New York: 1998. [Google Scholar]
- Kok G, Harterink P, Vriens P, de Zwart O, Hospers H. The Gay Cruise: Developing a theory- and evidence-based internet HIV-prevention intervention. Sexuality Research & Social Policy. 2006;3(52):67. [Google Scholar]
- Kusseling F, Shapiro M, Greenberg J, Wenger N. Understanding why heterosexual adults do not practice safer sex: A comparison of two samples. AIDS Education and Prevention. 1996;8:247–257. [PubMed] [Google Scholar]
- Lansky A, Nakashima A, Jones J. Risk behaviours related to heterosexual transmission from HIV-infected persons. Sexually Transmitted Diseases. 2000;27:483–489. doi: 10.1097/00007435-200009000-00012. [DOI] [PubMed] [Google Scholar]
- Logan T, Cole J, Leukefeld C. Women, sex and HIV: Social and contextual factors, meta-analysis of published interventions, and implications for practice and research. Psychological Bulletin. 2002;128:851–885. doi: 10.1037/0033-2909.128.6.851. [DOI] [PubMed] [Google Scholar]
- Manstead A. The role of moral norm in the attitude-behaviour relation. In: Terry D, Hogg M, editors. Attitudes, behaviour, and social context: The role of norms and group membership. Lawrence Erlbaum Associates, Publishers; Mahwah, NJ: 2000. pp. 22–30. [Google Scholar]
- Marks G, Burris S, Peterman T. Reducing sexual transmission of HIV from those who know they are infected: The need for personal and collective responsibility. AIDS. 1999;13:297–306. doi: 10.1097/00002030-199902250-00001. [DOI] [PubMed] [Google Scholar]
- McNair L, Carter J, Williams MK. Self-esteem, gender, and alcohol use: Relationships with HIV risk perception and behaviours in college students. Journal of Sex and Marital Therapy. 1998;24:29–36. doi: 10.1080/00926239808414666. [DOI] [PubMed] [Google Scholar]
- Moore S, Rosenthal D. Condoms and coitus: Adolescents attitudes to AIDS and safe sex behaviour. Journal of Adolescence. 1991;14:211–227. doi: 10.1016/0140-1971(91)90017-l. [DOI] [PubMed] [Google Scholar]
- Morrison D, Gillmore M, Baker S. Determinants of condom use among high-risk adults: A test of the theory of reasoned action. Journal of Applied Social Psychology. 1995;25:651–676. [Google Scholar]
- Needle R, Fisher D, Weatherby N, Brown B, Cesari H, Chitwood D, et al. The reliability of self-reported HIV-risk behaviours of drug users. Psychology of Addictive Behaviours. 1995;9:242–250. [Google Scholar]
- Nguyen M, Saucier J, Pica L. Influence of attitudes on intention to use condoms in Quebec sexually active male adolescents. Journal of Adolescent Health. 1994;15:269–274. doi: 10.1016/1054-139x(94)90515-0. [DOI] [PubMed] [Google Scholar]
- Pulerwitz J, Amaro H, De Jong W, Gortmaker S, Rudd R. Relationship power, condom use and HIV risk among women in the US. AIDS Care. 2002;14:789–800. doi: 10.1080/0954012021000031868. [DOI] [PubMed] [Google Scholar]
- Robinson B, Bockting W, Rosser B, Miner M, Coleman E. The sexual health model: Application of a sexological approach to HIV prevention. Health Education Research. 2002;17:43–57. doi: 10.1093/her/17.1.43. [DOI] [PubMed] [Google Scholar]
- Ross M, Timpson S, Williams M, Bowen A. Situational correlates of condom use in a sample of African American drug users who are primarily crack cocaine users. AIDS and Behaviour. 2003;7:55–60. doi: 10.1023/a:1022561423599. [DOI] [PubMed] [Google Scholar]
- Sheeran P, Orbell S. Do intentions predict condom use? Meta-analysis and examination of six moderator variables. British Journal of Social Psychology. 1998;37:231–250. doi: 10.1111/j.2044-8309.1998.tb01167.x. [DOI] [PubMed] [Google Scholar]
- Sutton S, McVey D, Glanz A. A comparative test of the theory of reasoned action and the theory of planned behaviour in the prediction of condom use intentions in a national sample of English young people. Health Psychology. 1999;18:72–81. doi: 10.1037//0278-6133.18.1.72. [DOI] [PubMed] [Google Scholar]
- Tabachnick C, Fidell L. Using multivariate statistics. Harper Collins; New York: 1996. [Google Scholar]
- Terry D. Self-efficacy expectancies and the theory of reasoned action. In: Terry D, Gallois C, McCamish M, editors. The theory of reasoned action: Its application to AIDS-prevention behaviour. Pergamon Press; Oxford: 1993. [Google Scholar]
- Timpson S, Williams M, Ross M, Keel K. Attitudes and beliefs about male and female condoms among African American crack cocaine users. Journal of Substance Abuse. 2005;10:207–213. [Google Scholar]
- Triandis H. Culture and social behaviour. McGraw-Hill; New York: 1994. [Google Scholar]
- van Empelen P, Schaalma H, Kok G, Jansen M. Predicting condom use with casual and steady sex partners among drug users. Health Education Research. 2001;16:293–305. doi: 10.1093/her/16.3.293. [DOI] [PubMed] [Google Scholar]
- Varga C. Coping with HIV/AIDS in Durban’s commercial sex industry. AIDS Care. 2001;13:351–365. doi: 10.1080/09540120120044008. [DOI] [PubMed] [Google Scholar]
- von Haeften I, Kenski K. Multi-partnered heterosexuals’ condom use for vaginal sex with their main partner as a function of attitude, subjective norm, partner norm, perceived behavioural control and weighted control beliefs. Psychology, Health, and Medicine. 2001;6:165–177. [Google Scholar]
- Watters J, Biernacki P. Targeted sampling: Options for the study of hidden populations. Social Problems. 1989;36:416–430. [Google Scholar]
- Williams M, Bowen A, Elwood W, McCoy C, McCoy H, Freeman R, et al. An elicitation of the determinants of condom use among African Americans who smoke crack cocaine. Culture, Health. and Sexuality. 2000;2:15–32. [Google Scholar]
- Williams M, Ross M, Bowen A, Timpson S, McCoy H, Perkins K, et al. An investigation of condom use by frequency of sex. Sexually Transmitted Infections. 2001;77:433–435. doi: 10.1136/sti.77.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood G, DiClemente R. Partner influences and gender-related factors associated with non-condom use among young adult African American women. American Journal of Community Psychology. 1998;26:29–51. doi: 10.1023/a:1021830023545. [DOI] [PubMed] [Google Scholar]
- Wolitski R, Parsons J, Gomez C. Prevention with HIV-seropositive men who have sex with men: Lessons from the Seropositive Urban Men’s Study (SUMS) and the Seropositive Urban Men’s Intervention Trial (SUMIT) Journal of Acquire Immune Deficiency Syndromes. 2004;37:S101–S109. doi: 10.1097/01.qai.0000140608.36393.37. [DOI] [PubMed] [Google Scholar]
- Zimmerman R, Vernberg D. Model of preventive health behaviour: Comparison, critique, and meta-analysis. In: Albrecht G, editor. Advances in medical sociology: A reconsideration of Health Behaviour Change Models. JAI Press; Greenwich, CT: 1994. pp. 45–67. [Google Scholar]