ABSTRACT
OBJECTIVE
To assess whether regular care from a family physician is associated with regular participation in screening mammography.
DESIGN
Secondary analysis of the 2006 Canadian Community Health Survey data.
SETTING
Canada.
PARTICIPANTS
Cross-sectional sample of 15 195 Canadian women aged 50 to 69 years.
MAIN OUTCOME MEASURES
The outcome of interest was screening mammography within the past 2 years; the key explanatory factor was active interaction with a family physician. Control factors included sociodemographic characteristics, other cancer screening behaviour, and other cancer risk habits.
RESULTS
Active interaction with a regular family doctor doubled the odds that a woman had received a recent screening mammogram. Other cancer screening and preventive measures were also strongly associated with that outcome. A woman who had had a recent Papanicolaou test was more than 3 times as likely to have had a recent mammogram; nonsmokers were much more likely to have had a recent mammogram than smokers.
CONCLUSION
Adults who receive regular care from family physicians are more likely to participate in screening mammography within the recommended time frames.
RÉSUMÉ
OBJECTIF
Déterminer si le fait d’être suivi régulièrement par un médecin de famille s’accompagne d’une participation régulière au dépistage par la mammographie.
TYPE D’ÉTUDE
Analyse secondaire des données de l’Enquête sur la santé des collectivités canadiennes de 2006.
CONTEXTE
Le Canada.
PARTICIPANTES
Un échantillon transversal de 15 195 Canadiennes de 50 à 69 ans.
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
L’issue considérée était une mammographie de dépistage au cours des 2 dernières années; le facteur explicatif était une interaction active avec un médecin de famille. Les facteurs contrôlés incluaient les caractéristiques démographiques, les habitudes de dépistage pour d’autres cancers et les autres habitudes causant un risque de cancer.
RÉSULTATS
Les femmes qui communiquaient régulièrement avec un médecin de famille avaient 2 fois plus de chances d’avoir eu une mammographie récemment. Cet examen était aussi fortement associé à la probabilité d’avoir fait l’objet de dépistages ou de mesures préventives pour d’autres types de cancers. Les femmes qui avaient subi un test de Papanicolaou récemment avaient 3 fois plus de chances d’avoir subi une mammographie récente. Les non-fumeuses étaient 2 fois plus susceptibles que les fumeuses d’avoir eu une mammographie récemment.
CONCLUSION
Les femmes adultes qui sont suivies régulièrement par un médecin de famille sont plus susceptibles de participer au dépistage par mammographie en respectant les intervalles de temps recommandés.
Despite recent improvements in mortality, breast cancer continues to be a big health concern for Canadian women—1 in 9 will be diagnosed with breast cancer in her lifetime and 1 in 27 will die from this disease.1 However, Canadian mortality rates from breast cancer have steadily declined since 1986; improvements to both screening and treatment are credited with contributing to this decline. A prominent US network estimated that screening has been responsible for 8% to 23% of a similar US decline in mortality from 1990 to 2000.2 Organized screening programs began in Canada in 1988 in British Columbia. Since then, all provinces and territories (with the exception of Nunavut) have introduced programs, and national targets for screening participation have been established.3 However, although evidence shows that screening mammography prolongs lives, not all eligible women take advantage of these programs.
Why do some women get screened regularly while others do not? Having a regular family doctor has been strongly associated with screening participation.4 Using the 1996–1997 National Population Health Survey, Maxwell et al determined that having regular physicians doubled the odds that women would receive regular mammograms.5 A study of rural women in the United States, using data from 1998, also found that physician recommendation was the strongest predictor of both starting and continuing screening mammography.6 Other studies considered the association between health promotion behaviour (such as breast self-examination, physical activity, and not smoking) and screening behaviour.5,7–9 These factors, although important, might not be as important as having a family doctor.
Studies demonstrating the importance of family doctors to screening participation are now more than a decade old. Since their publication, the number of family doctors trained annually in Canada has declined, with many medical students turning to other specialties.10,11 Further, many family doctors have reduced their hours of work (17.2%) or plan to do so (24.6%).12 Patients indicate they have trouble accessing their family doctors and many report that they are currently without family doctors.13 Given these trends, as well as emphasis by the First Ministers’ Accord on Health Care Renewal14 on improving participation in screening mammography programs, we wanted to reevaluate using more recent data whether having family doctors continues to be strongly associated with women’s participation in regular screening mammography.
METHODS
Data source
This is a cross-sectional study using secondary analysis of survey data from the 2006 cycle of the Canadian Community Health Survey (CCHS), a biannual survey of the Canadian population. The CCHS collects information on health status, health care use, and other determinants of health for Canadians older than 12 years of age.* Respondents are asked questions about their general health and health care behaviour, including whether they have family doctors and how often they have seen their family doctors in the past 12 months. Questions about cancer screening practices, specifically mammograms and Papanicolaou tests, are included, along with reasons for and timing of most recent tests. Other factors of interest for this study include those associated with the risk of cancer, such as body weight, smoking behaviour and history, and alcohol use. Standard sociodemographic information, such as income, education, age, residence, and immigration status, are also available from the survey. We used the public release data file made available through the University of British Columbia,15 the use of which is governed by the University of British Columbia’s Behaviour Research Ethics Board policy number 89 for publicly available data.16
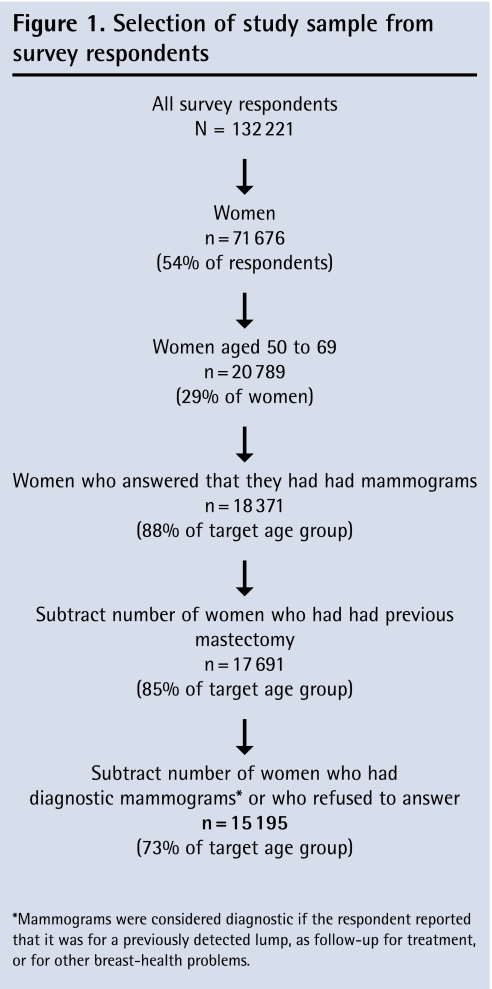
Study population
This study focused on Canadian women aged 50 to 69 years, the age range consistent with the national target established by the First Ministers’ Accord on Health Care Renewal.14 Excluded from the study were men, women who did not answer the questions about whether they had received mammograms, women who reported having had mastectomies, and women considered to have received diagnostic mammograms. The mammogram was considered diagnostic if the respondent reported that it was for a previously detected lump, as follow-up for treatment, or for other breast health problems.
Variables
The main outcome measure was participation in screening mammography within the past 2 years, which was derived from survey questions regarding the timing of and reason for the latest mammogram. Respondents were grouped into 2 categories: “recent mammogram” or “no recent mammogram” (if more than 2 years had elapsed since the last mammogram or if the respondent had never had a mammogram).
The key explanatory variable of interest—active interaction with a family doctor—was derived from survey questions about whether the respondent had a family doctor and the reported number of visits to that doctor in the past 12 months. We organized this variable into 3 response categories: respondents who reported visiting regular family doctors 1 or more times in the past year were coded as “regular family doctor”; respondents who reported having regular doctors but with no visits in the past year were coded as “family doctor, not regular user”; and those reporting not having regular doctors were coded as “no family doctor.”
Several other groups of control variables were developed to adjust for differences in factors that might influence either a woman’s likelihood of having a family doctor or her likelihood of seeking screening mammography:
Sociodemographic characteristics, such as age, marital status, income, education, province of residence, and immigrant status.
Cancer screening behaviour, such as breast self-examination (derived from the optional part of the survey for only a subset of the study sample) and Pap testing in the past 3 years.
Other factors associated with cancer risk, including body mass index (BMI), smoking, and alcohol use.
Analysis
Analysis was conducted using SAS version 9.1. Frequency distributions were calculated; where responses to study questions were missing, the response was coded as “not stated.” As the CCHS was designed to oversample key groups, probability weights were used to produce unbiased estimates and variances.
Women in the “recent mammogram” group were compared with those who reported “no recent mammogram” to examine key differences in weighted proportions of the explanatory and control variables; χ2 statistics were used to calculate significance.
Logistic regression modeling was conducted to examine the relationship between explanatory variables and the key outcome variable of interest. Statistical significance was tested for individual variables using confidence intervals and P values. The independent associations among control variables, the key explanatory variable of interest, and the outcome variable were reported as unadjusted odds ratios with 95% confidence intervals.
Two stepwise multiple logistic regression models were developed. The first (model 1) included significant control variables only, while the second (model 2) included those variables plus the key explanatory variable of interest. To develop the first model, variables having statistically significant associations with the mammography screening behaviour at the bivariate level were entered sequentially. After each addition, variables that were not significant were removed. The final model included the key explanatory variable—interaction with a family doctor—as well as all of the variables that remained in the first model.
Using a Web-based sample size power calculator,17 we estimated that this study was powered to detect a difference in effect of 1%, with type I error < .05 and type II error < .20.
RESULTS
Based on exclusions, the final study population used for analysis was a cross-sectional sample of 15 195 Canadian women. Figure 1 delineates how the total study population was derived. A total of 2590 women did not provide answers to all the questions used for analysis. The level of incomplete responses was highest for sociodemographic variables—15.8% of respondents did not answer questions about income and 2.2% did not provide information on education. Overall, respondents who did not answer 1 or more of the questions tended to be younger, had lower incomes, had less education, were slightly more likely to be immigrants, and were less likely to have partners. They were much less likely to have had Pap tests in the past 3 years. Finally, with respect to the key independent variable, they were much less likely to report having family doctors. Further data are available upon request.
Figure 1.
Selection of study sample from survey respondents
Table 1 shows the characteristics of women who had had screening mammograms in the past 2 years compared with those who had not. Based on χ2 tests, the weighted proportion of women who had recent screening mammograms was different across each factor tested. Large differences in the proportions of women screened were observed among those who reported recent Pap tests. There were also differences for women according to how they reported interaction with family doctors: those who had no family doctor had the lowest proportion of screening mammography (68.5%); those who had family doctors but who had not recently visited them had a higher proportion of screening mammography (74.1%); and women who had seen their family doctors in the past 12 months reported the highest proportion of screening mammography (85.4%). Although almost 95% of women reported having family doctors, a small percentage of those women (9.8%) had not seen that doctor in the previous 12 months. This percentage was higher in the group of women who had not had recent mammograms.
Table 1.
Characteristics of women (N = 15 195) aged 50 to 69 years who had screening mammograms in the past 2 years compared with those with no recent mammogram: All proportions were statistically and significantly different using χ2 tests.
| VARIABLE | RECENT SCREENING MAMMOGRAM, UNWEIGHTED %* | NO RECENT SCREENING MAMMOGRAM, UNWEIGHTED %* | TOTAL NO. | PROPORTION WHO HAD RECENT SCREENING MAMMOGRAMS, WEIGHTED |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Age, y | ||||
| • 50 to 54 | 24.6 | 25.4 | 3757 | 82.9 |
| • 55 to 59 | 29.3 | 25.9 | 4366 | 84.6 |
| • 60 to 64 | 25.3 | 24.9 | 3836 | 83.8 |
| • 65 to 69 | 20.8 | 23.8 | 3236 | 81.7 |
| Marital status | ||||
| • Single or never married | 7.2 | 9.2 | 1150 | 80.0 |
| • Common law | 5.4 | 5.6 | 825 | 81.1 |
| • Married | 58.2 | 49.0 | 8610 | 85.2 |
| • Widowed, separated, or divorced | 29.0 | 36.1 | 4591 | 79.4 |
| • Not stated | 0.1 | 0.2 | 19 | 84.3 |
| Income, $ | ||||
| • < 15 000 | 8.8 | 14.9 | 1495 | 76.1 |
| • 15 000 to 29 999 | 17.4 | 19.0 | 2686 | 81.2 |
| • 30 000 to 49 999 | 21.9 | 20.9 | 3296 | 83.8 |
| • 50 000 to 79 999 | 20.6 | 16.0 | 3014 | 86.2 |
| • 80 000 or more | 15.6 | 12.7 | 2301 | 84.5 |
| • Not stated | 15.7 | 16.6 | 2403 | 82.1 |
| Education | ||||
| • Some secondary school or less | 23.0 | 28.1 | 3622 | 80.0 |
| • Secondary school graduation | 18.1 | 16.1 | 2695 | 85.0 |
| • Some postsecondary | 6.0 | 6.2 | 912 | 82.7 |
| • Postsecondary graduation | 51.0 | 46.6 | 7636 | 84.5 |
| • Not stated | 2.0 | 2.9 | 330 | 78.1 |
| Province of residence | ||||
| • British Columbia | 10.8 | 13.9 | 1722 | 80.2 |
| • Alberta | 7.6 | 8.5 | 1177 | 82.1 |
| • Saskatchewan | 5.5 | 4.4 | 814 | 84.2 |
| • Manitoba | 5.1 | 5.3 | 776 | 80.7 |
| • Ontario | 32.3 | 30.4 | 4853 | 84.9 |
| • Quebec | 24.7 | 23.3 | 3715 | 83.4 |
| • New Brunswick | 4.7 | 4.6 | 706 | 83.6 |
| • Nova Scotia | 3.8 | 3.2 | 557 | 85.2 |
| • Prince Edward Island | 1.4 | 1.5 | 215 | 80.2 |
| • Newfoundland and Labrador | 3.2 | 3.2 | 488 | 83.6 |
| • Territories | 1.0 | 1.7 | 172 | 79.3 |
| Immigrant status | ||||
| • Nonimmigrant | 83.5 | 83.1 | 12 678 | 83.2 |
| • < 10 y | 0.5 | 0.5 | 81 | 86.1 |
| • ≥ 10 y | 14.3 | 13.9 | 2165 | 84.6 |
| • Not stated | 1.6 | 2.5 | 271 | 78.1 |
| Cancer screening behaviour | ||||
| Breast self-examination† | ||||
| • Yes | 84.0 | 79.5 | 887 | 84.4 |
| • No | 16.0 | 20.5 | 178 | 88.2 |
| Papanicolaou test | ||||
| • None in past 3 y | 25.0 | 55.7 | 4600 | 69.1 |
| • Within past 3 y | 75.0 | 44.3 | 10 595 | 88.9 |
| Other cancer risks | ||||
| Self-reported BMI | ||||
| • Underweight | 1.6 | 2.2 | 256 | 84.8 |
| • Normal | 40.6 | 38.8 | 6126 | 84.0 |
| • Overweight | 34.3 | 33.4 | 5182 | 83.9 |
| • Obese | 20.7 | 22.4 | 3183 | 81.8 |
| • Not stated | 2.0 | 3.2 | 448 | 79.5 |
| Smoking | ||||
| • Not at all | 82.9 | 70.5 | 12 279 | 85.4 |
| • Occasional | 2.7 | 3.2 | 428 | 85.1 |
| • Daily | 14.1 | 25.8 | 2448 | 71.7 |
| • Not stated | 0.2 | 0.5 | 40 | 62.9 |
| Alcohol | ||||
| • Never | 6.6 | 7.9 | 1037 | 82.8 |
| • Former drinker | 16.1 | 20.5 | 2557 | 81.1 |
| • Occasional drinker | 22.2 | 25.2 | 3456 | 81.2 |
| • Regular drinker | 54.0 | 44.8 | 7973 | 85.3 |
| • Not stated | 1.0 | 1.6 | 172 | 72.6 |
| Interaction with family doctor | ||||
| • None (no family doctor) | 4.9 | 11.4 | 909 | 68.5 |
| • Occasional (family doctor, not regular user) | 8.9 | 14.3 | 1490 | 74.1 |
| • Active (regular family doctor) | 86.2 | 74.3 | 12 796 | 85.4 |
| Total sample | 15 195 | 83.4 | ||
BMI—body mass index, CCHS—Canadian Community Health Survey.
Distributed proportions might not add up to 100 owing to rounding.
From optional part of the 2006 CCHS, asked only of women in Nova Scotia and Newfoundland (n = 1045).
As observed in Table 2, unadjusted odds ratios demonstrate a similar pattern to Table 1, with significant effects across all variables except breast self-examination (likely owing to small numbers). Again, reporting a recent Pap test and visiting a family doctor in the past 12 months were both meaningful indicators, highly increasing the odds that a woman reported a screening mammogram in the past 2 years.
Table 2.
Factors associated with recent screening mammography (within past 2 years): ORs that were statistically significant are presented in boldface.
| VARIABLE | UNADJUSTED OR (95% CI) | ADJUSTED OR (95% CI), MODEL 1* | ADJUSTED OR (95% CI), MODEL 2 |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Age, y | P < .01 | P < .001 | P = .02 |
| • 50 to 54 | Reference | Reference | Reference |
| • 55 to 59 | 1.13 (1.01–1.27) | 1.18 (1.05–1.33) | 1.19 (1.06–1.35) |
| • 60 to 64 | 1.06 (0.94–1.19) | 1.20 (1.050–1.36) | 1.18 (1.04–1.34) |
| • 65 to 69 | 0.92 (0.81–1.04) | 1.15 (1.00–1.32) | 1.12 (0.98–1.29) |
| Marital status | P < .0001 | P < .001 | P < .001 |
| • Single or never married | Reference group | Reference group | Reference group |
| • Common law | 1.07 (0.85–1.35) | 1.24 (0.97–1.58) | 1.22 (0.96–1.56) |
| • Married | 1.44 (1.21–1.71) | 1.32 (1.10–1.58) | 1.29 (1.08–1.56) |
| • Widowed, separated, or divorced | 0.97 (0.80–1.16) | 1.02 (0.84–1.24) | 1.02 (0.84–1.24) |
| • Not stated | 1.34 (0.32–5.68) | NA | 1.08 (0.23–5.05) |
| Income, $ | P < .0001 | P < .001 | P < .001 |
| • < 15 000 | Reference group | Reference group | Reference group |
| • 15 000 to 29 999 | 1.36 (1.12–1.64) | 1.11 (0.91–1.37) | 1.10 (0.90–1.36) |
| • 30 000 to 49 999 | 1.62 (1.35–1.95) | 1.18 (0.97–1.44) | 1.18 (0.97–1.44) |
| • 50 000 to 79 999 | 1.96 (1.63–2.36) | 1.32 (1.10–1.58) | 1.31 (1.07–1.61) |
| • 80 000 or more | 1.71 (1.43–2.05) | 0.94 (0.77–1.16) | 0.96 (0.78–1.18) |
| • Not stated | 1.44 (1.20–1.73) | 1.02 (0.83–1.24) | 1.03 (0.84–1.26) |
| Education | P < .0001 | NA | NA |
| • Some secondary school or less | Reference group | Not included | Not included |
| • Secondary school graduation | 1.42 (1.24–1.64) | ||
| • Some postsecondary | 1.20 (0.99–1.46) | ||
| • Postsecondary graduation | 1.36 (1.23–1.52) | ||
| • Not stated | 0.89 (0.70–1.14) | ||
| Province of residence | P = .001 | NA | NA |
| • British Columbia | Reference | Not included | Not included |
| • Alberta | 1.14 (0.95–1.36) | ||
| • Saskatchewan | 1.32 (0.99–1.77) | ||
| • Manitoba | 1.03 (0.80–1.32) | ||
| • Ontario | 1.39 (1.22–1.59) | ||
| • Quebec | 1.24 (1.08–1.42) | ||
| • New Brunswick | 1.26 (0.95–1.67) | ||
| • Nova Scotia | 1.43 (1.07–1.91) | ||
| • Prince Edward Island | 1.00 (0.53–1.89) | ||
| • Newfoundland and Labrador | 1.26 (0.90–1.78) | ||
| • Territories | 0.95 (0.36–2.47) | ||
| Immigrant status | P < .01 | NA | NA |
| • Nonimmigrant | Reference group | Not included | Not included |
| • < 10 y | 1.25 (0.85–1.84) | ||
| • ≥ 10 y | 1.11 (1.00–1.24) | ||
| • Not stated | 0.72 (0.56–0.93) | ||
| Cancer screening behaviour | |||
| Breast self-examination† | P > .05 | NA | NA |
| • Yes | 0.75 (0.44–1.27) | Not included | Not included |
| • No | Reference group | ||
| Papanicolaou test | P < .0001 | P < .001 | P < .0001 |
| • None in past 3 y | Reference group | Reference group | Reference group |
| • Within past 3 y | 3.59 (3.29–3.92) | 3.54 (3.23–3.89) | 3.41 (3.11–3.74) |
| Other cancer risks | |||
| Self reported BMI | P < .01 | NA | NA |
| • Underweight | 1.06 (0.76–1.49) | Not included | Not included |
| • Normal | Reference group | ||
| • Overweight | 0.99 (0.90–1.10) | ||
| • Obese | 0.85 (0.76–0.96) | ||
| • Not stated | 0.74 (0.58–0.94) | ||
| Smoking | P < .0001 | P < .01 | P < .0001 |
| • Not at all | Reference group | Reference group | Reference group |
| • Occasional | 0.97 (0.74, 1.28) | 1.04 (0.79, 1.38) | 1.08 (0.81, 1.43) |
| • Daily | 0.43 (0.39, 0.48) | 0.48 (0.43, 0.54) | 0.49 (0.44, 0.55) |
| • Not stated | 0.29 (0.16, 0.52) | 0.41 (0.18, 0.96) | 0.41 (0.22, 0.78) |
| Alcohol | P < .0001 | NA | NA |
| • Never | Reference group | Not included | Not included |
| • Former drinker | 0.89 (0.74–1.07) | ||
| • Occasional drinker | 0.90 (0.75–1.07) | ||
| • Regular drinker | 1.20 (1.02–1.42) | ||
| • Not stated | 0.55 (0.40–0.76) | ||
| Interaction with family doctor | P < .0001 | NA | P < .0001 |
| • None (no family doctor) | Reference group | Not included | Reference group |
| • Occasional (family doctor, not regular user) | 1.36 (1.09–1.59) | 1.20 (0.99–1.47) | |
| • Active (regular family doctor) | 2.69 (2.30–3.15) | 2.23 (1.89–2.64) | |
BMI—body mass index, CCHS—Canadian Community Health Survey, NA—not applicable, OR—odds ratio.
Model 1 excludes the key explanatory variable—active interaction with regular family doctor.
From optional part of the CCHS, asked only of women in Nova Scotia and Newfoundland (n = 1045).
In model 1, many of the sociodemographic variables (education, province of residence, and immigrant status) when combined with other variables, were no longer significant at the 95% confidence level; BMI was also eliminated from the model.
Model 2 included variables from each of the 3 main categories. Within the sociodemographic variables, those in the age groups of 55 to 59 years and 60 to 64 years were the most likely to have had recent mammograms. Being married was also associated with an increased likelihood of reporting a recent mammogram, and only the $50 000 to $79 999 income level continued to be significant (P = .0364). With respect to cancer risk variables, daily smokers were much less likely to have had recent mammograms; those who did not answer questions about their smoking habits were also less likely to participate in screening. With respect to the cancer screening variables, women who reported meeting the screening guidelines for Pap tests were more than 3 times as likely to also meet the breast cancer guidelines.
Lastly, responses indicated that having a regular family doctor and seeing that doctor in the past 12 months more than doubled the odds that the woman had had a recent mammogram. However, reporting having a family doctor but not having seen that doctor in the past year was no longer significantly associated with recent screening mammography.
DISCUSSION
A strength of this study, which differentiates it from earlier studies, is that we were able to focus exclusively on screening mammography. Previous studies did not differentiate between diagnostic and screening mammography; this might be somewhat misleading with respect to understanding screening motivations, and likely biased findings toward detecting a relationship between having a family doctor and participating in screening mammography. An additional strength is that we were able to look at reported behaviour over a 2-year period—consistent with the national benchmark for screening—rather than the shorter 1-year period used by some published research.7–9
Our study contributes new understanding of the association between screening participation and having a family doctor by exploring whether or not recent interaction is also important. As with earlier studies,5,9 we found that seeing a family doctor in the past 12 months more than doubles the odds of having had a screening mammogram in the past 2 years. However, this association did not remain significant for the less than 10% of women who reported having family doctors but who had not interacted with their doctors in the previous year.
Consistent with earlier studies,7,18 participation in cervical cancer screening more than triples the likelihood of recent breast cancer screening mammograms; and as with other studies, we found that smokers are less likely to undergo screening mammography. While most epidemiologists do not believe that there is an association between smoking and breast cancer,19 an earlier study showed that smokers believe that they are at a higher risk of breast cancer.20 Despite this perceived risk, however, both our study and the study by Maxwell et al5 found that smokers are less likely to be screened. In contrast, while Qi et al found that BMI was associated with screening mammography,9 this was not the case in our study.
Limitations
We did not analyze the survey results of women who did not answer the questions about whether they had had recent mammograms; the outcome of interest and key explanatory factor for these women might differ from those of the study population. A further limitation to this study and other studies that rely on surveys of reported behaviour is that self-reported behaviour tends to overestimate actual behaviour. May and Trontell found that self-reported mammography rates in the United States were up to 50% higher than those derived from Medicare data,21 and Hancock et al found that self-reported cervical cancer screening rates were 13% to 29% higher than utilization data would suggest.22 Finally, our finding of an association between regular interaction with a family doctor and participation in screening mammography does not imply causation. Women who seek preventive care are likely to also seek regular care from family doctors; other factors might also be responsible for this association.
Conclusion
Despite declining numbers of family doctors, active interaction with a family doctor continues to be substantially associated with participation in breast cancer screening. Further research exploring the relationship between family doctors and screening behaviour is needed to understand what makes this interaction effective. In the meantime, encouraging healthy women who do not have regular doctors to book their own mammograms with organized screening programs might be a worthwhile endeavour to increase participation. As well, educating women about the importance of having family doctors whom they see regularly might not only encourage breast cancer screening but overall health outcomes.
Acknowledgments
This study was conducted as part of Ms Poole’s doctoral program at the University of British Columbia in Vancouver, which was funded by the Western Regional Training Centre. Ms Poole thanks Dr Mieke Koehoorn for her support and guidance.
EDITOR’S KEY POINTS
Breast cancer remains a big health concern for Canadian women, with a lifetime prevalence of 1 in 9 and with 1 in 27 dying from the disease.
Over the past 25 years breast cancer mortality has declined substantially owing to improvements in treatment and screening in particular.
This secondary analysis of a cross-sectional sample of 15 195 Canadian women aged 50 to 69 years revealed that having a regular family doctor doubled a woman’s odds of having recently received a mammogram. Further, receiving other screening and preventive maneuvers (such as a Papanicolaou test, for example) was strongly associated with also having a recent mammogram.
Women who receive regular care from a family physician are much more likely to participate in screening mammography within the recommended time frames.
POINTS DE REPÈRE DU RÉDACTEUR
Le cancer du sein demeure une préoccupation majeure pour les Canadiennes, sa prévalence au cours de la vie étant de 1 sur 9, 1 femme sur 27 mourant de cette maladie
La mortalité due au cancer du sein a considérablement diminué au cours des 25 dernières années, grâce à l’amélioration du traitement et notamment du dépistage.
Cette analyse secondaire d’un échantillon transversal de 15 195 canadiennes âgées de 50 à 69 ans a révélé que celles qui avaient un médecin de famille régulier avaient 2 fois plus de chances d’avoir eu une mammographie récemment. En outre, le fait d’avoir eu une mammographie récente était fortement associé au fait d’avoir subi d’autres formes de dépistage et examens préventifs (tels que le Pap test).
Les femmes qui sont régulièrement suivies par un médecin de famille sont beaucoup plus susceptibles de subir une mammographie de dépistage aux intervalles de temps recommandés.
Footnotes
Excluded are people living on Native reserves or Crown lands, residents of institutions, full-time members of the Canadian Forces, and residents of certain remote regions.
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Ms Poole, Dr Gelmon, and Ms Kan each contributed to the concept and design of the study; Ms Poole to the data gathering; Ms Poole, Dr Black, and Ms Kan to the analysis; and Ms Poole, Dr Black, Dr Gelmon, and Ms Kan to the interpretation of the results and the preparation of the article for submission.
Competing interests
None declared
References
- 1.Canadian Cancer Society, National Cancer Institute of Canada . Canadian cancer statistics 2007. Toronto, ON: Canadian Cancer Society; 2007. Available from: www.cancer.ca/Canada-wide/About%20us/Media%20centre/CW-Media%20releases/CW-2007/~/media/CCS/Canada%20wide/Files%20List/English%20files%20heading/pdf%20not%20in%20publications%20section/2007%20Canadian%20Cancer%20Statistics%20%20PDF%20English_1816216925.ashx. Accessed 2010 Feb 23. [Google Scholar]
- 2.Cancer Intervention and Surveillance Modeling Network (CISNET) Breast Cancer Collaborators Executive summary. J Natl Cancer Inst Monogr. 2006. pp. 1–2. Available from: http://jncimono.oxfordjournals.org/cgi/content/full/2006/36/1. Accessed 2010 Feb 23.
- 3.Public Health Agency of Canada . Organized breast cancer screening programs in Canada. Report on program performance in 2001 and 2002. Ottawa, ON: Public Health Agency of Canada; 2005. Available from: www.phac-aspc.gc.ca/publicat/obcsp-podcs01/index-eng.php. Accessed 2010 Feb 24. [Google Scholar]
- 4.McIsaac WJ, Fuller-Thomson E, Talbot Y. Does having regular care by a family physician improve preventive care? Can Fam Physician. 2001;47:70–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Maxwell CJ, Bancej CM, Snider J. Predictors of mammography use among Canadian women aged 50–69: findings from the 1996/97 National Population Health Survey. CMAJ. 2001;164(3):329–34. [PMC free article] [PubMed] [Google Scholar]
- 6.Rauscher GH, Hawley ST, Earp JA. Baseline predictors of initiation vs. maintenance of regular mammography use among rural women. Prev Med. 2005;40(6):822–30. doi: 10.1016/j.ypmed.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 7.Zapka JG, Stoddard AM, Costanza ME, Greene HL. Breast cancer screening by mammography: utilization and associated factors. Am J Public Health. 1989;79(11):1499–502. doi: 10.2105/ajph.79.11.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jelinski SE, Maxwell CJ, Onysko J, Bancej CM. The influence of breast self-examination on subsequent mammography participation. Am J Public Health. 2005;95(3):506–11. doi: 10.2105/AJPH.2003.032656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qi V, Phillips SP, Hopman WM. Determinants of a healthy lifestyle and use of preventive screening in Canada. BMC Public Health. 2006;6:275. doi: 10.1186/1471-2458-6-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kondro W. Family practice a tough sell. CMAJ. 2007;176(11):1570–1. doi: 10.1503/cmaj.070577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Avinashi V, Shouldice E, Canadian Federation of Medical Students Increasing interest in family medicine. CMAJ. 2006;174(6):761–2. doi: 10.1503/cmaj.050752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Busing N, Newbery P. Robust description of family practice. A look at the National Physician Survey. Can Fam Physician. 2005;51(5):640–2. 647–9. Eng. (Fr). [PMC free article] [PubMed] [Google Scholar]
- 13.Luneau K. How to find a family doctor. Macleans.ca. 2008. Jan 3, Available from: www.macleans.ca/article.jsp?content=20080103_101501_5548. Accessed 2010 Feb 24.
- 14.Advisory Committee on Governance and Accountability . Plan for reporting comparable health indicators in November 2004. Ottawa, ON: Canadian Institute for Health Information; 2004. Available from: www.cihi.ca/cihiweb/en/downloads/ACGA_CBN_TO_CDM_ENG.pdf. Accessed 2010 Feb 24. [Google Scholar]
- 15.Health Statistics Division . Canadian community health survey (CCHS), cycle 3.1, 2005. Public use microdata file. Ottawa, ON: Statistics Canada; 2006. Available from: www.chass.utoronto.ca/datalib/inventory/0000/460.htm. Accessed 2010 Feb 24. [Google Scholar]
- 16.The University of British Columbia Board of Governors . Research and other studies involving human subjects. Vancouver, BC: University of British Columbia; 2006. Policy No. 89. Available from: www.universitycounsel.ubc.ca/policies/policy89.pdf. Accessed 2010 Feb 24. [Google Scholar]
- 17.Web-based sample size/power calculations [website] Vancouver, BC: University of British Columbia; Available from: www.stat.ubc.ca/~rollin/stats/ssize. Accessed 2010 Feb 24. [Google Scholar]
- 18.Phillips KA, Kerlikowske K, Baker LC, Chang SW, Brown ML. Factors associated with women’s adherence to mammography screening guidelines. Health Serv Res. 1998;33(1):29–53. [PMC free article] [PubMed] [Google Scholar]
- 19.Volume 83. Tobacco smoke and involuntary smoking. Lyon, FR: World Health Organization International Agency for Research on Cancer; 2004. IARC Monographs on the evaluation of carcinogenic risks to humans. Available from: http://monographs.iarc.fr/ENG/Monographs/vol83/index.php. Accessed 2010 Feb 24. [PMC free article] [PubMed] [Google Scholar]
- 20.Vernon SW, Vogel VG, Halabi S, Bondy ML. Factors associated with perceived risk of breast cancer among women attending a screening program. Breast Cancer Res Treat. 1993;28(2):137–44. doi: 10.1007/BF00666426. [DOI] [PubMed] [Google Scholar]
- 21.May DS, Trontell AE. Mammography use by elderly women: a methodological comparison of two national data sources. Ann Epidemiol. 1998;8(7):439–44. doi: 10.1016/s1047-2797(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 22.Hancock L, Sanson-Fisher R, Kentish L. Cervical cancer screening in rural NSW: Health Insurance Commission data compared to self-report. Aust N Z J Public Health. 1998;22(3 Suppl):307–12. doi: 10.1111/j.1467-842x.1998.tb01382.x. [DOI] [PubMed] [Google Scholar]