Abstract
The data from 11,040 patients of the European Cardiovascular Magnetic Resonance (EuroCMR) registry pilot phase offer the first documentation of the clinical use of CMR in a routine setting. The pilot data show that CMR is frequently performed in clinical practice, is a safe procedure with excellent image quality, and has a strong impact on patient management. In the future, the EuroCMR registry will help to set international benchmarks on appropriate indications, quality, and safety of CMR. In addition, outcome and cost effectiveness will be addressed on an international level in order to develop optimized imaging-guided clinical pathways and to avoid unnecessary or even harmful testing.
Keywords: Cardiovascular magnetic resonance, Registry, Quality, Safety, Impact on patient management, Outcome, Effectiveness
Introduction
Cardiovascular imaging is a source of innovation and controversy for the health care community. Rapid technological advances and new clinical applications in cardiovascular imaging technology have led to explosive growth in cardiovascular imaging. However, there are increasing concerns that the rapid dissemination of cardiovascular imaging may cause harm [1, 2], and may be a prime example of a costly technology that is enthusiastically embraced without appropriate supporting scientific evidence. In general, the “value” of cardiac imaging technologies in terms of improved health outcomes or reduced cardiovascular events remains subjective with limited evidence [3, 4]. Furthermore, especially in economically challenging times, considerations like length of stay and cost effectiveness become increasingly important.
In the past decade, cardiovascular magnetic resonance (CMR) has been added to the armamentarium of noninvasive imaging tools. One of the major advantages of CMR is the unique concept of pulse sequences, which can be arranged in a variety of protocols, allowing a greater range of clinical questions to be addressed within a single examination than any other noninvasive imaging technique. Depending on the protocol, CMR can be used for assessment of cardiac morphology, function, ischemia, viability, valves, and great vessels, as well as for myocardial tissue characterization [5–10].
Although the data available from controlled single and multicenter trials are very promising, safety, clinical utility, impact on patient management, and prognostic value of CMR used in daily clinical practice remain unknown. The EuroCMR registry sought to answer these questions and to elucidate the current clinical role of CMR in an international multicenter and multivendor real-life scenario.
Results of the German Pilot Phase
With 11,040 patients from 20 German centers enrolled between April 2007 and January 2009, the pilot phase offers the first possibility to document and investigate the clinical practice of CMR [11].
The most frequent CMR indications were work-up of myocarditis and cardiomyopathies (31.9%), risk stratification in suspected coronary artery disease (CAD)/ischemia testing (30.8%), and viability imaging (14.8%).
In contrast with most previous clinical trials, patients with complicating conditions such as dyspnea at rest, obesity, or atrial fibrillation were not excluded from the registry. Nevertheless, image quality was rated as “good or diagnostic” in more than 98% of studies.
CMR had significant impact on patient management in nearly two thirds of all subjects by direct therapeutic consequences or revealing a completely new diagnosis (16.4%) not suspected before. Notably, in a subgroup of 23% of EuroCMR registry patients with no other imaging test performed prior to CMR, impact on patient management remained equally high without the need for additional imaging procedures post-CMR in the majority of patients (80%) in this subgroup.
In patients (n = 3,351) who underwent stress CMR for work-up of suspected CAD or evaluation of ischemia in known CAD, invasive angiography could be avoided in 45% of cases.
Finally, CMR was a safe procedure in the routine clinical setting with severe complications occurring in 0.05% of patients only, exclusively related to stress testing. Not one patient died during or due to CMR.
Lessons Learned from the Pilot Phase
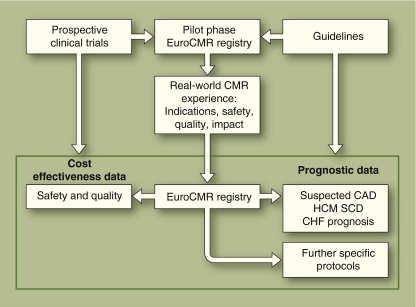
First of all and given the high and increasing number of patients enrolled in the registry, the basic strength of the registry is to constantly redefine and monitor current CMR utilization patterns in a routine clinical setting. At present, work-up of heart failure, CAD, and viability imaging are the major indications for referral to CMR imaging in Germany. However, the registry data also suggest that new indications may grow over time, such as work-up of valvular heart disease prior to percutaneous aortic valve replacement [12], perfusion stress imaging at 3.0 T [13], or interventional CMR related to electrophysiology studies [14]. These data reflecting the distribution of indications in real-life cardiology are essential to monitor the adherence of CMR practitioners to current guidelines and appropriateness criteria for imaging, which is an important part of quality control. Thus, the list of indications derived from the pilot phase datasets of the EuroCMR registry suggests that current clinical CMR practice is in good agreement with the appropriateness criteria [15]. In the future, however, a change in indications may inversely stimulate changes in guidelines or promote new prospective clinical trials (Fig. 1).
Fig. 1.
The role and interaction of the European Cardiovascular Magnetic Resonance (EuroCMR) registry to promote optimized patient management. CAD—coronary artery disease; CHF—congestive heart failure; HCM—hypertrophic cardiomyopathy; SCD—sudden cardiac death. (From Bruder et al. [11]; with permission.)
The second lesson to be learned from the EuroCMR registry is that of procedural quality and safety. The data from the pilot phase clearly indicate that routine CMR performed by cardiologists or radiologists is a safe procedure with very few major complications that are exclusively related to stress testing. Furthermore, the German pilot data demonstrate that image quality is diagnostic in most routine patients without the limitations of strict exclusion criteria as commonly encountered in previous controlled trials.
Launching the second phase of the EuroCMR registry on a European level and later the third phase on an intercontinental level will offer the unique possibility of setting international benchmarks for safety, quality, and cost of CMR imaging. Participating centers in return will be able to constantly challenge the safety and quality of their local setups with these international benchmarks derived from the registry.
The diagnostic performance of CMR has been highlighted by many landmark studies, such as on stress CMR for the detection of CAD [9, 16, 17••], viability imaging [6], or tissue characterization in patients with ischemic or nonischemic cardiomyopathies [8, 18, 19]. The second step to developing effective imaging strategies would be to relate CMR parameters to clinical outcome and to demonstrate their independent prognostic capability in comparison with the established clinical prognosticators in single or multicenter/multivendor trials. As a result of these scientific efforts, preliminary knowledge has been generated about the prognostic impact of stress CMR in patients with known or suspected CAD [20], the extent of late gadolinium enhancement (LGE) as a prognosticator of recovery of function in patients with ischemic heart disease [7], or the presence and extent of LGE in patients with dilated cardiomyopathies [21]. For taking the third step toward an optimal imaging strategy, data are needed on the impact of CMR results on patient management. For the first time, the EuroCMR registry pilot offers this crucial piece of information to CMR imagers around the world. This generates the pilot data’s third lesson, that the clinical effectiveness (accuracy and outcome) of CMR can be translated in a strong impact on patient management. CMR, in the real world, alters patient management by changes in medical treatment, diagnostic procedures, or timing of hospital discharge/admission. Remarkably, in a substantial number of studies CMR offered a completely unexpected and new diagnosis for further clinical decision making, which is in good agreement with the personal experience of many CMR investigators. However, this information has not been available on a scientific basis so far.
Developing optimized clinical pathways for cardiac imaging modalities like CMR inevitably includes the reduction of unnecessary testing, including layer testing and repeat testing. In order to pursue this objective, the EuroCMR registry part one (quality/safety/utility) will also monitor procedures done before and after CMR imaging. On this topic, the pilot data offer new and important information as well:
CMR reduces the need for additional post-test imaging: CMR avoids unnecessary invasive angiography in nearly half of patients undergoing stress CMR. Additional noninvasive imaging involving ionizing radiation (ie, single photon emission CT [SPECT] imaging and CT coronary angiography) is performed only in a minority of patients following CMR. CT and nuclear imaging are the main sources of radiation exposure of the general population in the United States [22]. And although dose reduction algorithms are becoming increasingly available with CT coronary angiography, there is still a broad range of radiation exposure in a real-life international, multicenter, and multivendor setting [23••].
In a subgroup of patients or with specific indications, CMR may serve as the only imaging procedure needed to satisfy all questions of the referrer, which was the case in about 25% of patients in the German pilot phase.
In contrast with clinical trials on new medical or invasive treatment options, patient-focused outcome research in cardiac imaging, answering the ultimate question “does the patient live better and/or longer by using CMR” compared to standard imaging is more challenging for the advanced imaging modalities. However, limiting radiation exposure and invasiveness, a lesson learned from the EuroCMR pilot data, may be regarded as a surrogate parameter for an improvement in patient care and quality of life.
Only after proper investigation of quality, safety, and impact of CMR imaging, trials investigating comparative outcome and cost efficiency can be addressed. An excellent example of a comparative outcome and cost effectiveness trial is the ISCHEMIA trial, which compares stress echocardiography, CMR, and SPECT followed by invasive coronary angiography or optimal medical treatment in patients with suspected CAD. The authors speculate that, given the high effectiveness and clinical utility of CMR, stress CMR without the risk of radiation exposure may turn out to be the cornerstone of a patient-targeted imaging strategy in suspected CAD, replacing SPECT nuclear imaging in the near future.
Conclusions
With growing availability of diagnostic procedures and an increasing need for cost-effective utilization of medical resources, “ordering the right test for the right patient” will be the major challenge for cardiac imaging in the future. To achieve this ambitious goal, scientific knowledge must be generated through interaction of prospective clinical trials, guidelines, and registries (Fig. 1). As only registries finally reflect every day imaging reality, they play an essential role in this process. The EuroCMR registry offers the unique platform for promoting quality and impact of CMR imaging. As the number of participating centers and patient enrollment is constantly growing, the authors are rather optimistic to pursue these objectives on an international level.
Importantly, the EuroCMR registry is open to new specific protocols. Scientists in the field of CMR are encouraged to submit proposals about additional specific protocols to the steering committee. Further details, publications, and the current status of the registry are accessible at www.eurocmr-registry.com.
Acknowledgments
Disclosure
The EuroCMR registry is supported by unrestricted educational grants from the following companies (alphabetical order): Medtronic Inc., Minneapolis, MN; Novartis International AG, Basel, Switzerland; and Siemens Healthcare, Erlangen, Germany.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
Papers of particular interest, published recently, have been highlighted as:••Of major importance
- 1.Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298:317–323. doi: 10.1001/jama.298.3.317. [DOI] [PubMed] [Google Scholar]
- 2.Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 3.Redberg RF. Computed tomographic angiography: more than just a pretty picture? J Am Coll Cardiol. 2007;49:1827–1829. doi: 10.1016/j.jacc.2006.09.056. [DOI] [PubMed] [Google Scholar]
- 4.Shah BR, Patel MR, Peterson ED, et al. Defining optimal research study design for cardiovascular imaging using computed tomography angiography as a model. Am J Cardiol. 2008;102:943–948. doi: 10.1016/j.amjcard.2008.05.037. [DOI] [PubMed] [Google Scholar]
- 5.Klem I, Heitner JF, Shah DJ, et al. Improved detection of coronary artery disease by stress perfusion cardiovascular magnetic resonance with the use of delayed enhancement infarction imaging. J Am Coll Cardiol. 2006;47:1630–1638. doi: 10.1016/j.jacc.2005.10.074. [DOI] [PubMed] [Google Scholar]
- 6.Wagner A, Mahrholdt H, Holly TA, et al. Contrast-enhanced MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet. 2003;361:374–379. doi: 10.1016/S0140-6736(03)12389-6. [DOI] [PubMed] [Google Scholar]
- 7.Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445–1453. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 8.Mahrholdt H, Goedecke C, Wagner A, et al. Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation. 2004;109:1250–1258. doi: 10.1161/01.CIR.0000118493.13323.81. [DOI] [PubMed] [Google Scholar]
- 9.Nagel E, Lehmkuhl HB, Bocksch W, et al. Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of high-dose dobutamine stress MRI: comparison with dobutamine stress echocardiography. Circulation. 1999;99:763–770. doi: 10.1161/01.cir.99.6.763. [DOI] [PubMed] [Google Scholar]
- 10.Pennell DJ, Sechtem UP, Higgins CB, et al. Clinical indications for cardiovascular magnetic resonance (CMR): Consensus Panel report. Eur Heart J. 2004;25:1940–1965. doi: 10.1016/j.ehj.2004.06.040. [DOI] [PubMed] [Google Scholar]
- 11.Bruder O, Schneider S, Nothnagel D, et al. EuroCMR (European Cardiovascular Magnetic Resonance) registry: results of the German pilot phase. J Am Coll Cardiol. 2009;54:1457–1466. doi: 10.1016/j.jacc.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Tops LF, Delgado V, van der Kley F, et al. Percutaneous aortic valve therapy: clinical experience and the role of multi-modality imaging. Heart. 2009;95:1538–1546. doi: 10.1136/hrt.2008.151498. [DOI] [PubMed] [Google Scholar]
- 13.Cheng AS, Pegg TJ, Karamitsos TD, et al. Cardiovascular magnetic resonance perfusion imaging at 3-tesla for the detection of coronary artery disease: a comparison with 1.5-tesla. J Am Coll Cardiol. 2007;49:2440–2449. doi: 10.1016/j.jacc.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 14.Dukkipati SR, Mallozzi R, Schmidt EJ, et al. Electroanatomic mapping of the left ventricle in a porcine model of chronic myocardial infarction with magnetic resonance-based catheter tracking. Circulation. 2008;118:853–862. doi: 10.1161/CIRCULATIONAHA.107.738229. [DOI] [PubMed] [Google Scholar]
- 15.Hendel RC, Patel MR, Kramer CM, et al. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol. 2006;48:1475–1497. doi: 10.1016/j.jacc.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Schwitter J, Nanz D, Kneifel S, et al. Assessment of myocardial perfusion in coronary artery disease by magnetic resonance: a comparison with positron emission tomography and coronary angiography. Circulation. 2001;103:2230–2235. doi: 10.1161/01.cir.103.18.2230. [DOI] [PubMed] [Google Scholar]
- 17.Schwitter J, Wacker CM, van Rossum AC, et al. MR-IMPACT: comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. Eur Heart J. 2008;29:480–489. doi: 10.1093/eurheartj/ehm617. [DOI] [PubMed] [Google Scholar]
- 18.McCrohon JA, Moon JC, Prasad SK, et al. Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation. 2003;108:54–59. doi: 10.1161/01.CIR.0000078641.19365.4C. [DOI] [PubMed] [Google Scholar]
- 19.Mahrholdt H, Wagner A, Deluigi CC, et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006;114:1581–1590. doi: 10.1161/CIRCULATIONAHA.105.606509. [DOI] [PubMed] [Google Scholar]
- 20.Jahnke C, Nagel E, Gebker R, et al. Prognostic value of cardiac magnetic resonance stress tests: adenosine stress perfusion and dobutamine stress wall motion imaging. Circulation. 2007;115:1769–1776. doi: 10.1161/CIRCULATIONAHA.106.652016. [DOI] [PubMed] [Google Scholar]
- 21.Assomull RG, Prasad SK, Lyne J, et al. Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol. 2006;48:1977–1985. doi: 10.1016/j.jacc.2006.07.049. [DOI] [PubMed] [Google Scholar]
- 22.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009;361:849–857. doi: 10.1056/NEJMoa0901249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500–507. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]