Abstract
We investigated antidepressant prescriptions and reasons for use. According to our data, the top 10 molecules represent ∼95% of total antidepressant prescriptions for both primary care physicians (PCPs) and psychiatrists. The primary difference between PCPs and psychiatrists was the increased use of buproprion and tricyclics/tetracyclics by psychiatrists. The selective serotonin reuptake inhibitors (SSRIs) and other newer antidepressants such as venlafaxine (Effexor) and buproprion (Wellbutrin) are used to treat depression, anxiety, and bipolar disorders. The noted exception is duloxetine (Cymbalta), which looks like a blend between the newer agents and the tricyclics where there is use beyond the traditional central nervous system (CNS) disorders into pain and migraine.
Keywords: antidepressant, SSRI, tricyclic, psychiatrist, primary care physician, prescription
Introduction
To better understand prescription patterns of antidepressants, we conducted an analysis of antidepressant prescribing by primary care physicians (PCPs) and psychiatrists. We also examined reasons for antidepressant use and looked for variation among different molecules.
Methods
We obtained data from two different sources: 1) quarterly total retail prescriptions of antidepressants from Vector One National (VONA), which captures nearly half of all prescription activity in the US; and 2) annual data from Verispan's Prescription Drug and Diagnosis Audit (PDDA) database regarding reasons for antidepressant use. PDDA captures data on disease state and associated therapy from 3,100 office-based physicians representing 29 specialties across the US.
Results
As seen in Figure 1, the top 10 antidepressants account for approximately 95 percent of total prescriptions for both PCPs and psychiatrists. Sertraline (Zoloft) was the molecule most commonly prescribed by PCPs, while buproprion (Wellbutrin) topped the list for psychiatrists. Outside of buproprion use, the other major difference between PCPs and psychiatrists was the increased use of tricyclics/ tetracyclics by psychiatrists.
Figure 1.
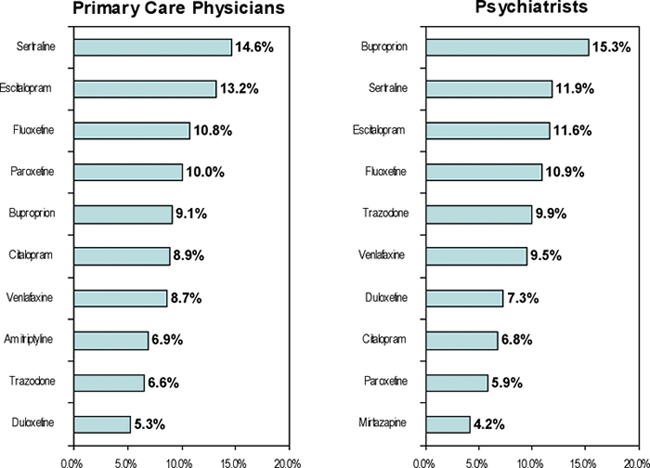
Top 10 antidepressants prescribed, July, 2007, through September, 2007
SOURCE: Verispan VONA, Antidepressant Market, July, 2007, through September, 2007
In Figure 2, we present a summary of the most common reasons for antidepressant use. As seen in Figure 2, the selective serotonin reuptake inhibitors (SSRIs) and other newer antidepressants, such as venlafaxine (Effexor) and buproprion (Wellbutrin), are primarily used to treat depression, anxiety, and bipolar disorders. The noted exception is duloxetine (Cymbalta) where 17 percent of uses are in various pain syndromes as compared to use of only one percent of other SSRI/SNRIs in pain. The trend toward use of antidepressants beyond depression, anxiety, and bipolar disorders is even more pronounced for amitriptyline where only 25 percent of uses were for these central nervous system (CNS) conditions. Similar to duloxetine, amitriptyline is used significantly in various neuropathic and muscular pain conditions (46%) and for migraine (8%).
Figure 2.
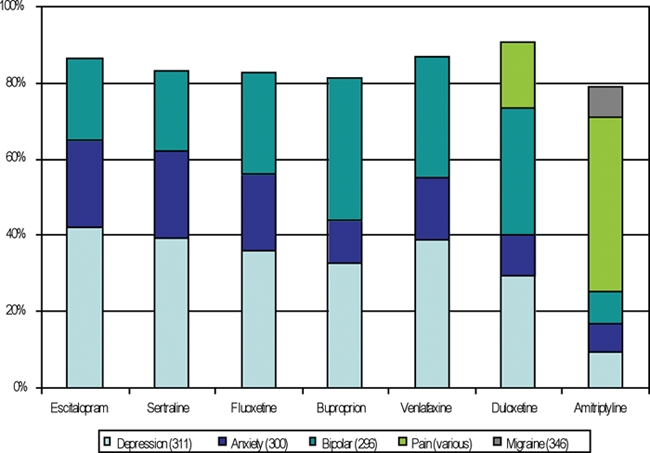
Reasons for Use of Selected Antidepressants
SOURCE: Verispan PDDA, ICD-9 diagnoses associated with selected antidepressants, September, 2006, through August, 2007.
Expert Commentary
The Trend Watch data confirm that there are small, but meaningful differences in the antidepressant prescribing practices of primary care physicians and psychiatrists, which to some extent reflect the differences in the types of patients seen by the two disciplines. The data further documents that a significant minority of prescriptions for this class of medications appear to be for illnesses other than anxiety and depression. The data also dramatically illustrate the current “state of the marketplace” for antidepressants, which no doubt will figure prominently in the planning how new antidepressants will be introduced over the next decade.
With respect to the first point, psychiatrists are much greater prescribers of tricyclic antidepressants (TCAs) and the norepinephrine dopamine reuptake inhibitor bupropion than their primary care colleagues. The TCAs continue to be a time-honored third line of therapy for patients who do not respond to SSRIs, either alone or in combination with a SSRI, which no doubt explains their continued greater use by psychiatrists.1 Results of the STAR*D study did not confirm that TCA nortriptyline was superior to mirtazapine after two courses of newer therapies,2 however, and measures of treatment adequacy, including average daily dose, raise concerns that when TCAs are used, they made not be prescribed vigorously enough. Bupropion accounts for about 15 percent of the antidepressant prescriptions written by psychiatrists, as compared to only about nine percent of those written in primary care. There are several good reasons for this: 1) Bupropion has been a preferred drug for treatment of the depressed phase of bipolar disorder for more than 10 years3 and these patients are more likely to be under the care of a psychiatrist; 2) bupropion is one of the preferred medications for use in combined antidepressant strategies for treatment-resistant depressive syndromes,1 a practice used more often by psychiatrists than primary care physicians;4 and 3) bupropion continues to be used by some physicians as an antidote of sexual dysfunction during therapy with SSRIs and SNRIs, which again is linked to psychiatrists' greater willingness to combine antidepressants. Without a doubt, bupropion is a useful medication and is the only one of the widely prescribed antidepressants that is essentially devoid of sexual side effects.5 Ironically, some of the reasons that psychiatrists preferentially use bupropion have not been supported by the results of recent controlled studies of bipolar depression, in which its efficacy and tolerability were comparable to the SSRIs sertraline6 and paroxetine,7 and no more effective than placebo.7 Likewise, superiority as an adjunctive medication was not demonstrated versus buspirone in STAR*D for management of treatment-resistant,8 nor was the value as an “antidote” for SSRI-induced sexual dysfunction confirmed in one small placebo-controlled study.9
With respect to prescription of antidepressants for clinical indications other than depression and anxiety, it would appear that approximately one fifth of antidepressant use is for some other disorder. One is never sure to what extent these numbers are clouded by artifact (i.e., a physician codes for a concomitant medical disorder, such as irritable bowel syndrome, even though he or she is prescribing to lessen symptoms of anxiety or depression to avoid stigmatizing the patient). Nevertheless, it is also true that two of the antidepressants are truly outliers in this respect: Duloxetine and amitriptyline are both heavily prescribed for patients with various pain syndromes, with amitriptyline also prescribed for a variety of other conditions in the somatic/psychosomatic realm. As duloxetine is the only one of the modern antidepressants to have an official FDA indication for pain management (i.e., management of diabetic neuropathic pain), this is not too surprising, although it is noteworthy that amitriptyline is actually now prescribed far less for depression and anxiety than for other disorders. This perhaps reflects the fact that there are many good alternatives for treatment of uncomplicated anxiety and depression, but few for the common somatoform disorders.
With respect to the current antidepressant marketplace, the data confirm that we are now practicing in an era in which generic medications are prescribed first and, usually, second, before branded medications are considered; this observation is equally true in primary care and psychiatric settings. Indeed, the three still patent-protected antidepressants on the Trend Watch list—escitalopram, venlafaxine XR, and duloxetine—account for little more than a quarter of all prescriptions. As the generic SSRIs and the various generic formulations of bupropion represent reasonably safe and effective inexpensive options, the manufacturers of novel compounds still under development have a relatively exacting target to hit in order to reach commercial success: We need medications that are either significantly more effective (and equally well-tolerated), significantly better tolerated (and equally effective), or effective for an identifiable subset of patients who are not effectively treated by existing standards.
Contributor Information
Elisa F. Cascade, Ms. Cascade is Vice President, Strategic Research and Safety, Quintiles Inc., Falls Church, Virginia
Amir H. Kalali, Dr. Kalali is Vice President, Global Therapeutic Group Leader CNS, Quintiles Inc., San Diego, California, and Professor of Psychiatry, University of California, San Diego.
Michael E. Thase, Dr. Thase is Professor, Departments of Psychiatry, University of Pennsylvania School of Medicine, Philadelphia Veterans Affairs Medical Center, and University of Pittsburgh Medical Center.
References
- 1.Thase ME. Therapeutic alternatives for difficult-to-treat depression: A narrative review of the state of the evidence. CNS Spectr. 2004;9(11):808–21. doi: 10.1017/s1092852900002236. [DOI] [PubMed] [Google Scholar]
- 2.Fava M, Rush AJ, Wisniewski SR, et al. A comparison of mirtazapine and nortriptyline following two consecutive failed medication treatments for depressed outpatients: A STAR*D report. Am J Psychiatry. 2006;163(7):1161–72. doi: 10.1176/ajp.2006.163.7.1161. [DOI] [PubMed] [Google Scholar]
- 3.Kahn DA, Sachs GS, Printz DJ, et al. Medication treatment of bipolar disorder 2000: A summary of the expert consensus guidelines. J Psychiatr Pract. 2000;6(4):197–211. doi: 10.1097/00131746-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Cascade EF, Kalali AH, Blier P. Treatment of depression: Antidepressant monotherapy and combination therapy. Psychiatry. 2007;4(11):25–7. [PMC free article] [PubMed] [Google Scholar]
- 5.Thase ME, Haight BR, Richard N, et al. Remission rates following antidepressant therapy with bupropion or selective serotonin reuptake inhibitors: A meta-analysis of original data from 7 randomized controlled trials. J Clin Psychiatry. 2005;66(8):974–81. doi: 10.4088/jcp.v66n0803. [DOI] [PubMed] [Google Scholar]
- 6.Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry. 2006;189:124–31. doi: 10.1192/bjp.bp.105.013045. [DOI] [PubMed] [Google Scholar]
- 7.Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711–22. doi: 10.1056/NEJMoa064135. [DOI] [PubMed] [Google Scholar]
- 8.Trivedi MH, Fava M, Wisniewski SR, et al. STAR*D Study Team. Medication augmentation after the failure of SSRIs for depression. N Engl J Med. 2006;354(12):124–352. doi: 10.1056/NEJMoa052964. [DOI] [PubMed] [Google Scholar]
- 9.DeBattista C, Solvason B, Poirier J, et al. A placebo-controlled, randomized, double-blind study of adjunctive bupropion sustained release in the treatment of SSRI-induced sexual dysfunction. J Clin Psychiatry. 2005;66(7):844–8. doi: 10.4088/jcp.v66n0706. [DOI] [PubMed] [Google Scholar]


