Short abstract
Of all clinically marketed drugs, greater than thirty percent are modulators of G protein–coupled receptors (GPCRs). Nearly 400 GPCRs (i.e., excluding odorant and light receptors) are encoded within the human genome, but only a small fraction of these seven-transmembrane proteins have been identified as drug targets. Chronic pain affects more than one-third of the population, representing a substantial societal burden in use of health care resources and lost productivity. Furthermore, currently available treatments are often inadequate, underscoring the significant need for better therapeutic strategies. The expansion of the identified human GPCR repertoire, coupled with recent insights into the function and structure of GPCRs, offers new opportunities for the development of novel analgesic therapeutics.
Abstract
Of all clinically marketed drugs, greater than thirty percent are modulators of G protein–coupled receptors (GPCRs). Nearly 400 GPCRs (i.e., excluding odorant and light receptors) are encoded within the human genome, but only a small fraction of these seven-transmembrane proteins have been identified as drug targets. Chronic pain affects more than one-third of the population, representing a substantial societal burden in use of health care resources and lost productivity. Furthermore, currently available treatments are often inadequate, underscoring the significant need for better therapeutic strategies. The expansion of the identified human GPCR repertoire, coupled with recent insights into the function and structure of GPCRs, offers new opportunities for the development of novel analgesic therapeutics.
Introduction
The G protein–coupled receptors (GPCRs) comprise the largest superfamily of transmembrane receptors. Their function is to transduce extracellular stimuli into intracellular responses. These stimuli can be remarkably diverse, ranging from physical stimuli (e.g., photons or heat) to chemical signals in the form of ions (e.g., Ca2+, H+), chemical neurotransmitters (e.g., dopamine, noradrenaline, adrenaline, acetylcholine, or nucleotides), peptides and protein hormones (e.g., chemokines or opiates), and lipids and eicosanoids (e.g., sphingolipids or leukotrienes). GPCRs mediate and/or modulate virtually all physiological processes in eukaryotic organisms, including acute and chronic pain (1).
Disorders resulting in persistent pain are among the most common forms of chronic illness in North Americans. In individuals age sixty and under, the prevalence of migraine and chronic back pain is ten and fifteen percent, respectively. Arthritis among people less than sixty years of age occurs at a rate of twelve percent, and the frequency rises to forty-six percent for the population that is older than sixty (2). Medical conditions including diabetes, AIDS, and multiple sclerosis all have a high incidence of chronic neuropathic pain. Because pain impairs one’s ability to carry out a productive life, it has serious economic consequences in addition to being a major health problem. In the US alone, an estimated $100 billion is spent each year on health care associated with chronic pain, and an equal amount is further estimated for the related loss of productivity (3, 4). Available therapeutic interventions, such as morphine, are not always able to adequately control pain; not only is drug efficacy at issue, but intolerable side effects, such as sedation, respiratory depression, and gastrointestinal impairment, can also preclude effective pain management. The development of new drugs that target members of the GPCR superfamily holds great promise for the treatment of acute and chronic pain, reaching far beyond the use of traditional opioid receptor agonists.
In this review, we will first provide an overview of GPCR function with regard to the pain signaling system. Second, we will discuss emerging insights into GPCR function that relate to nociceptive transmission. Finally, we will conclude with a brief summary of the role of each GPCR family in nociception.
G Proteins in Signaling
Upon GPCR activation, intracellular signaling systems are activated that couple to a diverse array of downstream effector systems. By definition, signal transduction through GPCRs involves the heterotrimeric GTP-binding proteins (G proteins) to which these receptors are coupled. Current estimates, based on the sequencing of the human genome, predict that the G proteins in human cells can be assembled from among sixteen α, five β, and fourteen γ subunits, with each heterotrimeric combination corresponding to a distinct complement of effector targets (5, 6). The approximately 400 human GPCRs (exclusive of odorant and light receptors) are differentially expressed by specific tissues, allowing for a diversity of signaling cascades that may further be localized with respect to distinct intracellular domains and associated with specific G proteins. In addition, each GPCR may be sensitive to multiple endogenous agonists, and agonists may act at multiple receptor isoforms. Furthermore, data are emerging that GPCRs also elicit G protein–independent intracellular effects, further increasing the spectrum of possibilities (7).
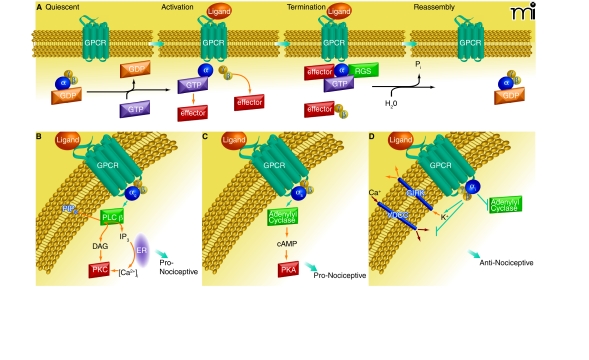
The basic cycle of G protein activation and inactivation is illustrated in Figure 1. Agonist binding and receptor activation induce a conformational change in the heterotrimeric G protein such that the α subunit binds GTP in exchange for GDP, thereby causing the G protein to dissociate into a GTP-bound α monomer and a βγ dimer. The α monomer and βγ dimer are subsequently free to engage target effectors. A mechanism for terminating G–protein signaling to effector systems is built in to the α subunit by means of its intrinsic GTPase activity. Hydrolysis of GTP returns the α subunit to its GDP-bound state, which assembles with the βγ dimer to reform the inactive, heterotrimeric G protein. A number of regulators of G protein signaling, or RGS proteins, enhance the GTPase function of the α subunit and thereby reduce the duration of GPCR signaling. The G protein families primarily involved in the modulation of neurotransmission utilize αs, αi/o, or αq/11 subunits (Figure 1B); members within each family show differences in their patterns of expression (8). Downstream effectors also show isoform-specific intracellular targeting and tissue-specific distribution patterns, providing another level of selectivity in the signaling pathways activated by GPCRs in different cell types.
Figure 1.
Overview of GPCR signaling. A) Diagram of the cycle of G protein activation and inactivation. In the absence of GPCR signaling (Quiescent), G proteins are present as inactive αβγ trimers; the α subunit is bound to GDP. Binding of ligand to GPCR (Activation) causes a conformational change that promotes binding of the receptor to its preferred trimeric G protein and concomitant displacement of bound GDP by incoming GTP at α subunit. Upon GTP binding, the αβγ trimer dissociates into GTP-bound monomer and βγ dimer, each of which can then interact with respective effectors. Signaling is terminated by the GTPase activity of the α subunit; this GTPase activity can be enhanced by RGS proteins. The α subunit–catalyzed hydrolysis of GTP causes subunits to reassemble into the trimeric G protein. The GPCR is generally desensitized and internalized for recycling or destruction (see text). B–D) Diagrams of the canonical signaling pathways for the major G protein families, as described in the text. (ER, endoplasmic reticulum.)
Gs proteins (i.e., heterotrimeric G proteins that possess an αs subunit) exert their effects primarily by activating adenylyl cyclase, resulting in increased intracellular cyclic AMP (cAMP), which in turn activates downstream effectors, including protein kinase A (PKA). Activated PKA phosphorylates numerous proteins that determine the physiological properties of nociceptors (see below). There are also reports that in some cell types, including some nociceptors (sensory neurons that detect noxious stimuli), Gs signaling can lead to activation of protein kinase C (PKC) through the cAMP-activated guanine exchange factor Epac (9, 10). These phosphorylation events are regulated in turn by phosphatases and their downstream substrates. PKA may also activate transcription factors, including the cAMP response element binding protein (CREB), leading to long-term changes in the physiological properties of affected neurons. Gs activation typically results in increased neuronal excitability.
Gi/o proteins mediate the widespread inhibitory effects of many neurotransmitters. Especially significant for the purposes of our discussion, Gi/o proteins also mediate the effects of almost all analgesic GPCR agonists. Several mechanisms account for the inhibitory activity of Gi/o proteins. First, the GTP-bound αi/o subunit inhibits adenyly cyclase, counteracting the effects of Gs activation. Second, the dimer acts to inhibit voltage-dependent calcium channels, resulting in reduced neurotransmitter release and negative regulation of calcium-activated transcription. Third, they directly hyperpolarize neurons by activation of the G protein–gated inwardly rectifying potassium channels (GIRKs), which results in reduced excitability. In addition to affecting channel activity, Gi/o proteins can also modulate neurotransmitter release by interacting directly with release proteins (11). An important function of αi/o subunits is to activate the ERK/MAPK cascade, resulting in regulation of gene expression. [For a comprehensive review of presynaptic signaling by heterotrimeric G proteins, see (12).]
Gq/11 proteins function mainly through phospholipase C beta (PLCβ), of which there are four known isoforms. PLCβ hydrolyzes membrane phosphatidylinositol-4,5-bisphosphate (PIP2) to form IP3, which evokes release of intracellular calcium stores (by activation of IP3 receptors), and diacylglycerol (DAG); both products lead to activation of protein kinase C (PKC). DAG may also activate protein kinase D. Increased intracellular calcium can promote neurotransmitter release at the presynaptic terminal, activates calmodulin-dependent mechanisms (e.g., calcium/calmodulin-dependent protein kinase), and may lead to transcription factor activation. PKC is a major effector for the functional modulation of neuronal signaling machinery downstream of GPCRs. PKCɛ appears to be particularly important in the sensitization of primary afferent nociceptors in response to activation of Gq/11 protein–coupled receptors, but other family members contribute to this process as well (13).
Receptor activation can be terminated by G protein–coupled receptor kinases (GRKs) and arrestins [for review, see (14, 15)]. Following prolonged GPCR activation, GRKs phosphorylate the intracellular loops and C terminus of the receptor, which causes arrestins to associate with the GPCR and promotes receptor internalization. Internalized receptors may be recycled or targeted for degradation by ubiquitination. For many receptors, desensitization and internalization appear to be separate processes; the underlying mechanisms are under investigation (14, 15).
In summary, GPCRs alter neuronal functional properties both by covalent modification of the signaling machinery (e.g., phosphorylation) and transcriptional activation of targeted genes. A basic overview of these pathways is provided in Figure 1. Our knowledge of the diverse pathways activated by GPCRs continues to expand [for review see (16)].
Pain Signaling
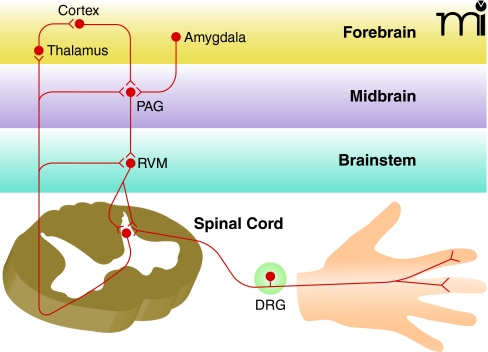
Normal nociceptive transmission (see Box 1) begins when nociceptive axons innervating the target organ (e.g., skin, viscera, or joint) are activated by noxious stimuli. Primary sensory neurons transmit this information from the periphery to the spinal cord dorsal horn, where the nerve impulse is subject to local modulatory control. A subset of postsynaptic spinal neurons (i.e., secondary sensory neurons) send ascending axons to the thalamus, where they relay the information to higher cortical centers. The ascending fibers also send collateral branches into brainstem (i.e., the rostral ventral medulla) and midbrain regions involved in pain modulation (i.e., the periaqueductal grey) and attention and emotion (i.e., the amygdala). These supraspinal centers in turn send descending projections to the spinal cord that can either inhibit or facilitate nociception. Many of the analgesic medications currently available target GPCRs in these descending pathways (17, 18).
Box 1.
Pain vs Nociception
Pain is defined by the International Association for the Study of Pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” In contrast, nociception refers to the transduction of noxious stimuli, irrespective of cognitive awareness. A nociceptor is a sensory neuron preferentially sensitive to a noxious stimulus or to a stimulus which would become noxious if prolonged. Excitatory and inhibitory influences on nociception are referred to as pro- or antinociceptive, respectively. Increases and decreases in the experience of pain are referred to as proalgesic and analgesic, respectively.
In chronic pain conditions, the normal regulation of nociceptive signaling may be altered. For example, inflammatory mediators released by peripheral tissues and immune cells in response to injury act at GPCRs to sensitize peripheral nociceptors (see Box 1), making them more responsive to both noxious and innocuous stimuli. Persistent firing of peripheral nociceptors causes spinal cord neurons to become more responsive to nociceptive input through a process known as central sensitization. Sensitization also occurs at higher-order relays in the brain. Neurons at each step in the pain pathway, both ascending and descending, are subject to modulation by GPCRs that thus represent potential targets for therapeutic intervention into persistent pain. An overview of the pain signaling system is provided in Figure 2.
Figure 2.
Overview of pain transmission. Nociception begins in the periphery with the activation of nociceptive sensory neurons by noxious stimuli (e.g., heat, acid, or tissue injury). These neurons, which have their cell bodies in the dorsal root ganglia (DRG), synapse on neurons in the spinal cord that send ascending projections to the thalamus, which in turn projects to forebrain regions involved in the subjective experience of pain. Descending inhibitory and excitatory pathways are activated by both ascending input from the spinal cord and descending input from the forebrain and limbic structures, including the amygdala. The major structures modulating descending modulation are found in the brainstem rostral ventral medulla (RVM) and midbrain regions [periaqueductal grey, PAG)].
Emerging Concepts in GPCR Signaling and Pain Modulation
GPCR Signaling and Modulation of Peripheral Nociceptive Channels
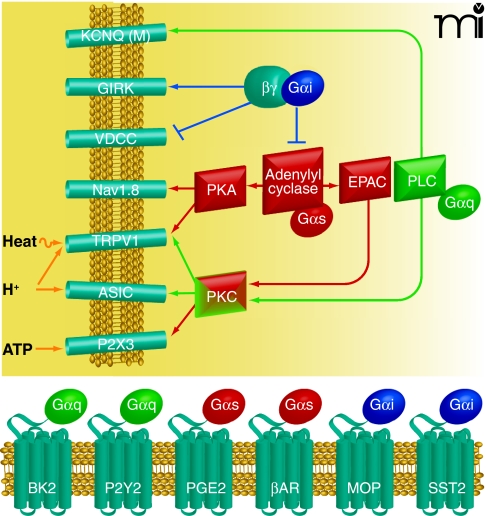
GPCRs modulate the function of a wide variety of ion channels and signaling molecules in sensory neurons, allowing neurons to rapidly adjust their sensitivity in response to changes in peripheral target tissues and at the central synapse. In particular, GPCRs modulate ligand-gated and voltage-dependent ion channels that determine key physiological characteristics of nociceptors (19). These channels include members of the transient receptor potential (TRP) family of ligand-gated cation channels, such as TRPV1 and TRPA1, ATP-gated P2X channels, acid-sensing ion channels (ASICs), TTX-resistant sodium channels, voltage-dependent calcium channels, and M-type potassium channels.
TRPV1, a cation channel gated by heat and protons, is selectively expressed in a subset of primary afferent nociceptors and plays a key role in the sensitization of nociceptors in response to inflammation. Numerous GPCRs have been found to regulate TRPV1 (20, 21). Both Gs and Gq protein–coupled receptor signaling enhance TRPV1 function, resulting in peripheral sensitization of nociceptors and reduced pain threshold. Activation of PKCɛ by Gq signaling plays a major role in the modulation of TRPV1. A related family member, TRPA1, shares many of the same regulatory mechanisms and is largely co-expressed with TRPV1. Several studies suggest that constitutive modulation of TRPV1 by GPCR signaling is required to maintain normal TRPV1 function (20). Additional TRP family members have also been implicated in the transduction of thermal stimuli (21).
P2X3 is a member of the P2X family of ATP-gated ion channels that is preferentially expressed in the non-peptidergic subset of nociceptive sensory neurons. During inflammation, P2X3 currents are enhanced through phosphorylation by PKC. This occurs through an indirect pathway in which the Gs protein–coupled prostaglandin receptor PGE2 acts through Epac1 to activate PKC (9). ASICs are also positively regulated by GPCRs, including serotonin receptors, through the action of PKC. Phosphorylation appears to be selective for the ASIC2b subunit, although it affects currents through heteromeric channels, including those that contain ASIC3 subunits (22). Whereas ASIC2b is expressed by many sensory neurons, ASIC3 is more restricted to peptidergic nociceptors and a subset of larger-diameter neurons of unknown modality (23).
M-type potassium currents, generated by channels consisting of KCNQ subunits, play a key role in regulating nociceptor sensitivity. M-type potassium currents are negatively modulated through Gq protein–mediated signaling; this negative modulation acts to depolarize the resting membrane potential and thereby enhances nociceptive signaling (24). Voltage-dependent calcium channels regulate action potential kinetics and neurotransmitter release as well as neuronal activity–dependent transcription. In nociceptors, these channels contribute significantly to the duration of the action potential. Gi/o protein–coupled receptors such as the opioid receptors inhibit primary afferent signaling in part by inhibiting calcium channels through a direct action of the G protein βγ subunits (25).
Tetrodotoxin-resistant sodium channels Nav1.8 and Nav1.9 are selectively expressed in nociceptors and contribute to injury-evoked changes in neuronal excitability. These channels are modulated through GPCR signaling cascades initiated by inflammatory mediators such as prostaglandins, serotonin, and adenosine (19). Regulation of these sodium channels can occur both through Gs signaling through PKA, which is antagonized by Gi, and by Gq activation of PKC.
Protein Scaffolding and the Organization of Signaling Molecules
The great diversity of GPCR signaling entails a large number of receptors that must evoke selective, often tissue-specific, cellular responses, despite a relatively small complement of G proteins. There is increasing evidence that the functional selectivity of GPCRs is tightly regulated through targeting of signaling components to macromolecular signaling complexes (so-called trans-ducisomes) at specialized membrane compartments known as lipid rafts. Lipid rafts are membrane domains of reduced fluidity, enriched in cholesterol and glycosphingolipids, that promote the assembly of signaling protein complexes (26). These complexes are organized through protein–protein interaction domains (e.g., PDZ, SH2, and SH3 domains) and specialized scaffold proteins that physically coordinate the signaling effector molecules in the transducisome (27). This structural organization allows for highly-efficient regulation of effector function. For example, in some cells, Gq protein–coupled glutamate receptors in the plasma membrane are physically associated with the IP3 receptors on endoplasmic reticulum that regulate calcium stores. This process occurs through binding of the scaffolding protein Homer (28). In nociceptors, some ion channels modulated by G protein signaling are also associated with the transducisome. Examples of channels that are rapidly modulated upon nociceptive GPCR activation and are likely to be associated with scaffolding proteins include the heat- and acid-gated channel TRPV1 and the M-type potassium channel (discussed above) (29).
Available evidence suggests that GPCRs and G proteins are modified by fatty acid acylation, particularly palmitoylation and myristylation, and that these modifications, along with specific polypeptide sequences within the GPCR transmembrane domains, are responsible for directing these proteins to lipid rafts. However, other mechanisms, as yet unidentified, are likely to be important in determining whether a GPCR is targeted to lipid rafts (30). The formation of signaling complexes in lipid rafts provides a mechanism for specialized and highly efficient signal transduction, with pathway selectivity determined by the association of specific effector molecules and receptors through scaffolding proteins.
Integrins are transmembrane proteins associated with lipid rafts and mediate focal adhesions at which the intracellular cytoskeleton connects to extracellular matrix. Integrins contribute to the formation of signaling complexes that are activated in response to binding of extracellular matrix proteins. Studies by Levine and colleagues indicate that integrin binding to the extra-cellular matrix, along with intact lipid rafts, is essential for signaling through a number of GPCRs in inflammatory hyperalgesia (31). The extent to which aberrant nociceptive GPCR signaling or malformation of signaling complexes might underlie persistent pain states is a largely untapped area of investigation.
Ligand-and G Protein–Independent GPCR Signaling
There have been several reports that GPCRs can engage with components of the intracellular signaling complex and activate G protein signaling in the absence of extracellular ligands. Signaling complex components that have been implicated in such interactions include adhesion molecules such as integrins, scaffolding molecules such as Homer, and growth factor receptor tyrosine kinases such as the nerve growth factor receptor TrkA and the epidermal growth factor receptor. This kind of receptor transactivation has been described in both directions; GPCRs may also activate signaling through receptor tyrosine kinases or integrins (16).
In addition, increasing evidence supports the idea that signaling by GPCRs may occur independently of G proteins. The molecules most clearly involved in this process are the β-arrestins, which are widely understood to be involved in the desensitization and recycling of GPCRs. β-arrestins are also able to function as scaffolding molecules for GPCRs and downstream effectors, such as Src tyrosine kinase family members and the MAP kinases, and may actually allow transactivation of these molecules independently of G protein actions (32). However, pathways also exist for the activation of MAP kinases by G protein subunits, suggesting that the pathway used for activation of a specific effector molecule in a given cell type is highly context-dependent (16). These data raise the possibility that there are GPCR-mediated effects in nociceptors that are ligand- and/or G protein–independent (33).
GPCR Oligomerization
It is now recognized that GPCRs, traditionally envisaged monomeric, can form oligomeric complexes. These associations can result in novel pharmacological properties distinct from either component receptor, including alterations in ligand binding affinity, changes in signal transduction, and altered receptor trafficking [for review see (34–37)]. The recognition of oligomeric GCPRs has led to significant re-evaluation of the in vivo mechanisms thought to be involved in GPCR function. Homo- and hetero-oligomerization has been documented within GPCR families, (e.g., the opioid receptor family) and across GPCR families. For example, the functional implications of GPCR–GPCR interactions includes the “unmasking” of opioid binding sites when both the μ- and δ-opioid receptors are co-expressed (38). In addition, the formation of functional GABAB receptors is predicated on a requirement for co-expression of both GABABR1/GABABR2 receptor species (39–41). Although the potential in vivo relevance of these data for neuronal function remains an open question, the existence of oligomers has significant implications for drug development. For example, if the functional receptor is heteromeric, strategies to identify GPCR ligands that rely on cell systems expressing only a single receptor type may not be successful. It is therefore possible that the large number of currently orphaned GPCRs reflects the use of screening paradigms that rely on monomeric rather than heteromeric systems.
Regulation of Cell Surface Expression
The regulation of GPCR internalization and recycling to the cell surface following agonist activation is an area of intense research and has been reviewed extensively elsewhere (42, 43). An interesting new development, with relevance to analgesic drug discovery, is the observation that receptor signaling, internalization, desensitization, and recycling can differ, depending on the specific ligand used (44). This ligand-specific regulation has enormous implications for the development of clinically useful agents with reduced risk of tolerance.
To become functionally competent, GPCRs must be properly synthesized and trafficked to the cell membrane, processes that are under tight cellular control [for review, see (7)]. The cell surface expression of the δ-opioid receptor (DOP) subtype is a case in point. In axon terminals, DOP is associated with large, dense-core vesicles (LDCVs) and in sensory and spinal cord neuron cell bodies, expression is primarily intracellular. In both axons and cell bodies, DOP appears to be inserted into the plasma membrane in a stimulus-dependent manner [see (37, 45, 46)]. DOP may also be translocated in response to chronic morphine exposure, peripheral inflammation, inflammatory mediators, and chronic nociceptive stimuli. As a consequence, sensitivity to DOP agonists is increased. For example, chronic morphine treatment results in an increase both in intrathecal DOP agonist–induced analgesia and in the number of plasma membrane–associated DOP-immunoreactive particles (47).
GPCR Families in Pain Modulation
Early attempts to study, classify, and target GPCRs relied on measurable functional endpoints and on the availability of compounds to selectively stimulate or antagonize those responses. Historically, the modification of these compounds provided the primary approach to the development of new drugs with improved properties. For example, there are at least two dozen different chemical entities in clinical use that target opioid receptors (e.g., morphine and methadone), and most exist in multiple formulations optimized with regard for route of administration or half-life in the plasma. As a result, currently available drugs target only a small fraction of GPCRs.
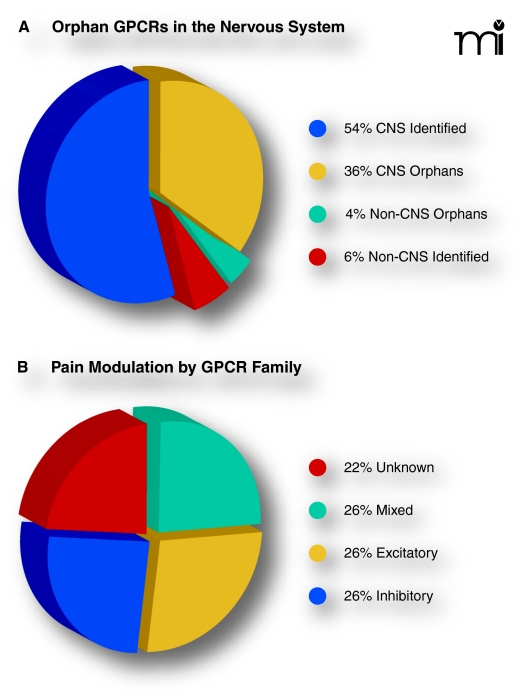
The human genome project has identified more than 800 different GPCRs, approximately half of which are predicted to respond to endogenous (non-light and non-odorant) ligands (48, 49). Of the 379 GPCRs (i.e., exclusive of odorant and light receptors) by the International Union of Basic and Clinical Pharmacology Committee on Receptor Nomenclature and Drug Classification (NC-IUPHAR), an estimated ninety percent are expressed in the central nervous system (50), and nearly forty percent of all GPCRs remain orphans with no identified ligand (49). These numbers predict that over 100 new GPCRs of currently unknown function remain to be identified in the central nervous system, and indeed, new potential targets for drug development have been identified along with previously unknown neurotransmitters. Further insights into GPCR identification and characterization will undoubtedly advance our understanding of pain transmission.
We used the NC-IUPHAR classification system (www.iuphar.org/nciuphar.html) to survey the role(s) of each of the currently proposed GPCR families in pain processing. We were astounded to discover that nearly eighty percent (47/61) of the currently identified families have a known role in the modulation of pain. These survey results speak to the enormous physiological importance of pain modulation by GPCRs. A brief summary of our current understanding of the role of each GPCR family in nociception is provided in Table 1.
Table 1.
GPCR Families and Their G Protein–Dependent Roles in Pro- and Antinociceptive Processing
| GPCR familya | Rolec | Subtype(s) | G protein(s)a, b | Description | Source |
|---|---|---|---|---|---|
| 5-HT (Serotonin) | +/−d | 5-HT1A,B,D,E,F | Gi/o | Descending facilitation and inhibition; peripheral sensitization. 5-HT1 agonists are used to treat migraine. | 17, 51 |
| 5-HT2A,B,C | Gq/11 | ||||
| 5-HT4,5A,6,7 | Gs | ||||
| Acetylcholine (muscarinic) | −e | M2,M5 | Gi/o | Antinociceptive by supraspinal and spinal mechanisms; support analgesic effects of opioid and α2AR agonists. Cholinesterase inhibition (neostigmine) produces analgesia in acute and chronic pain in humans. | 52, 53 |
| M1, M3, M5 | Gq/11 | ||||
| Adenosine | − | A1 | Gi/o | Antinociceptive and antihyperalgesic actions in spinal cord. Systemic agonists elicit severe motor effects, but enzymatic conversion of extracellular AMP to adenosine in the spinal cord produces analgesia without motor effects, suggesting novel approach for analgesic therapeutics. | 54–56 |
| A2A,B | Gs | ||||
| A3 | Gi/o | ||||
| Adrenergic | +/− | α1A,B,D | Gq/11 | α1ARs are pronociceptive, particularly in sympathetic nervous system dysfunction. α2AR agonists have analgesic actions throughout the CNS in acute, inflammatory, and neuropathic pain. βARs are involved in the negative affective component of pain and endogenous pain sensitivity in humans. | 57–60 |
| α2A,B,C | Gi/o | ||||
| β1,2,3 | Gs | ||||
| Angiotensin | +f | AT1 | Gq/11,Gi/o | Supraspinal angiotensin is pronociceptive. Spinal administration appears ineffective. | 61, 62 |
| AT2 | Gi/o | ||||
| Anaphylatoxin | + | C3a | Gi/o | C3a and C5a, components of the activated complement system, mediate neuroimmune function. Blockade of the complement system reduces pain in animal models of acute, inflammatory, and neuropathic pain. | 63–66 |
| C5a | Gi/o, G16 | ||||
| C5L2 | NA | ||||
| Apelin | − | APJ | Gi/o | One study, linking the apelin receptor to nociception, reports that supraspinal administration of apelin-13 produced antinociception and potentiated morphine. | 67 |
| Bile aid | NAg | GPBA | Gs | Bile acids induce visceral pain, but GPBA is not nociceptive per se; levels of GPBA are low in CNS. | 68, 69 |
| Bombesin | +/− | BB1–3 | Gq/11 | Bombesin receptors exist throughout CNS. Supraspinal bombesin receptors produce antinociception, but spinal activation results in hypersensitivity. | 70, 71 |
| Bradykinin | + | B1 | Gi/o, Gq/11 | Peripheral injection of bradykinin causes pain behavior and heat hyperalgesia. B2 is constitutively expressed in sensory neurons. B1 expression is upregulated in response to inflammation, nerve injury, and trophic factor application. | 72–74 |
| B2 | Gs,Gi/0,Gq/11 | ||||
| Calcitonin | +/− | CT, AMY1–3, CGRP, AM1,2w | Gs | CGRP is expressed by a subset of predominantly nociceptive sensory neurons and mediates central and peripheral sensitization and neurogenic inflammation. CGRP antagonists are under exploration as antimigraine agents. Calcitonin is reportedly analgesic in humans. Amylin is expressed by small sensory neurons, implying nociception. Activation of AM receptors in the spinal cord produces heat hyperalgesia. | 75–77 |
| Cannabinoid | − | CB1,2 | Gi/0 | CB1 receptors are expressed in CNS and produce both analgesic and psychoactive effects. CB2 receptors, putatively absent in CNS, inhibit acute, inflammatory, and neuropathic pain. Clinical utility of cannabinoid agonists is under study. | 18, 78, 79 |
| Calcium-sensing | NA | CaS | Gi/o, Gq/11 | Calcium-sensing GPCRs are widespread among neurons, oligodendrocytes, and keratinocytes and respond to extracellular calcium, magnesium, polyamines, L-amino acids, ionic strength, and pH. GPRC6A was identified by genomic screening and is a promiscuous amino acid receptor. | 49 |
| GPRC6 | Gq/11 | ||||
| Chemokine | + | CCR1–10, CXCR1–6, CX3CR1, XCR1 | Gi/0 | Chemokine receptors modulate calcium channel activity through Gi/o. Chemokines have emerged as key modulators of neuropathic and inflammatory chronic pain. Chemokines and their receptors form a link between the immune and nervous systems. | 80–83 |
| Cholecystokinin | + | CCK1,2 | Gq/11 | Activation of CCK receptors has pronociceptive and/or antiopioid activity at several levels along the neuroaxis. | 17, 84 |
| Corticotropin-releasing factor | +/− | CRF1,2 | Gs | Brain CRF receptors are critical to hypothalamic-pituitary axis responses to pain and stress. Acute activation of this system results in analgesia; chronic activation may enhance pain. Many chronic pain states are associated with HPA axis dysfunction. | 85–87 |
| Dopamine | +/− | D1,5 | Gq/11 | Dopamine receptors are widely expressed throughout the brain and contribute to descending pain modulation. Evidence exists for both antinociceptive D2 and pronociceptive D1 actions in spinal cord. | 17, 88 |
| D2–4 | Gi/0 | ||||
| Endothelin | +/− | ETA | Gq/11 | Endothelins are involved in the maintenance of vascular tone. Peripheral ETA activation promotes pain-like behavior; ETB receptor activation is analgesic (possibly by endogenous peripheral opioid activation analgesia. | 89, 90 |
| ETB | Gs,Gi/0,Gq/11 | ||||
| Estrogen | + | GPER | Gs | Previously designated as orphan receptor GPR30, the G protein–coupled estrogen receptor functions autonomously from the steroid receptors ERα and ERβ. GPER is expressed in small sensory neurons; its activation increases CFA-induced allodynia in the masseter muscle. | 91 |
| Formylpeptide | NA | FPR1, FPR2 | Gi/o | Formylpeptide receptors are expressed in brain, spinal cord and peripheral nervous system. A role for the formylpeptide receptors in nociception has not been investigated. | 92 |
| FPR3 | NA | ||||
| Frizzled | NA | FZD1,7 | Gq/11, Gi/o | Frizzled receptors are important in embryonic development and adult tissue homeostasis; their modulation of bone remodelling may have relevance to arthritis. | 93, 94 |
| FZD2,4,6,9,10 | Gi/o | ||||
| FZD3 | Gq/11, Gi/o, Gs | ||||
| FZD5,8 | Gq/11 | ||||
| SMO | NA | ||||
| Free fatty acid | NA | FFA1, FFA2 | Gq/11 | Free fatty acids as ligands for a family of orphan GPCRs is a new concept in cell surface receptor signaling. Fatty acids are involved in the immune response and may be important in neuroimmune interactions; a role in pain remains to be investigated. | 92 |
| FFA3 | Gi/o | ||||
| GPR42 | NA | ||||
| Galanin | − | GAL1,3 | Gi/o | Endogenous galanin modulates spinal nociception primarily in an inhibitory manner and is highly upregulated in sensory neurons following peripheral nerve injury. Galanin is also expressed by neurons that send descending projections to spinal cord. | 17, 95, 96 |
| GAL2 | Gq/11 | ||||
| GABAB | − | GABAB1, GABAB2 | Gi/o | The GABAB agonist baclofen is used clinically to treat pain in patients with spasticity, but also has efficacy in neuropathic, stroke, spinal cord injury, and musculoskeletal pain. | 6, 18 |
| Ghrelin | − | Ghrelin | Gq/11 | Ghrelin has antinociceptive activity following central, systemic, and local peripheral administration. The ghrelin receptor is expressed in the dorsal horn, directly inhibiting spinal neurotransmission. | 97, 98 |
| Glucagon | − | GHRH, GIP, GLP-1, glucagon, secretin | Gs | Neither glucagon or the glucagon-like peptide have been reported to directly modulate nociception; however, activation of the growth hormone–releasing hormone receptor attenuates inflammatory hypersensitivity. Reduced GHRH levels have been associated with fibromyalgia. | 99–101 |
| GLP-2 | NA | ||||
| Glycoprotein hormone | +/− | FSH, LH, TSH | Gs | Acute activation of the hypothalamic-pituitary-adrenal axis results in analgesia; chronic activation may enhance pain. Disturbances in the HPA axis are observed in chronic pain. | 86, 87, 102 |
| Gonadotrophin- releasing hormone | +/− | GnRH | Gq/11 | The GnRH receptor, regulating the biosynthesis and secretion of the gonadotropins, may affect pain thresholds by regulating estrogen and testosterone levels. Altered gonadotropin levels have been detected in spinal fluid from chronic headache patients. | 103, 104 |
| GnRH2 | NA | ||||
| Histamine | + | H1,2 | Gq/11 | Histamine activates nociceptors, releases pronociceptive neuropeptides, and is painful when injected into skin. It contributes to neurogenic inflammaton and peripheral sensitization. H1 receptor antagonists and other antihistaminics are analgesic. Histamine receptors in the CNS may be involved in nociception. | 105 |
| H3,4 | Gi/o | ||||
| KiSS1-derived peptide | NA | KISS1 | Gq/11 | Formerly known as the orphan receptor GPR54, KISS1 is expressed in brain and spinal cord. | 106 |
| Leukotriene | + | BLT1,2, CysLT1,2 | Gq/11, Gi/o | Leukotrienes are pro-inflammatory lipid mediators synthesized by leukocytes, macrophages, and mast cells, and can sensitize nociceptors. | 81, 107–109 |
| OXE | Gi/o | ||||
| Lysophospho-lipid | + | LPA1,2, S1P1–3 | Gi/o | Lysophospholipids, produced by phospholipase C activity, agonize a newly recognized GPCR family. Lysophospholipids contribute to peripheral sensitization via direct action on LPA1 on sensory neurons, produce hyperalgesia if injected intrathecally, and are required for nerve injury–induced hypersensitivity. Sphingolipid S1P receptor activation is implicated in peripheral sensitization. | 110, 111 |
| LPA3 | Gq/11 | ||||
| S1P4,5 | G12 | ||||
| Melatonin | − | MT1,2 | Gi/o | Melatonin receptors are localized in brain and spinal cord; spinal and supraspinal levels of melatonin are antinociceptive in acute, inflammatory, and neuropathic pain. Melatonin inhibits the production of pro-inflammatory cytokines. | 112 |
| Melanocortin | +/− | MC1–5 | Gs | Peptide agonists encoded by the pro-opiomelanocortin POMC gene activate CNS receptors and are reportedly analgesic, hyperalgesic, and anti-opioid. Variants of the MC1 gene are associated with altered pain sensitivity in humans. | 113, 114 |
| Glutamate metabotropic | +/− | mGlu1,5 | Gq/11 | All three groups are expressed throughout CNS. Group I (listed first) is pro-nociceptive and contributes to central sensitization. Group II and III receptors produce analgesia both centrally and in the periphery. | 18, 115 |
| mGlu2,3 | Gi/o | ||||
| mGlu4,6–8 | Gi/o | ||||
| Melanin-concentrating hormone | NA | MCH1 | Gs,Gi/o,Gq/11 | Categorized as orphan receptors prior to 1999, the MCH receptor family is most highly expressed in brain and is implicated in regulating food intake, emotion, stress, and motivation. | 116 |
| MCH2 | Gq/11 | ||||
| Motilin | NA | Motilin | Injection of motilin induces visceral pain behavior reversed by a selective receptor antagonist. Drugs targeting this receptor may be useful for gastrointestinal disorders such as irritable bowel syndrome. | 117, 118 | |
| Neurotensin | +/− | NTS1,2 | Gq/11 | Activation of neurotensin receptors in the brainstem is pronociceptive. In contrast, intrathecal neurotensin produces antinociception via actions on both spinal cord and dorsal root ganglia neurons. Neurotensin knockout mice display defects in both basal nociceptive responses and stress-induced analgesia. | 17, 119 |
| Neuromedin U | + | NMU1 | Gq/11 | Intrathecal administration of neuromedin U causes hyperalgesia. Studies in knockout mice suggest that NMU2 mediates these pronociceptive effects. | 120, 121 |
| NMU2 | NA | ||||
| Neuropeptide S | NA | NPS | NA | The NPS receptor, isolated as an orphan GPCR ligand in 2002, is expressed nearly exclusively in the brain. Central administration of NPS results in increased arousal and an altered anxiolytic profile. | 122, 123 |
| Neuropeptide Y | +/− | Y1,2,5 | Gi.o | After peripheral nerve injury, there is a dramatic increase of NPY in DRG neurons, especially in larger cells. NPY apparently has both pro- and antinociceptive actions, but the antinocicepive actions appear to dominate. | 124, 125 |
| Y4 | Gq/11 | ||||
| Neuropeptide W/Neuropeptide B | − | NPBW1,2 | Gi.o | Neuropeptides B and W were recently identified as endogenous ligands of the GPR7 NPBW1 and GPR8 NPBW2 receptors. Intrathecal injection of either peptide inhibits inflammation-induced mechanical but not thermal hyperalgesia. | 126–128 |
| Neuropeptide FF/neuropeptide AF | +/− | NPFF1,2 | Gi/o | NPFF receptors are present in superficial layers of spinal cord and in brain. Supraspinal injection of NPFF analogs results in pronociceptive and anti-opioid activity; intrathecal injection induces analgesia and enhances opioid effects. | 129, 130 |
| Nicotinic acid | NA | GPR81, GPR109A, GPR109B temporary names | Gi/o | Nicotinic acid was the first orally available drug to treat high cholesterol, but only recently have three GPCRs been identified to recognize this ligand. | 131 |
| Opioid | − | DOP, MOP, KOP, NOP | Gi/o | Activation of DOP, MOP or KOP reduces nociceptive transmission throughout the CNS. Synthetic agonists are common in pain management, but side effects include constipation and respiratory depression. The long-term use of opioids for non-terminal chronic pain is a topic of intense debate. | 18, 132 |
| Orexin | − | OX1 | Gi/o, Gq/11 | In the last decade, orexins were identified as endogenous ligands for two orphan GPCRs. Spinal and supraspinal administration of orexins inhibits nociceptive transmission in acute, inflammatory, and neuropathic pain. | 18 |
| OX2 | Gq/11 | ||||
| P2Y | + | P2Y1,2,4,6,11 | Gq/11 | Gq/11- and Gi/o-coupled P2Y receptors are expressed in sensory neurons, including nociceptors, and glia. P2Y2 mediates thermal sensitivity and inflammatory pain. P2Y12 mediates tactile allodynia after nerve injury. Stimulated keratinocytes release ATP, suggesting a role in sensory transduction. | 20, 133, 134 |
| P2Y12–14 | Gi/o | ||||
| Parathyroid hormone | NA | PTH1,2 | Gs | Parathyroid hormone regulates calcium metabolism and bone growth and remodeling. PTH function in nociception is unclear; its protective effects on bone destruction may reduce arthritic pain. | 135 |
| Platelet-activating factor | + | PAF | Gq/11 | PAF is a lipid mediator of peripheral inflammation; intrathecal injection induces thermal and mechanical hypersensitivity; inhibition of PAF attenuates inflammatory pain. | 136, 137 |
| Prostanoid | + | DP1, EP2,4, IP1 | Gs | The COX enzymes participate in prostaglandin and prostanoid synthesis. Prostanoids commonly act as localized pro-inflammatory/pro-nociceptive mediators. Prostanoid receptors on sensory neurons may cause direct excitation. COX inhibitors mediate analgesia mainly by reducing prostaglandin synthesis. | 81 |
| DP2, EP3 | Gi/o | ||||
| EP1, FP, TP | Gq/11 | ||||
| Prokineticin | + | PKR1 | Gq/11 | The two newly recognized PKRs are expressed by DRG neurons; prokineticin peptides produce hyperalgesia. PKRs on nociceptors mediate heat hyperalgesia by sensitizing TRPV1. PKR1 mediates pain behavior in mice as well as TRPV1 function. | 138–140 |
| PKR2 | Gs | ||||
| Protease-activated | +/− | PAR1,2,4 | Gq/11 | The proteolytic generation of an N-terminal “tethered” receptor-stimulating ligand is unique to PARs. The release of proteinases in arthritis orchestrates joint tissue remodeling and degeneration. Activation of PAR subtypes on sensory neurons can be either pronociceptive (i.e., PAR2) or antinociceptive. PAR2 triggers neuropeptide release, neurogenic inflammation, and TRPV1 sensitization. Sub-inflammatory doses of PAR1 and PAR4 activators reduce inflammatory pain. | 141–143 |
| PAR3 | NA | ||||
| Prolactin-releasing peptide | − | PRRP | Gi/o | PRRP was formerly designated as orphan receptor GPR10. Intracerebral injection of PrRP is normally antinociceptive and reduces allodynia in neuropathic rats. | 144 |
| Relaxin | NA | RXFP1, RXFP2 | Gs, Gi/o | Relaxins modulate the formation of connective tissue. Serum relaxin levels correlate to pelvic pain during pregnancy but more likely reflect the remodeling of pelvic connective tissue rather than a direct role in nociception. | 145 |
| RXFP3, RXFP4 | Gi/o | ||||
| Somatostatin | − | SST1–5 | Gi/o | Somatostatin is expressed in non-peptidergic C-fibers; most SST2 receptors are expressed by TRPV1-containing neurons. Peripheral somatostatin, released upon injury, inhibits neuropeptide release and prevents nociceptor sensitization. Peripheral SST receptors may tonically inhibit TRPV1. Intrathecal administration of agonists inhibits inflammatory and neuropathic pain. | 18, 146, 147 |
| Tachykinin | + | NK1–3 | Gq/11 | Tachykinins (i.e., substance P and neurokinins A and B) are positively implicated in pain modulation. SP and NKA are expressed by small and medium-sized primary sensory neurons. Tachykinins contribute to peripheral and central sensitization. NK1 receptors are expressed by ascending spinal cord neurons; the analgesic inefficacy of NK1 antagonists in humans was unexpected. | 148, 149 |
| Thyrotropin-releasing hormone | − | TRH1 | Gq/11 | TRH receptors can activate descending inhibitory pathways. A systemically administered TRH analog mediates antinociception at the supraspinal level. | 150 |
| Trace amineh | NA | TA1 | Gs | Trace amines are metabolites of biogenic amine neurotransmitters. TA modulation of the CNS was only recently linked GCPR signaling. Of nine family members, eight receptors remain orphans with unidentified ligands; the potential for relevant drug targets is unexplored. Ingested TA can precipitate headaches. | 151, 152 |
| Urotensin | NA | UT | Gq/11 | Urotensin, expressed in brainstem and spinal cord, was recently identified as the ligand for an orphan GPCR. Supraspinal injection reportedly causes anxiogenic and depressant-like effects in mice without altering nociceptive. | 153 |
| Vasopressin/oxytocin | +/− | V1A,1B | Gq/11 | Vasopressin and oxytocin are synthesized in the hypothalamus and stored in vesicles at the posterior pituitary. Although released predominately into the bloodstream, a fraction acts directly in the brain. V1B receptors appear to have pronociceptive and anti-opioid actions, whereas V1A receptors in the spinal cord are analgesic. | 154–156 |
| V2 | Gs | ||||
| OT | Gq/11 | ||||
| VIP/PACAP | + | PAC1, VPAC1,2 | Gs | Vasoactive intestinal peptide and pituitary adenylate cyclise–activating polypeptide are expressed in nociceptive sensory neurons and are upregulated following nerve injury. PAC1 mediates hyperalgesia in inflammatory and neuropathic pain; VIP and PACAP receptor antagonists are analgesic. | 157–159 |
Family name and nomenclature are based on the recommendations of the International Union of Basic and Clinical Pharmacology Committee on Receptor Nomenclature and Drug Classification NC-IUPHAR as of July 2009 (49).
Refers only to each receptors primary or preferred α-subunit as provided by IUPHAR or the selected references. In several cases more than one is listed as equally preferred. Note that most GPCRs will couple to more than one Gα with varying affinity.
A family was considered to be positive if at least one study showing a direct action on nociception was identified. In some of the negative cases, appropriate experiments have not yet been performed.
Mixed effects.
Inhibitory.
Excitatory.
None ascertained.
Trace amine associated receptors, TAAR2–9, are currently classified as orphans.
Conclusions
Regulation of pain transmission by GPCRs occurs throughout the central nervous system, providing a dominant focus for clinical analgesic therapy. However, modulation of nociceptive transduction and processing also occurs in the primary afferent neurons and in peripheral tissues, and all of these sites represent potential targets for novel analgesics. Indeed, it is becoming increasingly clear that GPCRs provide a fundamental mechanism of regulation in an integrated network of communication among sensory axon terminals, their peripheral target tissues, and immune cells (20). The identification of receptors and mechanisms of regulation of GPCRs in pain transmission remains a fertile and largely unexplored field for the development of novel therapeutics for acute and chronic pain, particularly given the paucity of currently available drugs.
Laura S. Stone, PhD, received her doctoral degree at the University of Minnesota and postdoctoral training at the Oregon Health and Sciences University (OHSU). Following a brief interlude in biotechnology, she returned to academia and is currently an Assistant Professor in the Faculty of Dentistry at McGill University. Her research program utilizes both human and pre-clinical models to study synergistic interactions among GPCRs in pain and analgesia. Her work also concerns the etiology and treatment of chronic low back pain. Send correspondence to LSS. Email laura.s.stone@mcgill.ca; fax 514-398-7203.

Derek C. Molliver, PhD, received his doctoral degree at Washington University in St. Louis and postdoctoral training at the Oregon Health and Science University (OHSU). He is currently an Assistant Professor in the Departments of Medicine and Neurobiology at the University of Pittsburgh and a member of the Pittsburgh Center for Pain Research. His interests are focused on mechanisms underlying the regulation of sensory neuron development and functional plasticity by G protein–coupled receptors and neurotrophic factors.
Figure 3.
GPCR modulation of nociceptor excitability. GPCR activation, in response to tissue damage or inflammatory mediators, can often result in the covalent modification (e.g., phosphorylation) of ion channels; such channel modification can modulate important physiological properties of nociceptors. A few examples of GPCRs and ion channels that are involved in the modulation of nociceptor activity are shown (see text for details); many other GPCRs have also been implicated in this process. GPCRs also regulate functional properties of neurons at the level of transcription (not shown here). Channels that are regulated by GPCR activation include the ligand-gated ion channels TRPV1, ASICs, and P2X3; voltage-dependent channels including tetrodotoxin-resistant sodium channels Nav1.8 and Nav1.9; voltage-dependent calcium channels; KCNQ channels mediating the M-type potassium current; and G protein–activated potassium channels (GIRK). GPCR-mediated pathways regulating channel function represent an active area of investigation.
Figure 4.
Current status and opportunities in GPCR targeting. A) Predicted proportions of human GPCRs by nervous system expression (90%) and orphan status (40%). Approximately one-third of all GPCR genes encode orphan receptors that are expressed in the CNS. The endogenous ligand(s) and physiological function(s) of these receptors remain to be discovered, representing enormous opportunities for drug development. B) Modulatory effects of GPCRs organized by family. The equal distribution of inhibitory, excitatory, and mixed functional families suggests an equal balance between pro- and anti-nociception.
Acknowledgments
Acknowledgments
LSS is supported by CIHR MOP-86691 and FRSQ Bourse de chercheur-boursier. DCM is supported by the National Institutes of Health [Grant NS056122].
References
- 1.Römpler H, Stäubert, C, Thor, D, Schulz, A, Hofreiter, M and Schöneberg, T. G protein–coupled time travel: Evolutionary aspects of GPCR research. Mol Interv 7, 17–25 (2007). [DOI] [PubMed] [Google Scholar]
- 2.Rapoport J, Jacobs, P, Bell, NR and Klarenbach, S. Refining the measurement of the economic burden of chronic diseases in Canada. Chronic Dis Can 25, 13–21 (2004.). [PubMed] [Google Scholar]
- 3.McCarberg BH and Billington, R. Consequences of neuropathic pain: Quality-of-life issues and associated costs. Am J Manag Care 12, S263–268 (2006). [PubMed] [Google Scholar]
- 4.Stewart WF, Ricci, JA, Chee, E, Morganstein, D and Lipton, R. Lost productive time and cost due to common pain conditions in the US work-force. JAMA 290, 2443–2454 (2003). [DOI] [PubMed] [Google Scholar]
- 5.Milligan G and Kostenis, E. Heterotrimeric G proteins: A short history. Br J Pharmacol 147, S46–S55 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanders RD, Brian, D and Maze, M. G protein–coupled receptors. Handb Exp Pharmacol 182, 93–117 (2008). [DOI] [PubMed] [Google Scholar]
- 7.Dupre DJ and Hebert, TE. Biosynthesis and trafficking of seven-trans-membrane receptor signalling complexes. Cell Signal 18, 1549–1559 (2006). [DOI] [PubMed] [Google Scholar]
- 8.Offermanns S. G proteins as transducers in transmembrane signalling. Prog Biophys Mol Biol 83, 101–130 (2003). [DOI] [PubMed] [Google Scholar]
- 9.Wang C, Gu, Y, Li, GW and Huang, LY. A critical role of the cAMP sensor Epac in switching protein kinase signalling in prostaglandin E2-induced potentiation of P2X3 receptor currents in inflamed rats. J Physiol 584, 191–203 (2007). This study demonstrated that the pro-inflammatory mediator prostaglandin E2, which activates G protein–coupled prostanoid receptors, produces a large increase in ATP-gated currents. This is an example of GPCR-mediated modulation of ion channel function in sensory neurons and suggests a mechanism contributing to inflammation-induced peripheral sensitization.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hucho TB, Dina, OA and Levine, JD. Epac mediates a cAMP-to-PKC signaling in inflammatory pain: An isolectin B4(+) neuron-specific mechanism. J Neurosci 25, 6119–6126 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kupchik YM, Rashkovan, G, Ohana, L, Keren-Raifman, T, Dascal, N, Parnas, H and Parnas, I. Molecular mechanisms that control initiation and termination of physiological depolarization-evoked transmitter release. Proc Natl Acad Sci USA 105, 4435–4440 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown DA and Sihra, TS. Presynaptic signaling by heterotrimeric G proteins. Handb Exp Pharmacol 18, 207–260 (2008). [DOI] [PubMed] [Google Scholar]
- 13.Khasar SG, Lin, YH, Marti, A, et al. A novel nociceptor signaling pathway revealed in protein kinase C epsilon mutant mice. Neuron 24, 253–260 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tilakaratne N and Sexton, PM. G protein–coupled receptor–protein interactions: Basis for new concepts on receptor structure and function. Clin Exp Pharmacol Physiol 32, 979–987 (2005). [DOI] [PubMed] [Google Scholar]
- 15.Gainetdinov RR, Premont, RT, Bohn, LM, Lefkowitz, RJ and Caron, MG. Desensitization of G protein–coupled receptors and neuronal functions. Annu Rev Neurosci 27, 107–144 (2004). [DOI] [PubMed] [Google Scholar]
- 16.Rozengurt E. Mitogenic signaling pathways induced by G protein–coupled receptors. J Cell Physiol 213, 589–602 (2007). [DOI] [PubMed] [Google Scholar]
- 17.Millan MJ. Descending control of pain. Prog Neurobiol 66, 355–474 (2002). [DOI] [PubMed] [Google Scholar]
- 18.Pan HL, Wu, ZZ, Zhou, HY, Chen, SR, Zhang, HM and Li, DP. Modulation of pain transmission by G protein–coupled receptors. Pharmacol Ther 117, 141–161 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCleskey EW and Gold, MS. Ion channels of nociception. Annu Rev Physiol 61, 835–856 (1999). [DOI] [PubMed] [Google Scholar]
- 20.Dussor G, Koerber, HR, Oaklander, AL, Rice, FL and Molliver, DC. Nucleotide signaling and cutaneous mechanisms of pain transduction. Brain Res Rev 60, 24–35 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patapoutian A, Tate, S and Woolf, CJ. Transient receptor potential channels: Targeting pain at the source. Nat Rev Drug Discov 8, 55–68 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deval E, Salinas, M, Baron, A, Lingueglia, E and Lazdunski, M. ASIC2b-dependent regulation of ASIC3, an essential acid-sensing ion channel subunit in sensory neurons via the partner protein PICK-1. J Biol Chem 279, 19531–19539 (2004). [DOI] [PubMed] [Google Scholar]
- 23.Molliver DC, Immke, DC, Fierro, L, Paré, M, Rice, FL and McCleskey, EW. ASIC3, an acid-sensing ion channel, is expressed in metaboreceptive sensory neurons. Mol Pain 1, 35 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Passmore GM, Selyenko, AA, Mistri, M, et al. KCNQ/M currents in sensory neurons: significance for pain therapy. J Neurosci 23, 7227–7236 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strock J and Diverse-Pierluissi, MA. Ca2+ channels as integrators of G protein-mediated signaling in neurons. Mol Pharmacol 66, 1071–1076 (2004). [DOI] [PubMed] [Google Scholar]
- 26.Insel PA, Head, BP, Patel, HH, Roth, DM, Bundey, RA and Swaney, JS. Compartmentation of G protein–coupled receptors and their signalling components in lipid rafts and caveolae. Biochem Soc Trans 33, 1131–1134 (2005). [DOI] [PubMed] [Google Scholar]
- 27.Pawson T and Scott, JD. Signaling through scaffold, anchoring, and adaptor proteins. Science 278, 2075–2080 (1997). [DOI] [PubMed] [Google Scholar]
- 28.Hoshi N, Langeberg, LK and Scott, JD. Distinct enzyme combinations in AKAP signalling complexes permit functional diversity. Nat Cell Biol 7, 1066–1073 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qanbar R and Bouvier, M. Role of palmitoylation/depalmitoylation reactions in G protein–coupled receptor function. Pharmacol Ther 97, 1–33 (2003). [DOI] [PubMed] [Google Scholar]
- 30.Dina O, Hucho, T, Yeh, J, Malik-Hall, M, Reichling, D and Levine, J. Primary afferent second messenger cascades interact with specific inte-grin subunits in producing inflammatory hyperalgesia. Pain 115, 191–203 (2005). This study was among the first to suggest that integrins play a critical role in inflammatory pain by interacting with components of second messenger cascades that mediate inflammatory hyperalgesia, and that such interactions may be organized by lipid rafts.. [DOI] [PubMed] [Google Scholar]
- 31.Delcourt N, Bockaert, J and Marin, P. GPCR-jacking: From a new route in RTK signalling to a new concept in GPCR activation. Trends Pharmacol Sci 28, 602–607 (2007). [DOI] [PubMed] [Google Scholar]
- 32.Hall RA, Ostedgaard, LS, Premont, RT, Blitzer, JT, Rahman, N, Welsh, MJ and Lefkowitz, RJ. A C-terminal motif found in the beta2-adrenergic receptor, P2Y1 receptor and cystic fibrosis transmembrane conductance regulator determines binding to the Na+/H+ exchanger regulatory factor family of PDZ proteins. Proc Natl Acad Sci USA 95, 8496–8501 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Bartolomeis A and Iasevoli, F. The Homer family and the signal transduction system at glutamatergic postsynaptic density: Potential role in behavior and pharmacotherapy. Psychopharmacol Bull 37, 51–83 (2003). [PubMed] [Google Scholar]
- 34.George SR, O’Dowd, BF and Lee, SP. G protein–coupled receptor oligomerization and its potential for drug discovery. Nat Rev Drug Discov 1, 808–820 (2002). [DOI] [PubMed] [Google Scholar]
- 35.Bulenger S, Marullo, S and Bouvier, M. Emerging role of homo- and heterodimerization in G protein–coupled receptor biosynthesis and maturation. Trends Pharmacol Sci 26, 131–137 (2005). [DOI] [PubMed] [Google Scholar]
- 36.Prinster SC, Hague, C and Hall, RA. Heterodimerization of G protein coupled–receptors: Specificity and functional significance. Pharmacol Rev 57, 289–298 (2005). [DOI] [PubMed] [Google Scholar]
- 37.Milligan G. G protein-coupled receptor hetero-dimerization: Contribution to pharmacology and function. Br J Pharmacol 158, 1–4 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gomes I, Jordan, BA, Gupta, A, Trapaidze, N, Nagy, V and Devi, LA. Heterodimerization of mu and delta opioid receptors: A role in opiate synergy. J Neurosci 20, RC110 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaupmann K, Malitschek, B, Schuler, V, et al. GABA(B)-receptor subtypes assemble into functional heteromeric complexes. Nature 396, 683–687 (1998). [DOI] [PubMed] [Google Scholar]
- 40.White JH, Wise, A, Main, MJ, et al. Heterodimerization is required for the formation of a functional GABA(B) receptor. Nature 396, 679–682 (1998). [DOI] [PubMed] [Google Scholar]
- 41.Jones KA, Borowsky, B, Tamm, JA, et al. GABA(B) receptors function as a heteromeric assembly of the subunits GABA(B)R1 and GABA(B)R2. Nature 396, 674–679 (1998). [DOI] [PubMed] [Google Scholar]
- 42.Drake MT, Shenoy, SK and Lefkowitz, RJ. Trafficking of G protein–coupled receptors. Circ Res 99, 570–582 (2006). [DOI] [PubMed] [Google Scholar]
- 43.Moore CA, Milano, SK and Benovic, JL. Regulation of receptor trafficking by GRKs and arrestins. Annu Rev Physiol 69, 451–482 (2007). [DOI] [PubMed] [Google Scholar]
- 44.Pineyro G and Archer-Lahlou, E. Ligand-specific receptor states: implications for opiate receptor signalling and regulation. Cell Signal 19, 8–19 (2007). [DOI] [PubMed] [Google Scholar]
- 45.Zhang X, Bao, L and Guan, JS. Role of delivery and trafficking of delta-opioid peptide receptors in opioid analgesia and tolerance. Trends Pharmacol Sci 27, 324–329 (2006). [DOI] [PubMed] [Google Scholar]
- 46.Cahill CM, Holdridge, SV and Morinville, A. Trafficking of delta-opioid receptors and other G protein–coupled receptors: Implications for pain and analgesia. Trends Pharmacol Sci 28, 23–31 (2007). [DOI] [PubMed] [Google Scholar]
- 47.Cahill CM, Morinville, A, Lee, MC, Vincent, JP, Collier, B and Beaudet, A. Prolonged morphine treatment targets delta opioid receptors to neuronal plasma membranes and enhances delta-mediated antinociception. J Neurosci 21, 7598–7607 (2001). This study demonstrated an increase in targeting of the delta opioid receptor (DOP)-immunoreactive particles to the plasma membranes of spinal cord neurons following chronic morphine exposure in the absence of neosynthesis. This translocation was associated with a marked potentiation in DOP-mediated spinal antinociception, suggesting that DOP targeting to the plasma membrane may be a mechanism by which opioid receptor activation is regulated in vivo. The regulation of cell surface expression is emerging as an important regulatory mechanism for some GPCRs.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Foord SM, Bonner, TI, Neubig, RR, Rosser, EM, Pin, JP, Davenport, AP, Spedding, M and Harmar, AJ. International Union of Pharmacology. XLVI. G protein–coupled receptor list. Pharmacol Rev 57, 279–288 (2005). [DOI] [PubMed] [Google Scholar]
- 49.Harmar AJ, Hills, RA, Rosser, EM, et al. IUPHAR-DB: The IUPHAR database of G protein–coupled receptors and ion channels. Nucleic Acids Res 37, D680–D685 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vassilatis DK, Hohmann, JG, Zeng, H, et al. The G protein–coupled receptor repertoires of human and mouse. Proc Natl Acad Sci USA 100, 4903–4908 (2003). This study used bioinformatics to describe a total of 367 GPCRs for endogenous ligands in the human genome, including previously unidentified receptors. Expression profiling of 100 of the identified GPCRs demonstrated that the majority are expressed in more than one tissue and over 90% are expressed in the brain. Sequence analysis was used to predict the ligand type for dozens of orphan receptors. This study illustrates the vast untapped potential of uncharacterized GPCRs in neurobiology.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sommer C. Serotonin in pain and analgesia: Actions in the periphery. Mol Neurobiol 30, 117–125 (2004). [DOI] [PubMed] [Google Scholar]
- 52.Eisenach JC. Muscarinic-mediated analgesia. Life Sci 64, 549–554 (1999). [DOI] [PubMed] [Google Scholar]
- 53.Wess J, Duttaroy, A, Gomeza, J, et al. Muscarinic receptor subtypes mediating central and peripheral antinociception studied with muscarinic receptor knockout mice: A review. Life Sci 72, 2047–2054 (2003). [DOI] [PubMed] [Google Scholar]
- 54.Sawynok J. Adenosine receptor activation and nociception. Eur J Pharmacol 347, 1–11 (1998). [DOI] [PubMed] [Google Scholar]
- 55.Gomes JA, Li, X, Pan, HL and Eisenbach, JC. Intrathecal adenosine interacts with a spinal noradrenergic system to produce antinociception in nerve-injured rats. Anesthesiology 91, 1072–1079 (1999). [DOI] [PubMed] [Google Scholar]
- 56.Zylka MJ, Sowa, NA, Taylor-Blake, B, Twomey, MA, Herrala, A, Voikar, V and Vihko, P. Prostatic acid phosphatase is an ectonucleoti-dase and suppresses pain by generating adenosine. Neuron 60, 111–122 (2008). This study demonstrated that a previously unidentified extracellular enzyme localized at nociceptor terminals in the spinal cord represents a mechanism for endogenous analgesia by producing adenosine to act at anti-nociceptive adenosine receptors. The authors devised a novel approach for exploiting this endogenous mechanism by intrathecally injecting soluble enzyme to produce powerful analgesia in chronic pain models..18940592 [Google Scholar]
- 57.Teasell RW and Arnold, JM. Alpha-1 adrenoceptor hyperresponsive-ness in three neuropathic pain states: complex regional pain syndrome 1, diabetic peripheral neuropathic pain and central pain states following spinal cord injury. Pain Res Manag 9, 89–97 (2004). [DOI] [PubMed] [Google Scholar]
- 58.Fairbanks CA, Stone, LS and Wilcox, GL. Pharmacological profiles of alpha 2 adrenergic receptor agonists identified using genetically altered mice and isobolographic analysis. Pharmacol Ther 123, 224–238 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Deyama S, Katayama, T, Ohno, A, Nakagawa, T, Kaneko, S, Yamaguchi, T, Yoshioka, M and Minami, M. Activation of the beta-adrenoceptor-protein kinase A signaling pathway within the ventral bed nucleus of the stria terminalis mediates the negative affective component of pain in rats. J Neurosci 28, 7728–7736 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nackley AG, Tan, KS, Fecho, K, Flood, P, Diatchenko, L and Maixner, W. Catechol-O-methyltransferase inhibition increases pain sensitivity through activation of both beta2- and beta3-adrenergic receptors. Pain 128, 199–208 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Takai S, Song, K, Tanaka, T, Okunishi, H and Miyazaki, M. Antinoci-ceptive effects of angiotensin-converting enzyme inhibitors and an angio-tensin II receptor antagonist in mice. Life Sci 59, PL331–PL336 (1996). [DOI] [PubMed] [Google Scholar]
- 62.Kaneko S, Mori, A, Tamura, S, Satoh, M and Takagi, H. Intracerebro-ventricular administration of angiotensin II attenuates morphine-induced analgesia in mice. Neuropharmacology 24, 1131–1134 (1985). [DOI] [PubMed] [Google Scholar]
- 63.Twining CM, et al. Activation of the spinal cord complement cascade might contribute to mechanical allodynia induced by three animal models of spinal sensitization. J Pain 6, 174–183 (2005). [DOI] [PubMed] [Google Scholar]
- 64.Clark JD, Oiao, Y, Li, X, Shi, X, Angst, MS and Yeomans, DC. Blockade of the complement C5a receptor reduces incisional allodynia, edema, and cytokine expression. Anesthesiology 104, 1274–1282 (2006). [DOI] [PubMed] [Google Scholar]
- 65.Griffin RS, Costigan, M, Brenner, GJ, et al. Complement induction in spinal cord microglia results in anaphylatoxin C5a-mediated pain hypersensitivity. J Neurosci 27, 8699–8708 (2007). This study identified several immune-related components that were highly regulated in spinal cords following peripheral nerve injury including complement component C5 and the C5a receptor (C5aR), which were upregulated in spinal microglia after peripheral nerve injury. Furthermore, intrathecal administration of C5a produced hypersensitivity in naive mice and a C5aR antagonist reduced behavioral signs of neuropathic pain. This study illustrates several important concepts, including the potential importance of non-neuronal targets, the emerging role of neuroimmune interactions in chronic pain, and the ability of new technologies to reveal previously unanticipated roles for GPCRs in pain and analgesia.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ting E, Guerrero, AT, Cunha, TM, et al. Role of complement C5a in mechanical inflammatory hypernociception: Potential use of C5a receptor antagonists to control inflammatory pain. Br J Pharmacol 153, 1043–1053 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xu N, Wang, H, Fan, L and Chen, O. Supraspinal administration of apelin-13 induces antinociception via the opioid receptor in mice. Peptides 30, 1153–1157 (2009). [DOI] [PubMed] [Google Scholar]
- 68.Zhang L, Zhang, X and Westlund, KN. Restoration of spontaneous exploratory behaviors with an intrathecal NMDA receptor antagonist or a PKC inhibitor in rats with acute pancreatitis. Pharmacol Biochem Behav 77, 145–153 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Traub RJ, Tang, B, Ji, Y, Pandya, S, Yfantis, H and Sun, Y. A rat model of chronic postinflammatory visceral pain induced by deoxycholic acid. Gastroenterology 135, 2075–2083 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pert A, Moody, TW, Pert, CB, Dewald, LA and Rivier, J. Bombesin: Receptor distribution in brain and effects on nociception and locomotor activity. Brain Res 193, 209–220 (1980). [DOI] [PubMed] [Google Scholar]
- 71.Cridland RA and Henry, JL. Bombesin, neuromedin C and neuromedin B given intrathecally facilitate the tail flick reflex in the rat. Brain Res 584, 163–168 (1992). [DOI] [PubMed] [Google Scholar]
- 72.Vellani V, Zachrisson, O and McNaughton, PA. Functional bradykinin B1 receptors are expressed in nociceptive neurones and are upregulated by the neurotrophin GDNF. J Physiol 560, 391–401 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang H, Kono, T, Amaya, F, et al. Bradykinin produces pain hypersensitivity by potentiating spinal cord glutamatergic synaptic transmission. J Neurosci 25, 7986–7992 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Prado GN, et al. Mechanisms regulating the expression, self-maintenance, and signaling-function of the bradykinin B2 and B1 receptors. J Cell Physiol 193, 275–286 (2002). [DOI] [PubMed] [Google Scholar]
- 75.Ma W, Chabot, JG and Quirion, R. A role for adrenomedullin as a pain-related peptide in the rat. Proc Natl Acad Sci USA 103, 16027–16032 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tepper SJ and Stillman, MJ. Clinical and preclinical rationale for CGRP-receptor antagonists in the treatment of migraine. Headache 48, 1259–1268 (2008). [DOI] [PubMed] [Google Scholar]
- 77.Gennari C. Analgesic effect of calcitonin in osteoporosis. Bone 30, 67S–70S (2002). [DOI] [PubMed] [Google Scholar]
- 78.Hosking RD and Zajicek, JP. Therapeutic potential of cannabis in pain medicine. Br J Anaesth 101, 59–68 (2008). [DOI] [PubMed] [Google Scholar]
- 79.Malan TP, Ibrahim, MM, Lai, J, Vanderah, TW, Makrivannis, A and Porreca, F. CB2 cannabinoid receptor agonists: Pain relief without psychoactive effects. Curr Opin Pharmacol 3, 62–67 (2003). [DOI] [PubMed] [Google Scholar]
- 80.White FA, Jung, H and Miller, RJ. Chemokines and the pathophysiol-ogy of neuropathic pain. Proc Natl Acad Sci USA 104, 20151–20158 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marchand F, Perretti, M and McMahon, SB. Role of the immune system in chronic pain. Nat Rev Neurosci 6, 521–532 (2005). [DOI] [PubMed] [Google Scholar]
- 82.Scholz J and Woolf, CJ. The neuropathic pain triad: Neurons, immune cells and glia. Nat Neurosci 10, 1361–1368 (2007). [DOI] [PubMed] [Google Scholar]
- 83.Abbadie C. Chemokines, chemokine receptors and pain. Trends Immunol 26, 529–534 (2005). [DOI] [PubMed] [Google Scholar]
- 84.Xie JY, Herman, DS, Stiller, CO, et al. Cholecystokinin in the rostral ventromedial medulla mediates opioid-induced hyperalgesia and anti-nociceptive tolerance. J Neurosci 25, 409–416 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gallagher JP, Orozco-Cabal, LF, Liu, J and Shinnick-Gallagher, P. Synaptic physiology of central CRH system. Eur J Pharmacol 583, 215–225 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bomholt SF, Harbuz, MS, Blackhorn-Monro, G and Blackhorn-Monro, RE. Involvement and role of the hypothalamo-pituitary-adrenal (HPA) stress axis in animal models of chronic pain and inflammation. Stress 7, 1–14 (2004). [DOI] [PubMed] [Google Scholar]
- 87.McFarlane AC. Stress-related musculoskeletal pain. Best Pract Res Clin Rheumatol 21, 549–565 (2007). [DOI] [PubMed] [Google Scholar]
- 88.Potvin S, Grignon, S and Marchand, S. Human evidence of a supra-spinal modulating role of dopamine on pain perception. Synapse 63, 390–402 (2009). [DOI] [PubMed] [Google Scholar]
- 89.Khodorova A, Navarro, B, Jouaville, LS, et al. Endothelin-B receptor activation triggers an endogenous analgesic cascade at sites of peripheral injury. Nat Med 9, 1055–1061 (2003). [DOI] [PubMed] [Google Scholar]
- 90.Khodorova A, Fareed, MU, Gokin, A, Strichartz, GR and Davar, G. Local injection of a selective endothelin-B receptor agonist inhibits endothelin-1-induced pain-like behavior and excitation of nociceptors in a naloxone-sensitive manner. J Neurosci 22, 7788–7796 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liverman CS, Brown, JW, Sandhir, R, McCarson, KE and Berman, NE. Role of the oestrogen receptors GPR30 and ERalpha in peripheral sensitization: Relevance to trigeminal pain disorders in women. Cephalalgia 29, 729–741 (2009). This study reports a pronocicep-tive role for the estrogen receptor GPER (formerly known as the orphan receptor GPR30) in inflammation-induced sensitization. Although the modulatory effects of estrogen on nociception are well described, they had previously been attributed exclusively to the nuclear steroid hormone receptors ERα and ERβ. The discovery of GPER may lead to significant revision of our understanding of estrogen-mediated modulation of nociception. GPER is an excellent example of how GPCR genomics is expected to revolutionize our understanding of CNS modulatory processes.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Becker EL, Forouhar, FA, Grunnet, ML, et al. Broad immunocy-tochemical localization of the formylpeptide receptor in human organs, tissues, and cells. Cell Tissue Res 292, 129–135 (1998). [DOI] [PubMed] [Google Scholar]
- 93.Egger-Adam D and Katanaev, VL. Trimeric G protein–dependent signaling by Frizzled receptors in animal development. Front Biosci 13, 4740–4755 (2008). [DOI] [PubMed] [Google Scholar]
- 94.Luyten FP, Tylzanowski, P and Lories, RJ. Wnt signaling and osteoarthritis. Bone 44, 522–527 (2009). [DOI] [PubMed] [Google Scholar]
- 95.Xu XJ, Hokfelt, T and Wiesenfeld-Hallin, Z. Galanin and spinal pain mechanisms: Where do we stand in 2008. Cell Mol Life Sci 65, 1813–1819 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lundstrom L, Elmquist, A, Bartfai, T and Langel, U. Galanin and its receptors in neurological disorders. Neuromolecular Med 7, 157–180 (2005). [DOI] [PubMed] [Google Scholar]
- 97.Sibilia V, Lattuada, N, Rapetti, D, et al. Ghrelin inhibits inflammatory pain in rats: Involvement of the opioid system. Neuropharmacology 51, 497–505 (2006). [DOI] [PubMed] [Google Scholar]
- 98.Vergnano AM, Ferrini, F, Salio, C, Lassi, L, Baratta, M and Merighi, A. The gastrointestinal hormone ghrelin modulates inhibitory neu-rotransmission in deep laminae of mouse spinal cord dorsal horn. Endocrinology 149, 2306–2312 (2008). [DOI] [PubMed] [Google Scholar]
- 99.Authier F and Desbuquois, B. Glucagon receptors. Cell Mol Life Sci 65, 1880–1899 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Talhouk RS, Saadé, NE, Mouneimne, G, Masaad, CA and Safieh-Garabedian, B. Growth hormone releasing hormone reverses endotoxin-induced localized inflammatory hyperalgesia without reducing the upregulated cytokines, nerve growth factor and gelatinase activity. Prog Neuropsychopharmacol Biol Psychiatry 28, 625–631 (2004). [DOI] [PubMed] [Google Scholar]
- 101.Leal-Cerro A, Povedano, J, Astorga, R, et al. The growth hormone (GH)-releasing hormone-GH-insulin-like growth factor-1 axis in patients with fibromyalgia syndrome. J Clin Endocrinol Metab 84, 3378–3381 (1999). [DOI] [PubMed] [Google Scholar]
- 102.Blackburn-Munro G. Hypothalamo-pituitary-adrenal axis dysfunction as a contributory factor to chronic pain and depression. Curr Pain Headache Rep 8, 116–124 (2004). [DOI] [PubMed] [Google Scholar]
- 103.Elwan O, Abdella, M, el Bayad, AB and Hamdy, S. Hormonal changes in headache patients. J Neurol Sci 106, 75–81 (1991). [DOI] [PubMed] [Google Scholar]
- 104.Hurley RW and Adams, MC. Sex, gender, and pain: An overview of a complex field. Anesth Analg 107, 309–317 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Raffa RB. Antihistamines as analgesics. J Clin Pharm Ther 26, 81–85 (2001). [DOI] [PubMed] [Google Scholar]
- 106.Kotani M, Detheux, M, Vandenbogaerde, A, et al. The metastasis suppressor gene KiSS-1 encodes kisspeptins, the natural ligands of the orphan G protein–coupled receptor GPR54. J Biol Chem 276, 34631–34636 (2001). [DOI] [PubMed] [Google Scholar]
- 107.Funk CD. Prostaglandins and leukotrienes: Advances in eicosanoid biology. Science 294, 1871–1875 (2001). [DOI] [PubMed] [Google Scholar]
- 108.Shimizu T. Lipid mediators in health and disease: enzymes and receptors as therapeutic targets for the regulation of immunity and inflammation. Annu Rev Pharmacol Toxicol 49, 123–150 (2009). [DOI] [PubMed] [Google Scholar]
- 109.Back M. Functional characteristics of cysteinyl-leukotriene receptor subtypes. Life Sci 71, 611–622 (2002). [DOI] [PubMed] [Google Scholar]
- 110.Park KA and Vasko, MR. Lipid mediators of sensitivity in sensory neurons. Trends Pharmacol Sci 26, 571–577 (2005). [DOI] [PubMed] [Google Scholar]
- 111.Anliker B and Chun, J. Cell surface receptors in lysophospholipid signaling. Semin Cell Dev Biol 15, 457–46 (2004). [DOI] [PubMed] [Google Scholar]
- 112.Ambriz-Tututi M, Rocha-Gonzalez, HI, Cruz, SL, et al. Melatonin: A hormone that modulates pain. Life Sci 84, 489–498 (2009). [DOI] [PubMed] [Google Scholar]
- 113.Starowicz K and Przewlocka, B. The role of melanocortins and their receptors in inflammatory processes, nerve regeneration and nocicep-tion. Life Sci 73, 823–847 (2003). [DOI] [PubMed] [Google Scholar]
- 114.Oertel B and Lotsch, J. Genetic mutations that prevent pain: Implications for future pain medication. Pharmacogenomics 9, 179–194 (2008). [DOI] [PubMed] [Google Scholar]
- 115.Neugebauer V. Metabotropic glutamate receptors—important modulators of nociception and pain behavior. Pain 98, 1–8 (2002). [DOI] [PubMed] [Google Scholar]
- 116.Saito Y and Maruyama, K. Identification of melanin-concentrating hormone receptor and its impact on drug discovery. J Exp Zoolog A Comp Exp Biol 305, 761–768 (2006). [DOI] [PubMed] [Google Scholar]
- 117.Sudo H, Yoshida, S, Ozaki, K, et al. Oral administration of MA-2029, a novel selective and competitive motilin receptor antagonist, inhibits motilin-induced intestinal contractions and visceral pain in rabbits. Eur J Pharmacol 581, 296–305 (2008). [DOI] [PubMed] [Google Scholar]
- 118.Scarpignato C and Pelosini, I. Management of irritable bowel syndrome: Novel approaches to the pharmacology of gut motility. Can J Gastroenterol 13, 50A–65A (1999). [DOI] [PubMed] [Google Scholar]
- 119.Dobner PR. Neurotensin and pain modulation. Peptides 27, 2405–2414 (2006). [DOI] [PubMed] [Google Scholar]
- 120.Torres R, Croll, SD, Vercollone, J, et al. Mice genetically deficient in neuromedin U receptor 2, but not neuromedin U receptor 1, have impaired nociceptive responses. Pain 130, 267–278 (2007). [DOI] [PubMed] [Google Scholar]
- 121.Cao CQ, Yu, XH, Dray, A, Filosa, A and Perkins, MN. A pro-nocice-ptive role of neuromedin U in adult mice. Pain 104, 609–616 (2003). [DOI] [PubMed] [Google Scholar]
- 122.Xu YL, Gall, CM, Jackson, VR, Civelli, O and Reinscheid, RK. Distribution of neuropeptide S receptor mRNA and neurochemical characteristics of neuropeptide S-expressing neurons in the rat brain. J Comp Neurol 500, 84–102 (2007). [DOI] [PubMed] [Google Scholar]
- 123.Reinscheid RK, Xu, YL and Civelli, O. Neuropeptide S: A new player in the modulation of arousal and anxiety. Mol Interv 5, 42–46 (2005). [DOI] [PubMed] [Google Scholar]
- 124.Hokfelt T, Brumovsky, P, Shi, T, Pedrazzini, T and Villar, M. NPY and pain as seen from the histochemical side. Peptides 28, 365–372 (2007). [DOI] [PubMed] [Google Scholar]
- 125.Smith PA, Moran, TD, Abdulla, F, Tumber, KK and Taylor, BK. Spinal mechanisms of NPY analgesia. Peptides 28, 464–474 (2007). [DOI] [PubMed] [Google Scholar]
- 126.Hondo M, Ishii, M and Sakurai, T. The NPB/NPW neuropeptide system and its role in regulating energy homeostasis, pain, and emotion. Results Probl Cell Differ 46, 239–256 (2008). [DOI] [PubMed] [Google Scholar]
- 127.Yamamoto T, Saito, O, Koyo, S and Tanabe, S. Anti-hyperalgesic effects of intrathecally administered neuropeptide W-23, and neuropep-tide B, in tests of inflammatory pain in rats. Brain Res 1045, 97–106 (2005). [DOI] [PubMed] [Google Scholar]
- 128.Kelly MA, Beuckmann, CT, Williams, SC, et al. Neuropeptide B-deficient mice demonstrate hyperalgesia in response to inflammatory pain. Proc Natl Acad Sci USA 102, 9942–9947 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yang HY, Tao, T and Iadarola, MJ. Modulatory role of neuropeptide FF system in nociception and opiate analgesia. Neuropeptides 42, 1–18 (2008). [DOI] [PubMed] [Google Scholar]
- 130.Yang HY and Iadarola, MJ. Modulatory roles of the NPFF system in pain mechanisms at the spinal level. Peptides 27, 943–952 (2006). [DOI] [PubMed] [Google Scholar]
- 131.Soudijn W, van Wijngaarden, I and Ijzerman, AP. Nicotinic acid receptor subtypes and their ligands. Med Res Rev 27, 417–433 (2007). [DOI] [PubMed] [Google Scholar]
- 132.Trescot AM, Helm, S, Hansen, H, et al. Opioids in the management of chronic non-cancer pain: An update of American Society of the Interventional Pain Physicians’ (ASIPP) Guidelines. Pain Physician 11, S5–S62 (2008). [PubMed] [Google Scholar]
- 133.Donnelly-Roberts D, McGaraughty, S, Shieh, CC, Honore, P and Jarvis, MF. Painful purinergic receptors. J Pharmacol Exp Ther 324, 409–415 (2008). [DOI] [PubMed] [Google Scholar]
- 134.Tozaki-Saitoh H, Tsuda, M, Miyata, H, Ueda, K, Kohsaka, S and Inoue, K. P2Y12 receptors in spinal microglia are required for neuropathic pain after peripheral nerve injury. J Neurosci 28, 4949–4956 (2008). This study indicates the importance of nucleotide-activated GPCRs in the activation of glial responses to nerve injury that play a critical role in the development of chronic neuropathic pain. The results underscore the importance of glial mechanisms in persistent pain and the potential value of glial GPCRs as therapeutic targets.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nagae M, Hiraga, T, Wakabayashi, H, Wang, L, Iwata, K and Yoneda, T. Osteoclasts play a part in pain due to the inflammation adjacent to bone. Bone 39, 1107–1115 (2006). [DOI] [PubMed] [Google Scholar]
- 136.Morita K, Morioka, N, Abdin, J, Kitayama, S, Nakata, Y and Dohi, T. Development of tactile allodynia and thermal hyperalgesia by intrathe-cally administered platelet-activating factor in mice. Pain 111, 351–359 (2004). [DOI] [PubMed] [Google Scholar]
- 137.Teather LA, Magnusson, JE and Wurtman, RJ. Platelet-activating factor antagonists decrease the inflammatory nociceptive response in rats. Psychopharmacology (Berl) 163, 430–433 (2002). [DOI] [PubMed] [Google Scholar]
- 138.Negri L, Lattanzi, L, Giannini, E and Melchiorri, P. Bv8/Prokineticin proteins and their receptors. Life Sci 81, 1103–1116 (2007). [DOI] [PubMed] [Google Scholar]
- 139.Vellani V, Colucchi, M, Lattanzi, R, et al. Sensitization of transient receptor potential vanilloid 1 by the prokineticin receptor agonist Bv8. J Neurosci 26, 5109–5116 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Negri L, Lattanzi, R, Giannini, E, et al. Impaired nociception and inflammatory pain sensation in mice lacking the prokineticin receptor PKR1: Focus on interaction between PKR1 and the capsaicin receptor TRPV1 in pain behavior. J Neurosci 26, 6716–6727 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hollenberg MD and Compton, SJ. International Union of Pharmacology. XXVIII. Proteinase-activated receptors. Pharmacol Rev 54, 203–217 (2002). [DOI] [PubMed] [Google Scholar]
- 142.Russo A, Soh, UJK and Trejo, J. Proteases display biased agonism at protease-activated receptors: Location matters!. Mol Interv 9, 168–170 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Russell FA and McDougall, JJ. Proteinase activated receptor (PAR) involvement in mediating arthritis pain and inflammation. Inflamm Res 58, 119–126 (2009). [DOI] [PubMed] [Google Scholar]
- 144.Kalliomaki ML, Petrovaara, A, Brandt, A, et al. Prolactin-releasing peptide affects pain, allodynia and autonomic reflexes through medullary mechanisms. Neuropharmacology 46, 412–424 (2004). [DOI] [PubMed] [Google Scholar]
- 145.Kristiansson P, Svardsudd, K and von Schoultz, B. Serum relaxin, symphyseal pain, and back pain during pregnancy. Am J Obstet Gynecol 175, 1342–1347 (1996). [DOI] [PubMed] [Google Scholar]
- 146.Carlton SM, Zhou, S, Du, J, Hargett, G, Ji, G and Coggeshall, R. Somatostatin modulates the transient receptor potential vanilloid 1 (TRPV1) ion channel. Pain 110, 616–627 (2004). This study indicates that Gi protein–coupled somatostatin receptors expressed in peripheral nociceptors inhibit nociceptive signalling and reduce pain behavior. Furthermore, it provides evidence that nociceptive signaling (in this case the action of TRPV1) is under tonic inhibitory regulation by Gi protein–coupled receptors.. [DOI] [PubMed] [Google Scholar]
- 147.Pinter E, Helyes, Z and Szolcsanyi, J. Inhibitory effect of somatostatin on inflammation and nociception. Pharmacol Ther 112, 440–456 (2006). [DOI] [PubMed] [Google Scholar]
- 148.Mantyh PW. Neurobiology of substance P and the NK1 receptor. J. Clin. Psychiatry 63 Suppl_11, 6–11 (2002). [PubMed] [Google Scholar]
- 149.Hill R. NK1 (substance P) receptor antagonists--why are they not analgesic in humans. Trends Pharmacol Sci 21, 244–246 (2000). [DOI] [PubMed] [Google Scholar]
- 150.Tanabe M, Tokuda, Y, Takas, UK, Ono, K, Honda, M and Ono, H. The synthetic TRH analogue taltirelin exerts modality-specific antinociceptive effects via distinct descending monoaminergic systems. Br J Pharmacol 150, 403–414 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lindemann L and Hoener, MC. A renaissance in trace amines inspired by a novel GPCR family. Trends Pharmacol Sci 26, 274–281 (2005). This review discusses the recently identified family of trace amine binding GPCRs. Trace amines are present in the CNS at low levels and are typically metabolic products of the biogenic amine neu-rotransmitters. Although trace amines had been previously linked to neurological disorders, their mechanism of action was unknown. The discovery of this novel family of GPCRs suggests a role for trace amines as neurotransmitters or neuromodulators; these receptors are prime candidates for new drug discovery.. [DOI] [PubMed] [Google Scholar]
- 152.D’Andrea G, Terrazzino, S, Leon, A, et al. Elevated levels of circulating trace amines in primary headaches. Neurology 62, 1701–1705 (2004). [DOI] [PubMed] [Google Scholar]
- 153.Do-Rego JC, Chatenet, D, Orta, MH, et al. Behavioral effects of urotensin-II centrally administered in mice. Psychopharmacology (Berl) 183, 103–117 (2005). [DOI] [PubMed] [Google Scholar]
- 154.Honda K and Takano, Y. New topics in vasopressin receptors and approach to novel drugs: Involvement of vasopressin V1a and V1b receptors in nociceptive responses and morphine-induced effects. J Pharmacol Sci 109, 38–43 (2009). [DOI] [PubMed] [Google Scholar]
- 155.Koshimizu TA and Tsujimoto, G. New topics in vasopressin receptors and approach to novel drugs: Vasopressin and pain perception. J Pharmacol Sci 109, 33–37 (2009). [DOI] [PubMed] [Google Scholar]
- 156.Zingg HH and Laporte, SA. The oxytocin receptor. Trends Endocrinol Metab 14, 222–227 (2003). [DOI] [PubMed] [Google Scholar]
- 157.Dickinson T and Fleetwood-Walker, SM. VIP and PACAP: very important in pain. Trends Pharmacol Sci 20, 324–329 (1999). [DOI] [PubMed] [Google Scholar]
- 158.Jongsma H, Pettersson, LM, Zhang, YZ, et al. Markedly reduced chronic nociceptive response in mice lacking the PAC1 receptor. Neuroreport 12, 2215–2219 (2001). [DOI] [PubMed] [Google Scholar]
- 159.Mabuchi T, Shintani, N, Matsumara, S, et al. Pituitary adenylate cycla-se-activating polypeptide is required for the development of spinal sensitization and induction of neuropathic pain. J Neurosci 24, 7283–7291 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]