Abstract
The aim of the current investigation was to examine uni-morbid and co-occurring tobacco and marijuana use in relation to the negative emotional symptoms of anxiety and depression. Participants were 250 adult individuals (132 female; mage = 22.43, SD = 9.00), falling into one of four non-overlapping substance use categories: tobacco use only (n = 39), marijuana use only (n = 62), co-occurring tobacco and marijuana use (n = 82), and neither tobacco nor marijuana use (n = 67). Results revealed three key findings. First, tobacco-only using individuals reported significantly greater negative affectivity than any of the other groups. Second, tobacco-only users reported greater anxious arousal symptoms than either the marijuana or non-substance-using groups, but not the combined group. Third, tobacco-only users reported greater levels of depressive symptoms than either marijuana users or non-substance-users. These findings provide novel information about tobacco and marijuana use, and how these variables relate to the experience of general and specific types of negative emotional symptoms.
Keywords: Marijuana, Tobacco, Polysubstance, Negative Affect, Anxiety, Depression
There has been growing scientific interest in understanding the linkages between substance use disorders and anxiety and mood symptoms and disorders1,2. These efforts have been guided by the clinical and empirical recognition that anxiety/depressive symptoms and disorders often frequently co-occur with substance use disorders, and that there are clinically meaningful bi-directional associations between these factors3.
In terms of cigarette smoking (referred to as tobacco use from this point forward), greater rates of tobacco use are related to higher concurrent and prospective levels of anxiety symptoms (e.g., panic attacks4-9) and interoceptive-oriented fears (e.g., worry about bodily sensations10,11). Additionally, anxiety symptoms and disorders as well as fears of such symptoms (anxiety sensitivity) are related to poorer success in quitting smoking12-14. Depressive symptoms and disorders also are common among daily smokers. For example, over 30% of patients with current depression are daily smokers,15,16 and nearly 60% with a lifetime history of depression are current or past smokers17. Smokers, as compared to non-smokers, have significantly higher rates of lifetime depression18, especially those that are nicotine dependent19. In terms of depressive symptoms and disorders and difficulties with smoking cessation, depressive symptoms prior to smoking cessation treatment, as well as increases in such symptoms during treatment, possibly due to the removal of the stimulant effects of tobacco that might have previously aided in the reduction of depressive symptoms, are routinely significant predictors of relapse20-23.
There also has been increased study of possible associations between marijuana use and its disorders and anxiety and depressive symptoms and their disorders24. Although this body of scientific work is less well-developed than that focused on tobacco use, some intriguing findings have emerged in terms of anxiety and depression. Here, studies have found that both treatment-seeking and non-treatment seeking adults and adolescents meeting criteria for marijuana abuse or dependence generally have significantly higher rates of psychological symptoms and disorders relative to those not abusing or dependent on marijuana25-29. In terms of anxiety symptoms, specifically, Hathaway30 found that among weekly users of marijuana, approximately 40% reported having had at least one panic attack related to such use; these prevalence rates are noteworthy in light of lifetime rates of panic attacks among the general population of approximately 5%-8%31. Other work has found that a lifetime history of marijuana dependence is related to an increased risk of panic attacks, although such effects are not evident above and beyond tobacco use32,33. Additionally, marijuana use prior to a cessation attempt is associated with increased levels of anxiety post-cessation and post-cessation anxiety increases risk for marijuana relapse34. Scientific work on marijuana and depression, on the other hand, has historically been fueled by the clinical observation that regular marijuana users (e.g., daily or weekly basis) often report a ‘lack of motivation’ for completing day-to-day activities (e.g., going to school35). The depression-marijuana literature has inconsistently identified statistically significant relations between marijuana use and depressive symptoms and disorders36. However, the most recent work in this domain has indicated that the strength of such marijuana-depressive associations may be markedly attenuated after controlling for gender37,38.
Despite the possible, but not necessarily uniform, interconnection between negative mood states (e.g., anxiety, depression) and tobacco and marijuana use behavior, research in this domain is limited in a number of key respects. First, extant work has focused on the examination of one form of substance use (e.g., tobacco use) in relation to a particular type of negative emotional experience (e.g., depression). This limitation is problematic in terms of clarifying the unique and shared relations, as tobacco and marijuana use often co-occur at high rates. For example, marijuana is the most frequently used illicit drug among tobacco users39. Likewise, tobacco use often co-occurs among active marijuana users40. Due to these high rates of co-occurrence, it would be valuable to parse apart the linkages between tobacco and marijuana use by exploring uni-morbid and co-occurring patterns of such use in relation to negative mood states such as anxiety and depression. This type of test would inform efforts to understand how general or specific the association between smoking and marijuana use is to negative mood states, and whether such effects are addictive or synergistic.
A second limitation is that previous work has not consistently excluded for the presence of Axis I disorders when examining the linkages between these types of drug use and negative mood states (e.g.37,33). Although the inclusion of Axis I disorders often increases the chance of accessing a full range of upper-end negative affective symptoms, it cannot allow for an examination as to whether such relations exist in a psychological state ‘free’ from existing psychopathology. This type of test would clarify how robust the linkages are between tobacco and marijuana use, in singular and co-occurring forms, in terms of negative mood states. This type of information also is central to informing efforts to understand the etiological role of marijuana and tobacco use in the experience of negative mood vulnerability.
Together, the overarching aim of the current investigation was to examine uni-morbid and co-occurring tobacco and marijuana use in relation to the negative emotional symptoms of anxiety and depression. Participants were adult individuals recruited through the community, falling into one of four non-overlapping categories: tobacco use only, marijuana use only, co-occurring tobacco and marijuana use, and neither tobacco nor marijuana use. The dependent variables included three affective variables: global levels of negative affect, anxious arousal symptoms (symptoms of anxiety that do not overlap with depressive states), and anhedonic depressive symptoms (symptoms of depression that do not overlap with anxiety states41). Importantly, the inclusion of these three affect-based dependent variables allowed for empirical evaluation of the general and specific features of negative affect symptoms in terms of the three groups (e.g., whether certain effects were specific to non-overlapping symptom features of anxiety or depressive states). It was expected that while tobacco and marijuana use would each be related to greater negative affect, anxious arousal, and anhedonic depression, their combination (co-occurring cases) would be related to the greatest indices of concurrent symptoms across the dependent measures. This hypothesis is based on the idea that although each of these types of substance use have been related to greater negative mood, including both anxiety and depression, individuals using both of these substances in combination would likely increase their chances of being exposed to a greater range of emotional vulnerability. Given some work has found that the effects of tobacco use are evident above and beyond marijuana use, but not vice versa, in terms of anxious arousal symptoms33, it also was hypothesized that the singular effects for cigarette use would be greater than those found for singular marijuana use.
Method
Participants
The total sample consisted of 250 adult individuals (132 female; mage = 22.43, SD = 9.00) who were recruited from the greater Burlington, Vermont community (see Procedure for more details about the study recruitment methodology). Generally consistent with the racial distribution of Vermont42, 91.6% of the total sample was Caucasian, 2.0% identified as Black, 0.8% as Asian, 0.4% as Native American, 0.8% as Hispanic, 1.2% as Biracial, and 0.8% identified themselves as “other”, while 2.4% of participants chose not to specify their race. This sample was made up of four non-overlapping groups: (1) current tobacco users who did not report marijuana use within the past 30 days (“tobacco-only”; n = 39; 17 female; mage = 33.31, SD = 14.16), (2) current marijuana users (use within past 30 days) who reported no current tobacco use (“marijuana-only”; n = 62; 39 female; mage = 18.76, SD = 1.07), (3) individuals who reported both current marijuana and tobacco use (“combined-users”; n = 82; 31 female; mage = 22.37, SD = 7.73), and (4) individuals who reported neither current tobacco or marijuana use (“non-substance-users”; n = 67; 45 female; mage = 19.57, SD = 4.96). Current alcohol use was allowed in any of the 4 groups because of its high rate of co-occurrence across each group (see Results section for a description of alcohol use across groups).
Among the tobacco-only group, smokers reported using an average of 18.03 cigarettes daily. In addition, approximately 72.2% of the tobacco-only group reported at least some alcohol use, averaging 3 or 4 drinks approximately 2-4 times monthly. Additionally, participants in this group scored an average of 7.56 on the Alcohol Use Disorders Identification Test (SD = 8.02) (AUDIT43), with 41.7% of participants in the tobacco group meeting criteria for at least moderate alcohol problems (indexed by a score of 8 or greater on the AUDIT).
The marijuana-only group reported using marijuana weekly, on average, with 27.4% of the group meeting DSM-IV criteria44 for marijuana abuse, and 22.6% meeting DSM-IV criteria for marijuana dependence. Participants reported initiating regular marijuana use at an average age of 15.30. Regarding alcohol use, all participants in the marijuana-only group reported at least some use, averaging 5 or 6 drinks approximately 2-3 times weekly. Regarding alcohol use problems, participants in this group scored an average of 11.70 on the AUDIT (SD = 5.50), with 82.0% of participants in the marijuana group meeting criteria for at least moderate alcohol problems.
Among the combined tobacco and marijuana group, participants smoked an average of 13.51 cigarettes daily, with marijuana being used a couple times per week. Regarding DSM-IV marijuana disorders, 32.9% of individuals in the combined group abused marijuana, with an additional 32.9% of participants reporting dependence on marijuana. Individuals in this group reported regular marijuana use by 15.27 years of age. At least some alcohol use within this combined group was reported by 97.5% of participants, averaging 5 or 6 drinks approximately 2-3 times weekly. Regarding alcohol use problems, participants in the combined group scored an average of 12.11 on the AUDIT (SD = 5.53), with 81.2% of participants meeting criteria for at least moderate alcohol problems.
Finally, among the group reporting no tobacco or marijuana use, 86.6% reported at least some alcohol use, averaging 3 or 4 drinks approximately 2-4 times monthly. In terms of alcohol use problems, participants scored an average of 6.79 on the AUDIT (SD = 5.39), with 38.8% of participants meeting criteria for at least moderate alcohol problems.
Exclusionary criteria for the investigation included: (1) current axis I psychopathology (with the exception of tobacco, marijuana, or alcohol abuse and dependence); (2) current use of psychotropic medication; (3) current suicidality or homicidality; (4) current or past chronic cardiopulmonary illness (e.g., chronic obstructive pulmonary disease; severe asthma); (5) current, acute respiratory illness (e.g., bronchitis); (6) seizure disorder, cardiac dysfunction, or other serious medical illness (e.g., history of seizures, emphysema); (7) pregnancy (specific to females); and (8) limited mental competency, inability to give informed, written consent. Overall, these screening criteria were employed to increase the study's internal validity (e.g., differences between groups are not alternatively explained by co-occurring psychopathology or medical illness45).
Measures
Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-N/P46)
The SCID-N/P was administered as a screener in order to rule out psychopathology and assess for current suicidal ideation (see exclusionary criteria). Although the SCID-N/P has high rates of reliability in terms of inter-rater agreement46, we did not compute such reliability ratings in the current study because just the screening aspect of the measure was employed.
Smoking History Questionnaire (SHQ47)
The SHQ is a self-report questionnaire used to assess smoking history and pattern. The SHQ includes items pertaining to smoking rate, age of onset of smoking initiation, and years of being a daily smoker, and number of serious quit attempts made. The SHQ has been successfully used in previous studies as a measure of smoking history (e.g., onset of regular smoking), pattern (e.g., number of cigarettes consumed per day), past quit attempts, and problematic symptoms experienced during quitting47,48.
Marijuana Smoking History Questionnaire (MSHQ49)
The MSHQ is a self-report instrument that includes items pertaining to marijuana smoking rate (lifetime and past 30 days), quantity of marijuana smoked, age of onset at initiation, years of being a regular marijuana smoker, and other descriptive information (e.g., number of attempts to discontinue using marijuana). The MSHQ has been employed successfully in the past (e.g.50). In the present investigation, the MSHQ was used to provide a descriptive analysis of the marijuana smoking history characteristics of the sample.
Alcohol Use Disorders Identification Test (AUDIT43)
The AUDIT is a 10-item self-report screening measure developed by the World Health Organization to identify individuals with alcohol problems43. There is a large body of literature attesting to the reliability and validity of the AUDIT51. In the present study, the AUDIT was utilized to assess the frequency and quantity of alcohol use. Additionally, the AUDIT total score was utilized to identify current alcohol problems.
Positive Affect Negative Affect Scale (PANAS52)
The PANAS is a 20-item measure in which respondents indicate, on a 5-point Likert-type scale (1 = “very slightly or not at all” to 5 = “extremely”), the extent to which they generally feel different feelings and emotions (e.g., “Hostile”). The PANAS is a well-established mood measure commonly used in psychopathology research52 and factor analysis indicates that the PANAS assesses the global dimension of negative affect (PANAS-NA). In the current study, the negative affect subscale of the PANAS was employed.
Mood and Anxiety Symptom Questionnaire (MASQ41)
The MASQ is a comprehensive measure of affective symptoms41. The MASQ-AA as well as the MASQ-AD subscales have shown high levels of internal consistency (range of alpha coefficients: .86 to .90 and .90 to .93 respectively). Participants indicate how much they have experienced each symptom from 1 (“not at all”) to 5 (“extremely”). In the present study, the MASQ-AA and MASQ-AD subscales were used to index anxiety and depressive symptoms, respectively. These scales measure the non-overlapping features of anxiety and depressive symptoms (i.e., the anxiety symptoms that do not overlap with depressive states and the depressive symptoms that do not overlap with anxiety states41).
Procedure
The present data are derived from a larger investigation. The current data have not been reported previously, and therefore, are novel (i.e., make a unique contribution). Participants were recruited from the Burlington, VT community for participation in a laboratory study on “emotion” via placement of specifically-tailored (i.e., “Are you a [cigarette] smoker?) study flyers throughout various community settings and posting of printed advertisements in local newspapers. Interested participants who contacted the research team about the study were given a detailed description of the investigation via telephone and scheduled for an initial laboratory visit. Upon arrival to the laboratory, participants provided verbal and written informed consent and were administered the SCID-I/NP-screener46 by trained interviewers to assess for current or past psychotic-spectrum symptoms. If deemed eligible, participants then completed a battery of self-report measures. At the completion of the study, participants were debriefed and compensated $20 for their time and effort. The procedures followed in the present investigation were in accordance with the ethical standards of the Institutional Review Board (IRB) at the University of Vermont.
Results
Three separate Analyses of Variance (ANOVA) were conducted to determine if differences existed in the use of common substances between substance use groups. Here, differences in alcohol use volume (frequency by quantity) were examined between all four groups using a tetratomously coded substance use grouping variable (1 = tobacco use only, 2 = marijuana use only, 3 = tobacco and marijuana use, and 4 = neither tobacco nor marijuana use). Differences in tobacco use frequency were examined between the tobacco use only and the combined tobacco and marijuana use group. Finally, differences in marijuana use frequency were examined between the marijuana use only group and the combined group. For all ANOVA procedures that did not meet the criterion of homogeneity of variances, a Brown-Forsythe correction was used. In addition, if the ANOVA procedures were significant, then, planned comparisons were used.
In terms of alcohol use volume, group differences were found (F(3,242) = 19.35, p < .01, η2 = .20). Specifically, the tobacco-only group and the group that used neither tobacco nor alcohol, each used significantly less alcohol than either the marijuana-only or combined groups. No significant differences existed between the tobacco-only and the non-substance using group, or between the marijuana-only and combined group. In terms of tobacco use, the tobacco-only group smoked significantly more than the combined group (F(1,120) = 9.44, p < .01, η2 = .07). The opposite pattern was observed for marijuana use, with the combined group reporting significantly greater marijuana use than the marijuana-only group (F(1,143) = 9.77, p < .01, η2 = .06).
Three separate ANOVAs were conducted to determine the relations between the tetratomously coded substance use grouping variable (see above) and (1) negative affectivity, (2) anxious arousal, and (3) anhedonic depression. In terms of negative affectivity, individuals using only tobacco reported significantly greater negative affectivity than any of the other 3 groups (Brown-Forsythe(3,110.02) = 4.09, p < .01, η2 = .06), with no other differences observed (see Figure 1).
Figure 1.
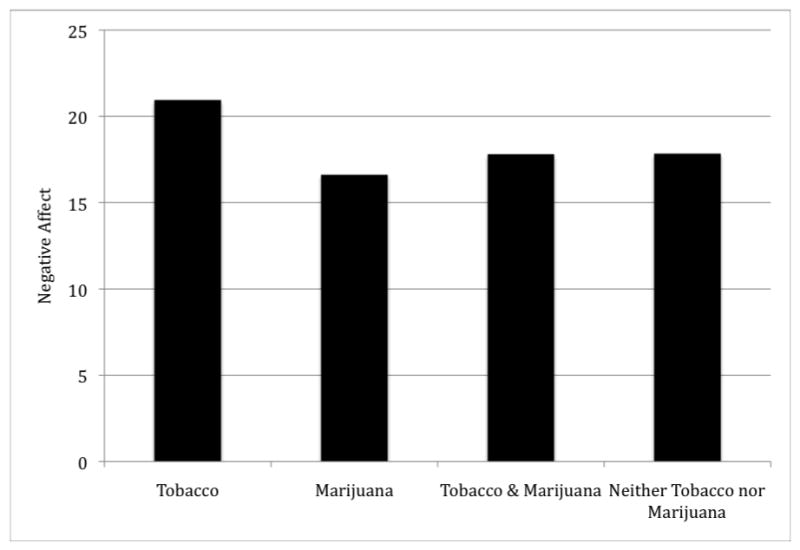
Mean levels of negative affectivity across groups.
Regarding anxious arousal, tobacco-only users reported greater anxious arousal symptoms than either the marijuana or non-substance-using groups, and the combined tobacco and marijuana users reporting significantly more anxiety symptoms than the marijuana-only users and non-substance-users (Brown-Forsythe(3,102.74) = 4.93, p < .01, η2 = .07). No differences existed between tobacco-only users and combined substance users, or between marijuana users and non-substance-users (see Figure 2). In terms of anhedonic depression symptoms, individuals using only tobacco reported greater levels of depressive symptoms than either marijuana users or non-substance-users (Brown-Forsythe(3,159.80) = 2.72, p < .05, η2 = .04). No other significant group differences were observed (see Figure 3). Please see Footnote 1.
Figure 2.
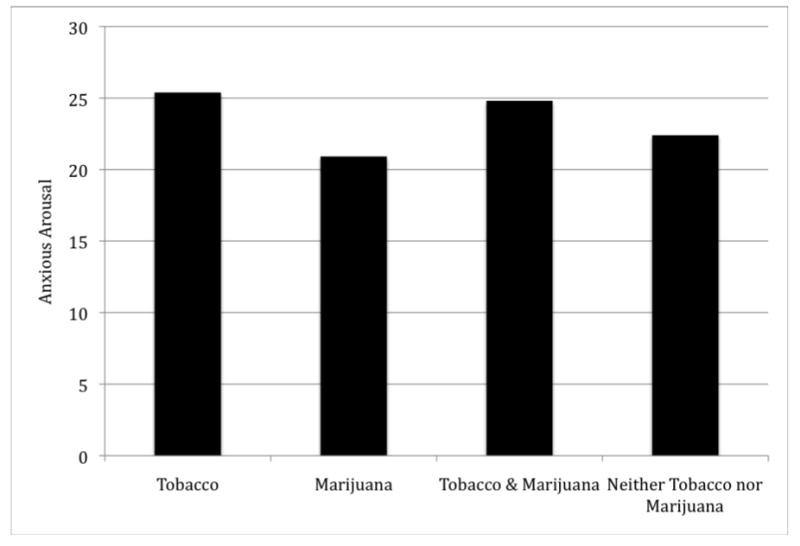
Mean levels of anxious arousal symptoms across groups.
Figure 3.
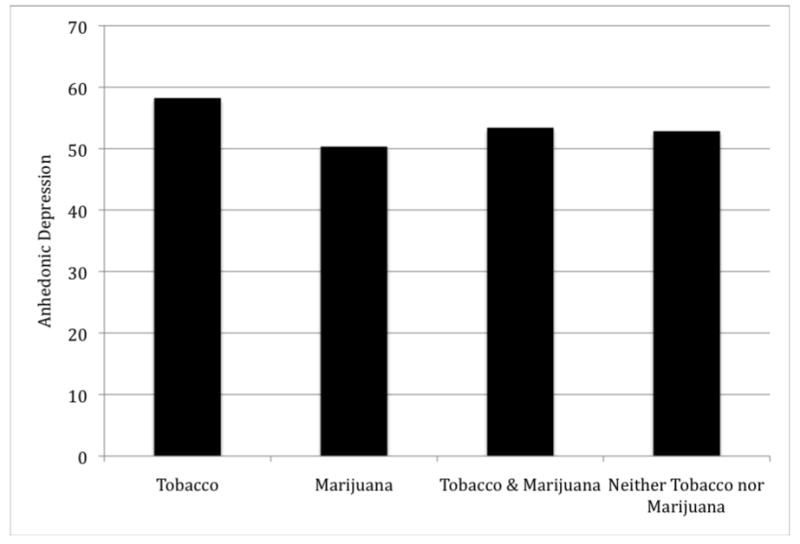
Mean levels of anhedonic depression symptoms across groups.
Discussion
Although there has been a documented interconnection between negative mood states (e.g., anxiety, depression) and tobacco and marijuana use behavior, tests evaluating uni-morbid and co-occurring patterns of such use in relation to negative mood states is non-existent. To fill this gap in the empirical literature, the current study examined uni-morbid and co-occurring tobacco and marijuana use in relation to the negative emotional symptoms of anxiety and depression.
Results were only partially consistent with original prediction, but revealed novel empirical insight into the nature of tobacco and marijuana use in terms of negative affective symptoms among adults. Three key observations were made. First, tobacco only using individuals reported significantly greater negative affectivity than any of the other groups. These data suggest that there is an overall higher global level of negative affectivity experienced by individuals just using tobacco when compared to non-users as well as uni-morbid and co-occurring marijuana users. Second, regarding anxious arousal, tobacco-only users reported greater anxious arousal symptoms than either the marijuana or non-substance-using groups, but not the combined group. Also, the combined tobacco and marijuana users reported significantly more anxious arousal symptoms than the marijuana-only users and non-substance-users. These data suggest that the experience of anxiety symptoms that do not overlap with depressive symptoms is closely tied to tobacco use whether in the uni-morbid tobacco group or the co-occurring tobacco and marijuana group. These results are in accordance with past work documenting a robust relationship between tobacco use and anxiety and its disorders4,7. Third, individuals using only tobacco reported greater levels of depressive symptoms than either marijuana users or non-substance-users. No other significant group differences were observed within the present investigation. These findings suggest that anhedonic depressive symptoms, similar to the findings with anxious arousal, are closely linked to tobacco use - whether in a uni-morbid or co-occurring pattern of current use. Overall, the present findings suggest that there is a striking relationship between tobacco use, especially uni-morbid use, and both global and specific types of negative affect symptoms.
Although not the primary aim of the current study, it is noteworthy that analyses of co-occurring substance use rates revealed that tobacco use was greater among the tobacco-only group as compared to the combined group. This finding is possibly clinically important, as higher rates of tobacco use are associated with greater risk for anxiety and possibly related negative emotional symptoms53. Interestingly, an opposite pattern was evident for marijuana use, with the combined tobacco-marijuana group reporting greater marijuana use frequency than the marijuana only group. Thus, co-occurring marijuana and tobacco use is related to greater levels of marijuana use, but not tobacco use, when compared to uni-morbid use of these substances. In terms of alcohol use, the groups that included marijuana users (marijuana use only and the combined substance group) reported greater alcohol use consumption than the tobacco and non-using groups. These data suggest that co-occurrence of one substance is not universally applicable to other drugs (e.g., alcohol). More specifically, the findings indicate that uni- or co-occurring marijuana use is related to greater rates of current alcohol use relative to uni-morbid tobacco users or non-users. Overall, the present data empirically underscore the importance of assessing for polysubstance use among tobacco and marijuana using samples, and document that the nature of co-occurring patterns of use are not necessarily straightforward and may vary by drug use type.
There are a number of interpretative caveats and future directions that warrant comment. First, the present study employed a cross-sectional design, and therefore, does not permit inference about the temporal stability or possible causal direction of the findings. One possible area of future exploration would be to utilize a prospective design to explore individual changes in negative emotional states over time, and whether changes in group membership similarly correspond to changes in such emotional states. For example, if a combined marijuana-tobacco user later stops using marijuana and becomes a tobacco-only user, does their negative emotional symptomatology increase? Second, this sample consisted of relatively homogeneous participants in terms of age and ethnicity. Future work might strive to replicate and extend the current findings among more heterogeneous populations. Third, the present investigation utilized established psychometrically-sound self-report instruments as the principal assessment strategy. Future work might build upon the present findings and incorporate multi-method approaches. Fourth, the sample was an intentionally psychiatrically healthy sample for the purpose of an internally valid test of differences in substance use behavior. Based upon these findings, future study could thus explore the generalizability of these findings among clinical samples and among a representative sample from the more general population. Finally, aside from tobacco, alcohol, and marijuana, other forms of substance use were not assessed in the current sample. Future work may benefit by more comprehensively assessing other types of substance use in addition to those examined in the present investigation.
Overall, the present investigation examined uni-morbid and co-occurring cigarette smoking and marijuana use in relation to negative emotional symptoms. Findings generally indicated an interesting set of findings, namely, that tobacco-only users reported the greatest emotional distress as compared to other patterns of uni-morbid or co-occurring substance use. These findings provide novel information about the interrelation between tobacco and marijuana use and how such relations pertain to negative emotional symptoms frequently observed among these drug using populations.
Acknowledgments
This work was supported by the Department of Veterans Affairs Health Services Research and Development Service funds. This work was supported by National Institute on Mental Health research grant (1 R01 MH076629-01) awarded to Dr. Zvolensky. The views expressed here are the authors' and do not necessarily represent those of the Department of Veterans Affairs.
Footnotes
Analyses were re-run in a follow-up fashion with the inclusion of gender as a covariate using an Analysis of Covariance (ANCOVA). All findings remained statistically significant (p < .05).
Contributor Information
Marcel O. Bonn-Miller, Center for Health Care Evaluation, Veterans Affairs, Palo Alto Health Care System and Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine
Michael J. Zvolensky, The University of Vermont
Kirsten A. Johnson, The University of Vermont
References
- 1.Morissette SB, Tull MT, Gulliver SB, Kamholz BW, Zimering RT. Anxiety, anxiety disorders, tobacco use, and nicotine: A critical review of interrelationships. Psychol Bull. 2007;133:245–72. doi: 10.1037/0033-2909.133.2.245. [DOI] [PubMed] [Google Scholar]
- 2.Ziedonis D, Hitsman B, Beckham J, Zvolensky MJ, Adler L, Audrain-McGovern J, Breslau N, Brown RA, George T, Williams J, Calhoun P, Riley W. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health (NIMH) Report. Nicotine Tob Res. 2008;10:1691–1715. doi: 10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]
- 3.Kalman D, Morissette SB, George TP. Co-morbidity of smoking and psychiatric and substance use disorders. Am J Addict. 2005;14:106–23. doi: 10.1080/10550490590924728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abrams K, Zvolensky MJ, Dorflinger L, Galatis A, Blank M, Eissenberg T. Fear reactivity to bodily sensations among heavy smokers and non-smokers. Exp Clin Psychopharmacol. 2008;16:230–9. doi: 10.1037/1064-1297.16.3.230. [DOI] [PubMed] [Google Scholar]
- 5.Breslau N, Klein DF. Smoking and panic attacks: An epidemiologic investigation. Arch Gen Psychiatry. 1999;56:1141–7. doi: 10.1001/archpsyc.56.12.1141. [DOI] [PubMed] [Google Scholar]
- 6.Breslau N, Novak SP, Kessler RC. Daily smoking and the subsequent onset of psychiatric disorders. Psychol Med. 2004;34:323–33. doi: 10.1017/s0033291703008869. [DOI] [PubMed] [Google Scholar]
- 7.Goodwin RD, Lewinsohn PM, Seeley JR. Cigarette smoking and panic attacks among young adults in the community: The role of parental smoking and anxiety disorders. Biol Psychiatry. 2005;58:686–93. doi: 10.1016/j.biopsych.2005.04.042. [DOI] [PubMed] [Google Scholar]
- 8.Isensee B, Wittchen HU, Stein MB, Höfler M, Lieb R. Smoking increases the risk of panic: Findings from a prospective community study. Arch Gen Psychiatry. 2003;60:692–700. doi: 10.1001/archpsyc.60.7.692. [DOI] [PubMed] [Google Scholar]
- 9.Johnson JG, Cohen P, Pine DS, Klein DF, Kasen S, Brook JS. Association between cigarette smoking and anxiety disorders during adolescence and early adulthood. JAMA. 2000;284:2348–51. doi: 10.1001/jama.284.18.2348. [DOI] [PubMed] [Google Scholar]
- 10.McLeish AC, Zvolensky MJ, Bucossi MM. Interaction between smoking rate and anxiety sensitivity: Relation to anticipatory anxiety and panic-relevant avoidance among daily smokers. J Anxiety Disord. 2007;21:849–59. doi: 10.1016/j.janxdis.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Zvolensky MJ, Leen-Feldner EW, Feldner MT, Bonn-Miller MO, Lejuez CW, Kahler CW, Stuart G. Emotional responding to biological challenge as a function of panic disorder and smoking. J Anxiety Disord. 2004;18:19–32. doi: 10.1016/j.janxdis.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Zvolensky MJ, Bernstein A, Cardenas SJ, Colotla VA, Marshall EC, Feldner MT. Anxiety sensitivity and early relapse to smoking: A test among Mexican daily, low-level smokers. Nicotine Tob Res. 2007;9:483–91. doi: 10.1080/14622200701239621. [DOI] [PubMed] [Google Scholar]
- 13.Zvolensky MJ, Bonn-Miller MO, Bernstein A, Marshall EC. Anxiety sensitivity and abstinence duration to smoking. J Ment Health. 2006;15:659–70. [Google Scholar]
- 14.Zvolensky MJ, Gibson LE, Vujanovic AA, Gregor K, Bernstein A, Kahler C, Lejuez CW, Brown RA, Feldner MT. Impact of posttraumatic stress disorder on early smoking lapse and relapse during a self-guided quit attempt among community-recruited daily smokers. Nicotine Tob Res. 2008;10:1415–1427. doi: 10.1080/14622200802238951. [DOI] [PubMed] [Google Scholar]
- 15.Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 16.Waxmonsky JA, Thomas MR, Miklowitz DJ, Allen MH, Wisniewski SR, Zhang H, Ostacher MJ, Fossey MD. Prevalence and correlates of tobacco use in bipolar disorder: Data from the first 2000 participants in the Systematic Treatment Enhancement Program. Gen Hosp Psychiatry. 2005;27:321–8. doi: 10.1016/j.genhosppsych.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Lasser K, Boyd JW, Woolhander S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284:2606–10. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 18.Breslau N, Kilbey MM, Andreski P. Nicotine withdrawal symptoms and psychiatric disorders: Findings from an epidemiologic study of young adults. Am J Psychiatry. 1992;149:464–9. doi: 10.1176/ajp.149.4.464. [DOI] [PubMed] [Google Scholar]
- 19.Breslau N, Johnson EO. Predicting smoking cessation and major depression in nicotine-dependent smokers. Am J Public Health. 2000;90:1122–7. doi: 10.2105/ajph.90.7.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burgess ES, Brown RA, Kahler CW, Niaura R, Abrams DB, Goldstein MG, Miller IW. Patterns of change in depressive symptoms during smoking cessation: Who's at risk for relapse? J Consul Clin Psychol. 2002;70:356–61. doi: 10.1037//0022-006X.70.2.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Covey L, Glassman A, Stetner F. Depression and depressive symptoms in smoking cessation. Compr Psychiatry. 1990;31:350–4. doi: 10.1016/0010-440x(90)90042-q. [DOI] [PubMed] [Google Scholar]
- 22.Kahler C, Brown R, Ramsey S, Niaura R, Abrams D, Goldstein M, et al. Negative mood, depressive symptoms, and major depression after smoking cessation treatment in smokers with a history of major depressive disorder. J Abnorm Psychol. 2002;111:670–675. doi: 10.1037//0021-843x.111.4.670. [DOI] [PubMed] [Google Scholar]
- 23.Zelman DC, Brandon TH, Jorenby DE, Baker TB. Measures of affect and nicotine dependence predict differential response to smoking cessation treatments. J Consul Clin Psychol. 1992;60:943–52. doi: 10.1037//0022-006x.60.6.943. [DOI] [PubMed] [Google Scholar]
- 24.Zvolensky MJ, Bernstein A, Marshall EC. Anxiety vulnerability factors and disorders and tobacco and marijuana use and disorders: Emerging theory and research explicating their relations. Addict Behav. 2008;33:1383–4. doi: 10.1016/j.addbeh.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agosti V, Nunes E, Levin F. Rates of psychiatric comorbidity among U.S. Residents with lifetime cannabis dependence. Am J Drug Alcohol Abuse. 2002;28:643–52. doi: 10.1081/ada-120015873. [DOI] [PubMed] [Google Scholar]
- 26.Arendt M, Munk-Jorgensen P. Heavy cannabis users seeking treatment: Prevalence of psychiatric disorders. Soc Psychiatry Psychiatr Epidemiol. 2004;39:97–105. doi: 10.1007/s00127-004-0719-7. [DOI] [PubMed] [Google Scholar]
- 27.Bovasso GB. Cannabis abuse as a risk factor for depressive symptoms. Am J Psychiatry. 2001;158:2033–7. doi: 10.1176/appi.ajp.158.12.2033. [DOI] [PubMed] [Google Scholar]
- 28.Miller NS, Klamen D, Hoffmann NG, Flaherty JA. Prevalence of depression and alcohol and other drug dependence in addictions treatment populations. J Psychoactive Drugs. 1996;28:111–24. doi: 10.1080/02791072.1996.10524384. [DOI] [PubMed] [Google Scholar]
- 29.Troisi A, Pasini A, Saracco M, Spalletta G. Psychiatric symptoms in male cannabis users not using other illicit drugs. Addiction. 1998;93:487–92. doi: 10.1046/j.1360-0443.1998.9344874.x. [DOI] [PubMed] [Google Scholar]
- 30.Hathaway AD. Cannabis effects and dependency concerns in long-term frequent users: A missing piece of the public health puzzle. Addict Res Theory. 2003;11:441–58. [Google Scholar]
- 31.Katerndahl DA, Realini JP. Lifetime prevalence of panic states. Am J Psychiatry. 1993;150:246–249. doi: 10.1176/ajp.150.2.246. [DOI] [PubMed] [Google Scholar]
- 32.Zvolensky MJ, Bernstein A, Sachs-Ericcson N, Schmidt NB, Buckner J, Bonn-Miller MO. Cannabis use, abuse, and dependence and panic attacks in a representative sample. J Psychiatr Res. 2006;40:477–86. doi: 10.1016/j.jpsychires.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Zvolensky MJ, Lewinsohn P, Bernstein A, Schmidt NB, Buckner JD, Seeley J, Bonn-Miller MO. Prospective associations between cannabis use, abuse, and dependence and panic attacks and disorder. J Psychiatr Res. 2008;42:1017–23. doi: 10.1016/j.jpsychires.2007.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bonn-Miller MO, Moos RH. Marijuana discontinuation, anxiety symptoms, and relapse to marijuana. Addict Behav. 2009;34:782–785. doi: 10.1016/j.addbeh.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 35.Tunving K. Psychiatric effects of cannabis use. Acta Psychiatr Scand. 1985;72:209–17. doi: 10.1111/j.1600-0447.1985.tb02597.x. [DOI] [PubMed] [Google Scholar]
- 36.Chen CY, Wagner FA, Anthony JC. Marijuana use and the risk of major depressive episode: Epidemiological evidence from the United States National Comorbidity Survey. Soc Psychiatry Psychiatr Epidemiol. 2002;37:199–206. doi: 10.1007/s00127-002-0541-z. [DOI] [PubMed] [Google Scholar]
- 37.Brook JS, Rosen Z, Brook DW. The effect of early marijuana use on later anxiety and depressive symptoms. NYS Psychologist. 2001 Jan;:35–9. [Google Scholar]
- 38.Degenhardt L, Hall W, Lynskey M. Alcohol, cannabis, and tobacco use among Australians: A comparison of their associations with other drug use and disorders, affective and anxiety disorders, and psychosis. Addiction. 2001;96:1603–14. doi: 10.1046/j.1360-0443.2001.961116037.x. [DOI] [PubMed] [Google Scholar]
- 39.Smart RG, Ogborne AC. Drug use and drinking among students in 36 countries. Addict Behav. 2000;25:455–460. doi: 10.1016/s0306-4603(99)00013-1. [DOI] [PubMed] [Google Scholar]
- 40.Amos A, Wiltshire S, Bostock Y, Haw S, McNeill A. You can't go without a fag…you need it for your hash- a qualitative exploration of smoking, cannabis, and young people. Addiction. 2004;99:77–81. doi: 10.1111/j.1360-0443.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- 41.Watson D, Weber K, Assenheimer JS, Clark LA, Strauss O, McCormick J. Testing a tripartite model. I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. J Abnorm Psychol. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- 42.State of Vermont Department of Health. Retrieved June 30, 2007, from http://www.healthyvermonters.info/
- 43.Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT: The alcohol use disorders identification test Guidelines for use in primary health care. World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]
- 44.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- 45.Forsyth JP, Zvolensky MJ. Experimental psychopathology, clinical science, and practice: An irrelevant or indispensable alliance? Applied and Preventive Psychology: Current Scientific Perspectives. 2002;10:243–264. [Google Scholar]
- 46.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV patient edition (SCID-N/P, Version 2.0) New York: Biometrics Research Department; 1994. [Google Scholar]
- 47.Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111:180–5. [PubMed] [Google Scholar]
- 48.Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Nonclinical panic attack history and smoking cessation: An initial examination. Addict Behav. 2004;29:825–30. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 49.Bonn-Miller MO, Zvolensky MJ. An evaluation of the nature of marijuana use and its motives among young adult active users. Am J Addict. 2009;18:409–416. doi: 10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- 50.Bonn-Miller MO, Zvolensky MJ, Leen-Feldner EW, Feldner MT, Yartz AR. Marijuana use among daily tobacco smokers: Relationship to anxiety-related factors. J Psychopathol Behav Assess. 2005;27:279–89. [Google Scholar]
- 51.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the AUDIT: WHO collaborative project on early detection of persons with harmful alcohol consumption – II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 52.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol. 1988;54:1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 53.Zvolensky MJ, Bernstein A. Cigarette smoking and panic psychopathology. Curr Dir Psychol Sci. 2005;14:301–305. [Google Scholar]


