Abstract
Background. Breast cancer is the leading cause of cancer among women in Chile and in many Latin American countries. Breast cancer screening is an effective strategy to reduce mortality, but it has a very low compliance among Chilean women.
Objective. To understand barriers and facilitators for breast cancer screening in a group of Chilean women aged 50–70.
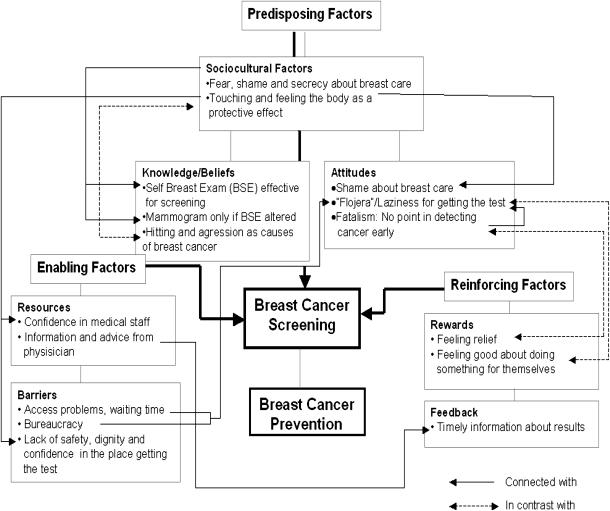
Methods. Following the Predisposing, Enabling and Reinforcing (PRECEDE) framework, seven focus groups (N = 48 women) were conducted with women that have had diverse experiences with breast cancer and screening practices. Information was collected using field notes and audio and video recording. Following the grounded theory model, a sequential process of open, axial and selective coding was used for the information analysis. Atlas ti 5.5 software was used for coding and segmenting the data obtained from the interviews.
Results. The presence of symptoms and/or the finding of lumps through breast self-examination (BSE) were the main predisposing factors for getting a mammogram. Secrecy, embarrassment and fatalism about breast cancer were significant cultural factors that influenced the decision to seek mammogram screening. Confidence in medical staff and dignity in the treatment at the clinic were important enabling factors. The main reinforcing factors for getting the test were a sense of fulfilment by doing something good for themselves and getting timely information about the results.
Conclusions. Primary health care providers should use culturally appropriate strategies to better inform women about the importance of mammography screening and the limitations of BSE for preventing advanced breast cancer.
Keywords: Breast cancer, Chile, qualitative evaluation, screening
Introduction
During the last decade, breast cancer has emerged as one of the most important health problems in many Latin American countries.1,2 Currently, breast cancer is the one with the highest incidence among Chilean women. The cumulative risk up to age 75 is 3.4%.3 Mortality rates from breast cancer in Chile have remained high during the last 10 years.4
Preventive strategies for breast cancer have been inconsistent and of very low impact in most Latin American countries. Compared with the USA, Western Europe or Japan, survival rates from breast cancer in South America are, on average, <20%. Among the main factors associated with this difference is diagnosis in the later stages of the disease among South American women.5,6 In Chile, for example, it has been estimated that only 5% of breast cancer cases were diagnosed in an early stage (in situ stage) in 2003, with 80% being diagnosed and treated with the disease in an advanced stage (stage II, III or IV). This low percentage of early detection among Chilean women is very similar to the percentages reported in other South American countries such as Brazil or Peru.4,6,7
When performed systematically in women who are at least 50 years old, mammography has been shown to be an effective strategy to detect breast cancer in an early stage and to reduce mortality rates.8 However, compliance rates for breast cancer screening in many Latin American countries are very low and range between 10 and 35%.9
Many countries in Latin America have begun to implement new health policies directed at improving breast cancer screening using mammography tests. Until 2005, Chile had a breast cancer screening programme that was based on clinical breast examination. It was associated with the national cervical cancer screening programme. In 2006, Chile started a free population-based mammography screening programme for women aged ≥50. The programme encourages clinical- and community-based strategies to improve mammography screening and includes universal financial coverage for complementary diagnostic tests and required therapy if breast cancer is detected.4
However, there is consistent evidence showing that availability of mammography to the population is not sufficient for improving breast cancer screening practices10–12 Numerous investigations conducted mainly in the USA and Western Europe have used different ecological and behavioural models to explain the disproportionate burden of breast cancer and mammography utilization among various ethnic, migrant and socio-economic groups. Social and cultural factors related to knowledge, beliefs and attitudes as well as factors related to the organization of health services have been identified as barriers and facilitators for improving mammography screening practices.12,13 The importance of incorporating these factors in the design and implementation of breast cancer screening programmes in Latin America has been strongly emphasized by public health authorities.14 However, there is a lack of information about the characteristics of these factors among Latin American women.
In this paper, we analyze the primary sociocultural, predisposing, enabling and reinforcing factors related to breast cancer screening in seven different groups of Chilean women living in Santiago.
Methods
Setting
The study was conducted in El Castillo, an area of low socio-economic status located in the Municipality of La Pintana in the Southeast area of Santiago, Chile. Most of the population living in El Castillo receives free health care services at a university clinic. La Pintana has a high concentration of the poorest population in Santiago.15 The extent of education in La Pintana, as measured by years of schooling, is 30% lower than that in the rest of the country.
Women registered at the university clinic have been able to receive free mammogram screenings since 2006. Baseline information available at the clinic for the year 2007 showed that only 12% of women aged 50–70 years had received a mammogram during the last 2 years.
Focus groups
Participants were selected from the electronic registration system available at the University clinic. The main criteria for selecting participants were age (50–70 years), use of the clinic during the last year (at least one appointment with any professional), adherence with mammographic screening and diagnosis of breast cancer. The sample included two groups of women who had never had a mammogram (non-compliers, G1 and G2), two groups of women who had a mammogram during the last 2 years (compliers, G4 and G5), one mixed group of compliers and non-compliers (G3) and two groups of women who had been diagnosed with breast cancer (G6 and G7). The sampling design provided subgroups of women with diverse experiences related to prevention and breast cancer disease. All participants read and signed an informed consent form prior to participation.
The number of participants per group varied between six and eight women. Each group was conducted by two facilitators, a psychologist and a social worker with experience in primary care and qualitative research. One facilitator conducted the session and was in charge of maintaining the rhythm of the conversation and the inclusion and interaction of participants. The other facilitator kept notes about the main verbalized concepts but also registered silences, attitudes and the quality of the interaction between women. After the focus group, facilitators met and analyzed field notes and compared their perceptions of the session. This information was relevant for the final analysis but also for defining specific issues that needed to be explored in more detail with the next group. Therefore, a sequential strategy was used for conducting the focus groups. Using this strategy, significant information from the previous group was considered for defining specific issues to be addressed or contrasted in more detail in subsequent sessions.
Theoretical model
The Predisposing, Enabling and Reinforcing (PRECEDE) model was used as a general framework to explore the experiences of women participating in the study. The PRECEDE model has been extensively used in health promotion strategies and has been especially recommended for exploring cancer screening practices across cultures.13 The model helps in understanding cultural and contextual factors that facilitate or complicate preventive practices and therefore provides valuable information for planning interventions.
Factors included in the PRECEDE model can be divided into three interrelated dimensions. The first dimension includes ‘predisposing’ factors. This dimension involves sociocultural variables and factors such as knowledge, attitudes and practices. The second dimension consists of ‘enabling’ factors, which include skills, resources and barriers. Finally, the ‘reinforcing’ dimension incorporates factors related to reward and feedback.13
Instruments
A semi-structured questionnaire was used to explore the women's experiences using the PRECEDE model. The questionnaire included eight topics and was based on open-ended questions. Predisposing factors were explored by asking knowledge and belief questions related to either keeping the breasts healthy or ways to detect breast cancer in an early stage. Attitudinal questions included those related to the decision to get a mammogram and factors and situations associated with considering whether to undergo the screening test. Breast care and cancer preventive practices were also addressed in the different groups of participants. Enabling factors were addressed by asking about barriers and facilitators for getting a mammogram. Potential consequences, positive or negative effects and rewards were assessed to identify reinforcing factors.
Analysis
The analysis was based on the grounded theory model. In this model, the research aims to develop a theory closely related to the context of the phenomenon being studied.16
All the information from the focus groups was audio and video recorded and then transcribed in full. The transcription was enriched by field notes recorded by one of the two interviewers who conducted each session.
The process of data analysis was conducted using the software ATLAS/ti 5.5 and followed the standard steps used in grounded theory. The first step consisted of open coding of the data; that is, segmenting the information of the text based on key words and concepts to form categories. Subsequently, axial coding of the information was used to identify central phenomena, strategies, intervening conditions and consequences. Lack of phenomena and strategies were also explored in this stage. Selective coding was the third step of the process. In this step, specific themes and hypotheses were identified. The software allowed us to summarize, using a graphical representation (concept map), the model that emerged after the analyses.
Results
Forty-eight women participated in the seven focus groups conducted. Participants were from of low socio-economic status (average monthly family income of Ch$ 244 000/US$ 478) and had a low level of education (average years of schooling of 7.8 with a range of 6–12 years). Most women were married (68% married, 21% divorced and 10% single), had children (average number of children 2.3) and worked as housewives (80% housewife, 12% domestic work and 8% others). Table 1 presents the general characteristics of the participants according to the groups to which they belonged. Time with the focus groups ranged from 1.2 to 1.8 hours with a total time of 10.8 hours (651 minutes) of content recorded.
TABLE 1.
Characteristics of participants in focus groups related with breast cancer prevention
| Number of participants | Age (years) (mean) | Mammogram screening: never/last 2 years | Breast cancer | |
| Group 1 | 8 | 52 | Never: eight women | No |
| Group 2 | 6 | 56 | Never: eight women | No |
| Group 3 | 8 | 58 | Never: eight women | No |
| Last 2 years: four women | ||||
| Group 4 | 8 | 60 | Last 2 years: eight women | No |
| Group 5 | 8 | 55 | Last 2 years: eight women | No |
| Group 6 | 6 | 62 | Never: four women | Yes |
| Last 2 years: two women | ||||
| Group 7 | 4 | 51 | Never: four women | Yes |
| Total | 48 | 56 | 38 women without breast cancer | |
| 10 women with breast cancer |
Predisposing factors: sociocultural variables, beliefs and attitudes
Table 2 shows the main categories and themes related to predisposing factors that emerged during the interviews. The main categories included in the analysis of predisposing factors were sociocultural variables, beliefs and attitudes. Themes within each category are described and exemplified by a representative quotation. Quotations are identified by the informant's and participant's group numbers.
TABLE 2.
Predisposing factors related to mammogram screening and breast cancer prevention
| Categories | Themes | Data: quotations | Informant (I)/Group (G) |
| Sociocultural factors | Fear, shame and secrecy about breast care | ‘I feel uncomfortable when a man has to do the exam, I always ask for a woman, I don’t like to be exposed (arms covering her chest). It is really the first time I feel I can openly talk about this. Breast care is so private and I feel so scared of having breast cancer.’ | I.5/G.1 |
| Knowledge and beliefs | BSE as the main strategy for breast cancer detection | ‘Everyday when I take a shower I touch myself [touches her breasts with her two hands] and I know that if I find something I have to go to the doctor for a test. Everybody knows that that is the best way to take care of your breasts. If you get in contact with your body, you know better when something is wrong. If there is something wrong you need a mammogram’ | I.2,G.5 |
| Mammogram useful only if there are breast symptoms or the feeling of something unusual in the breast | ‘I felt something weird, like a pimple, then I decided to get the mammogram and it was there, I never thought that it was cancer, I felt it so small. I found out that it might have been there for five years, a long time, and I didn’t feel anything.’ | I.1/G.7 | |
| Mammogram useful even when there are no symptoms | ‘I don’t think I need the test, I’ve never found anything wrong, thank God.’ | I.6/G.2 | |
| Bumps and hits as risk factors for breast cancer | ‘I still think that it happened when playing with my partner, the doctor says it was not the cause but I think it was, it happened when receiving a hit from my partner. I should have got a mammogram after the bump to find out.’ | I.2/G.6 | |
| Attitudes | Laziness (Flojera) for getting a mammogram | ‘I received the medical order for the test a couple of years ago and I left the paper there, I don’t know, it is all due to “flojera” (laziness), more than fear it is “flojera”’. | I.5/G.6 |
| Fatalism: no point in detecting cancer early | ‘That is why one doesn’t go and get it, I will not go to find that I have something wrong, better to live like this’. | I.3/G2 |
The main theme related to sociocultural variables that emerged in the analysis was related to the concepts of ‘fear, shame and secrecy’. In the majority of groups, most participants revealed that breast care was an intimate subject; they did not like to expose themselves to anyone for the purpose of having a mammogram. About half of the participants mentioned that breast care had to be kept private and was not something to share in a conversation with close friends, relatives or an unknown health care professional.
Three themes related to knowledge and beliefs emerged consistently in the majority of the groups interviewed. The first theme was the value of breast self-examination (BSE) as an essential strategy of breast care. The exam was perceived by the majority of participants as one of the very few intimate moments that women could keep for themselves in a very demanding and adverse reality. The second theme was the lack of relevance of mammography as a screening procedure and the confusing information associated with it. Mammography was mentioned by less than a third of the participants as an effective form of breast care and cancer prevention. Predisposition for the test was a strong function of BSE perceptions. In the two groups of women who had experienced breast cancer, mammography was mentioned as a preventive test by only one participant. Getting bumped or hit in the breasts was consistently perceived as a risk factor for breast cancer and therefore, an incentive for getting a mammogram. This was the third theme that appeared in this dimension.
Two themes appeared consistently when attitudes related to breast cancer screenings were explored. The concepts of laziness (flojera) and ‘self-neglect’ represented the first theme. These concepts were related to several factors such as limited time for taking care of themselves, a lack of energy for doing things that are not considered essential or the idea of becoming accustomed to not taking care of themselves, even if they had the time. Fatalism and determinism were the second theme that emerged in this dimension of the analysis. The concept of fatalism was expressed by most members of the groups who did not comply with mammogram screening but also in about half of the participants in groups 4 and 5 (‘compliers’). Women in groups 6 and 7 (those who had experienced breast cancer) referred to the disease as a ‘programmed’ death.
Enabling and reinforcing factors: resources, barriers, rewards and timely feedback
Table 3 presents the main themes associated with enabling and reinforcing factors for cancer screening practices. Physician support through medical advice was identified by most women as an essential resource for getting a mammogram screening. The advice of other health professionals (nurse and midwife), relatives or close friends was mentioned as a reference by only about a third of the participants. About a third of the women described access problems, long waiting times, bureaucracy and transportation as significant barriers that prevent them from getting mammograms. Confidence in health care institutions, safety and dignity were mentioned by about half of the participants as essential enabling factors for getting a mammogram.
TABLE 3.
Enabling and reinforcing factors related to mammogram screening and breast cancer prevention
| Categories | Themes | Data: quotations | Informant (I)/Group (G) |
| Enabling factors | |||
| Resources | Medical advice as a key factor to get a screening mammogram | ‘Finally, you follow the advice of your physician, the doctor has the final word, he writes the order. When I got cancer, I recommended everybody to have the mammogram, to just go and get the test, but only some of them heard me and all of them went to the doctor first. You don’t hear family or friends so much in this.’ | I.4/G.6 |
| Other professionals (nurses, midwife) or relatives and friends advice as important motivators for getting a mammogram | |||
| Safety, dignity and confidence in health care institutions | ‘The most important thing is that they give me confidence and treat me not like an object. I feel this confidence at this clinic, here I feel safe but not at the hospital where I have to get the mammogram. I am not motivated to get the test there because I don’t trust them.’ | I.5/G.3 | |
| Barriers | Long waiting times, bureaucracy and transportation as significant barriers for getting a mammogram | ‘I was working and asked for permission to get a mammogram. I went to the hospital, my appointment was at 8:30, I was there at 8:00 and they arrived at 12:00, they did not call me and I kept waiting, finally I got sick of it and left. You ask for a short permission in your job and in the end have to stay all day.’ | I.7/G.4 |
| Reinforcing factors | |||
| Feedback | Importance of getting timely feedback | ‘I have had the experience of getting tests and then not receiving the results for a long time. I think the same might happen with mammography, If I knew I would get the results soon I would consider getting one.’ | I.7/G.1 |
| Rewards | Feeling relief and good about herself when getting the test | ‘For me it is scary because I am always anxious about the result, but I like to feel the relief when I get the test and to feel that I have done something for myself’ | I.3/G.7 |
Feeling relief and the sense of having taken care of themselves after getting a mammogram were identified as rewarding factors by about half of the women interviewed.
The importance of receiving timely feedback when having a mammogram was also stressed by the majority of women.
Figure 1 presents a concept map that shows an explanatory model for connecting the main themes that emerged during the interviews.
FIGURE 1.
Factors associated with breast cancer screening according to the PRECEDE model.
Discussion
This study shows how the interaction among predisposing, enabling and reinforcing factors affects the decision of women to get breast cancer screening tests. The information obtained in this Chilean study improves our understanding of the specific factors behind the evidence that shows that the availability of free mammograms is not enough to increase screening rates in the population.11,12,17–19 The information provided in this study could lead to the design of appropriate primary care interventions directed at increasing mammography screening and improving the low rate of early breast cancer detection found in most Latin American countries.9
One of the main themes that emerged in all the groups in this study was the importance of BSE as an important way to detect breast cancer early. Mammography was relegated to second place. It was seen as a test to be used only when BSE produced an abnormal finding or if the woman felt that there was something wrong. There is consistent evidence that shows that BSE has important limitations as a screening strategy for breast cancer. It has not been demonstrated to reduce mortality rates from breast cancer when used as the only screening strategy. The exam has an unacceptably high false-positive rate leading to unnecessary tests and biopsies.20,21 Current expert recommendations discourage using BSE as the only screening strategy especially for women >40 years.8,22 Clearly, primary health care providers have a responsibility to improve the delivery of messages in a culturally appropriate way and to inform women about the importance of mammography and the risks of relying only on BSE.23,24
The belief about the importance of BSE should be interpreted in a culturally and socially appropriate context.13 In the present study population, BSE was seen as a concrete, intimate and personal way of self-care. This is consistent with the secrecy and intimacy associated with breast care and with the perception that physical aggression is related to breast cancer. On the other hand, being exposed to a strange and impersonal procedure such as a mammography was associated with fear and shame. Secrecy, fear and the importance of ‘feeling something wrong’ have been found to be critical predisposing factors for getting a mammogram in studies that involved Latino women.19,24 These factors have also been found to be important barriers for mammogram screening practices in European women living in underserved communities.25,26 Fear of pain, fear of a serious diagnosis, embarrassment and stress while anticipating the results were among the main factors described by Trigoni M et al.25 in a group of Greek women. Moreover, some studies have found that Latinas tend to believe that having a screening exam is not worth the risk of a breast cancer diagnosis.27,28 This perception has also been identified among Spanish women when asked about cancer prevention26 and was found to be an important predisposing factor in our study.
Distrust of health care providers has been found to be a relevant risk factor for breast and cervical cancer screening among Latinas.19,29 In our study, confidence in the primary care provider emerged as an important theme related to breast cancer screening. It was a relevant enabling factor associated with safety and the feeling of being treated with dignity. Feeling good about doing something for oneself was a third theme that emerged as a reinforcing factor for getting a mammogram. This factor has also been observed in other studies conducted in underserved populations30,31 but has not been consistently described in qualitative studies related to cancer screening in Latin women. This may represent a cultural shift among Chilean women, especially those who belong to more vulnerable groups. They may begin to value more clearly self-determination and the importance of self-care. Latin America, and especially Chile, has a long history of gender discrimination, but these attitudes have been changing during the last decade.32 This trend may represent a good opportunity to build on strategies that reinforce female self-determination and self-care.
Clearly, other players such as the mass media and health policy makers play a key role in informing women and empowering them to demand access to quality breast cancer screening. This study shows that most participants were misinformed about breast cancer prevention and distrust health care services, especially those provided at the hospital level. A recent review of effective community-based approaches shows that small media interventions and health policies directed at increasing access can improve breast cancer screening in the general population.33
Important methodological issues must be considered in the present study. First, it is relevant to ask whether the results obtained are ‘valid’. Validity in qualitative studies has been a highly discussed and controversial concept. Whittemore et al.34 highlighted the importance of achieving an adequate equilibrium between methodological rigour and creativity in qualitative research. They described two key components of defining validity: criteria and techniques. The theoretical model (PRECEDE) used in this study for the design, recollection and analysis of the information provided a general framework that contributed to the thoroughness and congruence of the information obtained. The sequential strategy for conducting the focus groups and the diverse groups of participants included (i.e. women with different experiences and perspectives of the health problem) contributed to the credibility and authenticity of the information obtained. These are all important validity criteria. The methods used for collecting the information based on field notes, audio and video recording and the coding process used for analyzing the information were helpful techniques that helped to enhance the validity of the study. We believe that the use of a concept map added to the creativity of presenting the results and proposed an interesting explanatory model for connecting the main themes that emerged during the interviews.
Another important issue in this study deals with the generalizability of the findings. In qualitative research, inferences and generalizations cannot be made in the same way as in quantitative investigations. In qualitative research, these concepts are understood in terms of the transferability of the results, i.e. the extent to which the information obtained in the study context would be relevant to other settings. This is an important topic because the present study aims to contribute to the understanding of barriers and facilitators for improving breast cancer screening in communities that are beginning to implement population-based strategies for increasing mammography use. To analyze the extent to which the findings of this study could be transferred to other local realities, it is important to consider that participants of this investigation were women of low socio-economic status with diverse experiences related to breast cancer prevention and were selected from a primary care setting.
In summary, this study shows that there is a combination of predisposing, enabling and reinforcing factors that facilitate and/or prevent women from getting mammography screening. Distrust of the health care providers and unpleasant environmental conditions may not justify the risk of getting a test if no symptoms or abnormalities are observed through BSE. The perceived ‘risk’ of finding something like cancer in a mammogram surpasses the perceived benefit of the test. In contrast, getting a mammogram may reinforce the value of doing something for oneself. Confidence in the health care provider, dignity and timely feedback appeared to be important facilitators of mammogram screening. Health care providers should use culturally appropriate strategies to better inform women about the importance of mammogram screening and the limitations of BSE for preventing advanced breast cancer. The predisposing, enabling and reinforcing factors found in this research should be considered when designing and implementing breast cancer screening strategies in settings with similar characteristics as the one in which this study was conducted.
Declarations
Funding: US National Institute of Health–Fogarty International Center (R03TW007900-01).
Ethical approval: Institutional Review Boards at the Fred Hutchinson Cancer Research Center in Seattle and School of Medicine at Pontificia Universidad Católica de Chile in Santiago.
Conflict of interest: None
References
- 1.Lozano-Ascencio R, Gómez-Dantés H, Lewis S, Torres-Sánchez L, López-Carrillo L. Breast cancer trends in Latin America and the Caribbean. Salud Pública Méx. 2009;51(suppl 1):S147–S56. doi: 10.1590/s0036-36342009000800004. [DOI] [PubMed] [Google Scholar]
- 2.Garcia M, Jemal A, Ward EM, et al. Global Cancer Facts and Figures 2007. Atlanta GA: American Cancer Society; 2007. [Google Scholar]
- 3.Ministerio de Salud Chile (MINSAL), Servicio de Salud Valdivia, International Agency of Cancer Registry (IARC) Registro poblacional del cancer provincia de valdivia 1998–2002. http://epi.minsal.cl/epi/html/frames/frame2.htm (accessed on 30 March 2009) [Google Scholar]
- 4.Ministerio de Salud Chile (MINSAL) Guía clínica cancer de mama en personas de 15 años y más. 1st edn. Santiago: MINSAL; 2005. http://www.minsal.cl/ici/guiasclinicas/CancermamaR_Mayo10.pdf (accessed on 30 March 2009) [Google Scholar]
- 5.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 6.Schwartsmann G. Breast cancer in South America: challenges to improve early detection and medical management of a public health problem. J Clin Oncol. 2001;19(18 suppl):S118–24. [PubMed] [Google Scholar]
- 7.Menke CH, Pohlmann PR, Backes A, et al. Tumor size as a surrogate end point for the detection of early breast cancer: a 30-year (1972-2002), single-center experience in southern Brazil. Breast J. 2007;13:448–56. doi: 10.1111/j.1524-4741.2007.00464.x. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Preventive Services Task Force. Screening for breast cancer: recommendations and rationale. Ann Intern Med. 2002;137(5 part 1):344–6. doi: 10.7326/0003-4819-137-5_part_1-200209030-00011. [DOI] [PubMed] [Google Scholar]
- 9.Reyes-Ortiz A, Freeman JL, Martha P, et al. Mammography use among older women of seven Latin American and Caribbean cities. Prev Med. 2006;42:375–80. doi: 10.1016/j.ypmed.2006.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Consedine NS, Magai C, Horton D, et al. Health belief model factors in mammography screening: testing for interactions among subpopulations of Caribbean women. Ethn Dis. 2005;15:444–52. [PubMed] [Google Scholar]
- 11.Achat H, Close G, Taylor R. Who has regular mammograms? Effects of knowledge, beliefs, socioeconomic status, and health-related factors. Prev Med. 2005;41:312–20. doi: 10.1016/j.ypmed.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 12.Halabi S, Skinner CS, Samsa GP, et al. Factors associated with repeat mammography screening. J Fam Pract. 2000;49:1104–12. [PubMed] [Google Scholar]
- 13.Pasick RJ, Burke NJ. A critical review of theory in breast cancer screening promotion across cultures. Annu Rev Public Health. 2008;29:351–68. doi: 10.1146/annurev.publhealth.29.020907.143420. [DOI] [PubMed] [Google Scholar]
- 14.Robles SC, Galanis E. Breast cancer in Latin America and the Caribbean. Rev Panam Salud Publica. 2002;11:178–85. doi: 10.1590/s1020-49892002000300007. [DOI] [PubMed] [Google Scholar]
- 15.Ministerio de Planificación Chile (MIDEPLAN) Encuesta de Caracterización Socioeconómica (Casen) 2006. http://www.mideplan.cl/final/categoria.php?secid=25&catid=124 (accessed on 30 March 2009) [Google Scholar]
- 16.Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Traditions. London: Sage Publications; 1998. [Google Scholar]
- 17.Wells KJ, Roetzheim RG. Health disparities in receipt of screening mammography in Latinas: a critical review of recent literature. Cancer Control. 2007;14:369–79. doi: 10.1177/107327480701400407. [DOI] [PubMed] [Google Scholar]
- 18.Puschel K, Thompson B, Coronado GD, Lopez LC, Kimball AM. Factors related to cancer screening in Hispanics: a comparison of the perceptions of Hispanic community members, health care providers, and representatives of organizations that serve Hispanics. Health Educ Behav. 2001;28:573–90. doi: 10.1177/109019810102800505. [DOI] [PubMed] [Google Scholar]
- 19.Buki LP, Borrayo E, Feigal BM, et al. Are all Latinas the same? Perceived breast cancer screening barriers and facilitative conditions. Psychol Women Q. 2004;28:400–11. [Google Scholar]
- 20.Kösters JP, Gøtzsche PC. Regular self-examination or clinical examination for early detection of breast cancer. Cochrane Database of Systematic Reviews. 2003;(2) doi: 10.1002/14651858.CD003373. CD003373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas DB, Gao DL, Ray RM, et al. Randomized trial of breast self-examination in Shanghai: final results. J Natl Cancer Inst. 2002;94:1445–57. doi: 10.1093/jnci/94.19.1445. [DOI] [PubMed] [Google Scholar]
- 22.Rosolowich V Breast Disease Committee of the Society of Obstetricians and Gynaecologists of Canada. Breast self-examination. J Obstet Gynaecol Can. 2006;28:728–30. doi: 10.1016/s1701-2163(16)32223-x. [DOI] [PubMed] [Google Scholar]
- 23.Del Giudice ME, Tannenbaum D, Goodwin PJ. Breast self-examination: resistance to change. Can Fam Physician. 2005;51:698–9. [PMC free article] [PubMed] [Google Scholar]
- 24.Schettino MR, Hernández-Valero MA, Moguel R, et al. Assessing breast cancer knowledge, beliefs, and misconceptions among Latinas in Houston, Texas. J Cancer Educ. 2006;21(1 suppl):S42–6. doi: 10.1207/s15430154jce2101s_9. [DOI] [PubMed] [Google Scholar]
- 25.Trigoni M, Griffiths F, Tsiftsis D, et al. Mammography screening: views from women and primary care physicians in Crete. BMC Womens Health. 2008;8:20–31. doi: 10.1186/1472-6874-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barroso P, Ruiz I, Puertas de Rojas F, Parrón T, Corpas E. Factors related to non participation in a breast cancer early detection program. Gac Sanit. 2009;23:44–8. doi: 10.1016/j.gaceta.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 27.Borrayo EA, Jenkins SR. Feeling healthy: so why should Mexican-descent women screen for breast cancer? Qual Health Res. 2001;11:812–23. doi: 10.1177/104973201129119550. [DOI] [PubMed] [Google Scholar]
- 28.Borrayo EA, Buki LP, Feigal BM. Breast cancer detection among older Latinas: is it worth the risk? Qual Health Res. 2005;15:1244–63. doi: 10.1177/1049732305281337. [DOI] [PubMed] [Google Scholar]
- 29.Agurto I, Bishop A, Sánchez G, et al. Perceived barriers and benefits to cervical cancer screening in Latin America. Prev Med. 2004;39:91–8. doi: 10.1016/j.ypmed.2004.03.040. [DOI] [PubMed] [Google Scholar]
- 30.Montaño DE, Thompson B, Taylor VM, Mahloch J. Understanding mammography intention and utilization among women in an inner city public hospital clinic. Prev Med. 1997;26:817–24. doi: 10.1006/pmed.1997.0215. [DOI] [PubMed] [Google Scholar]
- 31.Ahmed NU, Fort JG, Elzey JD, Bailey S. Empowering factors in repeat mammography: insights from the stories of underserved women. J Ambul Care Manage. 2004;27:348–55. doi: 10.1097/00004479-200410000-00007. [DOI] [PubMed] [Google Scholar]
- 32.International Service for Human Rights. Committee on the Elimination of Discrimination Against Women 36th Session 7–25 August 2006 Chile 4th Periodic Report. http://www.ishr.ch/hrm/tmb/treaty/cedaw/reports/cedaw_36/chile_cedaw_36.pdf (accessed on 6 January 2009) [Google Scholar]
- 33.Task Force on Community Preventive Services. Recommendations for client- and provider-directed interventions to increase breast, cervical, and colorectal cancer screening. Am J Prev Med. 2008;35(1 suppl):S21–5. doi: 10.1016/j.amepre.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 34.Whittemore R, Chase SK, Mandle CL. Validity in qualitative research. Qual Health Res. 2001;11:522–37. doi: 10.1177/104973201129119299. [DOI] [PubMed] [Google Scholar]