Abstract
Objective
To investigate the relieving effect on interface pressure of an alternate sitting protocol involving a sitting posture that reduces ischial support.
Design
Repeated measures in 2 protocols on 3 groups of subjects.
Setting
Laboratory.
Participants
Twenty able-bodied persons, 20 persons with paraplegia, and 20 persons with tetraplegia.
Interventions
Two 1-hour protocols were used: alternate and normal plus pushup. In the alternate protocol, sitting posture was alternated every 10 minutes between normal (sitting upright with ischial support) and with partially removed ischial support (WO-BPS) postures; in the normal plus pushup protocol, sitting was in normal posture with pushups (lifting the subject off the seat) performed every 20 minutes.
Main Outcome Measure
Interface pressure on seat and backrest.
Results
In WO-BPS posture, the concentrated interface pressure observed around the ischia in normal posture was significantly repositioned to the thighs. By cyclically repositioning the interface pressure, the alternate protocol was superior to the normal plus pushup protocol in terms of a significantly lower average interface pressure over the buttocks.
Conclusions
A sitting protocol periodically reducing the ischial support helps lower the sitting load on the buttocks, especially the area close to ischial tuberosities.
Keywords: Pressure ulcer, Rehabilitation, Spinal cord injuries, Wheelchairs
In the united states, nearly 50% of the 1.4 million people1–5 who rely on wheelchairs for mobility develop serious tissue breakdown at pressure points such as the ischium and greater trochanter because of prolonged sitting without proper pressure relief.6–10 The optimal treatment strategy for pressure ulcers is prevention11; however, no prevention strategies have proven effective.12
Of the wheelchair population, patients with spinal cord injury (SCI) are among the most susceptible to pressure ulcer formation because of intrinsic physiologic derangement,10 with a reduced vascular response to loading, reduced muscular tone, progressive loss of muscle bulk, and impaired sensory biofeedback systems.8,10
A number of risk factors have been cited for pressure ulcer formation in which pressure concentrated over bony prominences9,13,14 is thought to be the single most important etiologic factor. Prolonged high pressure results in local tissue ischemia and leads to tissue necrosis,4,15–17 which is associated with local perfusion failure of nutritive capillaries. Furthermore, sustained elevated pressure leads to impaired lymphatic circulation and hypoperfusion of the compressed tissue, resulting in an accumulation of toxic intracellular materials.18 Short-term loading produces elastic deformation and rapid elastic recovery, whereas long-term loading results in marked creep and requires significant time for complete tissue recovery. Soft tissues were found to be more tolerant to cyclic loading as compared with static loading.19
Because treatment of established pressure ulcers is extremely difficult and costly, the ideal solution is prevention.20 Current prevention strategies emphasize intermittent relief of interface pressure, such as performing pushups every 20 minutes,1,21 which has proven useful in preventing or ameliorating the symptoms of pressure ulcer.17,22,23 However, various factors limit compliance with these regimens. Merbitz et al24 found that only 57% of inpatients develop and maintain adequate pressure-relief behaviors, and Fisher and Patterson25 reported that one third of the subjects are not compliant.
To facilitate intermittent pressure relief, various seating designs have been developed to provide pressure relief during prolonged wheelchair sitting. Static seat cushions of various materials are the most common options; however, because these cushions are static designs, pressure redistribution is only momentarily accomplished because progressive loss of this effect occurs from compression and distortion of the seating material.26 Without dynamic pressure redistribution, these static cushions, when loaded to the “dense region,”27 eventually lose the ability to reduce the sitting load; therefore, the excessive load on soft tissue remains largely unrelieved. Dynamic cushions redistribute interface pressure through automatic cyclical inflation and deflation of the seat cushion. However, there is a lack of solid scientific research validating their efficacy. Additional approaches to pressure relief are with more expensive tilt and recline systems, but several drawbacks limited their clinical application. Tilt and recline systems are intended for powered wheelchairs, which make up less than 10% of all wheelchairs. Moreover, the reclined position, although it provides pressure relief,28 removes users from a functional position, preventing normal daily activities. Furthermore, because these systems lack sensory feedback mechanisms, a regular change in posture is dependent again on user compliance. Therefore, it calls for an automatic pressure-reliving seating system that does periodic pressure relief and, at the same time, does not remove the user from a functional sitting position.
The purpose of this study was to evaluate an alternate seating system for its pressure redistribution effect in areas susceptible to pressure ulcers (ie, in and around the area of ischial tuberosities). Specifically, the alternate sitting protocol was compared for its interface pressure distribution with that of a regular sitting protocol together with performing pressure-relief pushups. An alternate protocol was defined as sitting alternately between a normal posture (sitting upright with ischial support) and an author-defined sitting upright with reduced ischial support and with an enhanced lumbar support posture (WO-BPS). The control protocol, a normal plus pushup protocol, was characterized by sitting in the normal posture and performing the clinically recommended pressure-relief pushup routine.
The hypotheses were as follows: (1) when the back part of the seat is tilted down and lumbar support is included, pressure on the ischial tuberosities will be reduced and shifted to the thighs and the back, and (2) sitting with periodically reduced ischial support (alternate protocol) will redistribute the contact pressure in a cyclic pattern, which will reduce the buttocks’ exposure to high interface pressure more than a usual sitting plus pushups (normal plus pushup), in terms of a significantly lower average buttock-seat contact pressure throughout the sitting trial.
METHODS
Participants
Twenty male subjects with paraplegia (age, 34.8±6.8y; weight, 87.2±18.5kg; height, 180.0±7.6cm; body mass index [BMI], 27.0±6.0kg/m2) with injury level lower than T4, 20 subjects with tetraplegia (15 men, 5 women; age, 36.5±10.0y; weight, 81.8±16.1kg; height, 176.9±9.2cm; BMI, 26.4±6.0kg/m2), and 20 able-bodied subjects (10 men, 10 women; age, 39.3±14.8y; weight, 71.3±20.2kg; height, 169.9±12.8cm; BMI, 24.4±4.6kg/m2) with no history of neuromuscular disorders as controls were tested. Written informed consent following the guidelines of the institutional review board of Northwestern University was obtained before experiment. The inclusion criteria for the paraplegia group were those people who were able to independently do pushups for pressure relief. People with degenerative disorders of the spine and with histories of injury or surgery of the pelvis, hip joint, and thigh, or with hip contractures were excluded. Also excluded were those with severe pain, spasm, and psychologic concerns preventing proper cooperation.
Wheelchair and the Alternate Seating System
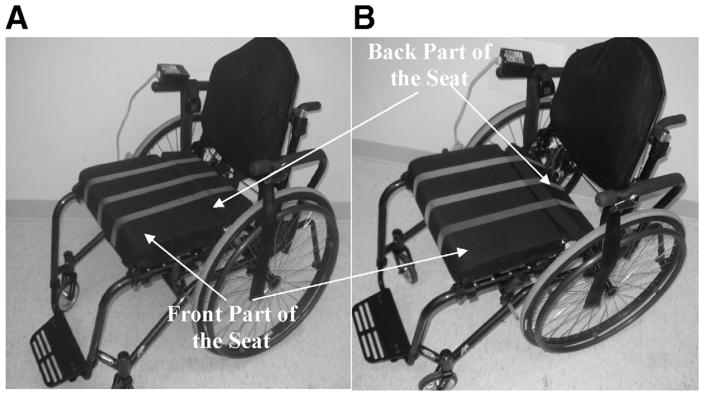
A wheelchair equipped with an alternate seating system was used for all tests. Shown in figure 1, the alternate seating system consisted of a split seat and a backrest with an enhanced lumbar support. The split seat had a movable back part of the seat that could be tilted downward (20°) to reduce the contact between the user’s buttocks and the seat. The backrest hosted an inflatable air pouch as an adjustable lumbar support. The air pouch had a size of 215.9×117.5mm2 when deflated and had a maximal thickness of 40mm when inflated. A customized system with a microprocessora was used to precisely regulate the tilting of the back part of the seat and the inflation and deflation of the lumbar air bladder via a motor and an air pump. The seating system can be set statically to a regular upright sitting posture (defined later in the text as a normal posture) and a sitting posture with the back part of the seat tilted down (defined later in the text as a WO-BPS posture). In addition, the seating system can also be set in a dynamic way to cyclically alter the sitting configuration of the wheelchair between the 2 standard sitting postures, normal and WO-BPS. In this way, the back part of the seat was cyclically tilted downward to reduce the sitting load exerted to the buttocks.
Fig 1.
The wheelchair equipped with alternate seating system used in this study. The alternate seating system consisted of a split seat and a backrest with an enhanced lumbar support. The split seat had a movable back part of the seat, which could be tilted downward (20°) to release the contact between the user’s ischia and the seat. The backrest hosted an inflatable air pouch as an adjustable lumbar support. The wheelchair is shown in the (A) normal and (B) WO-BPS configuration. Three light-color straps on the seat are for clearly showing the tilting of the back part of the seat.
Sitting Postures
Normal
Sitting upright with the back part of the seat at 0° (flat) and without enhanced lumbar support.
WO-BPS
Sitting upright with the back part of the seat tilted downward 20° and with enhanced lumbar support.
In the test, a proper sitting posture entailed sitting with the buttocks all the way back into the seat. In addition, the obtruded part of the lumbar support was adjusted so that it was in contact with the region around L4. In our previous study,29 we found that setting the lumbar support at this level and having the subject rest his/her back as much as he/she could helped to increase lumbar lordosis while not pushing the subject forward. The subject was asked to maintain the posture as consistently as possible during the 2 trials.
Sitting Protocols
The following 2 sitting protocols each lasted for 1 hour.
Alternate
The wheelchair configuration was periodically switched between normal and WO-BPS every 10 minutes during the 1-hour trial. The initial posture was randomized.
Normal plus pushup
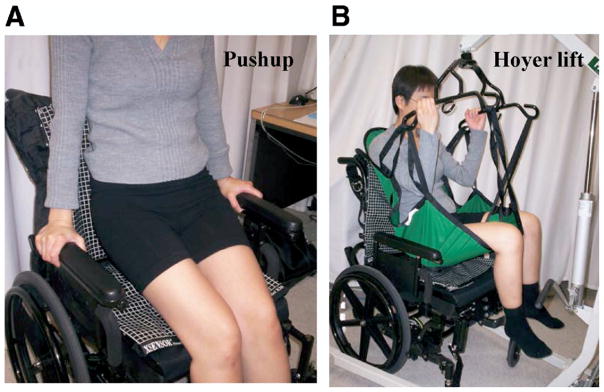
The wheelchair configuration remained at normal, and the subject did pushups every 20 minutes. A pushup entailed lifting the subject off the seat, either by themselves (fig 2A) or by using a Hoyer liftb (fig 2B) if the subject could not perform a pressure relief. Subjects in the control and paraplegia groups were asked to maintain each pushup as long as they can keep the body off the cushion.
Fig 2.
A demonstration of the pressure relief (ie, lifting the subject off the seat) used in the normal plus pushup protocol. (A) Arm pushups performed by participants in the paraplegic and control groups. (B) Pressure relief achieved by using a Hoyer lift for participants in the tetraplegic group.
Interface Pressure
A pressure-mapping devicec was used to record the interface pressure at 1Hz on backrest and the seat. For describing the spatial orientation of the interface pressure reading, a coordinate system was defined as the x axis pointing anteriorly, the y axis to the left, and the z axis to superior. The origin of this coordinate system for interface pressure reading on the seat pan was at the middle point of the rear edge.
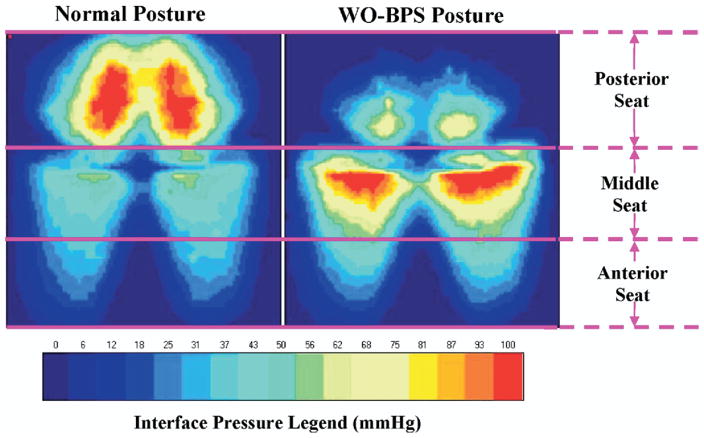
Data Processing
For evaluating the interface pressure distribution pattern, the interface pressure reading from the seat was grouped for 3 horizontal regions (anterior seat: anterior region; middle seat: middle region; posterior seat: posterior region). As shown in figure 3, the posterior portion of the seat cushion was the area between the buttock-thigh fold and the rear edge of the seat, where the back part of the seat was located. The area anterior to the buttock-thigh fold was bisected into the anterior portion and the middle portion of the seat cushion. From the interface pressure recordings, total contact area (TCA), average pressure, and peak interface pressure of both the backrest and the seat were obtained. TCA was calculated by multiplying 1.61cm2 (the area of a single cell of XSensorc device) with the number of cells that had pressure reading higher than a pressure threshold (5mmHg). The average pressure was calculated as the contact pressure averaged over the TCA XSensorc cells that had the pressure reading higher than the same pressure threshold used in TCA calculation. It was obtained as a measure for a general indication about the contact pressure applied to a specific body-seat interface or to the whole contact area. The reason to choose a threshold of pressure in TCA and average pressure calculation was to eliminate possible noise in the pressure data. The pressure threshold was 5mmHg. PPx and PPy (location of peak interface pressure in x and y directions) on seat and PPy and PPz (location of peak interface pressure in z direction) on backrest were calculated.
Fig 3.
The average interface pressure on the seat cushion for the Normal and WO-BPS postures. Results are from the average data of the 20 subjects in the control group. The method dividing the seat cushion for interface pressure data processing is also shown. The posterior portion of the seat cushion is from the rear edge of the seat to the buttock-thigh fold (posterior seat). The middle portion (middle seat) and the anterior portion (anterior seat) of the seat cushion are equal divisions of the area between the buttock-thigh fold to the front edge of the seat.
For the normal plus pushup protocol, the time of each pushup was recorded for both the paraplegic and tetraplegic groups. However, because most subjects in the tetraplegic group could not perform the arm pushup (see fig 2A) on their own but with the help of the Hoyer liftb by lifting (see fig 2B) them off the seat for a fixed 60 seconds, only pushup time from the paraplegic group was analyzed.
Statistical Analysis
For each group, a paired t test determined any significant differences in TCA, average pressure, peak interface pressures between the normal and WO-BPS sitting postures, and between the alternate and normal plus pushup trials. Besides, a 1-way analysis of variance was performed for each of these data to detect any group difference. All statistical tests were performed by using SAS softwared with the significance level as .05.
RESULTS
Participants
There was no age difference among the 3 groups (P>.05). The paraplegic group was significantly taller than the control group (P=.008) and had larger body weight (P=.027). However, no significant difference was found for BMI among the groups (P>.05).
Measurement in Normal and WO-BPS Postures
In figure 3, average interface pressure on the seat is shown for the 20 control subjects. In normal posture, the interface pressure was concentrated within the vicinity of ischial tuberosities (posterior portion of the seat cushion), with the thighs taking substantially less interface pressure. In WO-BPS posture, the concentrated interface pressure at ischial tuberosities was mostly shifted toward the thighs, and the middle part of the thighs took the most loads (middle portion of the seat cushion). A similar pattern for interface pressure was noted in all groups. The average parameters of interface pressure measured in normal and the WO-BPS postures are given in table 1.
Table 1.
Interface Pressure Parameters of the Seat in Normal and WO-BPS Postures for Control, Paraplegic, and Tetraplegic Subjects
| Group (n=20) | Sitting Postures | Whole Cushion | Anterior Seat | Middle Seat | Posterior Seat |
|---|---|---|---|---|---|
| Control | |||||
| TCA (cm2) | Normal | 1271.3±34.9 | 338.5±20.9 | 500.4±23.6 | 508.6±19.3 |
| WO-BPS | 1135.2±37.9* | 339.9±21.5 | 517.3±23.1* | 354.2±23.4* | |
| P | <.001 | >.05 | <.001 | <.001 | |
| Average pressure (mmHg) | Normal | 47.9±1.5 | 30.5±1.0 | 47.6±2.1 | 59.0±2.6 |
| WO-BPS | 49.9±1.7* | 34.2±1.2* | 65.7±2.5* | 41.2±2.6* | |
| P | .018 | <.001 | <.001 | <.001 | |
| Peak interface pressure (mmHg) | Normal | 176.1±6.8 | 74.9±10.1 | 137.1±11.7 | 172.5±6.8 |
| WO-BPS | 174.8±5.4 | 86.0±9.4* | 167.5±7.3* | 147.5±10.1* | |
| P | >.05 | <.001 | .001 | .005 | |
| PPx (cm) | Normal | 10.1±0.9 | NA | NA | NA |
| WO-BPS | 15.1±0.5* | ||||
| P | <.001 | ||||
| Paraplegic | |||||
| TCA (cm2) | Normal | 1363.5±47.9 | 401.3±35.8 | 559.9±18.7 | 453.2±26.5 |
| WO-BPS | 1278.6±51.6* | 405.3±34.5 | 581.7±20.2* | 347.8±26.6* | |
| P | <.001 | >.05 | <.001 | <.001 | |
| Average pressure (mmHg) | Normal | 57.6±2.2 | 30.7±2.0 | 49.5±3.1 | 88.9±4.2 |
| WO-BPS | 54.8±2.7* | 35.6±2.4* | 66.6±4.1* | 56.1±4.8* | |
| P | .006 | <.001 | <.001 | <.001 | |
| Peak interface pressure (mmHg) | Normal | 194.9±4.3 | 97.9±11.6 | 177.5±10.4 | 194.0±4.3 |
| WO-BPS | 194.2±4.4* | 120.6±12.1* | 188.9±6.4* | 177.3±10.6* | |
| P | .038 | <.001 | .033 | .043 | |
| PPx (cm) | Normal | 5.0±1.0 | NA | NA | NA |
| WO-BPS | 10.1±0.9* | ||||
| P | <.001 | ||||
| Tetraplegic | |||||
| TCA (cm2) | Normal | 1406.8±44.4 | 760.8±12.6 | 461.2±13.2 | 281.3±13.9 |
| WO-BPS | 1317.1±40.6* | 766.4±36.6 | 440.4±13.5* | 182.8±15.3* | |
| P | <.001 | >.05 | <.001 | <.001 | |
| Average pressure (mmHg) | Normal | 74.2±3.0 | 49.8±2.7 | 110.5±6.0 | 74.4±0.4 |
| WO-BPS | 74.5±2.2 | 68.3±3.3* | 111.7±4.0 | 41.8±2.2* | |
| P | >.05 | <.001 | >.05 | <.001 | |
| Peak interface pressure (mmHg) | Normal | 219.9±0.1 | 219.1±0.7 | 220.0±12.6 | 195.8±7.8 |
| WO-BPS | 219.4±0.6 | 220.0±0.0 | 219.7±0.3 | 96.3±8.7* | |
| P | >.05 | >.05 | >.05 | <.001 | |
| PPx (cm) | Normal | 4.9±0.4 | NA | NA | NA |
| WO-BPS | 11.1±0.3* | ||||
| P | <.001 | ||||
NOTE. Values are mean ± standard error (SE). The location of peak interface pressure along the posterior-anterior direction (PPx) is also given for the whole cushion. The P value concerns the “posture” effect between normal and WO-BPS postures.
Abbreviations: anterior seat, anterior portion of the seat cushion; middle seat, middle portion of the seat cushion; NA, not applicable; posterior seat, posterior portion of the seat cushion.
Statistical significance.
In normal posture, TCA on the seat was about 1300cm2 (see table 1), with no significant difference among groups. However, the distribution of the contact area differed among the groups. Among the 3 portions of the seat, the anterior portion of the seat cushion had the smallest contact area for both the control and paraplegic groups but the largest in the tetraplegic group. The contact area for the middle portion and the posterior portion of the seat cushion was virtually the same for control subjects (see table 1), but the middle portion of the seat cushion for subjects with SCI had larger contact area than the posterior portion of the seat cushion. Specifically, the tetraplegic group had the smallest contact on the posterior portion of the seat cushion among the 3 groups (P<.001). The average pressure on the whole seat differed significantly among the 3 groups (P<.001), with the highest average pressure from the tetraplegic group and the lowest from the control group. However, on the posterior portion of the seat cushion where the ischial tuberosities are usually positioned, the average pressure was the highest in the paraplegic group with a group average as 88.9±4.2mmHg and the lowest in controls as 59.0±2.6mmHg, almost 30mmHg lower. Peak interface pressure was also found to be 18.8mmHg higher in the paraplegic group and 43.8mmHg higher in the tetraplegic group than that in controls (see table 1).
In WO-BPS posture, TCA on the seat was about 1200cm2 (see table 1), with the tetraplegic group having the largest and the control the smallest (P=.019). For both SCI groups, the contact area on the posterior portion of the seat cushion was the smallest among the 3 seat portions. The average pressure in the tetraplegic group was significantly higher than that from the other groups by almost 20mmHg (P<.001). On the whole cushion, the tetraplegic group had the highest peak interface pressure, and the controls had the lowest (P<.001). On the posterior portion of the seat cushion, however, the tetraplegic group had the lowest peak interface pressure among the groups (P<.001).
Compared with the data for the normal posture, the TCA on the whole seat was significantly decreased in WO-BPS posture for all groups (P<.001). Looking more closely at the posterior portion of the seat cushion, a significant decrease in TCA, average pressure, and peak interface pressure was found in all groups. The TCA on the posterior portion of the seat cushion decreased by more than 30% (see table 1 for the absolute values of the data) in the control and tetraplegic groups and 24% for the paraplegic group (P<.001). Average pressure on the posterior portion of the seat cushion decreased from 28% to 42% (P<.001), with the largest decrease (42.8%) seen in the tetraplegic group (see table 1). The peak interface pressure also decreased significantly on the posterior portion of the seat cushion, with the largest decrease (50.7%) also seen in the tetraplegic group (see table 1). At the same time, the decrease of interface pressure parameters on the posterior portion of the seat cushion was accompanied by a substantial increase of them on the anterior portion and/or the middle portion of the seat cushion. The average pressure on the middle portion of the seat cushion increased significantly by 39.2% in the control group (P<.001) and by 36.2% in the paraplegic group (P<.001), whereas the increase of average pressure was noted mostly on the anterior portion of the seat cushion for the tetraplegic group (39.0%, P<.001) (see table 1). The peak interface pressure also increased significantly on the anterior portion and the middle portion of the seat cushion in the controls and paraplegic groups (range, 13.1% – 35.3%) but not in the tetraplegic group (P > .05) (see table 1).
With the posture changed to WO-BPS, the TCA on the backrest decreased in the paraplegic group (P=.035) but did not change in the control and tetraplegic groups (P>.05). At the same time, the increase of average pressure and the peak interface pressure were over 40% and 10%, respectively; all increases were statistically significant. The location of peak interface pressure was brought to a significantly more superior level for all groups.
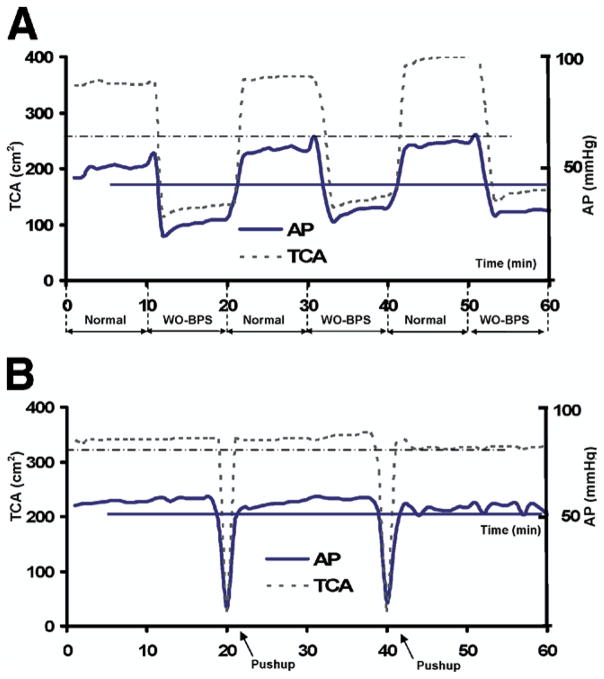
Measurement in the Alternate and Normal Plus Pushup Protocols
Figure 4 shows representative interface pressure continuously recorded from the ischial tuberosity for the alternate and normal plus pushup trials. In the alternate trial (see fig 4A), along with the cyclic change of the postures, the interface pressure (only average pressure and TCA was plotted for clarity) was changed accordingly. In the phases of normal posture, the average pressure and TCA were apparently at substantially higher levels than that in the WO-BPS phases. In the WO-BPS phases, the average pressure and TCA dropped dramatically to less than half in this specific example. By comparison, the average pressure and TCA experience little change during the entire normal plus pushup trial (see fig 4B), except when the subject was performing a pushup.
Fig 4.
Representative results of the alternate and normal plus pushup sitting protocols. Data are from 1 subject in the paraplegic group. (A) Average pressure (AP) and TCA on the posterior portion of the seat cushion during a trial of the alternate protocol. (B) Average pressure and TCA on the posterior portion of the seat cushion during a trial of the normal plus pushup protocol. NOTE. The horizontal lines indicate the average value over the entire 1-hour sitting trial.
Table 2 summarized the group average of interface pressure parameters, each obtained as the averaging value over the entire 1-hour trial for both protocols. The average buttock and thigh seat contact area on the whole seat and posterior portion of the seat cushion in the alternate protocol were significantly smaller than that in the normal plus pushup protocol. On the posterior portion of the seat cushion, the average pressure was significantly smaller by more than 15% in the alternate protocol than that in the normal plus pushup protocol for all groups (P<.001) (see table 2). At the same time, average pressure on the middle portion of the seat cushion was higher in the alternate protocol. On the anterior portion of the seat cushion, the average pressure in the SCI groups was both slightly (<9mmHg) but significantly (paraplegic group, P=.013; tetraplegic group, P<.001) higher in the alternate protocol, whereas there was no difference in the controls (P>.05) (see table 2). On the posterior portion of the seat cushion, peak interface pressures in the alternate protocol were lower in all 3 groups than those of the normal plus pushup protocol, and these decreases in the control and tetraplegic groups were significant (control group: 17.5mmHg decrease, P=.031; tetraplegic group: 71.1mmHg decrease, P<.001). The average pushup time ± standard error achieved by the paraplegic group was 49.0±2.8 seconds (n=20).
Table 2.
Average Interface Pressure Parameters of the Seat From the Alternate and Normal Plus Pushup Protocols for Control, Paraplegic, and Tetraplegic Subjects
| Group | Parameters | Whole Cushion | Anterior Seat | Middle Seat | Posterior Seat |
|---|---|---|---|---|---|
| Control (n=20) | TCA (cm2) | ||||
| Alternate | 1203.3±36.1 | 338.7±21.2 | 508.8±23.2 | 431.4±20.7 | |
| Normal plus pushup | 1287.8±45.0* | 394.6±22.7* | 456.3±23.9 | 479.3±21.6* | |
| P | .030 | .009 | >.05 | .048 | |
| Average pressure (mmHg) | |||||
| Alternate | 48.9±1.5 | 32.3±1.1 | 56.7±2.3 | 50.1±1.8 | |
| Normal plus pushup | 51.4±1.8 | 32.5±1.1 | 45.6±2.03 | 72.2±3.3* | |
| P | >.05 | >.05 | .001 | <.001 | |
| Peak interface pressure (mmHg) | |||||
| Alternate | 175.4±5.3 | 80.4±9.6 | 152.3±9.2 | 160.1±7.5 | |
| Normal plus pushup | 177.6±3.6 | 109.9±10.8* | 160.9±6.4 | 177.6±3.6* | |
| P | >.05 | .026 | >.05 | .031 | |
| Paraplegic (n=20) | TCA (cm2) | ||||
| Alternate | 1321.1±49.3 | 403.3±35.1 | 570.8±19.4 | 400.5±25.7 | |
| Normal plus pushup | 1356.3±49.3* | 409.3±34.7 | 537.4±20.4* | 456.0±25.3* | |
| P | .008 | >.05 | .002 | <.001 | |
| Average pressure (mmHg) | |||||
| Alternate | 56.2±2.4 | 33.2±2.2 | 58.1±3.4 | 72.5±4.3 | |
| Normal plus pushup | 57.5±2.5* | 31.8±2.0* | 48.7±3.3* | 88.6±5.2* | |
| P | .019 | .013 | <.001 | <.001 | |
| Peak interface pressure (mmHg) | |||||
| Alternate | 194.6±4.4 | 109.3±11.6 | 183.2±8.2 | 185.6±6.8 | |
| Normal plus pushup | 193.7±4.4* | 104.2±12.1 | 169.2±10.7* | 191.3±4.6 | |
| P | .046 | >.05 | .006 | >.05 | |
| Tetraplegic (n=20) | TCA (cm2) | ||||
| Alternate | 1361.9±41.9 | 763.6±37.8 | 450.8±13.1 | 232.0±13.9 | |
| Normal plus pushup | 1426.3±43.8* | 760.3±39.6 | 465.4±13.0* | 297.6±11.5* | |
| P | <.001 | >.05 | .002 | <.001 | |
| Average pressure (mmHg) | |||||
| Alternate | 74.3±2.5 | 59.0±2.9 | 111.1±4.6 | 58.1±2.8 | |
| Normal plus pushup | 71.9±3.1 | 50.1±3.1* | 109.3±6.9 | 76.9±4.9* | |
| P | >.05 | <.001 | >.05 | <.001 | |
| Peak interface pressure (mmHg) | |||||
| Alternate | 219.6±0.3 | 219.6±0.4 | 219.9±0.1 | 146.0±7.1 | |
| Normal plus pushup | 220.0±0.0 | 218.5±1.1 | 219.8±0.2 | 217.1±1.5* | |
| P | >.05 | >.05 | >.05 | <.001 | |
NOTE. Values are mean ± SE. Each interface pressure parameter is given as the averaging value over the entire 1-hour sitting trial. The P value concerns the difference between 2 protocols.
Abbreviations: see table 1.
Statistical significance.
DISCUSSION
This study measured interface pressure in 2 sitting postures (normal, WO-BPS) and during 2 sitting protocols (alternate, normal plus pushup) for able-bodied controls and subjects with paraplegia and tetraplegia. The effects on interface pressure distribution from these 2 different postures and 2 protocols were assessed. In general, the values of interface pressure in normal sitting posture, which is similar to the regular sitting posture used in other studies, were comparable to those previously reported.30–32
For WO-BPS posture, a distinct pattern of interface pressure distribution, which differed significantly from that of normal posture, was found in both controls and subjects with SCI, characterized by a significantly forward shift of the high interface pressure location from buttocks to the thighs. This forward shift of the concentrated interface pressure greatly decreased the sitting load applied to ischial tuberosities and repositioned a substantial amount of this load to the thighs. This decrease could be more than 40%, as seen in our tetraplegic group. At the same time, part of the sitting load was seen transferred to the backrest, as indicated by the substantial increase of average pressure and peak interface pressure there. Therefore, the WO-BPS posture repositioned the majority of the sitting load away from the area around ischial tuberosities and moves it to thighs and the backrest.
Most of the currently available alternate pressure-relief seats usually consist of cellular structures that provide small scale alternate interface support by cyclically shifting interface pressure among neighboring cells (eg, Airpulse PKe). The WO-BPS posture repositions high interface pressure from the ischia almost entirely to the thighs. This large-scale pressure repositioning has its own unique advantage in 2 senses. First, because it shifts most of the high interface pressure away from the entire ischial area to thighs, the unloading time for ischia can stay long. However, with the cellular design, because the interface pressure is shifted to neighboring units, still within the ischial area in which pressure ulcer risk is high, the unloading time for each cell should be limited to avoid overloading the neighboring area. Second, it has been reported that the load-bearing capacity of soft tissue in buttock-thigh area varies. Those on the thighs can sustain more than 80mmHg without injury, whereas that value for ischia is less than 40mmHg and for coccyx is even less, only 14mmHg.33 Therefore, shifting interface pressure to the area with less pressure ulcer risk and higher load-bearing capacity is the optimal solution.
In addition to shifting the load to thighs, part of the buttock sitting load was shifted to the backrest in WO-BPS posture. Our previously published29 data on able-bodied subjects showed that when the WO-BPS posture was used, the buttock load was repositioned to both thighs and the backrest. However, the increased load component in the superior-inferior direction on the backrest, which was the shear component in the lumbar area, was increased slightly by an average of 3.68±11.14N (P>.05) when subjects maintained upright posture and by 8.08±13.37N (P=.030) when subjects were fully relaxed when they were reclining on the backrest. Therefore, there should not be any significant concern about the shear load increase in the lumbar area.
The advantage of releasing buttock loading provided by WO-BPS posture can be dynamically extended into prolonged sitting by incorporating this posture into an alternate sitting protocol. Although in the current study only half of the time in the alternate protocol was dedicated to WO-BPS posture, the average results showed that the alternate protocol imposed significantly less sitting load on the buttock than that of using pushup routine. In the normal plus pushup protocol, pressure relief achieved by pushups was minimal and momentary. Bader34 reported that a full recovery of tissue perfusion could not be achieved within 2 minutes. His finding suggested that, to accomplish a full tissue perfusion recovery via pressure relief, the pressure relief must last long enough to allow the optimal perfusion level to be reached and maintained for a sufficient amount of time. It is apparent that the pushups, with an average pressure relieving time of 49 seconds, are far from enough for a full recovery of tissue perfusion. In the alternate protocol, however, the pressure-relieving time can last as long as the WO-BPS phase stays; therefore, by adjusting the duration of the WO-BPS phase, it is possible for the alternate protocol to provide sufficient time for a full perfusion recovery.
In a previously reported study,35 to evaluate the pressure-relieving effect of mattresses with pressure alternating function, a scale of Pressure Relief Index (PRI) was defined as the minutes per hour when the local interface pressure was below a certain level. The alternate protocol in our study is very flexible in the sense that the WO-BPS phases can be set up as long as the user prefers, although only the 50% configuration was reported in the current study. Therefore, PRI for our alternate device would be a variable depending on the configuration of the protocol.
In evaluating supporting devices, such as mattress and seat cushions, interface-pressure mapping is a good tool to visually quantify pressure load distribution. However, several factors prevent it from being the sole reliable index of the risk of tissue overload. Not only the absolute value of interface pressure varies from person to person but also the variation of the tissue composition around high-risk locations determines that the capability for soft tissues to sustain pressure load may vary accordingly. Therefore, the vulnerability to tissue breakdown can be a complicated issue in response to excessive or prolonged interface pressure. In this sense, using a universal value of interface pressure threshold to determine the risk of tissue breakdown helps little. It has been proposed by several groups36,37 that interface pressure should be used in conjunction with other measures, such as tissue perfusion, skin temperature, humidity, and so on. Further study on evaluating this alternate sitting protocol should be performed to collect other outcomes such as tissue perfusion to investigate how the reposition of superficial pressure load induces perfusion reactions in underlying soft tissues.
Study Limitations
There are limitations of this study. A limitation was the sex differences among the groups of subjects in which the paraplegic group included only men. Although we are not aware of any sitting pattern difference between women and men, the sex mismatch between the groups should be seriously considered. Another limitation was that our paraplegic participants were significantly taller (180.0±7.6cm vs 169.9±12.8cm, P=.008) and heavier (87.2±18.5kg vs 71.3±20.2kg, P=.027) than the able-bodied participants. Because the main part of our study was investigating the relative changes between postures and between sitting protocols, this part of findings should not be affected by the group difference on body build. However, for those findings related to group difference, we would advise readers take caution in interpreting the results of group comparison in this study.
CONCLUSIONS
The alternate seating system has significant effect in repositioning the concentrated high pressure from the ischial tuberosities to the thighs both in able-bodied and SCI populations. This interface-pressure repositioning mechanism showed its advantage in reducing buttock tissue sitting load, whereas it did not move the users away from their upright functioning positions. Because the interface pressure relief achieved by reducing ischial support when using WO-BPS posture can last as long as the user remains in this posture, it is expected that the alternate sitting mechanism evaluated in this study might be a better seating option for people sitting for a prolonged time.
Acknowledgments
We thank Susan Taylor for providing consultation regarding seating problems in SCI populations. We also thank Carolina Carmona and Ganapriya Venkatasubramanian for helping with data processing.
Supported by the National Institutes of Health (grant nos. R24 Rehab Network, R21 HD046844-01A1), Falk Medical Research Trust, and the Paralyzed Veterans Association (grant no. 2321-01).
Footnotes
BasicStamp; Parallax Inc, 599 Menlo Dr, Ste 100, Rocklin, CA 95765.
Hoyer hydraulic patient lift; Sunrise Medical, 7477 East Dry Creek Pkwy, Longmont, CO 80503.
XSensor Technology Corp, Ste 111, 319-2nd Ave SW, Calgary, AB T2P 0C5, Canada.
Version 9.1.3; SAS Institute Inc, 100 SAS Campus Dr, Cary, NC 27513.
Aquila Corp, 1309 Norplex Dr, Ste 6, La Crosse, WI 54601.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the author(s) or upon any organization with which the author(s) is/are associated.
References
- 1.Agency for Health Care Policy and Research. Clinical practice guideline no. 3. Rockville: U.S. Department of Health and Human Services, Public Health Service; 1992. Pressure ulcers in adults: prediction and prevention. [Google Scholar]
- 2.Allman RM. Epidemiology of pressure sores in different populations. Decubitus. 1989;2:30–3. [PubMed] [Google Scholar]
- 3.National Pressure Ulcer Advisory Panel. Pressure ulcers in America: prevalence, incidence and implications for the future. Reston: NPUAP; 2001. [DOI] [PubMed] [Google Scholar]
- 4.Dinsdale SM. Decubitus ulcers: role of pressure and friction in causation. Arch Phys Med Rehabil. 1974;55:147–52. [PubMed] [Google Scholar]
- 5.Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil. 1993;74:1172–7. [PubMed] [Google Scholar]
- 6.Barbenel JC. Pressure management. Prosthet Orthot Int. 1991;15:225–31. doi: 10.3109/03093649109164292. [DOI] [PubMed] [Google Scholar]
- 7.Henderson JL, Price SH, Brandstater ME, Mandac BR. Efficacy of three measures to relieve pressure in seated persons with spinal cord injury. Arch Phys Med Rehabil. 1994;75:535–9. [PubMed] [Google Scholar]
- 8.Patterson RP, Cranmer HH, Fisher SV, Engel RR. The impaired response of spinal cord injured individuals to repeated surface pressure loads. Arch Phys Med Rehabil. 1993;74:947–53. [PubMed] [Google Scholar]
- 9.Reuler JB, Cooney TG. The pressure sore: pathophysiology and principles of management. Ann Intern Med. 1981;94:661–6. doi: 10.7326/0003-4819-94-5-661. [DOI] [PubMed] [Google Scholar]
- 10.Salzberg CA, Byrne DW, Cayten CG, et al. Predicting and preventing pressure ulcers in adults with paralysis. Adv Wound Care. 1998;11:237–46. [PubMed] [Google Scholar]
- 11.Richardson GM, Gardner S, Frantz RA. Nursing assessment: impact on type and cost of interventions to prevent pressure ulcers. J Wound Ostomy Continence Nurs. 1998;25:273–80. doi: 10.1016/s1071-5754(98)90024-9. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Injury Prevention and Control. Injury fact book 2001–2002. Atlanta: Centers for Disease Control and Prevention; 2002. [Google Scholar]
- 13.Brienza DM, Karg PE, Geyer MJ, Kelsey S, Trefler E. The relationship between pressure ulcer incidence and buttock-seat cushion interface pressure in at-risk elderly wheelchair users. Arch Phys Med Rehabil. 2001;82:529–33. doi: 10.1053/apmr.2001.21854. [DOI] [PubMed] [Google Scholar]
- 14.Reddy NP, Krouskop TA, Newell PH., Jr Biomechanics of a lymphatic vessel. Blood Vessels. 1975;12:261–78. doi: 10.1159/000158062. [DOI] [PubMed] [Google Scholar]
- 15.Daniel RK, Priest DL, Wheatley DC. Etiologic factors in pressure sores: an experimental model. Arch Phys Med Rehabil. 1981;62:492–8. [PubMed] [Google Scholar]
- 16.Falanga V. Chronic wounds: pathophysiologic and experimental considerations. Prog Dermatol. 1992;26:1–8. doi: 10.1111/1523-1747.ep12472373. [DOI] [PubMed] [Google Scholar]
- 17.Kosiak M. Etiology of decubitus ulcers. Arch Phys Med Rehabil. 1961;42:19–29. [PubMed] [Google Scholar]
- 18.Knight SL, Taylor RP, Polliack AA, Bader DL. Establishing predictive indicators for the status of loaded soft tissues. J Appl Physiol. 2001;90:2231–7. doi: 10.1152/jappl.2001.90.6.2231. [DOI] [PubMed] [Google Scholar]
- 19.Edsberg LE, Mates RE, Baier RE, Lauren M. Mechanical characteristics of human skin subjected to static versus cyclic normal pressures. J Rehabil Res Dev. 1999;36:133–41. [PubMed] [Google Scholar]
- 20.Cervo FA, Cruz AC, Posillico JA. Pressure ulcers. Analysis of guidelines for treatment and management. Geriatrics. 2000;55:55–60. [PubMed] [Google Scholar]
- 21.Nixon V. Spinal cord injury: a guide to functional outcomes in physical therapy management. Rockville: Aspen; 1985. pp. 67–75. [Google Scholar]
- 22.Le KM, Madsen BL, Barth PW, Ksander GA, Angell JB, Vistnes LM. An in-depth look at pressure sores using monolithic silicon pressure sensors. Plast Reconstr Surg. 1984;74:745–56. doi: 10.1097/00006534-198412000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Russ GH, Motta GJ. Eliminating pressure: is less than 32mmHg enough for wound healing? Ostomy Wound Manage. 1991;34:60–3. [PubMed] [Google Scholar]
- 24.Merbitz CT, King RB, Bleiberg J, Grip JC. Wheelchair push-ups: measuring pressure relief frequency. Arch Phys Med Rehabil. 1985;66:433–8. [PubMed] [Google Scholar]
- 25.Fisher SV, Patterson P. Long term pressure recordings under the ischial tuberosities of tetraplegics. Paraplegia. 1983;21:99–106. doi: 10.1038/sc.1983.14. [DOI] [PubMed] [Google Scholar]
- 26.Drummond DS, Breed AL, Narechania R. Relationship of spine deformity and pelvic obliquity on sitting pressure distributions and decubitus ulceration. J Pediatr Orthop. 1985;5:396–402. doi: 10.1097/01241398-198507000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Ebe K, Griffin MJ. Factors affecting static seat cushion comfort. Ergonomics. 2001;44:901–21. doi: 10.1080/00140130110064685. [DOI] [PubMed] [Google Scholar]
- 28.Hobson DA. Comparative effects of posture on pressure and shear at the body seat interface. J Rehabil Res Dev. 1992;29:21–31. doi: 10.1682/jrrd.1992.10.0021. [DOI] [PubMed] [Google Scholar]
- 29.Makhsous M, Lin AF, Hendrix RW, Hepler M, Zhang LQ. Sitting with adjustable ischial and back supports: biomechanical changes. Spine. 2003;28:1113–21. doi: 10.1097/01.BRS.0000068243.63203.A8. [DOI] [PubMed] [Google Scholar]
- 30.Geyer MJ, Brienza DM, Karg P, Trefler E, Kelsey S. A randomized control trial to evaluate pressure-reducing seat cushions for elderly wheelchair users. Adv Skin Wound Care. 2001;14:120–9. doi: 10.1097/00129334-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Koo TK, Mak AF, Lee YL. Posture effect on seating interface biomechanics: comparison between two seating cushions. Arch Phys Med Rehabil. 1996;77:40–7. doi: 10.1016/s0003-9993(96)90218-x. [DOI] [PubMed] [Google Scholar]
- 32.Rosenthal MJ, Felton RM, Hileman DL, Lee M, Friedman M, Navach JH. A wheelchair cushion designed to redistribute sites of sitting pressure. Arch Phys Med Rehabil. 1996;77:278–82. doi: 10.1016/s0003-9993(96)90112-4. [DOI] [PubMed] [Google Scholar]
- 33.Bennett L, Kavner D, Lee BY, Trainor FS, Lewis JM. Skin blood flow in seated geriatric patients. Arch Phys Med Rehabil. 1981;62:392–8. [PubMed] [Google Scholar]
- 34.Bader DL. The recovery characteristics of soft tissues following repeated loading. J Rehabil Res Dev. 1990;27:141–50. doi: 10.1682/jrrd.1990.04.0141. [DOI] [PubMed] [Google Scholar]
- 35.Rithalia SV, Gonsalkorale M. Quantification of pressure relief using interface pressure and tissue perfusion in alternating pressure air mattresses. Arch Phys Med Rehabil. 2000;81:1364–9. doi: 10.1053/apmr.2000.9164. [DOI] [PubMed] [Google Scholar]
- 36.Jonsson A, Linden M, Lindgren M, Malmqvist LA, Backlund Y. Evaluation of antidecubitus mattresses. Med Biol Eng Comput. 2005;43:541–7. doi: 10.1007/BF02351025. [DOI] [PubMed] [Google Scholar]
- 37.Sachse RE, Fink SA, Klitzman B. Multimodality evaluation of pressure relief surfaces. Plast Reconstr Surg. 1998;102:2381–7. doi: 10.1097/00006534-199812000-00017. [DOI] [PubMed] [Google Scholar]