Abstract
Background and objective
Squint surgery is frequently performed successfully in Hyderabad. However, no study in any detail has been performed on the outcome of monocular surgery for horizontal squint in the region. This study aims to determine the results of monocular surgery for horizontal trabismus.
Design
Retrospective/observational study.
Subjects and methods
The study was conducted on patients aged under 45 years, presenting with horizontal strabismus and undergoing monocular squint surgery. Anterior segment slit lamp examination, and if possible, posterior segment examination with 90 diopter (D) and 78 D fundoscopes was performed. Angle of deviation was measured. Patients were divided into two groups (esotropia and exotropia). Investigations were performed. Surgery was done under general anesthesia. A second surgical procedure was performed after six months for any residual deviations.
Results
After squint surgery, patients in group 1 (79%) and in group 2 (73.3%) had residual deviation of less than 15 prism diopters (PD). The preoperative deviations of 60 PD or less illustrated excellent domino effects with residual deviation of fewer than 15 PD. Three patients with successive deviation underwent a second surgery with excellent outcomes.
Conclusion
Few extraocular muscles can be prevented due to monocular squint surgery when multiple surgeries are needed.
Keywords: horizontal strabismus, monocular surgery, Hyderabad
Introduction
Strabismus is a commonly recurrent clinical condition of ocular misalliance leading to deviation of the visual axis from bifoveal fixation, and is infrequently allied with developmental craniofacial incongruity, and certain neurological diseases such as cerebral palsy.
The worldwide incidence of strabismus varies from 3% to 5%,1,2 whereas Hu and colleagues3 identified strabismus in 2% to 4% of white populations, and Abrahamsson and colleagues4 reported strabismus in 0.6% of Asians3 and Africans.5 In a study conducted by Dana and colleagues5 in Sydney, the incidence of strabismus was established in 48 patients (2.8% of total population). In another study carried out by Donnelly and colleagues, the prevalence was 3.98%.6 In an analysis conducted amongst Afghan immigrants in Pakistan, strabismus was noticed in 1.4% of patients.7 Another study conducted at Peshawar in 2004 confirmed that the total frequency of squint was 2%.8
The clinical treatment of squint includes evaluation and correction of multiple errors of refraction, management of amblyopia, and surgical treatment. The first surgery on squint was executed in 1839 by a general surgeon, Johann Dieffenbach.9
The ocular realignment of visual axis by surgical intervention becomes necessary when conservative management is unsuccessful. Surgical interventions are able to improve diplopia, rectify three dimensional (3D) vision, broaden the visual field, and improve psychological status10 and cosmesis.11
Subjects and methods
This is a retrospective clinical analysis conducted on the patients of both sexes with horizontal strabismus presenting for the first time from June 2004 to December 2007.
All patients suffering concomitant monocular horizontal squint (esotropia and exotropia), with deviation under 60 prism diopters (PD) devoid of any coupled vertical deviations were included in the study.
All subjects with history of paretic or limited extra ocular muscle component, more than 60 PD angle deviations, nystagmus, past history of any squint surgical procedure, and repeated deviation, were excluded from the current study.
Initial primary inspection of all patients was performed in our outpatient department by two qualified experienced ophthalmologists and four medical officers. After obtaining informed consent, the subjects were assessed for the following:
General history: including age, sex, citizenship, occupation, any history of corrective lenses, and which eye was affected. Photos of patients at up to the age of ten years were requested from patients and assessed to rule out any congenital anomaly.
Visual acuity of dominant (fixating) eye and squinting (nonfixating) eye, was evaluated with the help of Snellen’s chart for educated subjects and an E-chart for uneducated children.
Slit lamp biomicroscopy, and applanation tonometry.
Indirect ophthalmoscopy by 90 D and 78 D fundoscopes with fully dilated pupils.
Ocular movements including versions and ductions in co-operative patients.
Measurement of deviation in PD for both distance and near vision. The divergence was calculated in patients with fine bilateral visual acuity by a prism and cover test for near (33 cm) and far (6 m) distance using a fixation object. The modified Krimsky test was used to measure deviation in patients with intense amblyopia, limited vision, or children younger than the age of five years.
In children, refraction under cycloplegia using cyclopentolate 1% eye drops was undertaken and any accommodative element of more than 2.0 D was excluded preoperatively.
Scheduled investigations at admission were examined thoroughly and included a complete blood picture, bleeding and clotting times, detailed urine analysis, and chest X-rays. All the patients and their attendants were fully informed of the postoperative results and probability of a subsequent surgery. A prophylactic antibiotic and ophthalmic drops, eg, ofloxacin and chloramphenicol, were administered every three to four hours the day surgery. A complete surgical procedure was carried out under general anesthesia after approval by consultation with a visiting physician and qualified anesthetist.
The surgical procedure consisted of monocular recession and resection of horizontal recti muscles of the nonfixing eye. The muscle was exposed by a limbal conjunctival incision with two radial relieving incisions. The muscle was then separated from its attachments by round-edge curved conjunctival scissors and destabilized by a muscle hook. Two 6’0 poly gelactin 910 absorbable sutures were used for two whip stitches; one at the upper border and other at the lower boundary of muscle in close proximity to its insertion point during recession, and far from the insertion point in the muscle cone during muscle resection. At the time of recession the muscle was incised in close proximity to its insertion point and during muscle resection, then it was incised far from its insertion point, finally the muscle was allowed to retract and draw back. Sutures were carried out of the conjunctival incision and left unfastened with one edge at the 12 o’clock position with the other in the opposite position. Recession was measured with a caliper from posteriorly at the beginning of the muscle insertion point and afterwards the muscle was sutured directly on the sclera by piercing the sclera with both the upper and lower suture needles opposite each other. Both needles were passed gently up to half the width of the sclera under resistance without penetrating deeply into uveal tissue. The uveal penetration was confirmed when the needle passed very easily through the sclera without resistance. As the sutures were tied, the retracted muscle was lifted and brought forward to be fastened to the attachment site, and it was sutured at its normal anatomical insertion point in case of resection. Absorbable sutures were used to close the conjunctiva. An antibiotic/steroid eye ointment (neomycin with betamethasone) was applied and the eye bandaged for 24 hours.
On every postoperative outpatient follow-up visit, a complete orthoptic assessment was performed, including visual acuity and a photograph of the patient to measure the angle of deviation. The final best-corrected visual acuity and angle of deviation was documented on a sixth month post-treatment follow up.
Secondary surgical procedures in the fixating eye for consecutive squint over 15 PDs were performed six months after initial surgery. The postoperative follow up compliance of study participants was excellent.
Results
Out of approximately 7000 ophthalmic patients, 87 (1.24%) patients presented with strabismus during the study period. Out of these patients, 46 patients fulfilled the study inclusion criteria. Seven subjects refused to undergo surgical procedure, while the remaining 39 patients (esotropia = 24 [61.5%] and exotropia = 15 [38.5%]) were selected for surgery. The successful surgical outcome was considered as an angle deviation of 15 PDs or less at the six-month postoperative follow-up. Table 1 summarizes the general characteristics of patients of both groups.
Table 1.
General characteristics of patients with strabismus: (n = 39)
| Characteristic | Number of patients | Percentage (%) | |
|---|---|---|---|
| Gender | Male | 17 | 43.6 |
| Female | 22 | 56.4 | |
| Age in years | 5 to 15 | 16 | 41.0 |
| 16 to 30 | 13 | 33.4 | |
| 31 to 45 | 10 | 25.6 | |
| Residency | Rural | 13 | 33.4 |
| Urban | 26 | 66.6 | |
| Use of lenses | 14 | 35.9 | |
| Financial status | Upper | Nil | Nil |
| Middle | 17 | 43.5 | |
| Lower | 22 | 56.5 |
Table 2 presents group 1 (esotropia) patient data including preoperative angles of deviation (Figure 1), surgical procedures and postoperative results (Figure 2). Table 3 presents group 2 (exotropia) patient data including all details (Figures 3 and 4).
Table 2.
Pre-and postoperative clinical characteristics of group 1 (esotropia)
| Number of patients | Age (years) | Angle of deviation (PD) | Post operative residual | Surgical technique |
|---|---|---|---|---|
| 10 | 05 to 15 | <15 | 15 | RC of MR |
| 8 patients | 2 patients | 5–6 mm over all | ||
| >33.3% | 8.4% | RS of LR | ||
| 7–9 mm over all | ||||
| 8 | 16 to 30 | <15 | <15 | |
| 6 patients | 2 patients | |||
| 25.0% | 8.4% | |||
| 6 | 31 to 45 | <15 | <15 | |
| 5 patients | 1 patient | |||
| 20.7% | 4.2% |
Notes: n = 24 (61.5%) Preoperative angle of deviation PD = 30 to 60 overall.
Abbreviations: PD, prism diopter; RC, recession; RS, resection; MR, medial rectus; LR, lateral rectus.
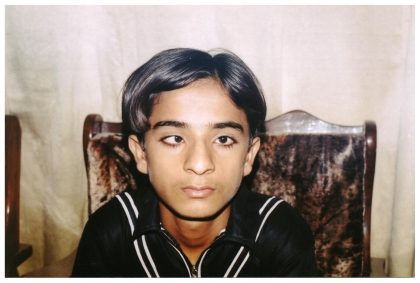
Figure 1.
A 13-year-old boy with right eye concomitant strabismus.
Figure 2.
A 13-year-old boy underwent right monocular strabismus surgery (15th postoperative day).
Table 3.
Pre and post-operative clinical characteristics of group 2 (exotropia)
| Number of patients | Age (years) | Angle of deviation (PD) | Post-operative residual | Surgical technique |
|---|---|---|---|---|
| 4 | 05 to 15 | <15 | >15 | RC of MR |
| 3 patients | 1 patients | 5–6 mm over all | ||
| 20.0% | 6.6% | RS of LR | ||
| 7–9 mm over all | ||||
| 6 | 16 to 30 | <15 | >15 | |
| 4 patients | 2 patients | |||
| 26.7% | 13.4% | |||
| 5 | 31 to 45 | <15 | >15 | |
| 4 patients | 1 patient | |||
| 26.7% | 6.6% |
Notes: n = 15 (38.5%) Preoperative angle of deviation in PD = 30 to 60 overall.
Abbreviations: PD, prism diopter; RC, recession; RS, resection; MR, medial rectus; LR, lateral rectus.
Figure 3.
A 16-year-old girl with left eye concomitant strabismus.
Figure 4.
A 16-year-old girl underwent left monocular strabismus surgery (15th postoperative day).
In group 1 (esotropia), five patients (19.0%) presented with residual deviation of more than 15 PDs. The remaining patients (79.0%) presented with successful surgical outcomes. Similarly, in group 2 (exotropia), patients presented with orthophoria (73.3%), while four (26.7%) patients demonstrated residual deviation.
Three patients in both groups developed suture-related foreign body granuloma formation, which resolved within a few weeks during the course of treatment. Ocular movements, including convergence, were normal in all patients except two (13.4%) in group 2, who underwent 10 mm recession of lateral rectus and experienced limitation in ocular movements. Muscle overcorrection was not encountered in either group. Out of 39 subjects, 12 patients were lost to follow-up, while the remaining 27 completed six months postoperative follow-up.
Of nine patients (23.0%) in both groups who exhibited consequent strabismus after six months, six patients did not agree to a second surgery and only three patients underwent successful secondary surgical intervention.
Discussion
Monocular strabismus surgery is a recommended procedure for patients suffering monocular concomitant squint. This procedure minimizes the handling of the dominant eye, thereby reducing surgical duration.12,13
Occasionally it becomes difficult to visually align the eyes by operating only on one eye because of larger deviations of more than 60 PDs. At this stage, clinical circumstances for a second surgery on the fixing eye or binocular squint surgery concerning more than two horizontal rectus muscles is the main and extensive used clinical procedure. This technique also avoids limitations in ocular movement.14–16 In our study, we acquired excellent outcomes through a surgical procedure carried out on the fixating eye in subjects who had developed residual deviation after the initial surgery on the nondominant, fixating eye.
Monocular squint surgery can be safely performed in adults under peribulbar anesthesia, with rapid recovery and less complications.17,18 Although there are some disadvantages of regional anesthesia including: retrobulbar hemorrhage, optic nerve injury, central retinal artery occlusion, and ptosis.19 In this study all the subjects in both groups were operated under general anesthesia.
Scott and colleagues define the accuracy of squint surgery as a residual deviation of 10 PDs or less. Scott also states that for larger angles, the surgical objective should be a small residual deviation rather than straight eyes.20 Following this concept of undercorrection, the residual deviation of 15 PDs and less was considered accurate in this study.
Restricted ocular movements are an occasional clinical problem following huge recessions. Multiple authors strongly recommend not exceeding a 7 mm recession on medial rectus and 8 mm recession on lateral rectus muscle to avoid diminished restricted ocular movements.21–23
In this study only two (13.4%) subjects in group 2, who underwent a 10 mm recession on lateral rectus muscle suffered postoperative limitation in ocular movements.
Footnotes
Disclosures
The authors report no conflicts of interest relevant to this research.
References
- 1.Arora A, Williums B, Arora AK. Decreasing strabismus surgery. Br J Ophthamol. 2005;89(4):409–412. doi: 10.1136/bjo.2004.053678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ziakas NG, Woodruff G, Smith LK, Thompson JR. A study of heredity as a risk factor in strabismus. Eye. 2002;16(5):519–521. doi: 10.1038/sj.eye.6700138. [DOI] [PubMed] [Google Scholar]
- 3.Hu DN. Prevalence and mode of inheritance of major genetic eye diseases in China. J Med Genet. 1987;24(10):584–588. doi: 10.1136/jmg.24.10.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abrahamsson M, Magnusson G, Sjostrand J. Inheritance of strabismus and the gain of using heredity to determine populations at risk of developing strabismus. Acta Ophthalmol Scand. 1999;77(6):653–657. doi: 10.1034/j.1600-0420.1999.770609.x. [DOI] [PubMed] [Google Scholar]
- 5.Robaei D, Rose KA, Kifley A. Factors associated with childhood strabismus: findings from a population-based study. Ophthalmology. 2006;113(7):1146–1153. doi: 10.1016/j.ophtha.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 6.Donnelly UM, Stewart NM, Hollinger M. Prevalence and outcomes of childhood visual disorders. Ophthalmic Epidemiol. 2005;12(4):243–250. doi: 10.1080/09286580590967772. [DOI] [PubMed] [Google Scholar]
- 7.Awan HRA, Ahsan T. Prevalence of visual impairment and eye diseases in Afghan refugees in Pakistan. East Mediterr Health J. 1998;4(3):560–566. [Google Scholar]
- 8.Ahmed Nisar, Aamir AH, Hussain Iqbal, Ghulam Shoukat. Annual prevalence of various diseases in hospitalized patients in a tertiary level teaching hospital at Peshawar. Pak J Med Res. 2004;43(4):166–171. [Google Scholar]
- 9.Cooper J, Medow N. Major review: intermittent exotropia, basic anddivergence excess type. binocular vision. Eye Muscle Surgery Quarterly. 1993;8(3):185–216. [Google Scholar]
- 10.Keenan JM, Willshaw HE. Outcome of strabismus surgery in congenital esotropia. Br J Ophthalmol. 1992;76(6):342–345. doi: 10.1136/bjo.76.6.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Willshaw HE, Keenen JM. Strabismus surgery in children: the prospects for binocular single vision. Eye. 1991;5(3):338–343. doi: 10.1038/eye.1991.54. [DOI] [PubMed] [Google Scholar]
- 12.Celebi S, Kukner AS. Large bilateral lateral rectus recession in large angle divergence excess exotropia. Eur J Ophthalmol. 2001;11(1):6–8. doi: 10.1177/112067210101100102. [DOI] [PubMed] [Google Scholar]
- 13.Livir-Rallatos G, Gunton KB, Calhoun JH. Surgical results in largeangle exotropia. J AAPOS. 2002;6(2):77–80. doi: 10.1067/mpa.2002.122059. [DOI] [PubMed] [Google Scholar]
- 14.Amitava AK, Goswami AK, Mishra A. Large-angle strabismus and primary true muscle transplantation. J Pediatr Ophthalmol Strabismus. 2005;42(4):211–215. doi: 10.3928/01913913-20050701-02. [DOI] [PubMed] [Google Scholar]
- 15.Currie ZI, Shipman T, Burke JP. Surgical correction of large-angle exotropia in adults. Eye. 2003;17(3):334–339. doi: 10.1038/sj.eye.6700347. [DOI] [PubMed] [Google Scholar]
- 16.Forrest MP, Finnigan S, Finnigan S, Gole GA. Three horizontal muscle squint surgery for large angle infantile esotropia. Clin Experiment Ophthalmol. 2003;31(6):509–516. doi: 10.1046/j.1442-9071.2003.00713.x. [DOI] [PubMed] [Google Scholar]
- 17.Ripart J, Lefrant JY, de La Coussaye JE, Prat-Pradal D, Vivien B, Eledjam JJ. Peribulbar versus retrobulbar anesthesia for ophthalmic surgery. Anesthesiology. 2001;94(1):56–62. doi: 10.1097/00000542-200101000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Greenberg MF, Pollard ZF. Adult strabismus surgery under propofol sedation with local versus general anesthesia. J AAPOS. 2003;7(2):116–120. doi: 10.1016/mpa.2003.S1091853102000149. [DOI] [PubMed] [Google Scholar]
- 19.Hamilton RC. Complications of ophthalmic regional anesthesia. Ophthalmol Clin North Am. 1998;11:99–114. [Google Scholar]
- 20.Scott WE, Reese PD, Hirsh CR, Flabetich CA. Surgery for large angle congenital esotropia. Arch Ophthalmol. 1986;104:374–377. doi: 10.1001/archopht.1986.01050150074030. [DOI] [PubMed] [Google Scholar]
- 21.Vroman DT, Hutchinson AK, Saunders RA, Wilson ME. Two-muscle surgery for congenital esotropia: rate of reoperation in patients with small versus large angles of deviation. J AAPOS. 2000;4(5):267–270. doi: 10.1067/mpa.2000.106960. [DOI] [PubMed] [Google Scholar]
- 22.Prieto-Díaz J, Souza-Dias C. Esotropias. In: Prieto-Díaz, Souza-Dias C, editors. Estrabismo. São Paulo, Brasil: Livraria Santos Editora; 2002. pp. 149–99. [Google Scholar]
- 23.Millán T, de Carvalho KM, Minguini N. Results of monocular surgery under peribulbar anesthesia for large-angle horizontal strabismus. Clinics. 2009;64(4):303–308. doi: 10.1590/S1807-59322009000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]