Not everything that can be counted counts, and not everything that counts can be counted.
Albert Einstein1
During the past 2 decades, considerable progress has been made in establishing the lipid hypothesis and the importance of lipid profiles, especially the levels of low-density lipoprotein cholesterol (LDL-C) but also levels of high-density lipoprotein cholesterol (HDL-C) and triglycerides (TGs), for predicting risk of coronary heart disease (CHD).2-5 Additionally, many large-scale randomized controlled studies of lipid intervention, especially with the statin family of medications, have established the role of improving lipid levels, particularly levels of LDL-C, for CHD risk reduction.6 However, despite the use of the highest doses of the most potent statins, many patients continue to have major cardiovascular (CV) events (or “residual risk”).
In this issue of Mayo Clinic Proceedings, Harper and Jacobson7 point out that, despite considerable evidence supporting focused efforts to reduce LDL-C in primary and secondary CHD prevention, this strategy has many limitations. Clearly, other lipid parameters, including TGs, HDL-C, total cholesterol/HDL ratio and, especially, non–HDL-C, may also be important for predicting CV outcomes in patients receiving LDL-C–lowering therapies.7,8 Harper and Jacobson's commentary particularly emphasizes the potential role of apolipoprotein (apo) B to predict clinical risk and to serve as a target of therapy, providing suggestions for the routine measurement of apo B and using this measurement in efforts to optimize medical intervention.
We do not dispute that levels of apo B are strongly related with CHD risk, which has also been argued for many years by other experts.9-11 This clearly makes sense because apo B is a key structural component of nearly all atherogenic lipoprotein particles. However, the major questions are whether clinicians really need another lipoprotein parameter to measure and whether measurement and intervention directed at apo B will clearly enhance existing efforts at CHD risk reduction.
Non–HDL-C
In an effort to reduce this “residual risk,” one can make a strong case to support efforts that address levels of non–HDL-C.7,8,12,13 Although non–HDL-C is not a new concept (this was defined as the second lipid target by the National Cholesterol Education Program/Adult Treatment Panel III [ATP III] guidelines in 2001),14 this has not been widely adopted in routine clinical practice. In fact, in our experience, many house staff and busy practicing clinicians are unfamiliar with what non–HDL-C represents, how to measure it, and the goals for non–HDL-C (see Table 1 in the commentary by Harper and Jacobson7). This is not surprising since a considerable amount of lipid education during the past decade has been directed at statins, with the emphasis predominantly directed at reducing levels of LDL-C. Although other families of lipid medications are also effective (eg, niacin, fibrates, omega-3 fatty acids), these have not received the same degree of attention that has been directed at statin intervention.4,5,15
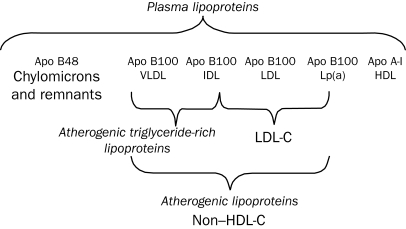
Importantly, a standard fasting lipid profile includes direct measurement of total cholesterol, HDL-C, and TG values. In contrast, LDL-C is almost always a calculated value, arrived at by subtracting the HDL-C and 1/5 of the TG (which represents very low-density lipoprotein cholesterol [VLDL-C]) from the total cholesterol. Non–HDL-C is simply the total cholesterol minus HDL-C.2,13,14 This calculation may be more accurate than the one for LDL-C, especially when TG values are moderately elevated (particularly TGs >400-500 mg/dL; to convert to mmol/L, multiply by 0.0113), making the VLDL-C calculation unreliable. Therefore, at no additional cost beyond the fasting lipid profile charge, non–HDL-C measures all atherogenic apo B–containing lipoproteins, including LDL-C and VLDL-C, and to a lesser extent intermediate-dense lipoprotein cholesterol (IDL-C), chylomicrons, chylomicron remnants, and lipoprotein(a) (Figure 1).7,13 According to ATP III guidelines, in patients with very high TG values (≥500 mg/dL), the primary goal is treating TGs, with LDL-C and non–HDL-C being secondary goals. However, in the vast majority of patients with either normal (<150 mg/dL) or borderline (150-199 mg/dL) TG values, the primary goal is LDL-C. In patients with elevated TG values (200-499 mg/dL), the primary goal is LDL-C, and non–HDL-C is the secondary goal. As illustrated in Table 1 in the article by Harper and Jacobson, the non–HDL-C goals are relatively simple to remember and use: 30 mg/dL higher than the LDL-C goal. For example, if the LDL-C goal is less than 100 mg/dL (to convert to mmol/L, multiply by 0.0259), the non–HDL-C goal would be less than 130 mg/dL (to convert to mmol/L, multiply by 0.0259), or if the patient is at high risk and the “optional” LDL-C goal of less than 70 mg/dL is targeted, the corresponding non–HDL-C goal would be less than 100 mg/dL.
FIGURE 1.
Potential targets of lipid intervention. Low-density lipoprotein cholesterol (LDL-C) and non–high-density lipoprotein cholesterol (non–HDL-C) are recommended as the primary and secondary targets of therapy. Apo = apolipoprotein; IDL = intermediate-density lipoprotein; Lp(a) = lipoprotein(a); VLDL = very low-density lipoprotein.
From J Am Coll Cardiol,13 with permission from Elsevier.
In fact, as Harper and Jacobson and others have demonstrated,7,8,12-17 levels of non–HDL-C correlate strongly with levels of apo B, and both non–HDL-C and apo B levels predict overall CV risk better than does LDL-C.7 Moreover, studies have demonstrated that lowering of non–HDL-C levels predicts CHD risk reduction in a 1:1 relationship in pharmacologic lipid intervention studies and that non–HDL-C performed nearly twice as effectively as did LDL-C for predicting CHD risk reduction.12,13
Apo B vs Non–HDL-C
Arguably, apo B appears to predict risk as well as or possibly slightly more accurately than does non–HDL-C.7,9-11 Although apo B levels predict risk considerably better than does LDL-C in statin-treated patients,7 they provide essentially no additive information beyond that obtained with non–HDL-C levels in predicting risk in such patients.13,16,17 Because statins are considered the first-line agents for CV risk reduction in almost all patients for primary and, particularly, secondary CHD prevention, non–HDL-C is virtually as good as apo B for most patients. And unlike apo B, non–HDL-C is easily determined from the standard lipid profile, requiring no additional expense and is therefore readily available.18 All considered, these issues provide a strong argument for routine measurement and intervention directed at non–HDL-C, rather than apo B or possibly even LDL-C.
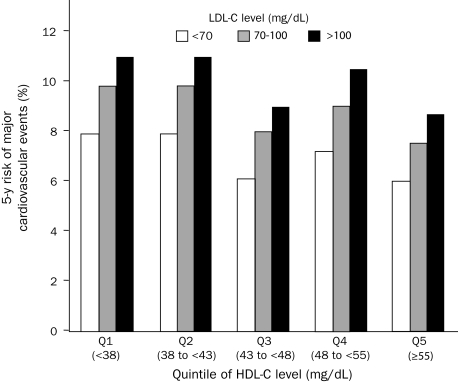
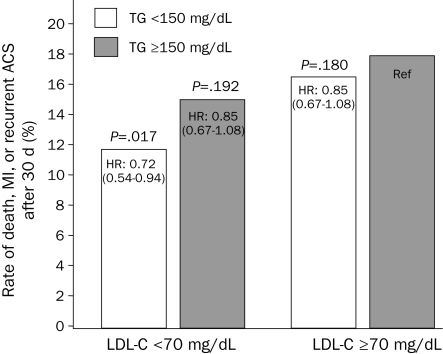
Currently, appreciable efforts are being directed toward adding therapies (eg, niacin, fibrates, and omega-3 polyunsaturated fatty acids) to statins in efforts to improve HDL-C and TG values, which would reduce both non-HDL and apo B values and hopefully lead to additional CV risk reduction.2,4,5,15,19,20 Certainly, in the TNT (Treatment to New Targets) trial of high-dose (80 mg) and low-dose (10 mg) atorvastatin in more than 10,000 patients with stable CHD, even in those who achieved LDL-C values lower than 70 mg/dL (mostly with high-dose therapy), CHD risk was still strongly influenced by low levels of HDL-C (Figure 2)21; the same is true in the PROVE IT-TIMI 22 (Prava statin or Atorvastatin Evaluation and Infection Therapy—Thrombolysis in Myocardial Infarction 22), which found that excess risk due to elevated TG values (≥150 mg dL) persisted even when LDL-C levels were lower than 70 mg/dL in patients receiving treatment (Figure 3).22 By definition, these patients with elevated TGs, particularly with concomitant low HDL-C, will have elevated levels of non–HDL-C. In the recent ARBITER 6-HALTS trial (Arterial Biology for the Investigation of the Treatment Effect of Reducing Cholesterol 6-HDL and LDL Treatment Strategies),23 niacin and statin therapy increased HDL-C levels, reduced carotid intima media thickness, and lowered CV events compared with statin and ezetimibe therapy, supporting the concept of HDL-C as a lipoprotein particle mediating reverse cholesterol transport through the action of apo AI. Large-scale studies are under way that will further assess the efficacy of the HDL/TG therapy; however, in the meantime, a recent meta-analysis from trials using statins, niacin, and fibrates failed to demonstrate that changes in HDL-C or TGs predicted CHD risk above and beyond those predicted from LDL-C reduction.24 In recent years, using levels of C-reactive protein (CRP) to predict risk has received considerable attention, with some evidence suggesting that CRP could be a target of therapy in both primary and secondary prevention and that CRP may be ready for “prime time” in preventive cardiology.25,26 Not surprisingly, apo AI may be a better predictor of risk than HDL-C, similar to apo B being a better predictor of risk than LDL-C.27 The apo B/apo AI ratio may also strongly predict risk; this was demonstrated to be the most powerful risk factor in the landmark INTERHEART study, which included nearly 30,000 participants from 52 countries.28 Additional tools are needed to improve CHD risk assessment, particularly to address and reduce the residual risk.29 Currently, we think that the most promising parameters are non–HDL-C and CRP; however, apo B may not be clinically necessary or economically feasible at this time. Finally, greater efforts at weight reduction and prevention of overweightness and obesity,30 maintaining high cardiorespiratory fitness with regular exercise training,31 and smoking cessation are all needed in a comprehensive program of primary and secondary CHD prevention.29
FIGURE 2.
In patients with stable chronic heart disease, levels of high-density lipoprotein cholesterol (HDL-C) continue to predict risk at any given level of low-density lipoprotein cholesterol (LDL-C) during treatment.
Adapted from N Engl J Med,21 with permission. Copyright ©2007 Massachusetts Medical Society. All rights reserved.
FIGURE 3.
In patients who have had an acute coronary syndrome (ACS), elevated levels of triglycerides (TGs) (≥150 mg/dL; to convert to mmol/L, multiply by 0.0113) predict risk even in those with low-density lipoprotein cholesterol (LDL-C) levels lower than 70 mg/dL (to convert to mmol/L, multiply by 0.0259). HR = hazard ratio; MI = myocardial infarction; Ref = reference.
Adapted from J Am Coll Cardiol,22 with permission from Elsevier.
Recommendations
How should clinicians and guidelines proceed with regard to apo B and other novel lipid parameters based on the current evidence? We certainly would not object if clinicians decide to measure and treat apo B, as suggested by Harper and Jacobson,7 Sniderman and others.9-11,32 Clearly, in some patients, apo B may identify moderate risk that was not suggested by LDL-C or non–HDL-C.11,32 The patients in the recent JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) trial33 represent an example of this, although all these patients had high levels of CRP. The question is whether clinicians should be routinely encouraged or mandated to measure and treat apo B. Although apo B has been suggested as an alternative target by the Canadian Working Group34 and a joint Consensus Statement by the American Diabetes Association and the American College of Cardiology,35 we doubt that most organizations or major guideline statements will endorse apo B as a routine parameter in the near future. Regarding assessment of lipoprotein concentrations, other lipoprotein parameters, and modified lipids beyond the standard lipid profile (including LDL particle size and density, and apo B), we agree with the recent guideline paper from the 2009 American College of Cardiology Foundations/American Heart Association that there is “no evidence that the assessment of additional lipid parameters leads to improved net health outcomes,” thus giving this a class III (level of evidence C) recommendation.36
In contrast, assessment of non–HDL-C requires no additional cost and is readily available for clinical use.13 Although this has been in the guidelines since 2001,14 only recently has interest in the clinical use of non–HDL-C been heightened. Currently, non–HDL-C is a secondary goal for all patients with elevated TGs (200-499 mg/dL), but considering the current level of evidence, we agree with the recent assertion by Robinson13 that “ultimately, it may be desirable to move toward non–HDL-C as the primary target of therapy once non–HDL-C has been routinely incorporated into clinical practice.” We also agree that intensive education of health care professionals regarding the value of non–HDL-C is urgently needed, as is a campaign to convince lipid laboratory directors to routinely report the non–HDL-C values and goals of therapy, which would greatly aid clinican education and acceptance of its importance. Efforts to also use apo B should currently be put on hold, with the emphasis being placed on LDL-C, TGs, HDL-C, and, particularly, non–HDL-C (all available from the simple lipid profile). As the Norwegian ethnologist Thor-Heyerdahl noted “Progress is man's ability to complicate simplicity,”37 which also reminds us that the famous Italian draftsman, sculptor, and painter Leonardo da Vinci said, “Simplicity is the ultimate sophistication.”38 For now, we should keep things simple, with the basic fasting lipid profile and greater emphasis on not only obtaining the LDL-C aggressive goals but also focusing on reducing levels and achieving goals for non–HDL-C.
Conclusion
We strongly support the routine assessment and treatment directed at levels of non–HDL-C, as well as including these values and goals in routine laboratory reports. Despite the well-written commentary by Harper and Jacobson7 and the excellent points that they make, we do not think that the overall evidence currently supports the need for routinely measuring and treating apo B in modern clinical practice.
REFERENCES
- 1.Einstein Albert.The Quotations Page Web site. http://www.quotationspage.com/quote/26950.html. http://www.quotationspage.com/quote/26950.html Accessed March 10, 2010.
- 2.Lavie CJ, Milani RV, O'Keefe JH. Statin wars: emphasis on potency vs event reduction and safety. Mayo Clin Proc. 2007;82(5):539-542 [DOI] [PubMed] [Google Scholar]
- 3.O'Keefe JH, Bybee KA, Lavie CJ. Intensive lipid intervention in the post-ENHANCE era. Mayo Clin Proc. 2008;83(8):867-869 [DOI] [PubMed] [Google Scholar]
- 4.Lavie CJ, Milani RV. Shedding light on high-density lipoprotein cholesterol: the post-ILLUMINATE era. J Am Coll Cardiol. 2008;51(1):56-58 [DOI] [PubMed] [Google Scholar]
- 5.Cardenas GA, Lavie CJ, Cardenas V, Milani RV, McCullough PA. The importance of recognizing and treating low levels of high-density lipoprotein cholesterol: a new era in atherosclerosis management. Rev Cardiovasc Med. 2008;9(4):239-258 [PubMed] [Google Scholar]
- 6.O'Keefe JH, Jr, Cordain L, Harris WH, Moe RM, Vogel R. Optimal low-density lipoprotein is 50 to 70 mg/dl: lower is better and physiologically normal. J Am Coll Cardiol. 2004;43(11):2142-2146 [DOI] [PubMed] [Google Scholar]
- 7.Harper CR, Jacobson TA. Using apolipoprotein B to manage dyslipidemic patients: time for a change? Mayo Clin Proc. 2010;85(5):440-445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arsenault BJ, Rana JS, Stroes ES, et al. Beyond low-density lipoprotein cholesterol: respective contributions of non-high-density lipoprotein cholesterol levels, triglycerides, and the total cholesterol/high-density lipoprotein cholesterol ratio to coronary heart disease risk in apparently healthy men and women. J Am Coll Cardiol. 2009;55(1):35-41 [DOI] [PubMed] [Google Scholar]
- 9.Sniderman AD. Counterpoint to (measure apo) B or not to (measure apo) B: a critique of modern medical decision-making. Clin Chem. 1997;43(8, pt 1):1310-1314 [PubMed] [Google Scholar]
- 10.Sniderman A. Targets for LDL-lowering therapy. Curr Opin Lipidol. 2009;20(4):282-287 [DOI] [PubMed] [Google Scholar]
- 11.Sniderman A, Williams K, Cobbaert C. ApoB versus non-HDL-C: what to do when they disagree. Curr Atheroscler Rep. 2009;11(5):358-363 [DOI] [PubMed] [Google Scholar]
- 12.Robinson JG, Wang S, Smith BJ, Jacobson TA. Meta-analysis of the relationship between non–high-density lipoprotein cholesterol reduction and coronary heart disease risk. J Am Coll Cardiol. 2009;53(4):316-322 [DOI] [PubMed] [Google Scholar]
- 13.Robinson JG. Are you targeting non high-density lipoprotein cholesterol [editorial]? J Am Coll Cardiol. 2009;55(1):42-44 [DOI] [PubMed] [Google Scholar]
- 14.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285(19):2486-2497 [DOI] [PubMed] [Google Scholar]
- 15.Lavie CJ, Milani RV, Mehra MR, Ventura HO. Omega-3 polyunsaturated fatty acids and cardiovascular diseases. J Am Coll Cardiol. 2009;54(7):585-594 [DOI] [PubMed] [Google Scholar]
- 16.Kastelein JJ, van der Stieg W, Holme I, et al. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation 2008;117(23):3002-3009 [DOI] [PubMed] [Google Scholar]
- 17.Ballantyne CM, Raichlen JS, Cain VA. Statin therapy alters the relationship between apolipoprotein B and low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol targets in high-risk patients: the MERCURY II (Measuring Effective Reductions in Cholesterol Using Rosuvastatin) trial. J Am Coll Cardiol. 2008;52(8):626-632 [DOI] [PubMed] [Google Scholar]
- 18.Blaha MJ, Blumenthal RS, Brinton EA, Jacobson TA, National Lipid Association Taskforce on Non-HDL Cholesterol The importance of non-HDL cholesterol reporting in lipid management. J Clin Lipidol. 2008;2(4):267-273 [DOI] [PubMed] [Google Scholar]
- 19.Jacobson TA. A “hot” topic in dyslipidemia management—“how to beat a flush”: optimizing niacin tolerability to promote long-term adherence and coronary disease prevention. Mayo Clin Proc. 2010;85(4):365-379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JH, O'Keefe JH, Lavie CJ, Marchioli R, Harris WS. Omega-3 fatty acids for cardioprotection. Mayo Clin Proc. 2008;83(3):324-332 [DOI] [PubMed] [Google Scholar]
- 21.Barter P, Gotto A, LaRosa J, et al. TNT Investigators HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007;357(13):1301-1310 [DOI] [PubMed] [Google Scholar]
- 22.Miller M, Cannon CP, Murphy SA, Qin J, Ray KK, Braunwald E, PROVE IT-TIMI 22 Investigators Impact of triglyceride levels beyond low-density lipoprotein cholesterol after acute coronary syndrome in the PROVE IT-TIMI 22 trial. J Am Coll Cardiol. 2008;51(7):724-730 [DOI] [PubMed] [Google Scholar]
- 23.Taylor AJ, Villines TC, Stanek EJ, et al. Extended-release niacin or ezetimibe and carotid intima-media thickness. N Engl J Med. 2009;361(22):2113-2122 [DOI] [PubMed] [Google Scholar]
- 24.Briel M, Ferreira-Gonzalez I, You JJ, et al. Association between change in high density lipoprotein cholesterol and cardiovascular disease morbidity and mortality: systemic review and meta-regression analysis. BMJ 2009;338:b92 http://www.bmj.com/cgi/content/full/338/feb16_1/b92 Published February 16, 2009. Accessed March 10, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lavie CJ, Milani RV, Verma A, O'Keefe JH. C-reactive protein and cardiovascular disease: is it ready for primetime? Am J Med Sci. 2009;338(6):486-492 [DOI] [PubMed] [Google Scholar]
- 26.O'Keefe JH, Carter MD, Lavie CJ, Bell DS. The gravity of JUPITER (Justification for the Use of Statins in Primary Prevention: an Intervention Trial Evaluating Rosuvastatin). Postgrad Med. 2009;121(3):113-118 [DOI] [PubMed] [Google Scholar]
- 27.Florvall G, Basu S, Larsson A. Apolipoprotein A1 is a stronger prognostic marker than are HDL and LDL cholesterol for cardiovascular disease and mortality in elderly men. J Gerontol A Biol Sci Med Sci. 2006;61(12):1262-1266 [DOI] [PubMed] [Google Scholar]
- 28.Yusuf S, Hawken S, Ounpuu S, et al. INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364(9438):937-952 [DOI] [PubMed] [Google Scholar]
- 29.O'Keefe JH, Carter MD, Lavie CJ. Primary and secondary prevention of cardiovascular diseases: a practical evidence-based approach. Mayo Clin Proc. 2009;84(8):741-757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53(21):1925-1932 [DOI] [PubMed] [Google Scholar]
- 31.Lavie CJ, Thomas RJ, Squires RW, Allison TG, Milani RV. Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clin Proc. 2009;84(4):373-383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sniderman AD, St-Pierre AC, Cantin B, Dagenais GR, Després JP, Lamarche B. Concordance/discordance between plasma apolipoprotein B levels and the cholesterol indexes of atherosclerotic risk. Am J Cardiol. 2003;91(10):1173-1177 [DOI] [PubMed] [Google Scholar]
- 33.Ridker PM, Danielson E, Fonseca FA, et al. JUPITER Study Group Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195-2207 [DOI] [PubMed] [Google Scholar]
- 34.Genest J, Frohlich J, Fodor G, McPherson R, Working Group on Hypercholesterolemia and Other Dyslipidemias Recommendations for the management of dyslipidemia and the prevention of cardiovascular disease: summary of the 2003 update [published correction appears in CMAJ. 2003;169(11):1149] CMAJ 2003;169(9):921-924 [PMC free article] [PubMed] [Google Scholar]
- 35.Brunzell JD, Davidson M, Furberg CD, et al. Lipoprotein management in patients with cardiometabolic risk: consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care 2008;31(4):811-822 [DOI] [PubMed] [Google Scholar]
- 36.Greenland P, Alpert JS, Beller GA, et al. 2009 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. In press [DOI] [PubMed]
- 37.Hyerdahl Thor. ThinkExist.Com Web site. Thor-Heyerdahl Quotes http://thinkexist.com/quotes/thor-heyerdahl/ Accessed March 10, 2010
- 38.Leonardo da Vinci ThinkExist.Com Web site. Leonardo da Vinci Quotes http://thinkexist.com/quotation/simplicity_is_the_ultimate_sophistication/213576.html Accessed March 10, 2010