ABSTRACT
OBJECTIVE
To determine the knowledge, counseling practices, and learning needs of practitioners in British Columbia regarding risk factors for listeriosis in pregnancy.
DESIGN
A 1-page, mailed, self-administered, anonymous questionnaire.
SETTING
British Columbia.
PARTICIPANTS
A total of 827 practitioners (614 family physicians, 93 midwives, and 120 family practice residents) were sent the questionnaire.
MAIN OUTCOME MEASURES
Awareness of listeriosis, knowledge of the risk factors for listeriosis, practices for counseling pregnant women, practitioners’ learning needs, and provider and practice characteristics.
RESULTS
A total of 340 practitioners (41%) completed the questionnaire. While most (88%) physicians and midwives had heard of listeriosis, few (18%) were aware that infection was more common during pregnancy. One-third (33%) of practitioners counseled pregnant women about the risk factors for listeriosis. The main reasons for not providing such counseling were lack of knowledge and the perception that listeriosis was rare and not an important concern for pregnant women. Rates of counseling were highest among midwives (84%) and lowest among physicians practising outside the Lower Mainland of British Columbia (12%). Of those practitioners providing prenatal care, 47% counseled pregnant women about the risks of unpasteurized milk and 41% counseled women about the risks of consuming soft cheese; few counseled about the risks of consuming deli meat or raw hot dogs (25%), unwashed fruit and vegetables (12%), or refrigerated smoked seafood (6%).
CONCLUSION
Most prenatal care providers in British Columbia are unaware of the risk factors for listeriosis or its propensity for pregnant women and do not counsel their pregnant patients about these risks.
RÉSUMÉ
OBJECTIF
Vérifier les connaissances, les habitudes de counseling et les besoins de formation des médecins de la Colombie-Britannique au sujet des facteurs de risque pour la listériose durant la grossesse.
TYPE D’ÉTUDE
Un questionnaire auto-administré d’une page envoyé par la poste.
CONTEXTE
La Colombie-Britannique.
PARTICIPANTS
On a adressé le questionnaire à 827 intervenants (614 médecins de famille, 98 sages-femmes et 120 résidents en médecine familiale).
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
Connaissance de la listériose et de ses facteurs de risque, habitudes de counseling pour les femmes enceintes, besoins de formation pour les intervenants, et caractéristiques des intervenants et des modes de pratique.
RÉSULTATS
Au total, 340 intervenants (41 %) ont répondu au questionnaire. Alors que la plupart des médecins et des sages-femmes (88 %) avaient entendu parler de la listériose, peu (18 %) savaient que cette infection était plus fréquente durant la grossesse. Un tiers des intervenants (33 %) conseillaient les femmes enceintes sur les facteurs de risque de listériose. Les principales raisons pour ne pas le faire étaient le manque de connaissances, et l’idée que la listériose était rare et ne constituait pas une préoccupation importante pour les femmes enceintes. Les sages-femmes avaient le plus fort taux de counseling (84 %) et les médecins exerçant ailleurs que dans les basses terres de la Colombie-Britannique continentale, le plus bas (12 %). Parmi les intervenants qui dispensaient des soins prénataux, 47 % conseillaient les femmes enceintes sur les risques du lait non pasteurisé et 41 % sur les risques de consommer du fromage mou; peu parlaient des risques de consommer de la charcuterie ou des hot-dogs non cuits (25 %), des fruits et légumes non lavés (12 %) ou des fruits de mer fumés réfrigérés (6 %).
CONCLUSION
La plupart de ceux qui prodiguent des soins prénataux en Colombie-Britannique ignorent les facteurs de risque pour la listériose ou son incidence plus élevée chez la femme enceinte, et ils n’avertissent pas leurs patientes enceintes de ces risques.
A recent outbreak of listeriosis that resulted from contaminated cold cuts from a Toronto, Ont, meat processing plant has brought this condition to the attention of the Canadian public and the medical community.1 Listeriosis, caused by the bacteria Listeria monocytogenes, causes approximately 2500 serious illnesses and 500 deaths in the United States annually.2 Between 1992 and 1999, the incidence rates in Canada ranged from 0.15 to 0.35 per 100 000 population.3 Listeriosis is 17 times more likely to occur in pregnant women than in the general population, with about one-third of all cases occurring in this group.4,5 While there is no maternal mortality,6 approximately 20% of pregnancies complicated by listeriosis end in spontaneous abortion or stillbirth, and two-thirds of surviving infants develop clinical neonatal listeriosis.7 Infected newborns can develop pneumonia, sepsis, and meningitis, similar to the syndromes associated with group B streptococcal infection.4,8 Listeria accounts for 20% of all cases of meningitis in neonates—second only to group B streptococcus.9,10 Although the overall incidence of listeriosis is relatively low, it has a high case-fatality rate: 20 to 30 deaths per 100 cases of illness.5,6,11
Scientists first recognized that Listeria could be spread through food in the early 1980s.12,13 Most infections are sporadic, with occasional outbreaks around the world.4,7,14 In the 1980s, there was an outbreak in Nova Scotia linked to coleslaw made from cabbage contaminated with sheep manure.7,8 There have been several outbreaks in the United States associated with Mexican-style soft cheese, queso fresco, made from unpasteurized milk9,12,15,16; pasteurized milk products17; and hot dogs or deli meat.2,18 In France and Denmark there have been episodes associated with a raw-milk soft cheese (Brie), pork tongue, and rillettes (pork pâté).16,19,20 More recent evidence has shown a possible association with several foods prepared in a retail environment, including cut melons and hummus.14 The foods with the highest risk are often ready-to-eat foods stored at refrigeration temperature for prolonged periods.6,21 In one American study, the overall prevalence of L monocytogenes in ready-to-eat foods such as luncheon meats, deli salads, blue-veined and soft cheeses, bagged salads, smoked seafood, and seafood salads was estimated to be 1.82%, and was as high as 4.7% in some of the food categories.22 Listeria is second only to Salmonella as the most costly food-borne pathogen for children younger than 10 years of age in the United States ($0.8 billion [US]).23 It is responsible for 27.6% of food-related deaths in the United States.11 The Centers for Disease Control and Prevention, the US Food and Drug Administration, the US Department of Agriculture, the American Congress of Obstetricians and Gynecologists, the Society of Obstetricians and Gynaecologists of Canada, and the Canadian Food Inspection Agency all recommend pregnant women avoid foods known to be at increased risk of contamination with Listeria.
Studies conducted in the United States and Australia found that pregnant women were not aware of the increased risk of food-borne illness in pregnancy, were not familiar with listeriosis, and were not given information on food safety by their health care providers.24–28 A small study of health care providers in the United States showed that few provided food safety information to pregnant women.29 To date, there have been no Canadian studies of the knowledge and counseling practices of health care providers about listeriosis in pregnancy. In the aftermath of the recent Canadian outbreak, one of the worst epidemics of listeriosis in history, it is important to understand the current state of knowledge and counseling practices of health care providers as a starting point for the development of new public health policy and educational programs.1 The objective of this study was to assess the knowledge, counseling practices, and learning needs of British Columbia physicians and midwives regarding listeriosis in pregnancy.
METHODS
The questionnaire was distributed to 827 practitioners in British Columbia by Canada Post or through intrahospital mail in June 2005. In an effort to survey clinicians who would be primary care opinion leaders and teachers for prenatal care in the province of British Columbia, specific groups were selected for sampling. These comprised 614 family physicians: all those on staff in the departments of family practice at BC Women’s Hospital in Vancouver (n = 161) and St Paul’s Hospital in Vancouver (n = 249), 79 practising in Prince George, and 125 general practitioners randomly selected from the directory of the College of Physicians and Surgeons of British Columbia, excluding those practising in the Vancouver area. The survey was also distributed to all 93 midwives registered with the College of Midwives of British Columbia, enclosed in a regular mailing from the College, and to all 120 family practice residents attending the June 2005 University of British Columbia Family Practice Residency Program Research Day, as part of their registration packages.
A 1-page, self-administered, anonymous questionnaire that included questions about awareness of listeriosis, knowledge of the risk factors for listeriosis, practices for counseling pregnant women, and practitioners’ learning needs with regards to listeriosis was developed using information drawn from a review of the literature. Respondents were also asked how long they had been in practice and whether they provided prenatal or intrapartum care. The questionnaire took approximately 3 minutes to complete. The questionnaire was pilot-tested by a statistician and several practitioners with interests in obstetrics or research design for face and content validity. Questionnaires were colour-coded to distinguish between the different groups surveyed and were returned by preaddressed, stamped envelope. Participants were invited to enter into a draw for a small prize by returning a preaddressed, stamped postcard. A copy of the questionnaire is available from the authors upon request.
Data from the completed questionnaires were entered into a computer database. Statistical analysis included frequency tables for categorical variables, and the associations between categorical variables were assessed using cross-tabulations and χ2 tests. We compared practitioners’ knowledge and behaviour with demographic variables. Statistical analysis was carried out using SPSS version 15.0. Assuming a response rate of approximately 50%, we anticipated receiving approximately 400 surveys that would provide a margin of error of 5%. The University of British Columbia Behavioural Research Ethics Board approved the study.
RESULTS
A total of 340 of the practitioners surveyed completed the questionnaire (41%). Table 1 outlines the demographic characteristics of the respondents; almost half (47%) were practising in the Vancouver area and were affiliated with large teaching hospitals. Physicians from outside the Lower Mainland and medical residents accounted for just over one-fifth of the study population each, and slightly more than 10% of respondents were midwives. More than half of respondents had been in practice for more than 10 years. Most were providing prenatal care to patients, and slightly more than half were providing labour and delivery care.
Table 1.
Characteristics of survey respondents
| CHARACTERISTICS | NO. | % |
|---|---|---|
| Study group | ||
| • BC Women’s Hospital staff | 70 | 20.6 |
| • St Paul’s Hospital staff | 90 | 26.5 |
| • Prince George physicians | 27 | 7.9 |
| • College of Physicians and Surgeons directory | 48 | 14.1 |
| • Family practice residents | 68 | 20.0 |
| • Midwives | 37 | 10.9 |
| • Total (n = 340) | 340 | 100.0 |
| Years in practice | ||
| • In training | 52 | 15.4 |
| • 0–9 | 94 | 27.9 |
| • 10–19 | 75 | 22.3 |
| • ≥ 20 | 116 | 34.4 |
| • Total (n = 337) | 337 | 100.0 |
| Providing prenatal care | ||
| • Yes | 269 | 79.8 |
| • No | 68 | 20.2 |
| • Total (n = 337) | 337 | 100.0 |
| Providing intrapartum care | ||
| • Yes | 176 | 52.4 |
| • No | 160 | 47.6 |
| • Total (n = 336) | 336 | 100.0 |
Knowledge
Most (88%) of the respondents had heard of listeriosis, and the likelihood of being aware of listeriosis was not affected by number of years in practice or location of practice. Midwives were more likely to have heard of listeriosis than physicians were (100% vs 86%, P = .017). Practitioners providing prenatal care were more likely to have heard of listeriosis than those not providing such care (92% vs 73.5%, P < .001). Rates of awareness of listeriosis were the same among practitioners providing prenatal care only and those providing both prenatal and intrapartum care.
Few practitioners (18%) were aware that listeriosis was more common in pregnant women than in the general population. Knowledge of the propensity of listeriosis for pregnant women was not significantly associated with years in practice, study group, or providing prenatal or intrapartum care (Table 2). Of those practitioners providing prenatal care (n = 251), midwives (24%) and physicians in the Lower Mainland (20%) were slightly more likely (P = .013) to be aware of the affinity of L monocytogenes for pregnant women than were residents (15%) or physicians practising elsewhere in the province (15%).
Table 2.
Participants’ awareness that listeriosis is more common among pregnant women
| CHARACTERISTICS |
AWARE |
NOT AWARE |
UNSURE |
TOTAL |
||||
|---|---|---|---|---|---|---|---|---|
| NO. | % | NO. | % | NO. | % | NO. | % | |
| Years in practice | ||||||||
| • In training | 10 | 20.0 | 9 | 18.0 | 31 | 62.0 | 50 | 16.5 |
| • 0–9 | 14 | 16.7 | 21 | 25.0 | 49 | 58.3 | 84 | 27.7 |
| • 10–19 | 12 | 17.6 | 16 | 23.5 | 40 | 58.8 | 68 | 22.4 |
| • ≥ 20 | 19 | 18.8 | 23 | 22.8 | 59 | 58.4 | 101 | 33.3 |
| • Total (n = 303); P = .99 | 55 | 18.2 | 69 | 22.8 | 179 | 59.1 | 303 | 100.0 |
| Study group | ||||||||
| • Doctors in Vancouver | 27 | 19.3 | 32 | 22.9 | 81 | 57.9 | 140 | 45.9 |
| • Doctors in rest of British Columbia | 9 | 14.3 | 8 | 12.7 | 46 | 73.0 | 63 | 20.7 |
| • Family practice residents | 10 | 15.4 | 14 | 21.5 | 41 | 63.1 | 65 | 21.3 |
| • Midwives | 9 | 24.3 | 15 | 40.5 | 13 | 35.1 | 37 | 12.1 |
| • Total (n = 305); P = .016 | 55 | 18.0 | 69 | 22.6 | 181 | 59.3 | 305 | 100.0 |
| Practitioners providing prenatal care | ||||||||
| • Yes | 46 | 18.3 | 63 | 25.1 | 142 | 56.6 | 251 | 83.1 |
| • No | 9 | 17.6 | 6 | 11.8 | 36 | 70.6 | 51 | 16.9 |
| • Total (n = 302); P = .094 | 55 | 18.2 | 69 | 22.8 | 178 | 58.9 | 302 | 100.0 |
| Practitioners attending deliveries | ||||||||
| • Yes | 33 | 19.9 | 44 | 26.5 | 89 | 53.6 | 166 | 55.1 |
| • No | 21 | 15.6 | 25 | 18.5 | 89 | 65.9 | 135 | 44.9 |
| • Total (n = 301); P = .093 | 54 | 17.9 | 69 | 22.9 | 178 | 59.1 | 301 | 100.0 |
Counseling practices
One-third (33%) of all practitioners surveyed counseled pregnant women about the risk factors for listeriosis (Table 3). Among those practitioners providing prenatal care, the rate of counseling was 40%. Rates of counseling within the study group (P < .001) were highest among midwives (84%) and lowest among physicians practising outside the Lower Mainland (12%; 15% of those providing prenatal care). Of the 270 respondents who provided prenatal or intrapartum care or both, less than half counseled pregnant patients about the risks of consuming unpasteurized milk products (47%) and soft cheeses (41%). One-quarter (25%) informed these patients of the risks of eating deli meat or raw hot dogs, and fewer provided counseling about the risks of eating unwashed fruits and vegetables (12%) and refrigerated smoked seafood (6%). Midwives were the most likely to counsel pregnant patients about each of the risk factors for listeriosis (Table 4). Physicians practising outside the Lower Mainland and residents were the least likely to provide counseling about most risk factors.
Table 3.
Characteristics of practitioners who did or did not counsel pregnant women about risk factors for listeriosis
| CHARACTERISTICS |
DID COUNSEL |
DID NOT COUNSEL |
TOTAL |
|||||
|---|---|---|---|---|---|---|---|---|
| NO. | % | NO. | % | NO. | % | |||
| Years in practice | ||||||||
| • In training | 16 | 31.4 | 35 | 68.6 | 51 | 16.5 | ||
| • 0–9 | 31 | 36.0 | 55 | 64.0 | 86 | 27.7 | ||
| • 10–19 | 25 | 36.8 | 43 | 63.2 | 68 | 21.9 | ||
| • ≥ 20 | 32 | 30.5 | 73 | 69.5 | 105 | 33.9 | ||
| • Total (n = 310); P = .78 | 104 | 33.5 | 206 | 66.5 | 310 | 100.0 | ||
| Study group | ||||||||
| • Doctors in Vancouver | 47 | 32.6 | 97 | 67.4 | 144 | 46.0 | ||
| • Doctors in rest of British Columbia | 8 | 12.1 | 58 | 87.9 | 66 | 21.1 | ||
| • Family practice residents | 18 | 27.3 | 48 | 72.7 | 66 | 21.1 | ||
| • Midwives | 31 | 83.8 | 6 | 16.2 | 37 | 11.8 | ||
| • Total (n = 313); P < .001 | 104 | 33.2 | 209 | 66.8 | 313 | 100.0 | ||
| Practitioners providing prenatal care | ||||||||
| • Yes | 102 | 40.2 | 152 | 59.8 | 254 | 81.9 | ||
| • No | 1 | 1.8 | 55 | 98.2 | 56 | 18.1 | ||
| • Total (n = 310); P < .001 | 103 | 33.2 | 207 | 66.8 | 310 | 100.0 | ||
| Practitioners attending deliveries | ||||||||
| • Yes | 76 | 45.5 | 91 | 54.5 | 167 | 54.0 | ||
| • No | 26 | 18.3 | 116 | 81.7 | 142 | 46.0 | ||
| • Total (n = 309); P < .001 | 102 | 33.0 | 207 | 67.0 | 309 | 100.0 | ||
Table 4.
Rates of counseling about the various risk factors for listeriosis among practitioners providing prenatal or intrapartum care: N = 270.
| RISK FACTOR |
DOCTORS IN VANCOUVER |
DOCTORS IN THE REST OF BRITISH COLUMBIA |
RESIDENTS |
MIDWIVES |
TOTAL |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| NO. | % | NO. | % | NO. | % | NO. | % | NO. | % | |
| Eating soft cheeses | ||||||||||
| • Counseled | 46 | 40.7 | 10 | 17.2 | 20 | 32.3 | 35 | 94.6 | 111 | 41.1 |
| • Did not counsel | 67 | 59.3 | 48 | 82.8 | 42 | 67.7 | 2 | 5.4 | 159 | 58.9 |
| • Total (n = 270); P < .001 | 113 | 58 | 62 | 37 | 270 | |||||
| Consuming unpasteurized milk or milk products | ||||||||||
| • Counseled | 55 | 48.7 | 15 | 25.9 | 24 | 38.7 | 33 | 89.2 | 127 | 47.0 |
| • Did not counsel | 58 | 51.3 | 43 | 74.1 | 38 | 61.3 | 4 | 10.8 | 143 | 53.0 |
| • Total (n = 270); P < .001 | 113 | 58 | 62 | 37 | 270 | |||||
| Eating deli meat or raw hot dogs | ||||||||||
| • Counseled | 24 | 21.2 | 7 | 12.1 | 10 | 16.1 | 26 | 70.3 | 67 | 24.8 |
| • Did not counsel | 89 | 78.8 | 51 | 87.9 | 52 | 83.9 | 11 | 29.7 | 203 | 75.2 |
| • Total (n = 270); P < .001 | 113 | 58 | 62 | 37 | 270 | |||||
| Eating unwashed fruits and vegetables | ||||||||||
| • Counseled | 11 | 9.7 | 6 | 10.3 | 2 | 3.2 | 13 | 35.1 | 32 | 11.9 |
| • Did not counsel | 102 | 90.3 | 52 | 98.7 | 60 | 96.8 | 24 | 64.9 | 238 | 88.1 |
| • Total (n = 270); P < .001 | 113 | 58 | 62 | 37 | 270 | |||||
| Eating refrigerated smoked seafood | ||||||||||
| • Counseled | 7 | 6.2 | 1 | 1.7 | 2 | 3.2 | 6 | 16.2 | 16 | 5.9 |
| • Did not counsel | 106 | 93.8 | 57 | 98.3 | 60 | 96.8 | 31 | 83.8 | 254 | 94.1 |
| • Total (n = 270); P = .021 | 113 | 58 | 62 | 37 | 270 | |||||
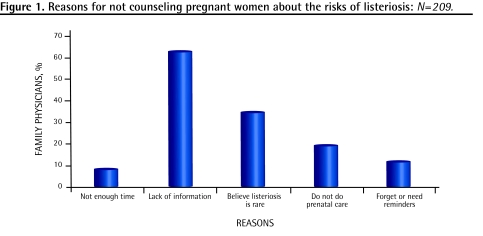
The most common reasons given for not counseling pregnant women about listeriosis (Figure 1) were lack of knowledge about the risk factors (64%) and the perception that listeriosis was rare and therefore not an important concern for pregnant women (34%). Of those practitioners providing prenatal or intrapartum care, physicians practising outside the Lower Mainland were the most likely (P ≤ .001) not to provide counseling because of the perception that listeriosis was rare (41%) compared with residents (23%), physicians practising in the Lower Mainland (20%), and midwives (8%). Physicians practising outside the Lower Mainland were also the most likely (P ≤ .001) to cite lack of knowledge of the risk factors for listeriosis as a reason for not providing counseling (57%), compared with residents (48%), physicians practising in the Lower Mainland (46%), and midwives (16%). Reasons for not providing counseling were not affected by years in practice.
Figure 1.
Reasons for not counseling pregnant women about the risks of listeriosis: N=209.
Learning needs
Most practitioners (82%) wanted more information about listeriosis in pregnancy (87% of practitioners providing prenatal care; P < .001) and more than half (54%) indicated that they would use a tool to screen for risk factors for listeriosis if one were available (31% were unsure).
DISCUSSION
We found that although most physicians and midwives had heard of listeriosis, few were aware that infection was more common in pregnancy. One-third of practitioners counsel pregnant women about the risk factors for listeriosis. The main reasons given for not counseling were lack of knowledge and the perception that listeriosis was rare and not an important concern for pregnant women. Rates of counseling were highest among midwives and lowest among physicians practising outside the Lower Mainland.
The low rate of counseling about prevention of listeriosis was consistent with other studies in which pregnant women reported that their health care providers rarely provided information on food safety.24,25 Focus groups conducted with 63 pregnant women in the United States showed that none of the participants had received information on listeriosis from her care provider.24 Most participants were not aware of the increased risk of food-borne illnesses during pregnancy or of current food safety recommendations, and most had not made any changes to their food-handling behaviour.
Very few studies have examined health care providers’ knowledge or practices with regard to listeriosis prevention. One American study of 23 health care providers showed that few (8/23) reported providing food safety information to pregnant women.29 As in our study, lack of knowledge of the risk factors was identified as a main barrier to counseling pregnant women. Limited contact time with patients was also seen as a prominent barrier; however, less than 10% of practitioners in our study identified lack of time as a substantial barrier.
Food safety experts in the United States, using a Web-based Delphi process, identified the following behaviour as the most important for reducing risk of food-borne illness in pregnant women: avoiding soft cheeses, cold smoked fish, and cold deli salads; heating hot dogs and cold cuts to 165°F (74°C); avoiding unpasteurized milk or cheese; avoiding raw or under-cooked eggs; and not handling pets while preparing food.30 While most of these recommendations were intended to decrease risk of exposure to L monocytogenes, the recommendation to avoid raw egg pertains to the risk of Salmonella, and the recommendation regarding avoidance of pet handling is to decrease exposure to Toxoplasma gondii. In our study, less than half of practitioners providing prenatal or intrapartum care were counseling patients about the risks of consuming soft cheeses and unpasteurized milk products, and few were advising their patients about the risks of deli meat, raw hot dogs, unwashed fruit and vegetables, and refrigerated smoked seafood. This is similar to the American study of 23 health care providers showing that health care providers were the least aware of recommendations to avoid soft cheeses, smoked fish, and cold deli salads and to heat hot dogs and cold cuts until steaming.29
In a study examining women’s attitudes toward these guidelines, there was low acceptance of many of these recommendations, especially avoiding soft cheeses, cold smoked fish, and cold deli salads, and heating luncheon meet until steaming hot.28 The women wanted clear explanations of the reasons behind the guidelines and stated that they would be most likely to trust food safety information provided by their doctors. In the same study, the participants were clear that they wanted to do what was necessary to protect the health of their unborn children and would make the recommended changes to their behaviour if they knew the health of their children was at risk.
Awareness of the risks of listeriosis might have changed since the recent outbreak in Canada. In particular, practitioners might be more aware of the risks associated with consuming deli meat. The magnitude of this outbreak, with 57 confirmed cases and 21 deaths, has focused considerable media attention on this issue.1,31 A smaller outbreak of listeriosis affecting Vancouver Island and the Lower Mainland in 2002, caused by contamination of cheese products from a small manufacturer, might explain the somewhat higher rates of counseling among physicians practising in the Lower Mainland compared with those elsewhere in the province. However, despite several targeted educational campaigns in the United States by government and the Centers for Disease Control and Prevention, as well as media attention drawn by several multistate outbreaks, most pregnant women in one American study had never heard of listeriosis.25
Health care providers expressed an interest in having more information on listeriosis in pregnancy and access to a screening tool to assess the risks for listeriosis. It is likely that additional foods could be implicated in causing listeriosis, and future outbreaks could be linked to food handling at retail outlets as well as food production and processing.14 It will be important for health care providers to be kept up-to-date about potential new high-risk foods. A prompt for counseling pregnant women about food safety on the provincial antepartum record and other maternity care guidelines might be helpful. Information campaigns on the risk of food-borne illness in pregnant women that address the reasons behind each recommendation for both the women and their health care providers will be important.28 Women feel that the best source of information about the risks of listeriosis is their health care providers.24,28 Several studies suggest that educational brochures on the risks of listeriosis would be a preferred tool for pregnant women.26,28,29 An interactive multimedia food safety education program viewed on a computer has also been shown to be well received by patients and effective at changing self-reported food safety behaviour.32 Future research to examine pregnant women’s knowledge of the risks of listeriosis and food safety practices, as well as the preferred educational tools for both practitioners and pregnant women, would be of benefit.
Limitations
These results should be interpreted in the context of several limitations. First, the relatively low response rate increases the likelihood of a selection bias. Although response rates of physicians to postal questionnaires tend to be lower than surveys of the general population,33,34 a second mailing of the survey might have been warranted and could have increased the response rate. Also the study population was specifically chosen to include practitioners with an interest in obstetrics, as reflected by half of respondents participating in intrapartum care. Physicians on staff at BC Women’s Hospital, an obstetrics referral centre, are more likely to be involved in obstetrical care, as are midwives and residents. The group surveyed would likely not be representative of the average general practitioner in British Columbia, and might over-estimate the interest in and awareness of listeriosis. Recall and social desirability biases can occur with self-reporting of behaviour. It was anticipated that the use of an anonymous, self-administered questionnaire might minimize this effect.
Conclusion
This is the first study in Canada to provide information on the knowledge and counseling practices of health care providers regarding listeriosis. The results of the study demonstrate that most family physicians providing prenatal care in British Columbia are unaware of the risk factors for listeriosis and do not counsel their pregnant patients about these risks. In contrast, most midwives, although unaware of the increased risk of listeriosis in pregnant women, do counsel their patients about some of the risk factors for listeriosis. Health care providers would like more information about the risk factors for listeriosis and expressed interest in a tool that would help them screen pregnant patients for potential risk factors.
Acknowledgments
We thank the College of Family Physicians of Canada for their support.
Dr Kirkham’s research was supported by the Vancouver Foundation through a BC Medical Services Foundation grant to the Community Based Clinical Investigator Program at the University of British Columbia’s Department of Family Practice. We also thank the Department of Family and Community Medicine at St Paul’s Hospital for their support and Drs Janusz Kaczorowski, Gina Ogilvie, Michael Klein, and Stephen Kurdyak and Ms Marsha Taylor for their review of the manuscript. We thank Sharon Lou Hing, Jean Kozoway, Joan Decker, and Mary Burgoyne for assistance with distribution and collection of surveys in their organizations.
EDITOR’S KEY POINTS
Listeriosis is 17 times more likely to occur in pregnant women than in the general population, with about one-third of all cases occurring in this group.
While there is no maternal mortality, approximately 20% of pregnancies complicated by listeriosis end in spontaneous abortion or stillbirth, and two-thirds of surviving infants develop clinical neonatal listeriosis. Listeria accounts for 20% of all cases of meningitis in neonates—second only to group B streptococcus.
The foods with the highest risk are often ready-to-eat foods stored at refrigeration temperature for prolonged periods.
Many agencies (although not all—see the Motherisk Update on page 341 of the April 2010 issue) recommend that pregnant women avoid foods known to be at increased risk of contamination with Listeria. The results of this study demonstrate that most family physicians providing prenatal care in British Columbia were unaware of the risk factors for listeriosis at the time of the study and did not counsel their pregnant patients about these risks.
POINTS DE REPÈRE DU RÉDACTEUR
Par rapport à la population générale, la femme enceinte est 17 fois plus susceptible de souffrir de listériose, environ un tiers de tous les cas survenant dans ce groupe.
Même s’il n’y a pas de mortalité maternelle, environ 20 % des grossesses compliquées de listériose aboutissent à un avortement ou à une mortinatalité spontanés, et les deux-tiers des nourrissons qui survivent développent une listériose néonatale. Le Listeria est responsable de 20 % des méningites chez les nouveau-nés—au deuxième rang derrière le streptocoque du groupe B.
Les aliments qui comportent le plus de risques sont souvent les plats cuisinés gardés réfrigérés durant une longue période.
Plusieurs agences (voir le numéro d’avril 2010 de Motherisk Update, page 341) recommandent à la femme enceinte d’éviter les aliments connus pour comporter davantage de risques de contamination par le Listeria. Nos résultats montrent qu’au moment de l’étude, la plupart des médecins de famille dispensant des soins prénataux en Colombie-Britannique ne connaissaient pas les facteurs de risque pour la listériose et n‘informaient pas leurs patientes enceintes de ces risques.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Dr Kirkham designed and conducted the study and wrote the manuscript. Dr Berkowitz conducted the statistical analysis of the data and critically revised the article.
Competing interests
None declared
References
- 1.Attaran A, MacDonald N, Stanbrook MB, Sibbald B, Flegel K, Kale R, et al. Listeriosis is the least of it. CMAJ. 2008;179(8):739–40. 743–4. doi: 10.1503/cmaj.081477. Eng. Fr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Multistate outbreak of listeriosis—United States, 2000. JAMA. 2001;285(3):285–6. [PubMed] [Google Scholar]
- 3.Public Health Agency of Canada . Notifiable diseases on-line [homepage on the Internet] Ottawa, ON: Public Health Agency of Canada; 2006. Available from: http://dsol-smed.phac-aspc.gc.ca/dsol-smed/ndis/c_time_e.html. Accessed 2009 Apr 15. [Google Scholar]
- 4.Silver HM. Listeriosis during pregnancy. Obstet Gynecol Surv. 1998;53(12):737–40. doi: 10.1097/00006254-199812000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Voelker R. Listeriosis outbreak prompts action—finally. JAMA. 2002;288(21):2675–6. [PubMed] [Google Scholar]
- 6.Rocourt J. Risk factors for listeriosis. Food Contr. 1996;7(4–5):195–202. [Google Scholar]
- 7.Mylonakis E, Paliou M, Hohmann EL, Calderwood SB, Wing EJ. Listeriosis during pregnancy: a case series and review of 222 cases. Medicine (Baltimore) 2002;81(4):260–9. doi: 10.1097/00005792-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Schuchat A. Listeriosis and pregnancy: food for thought. Obstet Gynecol Surv. 1997;52(12):721–2. doi: 10.1097/00006254-199712000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Braden CR. Listeriosis. Pediatr Infect Dis J. 2003;22(8):745–6. doi: 10.1097/01.inf.0000079439.30496.57. [DOI] [PubMed] [Google Scholar]
- 10.Posfay-Barbe KM, Wald ER. Listeriosis. Pediatr Rev. 2004;25(5):151–9. doi: 10.1542/pir.25-5-151. [DOI] [PubMed] [Google Scholar]
- 11.Mead PS, Slutsker L, Dietz V, McCaig LF, Bresee JS, Shapiro C, et al. Food-related illness and death in the United States. Emerg Infect Dis. 1999;5(5):607–25. doi: 10.3201/eid0505.990502. Comment in: Hedberg C. Food-related illness and death in the United States. Emerg Infect Dis 1999;5(6): 840–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linnan MJ, Mascola L, Lou XD, Goulet V, May S, Salminen C, et al. Epidemic listeriosis associated with Mexican-style cheese. N Engl J Med. 1988;319(13):823–8. doi: 10.1056/NEJM198809293191303. [DOI] [PubMed] [Google Scholar]
- 13.Formanek R., Jr Highlights of FDA food safety efforts: fruit juice, mercury in fish. FDA Consum. 2001;35(2):15–7. [PubMed] [Google Scholar]
- 14.Varma JK, Samuel MC, Marcus R, Hoekstra RM, Medus C, Segler S, et al. Listeria monocytogenes infection from foods prepared in a commercial establishment: a case-control study of potential sources of sporadic illness in the United States. Clin Infect Dis. 2007;44(4):521–8. doi: 10.1086/509920. Epub 2007 Jan 8. [DOI] [PubMed] [Google Scholar]
- 15.Outbreak of listeriosis associated with homemade Mexican-style cheese— North Carolina, October 2000–January 2001. MMWR Morb Mortal Wkly Rep. 2001;50(26):560–2. [PubMed] [Google Scholar]
- 16.Jensen A, Frederiksen W, Gerner-Smidt P. Risk factors for listeriosis in Denmark, 1989–1990. Scand J Infect Dis. 1994;26(2):171–8. doi: 10.3109/00365549409011781. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention Outbreak of Listeria monocytogenes infections associated with pasteurized milk from a local dairy— Massachusetts, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(40):1097–100. [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention Update: multistate outbreak of listeriosis—United States, 1998–1999. MMWR Morb Mortal Wkly Rep. 1999;47(51–52):1117–8. [PubMed] [Google Scholar]
- 19.Goulet V, Rocourt J, Rebiere I, Jacquet C, Moyse C, Dehaumont P, et al. Listeriosis outbreak associated with the consumption of rillettes in France in 1993. J Infect Dis. 1998;177(1):155–60. doi: 10.1086/513814. [DOI] [PubMed] [Google Scholar]
- 20.Goulet V, Jacquet C, Vaillant V, Rebiere I, Mouret E, Lorente C, et al. Listeriosis from consumption of raw-milk cheese. Lancet. 1995;345(8964):1581–2. doi: 10.1016/s0140-6736(95)91135-9. [DOI] [PubMed] [Google Scholar]
- 21.Bortolussi R. Listeriosis: a primer. CMAJ. 2008;179(8):795–7. doi: 10.1503/cmaj.081377. Epub 2008 Sep 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gombas DE, Chen Y, Clavero RS, Scott VN. Survey of Listeria monocytogenes in ready-to-eat foods. J Food Prot. 2003;66(4):559–69. doi: 10.4315/0362-028x-66.4.559. [DOI] [PubMed] [Google Scholar]
- 23.Buzby JC. Children and microbial foodborne illness. Food Rev. 2001;24(2):32–7. [Google Scholar]
- 24.Cates SC, Carter-Young HL, Conley S, O’Brien B. Pregnant women and listeriosis: preferred educational messages and delivery mechanisms. J Nutr Educ Behav. 2004;36(3):121–7. doi: 10.1016/s1499-4046(06)60148-6. [DOI] [PubMed] [Google Scholar]
- 25.Ogunmodede F, Jones JL, Scheftel J, Kirkland E, Schulkin J, Lynfield R. Listeriosis prevention knowledge among pregnant women in the USA. Infect Dis Obstet Gynecol. 2005;13(1):11–5. doi: 10.1080/02656730400025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Torvaldsen S, Kurinczuk JJ, Bower C, Parsons DE, Roberts CL. Listeria awareness among new mothers in western Australia. Aust N Z J Public Health. 1999;23(4):362–7. doi: 10.1111/j.1467-842x.1999.tb01276.x. [DOI] [PubMed] [Google Scholar]
- 27.Bondarianzadeh D, Yeatman H, Condon-Paoloni D. Listeria education in pregnancy: lost opportunity for health professionals. Aust N Z J Public Health. 2007;31(5):468–74. doi: 10.1111/j.1753-6405.2007.00120.x. [DOI] [PubMed] [Google Scholar]
- 28.Athearn PN, Kendall PA, Hillers VV, Schroeder M, Bergmann V, Chen G, et al. Awareness and acceptance of current food safety recommendations during pregnancy. Matern Child Health J. 2004;8(3):149–62. doi: 10.1023/b:maci.0000037648.86387.1d. [DOI] [PubMed] [Google Scholar]
- 29.Morales S, Kendall PA, Medeiros LC, Hillers V, Schroeder M. Health care providers’ attitudes toward current food safety recommendations for pregnant women. Appl Nurs Res. 2004;17(3):178–86. doi: 10.1016/j.apnr.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Kendall P, Medeiros LC, Hillers V, Chen G, DiMascola S. Food handling behaviors of special importance for pregnant women, infants and young children, the elderly, and immune-compromised people. J Am Diet Assoc. 2003;103(12):1646–9. doi: 10.1016/j.jada.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 31.Public Health Agency of Canada . Listeria monocytogenes outbreak [website] Ottawa, ON: Public Health Agency of Canada; 2009. Available from: www.phac-aspc.gc.ca/alert-alerte/listeria/listeria_2009-eng.php. Accessed 2010 Mar 15. [Google Scholar]
- 32.Trepka MJ, Newman FL, Davila EP, Matthew KJ, Dixon Z, Huffman FG. Randomized controlled trial to determine the effectiveness of an interactive multimedia food safety education program for clients of the special supplemental nutrition program for women, infants, and children. J Am Diet Assoc. 2008;108(6):978–84. doi: 10.1016/j.jada.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 33.Burns KE, Duffett M, Kho ME, Meade MO, Adhikari NK, Sinuff T, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179(3):245–52. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grava-Gubins I, Scott S. Effects of various methodologic strategies. Survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician. 2008;54:1424–30. [PMC free article] [PubMed] [Google Scholar]