Abstract
Background
Patellofemoral pain syndrome (PFPS) is one of the most common chronic knee injuries; however, little research has been done to determine the risk factors for this injury.
Hypothesis
Altered lower extremity kinematics and kinetics, decreased strength, and altered postural measurements will be risk factors.
Study Design
Prospective cohort.
Methods
1597 participants were enrolled in this investigation and prospectively followed from the date of their enrollment (July 2005, July 2006, or July 2007) through January 2008. Each participant underwent baseline data collection during their pre-freshman summer at the United States Naval Academy. Baseline data collection included three-dimensional motion analysis during a jump-landing task, six lower extremity isometric strength tests, and postural alignment measurements (navicular drop and Q-angle). Participants were prospectively followed from their date of enrollment to January 2008 (maximum of 2.5 years of follow up).
Results
Risk factors for the development of PFPS included decreased knee flexion angle, decreased vertical ground reaction force, and increased hip internal rotation angle during the jump-landing task. Additionally, decreased quadriceps and hamstring strength, increased hip external rotator strength, and increased navicular drop were risk factors for the development of PFPS.
Conclusions
Multiple modifiable risk factors for PFPS pain have been identified in this investigation. In order to decrease the incidence of this chronic injury, the risk factors for PFPS need to be targeted in injury prevention programs.
Clinical Relevance
Prevention programs should focus on increasing strength of the lower extremity musculature along with instructing proper mechanics during dynamic movements in order to decrease the incidence of PFPS.
Key Terms: incidence, anterior knee pain, risk factors
INTRODUCTION
Patellofemoral pain syndrome (PFPS) is one of the most common lower extremity conditions reported in physically active populations, affecting one in four individuals.4,5 Patellofemoral pain encompasses disorders in which pain and point tenderness present in or around the patellofemoral joint. Despite its high prevalence, little is known regarding the risk factors which predispose individuals to developing PFPS.
The development of PFPS can be devastating due to the common recurrence of symptoms and its influence on physical activity levels. In a retrospective case-control analysis of patients diagnosed with PFPS following 4–18 years after initial presentation, 91% of patients still had knee pain (68% of these were females), and in 36% of these patients PFPS restricted their physical activity.25 In addition, PFPS has been demonstrated to have an association with the development of patellofemoral osteoarthritis.28 Utting et al.28 reported that 22% of patients with patellofemoral osteoarthritis reported symptoms of anterior knee pain as an adolescent. Based on these findings, PFPS is considered a public health concern due to its detrimental affect on physical activity and its association with patellofemoral osteoarthritis. The development of prevention programs may be an effective strategy to decrease the occurrence of PFPS and in turn the occurrence of patellofemoral osteoarthritis.
There is a need to understand the risk factors for this disorder so that effective prevention strategies can be developed and implemented. Various risk factors have been proposed for PFPS, including lower extremity structural abnormalities, muscle weakness, and dynamic malalignment8,16,17,26,29; however, few studies have prospectively evaluated all of these risk factors.17,24,29 The few prospective cohort investigations that have been performed indicate decreased quadriceps flexibility, shortened reflex time of the vastus medialis oblique, reduction of vertical jump performance, increased medial patellar mobility, increased medial tibial intercondylar distance, and increased quadriceps strength as factors associated with the incidence of PFPS.17,29 Although these risk factors provide some information for the development of prevention programs for PFPS, several of these factors are non-modifiable. Therefore, there is a need for research which aims to identify modifiable risk factors for PFPS.
The modifiable risk factors that have been theorized to play a role in the development of PFPS include altered kinematics and kinetics during functional tasks and decreased strength of the hip and knee musculature.22 Alterations in kinematics and kinetics may lead to increased loads being placed across the patellofemoral joint22, and may ultimately lead to PFPS.13 It has also been proposed that weakness of the thigh and hip musculature can alter the alignment of the patella within the femoral trochlea, leading to abnormal patellar tracking.10 Prospective investigations have yet to identify if the above listed modifiable risk factors are associated with the development of PFPS.
Two additional risk factors that have been theorized to predispose individuals to PFPS are excessive pronation and increased Q-angle. Excessive pronation through the measure of navicular drop, has yet to be evaluated as a risk factor for the incidence of PFPS and although Q-angle has been investigated, researchers have not reported a clear association with an increased incidence of PFPS.6,9,15,29
The purpose of this investigation was to determine the biomechanical risk factors for PFPS. The specific factors examined were: lower extremity kinematics and kinetics during a jump-landing task, Q-angle, navicular drop, and the strength of the hip and knee musculature (hip abductors, hip extensors, hip external rotators, hip internal rotators, knee flexors, and knee extensors). We hypothesized that there would be an association between the development of PFPS and altered kinematics and kinetics, increased Q-angle, increased navicular drop, and decreased lower extremity strength.
METHODS
Study Design & Participants
A total of 1,597 midshipmen from the United States Naval Academy (USNA) were enrolled in this investigation. Inclusion criteria for enrollment into the cohort population included the following: 1) freshman at USNA at time of enrollment into the investigation, 2) no injury limiting participation in a jump-landing task and/or lower extremity strength tests. We chose this population due to the similar activity requirements placed on all midshipmen. Midshipmen are required to participate in a varsity or intramural sport every semester of their enrollment at the academy. Additionally, they must participate in military training that includes daily physical conditioning activities.
Enrolled study participants were spread among three classes of midshipmen [class of 2009 = 438 participants (females=189, males=249), class of 2010 = 525 participants (females=223, males=302), and class of 2011 = 562 participants (females=194, males=368)]. Each participant underwent a baseline biomechanical assessment during their first summer of enrollment at the USNA. This baseline assessment is part of on-going study of risk factors for ACL injury (the JUMP-ACL study) in which baseline data is collected for participants at all three service academies (USNA, United States Air Force Academy, and United States Military Academy). This paper utilizes data from the first three years of JUMP-ACL (2005–2007) and from one of the three sites (USNA).
Participants in this investigation were followed prospectively for the diagnosis of PFPS. The diagnosis of PFPS was determined based on a manual review of medical records by the first author. Participants in each class were followed prospectively from the date of their enrollment (July 2005, July 2006, or July 2007) in this investigation to January 2008. The criteria that had to be met to be included in the injury group are listed below.
- Must Demonstrate Both During Evaluation:
- Retropatellar knee pain during at least 2 of the following activities: ascending/descending stairs, hopping/jogging, prolonged sitting, kneeling, and squatting.
- Negative findings on examination of knee ligament, menisci, bursa, and synovial plica.
- Must Demonstrate One of the Following During Evaluation:
- Pain on palpation of medial or lateral patellar facets
- Pain on palpation of the anterior portion of the medial or lateral femoral condyles
Although duration of symptoms is commonly accounted for when defining PFPS, we did not account for this because of the lack of consistent documentation of duration of symptoms by military health professionals. However, if the mechanism of injury stated a traumatic blow to the knee/patella and the medical record note matched the above listed inclusion criteria, we did not include the individual in the injured cohort. Based on this, we attempted to only include individuals who developed PFPS over a period of time (chronic) and not due to an acute traumatic injury. Individuals with a history of PFPS in the previous six months were excluded from the cohort due to the potential influence of the injury history on baseline measurements (see Cohort Selection).
Baseline Assessment - Instrumentation
A Flock of Birds® (Ascension Technologies, Inc., Burlington, VT) electromagnetic motion analysis system controlled by Motion Monitor® software (Innovative Sports Training, Inc. Chicago, IL) was used to assess lower extremity kinematics at a sampling rate of 144Hz. A non-conductive force plate (Bertec Corporation, Columbus, OH, Model 4060-NC) collected ground reaction forces to allow for the calculation of lower extremity kinetics through inverse dynamic procedures. Force plate data was collected synchronously with the kinematic data at a sampling rate of 1440 Hz.
The Flock of Birds® was used to measure the position and orientation of three electromagnetic tracking sensors placed on the sacrum, femur, and tibia. A standard range transmitter consisting of three orthogonal coils generated a magnetic field. The three electromagnetic sensors attached to participants collected the changes in the electromagnetic flux in the field generated by the transmitter. Previous research has reported that electromagnetic tracking systems provide accurate1,18 and reliable1 data for three-dimensional movement of body segments and joints.
A hand-held dynamometer (Chatillon MSC-500, AMETEK, Inc, Largo, FL) was used to collect peak and mean isometric strength values for lower extremity musculature. A standard goniometer was used to measure Q-angle. Each participant’s height (Seca 206 Bodymeter, Hanover, MD) and weight (Seca 780, Hanover, MD) were measured using a height gauge and scale, respectively.
Baseline Assessment Testing Procedures
Prior to the start of baseline data collection, all subjects provided informed consent in accordance with National Naval Medical Center Bethesda Institutional Review Board. Additionally, subjects completed a baseline questionnaire which asked questions in regards to age, gender, history of participation in athletic activity, mental health, knee and lower limb injury history, and recent exercise and weight training history.
The jump-landing task consisted of participants jumping from a 30-cm high box set at a distance of 50% of their height, down to a force platform. Once subjects landed on the force platform, they jumped vertically for maximum height. Following task instruction, the subject was given as many practice trials as needed to perform the task successfully. A successful jump was characterized by landing with the entire foot of the dominant lower extremity on the force plate, landing with their entire foot of the non-dominant lower extremity off the force plate, and completing the task in a fluid motion.
Following task instruction and practice, electromagnetic tracking sensors were attached to the dominant lower extremity. The dominant lower extremity was defined as the leg used to kick a ball for maximum distance. Electromagnetic sensors were placed on the subjects' skin over the superior sacrum, lateral aspect of the thigh, and anteromedial aspect of the proximal tibia. Each sensor was placed over an area of the least muscle mass to minimize potential sensor movement and was secured using double sided tape, pre-wrap, and athletic tape. Six bony landmarks were digitized with the endpoint of a stylus on which a fourth receiver was mounted. The six bony landmarks were: medial and lateral epicondyles of the femur, medial and lateral malleoli of the ankle, and left and right anterior superior iliac spine (ASIS) of the pelvis. Medial and lateral malleoli and femoral epicondyles were digitized to determine the ankle joint center and knee joint center, respectively. Left and right ASIS were digitized to determine the hip joint center of rotation using the Bell method.2 Participants performed three successful trials of the jump-landing task.
Lower extremity isometric muscle strength tests were performed in the following order: knee extension (quadriceps), hip external rotation (hip external rotators), hip internal rotation (hip internal rotators), knee flexion (hamstrings), hip extension (gluteus maximus), and hip abduction (gluteus medius). A figure displaying participant and examiner positioning for each strength test is included in the appendix. During each test, participants were instructed to push as hard as they can, holding the contraction for five-seconds. Peak isometric strength values for two separate trials were collected. All strength data were normalized to the mass of the subject and averaged over the two trials. Intra-rater reliability (ICC2,k) calculated from pilot data for the strength tests ranged from 0.73–0.98.
The structural alignment measures assessed included Q-angle and navicular drop. Q-angle was measured with participants in a standing position using a standard goniometer. Q-angle was recorded in degrees for three separate trials. The average of the three trials was used for data analysis. Intra-rater reliability from pilot data showed good reliability for Q-angle measurement (ICC2,k= 0.83). Navicular drop was measured as the difference between the navicular tuberosity height in a non-weight bearing subtalar joint neutral position and a weight bearing position. The average of the three navicular drop measurements was used for data analysis. Intra-rater reliability from pilot data showed good reliability for navicular drop measurement (ICC2,k= 0.79).
Biomechanical Data Reduction
All kinematic data were filtered using a 4th order low pass Butterworth filter at 14.5 Hz. A global reference system was defined using the right hand rule, in which the x-axis was positive in the anterior direction, the y-axis was positive to the left of each participant, and the z-axis was positive in the superior direction. Lower extremity joint rotations were calculated using the Euler rotation method in the following order: Y, X, Z. The y-axis corresponded to the flexion-extension axis, the x-axis corresponded to the abduction-adduction axis, and the z-axis corresponded to the internal-external rotation axis.
The kinematic and kinetic data were reduced using custom Matlab software (Mathworks, Natick, MA). Three-dimensional peak knee and hip joint angles, peak vertical ground reaction force, and internal joint moments for hip abduction, hip external rotation, knee extension, and knee varus were determined during the stance phase. The stance phase was defined as the time period between initial ground contact with the force plate until takeoff for the rebound jump. Initial ground contact was the time point when vertical ground reaction force exceeded 10 N as the subject landed on the force plate from the 30-cm high platform. Takeoff was identified as the time when vertical ground reaction force dropped below 10 N following initial contact. The average of the peak values across the 3-trials was calculated for each of the kinematic and kinetic variables. The peak vertical ground reaction force was normalized to body weight (N) for each participant (% body weight). Peak internal joint moments were normalized to the product of body weight (N) and body height (m) (body weight * body height). Table 1 provides a list of all kinematic, kinetic, strength, and postural variables assessed in this investigation.
Table 1.
Means, standard deviations, F values, and P-values comparing injured and non-injured cohorts.
| Domain | Dependent Variable | Injured (Mean ± SD) |
Non-injured (Mean ± SD) |
F value | P-value |
|---|---|---|---|---|---|
| Kinematic Variables | Hip flexion angle (°) | −67.0±19.8 | −71.8±20.1 | 2.18 | 0.14 |
| Hip adduction angle (°) | 1.9±7.2 | 2.8±6.7 | 0.76 | 0.38 | |
| Hip internal rotation angle (°) | 7.6±8.9 | 7.2±8.4 | 0.09 | 0.76 | |
| Knee flexion angle (°) | 76.5±11.7 | 80.8±14.3 | 3.82 | 0.06 | |
| Knee valgus angle (°) | −13.6±7.8 | −14.1±7.9 | 0.14 | 0.71 | |
| Knee internal rotation angle (°) | 12.2±8.0 | 14.7±8.4 | 3.39 | 0.07 | |
| Kinetic Variables | Vertical ground reaction force (%BW) | 2.6±0.5 | 2.9±0.9 | 4.40 | 0.04 |
| Hip abduction moment (%BW*ht) | −0.13±0.08 | −0.14±0.07 | 0.99 | 0.32 | |
| Hip external rotation moment (%BW*ht) | −0.06±0.03 | −0.08±0.05 | 4.64 | 0.03 | |
| Knee extension moment (%BW*ht) | −0.21±0.05 | −0.23±0.05 | 4.70 | 0.03 | |
| Knee varus moment (%BW*ht) | 0.05±0.03 | 0.05±0.03 | 0.01 | 0.98 | |
| Muscle Strength Variables | Knee flexion strength (%BW) | 0.23±0.06 | 0.25±0.05 | 7.67 | 0.01 |
| Knee extension strength (%BW) | 0.46±0.09 | 0.52±0.12 | 13.22 | 0.01 | |
| Hip extension strength (%BW) | 0.30±0.07 | 0.32±0.09 | 2.09 | 0.15 | |
| Hip internal rotation strength (%BW) | 0.21±0.04 | 0.22±0.04 | 1.31 | 0.25 | |
| Hip external rotation strength (%BW) | 0.21±0.04 | 0.22±0.05 | 0.99 | 0.32 | |
| Hip abduction strength (%BW) | 0.35±0.09 | 0.38±0.09 | 3.83 | 0.05 | |
| Alignment Variables | Q-angle (°) | 10.1±4.2 | 9.8±4.3 | 0.22 | 0.64 |
| Navicular Drop (mm) | 8.1±3.2 | 7.2±2.7 | 4.24 | 0.04 | |
Follow-up Procedures
Physicians at USNA diagnosed cases of PFPS and the diagnosis code is entered into an electronic medical record database, the Armed Forces Health Longitudinal Technology Application (AHLTA). The Defense Medical Surveillance System (DMSS) was used to search for diagnosis codes in AHLTA. DMSS is a comprehensive database of military injuries maintained by the U.S. Army Center for Health Promotion and Preventive Medicine, which captures all illness and injury events in the U.S. Armed Forces resulting in a hospitalization or an ambulatory care facility visit to a military hospital or a military clinician. DMSS was searched to identify individuals within the cohort whose medical record contained one of the following diagnosis codes (ICD-9): 726.69 (Unspecified knee enthesopathy), 726.64 (patellar tendonitis), 717.7 (patella chondromalacia), and 719.46 (unspecified disorder of joint in lower leg). Following the DMSS search, individuals in the cohort identified with one of the above listed ICD-9 codes underwent a medical record review by the first author within AHLTA.
Athletic injuries that are evaluated and treated by the certified athletic trainers at the USNA are not included in the medical records for midshipmen. The certified athletic trainers use SportsWare™ (Computer Sports Medicine, Inc, Stoughton, MA) to record the athletic injuries they evaluate and treat. A keyword search through SportsWare™ was performed to determine the varsity athletes who developed PFPS (keywords: anterior knee pain, patellofemoral pain, and patella maltracking). Injury records highlighted by the keyword search were evaluated by the first author to determine inclusion into the injured group.
Cohort Selection
The total number of participants enrolled in this investigation was 1597 (females=632, males=965). Seventy-two of these participants (females=26, males=46) did not complete one or more of the baseline testing stations and were eliminated from the cohort. None of the eliminated participants were diagnosed with PFPS during the follow-up period. Additionally, 206 (females=93, males=113) participants reported a history of PFPS in the previous six months on the baseline questionnaire and therefore these participants were eliminated from the cohort. We eliminated these participants because at the time of baseline assessment, their performance on the jump-landing task and strength tests could have been influenced by the presence of prior PFPS.
Statistical Analysis
Means and standard deviation were computed for the injured and non-injured groups. Differences between these groups were assessed using ANOVA, with gender included in all models. Separate Poisson regression analyses were performed for each risk factor variable. Additionally, multivariate Poisson regression models were used to model the rate of PFPS as a function of domain specific risk factors. Domain specific models were developed to determine the risk factors associated with PFPS when adjusting for the other risk factor variables within each domain. See Table 1 for the dependent variables within each domain. Based on the findings from the domain specific Poisson regression models, two final multivariate models were developed including the risk factors across multiple domains. The risk factors that were included in the two final multivariate models had a P-value less than 0.20 in the domain specific models. All rate ratios (RR) were scaled so that each RR represents the effect of each variable at the 90th percentile relative to the 10th percentile of the distribution of the variable in the cohort (injured and non-injured groups combined). All statistical analyses were performed using SAS 9.1 (SAS Institute, Inc., Cary, NC). An a priori alpha level for all analyses was set at 0.05.
RESULTS
A total of 40 (females=24, males=16) participants with complete baseline testing and no history of PFPS developed PFPS during the follow-up period and met the inclusion criteria for the injured group. The non-injured group included 1279 (females=489, males=790) participants. The overall risk of PFPS was 3% in this population and the incidence rate was 22 injuries/1000 person-years (95% CI: 15/1000 person-years, 29/1000 person-years). No significant gender × group (AKP vs. non-injured) interactions were found following the ANOVA procedures (P>0.05). Results for injured and non-injured group comparisons are presented in Table 1.
Table 2 includes RR, confidence limit ratios (CLR), and P-values for the separate Poisson regression models for each variable. Table 2 also includes the RR, CLR, P-values for each variable in the domain adjusting for the other variables in the model, and the p-value for the domain specific model. A significantly predictive Poisson regression model was found for each of the following variables: knee flexion torque, knee extension torque, hip internal rotation torque, and navicular drop. There were no significant domain specific models (P>0.05)
Table 2.
Results from univariate and domain-specific Poisson regression models.
| Unadjusted (separate models) | Domain-Specific models (one model per domain) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Domain | Independent Variables | RR1 | 95% CI | CLR | P-value | RR2 | 95% CI | CLR | P-value | Model P-value |
| Kinematic Variables |
Hip flexion angle (°) | 1.47 | 0.64,3.35 | 5.18 | 0.36 | 0.89 | 0.25,3.25 | 13.10 | 0.87 | 0.83 |
| Hip adduction angle (°) | 0.86 | 0.39,1.91 | 4.90 | 0.71 | 0.77 | 0.30,1.97 | 6.51 | 0.59 | ||
| Hip internal rotation angle (°) | 1.30 | 0.60,2.82 | 4.68 | 0.50 | 1.99 | 0.72,5.50 | 7.66 | 0.19 | ||
| Knee flexion angle (°) | 0.52 | 0.22,1.18 | 5.16 | 0.12 | 0.38 | 0.11,1.37 | 12.71 | 0.14 | ||
| Knee valgus angle (°) | 1.04 | 0.46,2.37 | 5.17 | 0.92 | 0.71 | 0.23,2.20 | 9.59 | 0.55 | ||
| Knee internal rotation angle (°) | 0.70 | 0.32,1.52 | 4.72 | 0.37 | 0.63 | 0.28,1.41 | 5.02 | 0.26 | ||
| Kinetic Variables | Vertical ground reaction force (%BW) | 0.42 | 0.17,1.03 | 6.03 | 0.06 | 0.42 | 0.15,1.21 | 8.26 | 0.11 | 0.66 |
| Hip abduction moment (%BW*ht) | 1.19 | 0.51,2.79 | 5.52 | 0.69 | 0.64 | 0.22,1.81 | 8.07 | 0.40 | ||
| Hip external rotation moment (%BW*ht) | 1.75 | 0.69,4.42 | 6.37 | 0.23 | 1.54 | 0.54,4.37 | 8.09 | 0.42 | ||
| Knee extension moment (%BW*ht) | 2.00 | 0.79,5.05 | 6.38 | 0.14 | 1.69 | 0.57,5.01 | 8.80 | 0.34 | ||
| Knee varus moment (%BW*ht) | 1.00 | 0.46,2.19 | 4.75 | 0.99 | 1.53 | 0.64,3.68 | 5.73 | 0.33 | ||
| Muscle Strength Variables |
Knee flexion torque (%BW) | 0.30 | 0.13,0.68 | 5.20 | 0.01 | 0.37 | 0.11,1.21 | 11.21 | 0.10 | 0.16 |
| Knee extension torque (%BW) | 0.19 | 0.07,0.47 | 6.46 | 0.01 | 0.13 | 0.03,0.52 | 16.85 | 0.01 | ||
| Hip extension torque (%BW) | 0.48 | 0.20,1.18 | 5.95 | 0.11 | 1.37 | 0.44,4.27 | 9.72 | 0.59 | ||
| Hip internal rotation torque (%BW) | 0.42 | 0.18,0.97 | 5.37 | 0.04 | 0.94 | 0.28,3.11 | 11.00 | 0.92 | ||
| Hip external rotation torque (%BW) | 0.47 | 0.21,1.09 | 5.23 | 0.08 | 3.34 | 0.88,12.67 | 14.42 | 0.08 | ||
| Hip abduction torque (%BW) | 0.45 | 0.19,1.02 | 5.25 | 0.06 | 0.90 | 0.29,2.84 | 9.86 | 0.86 | ||
| Static Alignment Variables |
Q-angle (°) | 0.99 | 0.47,2.09 | 4.42 | 0.98 | 1.01 | 0.47,2.15 | 4.54 | 0.98 | 0.21 |
| Navicular Drop (mm) | 2.52 | 1.25,5.08 | 4.06 | 0.01 | 2.52 | 1.25,5.08 | 4.06 | 0.01 | ||
RR for all variables other than gender represents the effect of each variable at the 90th percentile of its distribution relative to the 10th percentile.
Adjusted for all other variables in that domain.
Due to the small number of individuals in the injured group (n=40), we could not include all risk factor variables in one model. Therefore, two final models were created with five or less variables in order to assess the risk factors across multiple domains. The two final models were a kinematics/kinetics/posture model and a muscle strength/posture model. The independent variables included in the kinematics/kinetics/posture model were hip internal rotation angle, knee flexion angle, vertical ground reaction force, navicular drop, and gender. The independent variables included in the muscle strength/posture model were knee flexion peak torque, knee extension peak torque, hip external rotation peak torque, navicular drop, and gender. Gender was included in both models due to the inherent differences between males and females for many of the independent variables in the models. Navicular drop was also included in both models because navicular drop was the most predictive variable.
Table 3 provides the RR, CLR, and P-values for the kinematic/kinetic/posture model and the muscle strength/posture model. Each model significantly predicted the development of PFPS (P<0.05). The RR in Table 3 represent the effect of each factor at its 90th percentile relative to the 10th percentile. Examples of how these results can be interpreted are as follows: Based on model 1, the rate of development of PFPS was 3.4 times greater for the individuals with navicular drop at the 90th percentile (10.7mm) relative to those at 10th percentile (4.0mm) when adjusting for all other variables in the model. Additionally, the rate of development of PFPS was 3.1 (RR: 0.32−1) times greater for the individuals with knee flexion angle at the 10th percentile (63.2°) relative to those at the 90th percentile (99.5°) when adjusting for all other variables in the model.
Table 3.
Results from the two final multivariate Poisson regression models.
| Final Models | Independent Variables | 10th percentile |
90th percentile |
RR1 | 95% CI | CLR | P- value |
Model P-value |
|---|---|---|---|---|---|---|---|---|
| Model 1: Kinematic/Kinetic/Posture |
Hip internal rotation angle (°) | −3.15 | 18.19 | 1.38 | 0.59,3.23 | 5.47 | 0.46 | 0.04 |
| Knee flexion angle (°) | 63.21 | 99.48 | 0.32 | 0.12,0.86 | 7.23 | 0.02 | ||
| Vertical ground reaction force (%BW) |
1.92 | 4.02 | 0.28 | 0.10,0.79 | 7.87 | 0.02 | ||
| Navicular drop (mm) | 4.00 | 10.67 | 3.39 | 1.62,7.11 | 4.39 | 0.01 | ||
| Gender2 | n/a | n/a | 1.92 | 1.00,3.68 | 3.68 | 0.05 | ||
| Model 2: Muscle Strength/Posture |
Knee flexion torque (%BW) | 0.19 | 0.32 | 0.34 | 0.11.1.06 | 9.80 | 0.06 | 0.02 |
| Knee extension torque (%BW) | 0.37 | 0.69 | 0.18 | 0.04,0.70 | 15.5 | 0.01 | ||
| Hip external rotation torque (%BW) | 0.16 | 0.28 | 4.02 | 1.03,15.72 | 15.29 | 0.04 | ||
| Navicular drop (mm) | 4.00 | 10.67 | 2.73 | 1.36,5.49 | 4.03 | 0.01 | ||
| Gender2 | n/a | n/a | 1.62 | 0.76,3.45 | 4.56 | 0.21 | ||
Adjusted for all other variables in that model. RR for all variables other than gender represents the effect of each variable at the 90th percentile of its distribution relative to the 10th percentile.
Female compared to male (reference category).
DISCUSSION
The main objective of this investigation was to determine the biomechanical risk factors for PFPS. Based on the descriptive analysis, individuals who developed PFPS were significantly weaker on measures of hip abduction, knee flexion, and knee extension strength. Additionally, people who developed PFPS had significantly lower vertical ground reaction force, knee extension moment, and hip external rotation moment, and displayed significantly more navicular drop at baseline assessment compared to those who did not develop PFPS. Based on the final Poisson regression models, decreased peak knee flexion angle and decreased peak vertical ground reaction force during the jump-landing task were risk factors for the development of PFPS. For the strength variables, decreased knee flexion and extension strength, and increased hip external rotation strength were risk factors for the development of PFPS. Finally, increased navicular drop and female gender were significant risk factors for the development of PFPS. Based on the above findings, we accept our hypothesis that there is an association between the development of PFPS and altered kinematics and kinetics, increased Q-angle, increased navicular drop, and decreased lower extremity strength.
Although there are not many investigations for comparison of our results, previous investigations have theorized many of the biomechanical variables we assessed as risk factors for PFPS.7,22,26 The findings of decreased knee flexion and extension strength, increased navicular drop, decreased knee flexion angle and increased hip internal rotation angle support the theorized biomechanical risk factors. However, increased hip external rotation strength and decreased vertical ground reaction force are not in agreement with the theorized risk factors. The next few paragraphs will provide a brief explanation of the following variables as risk factors for PFPS.
Excessive foot pronation has been theorized to predispose individuals to PFPS due to tibial internal rotation.27 Tiberio27 proposed that for the knee to extend with the tibia in an internally rotated position, the femur must also internally rotate. This internal rotation of the femur is thought to lead to malalignment of the patella within the femoral trochlea and compression of the lateral patellar facet.27 Previous research supports the theory that femoral internal rotation causes an increase in contact pressures on the lateral facets of the patella 13, therefore, excessive pronation has previously been proposed as a risk factor for the development of PFPS.
Muscle imbalances, including decreased strength of the hip and knee musculature, have also been proposed to be risk factors for PFPS. In vivo assessments of the vastus lateralis and vastus medialis oblique have confirmed their role as the primary dynamic stabilizers of the patella12,14; therefore, weakness in these muscles may lead to maltracking of the patella. The exact relationship between decreased hamstring strength and the development of PFPS is not clearly understood, however, decreased hamstring strength may be due to an overall weakness of the thigh musculature in individuals who develop PFPS.
The hip musculature has also been theorized to have an influence on the positioning of the patella within the femoral trochlea.22 The hip abductors and external rotators play a major role in controlling transverse and frontal plane motion of the femur. Weakness of the hip external rotators are proposed to cause an increase in hip internal rotation and knee valgus angles during dynamic tasks, and in turn, increase the lateral compressive forces at the patellofemoral joint.11,13,22 In this investigation, increased hip external rotation strength was a risk factor for PFPS, which does not agree with the theorized risk factors for this injury. We hypothesize that due to the increased hip internal rotation angle displayed during the jump-landing task, individuals who developed PFPS were commonly using their hip external rotators to counteract the increased hip internal rotation angle during dynamic tasks. If this hypothesis is true, these individuals may have developed increased hip external rotation strength over time in an attempt to counteract the increased hip internal rotation.
As mentioned previously, evidence does support increased patellofemoral joint contact pressures in various malaligned positions of the lower extremity. Lee et al.13 reported that greater than 30 degrees of femoral internal rotation causes a significant increase in patellofemoral joint contact pressures. Although none of the participants in this investigation displayed greater than 30 degrees of hip internal rotation, we speculate that over time, the increased hip internal rotation may have lead to the development of PFPS.
Many case-control investigations have reported individuals with PFPS display decreased knee flexion angles during functional tasks.3,19,21 Researchers have speculated that this is a compensatory strategy to decrease the amount of contact pressure of the patella in order to decrease pain.3,19,21 However, the findings in this investigation support decreased knee flexion angles as a risk factor for the development of PFPS, not a compensation to PFPS. We speculate that if individuals who ultimately develop PFPS also have lateral patellar malalignment due to the increased femoral internal rotation, the patellofemoral contact stress may be even more increased at the smaller knee flexion angles due to the decreased contact area at these decreased knee flexion angles.
Research has previously shown that decreased knee flexion angles during dynamic tasks lead to increased vertical ground reaction forces23,30, however, in this investigation we found the opposite. We assessed peak vertical ground reaction force and peak knee flexion angle over the stance phase of the jump-landing task. The peak vertical ground reaction force occurs much earlier than the peak knee flexion angle, therefore, we took steps to try and understand the decreased vertical ground reaction force in those who developed PFPS. We evaluated knee flexion and hip flexion displacement during the stance phase to determine if individuals who developed PFPS had a decreased amount of displacement, which may mean they do not efficiently absorb the vertical ground reaction force; however, there was no difference in the knee flexion and hip flexion displacements between the injured and non-injured groups. Additionally, we assessed the knee flexion and hip flexion angles at initial contact during the jump-landing task. Those who developed PFPS had significantly less knee flexion angle at initial contact compared to those who did not develop PFPS (P<0.05). There was no significant difference in hip flexion angle at initial contact between the two groups. Furthermore, we evaluated anterior/posterior and medial/lateral ground reaction forces to determine if individuals who developed PFPS may have increased ground reaction forces in other directions to compensate for the decreased vertical ground reaction force. We did not find any differences in peak anterior/posterior or medial/lateral ground reaction forces between the two groups. Based on our additional analysis, decreased vertical ground reaction force as a risk factor for PFPS warrants further investigation.
In order to understand how all of the above described risk factors may interact with each other leading to the development of PFPS, we have developed a conceptual model (Figure). When performing a dynamic task, individuals who have decreased quadriceps strength may display decreased knee flexion angles because the tasks demands a large amount of eccentric force from the quadriceps musculature and the quadriceps are weak in these individuals. Although, increased or decreased knee extension moment did not predict the development of PFPS, the descriptive analysis showed that individuals who developed PFPS had significantly less knee extension moment during the jump-landing task. Decreased knee extension moment and decreased quadriceps strength may lead to decreased dynamic control of the patella. Additionally, an increase in hip internal rotation possibly due to the increased navicular drop, may lead to a laterally aligned patella. The combination of increased hip internal rotation angle and decreased knee flexion angle will most likely increase the patellofemoral contact pressures, and over time, repetitive movements in this position may lead to the development of PFPS. As mentioned previously, we speculate that the increased hip external rotation strength is due to individuals constantly having to control the increased hip internal rotation angles during dynamic tasks. However, the finding of increased hip internal rotation angle along with the increased hip external rotation strength leads us to believe this may be a neuromuscular control issue, meaning individuals do not know when to recruit the hip external rotators during dynamic tasks, leading to the increased hip internal rotation angle.
Figure 1.
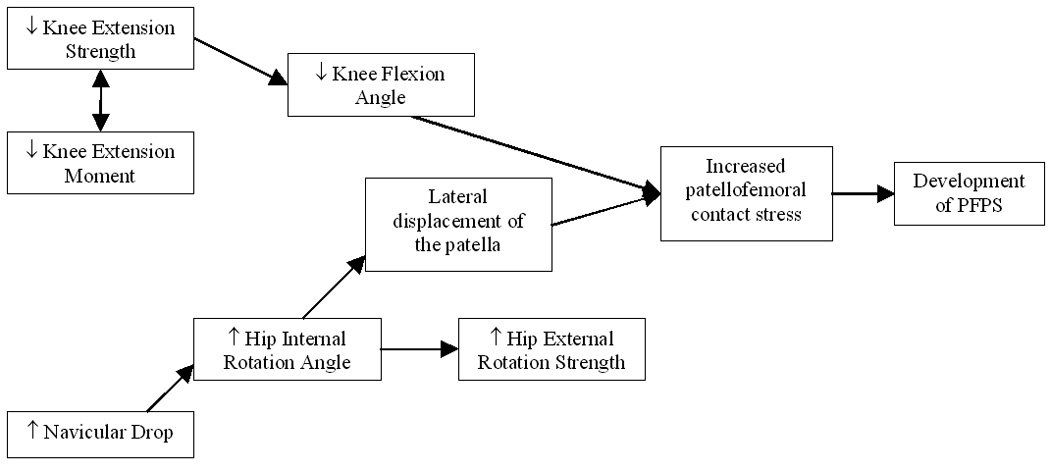
Conceptual model for the development of PFPS.
A limitation of this investigation is that this cohort population is not representative of the general population and results should only be generalized to young active individuals. Another limitation was the small number of individuals who met the criteria to be included in the injured group (n=40) and the decreased amount of follow-up time for the 2007 cohort. Possible explanations for the low incidence of PFPS in this investigation include a lack of information in the medical record to be included in the injured group, medical record charts not available for review, self-treatment for PFPS, and diagnosis by a physician outside of the USNA. It is very uncommon for individuals to see a physician outside of the USNA, therefore, we do not feel that this had a large effect on the number of diagnoses of PFPS. Additionally, only 5% of the individuals with an ICD-9 code in which we were interested did not have enough information in the medical record, therefore, this most likely did not significantly affect the number of individuals diagnosed with PFPS. A more plausible explanation is that 21 individuals who had an ICD-9 code that we were interested in did not have a medical record chart that was available for review during the follow up time for this investigation. This is a limitation of this study, however only 12% of the medical records in which we reviewed that had an ICD9 code for PFPS were actual cases that met our criteria. It is unlikely that this drastically decreased the number of individuals who were included in the injured group. The most reasonable explanation for the decreased incidence of PFPS in this investigation is due to self-treatment. Individuals who developed PFPS may have learned ways to compensate during activities to decrease the pain in their knee. Also, individuals may have been able to withstand the pain so a visit to a physician was not needed. Future investigations may attempt to follow individuals more closely with the use of questionnaires to determine those individuals who may self treat for PFPS.
Another limitation of this investigation includes the large variability in some of the risk factor variables. For example, hip external rotation strength has a CLR of 15.29 in the final model. A measure is thought to be precise if the confidence interval is narrow, decreasing the CLR.20 Very few of the variables in this investigation had a narrow confidence interval; therefore, the results of this investigation should be interpreted with caution. A final limitation was the assessment of only the peak kinematic and kinetics during the jump-landing task. We chose to assess the peak kinematics and kinetics because theory supports that the peak transverse and frontal plane angles are the factors that may be leading to the development of PFPS. Future investigations should determine if kinematics and kinetics during various time periods of a dynamic task are risk factors for the development of PFPS.
CONCLUSIONS
This is the first large scale prospective investigation to assess structural alignment, muscle strength, and dynamic movement patterns as risk factors for PFPS. The findings of this investigation support strengthening of the quadriceps and hamstring musculature along with teaching the proper technique for performing dynamic tasks (decrease hip internal rotation angle, increase knee flexion) as components of effective injury prevention programs, specifically for PFPS. Future research should investigate biomechanical risk factors in the general population and across multiple age groups to determine if these risk factors may differ from the young adult military population.
Supplementary Material
Appendix. Isometric strength tests
Reference List
- 1.An KN, Jacobsen MC, Berglund LJ, Chao EY. Application of a magnetic tracking device to kinesiologic studies. J Biomech. 1988;21:613–620. doi: 10.1016/0021-9290(88)90225-4. [DOI] [PubMed] [Google Scholar]
- 2.Bell AL, Pedersen DR, Brand RA. Prediction of hip joint center location from external landmarks. Hum Movement Sci. 1989;8:3–16. [Google Scholar]
- 3.Crossley K, Cowan S, Bennell K, McConnell J. Knee flexion during stair ambulation is altered in individuals with patellofemoral pain. J Orthop Res. 2004;22:267–274. doi: 10.1016/j.orthres.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 4.DeHaven KE, Lintner DM. Athletic injuries: Comparison by age, sport, and gender. Am J Sports Med. 1986;14:218–224. doi: 10.1177/036354658601400307. [DOI] [PubMed] [Google Scholar]
- 5.Devereaux M, Lachman S. Patellofemoral arthralgia in athletes attending a sports injury clinic. Br J Sports Med. 1984;18:18–21. doi: 10.1136/bjsm.18.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duffey MJ, Martin DF, Cannon DW, Craven T, Messier SP. Etiologic factors associated with anterior knee pain in distance runners. Med Sci Sports Exerc. 2000;32:1825–1832. doi: 10.1097/00005768-200011000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Earl J, Hertel J, Denegar C. Patterns of dynamic malalignment, muscle activation, joint motion, and patellofemoral-pain syndrome. J Sport Rehab. 2005;14:215–233. [Google Scholar]
- 8.El-Metwally A, Salminen JJ, Auvinen A, Kautiainen H, Mikkelson M. Risk factors for traumatic and non-traumatic lower limb pain among preadolescents: a population-based study of Finnish schoolchildren. Musculoskeletal Disorders. 2006;7:1–9. doi: 10.1186/1471-2474-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fairbank JT, Pynset PB, van Poortvliet JA, Phillips H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J Bone Joint Surg. 1984;66B:685–693. doi: 10.1302/0301-620X.66B5.6501361. [DOI] [PubMed] [Google Scholar]
- 10.Fulkerson J. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 11.Ireland M, Willson J, Ballantyne B, Davis I. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:671–676. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- 12.Koh TJ, Grabiner MD, De Swart RJ. In vivo tracking of the human patella. J Biomech. 1992;25:637–643. doi: 10.1016/0021-9290(92)90105-a. [DOI] [PubMed] [Google Scholar]
- 13.Lee T, Anzel S, Bennett K, Pang D, Kim W. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop. 1994:69–74. [PubMed] [Google Scholar]
- 14.Lin F, Wang G, Koh JL, Hendrix RW, Zhang LQ. In vivo and noninvasive three-dimensional patellar tracking induced by individual heads of quadriceps. Med Sci Sports Exerc. 2004;36:93–101. doi: 10.1249/01.MSS.0000106260.45656.CC. [DOI] [PubMed] [Google Scholar]
- 15.Messier SP, Davis SE, Curl WW, Lowery RB, Pack RJ. Etiologic factors associated with patellofemoral pain in runners. Med Sci Sports Exerc. 1991;23:1008–1015. [PubMed] [Google Scholar]
- 16.Mikkelson LO, Nupponen H, Kaprio J, Kautiainen H, Mikkelson M, Kujala UM. Adolescent flexibility, endeurance strength, and physical activity as predictors of adult tension neck, low back pain, and knee injury: a 25 year follow up study. Br J Sports Med. 2006;40:107–113. doi: 10.1136/bjsm.2004.017350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Milgrom C, Kerem E, Finestone A, Eldad A, Shlamkovitch N. Patellofemoral pain caused by overactivity. A prospective study of risk factors in infantry recruits. J Bone Joint Surg. 1991;73A:1041–1043. [PubMed] [Google Scholar]
- 18.Milne AD, Chess DG, Johnson JA, King GJ. Accuracy of an electromagnetic tracking device: a study of the optimal range and metal interference. J Biomech. 1996;29:791–793. doi: 10.1016/0021-9290(96)83335-5. [DOI] [PubMed] [Google Scholar]
- 19.Nadeau S, Gravel D, Hebert L, Arsenault A, Lepage Y. Gait study of patients with patellofemoral pain syndrome. Gait Posture. 1997;5:21–27. [Google Scholar]
- 20.Poole C. Low p-values or narrow confidence intervals: Which are more durable? Epidemiology. 2001;12:291–294. doi: 10.1097/00001648-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Powers C, Heino J, Rao S, Perry J. The influence of patellofemoral pain on lower limb loading during gait. Clin Biomech. 1999;14:722–728. doi: 10.1016/s0268-0033(99)00019-4. [DOI] [PubMed] [Google Scholar]
- 22.Powers C. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33:639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 23.Schmitz RJ, Kulas AS, Perrin DH, Riemann BL, Shultz SJ. Sex differences in lower extremity biomechanics during single leg landings. Clin Biomech. 2007;22:681–688. doi: 10.1016/j.clinbiomech.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Shrier I, Ehrmann-Feldman D, Rossignol M, Abenhaim L. Risk factors for development of lower limb pain in adolescents. J Rheumat. 2001;28:604–609. [PubMed] [Google Scholar]
- 25.Stathopulu E, Baildam E. Anterior knee pain: a long term follow-up. Rheumat. 2003;42:380–382. doi: 10.1093/rheumatology/keg093. [DOI] [PubMed] [Google Scholar]
- 26.Thomee R, Augustsson J, Karlsson J. Patellofemoral pain syndrome: A review of current issues. Sports Med. 1999;28:245–262. doi: 10.2165/00007256-199928040-00003. [DOI] [PubMed] [Google Scholar]
- 27.Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: A theoretical model. J Orthop Sports Phys Ther. 1987;9:160–165. doi: 10.2519/jospt.1987.9.4.160. [DOI] [PubMed] [Google Scholar]
- 28.Utting MR, Davies G, Newman JH. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee. 2005;12:362–365. doi: 10.1016/j.knee.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population: A two-year prospective study. Am J Sports Med. 2000;28:480–489. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- 30.Yu B, Lin C, Garrett WE. Lower extremity mechanics during the landing of a stop-jump task. Clini Biomech. 2006;21:297–305. doi: 10.1016/j.clinbiomech.2005.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix. Isometric strength tests


