Abstract
Purpose
To test the reliability and validity of questionnaires shortened from the National Eye Institute 25-item Vision Function Questionnaire (NEI VFQ-9 and NEI VFQ-8).
Design
A cross-sectional multi-center cohort study.
Methods
Reliability was assessed by Cronbach alpha coefficients. Validity was evaluated by studying the association of vision-targeted quality-of-life composite scores with objective visual function measurements.
Study population: A total of 5,482 women between the ages of 65 and 100 years participated in the Year-10 clinic visit in the Study of Osteoporotic Fractures (SOF). A total of 3,631 women with complete data were included in the visual acuity (VA) and visual field (VF) analysis of the NEI VFQ-9, which is defined for those who care to drive. and 5,311 in the analysis of the NEI VFQ-8. To assess differences in prevalent eye diseases, which were ascertained for a random sample of SOF participants, 853 and 1,237 women were included in the NEI VFQ-9 and the NEI VFQ-8 analyses, respectively.
Results
Cronbach alpha coefficient for the NEI VFQ-9 scale was 0.83 and that of the NEI VFQ-8 was 0.84. Using both questionnaires, women with VA worse than 20/40 had lower composite scores compared to those with VA 20/40 or better (p<0.001). Participants with mild, moderate, and severe binocular VF loss had lower composite scores compared to those with no binocular VF loss (p<0.001).Compared to women without chronic eye diseases in both eyes, women with at least one chronic eye disease in at least one eye had lower composite scores.
Conclusions
Both questionnaires showed high reliability across items and validity with respect to clinical markers of eye disease Future research should compare the properties of these shortened surveys to those of the NEI VFQ-25.
Introduction
The National Eye Institute Visual Function Questionnaire (NEI-VFQ) was devised to provide a self-reported measure of vision-targeted functioning. A 51-item questionnaire (NEI-VFQ) was originally developed,1 and the questionnaire was later shortened to 25 items (NEI VFQ-25).2 The instruments assess vision-related quality of life within different domains such as general, near, distance, and color vision, role limitations, dependency, mental health, and social function. They have been validated by a variety of studies showing they are useful tools in assessing vision-specific quality of life. 3–9
One advantage of these questionnaires is their comprehensiveness as they capture several dimensions of vision-targeted quality of life. Sub-scales, usually consisting of several items, can be used to provide an independent measure of visual ability within each domain.10 The length of the surveys, however, can be a challenge especially in large multi-purpose population-based studies involving a variety of other questionnaires. The developers of the NEI-VFQ and NEI VFQ-25, therefore, devised a 9-item instrument (NEI VFQ-9) that has been used in the National Health and Nutrition Examination Survey (NHANES) since 1999. No published studies have previously assessed the reliability and validity of the NEI VFQ-9.
The NEI VFQ-9 was administered to 5,482 women who participated in the Year-10 clinic visit in the Study of Osteoporotic Fractures in 1997–8. The purpose of this research is to evaluate the reliability and validity of the NEI VFQ-9, as well as the NEI VFQ-8, in which the driving question is excluded due to a large proportion of non-drivers and statistically significant differences between drivers and non-drivers.
Methods
Subjects
From 1986 to 1988, 9,704 ambulatory white female volunteers who were 65 years or older, with no history of osteoporosis or bilateral hip replacement, were enrolled in SOF, a multi-center, prospective longitudinal cohort study.11 These women were located in Baltimore, Maryland; Minneapolis, Minnesota; Portland, Oregon; and the Monongahela Valley, Pennsylvania. A cohort of 662 black women was recruited from population listings at each of the four clinic centers using the original recruitment criteria, between 1996 and 1998. From January, 1997 through September, 1998, all surviving participants were invited to participate in a follow-up clinical examination (Year-10 clinic visit), which included a comprehensive eye evaluation. All individuals in the study gave informed consent to participate after obtaining Institutional Review Board approvals from all study institutions. A total of 5,482 women, consisting of 4,820 white participants (63% of the surviving cohort) and 662 African America women, attended the Year-10 clinic visit. These 5,482 women completed the NEI VFQ-9 questionnaire.
Vision-Specific Quality of Life
The 9-item questionnaire was devised from the NEI-VFQ by the developers of the NEI-VFQ, using similar quantitative and qualitative analysis when developing the NEI VFQ-25.2 With respect to the domains represented on the 51-item version of the questionnaire, the 9-item version includes one question about the person’s general vision, three questions about near vision (reading normal newsprint; seeing well up close; finding objects on crowded shelf), one question about each of distance vision (going down stairs at night), driving (driving during the daytime in familiar places), peripheral vision (seeing objects off to side), role limitation (limited in endurance), and well-being/mental health (amount of time worrying about eyesight), and no questions about ocular pain, vision-specific social functioning, expectations for visual function, vision-specific role-functioning, dependency due to vision, or color vision. Table 1 lists questionnaire items and the set of response options; other than a question asking whether the person is currently driving, each question includes either 5 or 6 response options. The NEI VFQ-9 takes approximately 3 to 4 minutes to complete. The questionnaire was administered using written forms that participants returned in the mail or during clinic visits. Subjects with low vision were able to seek assistance in completing the forms during their clinic visit.
Table 1.
Nine-item National Eye Institute Visual Function Questionnaire (NEI-VFQ-9)
| NEI-VFQ-9 Questionnaire |
|---|
| Q1. General vision (6-level) |
|
At the present time, would you say your eyesight (with glasses or contact lenses, if you wear them) is: 1) excellent, 2) good, 3) fair, 4) poor, 5) very poor, or 6) are you completely blind? |
| Q2. Well being/mental health (5-level) |
|
How much of the time do you worry about your eyesight? 1) None of the time, 2) a little of time, 3) some of the time, 4) most of the time, or 5) all of the time. |
| Q3. Near vision, reading normal newsprint (6-level) |
|
How much difficulty do you have reading ordinary print in newspapers? 1) No difficulty at all, 2) a little difficulty, 3) moderate difficulty, 4) extreme difficulty, 5) stopped doing because of your eyesight, or 6) stopped doing this for other reasons or not interested in doing this. |
| Q4. Near vision, seeing well up close (6-level) |
|
How much difficulty do you have doing work or hobbies that require you to see well up close, such as cooking, sewing, fixing things around the house, or using hand tools? 1) No difficulty at all, 2) a little difficulty, 3) moderate difficulty, 4) extreme difficulty, 5) stopped doing because of your eyesight, or 6) stopped doing this for other reasons or not interested in doing this. |
| Q5. Distance vision, going down stairs at night (6-level) |
|
Because of your eyesight, how much difficulty do you have going down steps, stairs, or curbs in dim light or at night? 1) No difficulty at all, 2) a little difficulty, 3) moderate difficulty, 4) extreme difficulty, 5) stopped doing because of your eyesight, or 6) stopped doing this for other reasons or not interested in doing this. |
| Q6. Driving (6-level)* |
|
How much difficulty do you have driving during the daytime in familiar places? 1) No difficulty at all, 2) a little difficulty, 3) moderate difficulty, 4) extreme difficulty, stopped doing because of your eyesight, or 5) stopped doing this for other reasons or not interested in doing this. |
| Q7. Role limitation (5-level) |
|
Are you limited in how long you can walk or do other activities such as housework, child care, school, or community activities because of your vision? 1) All of the time, 2) most of the time, 3) some of the time, 4) a little of time, or 5) none of the time. |
| Q8. Peripheral vision (6-level) |
|
Because of your eyesight, how much difficulty do you have noticing objects off to the side while you are walking along? 1) No difficulty at all, 2) a little difficulty, 3) moderate difficulty, 4) extreme difficulty, 5) stopped doing because of your eyesight, or 6) stopped doing this for other reasons or not interested in doing this. |
| Q9. Near vision, finding objects on a crowded shelf (6-level) |
|
Because of your eyesight, how much difficulty do you have finding something on a crowded shelf? 1) No difficulty at all, 2) a little difficulty, 3) moderate difficulty, 4) extreme difficulty, 5) stopped doing because of your eyesight, or 6) stopped doing this for other reasons or not interested in doing this. |
For Q6, “not currently driving” was also an option, however, if selected, then the question was omitted and the remaining questions comprised the NEI-VFQ-8.
Assessment of Vision
Visual acuity and visual fields were assessed among all women who participated in the Year-10 clinic visit. The presence of eye diseases, specifically age-related macular degeneration (AMD), glaucoma, and visually significant cataract, was assessed among women who were randomly selected to have their eye photographs graded.
Visual acuity and visual field
Distance visual acuity (VA) was measured in each eye separately with habitual correction using Bailey-Lovie charts,12 and visual fields (VF) 13 were assessed in each eye separately using the Humphrey Field Analyzer suprathreshold 76-point 30 ° VF program (Humphrey Field Analyzer; Zeiss, Oberkochen, Germany),14 as described in a previous SOF publication.15
Eye Diseases
The presence of AMD was determined using forty-five degree stereoscopic fundus photographs. Early AMD was characterized by the presence of soft drusen (drusen area ≥95 microns but <960 microns in diameter) with retinal pigment epithelium (RPE) depigmentation or soft drusen (drusen area ≥960 microns in diameter) with or without pigmentary abnormalities. The presence of geographic atrophy or sub-foveal choroidal neovascularization indicated the existence of late AMD.16
Glaucoma was diagnosed based on the appearance of the optic nerve head in the optic disc photographs and 76-point VF screening results (at least one point missed). Glaucomatous optic nerves were those having diffuse and localized thinning of the neuroretinal rim, loss of retinal fiber layer, increased cupping, and/or asymmetry of the optic nerve cup-to-disc ratios of 0.2 or greater.17
Aphakia or pseudophakia was determined for each eye using external and/or lens photographs. Visually significant cataract was defined as the presence of nuclear, posterior subcapsular, or cortical cataract and visual acuity worse than 20/40.16
The presence of a chronic eye disease was defined as (1) the presence of late AMD, or the presence of early AMD with visual acuity worse than 20/40; (2) the presence of glaucoma, (3) the presence of visually significant cataract, or aphakia or pseudophakia due to cataract surgery.
Women included in the NEI VFQ-9 and NEI VFQ-8 analyses
The distinction between the NEI VFQ-9 and NEI VFQ-8 is in their treatment of driving, which raises conceptual issues relevant to quality of life, since not everyone wants to or cares to drive. Rather than artificially assigning average quality of life, the possible quality of life, or some other quality of life to those who do not care to drive, the approach taken here is to have two alternate scales; the NEI VFQ-9 for those who care to drive, and the NEI VFQ-8, which is applicable to all. For those who do not care to drive, we consider their NEI VFQ-9 score to be undefined. Accordingly, in the NEI VFQ-9 instrument, subjects are first asked whether they are currently driving. For those whose response is “not currently driving,” two additional options are provided on the reasons of not driving: “stopped because of eyesight” or “stopped for other reasons.” A person responding with the former option was coded as a non-driver and was included in the calculation of the NEI VFQ-9 composite score with the lowest possible item score (0), while a person responding with the latter option was also coded as a non-driver, but was considered to have an undefined NEI VFQ-9 composite score. Subjects who responded that they were “completely blind” were coded as non-drivers, and were included in the calculation of the NEI VFQ-9 composite score with the lowest possible item score (0).
Among the 5,482 women attending the SOF Year-10 clinic visit in this study, 9 did not respond to the driving question. Therefore, 1,793 subjects, including the 9 who did not respond to the driving question, 1,563 who did not provide the reason for not driving, and 221 women who stopped for other reasons, were excluded from the calculation of the NEI VFQ-9 composite score. They were included in the calculation of the NEI VFQ-8 composite score when they responded to the other 8 NEI VFQ questions.
Among the 5,482 women attending the SOF year-10 clinic visit, 8 did not return the questionnaire, and were excluded from the statistical analyses, resulting in a sample of 5,474 women. One additional individual did not respond to the driving question, and 1,886 (34%) were coded as non-drivers. Of the 1,886 women, 1,563 were “not currently driving” without stating the reason for not driving, 221 “stopped for other reasons,” 96 “stopped because of eyesight,” and 6 were “completely blind.” Approximately 97% (5,311/5,474) provided valid responses to the eight questions applicable to the NEI VFQ-8, of those who did not, 105 were drivers and 58 were non-drivers. To assess the differences in composite scores based on VA and VF, a total of 3,631 women were included in the analyses of the NEI VFQ-9 and 5,311 were part of the analyses of the NEI VFQ-8.
Eye diseases were diagnosed in a random sample of 1,274 women out of all participants in the Year-10 visit. Forty-two (3.5%) women had late AMD in at least one eye, 513 (43.1%) had early AMD in at least one eye, and 634 (53.3%) women did not have AMD in either eye. A total of 105 (8.5%) had glaucoma in at least one eye. A total of 376 (31.7%) women had aphakia or pseudophakia in both eyes, 332 (28.0%) had visually significant cataract in at least one eye, and 479 (40.4%) women did not have visually significant cataract in both eyes. To assess the differences in composite scores based on prevalent eye diseases, 853 women (out of 1,274 or 67%) had complete data for the 9-item analysis and 1,237 (out of 1,274 or 97%) had complete data for the 8-item analysis.
Statistical Analysis
Distributions of demographic and health characteristics are presented for all women who participated in the Year-10 clinic visit. Self-rated health status was measured by asking participants to rate their health relative to that of others as excellent, good, fair, poor, or very poor. These responses were grouped into: (1) fair, poor or very poor, or (2) excellent or good. Participants were asked about having been told by a doctor that they have one or more of 17 comorbidities such as heart attack, coronary, or myocardial infarction, stroke, diabetes, high blood pressure, Parkinson’s disease, and Dementia or Alzheimer’s disease.
The percentages of women with missing NEI VFQ-9 item-level responses at the missing, or with responses at the ceiling (best possible) or floor (worst possible) levels were calculated for the sample of women who had valid responses to all nine questions. Individuals characterizing their vision as excellent (Q1, General Vision), have a response at the ceiling level. The calculation of composite scores requires no missing values in any items.
To assess reliability, the internal consistencies of the VFQ-9 and the VFQ-8 were evaluated using Cronbach alpha coefficients.18 The Cronbach alpha coefficient varies from 0 to 1; higher alphas indicate greater internal consistency.
Spearman correlations between VA/binocular VF and both multi-item instruments were used to assess whether people with poorer vision had lower vision-specific quality of life. Number of points missed in binocular VF loss and log MAR score of VA in the better and worse eye were analyzed as continuous variables. To support validity, Spearman correlation coefficients should be negative indicating that a higher log MAR score (signifying worse VA) and more points missed in binocular VF are related to lower vision-specific quality of life.
The comparison of mean NEI VFQ-9 and NEI VFQ-8 scores by VA groups (20/40 or better and worse than 20/40) and by VF groups (no BVF loss, mild BVF loss [1–9 points missed], moderate BVF loss [10–19 points missed], and severe BVF loss [20 or more points missed]), were used to assess whether statistically significant differences existed in the composite scores between people with worse vision and those with good vision.
The validity of both multi-item questionnaires using comparisons between questionnaire composite scores was also assessed based on prevalent eye diseases. To support validity, women in the reference groups comprising of women with no chronic eye disease should have higher composite scores compared to those with an eye disease.
The statistical comparisons of composite scores included the following: (1) scores of women with VA 20/40 or better versus women with VA worse than 20/40 in the better eye and worse eye; (2) scores of women with no binocular VF loss versus those with mild, moderate, and severe binocular VF loss; (3) scores of women without any chronic eye diseases in both eyes versus those with at least one eye disease in at least one eye; (4) scores of women without any chronic eye diseases in both eyes versus those with early or late AMD in at least one eye; (5) scores of women without any chronic eye diseases in both eyes versus those with glaucoma in at least one eye; and (6) scores of women without any chronic eye diseases in both eyes compared to phakic women with visually significant cataract in at least one eye and those with aphakia/pseudophakia in both eyes. The composite scores range from 0 to 100, with a score of 100 showing the highest quality of life.
All statistical analyses were performed using SAS version 9.1 software (SAS Institute Inc., Cary, NC). Statistical significance was defined as p<0.05.
Results
General Characteristics of Participants
Table 2 presents the characteristics of the 5,482 women who participated in the SOF Year-10 clinic visit. The sample consisted of primarily older women; their mean age was 79.5±4.5 years with a range of 65 to 100 years. The majority of women (4,359/5,482, or 79%) were between the ages of 75 and 84 years. Approximately 7% (382/5,482) were in the age group 65 to 74 years, and 14% (741/5,482) were 85 years of age or older. African American women represented 12% of the sample (662/5,482); the remaining were white women. Approximately 80% (4,376/5,482) completed high school or had higher education. The same percentage of women reported excellent/good health status. The distribution of co-morbidities was skewed; the median number of co-morbidities was 1 with a range of 0 to 10 (out of 17 possible). Approximately 17% (920/5,482) had visual acuity worse than 20/40. In sum, the sample consisted of women who were primarily older, white, high school graduates or above, and in excellent/good self-rated health status.
Table 2.
Characteristics of Women Who Participated in the Study of Osteoporotic Fractures (SOF) Year-10 Clinic Visits. (N=5,482)
| Characteristics | Summary statistics |
|---|---|
| Study sites | |
| Baltimore | 1,279 (23%) |
| Minneapolis | 1,635 (30%) |
| Pittsburgh | 1,409 (26%) |
| Portland | 1,159 (21%) |
| Age (year) | |
| Mean ± SD (Range) | 79.5 ± 4.5 (65 to 100) |
| 65 – 74 | 382 (7%) |
| 75 – 79 | 2,704 (49%) |
| 80 – 84 | 1,655 (30%) |
| ≥85 | 741 (14%) |
| Race/Ethnicity | |
| Caucasian | 4,820 (88%) |
| African American | 662 (12%) |
| Education (year) | |
| <12 | 1,096 (20%) |
| ≥12 (HS graduate or above) | 4,380 (80%) |
| Self-rated health status | |
| Fair/Poor/Very Poor | 1,097 (20%) |
| Excellent/Good | 4,376 (80%) |
| Number of comorbidity (0 to 17) | |
| Median (Range) | 1 (0 to 10) |
| Habitual distance visual acuity in the better eye (log MAR) |
|
| Mean ± SD (Range) | 0.19 ± 0.18 (−0.18 to 1.36) |
| Worse than 20/40 | 920 (17%) |
SD = Standard deviation, HS=High school.
Item Responses
Table 3 shows that many women performed at the optimal level for near, distance, and peripheral vision. The percentage of women reporting responses at the ceiling level exceeded 60% for all but one question, reaching 92% for the role limitation question. A relatively low percentage (15%) of women, however, reported their eyesight was excellent (Table 3).
Table 3.
The Number and Percentage of Item Responses at Ceiling, Floor, or Missing for the 9-item National Eye Institute Visual Function Questionnaire (NEI VFQ-9) in Women Who Participated in the Study of Osteoporotic Fractures (SOF) Year-10 Clinic Visits (N=5474)*.
| NEI VFQ-9 items | Missing N (%) |
Floor N (%) |
Ceiling N (%) |
|---|---|---|---|
| General vision | |||
| 6-level general vision | 0 | 7 (0.1%) | 817 (15%) |
| Near vision | |||
| 6-level reading normal newsprint | 18 (0.3%) | 121 (2%) | 3,998 (73%) |
| 6-level seeing well up close | 59 (1%) | 114 (2%) | 4,018 (73%) |
| 6-level finding objects on crowded shelf |
13 (0.2%) | 19 (0.3%) | 4,615 (84%) |
| Distance vision | |||
| 6-level going down stairs at night | 94 (2%) | 39 (0.7%) | 3,922 (72%) |
| Driving | |||
| 6-level daylight familiar places | 1,785 (33%) |
102 (2%) | 3,484 (64%) |
| Peripheral vision | |||
| 6-level seeing objects off to side | 9 (0.2%) | 15 (0.3%) | 4,776 (87%) |
| Role limitation | |||
| 5-level limited in endurance | 4 (0.1%) | 74 (1%) | 5,030 (92%) |
| Well-being/Mental health | |||
| 5-level amount time: Worry | 1 (0.02%) | 234 (4%) | 3,644 (67%) |
Excluding eight women who did not have valid responses to all nine questions.
Reliability
The Cronbach alpha coefficient for the 9-item scale was 0.83 and for the 8-item was 0.84 (Table 4). When removing questions from the scale, the alphas remained relatively high decreasing slightly for all items except for the well-being/mental health question, which if removed would result in Cronbach coefficient alphas of 0.85 for the NEI VFQ-9 and 0.86 for the NEI VFQ-8.
Table 4.
Internal Consistency of the 9-item National Eye Institute Visual Function Questionnaire (NEI VFQ-9) in Women Who Participated in the Study of Osteoporotic Fractures (SOF) Year-10 Clinic Visits.
| NEI VFQ-9 item | NEI VFQ: Cronbach Alpha Coefficient |
|
|---|---|---|
| Composite Score (9-item)* N=3,631 |
Composite Score (8-item)† N=5,311 |
|
| Overall | 0.83 | 0.84 |
| Cronbach coefficient alpha for deleted NEI VFQ-9 item |
||
| General vision | ||
| 6-level general vision | 0.81 | 0.82 |
| Near vision | ||
| 6-level reading normal newsprint | 0.80 | 0.80 |
| 6-level seeing well up close | 0.80 | 0.80 |
| 6-level finding objects on crowded shelf |
0.81 | 0.81 |
| Distance vision | ||
| 6-level going down stairs at night | 0.82 | 0.81 |
| Driving | ||
| 6-level daylight familiar places | 0.82 | NA |
| Peripheral vision | ||
| 6-level seeing objects off to side | 0.82 | 0.82 |
| Role limitation | ||
| 5-level limited in endurance | 0.82 | 0.83 |
| Well-being/Mental health | ||
| 5-level amount time: Worry | 0.85 | 0.86 |
NEI VFQ-9 9 item composite score was calculated among women who had valid responses to all 9 items.
NEI VFQ-9 8 item composite score was calculated among women who had valid responses to all 8 items, except for the driving item.
Validity
Table 5 presents the validity of both multi-question instruments using VA and binocular VF assessments. Table 6 contains information regarding differences in prevalent eye diseases, specifically any chronic eye disease, AMD, glaucoma, and visually-significant cataract.
Table 5.
Nine-item National Eye Institute Visual Function Questionnaire (NEI VFQ-9) Composite Scores by Clinical Measure of Visual Function in Women Who Participated in the Study of Osteoporotic Fractures (SOF) Year-10 Clinic Visits.
| Clinical Measure of Visual Function | NEI VFQ | |
|---|---|---|
| Composite Score (9-item)* N=3,631 |
Composite Score (8-item)† N=5,311 |
|
| Overall: Mean ± SD (Median) | 91.3 ± 11.5 (95) | 88.8 ± 13.7 (94) |
| Visual acuity (log MAR) | ||
| Better eye | ||
| Spearman correlation coefficient | −0.21 P<0.001 |
−0.24 P<0.001 |
| Mean ± SD (Median) | ||
| 20/40 or better | 92.6 ± 8.5 (95) | 90.8 ± 10.4 (94) |
| Worse than 20/40 | 85.1 ± 17.3 (92) | 80.6 ± 19.7 (89) |
| P-value‡ | P<0.001 | P<0.001 |
| Worse eye | ||
| Spearman correlation coefficient | −0.23 P<0.001 |
−0.26 P<0.001 |
| Mean ± SD (Median) | ||
| 20/40 or better | 93.3 ± 8.1 (96) | 91.7 ± 9.8 (95) |
| Worse than 20/40 | 89.1 ± 12.8 (94) | 85.9 ± 15.5 (91) |
| P-value‡ | P<0.001 | P<0.001 |
| Binocular visual field loss (number of points missed)§ |
||
| Spearman correlation coefficient | −0.14 P<0.001 |
−0.16 P<0.001 |
| Mean ± SD (Median) | ||
| None (No point missed) | 93.6 ± 7.0 (96) | 92.4 ± 8.3 (95) |
| Mild (1–9 points missed) | 92.1 ± 9.2 (95) | 90.9 ± 10.2 (94) |
| Moderate (10–19 points missed) | 90.1 ± 11.1 (95) | 88.2 ± 12.1 (93) |
| Severe (20 or more points missed) |
87.0 ± 14.8 (92) | 83.0 ± 17.6 (89) |
| P-value‡ | P<0.001 | P<0.001 |
SD = Standard deviation.
NEI VFQ-9 9 item composite score was calculated among women who had valid responses to all 9 items.
NEI VFQ-9 8 item composite score was calculated among women who had valid responses to all 8 items, except for the driving item.
Kruskal-Wallis test.
Binocular visual field loss were calculated among women who had reliable (fixation loss ≤ 33%) visual field test in both eyes. Spearman correlation coefficient = −0.18 (p<0.001) between binocular visual field loss and NEI VFQ peripheral subscale.
Table 6.
Nine-item National Eye Institute Visual Function Questionnaire (NEI VFQ-9) Composite Scores by Eye Disease in Women Who Participated in the Study of Osteoporotic Fractures (SOF) Year-10 Clinic Visits.
| Eye Disease | NEI VFQ: Mean ± SD (Median) | |
|---|---|---|
| Composite Score (9-item)* N=853 |
Composite Score (8-item)† N=1,237 |
|
| Overall | 92.1 ± 9.9 (95) | 89.5 ± 12.8 (94) |
| Any chronic eye disease‡ | ||
| No eye diseases in both eyes (n=360)‡ |
94.1 ± 6.2 (96) (n=259) |
93.0 ± 7.4 (95) (n=351) |
| Yes in at least one eye (n=838) | 91.1 ± 11.2 (95) (n=549) |
88.0 ± 14.3 (94) (n=811) |
| P-value§ | P=0.005 | P<0.001 |
| Bilateral chronic eye disease (n=556) | 91.2 ± 11.8 (96) (n=353) |
87.9 ± 15.2 (94) (n=534) |
| Age-related macular degeneration (AMD) | ||
| No eye diseases in both eyes (n=219)‡ |
93.7 ± 6.7 (96) (n=162) |
92.8 ± 7.6 (95) (n=213) |
| Early AMD in at least one eye (n=513) | 92.5 ± 8.9 (96) (n=343) |
89.7 ± 12.6 (94) (n=495) |
| Late AMD in at least one eye (n=42) | 79.3 ± 23.6 (88) (n=24) |
72.8 ± 26.3 (86) (n=39) |
| Difference (no vs. late AMD) | 14.4 | 20 |
| P-value§ | P=0.003 | P<0.001 |
| Bilateral early AMD (n=286) | 92.3 ± 8.7 (95) (n=181) |
89.1 ± 13.3 (94) (n=273) |
| Bilateral late AMD (n=20) | 73.4 ± 29.8 (86) (n=9) |
62.3 ± 28.7 (59) (n=17) |
| Glaucoma | ||
| No eye diseases in both eyes (n=360)‡ |
94.1 ± 6.2 (96) (n=259) |
93.0 ± 7.4 (95) (n=351) |
| Glaucoma in at least one eye (n=105) | 92.7 ± 8.2 (96) (n=54) |
85.7 ± 16.5 (93) (n=102) |
| P-value§ | P=0.609 | P<0.001 |
| Bilateral glaucoma (n=57) | 91.4 ± 9.2 (95) (n=30) |
86.7 ± 14.1 (91) (n=54) |
| Visually significant cataract | ||
| No eye diseases in both eyes (n=360)‡ |
94.1 ± 6.2 (96) (n=259) |
93.0 ± 7.4 (95) (n=351) |
| Phakia with visually significant cataract in at least one eye (n=332) |
90.9 ± 10.7 (95) (n=220) |
88.0 ± 12.8 (93) (n=323) |
| Aphakia/pseudophakia in both eyes (n=376) |
91.0 ± 12.3 (96) (n=239) |
88.0 ± 15.6 (94) (n=359) |
| P-value§ | P=0.007 | P<0.001 |
| Bilateral phakia with visually significant cataract (n=87) |
93.3 ± 7.3 (96) (n=53) |
88.4 ± 12.8 (94) (n=86) |
| Bilateral aphakia/pseudophakia or phakia with visually significant cataract (n=517) |
91.2 ± 11.8 (96) (n=330) |
88.1 ± 14.9 (94) (n=495) |
SD = Standard deviation.
NEI VFQ-9 9 item composite score was calculated among women who had valid responses to all 9 items.
NEI VFQ-9 8 item composite score was calculated among women who had valid responses to all 8 items, except for the driving item.
Any chronic eye disease includes age-related macular degeneration, glaucoma, and visually significant cataract.
Kruskal-Wallis test.
Visual Acuity and Visual Field
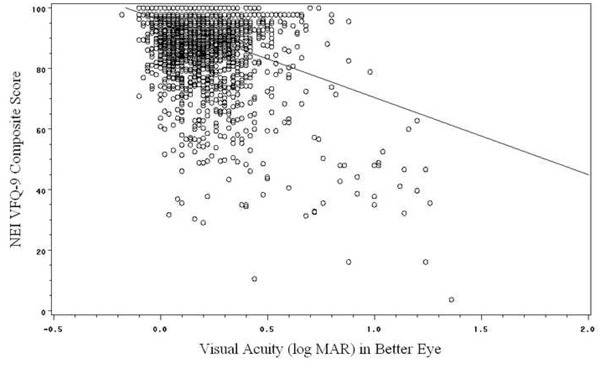
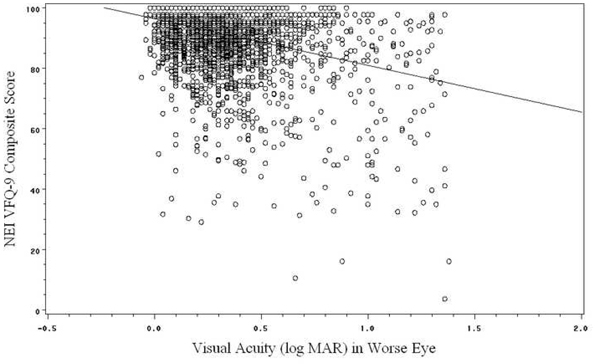
The majority of 3,631 subjects included in the 9-item scale analyses had high NEI VFQ scores and good visual acuity (Figure 1). The mean composite score among the 3,631 women was 91.3±11.5 with a median of 95 (Table 5). That of the 8-item questionnaire involving 5,311 women, was lower (88.8±13.7, with a median of 94). Women with a higher composite score of quality of life had superior visual acuity. The Spearman correlation coefficients were relatively lower for binocular VF loss than for VA: −0.14 (p<0.001) for the 9-item and −0.16 for the 8-item questionnaire (Table 5). Binocular visual field loss also showed similar correlation with the NEI VFQ peripheral subscale (Spearman correlation coefficient = −0.18, p<0.001).
Figure 1.
Scatter plots of NEI-VFQ-9 composite score with visual acuity in logMAR unit in better eye (Figure 1a) and worse eye (Figure 1b).
When binocular VF loss and VA in the worse and better eye were assessed using cut-off points, women with worse vision had lower composite scores. The differences in the groups were statistically significant for both VA and binocular VF loss for the multi-item instruments (p<0.001). For example, there was almost a 10 point difference in the composite scores between women with no binocular VF loss (92.4±8.3) compared to those with severe binocular VF loss (83.0±8.3) using the NEI VFQ-8.
Eye Diseases
The mean composite score among the 853 women included in the analysis of eye diseases was 92.1±9.9 with a median of 95 among women included in the NEI VFQ-9 analysis. That of the 8-item questionnaire involving 1,237 women was 89.5±12.8 with a median of 94. Women with at least one chronic eye diseases in at least one eye had lower composite scores compared to those with no chronic eye diseases in both eyes (p=0.005 for NEI VFQ-9 and p<0.001 for NEI VFQ-8). Individuals with AMD and cataract in both surveys and those with glaucoma in the NEI VFQ-8 analysis had lower composite scores compared to those without any chronic eye diseases (Table 6). The composite scores were very similar between phakic women with visually significant cataract in both eyes and those with aphakia/pseudophakia in both eyes using both instruments (p=0.585 for NEI VFQ-9 and p=0.532 for NEI VFQ-8).
Drivers versus Non-Drivers
Drivers had a higher than average NEI VFQ-8 composite score of 91.6±9.2 (median: 94) compared to 83.3±18.6 (median: 91) in non-drivers (p<0.001) (Table 7). Among non-drivers, glaucoma patients had significantly lower scores on the NEI VFQ-8 distance vision (p=0.003) and peripheral vision (p=0.024) questions than non-glaucoma subjects. Glaucoma patients who did not drive also had lower scores on the other six NEI VFQ non-driving questions than non-glaucoma subjects who did not drive although the differences were not statistically significant.
Table 7.
Characteristics of drivers and non-drivers
| Characteristics | Drivers (N=3587) |
Non-drivers (N=1886) |
P-value |
|---|---|---|---|
| Age (years): Mean±SD | 78.8±3.9 | 80.8±5.3 | <0.0001 |
| Self-rated health status: n (%) |
<0.0001 | ||
| Fair/Poor/Very Poor | 563 (16%) | 531 (28%) | |
| Excellent/Good | 3022 (84%) | 1348 (72%) | |
| VFQ-8 composite score: Mean±SD |
91.6±9.2 | 83.3±18.6 | <0.0001 |
Discussion
Overall, the two shortened versions of the NEI VFQ yielded similar results. Both the NEI VFQ-9 and NEI VFQ-8 showed high reliability across items and validity with respect to clinical markers of eye disease in a cohort of older women with an average age of 80 years. Women with severe binocular VF loss and VA worse than 20/40 in the better and worse eyes had lower composite scores compared to those with no VF loss and those with VA 20/40 or better. Between-group differences in composite scores in people with a particular eye disease versus those without any chronic eye diseases indicated that people with eye diseases had lower composite scores, except in the case of drivers with glaucoma.
Our primary goal was to assess the NEI VFQ-9, which is being used in the NHANES survey. Researchers face a similar challenge when there is a high percentage of non-drivers in the study population in using both the NEI VFQ-25 and NEI VFQ-9. We recommend reporting findings related to both the NEI VFQ-9 and NEI VFQ-8 when a high proportion of non-drivers exists, as in this study. Reporting findings for both questionnaires may provide more information since drivers and non-drivers have different characteristics. The population of individuals included in the 8-item questionnaire tended to consist of people with poorer health, which may be because non-drivers lack independence and have reduced physical and visual functioning. Drivers were younger and had better self-rated health status. In addition, the decision regarding which of the two shortened questionnaires to use may depend on the proportion of non-drivers in the study population. The percentage of older persons licensed to drive is increasing at the present time compared to past years,19–20 largely due to more older women driving.21 At the same time, the number of persons not driving increases with advancing age. In the SOF population, approximately a third of individuals were non-drivers compared to 16% in a sample consisting of relatively younger people in the study of Mangione and colleagues introducing the NEI VFQ-25.2
It is arguable whether the changes in composite scores between people with vision problems compared to those with no vision problems are clinically relevant. Marsala and associates found that a 4-point difference in the overall NEI VFQ-25, and a 5-point sub-scale change constitute a minimum clinically relevant change.22 Based on a 5-point change criterion, minimum clinically relevant changes were detected between: 1) women with VA 20/40 or better in the better eye and those with VA worse than 20/40, 2) women with no binocular VF loss and those with severe loss, and 3) participants with no AMD in both eyes and those with late AMD in at least one eye, using both questionnaires. Minimal clinical significant changes were observed more frequently when using the NEI VFQ-8 compared to the NEI VFQ-9, which may be because the women who completed all 9 questions represented a healthier population.
There were greater decreases in quality of life composite scores in women with glaucoma when using the NEI VFQ-8 compared to the NEI VFQ-9, and the declines using the NEI VFQ-9 had borderline significance. When removing the driving question, results were consistent with past research showing that patients with glaucoma have a decreased quality of life. The NEI-VFQ is considered the standard for assessing the quality of life in glaucoma patients.23 In a recent publication of the Los Angeles Latino Eye Study (LALES), glaucoma patients with VF loss had lower NEI VFQ-25 scores compared to glaucoma patients without VF loss.24 Using the NEI VFQ-25 and involving 5,213 subjects, LALES reported that VF loss was associated with driving difficulties,25 and the Advanced Glaucoma Intervention study found that patients with glaucoma reported greater driving difficulties than those without glaucoma.26 One explanation for the moderate decreases in quality of life in glaucoma patients who drove in this study might be that many individuals with glaucoma chose not to drive due to their glaucoma. Another interpretation is that people whose vision was intact to the extent where they could drive, were not affected by glaucoma in terms of quality of life at the time they completed the questionnaire. People with glaucoma may still perform well on vision-related tasks during the early stages of the disease. A study using the NEI-VFQ reported a modest correlation between visual field loss and driving ability among glaucoma patients.27 An investigation of 35 glaucoma patients found that lower contrast sensitivity, and not mild or moderate VF loss was associated with decreased driving performance, which was evaluated using driving simulation and self-report of past driving accidents. 28 In another study also using driving simulation and self-report of past driving accidents, reductions in the visual field to less than 100 degrees of horizontal extent were related to worse driving performance,29 indicating that more severe declines in VF may affect driving performance.
A surprising finding is that phakic women with visually significant cataract in both eyes and those with aphakia/pseudophakia in both eyes had very similar vision-specific quality of life composite scores. In sub-analysis, there were no statistically significant differences in NEI VFQ-9 (p=0.585) and NEI VFQ-8 (p=0.532) scores between patients with visually significant cataracts in both eyes and those with aphakia/pseudophakia in both eyes. Using the Activities of Daily Vision Scale (ADVS), Mangione and colleagues reported improved scores 12 months after cataract extraction.30 The results in this study might be due to people with cataract surgery being older, to better vision in one eye, or to other factors affecting their vision. The finding that those with cataract have a lower vision-specific quality of life compared to those with no cataract was consistent with past research.9
In terms of AMD, the differences in composite scores were slight between women with no AMD and early AMD but those between women with no and late AMD were as many as 20 points. The finding is not surprising given the great severity of late AMD; the progressive loss of central vision adversely affects quality of life.31 In a literature review of studies using the NEI VFQ-25, Finger and colleagues found that AMD adversely affected vision-specific quality of life.32
Strengths of this study include its large sample size, high overall response rate, and assessment of VA and VF using standardized methods among all participants. Another strength is the incorporation of binocular VF assessment.17 While visual acuity has been found to be the most important determinant of the VFQ score,10 it only provides a limited measure of vision performance. A linear association between inferior NEI VFQ-25 scores and VF declines existed in LALES.25
The study population was comprised of older women initially living in communities; therefore, the results might not apply to other populations such as men, younger women, or those with poorer health or living in institutions. The sample represents a relatively healthy, motivated, and educated population. Because this is a cross-sectional study, the authors could not evaluate changes in vision and quality of life over time. The administration of the NEI-VFQ abbreviated questionnaires may be feasible in large multipurpose population-based studies, although our findings do not address whether the NEI VFQ-25 can be replaced by the short questionnaires. The reliability and validity of NEI VFQ-9 and NEI VFQ-8 could not be compared to those of the NEI VFQ-25 in this study because SOF participants did not complete the longer questionnaire. Our study did not evaluate the usefulness of the brief questionnaires in clinical trials. Some driving seniors are reluctant to report they are driving due to fear that the response will be transmitted to the licensing authorities, resulting in the loss of permission to drive; therefore, there may be a misclassification of driving status in this study. In addition, some of the missing data on the reason for not driving may be due to response options being embedded in the question on the difficulty of driving. A smaller subset of women was used in the analyses of eye diseases; however, the subset was a random sample of all participants in the study. Differences in prevalent eye diseases by the severity of the disease were not assessed. While the assessment of binocular VF loss using the Esterman’s scoring algorithm15 calculations might be a limitation, results from calculated binocular VF are comparable to the results of the Esterman binocular VF test.33–36 Other analyses of NEI VFQ-8 and VFQ-9 data are possible, including a Rasch-model analysis that could be used to scrutinize the extent to which items conform to a single latent-variable construct.37 We regard such an approach as potentially interesting but beyond the scope of the present research, as in general, attempting to determine the latent variable structure among multivariate measurements is more involved than evaluating reliability and validity of a specific composite measure.
In conclusion, both questionnaires showed high reliability and validity with respect to clinically relevant markers. Longer surveys could result in a poorer response rate, which in term could affect validity.38 In systematic reviews of randomized trials using postal surveys, 39–40 higher response rates were seen when shorter questionnaires were used. Future research should compare the properties of the shortened surveys to those of the NEI VFQ-25.
Acknowledgments
ACKNOWLEDGMENTS/DISCLOSURE:
Funding/Support: Supported by an unrestricted grant from Research to Prevent Blindness to the Jules Stein Eye Institute and the Center for Eye Epidemiology, Jules Stein Eye Institute, University of California Los Angeles, CA. The Study of Osteoporotic Fractures (SOF) is supported by Public Health Service research grants from the National Institutes of Health (AR35582, AR35583, AR35584, R01 AG005407, R01 AG027576-22, 2 R01 AG005394-22A1, 2 R01 AG027574-22A1).
Financial Disclosures: None.
Author Contribution: Design and conduct of the study (ALC, JAC, KEE, KLS, MCH, CMM); collection and management (ALC, JAC, KEE, KLS, MCH, CMM); analysis (FY); interpretation of the data (GK, ALC, FY, JAC, KEE, KLS, MCH, KLP, CMM); preparation (GK, ALC, FY); review and approval of the manuscript (GK, ALC, FY, JAC, KEE, KLS, MCH, KLP, CMM).
Statement about Conformity with Author Information: Institutional Review Board approvals were obtained from the University of California, Los Angeles, the University of California, San Francisco, the University of Maryland, the University of Minnesota, Kaiser Permanente Center for Health Research in Portland, Oregon, and the University of Pittsburgh prior to the study.
E. Other Acknowledgments: None.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mangione CM, Berry S, Spritzer K, Janz NK, Klein R, Owsley C, et al. Identifying the content area for the 51-item National Eye Institute Visual Function Questionnaire: results from focus groups with visually impaired persons. Arch Ophthalmol. 1998;116:227–233. doi: 10.1001/archopht.116.2.227. [DOI] [PubMed] [Google Scholar]
- 2.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119:1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 3.Rossi GCM, Milano G, Tinelli Carmine. The Italian Version of the 25-Item National Eye Institute Visual Function Questionnaire: Translation, Validity, and Reliability. J Glaucoma. 2003;12:213–220. doi: 10.1097/00061198-200306000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Varma R, Wu J, Chong K, Azen SP, Hays RD, Los Angeles Latino Eye Study Group Impact of Severity and Bilaterality of Visual Impairment on Health-Related Quality of Life. Ophthalmology. 2006;113:1846–1853. doi: 10.1016/j.ophtha.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 5.Toprak AB, Eser E, Guler C, Baser FE, Mayali H. Cross-validation of the Turkish Version of the 25-Item National Eye Institute Visual Functioning Questionnaire (NEI-VFQ 25) Ophthalmic Epidemiol. 2005;12:259–269. doi: 10.1080/09286580590967763. [DOI] [PubMed] [Google Scholar]
- 6.Jampel HD, Friedman DS, Quigley H, Miller R. Correlation of the binocular visual field with patient assessment of vision. Invest Ophthalmol Vis Sci. 2002;43:1059–1067. [PubMed] [Google Scholar]
- 7.Klein R, Moss SE, Klein BE, Gutierrez P, Mangione CM. The NEI-VFQ-25 in people with long-term type 1 diabetes mellitus: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Arch Ophthalmol. 2001;119:733–740. doi: 10.1001/archopht.119.5.733. [DOI] [PubMed] [Google Scholar]
- 8.Brody BL, Gamst AC, Williams RA, Smith AR, Lau PW, Dolnak D, et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology. 2001;108:1893–1900. doi: 10.1016/s0161-6420(01)00754-0. [DOI] [PubMed] [Google Scholar]
- 9.Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD. Psychometric Properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ) Arch Ophthalmology. 1998;116:1496–1504. doi: 10.1001/archopht.116.11.1496. [DOI] [PubMed] [Google Scholar]
- 10.Owen CG, Rudnicka AR, Smeeth L, Evans JR, Wormald RP, Fletcher AE. Is the NEI-VFQ-25 a useful tool in identifying visual impairment in an elderly population? BMC Ophthalmology. 2006;6:24. doi: 10.1186/1471-2415-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cummings SR, Black DM, Nevitt MC, Browner WS, Cauley JA, Genant HK, et al. Appendicular bone density and age predict hip fracture in women. JAMA. 1990;263:665–668. [PubMed] [Google Scholar]
- 12.Bailey I, Lovie J. New design principles for visual acuity letter charts. Am J Optom Physiol Opt. 1976;53:740–745. doi: 10.1097/00006324-197611000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Esterman B. Functional scoring of the binocular field. Ophthalmology. 1982;89:1226–1234. doi: 10.1016/s0161-6420(82)34647-3. [DOI] [PubMed] [Google Scholar]
- 14.Topouzis F, Coleman AL, Yu F, Mavroudis L, Anastasopoulos E, Koskosas A, et al. Sensitivity and Specificity of the 76-Suprathreshold Visual Field Test to Detect Eyes with Visual Field Defect by Humphrey Threshold Testing in a Population-based Setting: Thessaloniki Eye Study. Am J Ophthalmol. 2004;137:420–425. doi: 10.1016/j.ajo.2003.09.045. [DOI] [PubMed] [Google Scholar]
- 15.Coleman AL, Cummings SR, Yu F, Kodjebacheva G, Ensrud KE, Gutierrez P, et al. Binocular visual-field loss increases the risk of future falls in older white women. J Am Geriatr Soc. 2007;55:357–364. doi: 10.1111/j.1532-5415.2007.01094.x. [DOI] [PubMed] [Google Scholar]
- 16.Coleman AL. Sources of binocular suprathreshold visual field loss in a cohort of older women being followed for risk of falls. Trans Am Ophthalmol Soc. 2007;105:312–329. [PMC free article] [PubMed] [Google Scholar]
- 17.Coleman AL, Stone KL, Kodjebacheva G, Yu F, Pedula KL, Ensrud KE, et al. Glaucoma risk and the consumption of fruits and vegetables among older women in the Study of Osteoporotic Fractures. Am J Ophthalmol. 2008;145:1081–1089. doi: 10.1016/j.ajo.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 18.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 19.U.S. Department of Transportation. Highway Statistics Summary to 1995 (No. 050-001-00323-6) Washington, DC: Office of Highway Information Management, Federal Highway Administration, U.S. Department of Transportation; 1997. [Google Scholar]
- 20.Rosenbloom S. Sustainability and automobility among the elderly: An international assessment. Transportation. 2001;28:375–408. [Google Scholar]
- 21.Spain D. Societal trends: The aging baby boom and women's increased independence (No. DTFH61-97-P-00314) Washington, DC: 1997. [Google Scholar]
- 22.Submacular Surgery Trials Research Group. Evaluation of minimum clinically meaningful changes in scores on the National Eye Institute Visual Function Questionnaire (NEI-VFQ) SST Report Number 19. Ophthalmic Epidemiol. 2007;14:205–215. doi: 10.1080/09286580701502970. [DOI] [PubMed] [Google Scholar]
- 23.Spaeth G, Walt J, Keener J. Evaluation of Quality of Life for Patients With Glaucoma. Am J Ophthalmol. 2006;141:13–14. doi: 10.1016/j.ajo.2005.07.075. [DOI] [PubMed] [Google Scholar]
- 24.McKean-Cowdin R, Wang Y, Wu J, Azen SP, Varma R. Impact of Visual Field Loss on Health-Related Quality of Life in Glaucoma. The Los Angeles Latino Eye Study. Ophthalmology. 2008;115:941–948.e1. doi: 10.1016/j.ophtha.2007.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP, Los Angeles Latino Eye Study Group Severity of visual field loss and health-related quality of life. Am J Ophthalmol. 2007;143:1013–1023. doi: 10.1016/j.ajo.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gutierrez P, Wilson MR, Johnson C, Gordon M, Cioffi GA, Ritch R, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115:777–784. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 27.Parrish RK, 2nd, Gedde SJ, Scott IU, Feuer WJ, Schiffman JC, Mangione CM, et al. Visual function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115:1447–1455. doi: 10.1001/archopht.1997.01100160617016. [DOI] [PubMed] [Google Scholar]
- 28.Szlyk JP, Taglia DP, Paliga J, Edward DP, Wilensky JT. Driving performance in patients with mild to moderate glaucomatous clinical vision changes. J Rehabil Res Dev. 2002;39:467–482. [PubMed] [Google Scholar]
- 29.Szlyk JP, Mahler CL, Seiple W, Edward DP, Wilensky JT. Driving Performance of Glaucoma Patients Correlates With Peripheral Visual Field Loss. J Glaucoma. 2005;14:145–150. doi: 10.1097/01.ijg.0000151686.89162.28. [DOI] [PubMed] [Google Scholar]
- 30.Mangione CM, Phillips RS, Lawrence MG, Seddon JM, Orav EJ, Goldman L. Improved visual function and attenuation of declines in health-related quality of life after cataract extraction. Arch Ophthalmol. 1994;112:1419–1425. doi: 10.1001/archopht.1994.01090230033017. [DOI] [PubMed] [Google Scholar]
- 31.Williams RA, Brody BL, Thomas RG, Kaplan RM, Brown SI. The psychosocial impact of macular degeneration. Arch Ophthalmol. 1998;116:514–520. doi: 10.1001/archopht.116.4.514. [DOI] [PubMed] [Google Scholar]
- 32.Finger RP, Fleckenstein M, Holz FG, Scholl HP. Quality of life in age-related macular degeneration: a review of available vision-specific psychometric tools. Qual Life Res. 2008;17:559–574. doi: 10.1007/s11136-008-9327-4. [DOI] [PubMed] [Google Scholar]
- 33.Crabb DP, Viswanathan AC, McNaught AI, Poinoosawmy D, Fitzke FW, Hitchings RA. Simulating binocular visual field status in glaucoma. Br J Ophthalmol. 1998;82:1236–1241. doi: 10.1136/bjo.82.11.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crabb DP, Viswanathan AC. Integrated visual fields: A new approach to measuring binocular visual field of view and visual disability. Graefes Arch Clin Exp Ophthalmol. 2005;243:210–216. doi: 10.1007/s00417-004-0984-x. [DOI] [PubMed] [Google Scholar]
- 35.Crabb DP, Fitzke FW, Hitchings RA, Viswanathan AC. A practical approach to measuring visual field component of fitness to drive. Br J Ophthalmol. 2004;88:1191–1196. doi: 10.1136/bjo.2003.035949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mills RP, Drance SM. Esterman disability rating in severe glaucoma. Ophthalmology. 1986;93:371–378. doi: 10.1016/s0161-6420(86)33732-1. [DOI] [PubMed] [Google Scholar]
- 37.Massof RW. Moving Toward Scientific Measurements of Quality of Life. Ophthalmic Epidemiology. 2008;15:209–211. doi: 10.1080/09286580802419736. [DOI] [PubMed] [Google Scholar]
- 38.Smeeth L, Fletcher AE Improving the response rates to questionnaires. Several common sense strategies are effective. BMJ. 2002;324:1168–1169. doi: 10.1136/bmj.324.7347.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Increasing response rates to postal questionnaires: systematic review. BMJ. 2002;324:1183. doi: 10.1136/bmj.324.7347.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nakash RA, Hutton JL, Jorstad-Stein EC, Gates S, Lamb SE. Maximizing response to postal questionnaires. A systematic review of randomized trials in health research. BMC Med Res Metodol. 2006;6:5. doi: 10.1186/1471-2288-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]