Abstract
OBJECTIVES:
To determine whether emergency physicians (EPs) who have skills in the other applications of ultrasound can apply these in appendicitis diagnosis.
METHODS:
EPs did not have focused training in bedside ultrasound for appendicitis. We identified patients receiving an ED bedside ultrasound evaluation for appendicitis from our ultrasound log. Criterion reference was radiology ultrasound (RUS), CT scan, or pathology report.
RESULTS:
We performed 155 ED ultrasounds for appendicitis. There were 27/155 cases where the ED ultrasound was true positive and agreed with pathology (sensitivity = 39%, 95% CI 28 – 52%). In 42/155 (27%) the ED ultrasound was non-diagnostic (false negative) with pathology positive. In 77 cases the ED ultrasound was true negative with non-visualization of the appendix in concert with non-visualization by RUS or CT scan (specificity = 90%, 95% CI 81–95%). In nine cases (6%), ED ultrasound was falsely positive, compared to CT scan with surgical consult.
CONCLUSION:
ED ultrasound by EPs prior to focused appendicitis ultrasound training is insufficiently accurate.
Keywords: appendicitis, bedside, emergency, ultrasound, retrospective
INTRODUCTION
Acute appendicitis, the most common abdominal surgical emergency, occurs in 7% of the population, with peak incidence age 10 – 30.1,2,3 Diagnosis by the emergency physician (EP) remains challenging, because clinical evaluation alone yields sensitivity of 39–74% and specificity of 57–84%.4 Despite current technology, more than one in five tests obtained in patients with negative laparatomies for appendicitis were falsely positive for appendicitis. 5 Moreover, perforated appendicitis, with its 4% mortality rate, is the most common abdominal disorder for malpractice claims and the fifth most expensive cause of claims against emergency physicians. 6,7 Not surprisingly, delay in diagnosis is the main factor leading to perforation. Imaging outside the ED prior to surgeon’s evaluation, such as RUS or CT, contributes to this delay. 8 Conversely, expediting appendicitis diagnosis would be valuable to crowded EDs.
The objective of this study is to determine if EPs, already skilled with other ultrasound applications, can identify patients with acute appendicitis. One previous study of EPs from Taiwan, following intensive abdominal ultrasound training, showed 96% sensitivity and 67% specificity for appendicitis diagnosis. 9 However, this level of training is impractical for many practicing EPs in the USA. This study examines ED ultrasound for appendicitis at the opposite end of the learning curve.
METHODS
Study Design
This was a retrospective registry-based cohort study of ED bedside right lower quadrant (RLQ) abdominal ultrasounds performed by EPs. Of interest was whether EPs with strong backgrounds in other ultrasound applications, but without focused training for appendicitis, could diagnose appendicitis with reasonable accuracy. All EPs had previous training in the following applications: gallbladder, aorta, trauma, lower extremity deep venous thrombosis, cardiac, renal, procedure guidance, and pelvis. Three of the 14 attending physicians were Registered Diagnostic Medical Sonographers (RDMS). Seven attending physicians performed at least 300 ultrasound examinations of all types, and held hospital credentials for clinical decision-making in the above applications. At no point during the study did EPs make independent clinical decisions based on ED ultrasound for appendicitis. While residents are required to perform 500 scans of all types prior to graduation, experience among the 18 residents varied widely from 50 scans to as many as 700. No EP received either didactic or hands-on instruction.
The study was done in a university hospital ED with American College of Surgeons’ Level I Trauma Center designation. Annual census was 46,000 patients. Each year, approximately 4000 EP-performed ED ultrasounds were videotaped and reviewed by the Director of Emergency Ultrasound (JCF) for accuracy. All attending EPs were board certified or prepared.
From the ED ultrasound log, we identified consecutive patients of all ages and genders who had right lower quadrant scans from January 2002 to January 2004. Patients were more likely to be scanned if there was concern to expedite their care by attempting to demonstrate acute appendicitis at the bedside. Patients were excluded if they did not receive any of three criterion references for final diagnosis of appendicitis: 1) radiology performed ultrasound (RUS), 2) CT scan with oral and IV contrast, or 3) pathology report at laparotomy. The imaging and pathology results were tiered criterion standards, with pathology results being the highest standard.
We performed all ED ultrasounds prior to RUS or CT. The sole primary sonographic criterion for the physician to make the diagnosis of appendicitis was a non-compressible RLQ tubular structure of at least six millimeters (Figures 1 and 2). Secondary sonographic findings such as appendicolith (Figure 3), hyperemia on color flow Doppler (Figure 4), interruption of the echogenic submucosa, or extraluminal fluid collections were not diagnostic criteria for this study.
Figure 1.
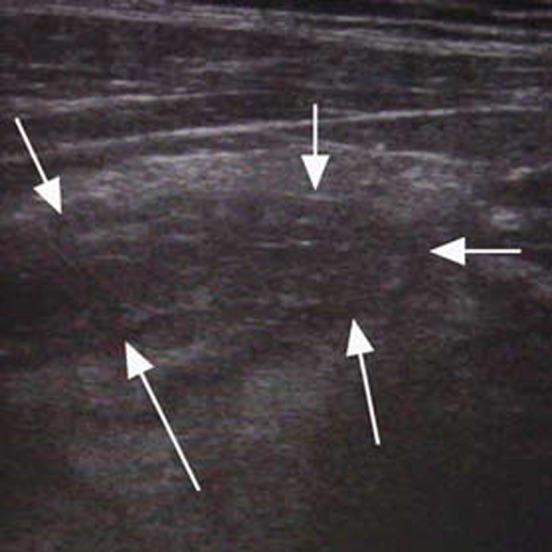
Inflamed appendix in long axis view
Figure 2.
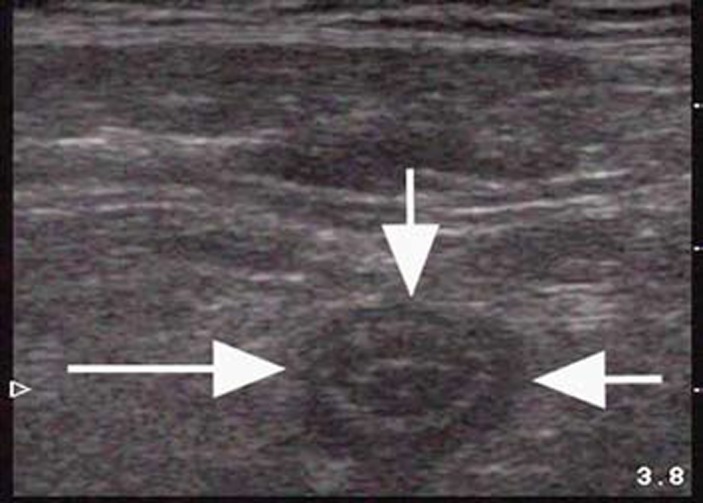
Inflamed appendix in short axis view
Figure 3.
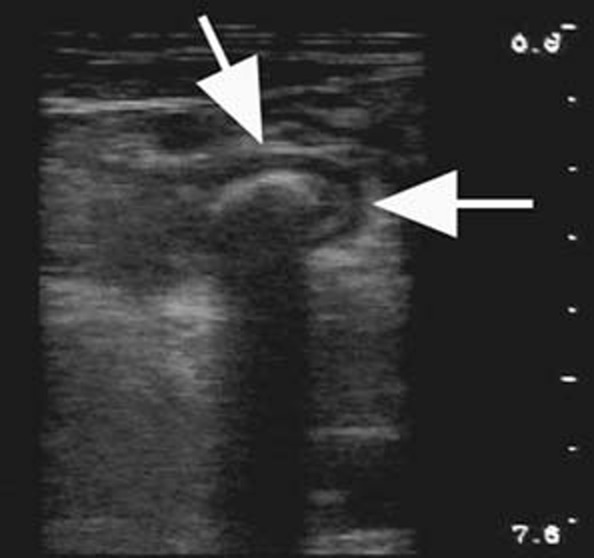
Appendicolith
Figure 4:
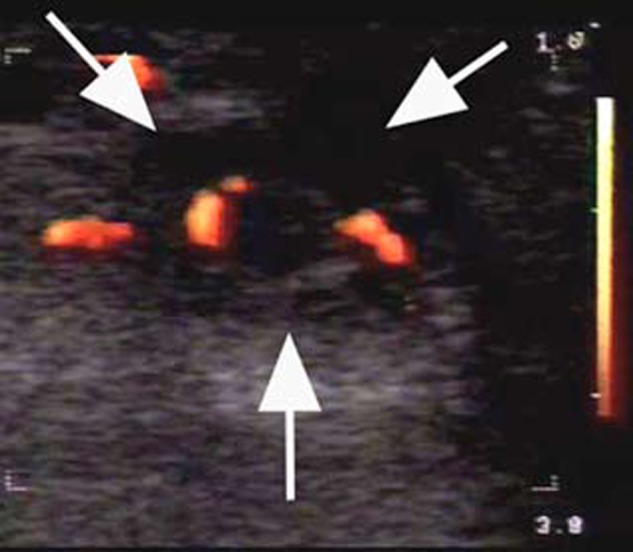
Ring of Fire. Hyperemia on color flow Doppler, interruption of the echogenic submucosa, or extraluminal fluid collections.
Data Analysis and Materials
With a B+K Hawk 2102’s 5.5 megahertz linear transducer (Copenhagen, Denmark), we performed ED ultrasounds of the RLQ, videotaped on a Sony Digital8 VCR. The data sheet required the EP to choose either a) “no appendix visualized” or b) “acute appendicitis.” If acute appendicitis was chosen, the physicians were instructed to base this solely on the primary criteria described above. This study was approved by the university’s Institutional Review Board.
We analyzed the data for sensitivity, specificity, positive and negative predictive values, and confidence intervals using an internet-based statistical calculator (http://faculty.vassar.edu/lowry/VassarStats.html).
RESULTS
Emergency physicians performed 186 RLQ ultrasounds for appendicitis during the study period. We excluded 31 subjects because no criterion reference was available, leaving 155 for data analysis. There were 91 adults, 64 children, 70 females and 85 males. Prevalence of appendicitis was 45% (69/155).
There were 27/155 cases where the ED ultrasound was true positive and agreed with surgical pathology (sensitivity = 39%, 95% CI 28 – 52%). In 42/155 (27.1%) the ED ultrasound was non-diagnostic (false negative) with surgical pathology positive. In 77 cases the ED ultrasound was true negative with non-visualization of the appendix in concert with non-visualization by RUS or CT scan (specificity = 90%, 95% CI 81–95%). In nine cases (6%), ED ultrasound was falsely positive, indicating appendicitis while CT scan with surgical consult did not. None of these went to surgery. Accuracy of ED ultrasound was 66% (95% CI 59–74%). The positive and negative predictive values were 75% (95% CI 57% to 87%) and 65% (95% CI 55 to 73%) respectively. (See Tables 1 & 2.)
Table 1:
Distribution of Patients
| Appendicitis | |||
|---|---|---|---|
| Present | Absent | Totals | |
| BUSA Positive | 27 | 9 | 36 |
| BUSA Negative | 42 | 77 | 119 |
| Total | 69 | 86 | 155 |
BUSA: Bedside Ultrasound for Appendicitis
Table 2:
BUSA Accuracy
| Accuracy of BUSA | Point Estimate | 95% Confidence Interval | |
|---|---|---|---|
| Prevalence | 0.45 | 0.37 | 0.53 |
| Sensitivity | 0.39 | 0.28 | 0.52 |
| Specificity | 0.90 | 0.81 | 0.95 |
| PPV | 0.75 | 0.57 | 0.87 |
| NPV | 0.65 | 0.55 | 0.73 |
BUSA: Bedside Ultrasound for Appendicitis
PPV: Positive Predictive Value
NPV: Negative Predictive Value
DISCUSSION
Approximately 3.4 million patients per year present to EDs in the United States with a chief complaint of abdominal pain, 10 of which 250,000 (7%) are diagnosed with appendicitis. 11 In crowded EDs, time is critical and rapid disposition is crucial. Moreover, delayed diagnosis of appendicitis leading to perforation is the leading cause of morbidity and mortality. 12,13
Bedside ED ultrasound is becoming widely available. Ultrasound training is required in EM residency,14 and emergency physicians have demonstrated the ability to accurately perform focused ultrasound examinations. 15,16,17 After an introductory course and minimal hands-on training, one investigator demonstrated that emergency medicine residents had a sensitivity of 92% and specificity of 96% on 1,138 scans of various applications.18
The technique of right lower quadrant ultrasound involves graded compression with a 5-7MHz linear probe optimizing lateral resolution and depth of penetration. Uniform pressure at the point of maximal pain displaces gasfilled bowel from the field of view, allowing visualization of the appendix.
The primary criterion for sonographic diagnosis of appendicitis is a non-compressible, 6 mm, blind-ended, tubular structure at the base of the cecum without peristalsis. 19,20 Secondary signs include circumferential hyperemia in transverse section by color-flow Doppler, peri-appendiceal fluid collections, visible appendicolith, and interruption of the echogenic submucosa (indicating perforation). 13,21 Conversely, an ovoid shape in the transverse plane along the entire appendiceal length reliably excludes appendicitis. 22 Using these criteria, radiologists have reported sensitivities of 75 to 90%, specificities of 86 to 100%, and positive predictive values of 91 to 94%. 14,23,24 Obermaier reviewed 69 publications of ultrasound in appendicitis and found no differences between surgeons and radiologists. 25 It is unclear whether emergency physicians can duplicate this accuracy.
Only one study has evaluated EPs’ accuracy in diagnosing appendicitis with ultrasound. 26 EPs completed a standard course of intensive training in gastrointestinal ultrasound and had 12 months of ultrasound experience. This group prospectively divided 317 patients with RLQ pain into two groups: those diagnosed by EP ultrasound and those by surgical judgment alone. Criterion references were pathology reports or two-week clinical follow-up. The EP ultrasound group had a sensitivity of 96.4% and a specificity of 67.6%, while the surgical judgment group had statistically inferior sensitivity (86.2%) and specificity (37.0%). It is difficult to generalize these results to other settings given the extensive ultrasound training and the 72% prevalence of appendicitis in their cohort. However, this study likely provides a ceiling of accuracy.
By contrast the current study assesses the floor and establishes a baseline from which to study the learning curve. Our physicians already knew the basics of ultrasound – how to optimize depth, gain, frequency, transducer selection, and patient positioning. We assessed whether EPs can expand their previous skill set and adapt to this new application.
Ultrasound of the appendix is one of the most “operator dependent” and difficult applications. 27,28 Our sensitivity of 39% underscores this. A prospective study is underway to assess whether a feasible level of EP training yields sufficient accuracy to justify widespread adoption.
Limitations:
By design, EPs were not trained in appendicitis ultrasound in order to assess baseline accuracy. Furthermore, EPs were not blinded to the clinical presentation of the patient. While this impairs scientific assessment of imaging in isolation, the clinician’s integration of ultrasound with the clinical presentation offers a distinct advantage.
A common limitation of retrospective registry-based studies is the lack of investigator control of examined variables, which can sometimes be affected by motivation, attitude, or cognitive issues of those entering data into the registry. These variables can limit the validity and generalizability of findings.
Additionally, no effort was made to control for variability in physician training. Three attending physicians were RDMS-abdomen certified, while others were residents with as little as 50 prior scans. No physician in the study had any previous experience with appendicitis ultrasound.
Finally, because we limited the diagnostic criteria (only non-compressible RLQ tubular structure ≥ 6mm was used), we may have underestimated the ability to diagnose appendicitis by other signs, such as fluid collections and discontinuity of the mucosal wall indicative of appendiceal perforation. These secondary diagnostic criteria could improve identification of patients with more advanced disease.
CONCLUSION
Emergency physicians without focused training cannot use bedside ultrasound to reliably diagnose patients with right lower quadrant pain. Until a prospective study following proper training demonstrates reasonable diagnostic accuracy, EPs should use more standard imaging methods.
REFERENCES
- 1.Brewer BJ, Golden GT, Hitch DC, Rudolf LE, Wangensteen SL. Abdominal pain. An analysis of 1,000 consecutive cases in a University Hospital emergency room. Am J Surg. 1976;131:219–23. doi: 10.1016/0002-9610(76)90101-x. [DOI] [PubMed] [Google Scholar]
- 2.Caterino S, Cavallini M, Meli C, Murante G, Schiffini L, Lotitio S, et al. Acute abdominal pain in emergency surgery. Clinical epidemiologic study of 450 patients. Ann Ital Chir. 1997;68(6):807–17. [PubMed] [Google Scholar]
- 3.Simmen HP, Decurtins M, Rotzer A, Duff C, Brutsch HP, Largiader F. Emergency room patients with abdominal pain unrelated to trauma: prospective analysis in a surgical university hospital. Hepatogastroenterology. 1991;38(4):279–82. [PubMed] [Google Scholar]
- 4.Paulson EK, Kalady MF, Pappas TN. Clinical practice. Suspected appendicitis. N Engl J Med. 2003 Jan 16;348(3):236–42. doi: 10.1056/NEJMcp013351. [DOI] [PubMed] [Google Scholar]
- 5.Flum DR, McClure TD, Morris A, Koepsell T. Misdiagnosis of appendicitis and the use of diagnostic imaging. J Am Coll Surg. 2005 Dec;201(6):933–9. doi: 10.1016/j.jamcollsurg.2005.04.039. [DOI] [PubMed] [Google Scholar]
- 6.Trautlein JJ, Lambert RL, Miller J.Malpractice in the Emergency Department--review of 200 cases Ann Emerg Med 198413(9 Pt 1):709–11. [DOI] [PubMed] [Google Scholar]
- 7.Reynolds SL, Jaffe DM, Glynn W. Professional liability in the pediatric emergency department. Pediatrics. 1991;87(2):134–7. [PubMed] [Google Scholar]
- 8.Roosevelt GE, Reynolds SL. Does the use of ultrasonography improve the outcome of children with appendicitis? Acad Emerg Med. 1998;5(11):1071–5. doi: 10.1111/j.1553-2712.1998.tb02664.x. [DOI] [PubMed] [Google Scholar]
- 9.Chen SC, Wang HP, Hsu HY, Huang PM, Lin FY. Accuracy of ED sonography in the diagnosis of acute appendicitis. Am J Emerg Med. 2000;18(4):449–52. doi: 10.1053/ajem.2000.7343. [DOI] [PubMed] [Google Scholar]
- 10.McCraig LF, Burt CW. Advance data from vital and health statistics No 320. Hyattsville, Md.: National Center for Health Statistics; 2001. National Hospital Ambulatory Medical Care Survey: 1999 emergency department summary; p. 24. [PubMed] [Google Scholar]
- 11.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910–25. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 12.Colson M, Skinner KA, Dunnington G. High negative appendectomy rates are no longer acceptable. Am J Surg. 1997;174(6):723–7. doi: 10.1016/s0002-9610(97)00183-9. [DOI] [PubMed] [Google Scholar]
- 13.Von Titte SN, McCabe CJ, Ottinger LW. Delayed appendectomy for appendicitis: causes and consequences. Am J Emerg Med. 1996;14(7):620–2. doi: 10.1016/S0735-6757(96)90074-1. [DOI] [PubMed] [Google Scholar]
- 14.Cook T, Roepke T. Prevalence and structure of ultrasound curricula in emergency medicine residencies. J Emerg Med. 1998;16(4):655–7. doi: 10.1016/s0736-4679(98)00064-x. [DOI] [PubMed] [Google Scholar]
- 15.Schlager D, Lazzareschi G, Whitten D, Sanders AB. A prospective study of ultrasonography in the ED by emergency physicians. Am J Emerg Med. 1994;12(2):185–9. doi: 10.1016/0735-6757(94)90244-5. [DOI] [PubMed] [Google Scholar]
- 16.Lanoix R, Leak LV, Gaeta T, Gernsheimer JR. A preliminary evaluation of emergency ultrasound in the setting of an emergency medicine training program. Am J Emerg Med. 2000;18(1):42–5. doi: 10.1016/s0735-6757(00)90046-9. [DOI] [PubMed] [Google Scholar]
- 17.Kuhn M, Bonnin RL, Davey MJ, Rowland JL, Langlois SL. Emergency department ultrasound scanning for abdominal aortic aneursym: accessible, accurate, and advantageous. Ann Emerg Med. 2000;36(3):219–23. doi: 10.1067/mem.2000.108616. [DOI] [PubMed] [Google Scholar]
- 18.Mandavia DP, Aragona J, Chan L, Chan D, Henderson SO. Ultrasound training for emergency physicians-a prospective study. Acad Emerg Med. 2000;7(9):1008–14. doi: 10.1111/j.1553-2712.2000.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 19.Kessler N, Cyteval C, Gallix B, Lesnik A, Blayac PM, Pujol J, et al. Appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US, and laboratory findings. Radiology. 2004;230(2):472–8. doi: 10.1148/radiol.2302021520. [DOI] [PubMed] [Google Scholar]
- 20.Jeffrey RB, Jr, Laing FC, Townsend RR. Acute appendicitis: sonographic criteria based on 250 cases. Radiology. 1988;167:327–9. doi: 10.1148/radiology.167.2.3282253. [DOI] [PubMed] [Google Scholar]
- 21.Birnbaum B, Wilson S. Appendicitis at the millennium. Radiology. 2000;215:337–348. doi: 10.1148/radiology.215.2.r00ma24337. [DOI] [PubMed] [Google Scholar]
- 22.Rettenbacher T, Hollerweger A. Ovoid shape of the vermiform appendix: a criterion to exclude acute appendicitis evaluation with US. Radiology. 2003;226:95–100. doi: 10.1148/radiol.2261011496. [DOI] [PubMed] [Google Scholar]
- 23.Paulson EK, Kalady MF, Pappas TN. Clinical practice. Suspected appendicitis. N Engl J Med. 2003 Jan 16;348(3):236–42. doi: 10.1056/NEJMcp013351. [DOI] [PubMed] [Google Scholar]
- 24.Poortman P, Lohle PN, Schoemaker CM. Comparison of CT and sonography in the diagnosis of acute appendicitis: a blinded prospective study. Am J Roentgenol. 2003;181(5):1355–9. doi: 10.2214/ajr.181.5.1811355. [DOI] [PubMed] [Google Scholar]
- 25.Obermaier R, Benz S, Asgharnia M, Kirchner R, Hope UT. Value of ultrasound in the diagnosis of acute appendicitis: interesting aspects. Eur J Med Res. 2003;8(10):451–6. [PubMed] [Google Scholar]
- 26.Chen S, Wang H, Hsu H, Huang P, Lin F. Accuracy of ED sonography in the diagnosis of acute appendicitis. Am J Emerg Med. 1990 Jul;18(4):449–452. doi: 10.1053/ajem.2000.7343. [DOI] [PubMed] [Google Scholar]
- 27.Birnholz JC, Hayes T. The effect of instrumentation and examination. In: McGahan JP, editor. Controversis in ultrasound. New York: Churchill Livingstone; 1987. pp. 143–52. [Google Scholar]
- 28.Pohl D, Golub R, Schwartz G, Stein H. Appendiceal ultrasonography performed by nonradiologists: Does it help in the diagnostic process? J Ultrasound Med. 1998;(17):217–221. doi: 10.7863/jum.1998.17.4.217. [DOI] [PubMed] [Google Scholar]


