Abstract
Aims
Positive affect is believed to predict cardiovascular health independent of negative affect. We examined whether higher levels of positive affect are associated with a lower risk of coronary heart disease (CHD) in a large prospective study with 10 years of follow-up.
Methods and results
We examined the association between positive affect and cardiovascular events in 1739 adults (862 men and 877 women) in the 1995 Nova Scotia Health Survey. Trained nurses conducted Type A Structured Interviews, and coders rated the degree of outwardly displayed positive affect on a five-point scale. To test that positive affect predicts incident CHD when controlling for depressive symptoms and other negative affects, we used as covariates: Center for Epidemiological Studies Depressive symptoms Scale, the Cook Medley Hostility scale, and the Spielberger Trait Anxiety Inventory. There were 145 (8.3%) acute non-fatal or fatal ischaemic heart disease events during the 14 916 person-years of observation. In a proportional hazards model controlling for age, sex, and cardiovascular risk factors, positive affect predicted CHD (adjusted HR, 0.78; 95% CI 0.63–0.96 per point; P = 0.02), the covariate depressive symptoms continued to predict CHD as had been published previously in the same patients (HR, 1.04; 95% CI 1.01–1.07 per point; P = 0.004) and hostility and anxiety did not (both P > 0.05).
Conclusion
In this large, population-based study, increased positive affect was protective against 10-year incident CHD, suggesting that preventive strategies may be enhanced not only by reducing depressive symptoms but also by increasing positive affect.
Keywords: Positive affect, Coronary artery disease, Depressive symptoms, Hostility, Anxiety
See page 1036 for the editorial comment on this article (doi:10.1093/eurheartj/ehq031)
Introduction
Previous studies have found that positive affect is associated with increased survival, improved immune function, and lower risk of diabetes and hypertension,1–4 whereas negative emotions such as anger/hostility5 and depression6,7 are associated with a higher risk of incident coronary heart disease (CHD). Positive affect is defined as the experience of pleasurable emotions such as joy, happiness, excitement, enthusiasm, and contentment.8 These feelings can be transient, but they are usually stable and trait-like, particularly in adulthood.3 Interestingly, positive affect is largely independent of negative affect, as someone who is generally a happy, contented person can also occasionally be anxious, angry, or depressed.9 Positive affect has been proposed as a protective factor for ill-health for many years.1–3 However, there has been little research to address the question of whether positive affect protects against CHD.2,4,10 We therefore examined whether clinically assessed positive affect is associated with a reduced risk of incident CHD independent of negative affect using data from a large population-based sample.
Methods
Study population
The Canadian Nova Scotia Health study11 is a population-based survey implemented by Heart Health Nova Scotia in partnership with the Nova Scotia Department of Health to estimate the distributions of selected health indicators and preventive practices of Nova Scotians. The sample was constructed based on a probability sample designed by Statistics Canada, the national statistical agency and census bureau, to be representative of the Nova Scotian population by age, gender, and geographic location. The targeted population consisted of all non-institutionalized Nova Scotians aged 18 and above whose names were listed in the Medical Service Insurance register, the government-sponsored, universal health insurance plan. The overall recruitment percentage (72%) is comparable to other large health surveys, and weights applied from propensity analyses to test for response bias revealed no meaningful biases.12 Pregnant women were excluded from the survey, as their CHD risk factors (e.g. weight, blood pressure, diabetes, etc.) were not considered stable at entry.
A group of 29 public health nurses took part in a 5-day training session on how to properly contact the identified participants and how to accurately collect data using the standardized measures. From March through November 1995, the nurses collected data by contacting survey participants, immediately interviewing those who agreed to participate. Participants were asked to attend health-care clinic 7 days after the interview for assessment of height and weight and to provide a fasting blood sample for lipid determination and sample banking. During the clinic visit, participants were asked to complete a structured interview that was videotaped for subsequent scoring. Further details of the study procedures have been previously published.11,13
Participants provided written consent, allowing linkage to their future and past health-care utilization data and for the storage and future use of videotapes. We restricted our sample to those who had attended the clinic session and completed the structured interview with no hospital discharge diagnoses of CHD in the 5 years prior to the baseline survey, determined by their single-payer electronic medical records (see below). IRB approval was originally obtained for the baseline protocol and was subsequently obtained for these analyses at both Dalhousie University in Canada and Columbia University in New York.
Assessment of coronary heart disease risk factors
At the baseline visit, we measured the levels of each component of the Framingham risk score, including sex, age, total cholesterol, HDL cholesterol, blood pressure, history of diabetes, and cigarette smoking.14 Nurses measured weight and height twice and reported the average of the two measurements for each. The averaged values were used to calculate body mass index (calculated as weight in kilograms divided by height in metres squared). Participants also reported if a physician had ever diagnosed them as having diabetes mellitus. Registered nurses measured resting systolic (SBP) and diastolic (DBP) blood pressures using a manual random zero sphygmomanometer. Two readings from home and two readings from the clinic session (usually 1 week later) were averaged to create the resting SBP and DBP measurements. Total cholesterol and high-density cholesterol were assayed from plasma samples by the Lipid Research Laboratory, University of Toronto.15 Low-density lipoprotein cholesterol was calculated using the Friedewald formula.16 Those who reported smoking in the last year or who reported smoking currently were categorized as smokers, and the remainder were coded as non-smokers.
Assessment of self-reported psychosocial risk factors
Three negative affect measures were included as covariates to test if positive affect was independently predictive of incident CHD.
Depressive symptoms
Depressive symptoms were measured using the Centers for Epidemiological Studies-Depressive symptoms (CES-D) scale,17 a 20-item self-report instrument that was designed for use in epidemiological studies as a measure of current level of depressive symptoms. Higher scores reflect increased depressive symptoms.
Hostility
Hostility was assessed with the Cook-Medley Hostility scale;18 50 true–false items commonly used to assess self-reported hostility.19,20
Anxious symptoms
Anxious symptoms were assessed with the Trait-subscale of the State-Trait Anxiety scale,21 a 20-item test that describes symptoms of anxiety (e.g. I worry too much over something that really doesn't matter). The scale requires respondents to indicate how frequently they experience a variety of anxiety symptoms using a four-point Likert scale.
Clinically assessed positive affect
The Expanded Structured Interview is a 12 min, interpersonally stressful interview designed to assess anger expression and stress reactions by asking participants about their characteristic responses to a variety of different situations.22 The interview is based on the original Type A Structured Interview,23 with additional questions on anger expression and interpersonal stress at work. Positive affect is a rating of the degree to which the participant expresses positive emotions, whether verbally or in behaviour (e.g. smiling) or tone of responses (e.g. cheerful). Positive affect may be demonstrated during the interview or can be based on the participant's level of positive affect reported to occur during day-to-day situations.
There are four steps to the creation of observer-based positive affect scores.24 First, nurse interviewers were trained and certified to conduct the structured interview and ensure that it was properly recorded on videotape. Second, the recorded interview was viewed to ensure the interviewer followed the script, and only those that passed interview quality filters were included. Third, staff were trained on how to properly code the interviews. Fourth, coding was randomly audited and only those staff passing preset reliability requirements were retained.
All interviews were scored for positive affect, rated from 1 (no positive affect expressed) to 5 (extreme positive affect) by the 23 certified coders. All coders additionally rated a common 30 tapes (unbeknownst to them). Three coders were found to be unreliable, and their tapes were then reassessed by another, reliable coder from the original bank of coders, whose data were then checked again at the end of the coding phase.
Surveillance of incident coronary heart disease
The main outcome variable was discharge documentation of incident fatal or nonfatal ischaemic heart disease determined by hospital discharge codes or death certificates [International Classification of Diseases (ICD)-9 codes25 (410–414) and ICD-10 codes26 (I21–I25). This included acute myocardial infarction (MI) and other forms of acute ischaemic heart disease, but excluded old or previous MIs (codes 412 and I22/I25.2). Because of the universal health care insurance system in Nova Scotia, data from the provincial health-care database provide accurate documentation for hospitalizations and outpatient visits of all residents, regardless of event or treatment location.27 Immediately upon discharge, physicians submit ICD codes to Department of Health. A data quality committee from the Department of Health of Nova Scotia meets regularly with health records personnel to ensure accuracy, conduct random chart reviews, and to adjudicate discrepancies in data entry. In order to limit the analyses to incident events, we excluded anyone with a CHD diagnosis prior to their baseline survey by searching for documentation of a CHD event in the 5 years prior to their survey date using the data sources described above.
All deaths are reported to provincial offices, which in turn notify the national census bureau, Statistics Canada, which applies a nationally consistent process of determining the underlying cause of death. Specifically, these data were converted to the ICD codes by staff at Statistics Canada, and only those codes listed above qualified as fatal CHD. Data were extracted by Population Health Unit of Dalhousie University. Participants were observed for up to 10 years, from the date of their initial visit in 1995 until the earliest of the following: 10-year anniversary of their initial visit date or March 2005 or the date of emigration, death from causes other than CHD, or documented incident CHD.
Data analysis
We conducted t-tests and χ2 tests on levels of cardiovascular risk factors to compare those with vs. those without an available positive affect score. The Cochran–Armitage test for trend was used to test for a linear trend in binomial proportions across levels of positive affect, and analysis of variance contrast analysis was used to test for linear trends in mean levels of continuous measures. Coder reliability was assessed by calculating the correlation between each coders' ratings and the average of the other coders' ratings (corrected item–total correlation) on the common 30 tapes.28 We constructed Cox proportional hazards models to estimate the adjusted hazard ratios of incident CHD by level of positive affect. Models were adjusted for age at baseline, sex, cardiovascular risk factors, and three negative affect scales of depression, hostility, and anxiety. All models were stratified by geographic region of the sampling frame. Because some of the participants were missing data on baseline characteristics, we calculated the average of the hazard ratio estimates based on five Markov chain Monte Carlo multiple imputations of the data set.29 We tested the proportional hazards assumption using the Kolmogorov-type supremum test30 based on 1000 simulated replications, and there was no evidence of violation of this assumption (P = 0.64). We examined the association between positive affect and CHD incidence non-parametrically with restricted cubic splines to provide a more accurate representation of the dose–response curve. Tests for non-linearity used the likelihood ratio test, comparing the model with only the linear term to the model with the linear and the cubic spline terms.31 All analyses were performed using SAS statistical software (version 9.1), and statistical significance was defined by a two-sided P ≤ 0.05.
Results
This prospective study included 1739 participants (862 men, 877 women) from the Nova Scotia Health Survey who were greater than 18 years old with no known CHD at baseline and who completed the survey, clinic exam, and structured interview. Compared with the 481 NSHS95 participants with no positive affect score, the 1739 included participants were younger (average age = 46.2 vs. 49; t = −2.87, P = 0.004), less hostile (19.0 vs. 20.7; t =− 3.32, P = 0.001), they were less likely to be male (44.0% vs. 49.5%; χ = 4.47; P = 0.035), and they had higher levels of diastolic pressures (average = 77.0 vs. 75.8; t = 2.14, P = 0.033). Table 1 shows the baseline characteristics of the 1739 participants included in the analysis. Those with higher levels of positive affect were more likely to be female (P < 0.001), less likely to be current smokers (P < 0.001), and they had lower levels of total cholesterol (P = 0.03), SBP (P = 0.008), and DBP (P = 0.006), levels of hostility (P < 0.001) and anxious symptoms (P = 0.03), suggesting that higher levels of positive affect are related to better overall health.
Table 1.
Baseline characteristics by level of positive affect expression
| Variable | Levels of positive affect |
P-value trenda | |||||
|---|---|---|---|---|---|---|---|
| Total | None | Little | Moderate | Quite a bit | Extreme | ||
| (N = 1739) | (n = 168) | (n = 755) | n = 592) | (n = 193) | (n = 31) | ||
| Age | 46.2 ± 18.0 | 45.6 ± 18.1 | 47.1 ± 17.8 | 45.7 ± 18.4 | 44.7 ± 17.5 | 45.6 ± 19.3 | 0.24 |
| Male | 862 (49.6%) | 112 (66.7%) | 411 (54.4%) | 264 (44.6%) | 68 (35.2%) | 7 (22.6%) | <0.001 |
| Active smoking | 451 (25.9%) | 58 (34.5%) | 206 (27.3%) | 142 (24.0%) | 38 (19.7%) | 7 (22.6%) | <0.001 |
| Body mass index (kg/m2) | 27.1 ± 5.6 | 27.5 ± 5.5 | 27.1 ± 5.4 | 27.1 ± 5.8 | 26.4 ± 4.9 | 27.7 ± 7.4 | 0.23 |
| Diabetes mellitus | 65 (3.7%) | 7 (4.2%) | 32 (4.2%) | 18 (3.0%) | 7 (3.4%) | 1 (3.2%) | 0.41 |
| Total cholesterol (mmol/L) | 5.3 ± 1.1 | 5.4 ± 1.2 | 5.3 ± 1.1 | 5.3 ± 1.1 | 5.2 ± 0.9 | 4.9 ± 1.2 | 0.03 |
| Low density lipids (mmol/L) | 3.2 ± 0.9 | 3.2 ± 0.9 | 3.3 ± 0.9 | 3.2 ± 0.9 | 3.2 ± 0.9 | 2.9 ± 1.0 | 0.24 |
| Systolic blood pressure (mmHg) | 124.7 ± 17.0 | 126.5 ± 16.2 | 125.6 ± 17.4 | 123.4 ± 16.6 | 123.6 ± 16.7 | 121.7 ± 18.9 | 0.008 |
| Diastolic blood pressure (mmHg) | 77.0 ± 9.7 | 78.7 ± 10.0 | 77.3 ± 10.0 | 76.4 ± 9.4 | 76.1 ± 9.4 | 76.6 ± 10.7 | 0.006 |
| Depressive symptoms | 7.4 ± 8.1 | 8.9 ± 9.4 | 7.3 ± 8.2 | 7.1 ± 7.8 | 6.9 ± 7.6 | 7.8 ± 6.6 | 0.06 |
| Hostility | 19.0 ± 8.1 | 21.1 ± 8.3 | 19.4 ± 8.4 | 18.4 ± 7.9 | 17.4 ± 7.1 | 17.3 ± 6.5 | <0.001 |
| Anxiety | 36.6 ± 8.4 | 37.6 ± 9.8 | 36.9 ± 8.2 | 36.3 ± 8.3 | 36.0 ± 7.9 | 35.5 ± 8.6 | 0.03 |
aχ2 Cochran–Armitage trend test or analysis of variance linear trends.
Coder reliability among pairs of coders was 0.90. No single coder appeared to be an outlier when examining the corrected item–total correlations. Positive affect was only minimally correlated with the negative affect measures of depressive symptoms (r = −0.04), hostility (r = −0.12), and anxious symptoms (r = −0.05), suggesting these measures had little common variance.
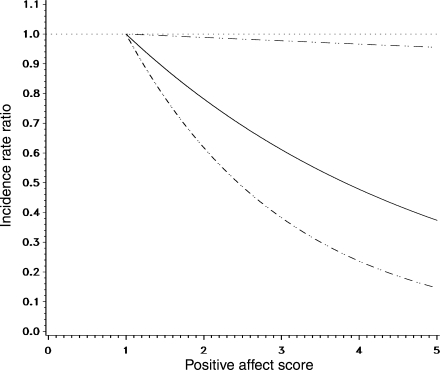
There were 145 (8.3%) incident CHD events (136 non-fatal, 9 fatal) during the 14 916 person-years of observation (incidence rate, 9.72 events/1000 person-years). Table 2 presents the Cox proportional hazards regression analyses. Even after adjusting for age, sex, cardiovascular risk factors, and negative affect, the rate of incident CHD was 22% lower for one point increase in positive affect score (95% CI 0.63–0.96; P = 0.02). The test for linear relation indicated that the association is indeed linear (P = 0.04). Figure 1 presents multivariate adjusted dose–response curve using a cubic spline in the fully adjusted model.
Table 2.
Hazard ratios (and 95% confidence intervals) for one unit increase in each psychosocial measure
| Predictor | Hazard rate (95% confidence interval) |
||
|---|---|---|---|
| Model 1a | Model 2b | Model 3c | |
| Positive affect | 0.73 (0.59–0.90) | 0.77 (0.63–0.95) | 0.78 (0.63–0.96) |
| Depressive symptoms | 1.04 (1.02–1.06) | 1.03 (1.01–1.05) | 1.04 (1.01–1.07) |
| Hostility | 1.02 (1.00–1.04) | 1.02 (1.00–1.04) | 1.01 (0.99–1.03) |
| Anxious symptoms | 1.01 (0.99–1.03) | 1.01 (0.99–1.03) | 0.97 (0.95–1.00) |
Baseline rates were allowed to vary by region.
aAdjusted for age at baseline (continuous) and sex.
bAdjusted for variables in Model 1 and smoking (smoking actively or within the past year vs. all others), history of diabetes mellitus (yes/no), body mass index (kg/m2), total cholesterol (mmol/L), low-density lipoprotein (mmol/L), systolic blood pressure (mmHg), and diastolic blood pressure (mmHg), measured as continuous terms.
cAdjusted for variables in Model 2 and symptoms of negative affect (continuous variables).
Figure 1.
Cubic spline analysis of the incidence rate ratio comparing each level of positive affect to a score of 1. Solid line indicates point estimate and dashed lines indicate 95% confidence interval. Dotted line indicates no association.
Discussion
In this large, randomly selected population-based study, increased positive affect was associated with a reduced risk of 10-year incident CHD, even after adjustment for depressive symptoms, hostility, and anxiety. To our knowledge, this is the first prospective study to examine this relationship.
Recent studies have begun to explore the protective effects of positive affect on physical health, including cardiovascular risk factors such as hypertension and diabetes.1–3 Prospective observational studies have reported an inverse association between positive affect and incident stroke32 and mortality in medical in-patients33 as well as diabetic patients,34 and others have shown that positive affect is protective against recurrent major clinical events in patients with cardiac stents.35 In the largest study to date, the Whitehall II cohort study did not find evidence of positive affect protecting against incident CHD, independent of negative affect.36 However, these studies utilized measurements of positive affect that were not ideal.37 In fact, some of these studies measured positive affect using instruments that were designed to assess depressive symptoms. In this analysis, trained observers estimated levels of positive affect rather than relying on self-reported levels or items originally designed to assess negative affect.
Positive affect, joy, happiness, and excitement, have previously been shown to be largely independent of negative affect.9 In our data, there was also a negligible correlation between positive affect and depressive symptoms. We had previously found that depressive symptoms were a significant predictor of CHD incidence in this sample, and so thought it was important to control for this important psychosocial risk factor.38 Our findings are consistent with an independent and clinically relevant relationship between CHD and positive affect (22% relative risk reduction for each one-point increment in positive affect on a five-point scale), a relationship that was not attenuated by adjustment for depressive symptoms.
Possible pathophysiological mechanisms
Various mechanisms may explain the potential cardiovascular benefits of higher levels of positive affect. For example, positive affect, but not negative affect, has been shown to predict enhanced parasympathetic modulation of heart rate.39 Positive affect is associated with blunted SBP, DBP, and norepinephrine reactivity during a standardized, stressful laboratory task and with lowered 30 min post-awakening cortisol levels in these same subjects.40 Increased positive affect may protect against CHD via improvements in sleep habits and smoking cessation. Steptoe et al.41 have found that higher positive affect is predictive of better sleep quality, independent of negative affect and other predictors of poor sleep, and Strong et al.42 found that higher levels of positive affect are associated with fewer urges to smoke during smoking cessation treatment, independent of levels of negative affect. However, further research is needed to explain the mechanisms by which positive affect might confer long-term CHD protection.3,43
Study limitations
Among the limitations of our analysis is the fact that information on cardiovascular risk factors were only measured at baseline and therefore, some misclassification is likely. Over the duration of follow-up, it is likely that patients experienced changes in their cardiovascular risk factors (e.g. development of diabetes), health behaviors (e.g. changes in physical activity or smoking status) and medications (e.g. starting or stopping cardio-protective drugs). However, this misclassification would likely have been non-differential and would lead to an underestimation of results. Similarly, levels of positive affect were also only measured at baseline and changes may have occurred over the 10 years of follow-up. First impressions of positive affect, even by strangers, are remarkably reliable and are in high agreement with ratings done by trained coders, life partners, clinicians, the person, and close friends.44 These ratings are also remarkably stable across decades of adulthood.45 It nevertheless remains possible that misclassification occurred, which again would have led to underestimation of the protection conferred by positive affect.
We aimed to exclude survey participants with pre-existing CHD. Therefore, we excluded participants with any self-reported CHD or CHD events documented in the patient charts for the 5 years prior to the survey date. However, since electronic records did not exist prior to 1990, it is not possible to obtain information farther back. Therefore, some participants who may have experienced prior CHD events more than 5 years before the baseline survey and denied a history of CHD may have been included in the current analysis. If those who experienced CHD events more than 5 years prior to the baseline visit were also more likely to demonstrate lower levels of positive affect, the results may be an overestimate of the true association.
Since this is an observational study, we cannot rule out the possibility of unmeasured or residual confounding. Participants with data available on positive affect were younger, less likely to be male, less likely to be hostile, and had higher blood pressures than the participants without positive affect scores who were excluded from this analysis. If those who were excluded differed greatly in their risk of CHD and also in their (unknown) levels of positive affect, it is possible that our results may be at least partially accounted for by a selection bias. Therefore, confirmatory studies are needed. Strengths of our analysis include the relatively large sample size, use of a structured interview with standardized assessment of positive affect, inclusion of standard negative affect scales as covariates, and long-term follow-up.
Conclusions and clinical implications
In summary, in this prospective population-based study, we found that positive affect was independently associated with risk of CHD. The positive affect we assessed is relatively easy to judge in a clinical situation. Does the patient smile and appear able to enjoy some aspects of life during the clinical interview or medical history taking? Do they report that they experience pleasure or excitement with some parts of their daily life? Assessment of positive affect may complement evaluations for CHD risk that only assess negative emotions such as depression.
Potential interventions to augment positive affect are usually labelled behavioral activation interventions,46 in which a patient notes which hobbies, daily activities, or other habits are enjoyable, with instructions to pursue those activities with increased and documented daily frequency. Conducting such a simple intervention results in patient-reported increases in quality of life. In fact, most successful depression interventions include increasing positive affect, as well as decreasing negative affect, as key components to psychotherapy.47 Furthermore, a recent study reports that the use of antidepressants without psychotherapy can result in lower levels of positive affect.48 Randomized controlled trials directly increasing positive affect in cardiopulmonary patients are now underway.49 However, as we report findings from an observational study, we do not yet have evidence to suggest that regular assessment of positive and negative affect should be recommended. Whether increasing positive affect would decrease the risk for CHD is an exciting, but as of yet untested hypothesis, remaining to be addressed.
Funding
The study was supported by grants HL-088117, HL-076857, HL-084034, HL-080665, HC25197, and HL-04458 from the National Institutes of Health, Bethesda, MD. This project was also supported by Grant UL1 RR024156 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. The National Health & Welfare of Canada, the Nova Scotia Department of Health, and the Heart and Stroke foundation of Canada all supported the original data collection. The study sponsors had no role in the study design, collection, analysis, writing, or interpretation.
Conflict of interest: none declared.
References
- 1.Fredrickson BL. What good are positive emotions? Rev Gen Psych. 1998;2:300–319. doi: 10.1037/1089-2680.2.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131:925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 4.Richman LS, Kubzansky L, Maselko J, Kawachi I, Choo P, Bauer M. Positive emotion and health: going beyond the negative. Health Psychol. 2005;24:422–429. doi: 10.1037/0278-6133.24.4.422. [DOI] [PubMed] [Google Scholar]
- 5.Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychol Bull. 2005;131:260–300. doi: 10.1037/0033-2909.131.2.260. [DOI] [PubMed] [Google Scholar]
- 6.Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. Am J Prev Med. 2002;23:51–61. doi: 10.1016/s0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- 7.Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27:2763–2774. doi: 10.1093/eurheartj/ehl338. [DOI] [PubMed] [Google Scholar]
- 8.Tomkins SS. Affect Imagery Consciousness: The Positive Affects. New York, NY: Springer Publishing Inc; 1963. [Google Scholar]
- 9.Diener E, Emmons RA. The independence of positive and negative affect. J Pers Soc Psychol. 1984;47:1105–1117. doi: 10.1037//0022-3514.47.5.1105. [DOI] [PubMed] [Google Scholar]
- 10.Rozanski A, Kubzansky LD. Psychologic functioning and physical health: a paradigm of flexibility. Psychosom Med. 2005;67:S47–S53. doi: 10.1097/01.psy.0000164253.69550.49. [DOI] [PubMed] [Google Scholar]
- 11.MacLean D, Scott J, Beanlands H, Hood R, Cogdon A, LeBlanc B, Davidson KW, Mills T, Wolf H, Elliott D, Kephart G, Farquharson J. The 1995 Nova Scotia Health Survey. Halifax, Nova Scotia: Department of Health; 1996. [Google Scholar]
- 12.Lawson BJ. Evaluation of Non-response Bias in the Nova Scotia Health Survey 1995. Halifax, Nova Scotia: Canada: Dalhousie University; 1999. [Google Scholar]
- 13.Rowan PJ, Haas D, Campbell JA, Maclean DR, Davidson KW. Depressive symptoms have an independent, gradient risk for coronary heart disease incidence in a random, population-based sample. Ann Epidemiol. 2005;15:316–320. doi: 10.1016/j.annepidem.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 15.Connelly PW, MacLean DR, Horlick L, O'Connor B, Petrasovits A, Little JA. Plasma lipids and lipoproteins and the prevalence of risk for coronary heart disease in Canadian adults. Canadian Heart Health Surveys Research Group. CMAJ. 1992;146:1977–1987. [PMC free article] [PubMed] [Google Scholar]
- 16.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 17.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 18.Cook W, Medley D. Proposed hostility and pharasaic-virtue scales for the MMPI. J Appl Psychol. 1954;38:414–418. [Google Scholar]
- 19.Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA. 2003;290:2138–2148. doi: 10.1001/jama.290.16.2138. [DOI] [PubMed] [Google Scholar]
- 20.Iribarren C, Sidney S, Bild DE, Liu K, Markovitz JH, Roseman JM, Matthews K. Association of hostility with coronary artery calcification in young adults: the CARDIA study. Coronary Artery Risk Development in Young Adults. JAMA. 2000;283:2546–2551. doi: 10.1001/jama.283.19.2546. [DOI] [PubMed] [Google Scholar]
- 21.Spielberger C, Gorusch R, Luschene R. Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press; 1970. [Google Scholar]
- 22.Hall P, Davidson KW, MacGregor MW, MacLean D. Expanded Structured Interview Administration Manual: Nova Scotia Health Survey 1995 (NSHS-95) Halifax, Nova Scotia: Dalhousie University, Heart Health Nova Scotia; 1998. [Google Scholar]
- 23.Rosenman RH. The interview method of assessment of the coronary-prone behavior pattern. In: Dembroski TM, Weiss SM, Shields JL, Haynes SG, Feinlab M, editors. Coronary-Prone Behavior. New York: Springer Verlag; 1987. pp. 55–70. [Google Scholar]
- 24.Davidson KW, MacGregor MW, Stuhr J, Dixon K, MacLean D. Constructive anger verbal behavior predicts blood pressure in a population-based sample. Health Psychol. 2000;19:55–64. doi: 10.1037//0278-6133.19.1.55. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. International Classification of Diseases, Ninth Revision (ICD-9) Geneva, Switzerland: World Health Organization; 1977. [Google Scholar]
- 26.World Health Organization. International Statistical Classification of Diseases, 10th Revision (ICD-10) Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 27.Manga P, Broyles RW, Angus DE. The determinants of hospital utilization under a universal public insurance program in Canada. Med Care. 1987;25:658–670. doi: 10.1097/00005650-198707000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Nunnally JC. Psychometric Theory. 2 ed. New York: McGraw-Hill; 1978. [Google Scholar]
- 29.Schafer JL. Analysis of Incomplete Multivariate Data. Boca Raton: CRC Press; 1997. [Google Scholar]
- 30.Lin DY, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of Martingale-based residuals. Biometrika. 1993;80:557–572. [Google Scholar]
- 31.Govindarajulu U, Spiegelman D, Thurston SW, Eisen EA. Comparing smoothing techniques for modeling exposure-response curves in Cox models. Stat Med. 2007;26:3735–3752. doi: 10.1002/sim.2848. [DOI] [PubMed] [Google Scholar]
- 32.Ostir GV, Markides KS, Peek MK, Goodwin JS. The association between emotional well-being and the incidence of stroke in older adults. Psychosom Med. 2001;63:210–215. doi: 10.1097/00006842-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Scherer M, Herrmann-Lingen C. Single item on positive affect is associated with 1-year survival in consecutive medical inpatients. Gen Hosp Psychiatry. 2009;31:8–13. doi: 10.1016/j.genhosppsych.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 34.Moskowitz JT, Epel ES, Acree M. Positive affect uniquely predicts lower risk of mortality in people with diabetes. Health Psychol. 2008;27:S73–S82. doi: 10.1037/0278-6133.27.1.S73. [DOI] [PubMed] [Google Scholar]
- 35.Denollet J, Pedersen SS, Daemen J, de Jaegere P, Serruys PW, van Domburg RT. Reduced positive affect (anhedonia) predicts major clinical events following implantation of coronary-artery stents. J Intern Med. 2008;263:203–211. doi: 10.1111/j.1365-2796.2007.01870.x. [DOI] [PubMed] [Google Scholar]
- 36.Nabi H, Kivimaki M, De Vogli R, Marmot MG, Singh-Manoux A. Positive and negative affect and risk of coronary heart disease: Whitehall II prospective cohort study. BMJ. 2008;337:a118. doi: 10.1136/bmj.a118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chang VW. Affect and heart disease. BMJ. 2008;337:a177. doi: 10.1136/bmj.a177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davidson KW, Schwartz JE, Kirkland SA, Mostofsky E, Fink D, Guernsey D, Shimbo D. Relation of inflammation to depression and incident coronary heart disease (from the Canadian Nova Scotia Health Survey [NSHS95] prospective population study) Am J Cardiol. 2009;103:755–761. doi: 10.1016/j.amjcard.2008.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhattacharyya MR, Whitehead DL, Rakhit R, Steptoe A. Depressed mood, positive affect, and heart rate variability in patients with suspected coronary artery disease. Psychosom Med. 2008;70:1020–1027. doi: 10.1097/PSY.0b013e318189afcc. [DOI] [PubMed] [Google Scholar]
- 40.Brummett BH, Boyle SH, Kuhn CM, Siegler IC, Williams RB. Positive affect is associated with cardiovascular reactivity, norepinephrine level, and morning rise in salivary cortisol. Psychophysiology. 2009;46:862–869. doi: 10.1111/j.1469-8986.2009.00829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Steptoe A, O'Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. J Psychosom Res. 2008;64:409–415. doi: 10.1016/j.jpsychores.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 42.Strong DR, Kahler CW, Leventhal AM, Abrantes AM, Lloyd-Richardson E, Niaura R, Brown RA. Impact of bupropion and cognitive-behavioral treatment for depression on positive affect, negative affect, and urges to smoke during cessation treatment. Nicotine Tob Res. 2009;11:1142–1153. doi: 10.1093/ntr/ntp111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Steptoe A, Wardle J. Positive affect and biological function in everyday life. Neurobiol Aging. 2005;26(Suppl. 1):108–112. doi: 10.1016/j.neurobiolaging.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 44.McCrae RR, Weiss A. Observer ratings of personality. In: Robins RW, Fraley CF, Krueger RF, editors. Handbook of Research Methods in Personality Psychology. New York: Guildford Press; 2007. [Google Scholar]
- 45.Conley JJ. Longitudinal stability of personality traits: a multitrait-multimethod-multioccasion analysis. J Pers Soc Psychol. 1985;49:1266–1282. doi: 10.1037//0022-3514.49.5.1266. [DOI] [PubMed] [Google Scholar]
- 46.Hopko DR, Lejuez CW, Ruggiero KJ, Eifert GH. Contemporary behavioral activation treatments for depression: procedures, principles, and progress. Clin Psychol Rev. 2003;23:699–717. doi: 10.1016/s0272-7358(03)00070-9. [DOI] [PubMed] [Google Scholar]
- 47.Cuijpers P, van Straten A, Warmerdam L. Behavioral activation treatments of depression: a meta-analysis. Clin Psychol Rev. 2007;27:318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 48.Price J, Cole V, Goodwin GM. Emotional side-effects of selective serotonin reuptake inhibitors: qualitative study. Br J Psychiatr. 2009;195:211–217. doi: 10.1192/bjp.bp.108.051110. [DOI] [PubMed] [Google Scholar]
- 49.Charlson ME, Boutin-Foster C, Mancuso CA, Peterson JC, Ogedegbe G, Briggs WM, Robbins L, Isen AM, Allegrante JP. Randomized controlled trials of positive affect and self-affirmation to facilitate healthy behaviors in patients with cardiopulmonary diseases: rationale, trial design, and methods. Contemp Clin Trials. 2007;28:748–762. doi: 10.1016/j.cct.2007.03.002. [DOI] [PubMed] [Google Scholar]