Abstract
Purpose
To report on the efficacy of selective laser trabeculoplasty (SLT) for elevated intraocular pressure (IOP) following subtenon injection of triamcinolone acetonide.
Method
SLT was performed on four of 148 eyes in which IOP was elevated after a subtenon injection of triamcinolone acetonide and could not be maintained within normal limits by conventional medications. Postoperative IOP and relative reduction of IOP were evaluated.
Results
IOP was reduced in three eyes to within the normal range without any medications six months after SLT alone, but trabeculotomy was performed on one eye. Percentage reduction in IOP after SLT was 21.6% at one month, 45.0% at three months, and 52.7% at nine months.
Conclusion
SLT may be effective in reducing elevated IOP following subtenon injection of triamcinolone acetonide and should be considered before glaucoma surgery.
Keywords: selective laser trabeculoplasty, steroid glaucoma, subtenon injection, triamcinolone acetonide
Introduction
One complication of intravitreal or subtenon injection of triamcinolone acetonide (SITA) is an elevation of intraocular pressure (IOP).1 Argon laser trabeculoplasty and selective laser trabeculoplasty (SLT) have been used to treat elevated IOP following intravitreal injection of triamcinolone acetonide (IVTA).2,3 However, the elevation of the IOP after SITA is different from that following IVTA because a higher dose is injected which may have a long-lasting effect.4 The effectiveness of SLT following SITA has not been examined. Thus, we have investigated whether SLT is effective in reducing elevated IOP after SITA.
Methods
SITA of 10 or 20 mg was performed on 148 eyes between 2004 and 2006 at the Keio University Hospital. Written informed consent was obtained from all patients before SITA. Institutional approval was obtained for this retrospective clinical review. All patients were followed for at least nine months.
IOP was measured before and after SITA by Goldmann applanation tonometry. SLT was performed when IOP had increased to >26 mmHg with intensive medications, including topical ocular medications and oral acetazolamide. Postoperative IOP and relative reduction of IOP were evaluated.
A Nd:YAG half-wave Q switch laser (SELECTA duet, Japan Lumenis, Tokyo) was used for the SLT at a wavelength at 532 nm, spot size 400 μm, and exposure time of 3 nsec. Forty spots were applied to the inferior 180° sector with an energy of 0.8 to 1.0 mJ, and small gas bubbles were observed after each shot. The preoperative topical and systemic medications were continued postoperatively. Topical hydrochloric apraclonidine was applied 30 minutes before and immediately after the SLT procedure. Anti-inflammatory medications, such as steroid eye drops, were not used.
Results
SITA of 10 or 20 mg was performed for retinal vein occlusion, choroidal neovascularization, or diabetic maculopathy before anti-vascular endothelial growth factor therapy was introduced. IOP increased to >21 mmHg in 44 (30%) of 148 eyes after SITA, and anti-glaucoma medications were used. SLT was performed in four eyes of four patients (one man and three women, mean age 37.5 ± 7.3 years) from two to three months after SITA when the IOP had not decreased after the use of anti-glaucoma medications. In the other 144 eyes, the IOP gradually decreased to baseline IOP in 10 months, with a reduction in the number of anti-glaucoma medications. The IOP before SITA in the four eyes in which SLT was performed ranged between 14 and 19 mmHg. The angle was classified as Shaffer 3 by gonioscopy. There was no evidence of angle neovascularization before SITA and SLT treatment (Table 1). The presence of glaucomatous disc cupping5,6 which was defined as a vertical cup-to-disc ratio >0.7 or a difference in the vertical cup-to-disc ratio between the two eyes >0.2 was not detected before SLT treatment. In addition, a decrease in sensitivity in the visual fields on Humphrey perimetric tests associated with ocular hypertension was also not present before the SLT treatment.
Table 1.
Preoperative condition of patients
| Case | Age | Gender | Baseline IOP (mmHg) | TA injection (mg) | Preop IOP (mmHg) | Preop medication |
|---|---|---|---|---|---|---|
| 1 | 47 | W | 19 | 20 | 27 | PG, beta, CAI |
| 2 | 39 | M | 17 | 20 | 28 | PG, beta, CAI, oral CAI |
| 3 | 34 | W | 17 | 10 | 30 | PG, beta, CAI |
| 4 | 30 | W | 14 | 20 | 35 | PG, beta, CAI, oral CAI |
Abbreviations: F, woman; M, man; IOP, intraocular pressure; PG, latanoprost; beta, 2% hydrochloric carteolol; CAI, topical dorzolamide; oral CAI, systemic acetazolamide; TA, triamcinolone acetonide.
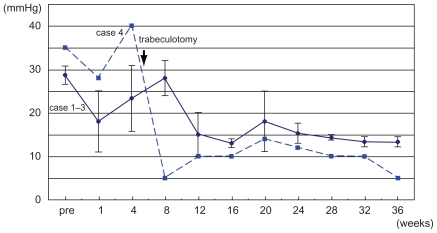
In three eyes, the mean ± standard deviation of the IOP before the SLT was 28.7 ± 2.1 mmHg, and the postoperative mean IOP was 23.3 mmHg at one month, 28.0 mmHg at two months, 15.0 mmHg at three months, 15.3 mmHg at six months, and 13.3 mmHg at nine months. The percentage reduction in IOP was 21.6% ± 16.9%, 6.0% ± 7.2%, 45.0% ± 26.9%, 48.0% ± 14.1%, and 52.7% ± 3.0% at the corresponding times. IOP in case 4 increased to 40 mmHg at four weeks after SLT and trabeculotomy (incision into Schlemm’s canal ab externo) was performed.7 In all cases, the ocular anti-hypertensive medications were discontinued after six months.
Discussion
SLT has been performed for open angle glaucoma, ocular hypertension, and steroid-induced glaucoma3,8 because it is less damaging to the trabecular meshwork.9 SLT was reported to reduce the mean IOP by 30% (7.7 ± 3.5 mmHg) for eyes with primary open-angle glaucoma.10 In our three eyes with a good response to SLT, IOP was reduced by 52.7% ± 3.0% at nine months, which was greater than that for eyes with primary open-angle glaucoma. SLT may be more effective for steroid-induced glaucoma after IVTA.3
It is possible that the disappearance of the drug from the subtenon space may have lowered the IOP. However, the typical increase in IOP response after IVTA has been reported to occur within one week in early cases but, in general, the increase in IOP peaks after a few months with a gradual decline to baseline between six to nine months after the injection.1,11–13 There are reports concluding that young age is a risk factor for elevated IOP after SITA and IVTA.1,4 Our findings suggested that SLT might lower the IOP from one month after SLT more effectively than the disappearance of the drug. In addition, SLT may be more effective for steroid-induced glaucoma as described for IVTA.3 However, we acknowledge that because of the lack of a treatment control group and the limited number of patients in the treatment group there exists the potential for misleading conclusions. Further investigations on a larger number of eyes are necessary to determine the efficacy of SLT by comparing the decrease with the natural decrease of IOP back to baseline.
Figure 1.
Mean intraocular pressure (IOP) before and after SLT. The IOP decreases gradually in three eyes and one eye had a trabeculotomy (case 4).
Abbreviations: IOP, intraocular pressure; SLT, selective laser trabeculoplasty.
Acknowledgments
The authors received no grant support in reporting their clinical observations. The corresponding author (MI) has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. KY, DS, RK, and SI analyzed and interpreted the patient data. MI, YK, and YO were major contributors in writing the manuscript. All authors read and approved the final manuscript.
References
- 1.Jonas JB, Degenring RF, Kreissig I, Akkoyun I, Kamppeter BA. Intraocular pressure elevation after intravitreal triamcinolone acetonide injection. Ophthalmology. 2005;112:593–598. doi: 10.1016/j.ophtha.2004.10.042. [DOI] [PubMed] [Google Scholar]
- 2.Viola F, Morescalchi F, Staurenghi G. Argon laser trabeculoplasty for intractable glaucoma following intravitreal triamcinolone. Arch Ophthalmol. 2006;124:133–134. doi: 10.1001/archopht.124.1.133. [DOI] [PubMed] [Google Scholar]
- 3.Pizzimenti JJ, Nickerson MM, Pizzmenti CE, Kasten-Aker AG. Selective laser trabeculoplasty for intraocular pressure elevation after intravitreal triamcinolone acetonide injection. Optom Vis Sci. 2006;83:421–425. doi: 10.1097/01.opx.0000225106.52653.72. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto Y, Komatsu T, Koura Y, Nishino K, Fukushima A, Ueno H. Intraocular pressure elevation after intravitreal or posterior sub-Tenon triamcinolone acetonide injection. Can J Ophthalmol. 2008;43:42–47. doi: 10.3129/i07-186. [DOI] [PubMed] [Google Scholar]
- 5.Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–242. doi: 10.1136/bjo.86.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iwase A, Suzuki Y, Araie M, et al. The Tajimi Study Group. The prevalence of primary open-angle glaucoma in Japanese. Ophthalmology. 2004;111:1641–1648. doi: 10.1016/j.ophtha.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 7.Honjo M, Tanihara H, Inatani M, Honda Y. External trabeculotomy for the treatment of steroid-induced glaucoma. J Glaucoma. 2000;9:483–485. doi: 10.1097/00061198-200012000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Mao AJ, Pan XJ, McIlraith I, Strasfeld M, Colev G, Hutnik C. Development of a prediction rule to estimate the probability of acceptable intraocular pressure reduction after selective laser trabeculoplasty in open-angle glaucoma and ocular hypertension. J Glaucoma. 2008;17:449–454. doi: 10.1097/IJG.0b013e31815f52cb. [DOI] [PubMed] [Google Scholar]
- 9.Latina MA, Park C. Selective targeting of trabecular meshwork cells: In vitro studies of pulsed and CW laser interactions. Exp Eye Res. 1995;60:359–671. doi: 10.1016/s0014-4835(05)80093-4. [DOI] [PubMed] [Google Scholar]
- 10.Melamed S, Ben Simon GJ, Levkovitch-Verbin H. Selective laser trabeculoplasty as primary treatment for open-angle glaucoma: A prospective, nonrandomized pilot study. Arch Ophthalmol. 2003;121:957–960. doi: 10.1001/archopht.121.7.957. [DOI] [PubMed] [Google Scholar]
- 11.Singh IP, Ahmad SI, Yeh D, et al. Early rapid rise in intraocular pressure after intravitreal triamcinolone acetonide injection. Am J Ophthalmol. 2004;138:286–287. doi: 10.1016/j.ajo.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Levy J, Tessler Z, Klemperer I, Lifshitz T. Acute intractable glaucoma after a single low-dose sub-Tenon’s corticosteroid injection for macular edema. Can J Ophthalmol. 2004;39:672–673. doi: 10.1016/s0008-4182(04)80035-8. [DOI] [PubMed] [Google Scholar]
- 13.Jonas JB, Degenring RF, Kamppeter BA, Kreissig I, Akkoyun I. Duration of the effect of intravitreal triamcinolone acetonide as treatment for diffuse diabetic macular edema. Am J Ophthalmol. 2004;138:158–160. doi: 10.1016/j.ajo.2004.02.025. [DOI] [PubMed] [Google Scholar]