Abstract
Japanese encephalitis (JE) is a severe disease and a risk for travelers who visit JE-endemic countries. We reviewed all published JE cases in travelers from non-endemic areas from 1973 through 2008, and assessed factors related to risk of infection. There were 55 cases that occurred in citizens of 17 countries. Age range of case-patients was 1–91 years (median = 34 years). Ten (18%) persons died and 24 (44%) had mild to severe sequelae. In a detailed risk assessment of 37 case-patients, 24 (65%) had spent ≥ 1 month in JE-endemic areas, and most had factors identified that may have increased infection risk. The estimate of overall JE risk was low, < 1 case/1 million travelers to JE-endemic countries. Nonetheless, for each traveler, a careful assessment of itinerary and activities, a decision on vaccination, and information on mosquito precautions are needed to reduce the risk of this disease.
Introduction
Japanese encephalitis virus (JEV) is a mosquito-borne flavivirus and a leading cause of encephalitis in Asia.1 Clinical illness develops in less than 1% of persons infected with JEV. However, when neurologic infection occurs, it is usually severe, with a case-fatality rate of up to 30% and sequelae in 30–50% of survivors.2–4
Transmission of JEV occurs throughout much of Asia and parts of the Western Pacific region. The risk of JEV infection varies among countries, in different areas within countries, and from year to year. In temperate regions, there is usually a seasonal pattern of JEV transmission, and large and explosive outbreaks can occur. In tropical regions, transmission usually occurs year-round, often with a peak during the rainy season.5,6 Japanese encephalitis virus is transmitted in an enzootic cycle between mosquitoes and vertebrate hosts, primarily pigs and wading birds. The main mosquito vector, Culex tritaeniorhynchus, commonly breeds in flooded rice fields and ground pools. It is an evening-biting and nighttime-biting mosquito that feeds most often in the outdoors, with peak biting times after sunset and again after midnight.7 The risk of infection is greatest in rural, agricultural areas, where all elements of the JEV transmission cycle are present. However, JE cases are occasionally reported from urban and peri-urban areas.8,9
There is no specific treatment for JE, but the disease is preventable by vaccination. A mouse brain–derived vaccine has been available for many decades, and a live, attenuated JE vaccine is increasingly available in Asia.5,10 An inactivated Vero cell-derived vaccine was licensed in 2009 for use in adult travelers in the United States, Europe, and Australia.11 In some JE-endemic countries, immunization programs have substantially reduced the incidence of JE among the local population. However, because JEV is maintained in an animal–mosquito cycle in nature, unvaccinated travelers to these countries are still at risk for infection.
The risk of JE in travelers to Asia is generally considered to be low, with previous estimates for U.S. and European travelers suggesting that its frequency is less than one case per one million travelers.12,13 Higher rates have been estimated for travelers from some countries to particular destinations, with risk estimates for Finnish and Swedish travelers to Thailand of 1 case/257,000 and 1 case/400,000 travelers, respectively.14,15 Risk for the individual traveler depends on many factors including length and season of travel, itinerary, type of accommodations, and activities. We reviewed all published cases of JE in travelers who originated from non-endemic countries, occurring during 1973–2008. Before 1973, publications focused on cases among military personnel, with more than 300 cases described among soldiers from the United States, the United Kingdom, Australia, and Russia.16–24 In 1993, summary information on travel-associated JE cases during 1978–1992 was published.12 We included and expanded on the previous data and assessed factors related to risk of infection.
Materials and Methods
Data sources.
The PubMed database, the Global Health database, and the EMBASE database were searched for articles published up until June 30, 2009. The search strategy used was “Japanese encephalitis” and “travel+” or “journey”. If one of the selected articles referred to another article in which a case of travel-associated JE was described and was not captured in the database search, then that article was also included. Communicable disease-related publications available on the internet from Australia (Communicable Diseases Intelligence), Canada (Canada Communicable Disease Report) and Europe (Eurosurveillance, United Kingdom Communicable Disease Report Weekly, United Kingdom Communicable Disease and Public Health, United Kingdom Health Protection Report) were searched for any additional published case reports. The authors were aware of one article “in press” at the time, which has subsequently been published and was also included.11 If any case reports required clarification or additional information, we attempted to contact the article's author or the clinician.
Study selection criteria.
A case of travel-associated JE was defined as a published report of JE in a traveler from a non-endemic country who had visited or lived in an Asian or Western Pacific country with JEV transmission. A traveler was defined as a tourist, expatriate or soldier. We selected articles that described travel-associated cases occurring during 1973–2008.
Japanese encephalitis case review and risk analysis.
For each case, we recorded information on age, sex, country of origin, year and places of travel, traveler type, vaccination status, laboratory testing performed, and outcome of illness. Sequelae were assessed as severe if the author described them as serious or severe, if the case-patient had permanent neurological sequelae at ≥ 3 months, or if there were physical and cognitive/intellectual sequelae.
We also conducted a more detailed descriptive risk analysis on a subset of cases with more complete information available. This analysis included a review of the length of time in country, season of travel, and potential risk-related exposures during the period in the JE-endemic area.
Results
Over the 36-year period from 1973 through 2008, we identified 55 published cases of travel-associated JE among tourists, expatriates, or soldiers who had visited one or more countries in Asia or the Western Pacific region (Table 1). A small increase in the number of published cases occurred in each of the three most recent decades: 1979–1988 (n = 14), 1989–1998 (n = 17), and 1999–2008 (n = 20). Two cases were reported from 1973–1978, and two cases had unknown dates of onset but occurred before 1993. Since 1980, most years had one or two reported cases, with a maximum of six cases in 1991 (Figure 1). Among the 46 cases for which age was recorded, patients ranged from 1 to 91 years of age (median = 34 years) (Figure 2). Overall, 29 (53%) of 55 cases were in males, 22 (40%) were in females, and 4 (7%) were in persons whose sex was not known. Laboratory confirmation was available for 38 (69%) cases, diagnosis was epidemiologically based for 1 (2%) case, and diagnostic test information was unavailable for 16 (29%) cases.
Table 1.
Published cases (n = 55) of travel-associated Japanese encephalitis, 1973–2008*
| Case | Year | Age (years) | Sex | Type | Citizenship | Probable country of JE virus acquisition | Outcome | Laboratory confirmed | JE vaccine | References |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2008 | 9 | M | Tourist–VFR | United States | Vietnam | Survived | Yes | No | 11 |
| 2 | 2008 | 91 | M | Tourist | Italy | Thailand | Died | U | U | 15 |
| 3 | 2008 | 37 | F | Tourist | Sweden | Thailand | Survived | Yes | U | 15 |
| 4 | 2008 | 36 | F | Tourist–VFR | Sweden | Thailand | Survived | Yes | U | 15 |
| 5 | 2006 | 59 | F | Tourist | Germany | China | Survived | Yes | No | 25 |
| 6 | 2006 | 49 | M | Tourist | Italy | Vietnam | Survived | Yes | No | 26 |
| 7 | 2005 | 68 | F | Tourist–VFR | United States | Philippines | Survived | Yes | No | 11 |
| 8 | 2004 | 60 | M | Tourist | Finland | Thailand | Survived | Yes | No | 14 |
| 9 | 2004 | 29 | F | Tourist | Netherlands | Indonesia | Survived | Yes | No | 27 |
| 10 | 2004 | 49 | F | Tourist | New Zealand | China | Survived | Yes | No | 28 |
| 11 | 2004 | 22 | F | Tourist–study abroad | United States | Thailand | Survived | Yes | No | 29 |
| 12 | 2004 | 66 | M | Expatriate | Germany† | Papua New Guinea | Survived | Yes | No | 30 |
| 13 | 2003 | 30 | F | Expatriate | United States | Thailand | Survived | Yes | No | 11 |
| 14 | 2003 | 32 | F | Tourist | New Zealand† | Malaysia | Survived | Yes | No | 31 |
| 15 | 2002 | 65 | F | Tourist | Sweden | Thailand | Survived | Yes | U | 15 |
| 16 | 2002 | 41 | M | Tourist | Sweden | Thailand | Survived | Yes | U | 15 |
| 17 | 2001 | U | M | Expatriate | Finland | China | Survived | Yes | No | 32 |
| 18 | 2001‡ | U | M | Tourist | Sweden | Thailand | Survived | Yes | No | 33 |
| 19 | 2000‡ | 22 | M | Tourist | France | Indonesia | Survived | Yes | No | 34 |
| 20 | 2000 | 80 | M | Tourist | Sweden | Indonesia | Survived | Yes | No | 35 |
| 21 | 1998 | 57 | M | Tourist | Norway | Philippines | Died | Yes | U | 15 |
| 22 | 1998 | 65 | M | Expatriate | Norway | Philippines | Died | Yes | U | 15 |
| 23 | 1997 | 25 | M | Tourist | Norway | Thailand | Survived | Yes | No | 36 |
| 24 | 1997 | 30 | F | Tourist | Netherlands | Thailand | Survived | Yes | No | 27 |
| 25 | 1996 | 59 | F | Tourist | France | Thailand | Survived | Yes | No | 37 |
| 26 | 1995 | 51 | M | Tourist | Denmark | Indonesia | Died | Yes | No | 38 |
| 27 | 1994 | 60 | F | Tourist | Sweden | Indonesia | Survived | Yes | No | 39 |
| 28 | 1993 | 3 | F | Expatriate | Australia | Indonesia | Survived | Yes | U | 40 |
| 29 | 1992 | 21 | F | Tourist | United Kingdom | Thailand | Survived | Yes | No | 41 |
| 30 | 1992 | 19 | M | Tourist | United States | Singapore | Survived | U | U | 12 |
| 31 | 1991 | 20 | M | Soldier | United States | Japan | Survived | Yes | No | 42 |
| 32 | 1991 | 35 | M | Soldier | United States | Japan | Survived | Yes | No | 42 |
| 33 | 1991 | 28 | M | Soldier | United States | Japan | Survived | Yes | No | 42 |
| 34 | 1991 | 33 | F | Expatriate | Russia | Japan | Survived | Yes | No | 16 |
| 35 | 1991 | U | U | U | Austria | Thailand | U | U | U | 12 |
| 36 | 1991 | U | M | U | Australia | Indonesia | Survived | Yes | U | 12, 40 |
| 37 | 1989 | 22 | F | Tourist | Israel | Thailand | Survived | U | U | 12 |
| 38 | 1988 | 10 | F | Tourist | Australia | Indonesia | Survived | Yes | No | 43 |
| 39 | 1988 | 64 | M | U | United States | U | U | U | U | 12 |
| 40 | 1986 | 55 | M | Soldier | United States | Philippines | Survived | U | U | 12, 44 |
| 41 | 1986 | U | M | Soldier | United States | Philippines | Survived | U | U | 12, 44 |
| 42 | 1985 | 30 | M | Tourist | Germany | Thailand | Died | U | U | 12 |
| 43 | 1985 | 9 | M | Tourist | Eastern Europe | Vietnam | Died | U | U | 12 |
| 44 | 1983 | 1 | M | Tourist | United States | U | U | U | U | 12 |
| 45 | 1983 | 30 | F | Tourist | Netherlands | Thailand | Survived | U | U | 12 |
| 46 | 1982 | 35 | F | Expatriate | United Kingdom | Hong Kong | Died | Yes | No | 45 |
| 47 | 1982 | 35 | F | U | Canada | China | U | Yes | U | 12, 46 |
| 48 | 1982 | 32 | M | Soldier | United States | U | U | U | U | 12 |
| 49 | 1982 | 62 | M | Tourist | United States | China | Died | No | U | 12, 47 |
| 50 | 1981 | 21 | M | Tourist–study abroad | United States | China | Died | Yes | No | 12, 48 |
| 51 | 1981 | U | U | U | Australia | U | U | U | U | 12 |
| 52 | 1978 | U | M | Expatriate | Italy | China | Died | U | U | 12 |
| 53 | 1973 | 30 | F | Expatriate | Russia | Myanmar | Survived | Yes | No | 16 |
| 54 | U§ | U | U | U | Denmark | Thailand | U | U | U | 12 |
| 55 | U§ | U | U | U | Germany | Thailand | U | U | U | 12 |
JE = Japanese encephalitis; VFR = visiting friends and relatives; U = unknown.
Hospitalized in Australia.
Year of onset not given but assumed from publication date and data in article.
Before 1993.
Figure 1.
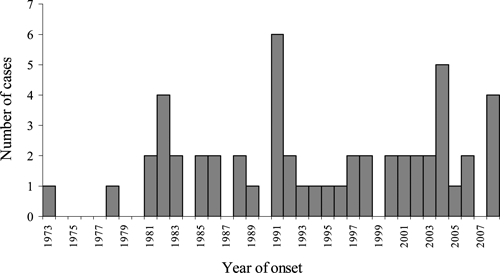
Year of onset of 53 travel-associated Japanese encephalitis cases. Dates of onset were not available for two cases, but both were before 1993.
Figure 2.
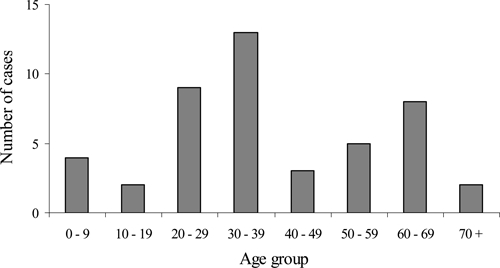
Travel-associated Japanese encephalitis cases by age group, 1973–2008 (n = 46).
Overall 33 (60%) of the cases were in tourists, 9 (16%) were in expatriates, 6 (11%) were in soldiers, and the type of travel was unknown in 7 (13%). The tourist category included three persons who were visiting friends and relatives (VFRs), and two students on study-abroad programs. None of the 29 travelers for whom information on vaccination status was available had been vaccinated.
The 55 cases occurred in citizens of 17 different non-JE-endemic countries. Only two non-endemic countries had more than five published cases over the 36-year period: the United States (n = 15) and Sweden (n = 7). Of the 15 published cases in U.S. citizens, nine occurred in tourists or expatriates and six occurred in military personnel. The countries where JE was likely acquired included at least ten different JE-endemic countries. Travel-associated cases of JE were most frequently reported from Thailand, which had 19 cases overall, including nine cases during the last 10 years, followed by Indonesia (n = 8), China (n = 7), and the Philippines (n = 5) (Table 2).
Table 2.
Number of travel-associated Japanese encephalitis cases by probable country of acquisition, 1973–2008
| Country | Travel-associated cases (n = 55) | |
|---|---|---|
| No. (%) | ||
| Thailand | 19 (35) | |
| Indonesia | 8 (15) | |
| China | 7 (13) | |
| Philippines | 5 (9) | |
| Japan | 4 (7) | |
| Vietnam | 3 (5) | |
| Hong Kong (now China) | 1 (2) | |
| Malaysia | 1 (2) | |
| Myanmar | 1 (2) | |
| Papua New Guinea | 1 (2) | |
| Singapore | 1 (2) | |
| Not available | 4 (7) | |
The case-fatality rate was 18% (10 of 55 cases). There were 24 (44%) patients who survived but had sequelae, 12 (22%) who recovered completely, 1 (2%) who survived but for whom the presence of sequelae had not been determined, and 8 (14%) who had an unknown outcome. Of the 24 patients with sequelae, 10 (42%) had severe sequelae, 7 (29%) had non-severe sequelae, and 7 (29%) had no detailed sequelae information. Severe sequelae included major neuropsychologic disturbances and serious physical sequelae, including total incapacitation. Less-severe outcomes included a mild residual tremor, poor concentration, and memory problems. One woman was infected in the sixth month of pregnancy and recovered; however, mild pyramidal signs were detected in her infant at one year of age.16
Detailed case review and risk analysis.
More complete information regarding travel itineraries and activities was available for 37 (67%) of 55 cases, and was included in the detailed descriptive risk analysis. Many reports documented exposures that would have increased the risk of JEV infection, including rural travel, residence on or near a farm, staying in unscreened accommodations, and participating in trekking or other outdoor activities (Table 3). Duration of travel or residence in a JE-endemic country ranged from 10 days to 34 years, and was ≥ 1 month in 24 (65%) cases.
Table 3.
Available exposure information for 37 published cases of travel-associated Japanese encephalitis, 1973–2008
| Case | Probable country of Japanese encephalitis virus acquisition (other countries visited) | Month of onset* | Duration of travel | Exposures |
|---|---|---|---|---|
| 12 | Papua New Guinea | Jan | 34 years | Lived on farm 20 km from Port Moresby |
| 46 | Hong Kong | Jul | 22 years | Lived in Hong Kong, urban pig problem at that time |
| 22 | Philippines | Aug | 3 years | No details |
| 53 | Myanmar | Jul | 3 years | Lived in Myanmar, wife of Russian embassy staff member |
| 28 | Indonesia | Dec | 2 years | Lived in Balinese jungle |
| 34 | Japan | Aug | 12 months† | Lived in Chiba City near Tokyo, took business trips |
| 13 | Thailand | Aug | 7 months | Lived on island off coast of southern Thailand |
| 50 | China | Sep | 4 months | Stayed mainly in urban areas but traveled through China by train |
| 2 | Thailand | Dec | 3 months | Stayed in Phuket, southern Thailand |
| 7 | Philippines | Jul | 3 months | Stayed with family in Manila |
| 21 | Philippines | Sep | Months | Traveled around Philippines |
| 29 | Thailand (Malaysia) | Sep | 9 weeks | Trekking in northern Thailand, beach resort in southern Thailand |
| 3 | Thailand | Feb | 8 weeks | In northern Thailand |
| 14 | Malaysia (Thailand, Cambodia, Vietnam) | May | 8 weeks | In Sarawak on a jungle trek, sleeping in longhouses |
| 31 | Japan | Jun | > 6 weeks | Military exercises in rural Okinawa |
| 32 | Japan | Sep | > 6 weeks | Military exercises in rural Okinawa |
| 33 | Japan | Oct | > 6 weeks | Military exercises in rural Okinawa |
| 9 | Indonesia | June | 6 weeks | In small islands around Flores in two weeks prior to onset |
| 4 | Thailand | Feb | 5 weeks | Traveled around northern Thailand |
| 10 | China (Japan) | Jul | 5 weeks | Three weeks in rural and urban China |
| 19 | Indonesia (India) | Oct | 5 weeks‡ | No details |
| 1 | Vietnam (Cambodia) | Feb | 4 weeks | Stayed with family in rural southern Vietnam |
| 11 | Thailand | Jun | 4 weeks | Stayed in unscreened dormitory in Chiang Mai City and one night in rural Chiang Mai Valley, northern Thailand |
| 17 | China (Singapore) | Sep | 4 weeks | Had relocated to China; lived 30km from Beijing with farms nearby |
| 15 | Thailand | Dec | < 4 weeks | Koh Lanta, southern Thailand |
| 24 | Thailand | Aug | > 3 weeks | Traveled through Thailand, including near Cambodian border |
| 6 | Vietnam | May | 3 weeks | Much of trip in rural north Vietnam |
| 20 | Indonesia | Apr | 3 weeks | Hotels on Java and Bali with day trips on the islands |
| 16 | Thailand | Apr | 2 weeks | Stayed in Phuket, southern Thailand; occasional day trips |
| 5 | China | Sep | 2 weeks | Stayed in suburb of northwest Beijing; rural trip for 2 days |
| 8 | Thailand | Dec | 2 weeks | Coastal hotels in Khao Lak and Phuket, southern Thailand; day trips to rural areas |
| 18 | Thailand | Jan | 2 weeks | Stayed in bungalow in Khao Lak, southern Thailand; day trip to national park with mangrove swamps |
| 23 | Thailand | Dec | 2 weeks | Beach holiday in Thailand |
| 38 | Indonesia | Jan | 2 weeks | Coastal hotel on Bali with a few day trips to rural areas |
| 26 | Indonesia | Jan | 12 days | Coastal hotel on Bali with a few trips inland |
| 25 | Thailand | May | 12 days | Hotels in Chiang Rai and Pattaya, northern and eastern Thailand |
| 27 | Indonesia | Mar | 10 days | Coastal hotel on Bali with one day trip to countryside |
Month of illness onset or month Japanese encephalitis virus infection acquired.
Japanese encephalitis occurred after 1 month.
Included travel time in Australia.
Of the 13 travelers with a shorter trip duration < 1 month, 10 (77%) traveled for 2 to < 4 weeks and 3 (23%) traveled for 10—12 days. The travel destinations for these shorter-term travelers were Thailand (n = 7), Indonesia (n = 4), China (n = 1), and Vietnam (n = 1). Three (23%) travelers spent most of their time in rural areas, 6 (46%) stayed in coastal or non-rural areas but took day trips to rural areas or national parks, 1 (8%) stayed in a coastal area and took day trips to unspecified destinations, and 3 (23%) had no exposure-related information. There were no cases among business or other short-term travelers who visited only urban areas.
Disease onset occurred in all months of the year, except November. Fourteen (61%) of the 23 travelers who visited a country that is considered to have a recognized peak JE transmission season were infected during that season. Two tourists acquired JEV infection in February in northern Thailand, where most JE cases occur during May–October. Although six other tourists to Thailand and one tourist to Vietnam acquired infection in the period during December–April, outside what is typically considered the peak transmission season, they visited only tropical, southern parts of these countries where the hotter climate typically means there is year-round JEV transmission.
Discussion
The 55 travel-associated JE cases identified over the 36-year period from 1973 through 2008 represent an average of 1.5 published cases per year. Although there was a small increase in case frequency over time, this may reflect the increase in overall tourist numbers during the same period, or possibly clinicians more frequently considering the diagnosis of JE. The majority of cases occurred among expatriates or tourists who visited JE-endemic countries for at least one month.
The risk of JE for travelers is clearly low, although the precise risk is unknown. Among U.S. citizens, only 15 travel-associated JE cases were identified during 1973–2008. The annual number of entries of U.S. citizens to Asia was approximately 2–3 million earlier in this period and increased to approximately 5.5 million entries in 2004.12,49 On the basis of these data, the approximate risk estimate was < 0.2 cases/1 million U.S. travelers. However, this figure does not differentiate between the lower risk for short-term travelers with low-risk itineraries and the greater risk for expatriates, travelers on long trips, or short-term travelers with high-risk itineraries. In addition, the JE vaccine licensed in the United States in 1992 undoubtedly has prevented cases. However, a recent survey in the United States found that only 47 (11%) of 415 travelers to JE-endemic countries with at-risk itineraries were vaccinated with ≥ 1 dose of JE vaccine (Duffy M and others, unpublished data). Despite this low rate of vaccination, only four cases have been reported in U.S. travelers since 1992, reinforcing the fact that the overall risk of JE in travelers is low.
The percentage of the total number of JE travel-associated cases that these 55 published cases represent is unknown. Some indication is given by using available national data. In Australia, for example, JE has been a nationally notifiable disease since 2001. During 2001–2008, three JE cases were reported nationally; case reports were published for two of the cases and the third patient had a mild, self-limiting illness (Marich A, New South Wales Department of Health, unpublished data).30,31,50 A recent review suggested that among Scandinavian patients, 7 (54%) of 13 cases that occurred during 1994–2008 were reported in the literature.15 Documents from health departments in the United Kingdom and Canada in 2008 indicated that all known cases that had occurred in their travelers had been published.51,52 These data suggest that at least 50%, and perhaps a higher percentage, of travel-associated JE cases that are diagnosed are published. It is likely that some travel-associated cases are never diagnosed as JE. Nevertheless, on the basis of the risk estimate calculated above of < 0.2 cases per 1 million travelers, and despite some degree of under-diagnosis and under-reporting, it is unlikely that the overall JE risk for travelers is > 1 case/1 million travelers.
The age groups represented among the reported cases ranged from young children to elderly adults. Before implementation of JE immunization programs in JE-endemic countries, the majority of cases characteristically occur in children less than 15 years of age because most of the older population has developed immunity from previous subclinical infection.6 However, unvaccinated travelers who enter JE-endemic areas are usually immunologically naive with respect to JEV. As a result, travelers of all ages are susceptible to infection as clearly demonstrated in this review.
Cases among two particular subgroups of tourists, VFRs and students on study-abroad programs, were noted. Both groups are important in relation to risk of travel-associated JE because they frequently spend several months in JE-endemic countries, often in rural or remote locations. Despite potentially high risk itineraries, many may not seek pre-travel advice. It is well-recognized that the perception of risk among VFRs is often low, particularly in those traveling back to their country of birth.53 Students may not always seek travel-related preventive medical advice, or receive appropriate interventions, for financial or other reasons.54 Organized travel programs, including study-abroad programs, should ensure that their clients receive appropriate preventive health information.
Cases of JE were reported in travelers to countries where there is no ongoing surveillance for JE, including Papua New Guinea, Myanmar, and the Philippines. In countries where JE cases among the local population are not routinely recognized or reported, a tourist may act as a sentinel for the presence of JEV transmission. In the late 1980s and early 1990s, it was the reporting of JE in tourists to Bali that accelerated recognition by the Indonesian government that JE was a public health problem.38,39,43,55 The lack of recognition and reporting of JE locally should not affect the decision to vaccinate tourists planning travel to areas considered to be JE-endemic.
Although many of the persons who visited countries with recognized peak JEV transmission seasons were infected during these periods, some travelers to Thailand and Vietnam acquired infection at other times of the year. Thailand has year-round JEV transmission in much of the country with a seasonal peak during May–October, mainly in the northern part of the country.56,57 Vietnam has seasonal transmission in its northern region but year-round transmission in the southern region.3,58 Because of prominent seasonal peaks in some areas of these countries, the year-round disease risk in many parts of both countries is often under-appreciated. Travel medicine providers should review each traveler's itinerary in detail to provide the most appropriate preventive recommendations for JE.
The U.S. Advisory Committee on Immunization Practices recommends JE vaccine for travelers who plan to spend a month or longer in JE-endemic areas during the JEV transmission season. Japanese encephalitis vaccine should be considered for short-term travelers (< 1 month) to JE-endemic areas during the transmission season if their activities will increase the risk of JEV exposure. Japanese encephalitis vaccine is not recommended for short-term travelers whose visit will be restricted to urban areas or times outside of a well-defined JEV transmission season.59 Although no minimum duration of travel eliminates a traveler's risk for JE, a longer itinerary increases the likelihood that a traveler will spend time in an area with active JEV transmission. Although a recent survey suggested that longer-term travelers comprise approximately 20% of U.S. travelers to JE-endemic countries (Duffy M and others, unpublished data), 65% of the cases included in this review were in expatriates and longer-term travelers, highlighting the increased JE risk in this group and need for protection by vaccination.
Among the 35% of case-patients who acquired infection during stays < 1 month, their itineraries, activities, or accommodations likely contributed to their risk of JEV exposure, despite their shorter lengths of stay. These cases demonstrate the complexity for both travelers and providers in assessing the risk presented by a specific travel itinerary. Decisions regarding the use of JE vaccine must weigh several factors. JE is a severe disease, no specific treatment is available, and disease outcome is often poor. Conversely, the overall risk of travel-associated JE disease is low, vaccination is costly, and there are potential side effects associated with vaccination.60
Because shorter-term travelers represent a much higher proportion of travelers overall, consideration of risk in this group is important. Among JE cases in our review with travel duration < 1 month, Thailand and Indonesia (Bali) were the two commonest destinations. On average, 4.5 million tourists from non JE-endemic countries visited Thailand each year during 2000–2008.61 On the basis of survey data from U.S. travelers to Asia, which indicated 80% of all travelers have short-term (< 1 month) itineraries (Duffy M and others, unpublished data), and a conservative assumption that twice as many travel-associated JE cases occurred than were published, the JE risk was approximately 1 case/3.3 million short-term travelers since 1996, when the first case was reported. In 1988, the first reported JE case in a short-term tourist to Bali occurred; since then three additional such case reports have been published. The most recent case occurred in 2000 in a tourist who traveled to Java and Bali but likely acquired his JEV infection in Bali. On average, approximately 620,000 tourists from non–JE-endemic countries have visited Bali annually during the past decade.62 Using conservative assumptions that annual tourists visits were half this amount in the 11 years before this decade, twice the number of cases occurred than were published, and 80% of Bali-visiting tourists had short-term itineraries, the JE risk in the 21-year period since 1988 was approximately 1 case/1.0 million short-term travelers.
The limitations of this review include that the 55 cases reported here cannot be considered a complete or representative sample of all travel-associated JE cases. Details of a case diagnosed and treated abroad may not be available in the person's home country. A case report is not published for every patient that is diagnosed, and the diagnosis may be missed. The reported cases may not be representative of all travel-associated JE cases, either diagnosed or undiagnosed. For example, publication may have been more likely if a case had a unique or more severe clinical presentation, unusual travel destination, or another noteworthy epidemiologic feature such as JEV infection associated with short-term travel. Our search strategy may not have detected all cases. Furthermore, we were unable to include 18 (33%) of the 55 cases in the detailed risk analysis because risk factor information was unavailable. Finally, we were able to conduct only a fairly simple, mostly qualitative description of possible risk factors for travel-associated JE. A more quantitative risk-factor study (e.g., a case–control study) would require a suitable comparison group of adequate size and composed of otherwise similar travelers who did not acquire JEV infection. Because constructing such a control group would be logistically extremely difficult, no analytic studies of this type have ever been published.
When consulted by a traveler planning to visit a JE-endemic country, travel medicine providers should perform a careful assessment of each traveler's itinerary, including destinations, duration and season of travel, and potential activities. All travelers should be advised of the risks of JE and the importance of personal protective measures to reduce the risk of mosquito bites. For some travelers who will be in a high-risk setting based on travel destination, duration, season, and activities, JE vaccine can further reduce the risk of infection.
Acknowledgments
We would like to thank the many persons who assisted with providing or translating information to assist with our review, especially Corine Delsing, Lars Eisen, Jacob Kool, Olga Kosoy, Luise Landreh, Lars Lindquist, Anthony Marfin, Andrew Marich, Jeremy McAnulty, James McCarthy, David Mercer, Pekka Nuorti, Maria Rotzen Östlund, Ann Richards, Robert Sweeney, and Piter Visser. We also thank Grant Campbell and J. Erin Staples for reviewing the manuscript.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily represent those of the Centers for Disease Control and Prevention.
Footnotes
Authors' addresses: Susan L. Hills, Anne C. Griggs, and Marc Fischer, Arboviral Diseases Branch, Division of Vector-Borne Infectious Diseases, National Center for Zoonotic, Vector-Borne and Enteric Diseases, Centers for Disease Control and Prevention, Fort Collins, CO, E-mails: shills@cdc.gov, anne.griggs@gmail.com, and mfischer@cdc.gov.
References
- 1.Halstead SB, Jacobson J. Japanese encephalitis. Adv Virus Res. 2003;61:103–138. doi: 10.1016/s0065-3527(03)61003-1. [DOI] [PubMed] [Google Scholar]
- 2.Solomon T. Control of Japanese encephalitis—within our grasp? N Engl J Med. 2006;355:869–871. doi: 10.1056/NEJMp058263. [DOI] [PubMed] [Google Scholar]
- 3.Tsai TF. New initiatives for the control of Japanese encephalitis by vaccination: minutes of a WHO/CVI meeting, Bangkok, Thailand, October 13–15, 1998. Vaccine. 2000;18((Suppl 2)):1–25. doi: 10.1016/s0264-410x(00)00037-2. [DOI] [PubMed] [Google Scholar]
- 4.Fischer M, Griggs A, Staples JE. Japanese encephalitis. CDC Health Information for International Travel 2010. Atlanta, GA: Centers for Disease Control and Prevention; 2009. pp. 74–81. [Google Scholar]
- 5.Fischer M, Hills S, Staples E, Johnson B, Yaich M, Solomon T. In: Emerging Infections 8. Scheld WM, Hammer SM, Hughes JM, editors. Washington, DC: American Society for Microbiology Press; 2008. pp. 93–124. (Japanese encephalitis prevention and control: advances, challenges, and new initiatives). [Google Scholar]
- 6.Vaughn DW, Hoke CH. The epidemiology of Japanese encephalitis: prospects for prevention. Epidemiol Rev. 1992;14:197–221. doi: 10.1093/oxfordjournals.epirev.a036087. [DOI] [PubMed] [Google Scholar]
- 7.Mackenzie JS, Williams DT, Smith DW. In: Emerging Viruses in Human Populations. Tabor E, editor. Amsterdam: Elsevier; 2007. pp. 201–268. (Japanese encephalitis virus: the geographic distribution, incidence, and spread of a virus with a propensity to emerge in new areas). [Google Scholar]
- 8.Ooi MH, Lewthwaite P, Lai BF, Mohan A, Clear D, Lim L, Krishnan S, Preston T, Chieng CH, Tio PH, Wong SC, Cardosa J, Solomon T. The epidemiology, clinical features, and long-term prognosis of Japanese encephalitis in central Sarawak, Malaysia, 1997–2005. Clin Infect Dis. 2008;47:458–468. doi: 10.1086/590008. [DOI] [PubMed] [Google Scholar]
- 9.Gingrich JB, Nisalak A, Latendresse JR, Pomsdhit J, Paisansilp S, Hoke CH, Chantalakana C, Satayaphantha C, Uechiewcharnkit K. A longitudinal study of Japanese encephalitis in suburban Bangkok, Thailand. Southeast Asian J Trop Med Public Health. 1987;18:558–566. [PubMed] [Google Scholar]
- 10.Beasley DW, Lewthwaite P, Solomon T. Current use and development of vaccines for Japanese encephalitis. Expert Opin Biol Ther. 2008;8:95–106. doi: 10.1517/14712598.8.1.95. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Japanese encephalitis among three U.S. travelers returning from Asia, 2003–2008. MMWR Morb Mortal Wkly Rep. 2009;58:737–740. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention Inactivated Japanese encephalitis virus vaccine. Recommendations of the advisory committee on immunization practices (ACIP) MMWR Morb Mortal Wkly Rep. 1993;42:1–16. [PubMed] [Google Scholar]
- 13.Hatz C, Werlein J, Mutsch M, Hufnagel M, Behrens RH. Japanese encephalitis: defining risk incidence for travelers to endemic countries and vaccine prescribing from the UK and Switzerland. J Travel Med. 2009;16:200–203. doi: 10.1111/j.1708-8305.2009.00334.x. [DOI] [PubMed] [Google Scholar]
- 14.Lehtinen VA, Huhtamo E, Siikamaki H, Vapalahti O. Japanese encephalitis in a Finnish traveler on a two-week holiday in Thailand. J Clin Virol. 2008;43:93–95. doi: 10.1016/j.jcv.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Buhl MR, Lindquist L. Japanese encephalitis in travelers: review of cases and seasonal risk. J Travel Med. 2009;16:217–219. doi: 10.1111/j.1708-8305.2009.00333.x. [DOI] [PubMed] [Google Scholar]
- 16.Pogodina VV, Bochkova NG, Leshchinskaia EV, Levina LS. Japanese encephalitis in citizens of Russia who travel abroad [in Russian] Vopr Virusol. 1996;41:8–11. [PubMed] [Google Scholar]
- 17.Long AP. Current status of immunization procedures: tetanus, and exotic diseases of military importance. Am J Public Health Nations Health. 1948;38:485–489. doi: 10.2105/ajph.38.4.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lincoln AF, Sivertson SE. Acute phase of Japanese B encephalitis: two hundred and one cases in American soldiers, Korea, 1950. J Am Med Assoc. 1952;150:268–273. doi: 10.1001/jama.1952.03680040010003. [DOI] [PubMed] [Google Scholar]
- 19.Pina FP, Merikangas UR. Japanese B encephalitis in an American soldier returning from Korea. N Engl J Med. 1953;249:531–532. doi: 10.1056/NEJM195309242491305. [DOI] [PubMed] [Google Scholar]
- 20.Hale JH, Farrant PC, Edwards D. A case of Japanese B encephalitis. J R Army Med Corps. 1954;100:117–120. [PubMed] [Google Scholar]
- 21.Fleming K. Japanese encephalitis in an Australian soldier returned from Vietnam. Med J Aust. 1975;2:19–23. doi: 10.5694/j.1326-5377.1975.tb95073.x. [DOI] [PubMed] [Google Scholar]
- 22.Ketel WB, Ognibene AJ. Japanese B encephalitis in Vietnam. Am J Med Sci. 1971;261:271–279. doi: 10.1097/00000441-197105000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Benenson MW, Top FH, Jr, Gresso W, Ames CW, Altstatt LB. The virulence to man of Japanese encephalitis virus in Thailand. Am J Trop Med Hyg. 1975;24:974–980. doi: 10.4269/ajtmh.1975.24.974. [DOI] [PubMed] [Google Scholar]
- 24.Aidem HP, Garagusi VF. Japanese B encephalitis: a case report from New York and a brief review of the literature. Ann Intern Med. 1961;55:324–327. doi: 10.7326/0003-4819-55-2-324. [DOI] [PubMed] [Google Scholar]
- 25.Reppel M, Landreh L, Gottschalk S, Schunkert H, Kurowski V, Seidel G. Japanese encephalitis in Western Europe. Clin Neurol Neurosurg. 2009;111:373–375. doi: 10.1016/j.clineuro.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Caramello P, Canta F, Balbiano R, Lipani F, Ariaudo S, De Agostini M, Calleri G, Boglione L, Di Caro A. A case of imported JE acquired during short travel in Vietnam. Are current recommendations about vaccination broader? J Travel Med. 2007;14:346–348. doi: 10.1111/j.1708-8305.2007.00140.x. [DOI] [PubMed] [Google Scholar]
- 27.Delsing CE, Ardesch J, Nihom J, Mulder L, Kootstra GJ, Hylkema BS. An unusual cause of meningo-encephalitis: Japanese encephalitis [in Dutch] Ned Tijdschr Geneeskd. 2005;149:2423–2427. [PubMed] [Google Scholar]
- 28.Cutfield NJ, Anderson NE, Brickell K, Hueston L, Pikholz C, Roxburgh RH. Japanese encephalitis acquired during travel in China. Intern Med J. 2005;35:497–498. doi: 10.1111/j.1445-5994.2005.00852.x. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention Japanese encephalitis in a U.S. traveler returning from Thailand, 2004. MMWR Morb Mortal Wkly Rep. 2005;54:123–125. [PubMed] [Google Scholar]
- 30.Hanson JP, Taylor CT, Richards AR, Smith IL, Boutlis CS. Japanese encephalitis acquired near Port Moresby: implications for residents and travelers to Papua New Guinea. Med J Aust. 2004;181:282. doi: 10.5694/j.1326-5377.2004.tb06274.x. [DOI] [PubMed] [Google Scholar]
- 31.Geraghty CM, McCarthy JS. Japanese encephalitis vaccine: is it being sufficiently used in travelers? Med J Aust. 2004;181:269–270. doi: 10.5694/j.1326-5377.2004.tb06268.x. [DOI] [PubMed] [Google Scholar]
- 32.Siikamaki H. Japanese encephalitis in a Finnish traveler: infected in Beijing [in Finnish] Suomen Laakarilehti. 2002;40:3989–3990. [Google Scholar]
- 33.Widerstrom M. Japanese encephalitis in a traveler to Thailand [in Swedish] Smittskydd. 2001;9:97. [Google Scholar]
- 34.Monnet FP. Behavioral disturbances following Japanese B encephalitis. Eur Psychiatry. 2003;18:269–273. doi: 10.1016/j.eurpsy.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 35.Ostlund MR, Kan B, Karlsson M, Vene S. Japanese encephalitis in a Swedish tourist after traveling to Java and Bali. Scand J Infect Dis. 2004;36:512–513. doi: 10.1080/00365540410020640. [DOI] [PubMed] [Google Scholar]
- 36.Hagen IJ. Japanese encephalitis after a two week beach holiday in Thailand [in Swedish] Smittskydd. 1998;1:5. [Google Scholar]
- 37.Bernard P, Jambaud E, Berbineau A, Brunot J, Flechaire A. Japanese encephalitis: an exceptional imported arbovirus [in French] Presse Med. 1998;27:1327. [PubMed] [Google Scholar]
- 38.Buhl MR, Black FT, Andersen PL, Laursen A. Fatal Japanese encephalitis in a Danish tourist visiting Bali for 12 days. Scand J Infect Dis. 1996;28:189. doi: 10.3109/00365549609049074. [DOI] [PubMed] [Google Scholar]
- 39.Wittesjo B, Eitrem R, Niklasson B, Vene S, Mangiafico JA. Japanese encephalitis after a 10-day holiday in Bali. Lancet. 1995;345:856. doi: 10.1016/s0140-6736(95)92990-8. [DOI] [PubMed] [Google Scholar]
- 40.Smith D. Japanese encephalitis case in Western Australia. Commun Dis Intell. 1994;18:149. [Google Scholar]
- 41.Burdon JT, Stanley PJ, Lloyd G, Jones NC. A case of Japanese encephalitis. J Infect. 1994;28:175–179. doi: 10.1016/s0163-4453(94)95640-5. [DOI] [PubMed] [Google Scholar]
- 42.Saito M, Sunagawa T, Makino Y, Tadano M, Haswqawa H, Kanemura K, Zamami Y, Killenbeck BJ, Fukunaga T. Three Japanese encephalitis cases in Okinawa, Japan, 1991. Southeast Asian J Trop Med Public Health. 1999;30:277–279. [PubMed] [Google Scholar]
- 43.Macdonald WB, Tink AR, Ouvrier RA, Menser MA, de Silva LM, Naim H, Hawkes RA. Japanese encephalitis after a two-week holiday in Bali. Med J Aust. 1989;150:334–336, 339. doi: 10.5694/j.1326-5377.1989.tb136498.x. [DOI] [PubMed] [Google Scholar]
- 44.Hoke CH. History of U.S. military contributions to the study of viral encephalitis. Mil Med. 2005;170:92–105. doi: 10.7205/milmed.170.4s.92. [DOI] [PubMed] [Google Scholar]
- 45.Rose MR, Hughes SM, Gatus BJ. A case of Japanese B encephalitis imported into the United Kingdom. J Infect. 1983;6:261–265. doi: 10.1016/s0163-4453(83)93693-9. [DOI] [PubMed] [Google Scholar]
- 46.Artsob H, Spence L. Imported arbovirus infections in Canada 1974–89. Can J Infect Dis. 1991;2:95–100. doi: 10.1155/1991/678906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Poland JD, Cropp CB, Craven RB, Monath TP. Evaluation of the potency and safety of inactivated Japanese encephalitis vaccine in U.S. inhabitants. J Infect Dis. 1990;161:878–882. doi: 10.1093/infdis/161.5.878. [DOI] [PubMed] [Google Scholar]
- 48.Trillen C. American Chronicles. Zei-da-man; New Yorker: 1985. pp. 61–94. October 7. [Google Scholar]
- 49.World Tourism Organization . Yearbook of Tourism Statistics: Data 2000–2004 [database on CD] Madrid; World Tourism Organization: 2006. p. 2006. [Google Scholar]
- 50.Australian Government Department of Health and Aging National Notifiable Disease Surveillance System. 2009. http://www9.health.gov.au/cda/Source/Rpt_4.cfm Available at. Accessed April 1, 2009.
- 51.Committee to Advise on Tropical Medicine and Travel Statement on protection against Japanese encephalitis. Can Commun Dis Rep. 2008;34:1–13. doi: 10.14745/ccdr.v37i00a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.National Travel Health Network and Centre Japanese Encephalitis. 2008. http://www.nathnac.org/pro/factsheets/japanese_enc.htm Available at. Accessed April 1, 2009.
- 53.Fulford M, Keystone JS. Health risks associated with visiting friends and relatives in developing countries. Curr Infect Dis Rep. 2005;7:48–53. doi: 10.1007/s11908-005-0023-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hartjes LB, Baumann LC, Henriques JB. Travel health risk perceptions an prevention behaviors of US study abroad students. J Travel Med. 2009;16:338–343. doi: 10.1111/j.1708-8305.2009.00322.x. [DOI] [PubMed] [Google Scholar]
- 55.Ompusunggu S, Hills SL, Maha MS, Moniaga VA, Susilarini NK, Widjaya A, Sasmito A, Suwandono A, Sedyaningsih ER, Jacobson JA. Confirmation of Japanese encephalitis as an endemic human disease through sentinel surveillance in Indonesia. Am J Trop Med Hyg. 2008;79:963–970. [PubMed] [Google Scholar]
- 56.Endy TP, Nisalak A. Japanese encephalitis virus: ecology and epidemiology. Curr Top Microbiol Immunol. 2002;267:11–48. doi: 10.1007/978-3-642-59403-8_2. [DOI] [PubMed] [Google Scholar]
- 57.Grossman RA, Edelman R, Gould DJ. Study of Japanese encephalitis virus in Chiangmai Valley, Thailand. VI. Summary and conclusions. Am J Epidemiol. 1974;100:69–76. doi: 10.1093/oxfordjournals.aje.a112010. [DOI] [PubMed] [Google Scholar]
- 58.Ha DQ, Hong VTQ, Loan HT, Thong DQ, Deubel V. Current situation of Japanese encephalitis in the south of Vietnam, 1976–1992. Trop Med. 1994;36:202–214. [Google Scholar]
- 59.Centers for Disease Control and Prevention ACIP Provisional Recommendations for the Use of Japanese Encephalitis Vaccine. 2009.. http://www.cdc.gov/vaccines/recs/provisional/downloads/je-july2009-508.pdf Available at. Accessed September 21, 2009.
- 60.Shlim DR, Solomon T. Japanese encephalitis vaccine for travelers: exploring the limits of risk. Clin Infect Dis. 2002;35:183–188. doi: 10.1086/341247. [DOI] [PubMed] [Google Scholar]
- 61.Office of Tourism Development International Tourist Arrivals, Year 1998–2007. 2009. http://www.tourism.go.th Available at. Accessed April 1, 2009.
- 62.Bali Tourism board Tourist Arrival. 2008. http://www.balitourismboard.org/stat_arrival.html Available at. Accessed April 1, 2009.


