Abstract
Asian women are known to have a larger amount of abdominal fat (AF) for the same level of BMI compared with Caucasian and African-American women. This study was aimed to determine whether waist circumference (WC) could be useful as an index of AF compared with AF measured by dual energy x-ray absorptiometry (DXA) before and after a weight-loss program in Asian women. Thirty-eight healthy, pre-menopausal obese Korean women (body fat percent > 30%) were enrolled and followed during a 6-week weight-loss program including herbal formula, calorie restriction, and exercise. Anthropometry and DXA measurements were performed before and after weight-loss. A specific region of interest (ROI, L2-iliac crest) by DXA was correlated with anthropometry at baseline: WC (γ = 0.91) > BMI (γ = 0.87) > Waist-Height ratio (WHtR, γ = 0.82) > WHR (γ = 0.46); and after weight loss: BMI (γ = 0.88) > WC (γ = 0.84) > WHtR (γ = 0.82), all p < 0.01. The change in DXA ROI showed a reasonable correlation with change in anthropometry: BMI (γ = 0.63, p < 0.01) > WC (γ = 0.39, p < 0.05) > WHtR (γ = 0.37, p < 0.05). A stepwise multiple regression analysis revealed that 83% of the variance in DXA derived AF was explained by WC at baseline, WC and BMI at follow-up, respectively. This study suggests that WC could be a good predictor of AF for Korean pre-menopausal women.
Keywords: abdominal fat, Dual energy x-ray absorptiometry, obesity, waist circumference, fat distribution
INTRODUCTION
It is well-known that abdominal subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) are related with several chronic diseases such as diabetes1,2 and cardiovascular disease.3 Asian women have a tendency to have a higher amount of abdominal fat for the same BMI compared to Caucasian and African-American women.4 A normal BMI however, does not necessarily infer normal levels of abdominal fat. Therefore, when assessing adipose tissue distribution for detecting risk of obesity related diseases, it is important to acquire an appropriate index of central obesity.
The most sensitive methods available to quantify intra-abdominal fat include imaging techniques, specifically computerized tomography (CT) and magnetic resonance imaging (MRI). MRI has become the more popular technique and is used for the in-vivo assessment of organs and tissues at the whole-body level with no risk of radiation. But limitations associated with both CT and MRI include high cost and a risk of ionizing radiation with CT.5
Dual energy x-ray absorptiometry (DXA) has been used to measure body composition as an advanced laboratory based method for close to two decades. DXA allows for the assessment of regional and total body fat, lean tissues, and bone mineral content.6,7 The advantages of DXA over CT and MRI as a means of estimating fat distribution include: relative ease of access to systems, simplicity of measurements, relatively low cost, and lower radiation exposure. Relative to waist circumference, DXA predicts fat mass with greater accuracy and reproducibility, making it easier to compare data from different studies. However, a major disadvantage of DXA is that it does not separate intra-abdominal and subcutaneous fat tissues.8-12
To acquire information specific to abdominal fat mass by DXA, over and above that provided by the conventional DXA trunk region, a specific Region of Interest (ROI) has been applied to estimate fat mass in the abdomen, excluding bony structure of ribs and spine. The conventional DXA trunk fat region (CV, coefficient of variation = 0.728%) includes chest, abdomen, and pelvis.
In 2002, Park et al. reported that DXA ROI of the upper L2-lower L4 (γ = 0.85, 0.96, respectively) and of upper L2-upper iliac crest (γ = 0.84, 0.97, respectively) shows high correlation with total VAT and abdominal adipose tissue (abdominal VAT plus SAT) by MRI.13
Several anthropometric indexes, such as waist circumference, waist to thigh circumference, waist to hip ratio (WHR), and sagittal abdominal diameter have been applied as surrogate measures of abdominal fat mass. Waist circumference (WC) is the most frequently used index of abdominal obesity in clinics due to its high relation with visceral fat in comparison with other anthropometric indexes14,15 and simplicity of measurement and analysis.16
The aim of this study was to determine whether WC is a valid technique for measuring abdominal obesity before and after weight-loss programs compared to a DXA ROI in obese pre-menopausal Korean women.
MATERIALS AND METHODS
Subjects
Overweight (body fat percent > 30% or BMI > 25kg/m2) pre-menopausal Korean women ages 24 and 45 years were enrolled after providing written consent, from 1st April to 31th July, 2003. Subjects underwent a DXA (Prodigy, GE Lunar, USA) scan before and after a 6-week weight-loss program. This study was approved by the Institutional Review Board of Kyung Hee Oriental Medical Center. Fifty women were recruited and 12 dropped out during the study leaving 38 completers. Inclusion criteria required the subjects to be non-exercising, non-smoking, and not taking medications that could potentially influence body composition. Participants with diabetes mellitus, renal or hepatic problem, change of body weight over 3kg during previous 3 months, possibility of pregnancy, and taking oral contraceptives were excluded from this study. Data from a participant with a compliance rate of less than 70% was removed from analysis. Recruitment was done through newspaper advertisements and internet websites.
Protocol
Volunteers were provided with a traditional Korean herbal formula (Slim-diet) which is made as powder in Kyung Hee university oriental medical center pharmacy. Formula was taken 3 times a day, 30 minutes after each meal for 6 weeks. The ingredients of the formula are listed in Table 1. All of the contents are approved by the Korean FDA as food. Volunteers were informed that the formula was to help control their weight. In addition, a calorie-reducing diet was prescribed for each participant for the purpose of reducing estimated daily energy intake by 1000kcal/day thereby providing subjects with a daily energy intake of > 1200kcal/day. Participants had to personally decide what to eat and were required to maintain this prescribed diet for 6 weeks. Participants were required to walk or jog outdoors 3 times a week, for over 30 minutes. Participants were required to write a self-reporting diary so that the study staff could monitor their daily calorie intake and exercise.
Table 1.
Ingredients of the Herbal Diet Formula (Slim-Diet)
| Herb | Amount (g) | Herb | Amount (g) |
|---|---|---|---|
| Ginseng Radix | 2 | Rehmanniae Radix Preparat | 12 |
| Citri Pericarpium | 8 | Lycii Fructus | 8 |
| Mori Folium | 12 | Angelicae gigantis Radix | 4 |
| Coicis Semen | 12 | Cnidii Rhizoma | 4 |
| Poria | 8 | Benincasae Semen | 4 |
| Polyporus | 8 | Mori Ramulus | 4 |
| Acanthopanacis Cortex | 4 | Pini Folium | 4 |
| Eucommiae Cortex | 4 | TOTAL | 98 |
Anthropometrics
Body weight and height were measured to the nearest 0.1kg and 0.5cm respectively, wearing a hospital gown. Waist circumference and hip circumference were measured by the same observer twice according to the World Health Organization (WHO) method, mid-point between the lower end of the rib cage and top of the iliac crest in a standing position, which is usually 3cm above the anterior superior iliac spine.17
Dual-Energy X-ray Absorptiometry (DXA)
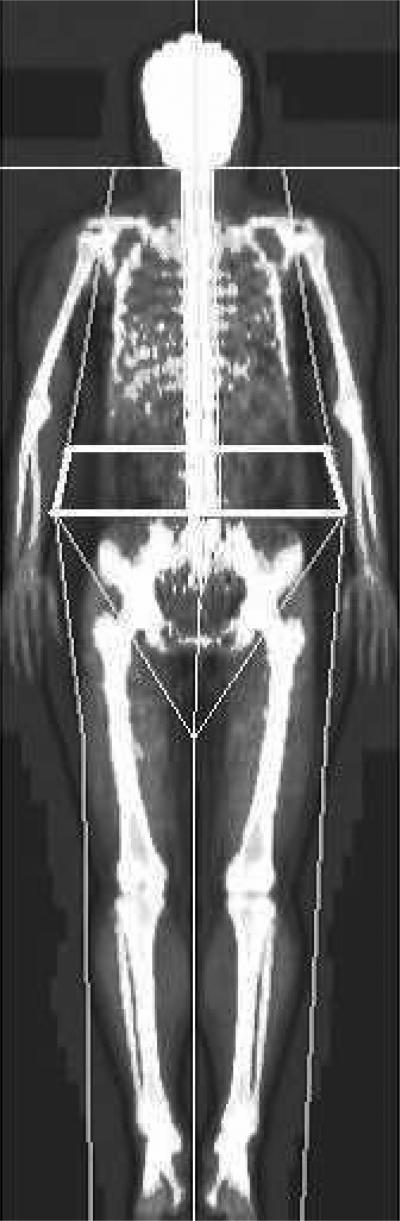
Fat free mass (FFM, body weight minus total body fat), bone mineral content (BMC) were measured with a whole-body DXA scanner (Prodigy, GE Lunar, USA) using version 9.3 software. A specific abdominal region of interest (ROI, upper L2 – upper iliac crest) was analyzed for fat tissue.13 Eight liters of methanol and water in bottles, simulating fat and fat-free soft tissues, were scanned daily as soft-tissue quality control markers. The range of measured CV for methanol and water over the study period was 0.062% and 0.112%. A DXA planogram demonstrating DXA ROI is presented in Figure 1.
Figure 1.
DXA planogram demonstrating DXA Region Of Interest (ROI): the upper edge of the second lumbar vertebra to above the iliac crest.
Statistical Analysis
All values are presented as mean ± SD. The statistical significance of the correlation between DXA ROI and WC was verified through correlation analysis (Pearson's correlation) and evaluated by simple linear regression analysis (SPSS 11.0 for windows). A p-value less than 0.05 was considered statistically significant.
RESULTS
Demographic characteristics of subjects
Subjects were 38 pre-menopausal Korean women between the ages of 24 and 45 and with a BMI of 26.2 to 41.0kg/m2. After the weight-loss program, BMI decreased to between 26.0 and 39.6kg/m2, showing statistically significant loss in weight. Eighteen subjects at baseline and 13 at follow-up had a BMI greater than 30kg/m2. Seven subjects at baseline and 5 at follow-up had a BMI greater than BMI 35kg/m2. All subjects’ BMI were less than 41kg/m2. Subject demographic and anthropometric characteristics are summarized in Table 2. DXA values at baseline and follow-up were also significantly reduced except for BMC (Table 3). The safety and efficacy of ‘Slim-Diet’ was reported previously by Song et al.18
Table 2.
Anthropometric Characteristics of Subjects (n=38)
| Baseline | Follow-up | Change | |
|---|---|---|---|
| Age (years) | 31.6±6.14 | ||
| Height (cm) | 160±5.34 | ||
| Weight (kg) | 81.3±11.5 | 78.4±10.9 | - 2.91±2.36* |
| BMI (kg/m2) | 31.7±3.50 | 30.6±3.36 | - 1.13±0.89* |
| Waist circumference (cm) | 94.4±7.05 | 91.4±7.20 | - 3.07±4.05* |
| Hip circumference (cm) | 112±7.02 | 112±17.0 | - 0.45±17.0 |
| Waist-to-hip ratio | 0.84±0.03 | 0.83±0.08 | - 0.01±0.08 |
| Waist-to-height ratio | 0.59±0.04 | 0.57±0.04 | - 0.02±0.03* |
Values are mean ± SD
Decreased significantly at p < 0.001(paired T test).
Table 3.
Body composition and abdominal fat measures by DXA (n=38)
| Baseline | Follow-up | change | p- value | |
|---|---|---|---|---|
| FFM (kg) | 45.9±6.18 | 45.1±6.00 | - 0.79±1.34 | 0.001 |
| BF (kg) | 34.5±6.63 | 32.9±6.64 | - 1.63±1.69 | 0.000 |
| Fat (%) | 42.8±3.71 | 42.0±3.65 | - 0.76±1.48 | 0.003 |
| BMC (kg) | 2.77±0.38 | 2.74±0.33 | - 0.03±0.15 | 0.298 |
| Trunk fat (kg) | 18.7±3.38 | 17.8±3.46 | - 0.90±1.17 | 0.000 |
| ROI (kg, upper L2- upper iliac) | 3.15±6.74 | 2.98±6.81 | -0.17±0.21 | 0.000 |
Values are mean ± SD; *, Decreased significantly at p < 0.001 (paired T test); FFM, fat free mass (DXA weight – body fat); BF, body fat; BMC, bone mineral content; ROI, region of interest (L2-upper iliac).
Association between DXA and anthropometry before and after weight-loss
Waist circumference showed the strongest correlation with DXA ROI and DXA trunk at baseline and BMI showed the highest correlation at follow-up. Correlations between DXA ROI and WC at baseline and follow-up (γ = 0.91, 0.84, respectively, p < 0.01) were not significantly different from the correlations between BMI (γ = 0.87, 0.88, respectively, p < 0.01) and WHtR (γ = 0.82, 0.82, respectively, p < 0.01). Correlations between DXA ROI and WHR were the lowest at baseline (γ = 0.46, p < 0.01) and were not significantly correlated at follow-up (γ = 0.23, p > 0.05) (Table 4).
Table 4.
Associations between DXA and Anthropometrics at baseline and follow-up of 6 week weight loss program (n=38)
| BMI | WC | WHR | WHtR | ||
|---|---|---|---|---|---|
| Trunk fat (DXA) | Baseline | 0.91** | 0.92** | 0.40** | 0.80** |
| Follow-up | 0.84** | 0.80** | 0.23 | 0.74** | |
| ROI (DXA) | Baseline | 0.87** | 0.91** | 0.46** | 0.82** |
| Follow-up | 0.88** | 0.84** | 0.23 | 0.82** |
Values are Pearson's correlation coefficient
significant at the 0.01 level (p-value)
*, significant at 0.05 level (p-value)
BMI, body mass index; WC, waist circumference; WHR, waist-to-hip ratio; WHtR, waist-to-height ratio; ROI, region of interest (upper L2-upper iliac).
Association between change of DXA ROI and anthropometry during weight-loss
The change in DXA ROI (ΔROI) showed significant correlations with ΔWC and ΔWHtR (γ = 0.39, 0.37, respectively, all p < 0.05) whereas the change in DXA conventional trunk fat (Δtrunk fat) was not significantly correlated with ΔWC or ΔWHtR (γ = 0.20, 0.19, respectively, all p > 0.05). The change in DXA ROI (ΔROI) was also highly correlated with weight and BMI (γ = 0.64, 0.63, respectively, all p < 0.01) (Table 5).
Table 5.
Associations between change in DXA measures and Anthropometry during weight-loss (n=38)
Values are Pearson's correlation coefficient
significant at the 0.01 level (p-value)
significant at 0.05 level (p-value)
BMI, body mass index; WC, waist circumference; WHR, waist-to-hip ratio; WHtR, waist-to-height ratio; ROI, region of interest (L2-upper iliac).
Prediction of DXA ROI through anthropometry
Linear regression analysis (y = abdominal fat, DXA ROI, x = WC) with DXA ROI as the dependent variable revealed that 83% and 71% of the variance in abdominal fat was predicted by WC at baseline and follow up. Fifteen percent of the variance for change of abdominal fat was predicted by WC (data not shown).
The result of a stepwise multiple regression analysis showed that 83% of the variance in AF (DXA ROI) was predicted by WC at baseline. After weight-loss, 83% of the variance in AF was predicted by BMI (77%), when WC (6%) was included as independent variables. The change of AF was predicted by BMI (40.3%) (Table 6).
Table 6.
Multiple-regression analysis DXA derived Abdominal Fat (DXA ROI, L2-upper iliac) prediction models
| Independent variable | Regression coefficient (±SE) | γ 2 | p | |
|---|---|---|---|---|
| Baseline | WC | 0.087(0.007) | 82.9% | <0.001 |
| Follow-up | BMI | 0.114(0.024) | 77.1% | <0.001 |
| WC | 0.038(0.012) | 82.5% | 0.003 | |
| Change | BMI | 1.53(0.314) | 40.3% | <0.001 |
DISCUSSION
WC is a well-known predictor of abdominal VAT and SAT.19 In 2001, the National Cholesterol Education Program – Adult Treatment Panel III (NCEP-ATP III) included WC as a risk factor for the metabolic syndrome.20 WC could possibly be a better predictor of risk of obesity for Asians as Asians have a tendency to have a higher percentage body fat and visceral fat than Caucasians and African Americans within the same BMI.21,22 However, the correlations between WC and VAT can range from 0.4 to 0.9, depending on sex, age, and severity of obesity. In older women, WC was shown to have a stronger correlation with total body fat (γ 2 = 0.69) than VAT (γ 2 = 0.40).23 But in pre-menopausal obese women, it has been reported that WC is strongly correlated with VAT by MRI (γ = 0.75).24 In the current study, participants were limited to pre-menopausal female.
Dual energy x-ray absorptiometry is a good method for body composition measurements as it differentiates three basic body components: bone mineral content, body fat, and lean tissue. However DXA does not distinguish intra-abdominal fat from subcutaneous fat. Because AF contains anterior and posterior subcutaneous fat, AF by DXA is a better predictor of total AF than intra-abdominal fat alone. In obese women, it has been reported that DXA was well correlated with VAT by MRI (γ = 0.74).24 Other studies carried out on obese women reported a similar correlation (γ range = 0.72 to 0.99) between AF measured by DXA and VAT measured by CT.9,11,12
To out knowledge, no study has previously compared differences before and after a weight-loss program. The present study indicates that a DXA ROI and DXA trunk fat have high correlations with WC, BMI, and WHtR before and after weight-loss in obese pre-menopausal Korean women. Highly correlated with DXA ROI were WC > BMI > WHtR at baseline (γ = 0.91, 0.87, 0.82, respectively and p < 0.01) and BMI > WC > WHtR at follow-up (γ = 0.88, 0.84, 0.82, respectively and p < 0.01).
The change in a DXA ROI (ΔROI) revealed the highest correlation with BMI (γ = 0.63, p < 0.01), followed by WC and WHtR (γ = 0.39, 0.37, respectively, p < 0.05). The change in conventional DXA trunk fat (Δtrunk fat) failed to show a significant correlation with ΔWC even after adjustment for age and total body fat, but was correlated with ΔBMI (γ = 0.44, p < 0.01)
We hypothesized that WC would be a good measure for the assessment of AF in Asian obese women in both cross-sectional and longitudinal studies where the latter reports on change in AF. However, the change in conventional DXA trunk fat (Δtrunk fat) failed to show a significant correlation with ΔWC even after adjustment for age and total body fat. When we adjusted DXA ROI instead, the correlation with ΔWC turned out to be significant. The change in a DXA ROI (ΔROI) revealed an association with WC and WHtR (γ = 0.39, 0.37, respectively, p < 0.05). WC was a better surrogate than WHR, which was only useful at baseline but not after weight loss in this study and in a previous study.25 The usefulness of ΔWC from DXA ROI in this study corresponds well with the result: ΔWC was associated with ΔVAT by MRI (γ = 0.80, p < 0.01; γ = 0.41, p < 0.05, respectively) reported in a previous study.26 We assume that the DXA ROI is more abdomen-specific and therefore a more valid index of abdominal adiposity than DXA trunk fat, however, more research is needed in this area.
Moreover, it would appear that BMI is a good surrogate for AF after weight loss. It showed the highest correlation with DXA trunk fat and DXA ROI at follow-up and with changes. ΔBMI was suggested as one of the best index of ΔVAT by MRI (γ = 0.85, p < 0.01) in obese-women27 where ΔBMI was better than ΔDXA ROI (lumbar vertebra 2 - 4, γ = 0.73, p < 0.01) for ΔVAT by MRI26. However, it should be noted that DXA estimates fat not adipose tissue which is similar but not identical.27
This study suggests that WC could be a useful predictor of AF both cross-sectionally and with weight loss induced changes. BMI could also be useful just after weight-loss. Future studies with a larger sample size and advanced imaging technique, such as CT or MRI, that can discriminate these data are necessary to further our understanding.
ACKNOWLEDGEMENTS
We give our thanks to Kil-Yeon Seo in the Department of the Nuclear Medicine of Kyung Hee Medical Center for analyzing the DXA data.
Footnotes
AUTHOR DISCLOSURES
Mi-Ja Hwang, Won-Suk Chung, Dympna Gallagher, Deog-Yoon Kim, Hyun-Dae Shin, and Mi-Yeon Song, no conflicts of interest.
REFERENCES
- 1.Ohlson LO, Larsson B, Svardsudd K, Welin L, Eriksson H, Wilhelmsen L, Bjorntorp P, Tibblin G. The influence of body fat distribution on the incidence of diabetes mellitus 13.5 years of follow-up of the participants in the study of men born in 1913. Diabetes. 1985;34:1055–8. doi: 10.2337/diab.34.10.1055. [DOI] [PubMed] [Google Scholar]
- 2.Seidell JC, Han TS, Feskens EJ, Lean ME. Narrow hips and broad waist circumferences independently contribute to increased risk of non-insulin-dependent diabetes mellitus. J Intern Med. 1997;242:401–6. doi: 10.1046/j.1365-2796.1997.00235.x. [DOI] [PubMed] [Google Scholar]
- 3.Lapidus L, Bengstsson C, Larsson B, Pennert K, Rybo E, Sjöström L. Distribution of adipose tissue and risk of cardiovascular disease and death: a 12 year follow up of participants in the population study of women in Gothenburg, Sweden. Br Med J. 1984;289:1257–61. doi: 10.1136/bmj.289.6454.1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park YW, Allison DB, Heymsfield SB, Gallagher D. Larger Amounts of visceral adipose tissue in Asian Americans. Obes Res. 2001;9:381–7. doi: 10.1038/oby.2001.49. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher D, Song MY. Evaluation of body composition: practical guidelines. In: Geroge AB, editor. Office management of obesity. Elservier; Newyork; Newyork: 2004. pp. 5–13. [Google Scholar]
- 6.Song MY, Kim J, Horlick M, Wang J, Pierson RN, Jr, Heo M, Gallagher D. Prepubertal Asians have less limb skeletal muscle. J Appl Physiol. 2002;92:2285–91. doi: 10.1152/japplphysiol.01066.2001. [DOI] [PubMed] [Google Scholar]
- 7.Kamimura MA, Avesani CM, Cendoroglo M, Canziani ME, Draibe SA, Cuppari L. Comparison of skinfold thickness and bioelectrical impedance analysis with dual-energy X-ray absorptiometry for the assessment of body fat in patients on long-term haemodialysis therapy. Nephrol Dial Transplant. 2003;18:101–5. doi: 10.1093/ndt/18.1.101. [DOI] [PubMed] [Google Scholar]
- 8.Schlemmer A, Hassager C, Haarbo J, Christiansen C. Direct measurement of abdominal fat by dual photon absorptiometry. Int J Obes. 1990;14:603–11. [PubMed] [Google Scholar]
- 9.Svendsen OL, Hassager C, Bergmann I, Christiansen C. Measurement of abdominal and intra-abdominal fat in postmenopausal women by dual x-ray absorptiometry and anthropometry: comparison with computerized tomography. Int J Obes Relat Metab Disord. 1993;17:45–51. [PubMed] [Google Scholar]
- 10.Taaffe DR, Lewis B, Marcus R. Regional fat distribution by dual-energy x-ray absorptiometry: comparison with anthropometry and application in a clinical trial of growth hormone and exercise. Clin Sci (Lond) 1994;87:581–6. doi: 10.1042/cs0870581. [DOI] [PubMed] [Google Scholar]
- 11.Jensen MD, Kanaley JA, Reed JE, Sheedy PF. Measurement of abdominal and visceral fat with computed tomography and dual-energy x-ray absorptiometry. Am J Clin Nut. 1995;61:274–8. doi: 10.1093/ajcn/61.2.274. [DOI] [PubMed] [Google Scholar]
- 12.Treuth MS, Hunter GR, Kekes-Szabo T. Estimating intraabdominal adipose tissue in women by dual-energy X-ray absroptiometry. Am J Clin Nutr. 1995;62:527–32. doi: 10.1093/ajcn/62.3.527. [DOI] [PubMed] [Google Scholar]
- 13.Park YW, Heymsfield SB, Gallagher D. Are dual-energy x-ray absorptiometry regional estimates associated with visceral adipose tissue mass? Int J Obes Relat Metab Disor. 2002;26:978–83. doi: 10.1038/sj.ijo.0801982. [DOI] [PubMed] [Google Scholar]
- 14.Jia WP, Lu JX, Xiang KS, Bao YQ, Lu HJ, Chen L. Prediction of abdominal visceral obesity from body mass index, waist circumference and waist-hip ratio in Chinese adults: receiver operating characteristic curves analysis. Biomed Environ Sci. 2003;16:206–11. [PubMed] [Google Scholar]
- 15.Chan DC, Watts GF, Barrett PH, Burke V. Waist circumference, waist-to-hip ratio and body mass index as predictors of adipose tissue compartments in men. QJM. 2003;96:441–7. doi: 10.1093/qjmed/hcg069. [DOI] [PubMed] [Google Scholar]
- 16.Lean MEJ, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311:158–64. doi: 10.1136/bmj.311.6998.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Eyben FE, Mouristen E, Holm J, Montvilas P, Dimcevski G, Suciu G, Helleberg I, Kristensen L, von Eyben R. Intra-abdominal obesity and metabolic risk factors: a study of young adults. Int J Obes Relat Metab Disord. 2003;27:941–9. doi: 10.1038/sj.ijo.0802309. [DOI] [PubMed] [Google Scholar]
- 18.Song MY, Chung WS, Shin HD. Clinical trial of herbal formula (Slim-diet) on weight loss in obese pre-menopausal Korean females. J Society of Kor Med for Obes Res. 2003;3(1):1–6. [Google Scholar]
- 19.Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr. 2002;75:683–8. doi: 10.1093/ajcn/75.4.683. [DOI] [PubMed] [Google Scholar]
- 20.Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 21.Fujimoto WY, Newell-Morris LL, Grote M, Bergstrom RW, Shuman WP. Visceral fat obesity and morbidity: NIDDM and atherogenic risk in Japanese-American men and women. Int J Obes. 1991;15:41–4. [PubMed] [Google Scholar]
- 22.Gallagher D, Heymisfield SB, Heo M, Jebb SA, Mrugatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72:694–701. doi: 10.1093/ajcn/72.3.694. [DOI] [PubMed] [Google Scholar]
- 23.Harris TB, Visser M, Everhart J, Cauley J, Tylaskey F, Fuerst T, Zamboni M, Taaffe D, Resnick HE, Scherzinger A, Nevitt M. Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women. The Health, Aging and Body Composition Study. Ann N Y Acad Sci. 2000;904:462–73. doi: 10.1111/j.1749-6632.2000.tb06501.x. [DOI] [PubMed] [Google Scholar]
- 24.Kamel EG, McNeill G, Van Wijk MC. Usefulness of anthropometry and DXA in predicting intra-abdominal fat in obese men and women. Obes Res. 2000;8:36–42. doi: 10.1038/oby.2000.6. [DOI] [PubMed] [Google Scholar]
- 25.van der Kooy K, Leenen R, Seidell JC, Deurenberg P, Droop A, Bakker CJG. Waist-hip ratio is a poor predictor of changes in visceral fat. Am J Clin Nutr. 1993;57:327–33. doi: 10.1093/ajcn/57.3.327. [DOI] [PubMed] [Google Scholar]
- 26.Kamel EG, McNeill G, Wijk MCWV. Change in intra-abdominal adipose tissue volume during weight loss in obese men and women: correlation between magnetic resonance imaging and anthropometric measurements. Int J Obes. 2000;24:607–13. doi: 10.1038/sj.ijo.0801204. [DOI] [PubMed] [Google Scholar]
- 27.Shen W, Wang Z, Punyanita M, Lei J, Sinav A, Kral JG, Imielinska C, Ross R, Heymsfield SB. Adipose tissue quantification by imaging methods : a proposed classification. Obes Res. 2003;11(1):5–16. doi: 10.1038/oby.2003.3. [DOI] [PMC free article] [PubMed] [Google Scholar]