Abstract
Purpose
Bevacizumab is an antibody that binds vascular endothelial growth factor and has activity in metastatic renal cell carcinoma (RCC). Interferon alfa (IFN-α) is the historic standard initial treatment for RCC. A prospective, randomized, phase III trial of bevacizumab plus IFN-α versus IFN-α monotherapy was conducted.
Patients and Methods
Patients with previously untreated, metastatic clear cell RCC were randomly assigned to receive either bevacizumab (10 mg/kg intravenously every 2 weeks) plus IFN-α (9 million units subcutaneously three times weekly) or the same dose and schedule of IFN-α monotherapy in a multicenter phase III trial. The primary end point was overall survival (OS). Secondary end points were progression-free survival (PFS), objective response rate, and safety.
Results
Seven hundred thirty-two patients were enrolled. The median OS time was 18.3 months (95% CI, 16.5 to 22.5 months) for bevacizumab plus IFN-α and 17.4 months (95% CI, 14.4 to 20.0 months) for IFN-α monotherapy (unstratified log-rank P = .097). Adjusting on stratification factors, the hazard ratio was 0.86 (95% CI, 0.73 to 1.01; stratified log-rank P = .069) favoring bevacizumab plus IFN-α. There was significantly more grade 3 to 4 hypertension (HTN), anorexia, fatigue, and proteinuria for bevacizumab plus IFN-α. Patients who developed HTN on bevacizumab plus IFN-α had a significantly improved PFS and OS versus patients without HTN.
Conclusion
OS favored the bevacizumab plus IFN-α arm but did not meet the predefined criteria for significance. HTN may be a biomarker of outcome with bevacizumab plus IFN-α.
INTRODUCTION
Metastatic renal cell carcinoma (RCC) has historically been treated with interferon alfa (IFN-α), with a 10% to 15% objective response rate and a median survival time of 12 months.1–3 IFN-α has also demonstrated a modest overall survival (OS) advantage over hormones and chemotherapy in randomized trials and a meta-analysis.1,2,4 The addition of interleukin-2, hormones, or antiproliferative agents such as cis-retinoic acid has not demonstrated significant advantages over IFN-α monotherapy in randomized trials.5–7 Thus, until the recent development of agents targeting the vascular endothelial growth factor (VEGF) and mammalian target of rapamycin pathways, IFN-α (and high-dose interleukin-2 in highly select patients based on durable complete responses) has been the historic standard of care.
More recently, the pathogenesis of RCC has been further elucidated, resulting in identification of relevant therapeutic targets. RCC is characterized by inactivation of a tumor suppressor gene known as Von Hippel-Lindau (VHL), the downstream effect of which is activation of the hypoxia response pathway and transcription of several genes, including VEGF.8–11 VEGF is a potent proangiogenic protein, acting through its cognate receptor and leading to increased vascular permeability and endothelial cell proliferation and migration.12 Phase III trials have demonstrated substantial clinical benefit from blocking the VEGF receptor with the small-molecule inhibitors sunitinib and sorafenib.13,14 Although a numerical OS advantage was demonstrated, the trials failed to meet prespecified statistical criteria for benefit. For example, sunitinib-treated patients had a median OS time of 26.4 months compared with 21.8 months for IFN-treated patients (P = .051).15 Sorafenib-treated patients had a median OS time of 17.8 months compared with 15.2 months for patients treated with placebo (hazard ratio [HR] = 0.88; 95% CI, 0.74 to 1.04; P = .15).16 In both trials, there was substantial patient cross over to subsequent active therapy, likely contributing to the lack of a demonstrable survival advantage.
Bevacizumab (Avastin; Genentech, South San Francisco, CA), an antibody that binds to circulating VEGF protein, produced a significant prolongation of time to disease progression compared with placebo in patients with treatment-refractory metastatic RCC in a small randomized trial.17 In addition, IFN has demonstrated antiangiogenic effects,18 and antibody-mediated VEGF inhibition has antitumor effects through improvement in dendritic cell function.19 Given these considerations, two phase III trials (a European study and the present study conducted by the Cancer and Leukemia Group B [CALGB]) were simultaneously undertaken and randomly assigned patients with metastatic RCC to IFN-α monotherapy or IFN-α plus bevacizumab. Both studies have previously reported significant advantages in objective response rate and progression-free survival (PFS) for bevacizumab plus IFN-α compared with IFN-α alone.20,21 The final OS results, the primary end point of the CALGB trial, are now reported here.
PATIENTS AND METHODS
Patients
Patients with metastatic RCC, a clear cell histologic component, and no prior systemic therapy for RCC were enrolled as previously described.21 Major eligibility criteria included a Karnofsky performance status of ≥ 70%; adequate end organ function; blood pressure less than 160/90 mmHg; and lack of CNS metastases, significant cardiac comorbidity, or recent history of bleeding or clotting. The protocol was approved by the central Institutional Review Board of the US National Cancer Institute (NCI) and by the institutional review board of each participating site, and all patients provided written informed consent.
Study Design
This study was conducted by the CALGB with the support of the Eastern Cooperative Oncology Group (ECOG), the National Cancer Institute of Canada Clinical Trials Group, and the NCI Cancer Trials Support Unit. Patients were randomly assigned with equal probability to receive either bevacizumab (10 mg/kg given intravenously every 2 weeks) plus IFN-α (9 million units [MU] subcutaneously three times a week) or the same dose and schedule of IFN-α as monotherapy. A stratified random block design was used, with random assignment stratified by nephrectomy status (yes v no) and number of adverse prognostic factors (zero, one to two, or ≥ three factors), which has been previously described for patients with metastatic RCC receiving IFN-based initial systemic therapy.3 Dose modifications for toxicity were undertaken as previously described.21
Bevacizumab was provided by the NCI Cancer Therapy Evaluation Program and was administered at a dose of 10 mg/kg actual body weight intravenously on days 1 and 15 of each 28-day cycle. IFN-α-2b (Intron; Schering, Kenilworth, NJ) was provided by the Cancer Therapy Evaluation Program and administered identically in both arms (subcutaneously at a starting dose of 9 MU on 3 nonconsecutive days per week with dose reduction to 6 MU and 3 MU permitted for IFN-related toxicity). Treatment was continued until disease progression per investigator assessment according to Response Evaluation Criteria in Solid Tumors (RECIST),22 unacceptable toxicity, or withdrawal of consent.
Efficacy and Safety
Response and progression were assessed according to the RECIST criteria and were determined by investigator assessment of radiographs. Tumor assessments were performed at baseline and every 12 weeks. Adverse events were graded according to the NCI Common Terminology Criteria for Adverse Events (version 3).
Statistical Design and Data Analysis
The primary end point was OS, which was defined as the time from registration to death as a result of any cause, with a target sample size of 700 patients. The following assumptions were made: an annual accrual rate of 233 patients accrued over a 3-year enrollment period (based on previous CALGB RCC trial accrual), a 2-year follow-up period, and survival time followed an exponential distribution. The trial was designed with 86% power to detect an HR of 0.76 (a 30% improvement in median survival in patients randomly assigned to bevacizumab plus IFN-α compared with patients assigned to IFN-α monotherapy) assuming a two-sided significance level of P = .05. The primary analysis of the OS end point was based on the stratified log-rank statistic. Secondary end points were PFS (defined from the date of random assignment to date of progression using RECIST criteria according to the first tumor assessment where disease progression was observed or death as a result of any cause, whichever occurred first), objective response rate using RECIST criteria, and safety. Patients who discontinued treatment for reasons other than progression were observed for disease progression or death.
The Lan and Demets analog of the O'Brien-Fleming sequential boundary was used to maintain the overall significance level of α = .05 while conducting interim analyses of the OS end point. Under the alternative hypotheses, 588 deaths were expected at the end of the trial. An intent-to-treat approach was used in the analysis. In addition, the Kaplan-Meier product-limit method was used to estimate the PFS time and duration of response in the two arms. The analysis of the PFS end point was based on a two-sided stratified log-rank test comparing the two arms, and the threshold for significance was P = .05. The χ2 test and Fisher's exact test were used to compare objective response rates and adverse events between the two treatment groups, respectively. All analyses were performed using SAS software (version 9.1; SAS Institute, Cary, NC).
CALGB Statistical Center personnel were responsible for patient registration, data collection, and quality assurance for all the data submitted by the participating institutions. Statistical analyses were performed by CALGB statisticians. As part of the quality assurance program of the CALGB, members of the Audit Committee visit all participating CALGB institutions at least once every 3 years to review source documents. The auditors verify compliance with federal regulations and protocol requirements, including those pertaining to eligibility, treatment, adverse events, tumor response, and outcome in a sample of protocols at each institution. Such on-site review of medical records was performed for a subgroup of 177 patients (24.2%) of the 732 patients enrolled onto this study, and no major problems or discrepancies were identified. The data presented here for clinical and safety parameters used a data cutoff date of March 24, 2009, representing 17 months of additional follow-up from the original report.21
RESULTS
Patient Characteristics
Between October 2003 and July 2005, 732 patients were enrolled. As previously reported, patients were predominantly male, 62% had ECOG performance status of 0, and 85% had prior nephrectomy. Twenty-six percent, 64%, and 10% of patients had good-risk, intermediate-risk, and poor-risk disease, respectively.3
Treatment Administration
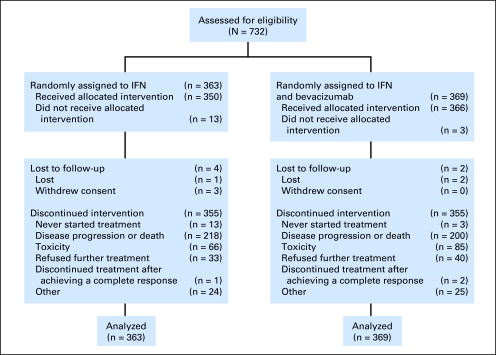
Three hundred sixty-three patients were randomly assigned to IFN-α monotherapy, and 369 were assigned to combination therapy (Fig 1). Patients on IFN-α monotherapy received a median of 4.2 cycles of therapy (range, 0.2 to 57 cycles) compared with 8.2 cycles (range, one to 59 cycles) in patients receiving bevacizumab plus IFN-α. Dose reductions of IFN-α to 6 MU and 3 MU were undertaken in 136 patients (37%) and 37 patients (10%), respectively, on the IFN-α monotherapy arm and in 170 patients (46%) and 68 patients (18%), respectively, on the bevacizumab plus IFN-α arm. In aggregate, treatment delays occurred in 31.6% of patients receiving IFN-α and 61.7% of patients receiving IFN-α plus bevacizumab. The majority of IFN-α dose modifications and delays were caused by fatigue. The majority of patients discontinued treatment as a result of disease progression or death (Fig 1).
Fig 1.
CONSORT diagram. IFN, interferon.
OS
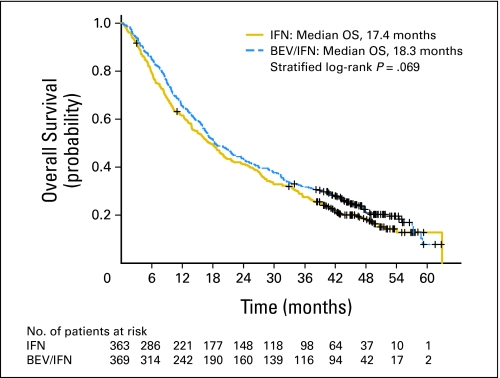
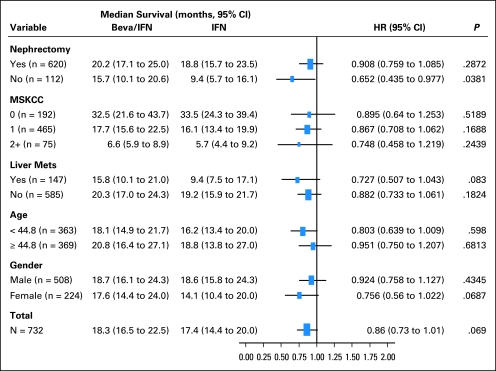
The median OS time was 18.3 months (95% CI, 16.5 to 22.5 months) for bevacizumab plus IFN-α and 17.4 months (95% CI, 14.4 to 20.0 months) for IFN-α monotherapy (unstratified log-rank P = .097; Fig 2). Adjusting on stratification factors, the HR was 0.86 (95% CI, 0.73 to 1.01; stratified log-rank P = .069) for patients receiving bevacizumab plus IFN-α compared with patients receiving IFN-α. The median duration of follow-up among surviving patients was 46.2 months (interquartile range, 45.2 to 48.2 months). Using Clark's C,23 the completeness of follow-up for this study is 95.7%. Applying Wu's modification to adjust for unreported deaths,24 the completeness of follow-up is 96.9%. The median OS times in the bevacizumab plus IFN-α and IFN-α arms were 32.5 months (95% CI, 21.6 to 43.7 months) and 33.5 months (95% CI, 24.3 to 39.4 months; P = .5189) for Memorial Sloan-Kettering Cancer Center good-risk patients, respectively; 17.7 months (95% CI, 15.6 to 22.5 months) and 16.1 months (95% CI, 13.4 to 19.9 months; P = .1688) for intermediate-risk patients, respectively; and 6.6 months (95% CI, 5.9 to 8.9 months) and 5.7 months (95% CI, 4.4 to 9.2 months; P = .2439) for poor-risk patients, respectively. Noting the limitations of subgroup analysis, the HRs for death for bevacizumab plus IFN-α versus IFN-α were 0.89, 0.87, and 0.76 for the good-, intermediate-, and poor-risk groups, respectively. There was no significant difference in OS when evaluated according to nephrectomy status, presence of liver metastases, age, or sex (Fig 3).
Fig 2.
Overall survival (OS) according to treatment arm. IFN, interferon; BEV, bevacizumab.
Fig 3.
Forest plot of overall survival of selected subgroups. HR, hazard ratio; IFN, interferon; Beva, bevacizumab; MSKCC, Memorial Sloan-Kettering Cancer Center; Mets, metastases.
No cross over on trial was permitted for patients randomly assigned to IFN-α monotherapy. Nonetheless, a substantial percentage of patients on both arms received systemic anticancer therapy subsequent to progression (62% of patients on IFN-α monotherapy and 54% of patients on bevacizumab plus IFN-α). The majority of these patients received VEGF-targeted agents such as sunitinib and sorafenib, which became available during the conduct of this trial.
Given the potential confounding effects of subsequent anticancer therapy on OS, a post hoc analysis was performed on patients who did not receive treatment after discontinuation of protocol therapy (n = 324) and patients who received subsequent therapy (n = 408). Notably, patients who received subsequent therapy, compared with those who did not, had more favorable baseline prognostic features, including a significantly higher percentage of patients with ECOG performance status of 0 (67% v 56%, respectively; P = .012), a greater percentage of patients with prior nephrectomy (88% v 80%, respectively; P = .004), and significantly more good-risk patients (29% v 22%) and fewer poor-risk patients (6% v 15%, respectively; P < .001). As seen in Table 1, the median OS time was greater for patients who received subsequent therapy, regardless of treatment arm. Furthermore, the HR for OS was consistent, favoring the patients receiving bevacizumab plus IFN-α regardless of receipt of subsequent therapy.
Table 1.
OS According to Treatment Arm and Subsequent Therapy
| Subsequent Therapy | No. of Patients | OS (months) |
Adjusted HR* | 95% CI | P | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bevacizumab + IFN-α (n = 369) |
IFN-α (n = 363) |
All Patients (N = 732) |
|||||||||
| Median | 95% CI | Median | 95% CI | Median | 95% CI | P | |||||
| Received | 408 | 31.4 | 25.6 to 37.8 | 26.8 | 21.5 to 29.4 | 28.2 | 25.6 to 32.3 | .079 | 0.80 | 0.64 to 1.01 | .055 |
| Did not receive | 324 | 13.1 | 10.0 to 15.7 | 9.1 | 7.8 to 10.2 | 10.2 | 9.1 to 13.0 | .059 | 0.82 | 0.65 to 1.04 | .108 |
| Total | 732 | 18.3 | 16.5 to 22.5 | 17.4 | 14.4 to 20.0 | 18.1 | 16.4 to 20.2 | .097 | 0.86 | 0.73 to 1.01 | .069 |
Abbreviations: OS, overall survival; IFN-α, interferon alfa; HR, hazard ratio.
HR for death for patients treated with bevacizumab plus IFN-α compared with IFN-α monotherapy adjusted by nephrectomy status (yes v no) and number of adverse prognostic factors (zero, one to two, or ≥ three factors).
Adverse Events
In patients evaluable for toxicity (n = 347 for IFN-α and n = 362 for bevacizumab plus IFN-α), 80% of patients receiving bevacizumab plus IFN-α experienced grade ≥ 3 toxicity compared with 63% of patients receiving IFN-α monotherapy (P < .001; Table 2). Noting that patients receiving combination therapy had a duration of treatment that averaged 4 months longer than IFN-α monotherapy, bevacizumab plus IFN-α resulted in significantly more grade ≥ 3 hypertension (HTN; 11% v 0%, respectively), anorexia (17% v 8%, respectively), fatigue (37% v 30%, respectively), and proteinuria (15% v < 1%, respectively). The incidence of grade 4 neutropenia and anemia was low in each arm, and there were no differences in the rate of febrile neutropenia or requirement for RBC transfusion (each < 1%). There were four treatment-related deaths on the IFN-α monotherapy arm and three on the bevacizumab plus IFN-α arm.
Table 2.
Treatment-Related Adverse Events
| Adverse Event | Bevacizumab + Interferon Alfa (n = 362) |
Interferon Alfa Monotherapy (n = 347) |
||||||
|---|---|---|---|---|---|---|---|---|
| All Grades |
Grade ≥ 3 |
All Grades |
Grade ≥ 3 |
|||||
| No. of Patients | % | No. of Patients | % | No. of Patients | % | No. of Patients | % | |
| Hematologic | ||||||||
| Anemia | 59 | 16 | 14 | 4 | 76 | 20 | 13 | 4 |
| Neutropenia | 158 | 43 | 33 | 9 | 124 | 36 | 31 | 9 |
| Thrombocytopenia | 38 | 10 | 8 | 2 | 30 | 9 | 2 | < 1 |
| Nonhematologic | ||||||||
| Cardiovascular | ||||||||
| Cardiac ischemia/infarction | 5 | 1 | 5 | 1 | 0 | 0 | 0 | 0 |
| Left ventricular dysfunction | 2 | < 1 | 2 | < 1 | 0 | 0 | 0 | 0 |
| Hypertension | 103 | 28 | 39 | 11 | 13 | 4 | 0 | 0 |
| Thrombosis/embolism | 14 | 4 | 6 | 2 | 6 | 2 | 3 | < 1 |
| Constitutional symptoms | ||||||||
| Fatigue | 336 | 93 | 135 | 37 | 312 | 90 | 105 | 30 |
| Weight loss | 57 | 16 | 15 | 4 | 42 | 12 | 5 | 1 |
| Endocrine | ||||||||
| Thyroid dysfunction | 2 | < 1 | 2 | < 1 | 0 | 0 | 0 | 0 |
| GI | ||||||||
| Anorexia | 258 | 71 | 63 | 17 | 213 | 61 | 28 | 8 |
| Nausea | 210 | 58 | 26 | 7 | 204 | 59 | 17 | 5 |
| Perforation, GI | 0 | 0 | 1 | < 1 | 0 | 0 | 0 | 0 |
| Hemorrhage/bleeding | ||||||||
| Hemorrhage, genitourinary | 3 | < 1 | 0 | 0 | 1 | < 1 | 0 | 0 |
| Hemorrhage, GI | 18 | 5 | 4 | 1 | 3 | < 1 | 1 | < 1 |
| CNS | ||||||||
| CNS cerebrovascular ischemia | 5 | 1 | 5 | 1 | 0 | 0 | 1 | < 1 |
| Pulmonary | ||||||||
| Dyspnea | 53 | 15 | 23 | 6 | 32 | 9 | 12 | 3 |
| Pneumonitis/pulmonary infiltrates | 3 | < 1 | 1 | < 1 | 4 | 1 | 3 | < 1 |
| Renal | ||||||||
| Proteinuria | 257 | 71 | 56 | 15 | 24 | 10 | 1 | < 1 |
| Maximum overall adverse events | 360 | 99 | 290 | 80 | 340 | 98 | 217 | 63 |
HTN As a Biomarker of Clinical Outcome to Bevacizumab Plus IFN-α
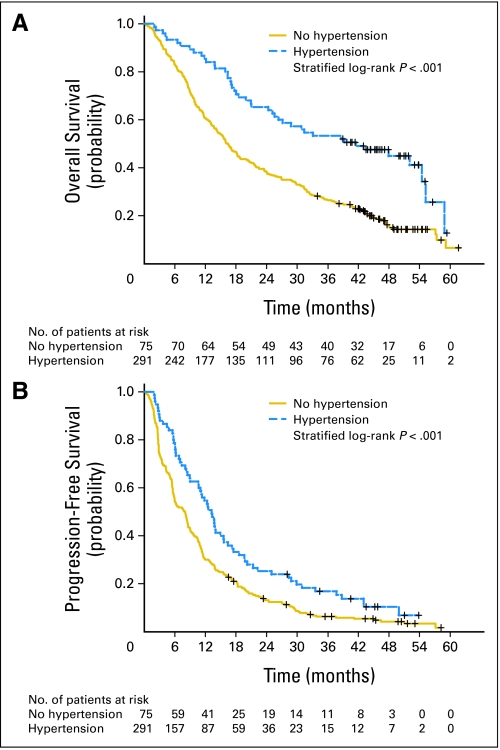
Given the observation with bevacizumab-based therapy in breast cancer25 and across solid tumors (including RCC) with a VEGF receptor inhibitor that treatment-induced HTN may be a biomarker of clinical outcome,26 a retrospective analysis of the current trial was undertaken. Ten (3%) of 350 patients on IFN-α monotherapy and 75 (21%) of 366 patients on bevacizumab plus IFN-α who received therapy and had available blood pressure data developed grade ≥ 2 HTN. There was no difference in baseline prognostic factors between patients who did or did not develop HTN, with the possible exception of a higher percentage of prior nephrectomy in patients who developed HTN (92% v 83%, respectively; P = .049). Patients on bevacizumab plus IFN-α who developed grade ≥ 2 HTN of any relation to study therapy had a significantly greater PFS and OS compared with patients who did not develop HTN (Table 3, Fig 4). There was no significant difference in the objective response rate based on the development of HTN. Results were similar when the analysis was restricted to the development of grade ≥ 3 HTN; to patients with HTN possibly, probably, or definitely related to study therapy; or to a landmark analysis of the development of HTN at 2 or 3 months on study therapy. On multivariate analysis, the development of HTN at 2 months was an independent predictor of OS, with an HR of 0.622 (95% CI, 0.390 to 0.992; P = .046). An analysis of HTN as a biomarker in the IFN-α monotherapy arm was not possible because of the limited number of events.
Table 3.
Clinical Outcome to Bevacizumab Plus Interferon Alfa According to the Development of Grade ≥ 2 Hypertension
| Outcome | Patients With Grade ≥ 2 Hypertension* (n = 75) | Patients Without Grade ≥ 2 Hypertension (n = 291) |
|---|---|---|
| ORR, % | 13.1 | 9.0 |
| 95% CI | 9.7 to 16.7 | 6.3 to 18.9 |
| P | .95 | |
| PFS, months | 13.2 | 8.0 |
| 95% CI | 10.6 to 15.5 | 5.9 to 8.6 |
| P | < .001 | |
| OS, months | 41.6 | 16.2 |
| 95% CI | 26.3 to 55.1 | 14.2 to 18.7 |
| P | < .001 | |
Abbreviations: ORR, objective response rate; PFS, progression-free survival; OS, overall survival.
Any relation to therapy according to Common Terminology Criteria for Adverse Events (version 3).
Fig 4.
Kaplan-Meier (A) overall survival and (B) progression-free survival according to development of grade ≥ 2 hypertension on bevacizumab plus interferon alfa.
DISCUSSION
This prospective randomized trial demonstrated a greater OS time in patients with metastatic clear cell RCC receiving bevacizumab plus IFN-α as initial systemic therapy compared with IFN-α alone, but the difference did not meet predefined criteria for statistical significance. However, the clinical benefit derived from the addition of bevacizumab to IFN-α is evident in the statistically significantly prolonged PFS and increased objective response rate, as reported previously in this trial and in a similar phase III trial.20,21
Although precedent certainly exists for trials in which improvements in PFS and objective response rate do not translate into an improvement in OS, an alternative explanation for the results observed in this trial are the confounding effects of the emergence of multiple active therapeutic options during the conduct of this trial. The majority of patients on this trial received one or more active therapies on disease progression before death. Therefore, it is possible that the initial impact of more favorable disease control with bevacizumab plus IFN-α (as reflected by the PFS advantage) did not translate into a statistically significant OS advantage for this reason. Although the HR for OS for bevacizumab plus IFN-α is preserved regardless of subsequent treatment, the most robust OS was achieved in patients who received initial bevacizumab-based therapy and then received subsequent therapy; in this case, the adjusted HR in favor of bevacizumab plus IFN-α approached significance with a P = .055. Indeed, the cohort of patients who received subsequent therapy after initial bevacizumab plus IFN-α had an OS time greater than 2.5 years.
These results are not surprising. First, baseline prognostic features such as performance status and risk group classification continue to influence outcome in metastatic RCC, even in the current era of active targeted therapy. Patients with the most favorable underlying disease biology will be fit enough at disease progression to receive further therapy. In addition, further therapy will include agents with proven antitumor activity in the treatment-refractory setting, extending control of tumor burden and thus OS.13,27,28 The fact that other contemporary phase III trials, including trials investigating sunitinib and sorafenib and the other phase III investigation of IFN-α plus bevacizumab versus IFN-α, have also failed to demonstrate a statistically significant OS advantage suggests that the same confounding effect of subsequent active therapy is operative.13,15 Indeed, the HRs for OS in favor of therapy containing VEGF-targeted treatment were identical across the current trial, a similar international trial comparing bevacizumab plus IFN-α to IFN-α monotherapy, and the phase III trial of sunitinib versus IFN-α. These similarities suggest a significant and consistent OS advantage of VEGF-targeted therapy compared with the historical standard of cytokine monotherapy. The numerical differences across trials in median OS likely reflect differences in patient selection. Furthermore, until new classes of active agents are developed, it is likely that clinical benefit in metastatic RCC trials will continue to be defined by a PFS end point. Indeed, the European and US regulatory authorities recently approved the combination of bevacizumab plus IFN-α for the treatment of metastatic RCC based on a PFS end point.
This study is limited by the lack of a placebo control arm and lack of independent review of radiographs. However, the objective response rate and HR for PFS demonstrated in this trial mirrored a similarly designed international trial that used both a placebo control and independent review of radiographs.20
Subset analysis failed to identify patient subgroups (according to baseline factors) with significantly better or significantly worse outcomes to bevacizumab plus IFN-α. Noting the limitations of retrospective subset analyses, these data highlight the fact that the current management of patients with metastatic RCC is empiric, based on data derived from clinical trials. Intriguingly, the development of HTN with bevacizumab plus IFN-α treatment identified a group of patients with superior clinical outcome, consistent with this observation across solid tumors and with multiple VEGF-targeted therapies. Further investigation of the underlying biology of this observation is warranted to maximally exploit this phenomenon for therapeutic benefit. The combination of IFN-α and bevacizumab is clearly a treatment option to be considered for patients with metastatic RCC. Perceived relative risks and benefits of each therapy, patient preference, availability in a given country including cost considerations, and physician experience all feed into the complex equation of individualized therapy. The development of patient- and/or tumor-specific characteristics to educate the risk-benefit ratio for a single patient should be a top research priority.
Appendix
The following institutions participated in this study: University of Oklahoma, Oklahoma, OK–Howard Ozer, MD, supported by CA37447; Christiana Care Health Services, Community Clinical Oncology Program (CCOP), Wilmington, DE–Stephen Grubbs, MD, supported by CA45418; Dana-Farber Cancer Institute, Boston, MA–Eric P. Winer, MD, supported by CA32291; Duke University Medical Center, Durham, NC–Jeffrey Crawford, MD; Evanston Northwestern Healthcare CCOP, Evanston, IL–Gershon Y. Locker, MD; Georgetown University Medical Center, Washington, DC–Minetta C. Liu, MD, supported by CA77597; Grand Rapids Clinical Oncology Program, Grand Rapids, MI–Marianne Lange, MD; Greenville CCOP, see above Cancer Center of Carolinas; Hematology-Oncology Associates of Central New York, Syracuse, NY–Jeffrey Kirshner, MD, supported by CA45389; Illinois Oncology Research Association, Peoria, IL–John W. Kugler, MD, supported by CA35113; Kansas City Community Clinical Oncology Program CCOP, Kansas City, MO–Jorge C. Paradelo, MD; Massachusetts General Hospital, Boston, MA–Michael L. Grossbard, MD, supported by CA12449; Missouri Baptist Medical Center, St Louis, MO–Alan P. Lyss, MD, supported by CA114558-02; Missouri Valley Cancer Consortium, Omaha, NE–Gamini S. Soori, MD; Mount Sinai Medical Center, Miami, FL–Rogerio Lilenbaum, MD, supported by CA45564; Mount Sinai School of Medicine, New York, NY–Lewis R. Silverman, MD, supported by CA04457; Nevada Cancer Research Foundation CCOP, Las Vegas, NV–John A. Ellerton, MD, supported by CA35421; New Hampshire Oncology-Hematology PA, Hooksett, NH–Douglas J. Weckstein, MD; Northern Indiana Cancer Research Consortium CCOP, South Bend, IN–Rafat Ansari, MD, supported by CA86726; Rhode Island Hospital, Providence, RI–William Sikov, MD, supported by CA08025; Roswell Park Cancer Institute, Buffalo, NY–Ellis Levine, MD, supported by CA02599; Southeast Cancer Control Consortium CCOP, Goldsboro, NC–James N. Atkins, MD, supported by CA45808; State University of New York Upstate Medical University, Syracuse, NY–Stephen L. Graziano, MD, supported by CA21060; The Ohio State University Medical Center, Columbus, OH–Clara D Bloomfield, MD, supported by CA77658; University of California at San Diego, San Diego, CA–Joanne Mortimer, MD, supported by CA11789; University of California at San Francisco, San Francisco, CA–Charles Ryan, MD, supported by CA60138; University of Chicago, Chicago, IL –Gini Fleming, MD, supported by CA41287; University of Illinois MBCCOP, Chicago, IL–Lawrence E. Feldman, MD, supported by CA74811; University of Iowa, Iowa City, IA–Gerald Clamon, MD, supported by CA47642; University of Maryland Greenebaum Cancer Center, Baltimore, MD–Martin Edelman, MD, supported by CA31983; University of Massachusetts Medical School, Worcester, MA–William V. Walsh, MD, supported by CA37135; University of Minnesota, Minneapolis, MN–Bruce A. Peterson, MD, supported by CA16450; University of Missouri/Ellis Fischel Cancer Center, Columbia, MO–Michael C. Perry, MD, supported by CA12046; University of Nebraska Medical Center, Omaha, NE–Anne Kessinger, MD, supported by CA77298; University of North Carolina at Chapel Hill, Chapel Hill, NC–Thomas C. Shea, MD, supported by CA47559; University of Texas Southwestern Medical Center, Dallas, TX–Debasish Tripathy, MD; Wake Forest University School of Medicine, Winston-Salem, NC–David D Hurd, MD, supported by CA03927; Washington University School of Medicine, St Louis, MO–Nancy Bartlett, MD, supported by CA77440; and Western Pennsylvania Cancer Institute, Pittsburgh, PA–Richard K. Shadduck, MD.
Footnotes
See accompanying article on page 2144
Supported in part by National Cancer Institute Grant No. CA31946 to the Cancer and Leukemia Group B (CALGB) and Grant No. CA33601 to the CALGB Statistical Center; and by National Cancer Institute Grants No. CA60138, CA41287, CA47642, CA45808, CA77440, CA14985, and CA77202.
Presented in part at the 45th Annual Meeting of the American Society of Clinical Oncology, May 29-June 2, 2009, Orlando, FL.
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
Clinical trial information can be found for the following: NCT00072046.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory Role: Brian I. Rini, Genentech (C); Walter M. Stadler, Genentech (C); Joel Picus, Genentech (C); Janice Dutcher, Genentech (C), Novartis (C) Stock Ownership: None Honoraria: Joel Picus, Genentech; Janice Dutcher, Pfizer, Novartis Research Funding: Walter M. Stadler, Genentech; Daniel A. Vaena, Genentech; Janice Dutcher, Novartis, Genentech, Pfizer Expert Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Brian I. Rini, Susan Halabi, Jonathan E. Rosenberg, Walter M. Stadler, Eric J. Small
Administrative support: Brian I. Rini, Susan Halabi, Eric J. Small
Provision of study materials or patients: Brian I. Rini, Jonathan E. Rosenberg, Walter M. Stadler, Daniel A. Vaena, James N. Atkins, Joel Picus, Piotr Czaykowski, Janice Dutcher, Eric J. Small
Collection and assembly of data: Brian I. Rini, Susan Halabi, Jonathan E. Rosenberg, Walter M. Stadler, Laura Archer, James N. Atkins, Piotr Czaykowski, Janice Dutcher, Eric J. Small
Data analysis and interpretation: Brian I. Rini, Susan Halabi, Jonathan E. Rosenberg, Walter M. Stadler, Daniel A. Vaena, Laura Archer, James N. Atkins, Joel Picus, Piotr Czaykowski, Janice Dutcher, Eric J. Small
Manuscript writing: Brian I. Rini, Susan Halabi, Jonathan E. Rosenberg, Walter M. Stadler, Daniel A. Vaena, James N. Atkins, Joel Picus, Piotr Czaykowski, Janice Dutcher, Eric J. Small
Final approval of manuscript: Brian I. Rini, Susan Halabi, Jonathan E. Rosenberg, Walter M. Stadler, Daniel A. Vaena, Laura Archer, James N. Atkins, Joel Picus, Piotr Czaykowski, Janice Dutcher, Eric J. Small
REFERENCES
- 1.Medical Research Council Renal Cancer Collaborators. Interferon-alpha and survival in metastatic renal carcinoma: Early results of a randomised controlled trial. Lancet. 1999;353:14–17. [PubMed] [Google Scholar]
- 2.Pyrhönen S, Salminen E, Ruutu M, et al. Prospective randomized trial of interferon alfa-2a plus vinblastine versus vinblastine alone in patients with advanced renal cell cancer. J Clin Oncol. 1999;17:2859–2867. doi: 10.1200/JCO.1999.17.9.2859. [DOI] [PubMed] [Google Scholar]
- 3.Motzer RJ, Bacik J, Murphy BA, et al. Interferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol. 2002;20:289–296. doi: 10.1200/JCO.2002.20.1.289. [DOI] [PubMed] [Google Scholar]
- 4.Coppin C, Porzsolt F, Awa A, et al. Immunotherapy for advanced renal cell cancer. Cochrane Database Syst Rev. 2005;25 doi: 10.1002/14651858.CD001425.pub2. CD001425. [DOI] [PubMed] [Google Scholar]
- 5.Negrier S, Escudier B, Lasset C, et al. Recombinant human interleukin-2, recombinant human interferon alfa-2a, or both in metastatic renal-cell carcinoma: Groupe Francais d'Immunotherapie. N Engl J Med. 1998;338:1272–1278. doi: 10.1056/NEJM199804303381805. [DOI] [PubMed] [Google Scholar]
- 6.Porzsolt F, Messerer D, Hautmann R, et al. Treatment of advanced renal cell cancer with recombinant interferon alpha as a single agent and in combination with medroxyprogesterone acetate: A randomized multicenter trial. J Cancer Res Clin Oncol. 1988;114:95–100. doi: 10.1007/BF00390492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Motzer RJ, Murphy BA, Bacik J, et al. Phase III trial of interferon alfa-2a with or without 13-cis-retinoic acid for patients with advanced renal cell carcinoma. J Clin Oncol. 2000;18:2972–2980. doi: 10.1200/JCO.2000.18.16.2972. [DOI] [PubMed] [Google Scholar]
- 8.Gnarra JR, Tory K, Weng Y, et al. Mutations of the VHL tumour suppressor gene in renal carcinoma. Nat Genet. 1994;7:85–90. doi: 10.1038/ng0594-85. [DOI] [PubMed] [Google Scholar]
- 9.Shuin T, Kondo K, Torigoe S, et al. Frequent somatic mutations and loss of heterozygosity of the von Hippel-Lindau tumor suppressor gene in primary human renal cell carcinomas. Cancer Res. 1994;54:2852–2855. [PubMed] [Google Scholar]
- 10.Wiesener MS, Munchenhagen PM, Berger I, et al. Constitutive activation of hypoxia-inducible genes related to overexpression of hypoxia-inducible factor-1alpha in clear cell renal carcinomas. Cancer Res. 2001;61:5215–5222. [PubMed] [Google Scholar]
- 11.Herman JG, Latif F, Weng Y, et al. Silencing of the VHL tumor-suppressor gene by DNA methylation in renal carcinoma. Proc Natl Acad Sci U S A. 1994;91:9700–9704. doi: 10.1073/pnas.91.21.9700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dvorak HF. Vascular permeability factor/vascular endothelial growth factor: A critical cytokine in tumor angiogenesis and a potential target for diagnosis and therapy. J Clin Oncol. 2002;20:4368–4380. doi: 10.1200/JCO.2002.10.088. [DOI] [PubMed] [Google Scholar]
- 13.Escudier B, Eisen T, Stadler WM, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;356:125–134. doi: 10.1056/NEJMoa060655. [DOI] [PubMed] [Google Scholar]
- 14.Motzer RJ, Hutson TE, Tomczak P, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007;356:115–124. doi: 10.1056/NEJMoa065044. [DOI] [PubMed] [Google Scholar]
- 15.Motzer RJ, Hutson TE, Tomczak P, et al. Overall survival and updated results for sunitinib compared with interferon alfa in patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27:3584–3590. doi: 10.1200/JCO.2008.20.1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Escudier B, Eisen T, Stadler WM, et al. Sorafenib for treatment of renal cell carcinoma: Final efficacy and safety results of the phase III treatment approaches in renal cancer global evaluation trial. J Clin Oncol. 2009;27:3312–3318. doi: 10.1200/JCO.2008.19.5511. [DOI] [PubMed] [Google Scholar]
- 17.Yang JC, Haworth L, Sherry RM, et al. A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med. 2003;349:427–434. doi: 10.1056/NEJMoa021491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slaton JW, Perrotte P, Inoue K, et al. Interferon-alpha-mediated down-regulation of angiogenesis-related genes and therapy of bladder cancer are dependent on optimization of biological dose and schedule. Clin Cancer Res. 1999;5:2726–2734. [PubMed] [Google Scholar]
- 19.Gabrilovich DI, Chen HL, Girgis KR, et al. Production of vascular endothelial growth factor by human tumors inhibits the functional maturation of dendritic cells. Nat Med. 1996;2:1096–1103. doi: 10.1038/nm1096-1096. [DOI] [PubMed] [Google Scholar]
- 20.Escudier B, Pluzanska A, Koralewski P, et al. Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: A randomised, double-blind phase III trial. Lancet. 2007;370:2103–2111. doi: 10.1016/S0140-6736(07)61904-7. [DOI] [PubMed] [Google Scholar]
- 21.Rini BI, Halabi S, Rosenberg JE, et al. Bevacizumab plus interferon alfa compared with interferon alfa monotherapy in patients with metastatic renal cell carcinoma: CALGB 90206. J Clin Oncol. 2008;26:5422–5428. doi: 10.1200/JCO.2008.16.9847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors: European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 23.Clark TG, Altman DG, De Stavola BL. Quantification of the completeness of follow-up. Lancet. 2002;359:1309–1310. doi: 10.1016/s0140-6736(02)08272-7. [DOI] [PubMed] [Google Scholar]
- 24.Wu Y, Takkenberg JJ, Grunkemeier GL. Measuring follow-up completeness. Ann Thorac Surg. 2008;85:1155–1157. doi: 10.1016/j.athoracsur.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 25.Schneider BP, Wang M, Radovich M, et al. Association of vascular endothelial growth factor and vascular endothelial growth factor receptor-2 genetic polymorphisms with outcome in a trial of paclitaxel compared with paclitaxel plus bevacizumab in advanced breast cancer: ECOG 2100. J Clin Oncol. 2008;26:4672–4678. doi: 10.1200/JCO.2008.16.1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rini BI, Schiller JH, Fruehauf JP, et al. Association of diastolic blood pressure (dBP) ≥ 90 mmHg with overall survival (OS) in patients treated with axitinib (AG- 013736) J Clin Oncol. 2008;26(suppl):163s. abstr 3543. [Google Scholar]
- 27.Motzer RJ, Escudier B, Oudard S, et al. Efficacy of everolimus in advanced renal cell carcinoma: A double-blind, randomised, placebo-controlled phase III trial. Lancet. 2008;372:449–456. doi: 10.1016/S0140-6736(08)61039-9. [DOI] [PubMed] [Google Scholar]
- 28.Rini BI, Michaelson MD, Rosenberg JE, et al. Antitumor activity and biomarker analysis of sunitinib in patients with bevacizumab-refractory metastatic renal cell carcinoma. J Clin Oncol. 2008;26:3743–3748. doi: 10.1200/JCO.2007.15.5416. [DOI] [PubMed] [Google Scholar]