Abstract
This study was conducted to investigate the prevalence of Leptospira species in Mazandaran Province of Iran by using nested polymerase chain reaction (PCR)/restriction fragment length polymorphism (RFLP) methods and sequencing analysis. Blood samples (n = 119) were collected from humans suspected of having leptospirosis from different parts of the province in 2007. By using an indirect immunofluorescent antibody test (IFAT), we determined that 35 (29.4%) of 119 suspected cases had leptospiral antibody titers ≥ 1:80, which confirmed the diagnosis of leptospirosis. Nested PCR assay also determined that 60 (50.4%) of 119 samples showed Leptospira infection. Furthermore, 44 (73.3%) of 60 confirmed leptospirosis amplified products were subjected to sequencing analysis. Sequence alignment identified L. interrogans, L. kirschneri, and L. wolffii species. All positive cases diagnosed by IFAT or PCR were in patients who reported contact with animals, high-risk occupational activities, and exposure to contaminated water. Therefore, it is important to increase attention about this disease among physicians and to strengthen laboratory capacity for its diagnosis in infected patients in Iran.
Introduction
Leptospirosis is a widespread zoonotic disease that is caused by spirochetes of the genus Leptospira. The pathogenic spirochetes are shed in the urine of host animals and human infection can occur through either direct or indirect contact with urine of the infected animals.1 Leptospirosis varies in severity from a mild influenza-like illness to severe and fatal forms. The diagnosis of leptospirosis is confirmed by laboratory investigations based on the serologic response of the host to the infecting organism or by observing the organism from clinical specimens in culture.1 Although recently developed molecular techniques are promising,2,3 serologic analysis continues to be the standard for diagnosis of leptospirosis.
The first report of human leptospirosis in Iran was by Rafyi and Magami in 1968.4 However, the current distribution of leptospirosis of Iran has not reported. The northern provinces of Iran, particularly Guilan and Mazandaran, are ideal areas for transmission of Leptospira because of their humid climate, high population densities, and rural agricultural (mostly rice farming) and fishing activities. Moreover, most farmers in these regions keep domestic animals in their houses and rodents are abundant.
Leptospirosis is a frequently missed diagnosis because clinical symptoms of infection are easily confused with those of other diseases common in Mazandaran Province, such as influenza and viral hepatitis. Thus, leptospirosis remains under-diagnosed in this region. Diagnostic confirmation of cases is usually made by using serologic tests (enzyme-linked immunosorbent assay5 (ELISA) and indirect immunofluorescent antibody test) (IFAT).6–8 In addition, on the basis of clinical evidence, the number of leptosiprosis cases has increased in northern of Iran, including some fatal cases. Therefore, the present investigation was conducted to determine the prevalence of circulating Leptospira species and the frequency of the primary Leptospira species in suspected cases of human leptospirosis in Mazandran Province in Iran by using a recently developed nested polymerase chain reaction (PCR)/restriction fragment length polymorphism (RFLP) analysis and sequencing analysis.
Materials and methods
Study areas and sample collection.
Mazandaran Province is in northern Iran located on the southern coast of the Caspian Sea (Figure 1). It is one of the most densely populated provinces of Iran (population = 2,922,432 in 2006). It has a moderate and humid temperate climate with a plenty of annual rainfall. Mazandaran Province is one of the main tourism areas of Iran, providing a range of activities from fishing, bathing, canoeing, foraging for mushrooms, and hunting. Rice farming, other agriculture, fishing, and cattle husbandry are the main activities in the flat region of this province. In addition to domestic animals, some wild animals live near villages and may carry Leptospira infection. Thus, climate, environment, and socioeconomic conditions are suitable for human leptospirosis in this region.
Figure 1.
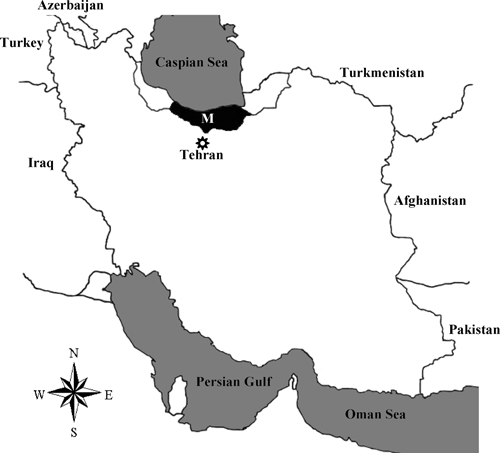
Map of Iran showing study sites. M = Mazandaran Province.
We collected 119 blood samples from persons suspected of having leptospirosis (based on physician diagnosis and the World Health Organization guidelines for diagnosis, surveillance, and control of this disease) from different parts of the province during the transmission season (April–October) in 2007. The suspected patients had a history or clinical manifestations of leptospirosis such as fever and headache or body aches associated with jaundice 2–3 days prior to sampling. These patients were admitted to the general hospitals in different parts of Mazandaran Province. Demographic and clinical information was obtained by patient interviews. Two milliliters of venous blood was collected in sterile tubes, serum was separated from the blood samples, and samples were stored at −20°C and then transferred to the main laboratory in Tehran. Prior to sample collection, written informed consent was obtained from all human adult participants and from the parents or legal guardians of children. This study was reviewed and approved by the Ethical Review Committee of Research in Pasteur Institute of Iran.
Indirect immunofluorescent antibody test.
Antibodies against Leptospira were detected by IFAT6–8 as a routine diagnostic test at the Amol Research Center (branch of the Pasteur Institute of Iran), which is located in Mazandaran Province. The Leptospira antigen from L. interrogans was prepared from culture. Briefly, 1 mL of each culture containing Leptospira was centrifuged at 12,000 × rpm at 4°C for 10 minutes. The pellet was washed with phosphate-buffered saline (PBS), pH 7.4, and resuspended in 1 mL of PBS. Ten microliters of this solution was applied to the wells of clean microscope slides and dried at room temperature. After drying, the slides were kept at −20°C until use. The frozen slides were removed from freezer and left in a wet chamber to thaw. They were then dried and fixed in cold acetone for 10 minutes. Each well on the slides were covered with 20 μL of a 1:10–1:1,280 diluted human serum sample sera and incubated in the wet chamber for 30 minutes. After the slides were washed three times with PBS, pH 7.4, the spaces between the wells were dried, each well was covered with 25 μL of the fluorescein-conjugated anti-human polyvalent IgG (diluted 1:100), and slides were incubated in the wet chamber for 30 min. After the slides were washed three times again with PBS, coverslips were placed on each slide and slides were examined under a fluorescence microscope (E200; Nikon, Tokyo, Japan) at magnification of ×200. Serum samples obtained from healthy persons (n = 15) and two known positive serum samples from humans infected with Leptospira were used as negative and positive controls, respectively.
Nested PCR and PCR/RFLP for 16S ribosomal RNA gene amplification.
Leptospiral genomic DNA was extracted from suspected human serum samples as described.9 The DNA was air-dried, dissolved in TE buffer (10 mM Tris-HCl, pH 8.0, 0.1 mM EDTA), and kept at −20°C until use. The DNA was quantified by agarose gel electrophoresis and spectrophotometrically by calculating the A260/A280 ratios and the A260 values to determine protein impurities and DNA concentrations. Leptospira DNA was amplified by using the primers previously described.9 These primers amplified all pathogenic and non-pathogenic Leptospira species. For the primary and secondary PCR amplification, DNA and the PCR product (1 μL) obtained in the primary reaction were used as the template, respectively.
The PCR was performed in a total volume of 25 μL containing 2 mM MgCl2, 200 μM dNTP mixture (Invitrogen, Carlsbad, CA), 1 unit of Taq polymerase (Invitrogen), and a pair of primers (10 pmol each) for both nested PCRs. The cycling conditions for both reactions were 94°C for 5 minutes; 30 cycles at 60°C for 2 minutes, 72°C for 1.5 minutes, and 94°C for 1 minute; 60°C for 2 minutes; and 72°C for 15 minutes. A negative control containing all the components of the reaction mixture without DNA was used in all nested PCRs. Secondary amplified DNA fragments were separated by electrophoresis on 2% agarose gels and visualized on an ultraviolet transilluminator after staining with ethidium bromide.
Restriction endonuclease analysis of PCR-amplified products.
All secondary PCR products (second nested PCR) were separately digested with ApoI (Invitrogen) according to the manufacturer's instructions. DNA fragments separated by electrophoresis were visualized on an ultraviolet transilluminator after staining with ethidium bromide.
Sequencing analysis.
In this study, a 331 basepairs of 16S ribosomal RNA gene sequences were used for differentiation of Leptospira species. Amplified fragments were gel-purified by using a DNA purification kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions. Direct sequencing of DNA fragments was performed in both directions for each PCR product by using the dideoxy chain termination procedure (Chemistry V3.1; Applied Biosystems, Foster City, CA) and the 3730XL DNA analyzer (Applied Biosystems) at a sequencing service (MilleGen, Labege, France). The forward and reverse primers of the first nested PCR amplification were used for sequencing. Nucleotide sequences reported in this study are available in the European Molecular Biology Laboratory, GenBank, and DNA Data Bank of Japan databases accession numbers GQ501005–GQ501010.
Statistical analysis.
The chi-square test was used to analyze the qualitative variables between leptospirosis and non-leptospirosis groups with respect to clinical signs and symptoms and risk exposures. P values < 0.05 was considered significant. Odds ratios and 95% confidence intervals were used to estimate the association of exposures with the risk for leptospirosis. Statistical analysis was performed by using SPSS software version 15.0 for windows (SPSS Inc., Chicago, IL).
Results
Epidemiologic features.
The median age of participants with suspected leptospirosis was 40 years (range = 13–78 years) and 95 (79.8%) of 119 were men. There were only 2 cases of school age children (13 and 14 years of age) who had been exposed to stagnant water on a farm. Risk factors for all participants are shown in Table 1. All positive cases diagnosed by PCR were patients who had contact with animals, had high-risk occupational activities, and had been exposed to water contaminated with urine of infected animals (P < 0.05) (Table 1). In Mazandaran Province, it is common for agricultural workers to reside in small urban areas and to travel to farms to work. Among confirmed leptospirosis cases detected by PCR, 51 (85%) of 60 were residents in urban areas with occupations in rural settings, exposure to rodents, dogs, or livestock, and contact with contaminated water of a farm with urine of infected animals. The most likely source of infection and the mode of exposure among persons infected with Leptospira were contaminated water and direct contact with livestock or their urine (P < 0.05) (Table 1).
Table 1.
Risk factors for suspected cases of leptospirosos, northern Iran*
| Variable | PCR-confirmed diagnosis (n = 60) | PCR-negative diagnosis (n = 59) | P | Odds ratio (95% CI) | ||
|---|---|---|---|---|---|---|
| No. (%) positive | NA | No. (%) negative | NA | |||
| Age > 30 years | 48 (80) | – | 41 (69.5) | 6 (10) | 0.732 | – |
| Male sex | 46 (76.6) | – | 49 (83) | – | 0.386 | – |
| Exposure to rodents | 15 (25) | – | 10 (17) | 5 (8.5) | 0.404 | – |
| Exposure to dogs | 13 (21.6) | – | 14 (23.7) | 5 (8.5) | 0.593 | – |
| Exposure to livestock | 27 (45) | – | 13 (22) | 4 (6.8) | 0.016 | 2.643 (1.184–5.90) |
| Exposure to contaminated water | 32 (53.3) | – | 15 (25.4) | 5 (8.5) | 0.006 | 2.971 (1.359–6.496) |
| Farmer | 50 (83.3) | – | 24 (40.6) | 7 (11.9) | 0.0001 | 5.833 (2.44–13.93) |
NA = not available; CI = confidence interval.
Clinical features.
From the clinical data available for 119 suspected cases, different symptoms were observed (Table 2). All suspected patients had fever, headache with myalgia, and other symptoms compatible with this disease. A total of 72 (60.5%) of 119 of suspected cases were hospitalized, and 42 (58%) of these persons were diagnosed as having leptospirosis by PCR. Confirmed cases of leptospirosis diagnosed by PCR were predominantly in adult men (76.6%) (Table 1); median age = 44 years (range = 21–73 years). The most common reported symptoms among these men were fever and chills (93.3%), myalgia (81.7%), and jaundice (53.3%) (Table 2). All studied patients recovered after treatment with antibiotics.
Table 2.
Clinical findings of clinically suspected cases of leptospirosis, northern Iran*
| Clinical findings | PCR-confirmed diagnosis (n = 60) | PCR-negative diagnosis (n = 59) | P | ||
|---|---|---|---|---|---|
| No. (%) positive | NA | No. (%) negative | NA | ||
| Fever and chills | 56 (93.3) | – | 50 (84.7) | 5 (8.5) | 0.877 |
| Myalgia | 49 (81.7) | 4 (6.6) | 43 (72.8) | 4 (6.8) | 0.193 |
| Jaundice | 32 (53.3) | – | 17 (28.8) | 5 (8.5) | 0.019 |
| Respiratory symptoms | 11 (18.3) | – | 8 (13.5) | – | 0.477 |
| Renal insufficiency | 19 (31.6) | – | 6 (10) | 2 (3.4) | 0.005 |
| Hemorrhage | 8 (13.3) | – | 8 (13.5) | – | 0.971 |
| Meningeal signs | 5 (8.3) | – | 8 (13.5) | – | 0.361 |
| Abdominal pain | 4 (6.6) | – | 4 (6.8) | – | 0.980 |
| Headache | 6 (10) | – | 1 (1.7) | – | 0.054 |
| Nausea | 4 (6.6) | – | 3 (5) | – | 0.714 |
| Rash | 5 (8.3) | – | 5 (8.5) | – | 0.978 |
NA = not available.
Indirect immunofluorescent antibody test.
Antibodies against Leptospira were detected in 35 (29.4%) of 119 patients. Of these patients, 28 (80%) were greater than 30 years of age and 29 (82.8%) were male patients. Of these 35 patients with suspected cases, 11 had an anti-Leptospira antibody titer of 1:80, 16 had a titer of 1:160, 7 had a titer of 1:320, and 1 had a titer of 1: 640 (Table 3A). The remaining cases had an anti-Leptospira antibody titers < 1:80.
Table 3A.
Serological and PCR diagnosis of leptospirosis by IFAT and PCR, northern Iran*
| Titer | IFAT+/PCR– | IFAT+/PCR+ | Total |
|---|---|---|---|
| 1:80 | 6 | 5 | 11 |
| 1:160 | 7 | 9 | 16 |
| 1:320 | 3 | 4 | 7 |
| 1:640 | – | 1 | 1 |
| Total | 16 | 19 | 35 |
IFAT = indirect immunofluorescent antibody test; PCR = polymerase chain reaction.
Nested PCR/RFLP analysis of clinical samples in suspected cases.
Nested PCR confirmed that 60 (50.4%) of 119 samples harbored Leptospira infections (Table 3B), and RFLP analysis confirmed that all positive cases had a pathogenic Leptospira species. All 15 samples from healthy persons were negative. Comparison of result of PCR and IFAT assays showed that the PCR diagnosed 41 (34.4%) of 119 more infected cases with Leptospira species than IFAT (Table 3B). However, 16 (13.4%) of 119 positive cases diagnosed by the IFAT were negative by the PCR and did not identify any Leptospira DNA in the samples (Table 3B).
Table 3B.
Serological and PCR diagnosis of leptospirosis
| No. (%) | PCR+ | IFAT+ |
|---|---|---|
| 19 (16) | + | + |
| 41 (34.4) | + | − |
| 16 (13.4) | − | + |
| 43 (36.2) | − | − |
| Total = 119 | 60 | 35 |
PCR = polymerase chain reaction; IFAT = indirect immunofluorescent antibody test.
Sequencing.
In the present study, 44 (73.3%) of 60 confirmed leptospirosis amplified products were subjected to sequencing analysis. All samples were sequenced and data confirmed the PCR/RFLP results. BLAST analysis of 16S ribosomal RNA gene sequences from human samples confirmed Leptospira infection. Fourteen sequenced samples were diagnosed as leptosiprosis by PCR and IFAT. However, 30 (68.1%) of 44 samples confirmed by PCR showed a negative titer (< 1:80). Sequence alignment identified L. interrogans, L. kirschneri, and L. wolffii species among 44 confirmed cases. Leptospira kirschneri and L. wolffii species were detected only in samples that showed positive results in the PCR.
On the basis of sequencing analysis, six allelic forms were identified (LPM-1–LPM-6). Alignment of the six allelic forms, of which one of each group were used and submitted to GenBank, are shown in Figure 2. BLAST analysis based on E values showed that LPM-1 (n = 1) has 99% identity with L. interrogans serovars Kremastos (FJ154564) and Canicola (FJ154561); LPM-2 (n = 1) has 99% similarity with L. kirschneri serovars Pomona (FJ154559) and Cynopteri (FJ154546); LPM-3 (n = 1) has 99% identity with L. interrogans serovars Kremastos (FJ154564), Canicola (FJ154561), and Pomona (FJ154544); LPM-4 (n = 1) has 99% identity with L. interrogans serovar Kremastos (FJ154564), Canicola (FJ154561), and Pomona (FJ154544); LPM-5 (n =33) has 99% identity with L. interrogans serovars Kremastos (FJ154564) and Canicola (FJ154561); and LPM-6 (n = 7) has 99% identity with L. wolffii (EF025496) and L. licerasiae serovar Varillal (EF612288).
Figure 2.
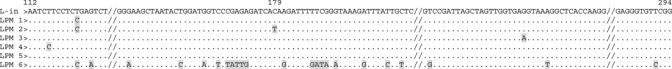
Partial 16S ribosomal RNA nucleotide sequences alignment of the six allelic forms, showing one representative sequence from each group. Sequences were compared with Leptospira interrogans serovar Canicola (AY996798). The representative allelic forms are LPM-1 (n = 1), which has 99% identity with L. interrogans serovars Kremastos (FJ154564) and Canicola (FJ154561); LPM-2 (n = 1), which has 99% identity with L. kirschneri serovars Pomona (FJ154559) and Cynopteri (FJ154546); LPM-3 (n = = 1), which has a 99% identity with L. interrogans serovars Kremastos (FJ154564), Canicola (FJ154561), and Pomona (FJ154544); LPM-4 (n = 1), which has 99% identity with L. interrogans serovar Kremastos (FJ154564), Canicola (FJ154561), and Pomona (FJ154544); LPM-5 (n =33), which has 99% identity with L. interrogans serovars Kremastos (FJ154564) and Canicola (FJ154561); and LPM-6 (n = 7), which has 99% identity with L. wolffii (EF025496) and L. licerasiae serovar Varillal (EF612288). // indicates conserved sequences and dots and dashes indicate identical residues and deletions, respectively.
Discussion
This investigation represents the first molecular epidemiologic study of human leptospirosis in Mazandaran Province in Iran, an area in which leptospirosis is endemic. To date, limited data exist on the human leptospiral infections in Iran. The preliminary aim of this investigation was to study and evaluate the presence and prevalence of Leptospira species in serum samples of suspected cases in humans in Mazandaran Province by using recently developed nested PCR/RFLP methods and sequencing analysis.
On the basis of epidemiologic features, our data indicated that males are affected more than females, which is consistent with data reported in other studies.10–14 The PCR showed that confirmed cases were also more likely to have symptoms such as jaundice and renal insufficiency than non-confirmed cases (P < 0.05). In addition, disease was also related to exposure to contaminated water or animals and patients' occupational activities (P < 0.05). The major occupational risk was among rice farming and cattle husbandry workers. Among the examined cases, 18.5% (22 of 119) used drinking water from wells and 52% of them had confirmed cases of infection with Leptospira diagnosed by PCR. Therefore, drinking water from wells could be considered as one of the infection sources in these areas.
Our results also confirm the presence of high transmission risks for leptospirosis in Mazandaran Province, particularly during the warm and rainy season (April–October), which supports survival of leptospires outside the animal host. This finding is consistent with the season of rice cultivation and the time that visitors come from other parts of Iran to Mazandaran Province. Therefore, the classic history of fever, headache, myalgia with jaundice, and renal insufficiency in suspected cases that have been in contact with rice fields during April–October could indicate leptospirosis in Mazandran Province.
Clinical misdiagnosis and the absence of earlier clinical recognition of leptospirosis may have contributed to the lack of reports of this disease and may have masked the true state of leptospirosis in Mazandaran Province. Definitive laboratory diagnosis of leptospirosis requires detection of the organism in a clinical specimen. In the present study, IFAT and a sensitive nested PCR assay were used to evaluate diagnostic methods for human leptospirosis. The IFAT is only able to detect circulating antibodies 7–10 days after the onset of disease. Maximum titers are observed by the third or fourth weeks,15 and patients remain seropositive for IgG for variable length of time up to 2 years.16–19
The PCR identified 60 (50.4%) of 119 cases of leptospirosis in Mazandaran Province, and serologic analysis identified 35 (29.4%) of 119 cases. Of these 35 serologically confirmed cases, 16 (45.7%) had no genomic DNA of Leptospira and showed false-positive results by PCR. Because all samples were collected 2–4 days after the onset of the disease, results suggested that the PCR is capable of detecting circulating leptospires during the first week of the disease before antibodies are detected in the blood. Our data indicate that the PCR was an efficient tool for early diagnosis of leptospirosis and was able to detect leptospiral DNA in serum samples before circulating antibodies could be detected by serologic analysis. Therefore, we recommended that the PCR should be used with the IFAT (or other serologic methods) in Mazandaran Province.
On the basis of sequencing analysis, L. interrogans (n = 36), L. kirschneri (n = 1), and L. wolffii (n = 7) species were detected among samples tested. Although large epidemiologic surveys in different disease-endemic regions would be useful in understanding the epidemiology of leptospirosis, the presence of L. wolffii in clinical samples must be also considered in control strategies in disease-endemic regions. Control strategies for the disease include improvements in environmental hygiene, control of rodents, and vaccination of domestic animals and persons with occupational and recreational risks of acquiring the disease. However, vaccination may be only partially effective because of the presence of several Leptospira serovars. Therefore, there is little or no cross-protection among serotypes, and vaccinated animals become carriers of the organisms.
Successful vaccination requires epidemiologic studies to provide knowledge of different Leptospira species and serovars that might cause the disease in a given population. In addition, there is evidence of a changing pattern of infections by various Leptospira serovars,20–22 which would affect the control of the disease. Therefore, correct identification of serovars and species is important. Most research has focused on developing techniques to correctly detect infecting serovars, but our findings reinforce the notion that precise detection of infectious species should be considered an important issue in the epidemiology of the disease.
The presence of different Leptospira species in Caspian provinces of Iran (Mazandaran in this study and Guilan)9 is alarming both epidemiologically and clinically. Therefore, further studies are needed to analyze specimens from human and animal cases of infection with Leptospira. In addition, it is epidemiologically important to determine the serogroups and serovars because such information will be essential in designing prevention strategies, such as rodent control measures and avoiding contaminated water and soil. Furthermore, it is important to increase awareness about leptospirosis among physicians in Iran and to strengthen laboratory capacity for its diagnosis in infected patients. Increasing knowledge, particularly in farmers, about leptospirosis and how to protect oneself from the pathogen (e.g., use of protective clothing, avoiding exposure to water or soil contaminated with urine of infected animals, knowledge of the route of transmission) must be considered important factors for disease control.
Acknowledgments
We thank the patients in Mazandran Province for their participation in the study; Zahra Farzaneh Nejad, Galia Amir Bozorgi, Batoul Amin Navaei, and Javad Davoudi for laboratory assistance with the IFAT and collection of clinical samples; and Samaneh Zoghi and Ali Ramezani for statistical analysis
Footnotes
Financial support: This study was supported by research grant no. 320 from the Pasteur Institute of Iran.
Authors' addresses: Sedigheh Zakeri, Neda Sepahian, Mandana Afsharpad, and Navid D. Djadid, Malaria and Vector Research Group (MVRG), Biotechnology Research Center, Pasteur Institute of Iran, Tehran, Iran. Behzad Esfandiari and Peyman Ziapour, Amol Research Center Branch of Pasteur Institute of Iran, Amole, Mazandaran, Iran.
Reprint requests: Sedigheh Zakeri, Biotechnology Research Centre, Pasteur Institute of Iran, Tehran, Iran, E-mails: zakeris@yahoo.com or zakeris@pasteur.ac.ir.
References
- 1.Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, Levett PN, Gilman RH, Willig MR, Gotuzzo E, Vinetz JM. Leptospirosis a zoonotic disease of global importance. Lancet Infect Dis. 2003;3:757–771. doi: 10.1016/s1473-3099(03)00830-2. [DOI] [PubMed] [Google Scholar]
- 2.Mérien F, Amouriaux P, Perolat P, Baranton G, Saint Girons I. Polymerase chain reaction for detection of Leptospira spp. in clinical samples. J Clin Microbiol. 1992;30:2219–2224. doi: 10.1128/jcm.30.9.2219-2224.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Léon A, Pronost S, Tapprest J, Foucher N, Blanchard B, André-Fontaine G, Laugier C, Fortier G, Leclercq R. Identification of pathogenic Leptospira strains in tissues of a premature foal by use of polymerase chain reaction analysis. J Vet Diagn Invest. 2006;18:218–221. doi: 10.1177/104063870601800216. [DOI] [PubMed] [Google Scholar]
- 4.Rafyi A, Magami GH. Leptospirose ovine et caprine. Arch Inst Razi. 1968;20:25–38. [Google Scholar]
- 5.Adler B, Murphy AM, Locarnini SA, Faine S. Detection of specific anti- leptospiral immunoglobulines M and G in human serum by solid-phase enzyme-linked immunosorbent assay. J Clin Microbiol. 1980;11:452–457. doi: 10.1128/jcm.11.5.452-457.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Torten M, Shenberg E, Van der Hoeden J. The use of immunofluorescence in the diagnosis of leptospirosis by a genus-specific antigen. J Infect Dis. 1966;116:537–543. doi: 10.1093/infdis/116.5.537. [DOI] [PubMed] [Google Scholar]
- 7.Udomsakdi S, Potha U. The diagnosis of leptospirosis by fluorescent antibody technique using saprophytic Leptospira as a genus-specific antigen. J Med Assoc Thai. 1972;55:101–104. [PubMed] [Google Scholar]
- 8.Appassakij H, Silpapojakul K, Wansit R, Woodtayakorn J. Evaluation of the immunofluorescent antibody test for the diagnosis of human leptospirosis. Am J Trop Med Hyg. 1995;52:340–343. doi: 10.4269/ajtmh.1995.52.340. [DOI] [PubMed] [Google Scholar]
- 9.Djadid ND, Ganji ZF, Gouya MM, Rezvani M, Zakeri S. A simple and rapid nested polymerase chain reaction-restriction fragment length polymorphism technique for differentiation of pathogenic and nonpathogenic Leptospira spp. Diagn Microbiol Infect Dis. 2009;63:251–256. doi: 10.1016/j.diagmicrobio.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Mansour-Ghanaei F, Sarshad A, Fallah MS, Pourhabibi A, Pourhabibi K, Yousefi-Mashhoor M. Leptospirosis in Guilan, a northern province of Iran: assessment of the clinical presentation of 74 cases. Med Sci Monit. 2005;11:219–223. [PubMed] [Google Scholar]
- 11.Laras K, Cao BV, Bounlu K, Nguyen TK, Olson JG, Thongchanh S, Tran NV, Hoang KL, Punjabi N, Ha BK, Ung SA, Insisiengmay S, Watts DM, Beecham HJ, Corwin AL. The importance of leptospirosis in Southeast Asia. Am J Trop Med Hyg. 2002;67:278–286. doi: 10.4269/ajtmh.2002.67.278. [DOI] [PubMed] [Google Scholar]
- 12.Yersin C, Bovet P, Mérien F, Wong T, Panowsky J, Perolat P. Human leptospirosis in the Seychelles (Indian Ocean): a population-based study. Am J Trop Med Hyg. 1998;59:933–940. doi: 10.4269/ajtmh.1998.59.933. [DOI] [PubMed] [Google Scholar]
- 13.Padre LP, Watt G, Tuazon ML, Gray MR, Laughlin LW. A serologic survey of rice-field leptospirosis in central Luzon, Philippines. Southeast Asian J Trop Med Public Health. 1988;19:197–199. [PubMed] [Google Scholar]
- 14.Ciceroni L, Stepan E, Pinto A, Pizzocaro P, Dettori G, Franzin L, Lupidi R, Mansueto S, Manera A, Ioli A, Marcuccio L, Grillo R, Ciarrocchi S, Cinco M. Epidemiological trend of human leptospirosis in Italy between 1994 and 1996. Eur J Epidemiol. 2000;16:79–86. doi: 10.1023/a:1007658607963. [DOI] [PubMed] [Google Scholar]
- 15.Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14:296–326. doi: 10.1128/CMR.14.2.296-326.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thai KT, Nga TT, Phuong HL, Giao PT, Hung le Q, Binh TQ, Van Nam N, Hartskeerl RA, de Vries PJ. Seroepidemiology and serological follow-up of anti-leptospiral IgG in children in southern Vietnam. Acta Trop. 2008;106:128–131. doi: 10.1016/j.actatropica.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Romero EC, Bernardo CC, Yasuda PH. Human leptospirosis: a twenty-nine-year serological study in São Paulo, Brazil. Rev Inst Med Trop Sao Paulo. 2003;45:245–248. doi: 10.1590/s0036-46652003000500002. [DOI] [PubMed] [Google Scholar]
- 18.Cumberland P, Everard CO, Wheeler JG, Levett PN. Persistence of anti-leptospiral IgM, IgG and agglutinating antibodies in patients presenting with acute febrile illness in Barbados 1979–1989. Eur J Epidemiol. 2001;17:601–608. doi: 10.1023/a:1015509105668. [DOI] [PubMed] [Google Scholar]
- 19.Silva MV, Camargo ED, Batista L, Vaz AJ, Brandão AP, Nakamura PM, Negrão JM. Behaviour of specific IgM, IgG and IgA class antibodies in human leptospirosis during the acute phase of the disease and during convalescence. J Trop Med Hyg. 1995;98:268–272. [PubMed] [Google Scholar]
- 20.Wohl JS. Canine leptospirosis. Compend Contin Educ Pract Vet. 1996;18:1215–1241. [Google Scholar]
- 21.Sasaki DM. Questions stated prevalence of leptospirosis in dogs. J Am Vet Med Assoc. 2002;220:1452–1453. [PubMed] [Google Scholar]
- 22.Aslantas O, Ozdemir V, Kiliç S, Babür C. Seroepidemiology of leptospirosis, toxoplasmosis, and leishmaniosis among dogs in Ankara, Turkey. Vet Parasitol. 2005;129:187–191. doi: 10.1016/j.vetpar.2004.11.037. [DOI] [PubMed] [Google Scholar]


