Abstract
Objective
Interstitial cystitis/painful bladder syndrome (IC/PBS) is a chronic pain condition with unclear underlying etiology. Our objectives were to determine if psychological distress was higher in twins with urological symptoms commonly found in IC/PBS than twins without, and if so, did familial influences contribute to this association.
Method
Data from 1,165 female twins in a community-based sample were used. Urological symptoms, symptoms of posttraumatic stress disorder (PTSD), depression, anxiety, and perceived stress were assessed with standardized questionnaires. Generalized estimating equation regression models were used to examine the relationship between psychological distress and urological symptoms.
Results
Compared to unaffected twins, twins with urological symptoms were more likely to report PTSD symptoms (OR = 3.9; CI = 2.6-5.8), depression (OR = 3.1; CI = 2.0-5.0), anxiety (OR = 3.4; CI = 2.3-5.2), and perceived stress (OR = 3.2; CI = 2.1-4.9). After adjusting for familial influences, the within-pair effects remained significant for PTSD symptoms (OR = 2.2; CI = 1.2-3.8) and perceived stress (OR = 2.2; CI = 1.2-3.8).
Conclusion
Familial influences partially explained the relationship between indicators of psychological distress and urological symptoms. Future research should examine shared environmental and genetic mechanisms that may further explain this relationship and improve diagnosis and treatment of this unexplained clinical condition.
Keywords: Interstitial Cystitis, Painful Bladder Syndrome, Psychological Distress, Twins
INTRODUCTION
Interstitial cystitis (IC)/Painful Bladder Syndrome (PBS) is a painful and debilitating chronic pelvic condition of unknown etiology that predominantly affects women. IC/PBS is characterized by increased urinary frequency and urgency, dysuria, nocturia, and pain or discomfort in the bladder and pelvic area. The condition has been related to several comorbid conditions, including fibromyalgia, headache, unspecified back disorder, irritable bowel syndrome, and endometriosis[1]. Similarly, psychological distress, especially posttraumatic stress disorder (PTSD) symptoms, depression, anxiety, and stress, is common in IC/PBS[1-4] and has been associated with increased pain and symptom severity[5]. These associations, however, are primarily based on studies of clinic-based or tertiary care patient samples, which may be biased by clinical ascertainment from a treatment-seeking population.
Limited but emerging research has found that IC/PBS occurs more frequently in family members of patients with IC/PBS[6], suggesting that genetics or shared environmental factors, together known as familial factors, may play a role in the etiology of the condition. Consistent with genetic influences on IC/PBS, one small twin study found greater concordance for IC/PBS among monozygotic than dizygotic twins[7]. Further, a substantial body of literature has documented the genetic and familial contributions to PTSD, depression, anxiety, and other indicators of psychological distress[8-10]. However, only two studies have specifically examined the potential familial link between IC/PBS and any measures of psychological distress. Both studies focused on the familial association between IC/PBS symptoms and panic disorder, a complex anxiety disorder characterized by recurrent episodes of uncontrollable fear and other symptoms, and found that first degree relatives of IC/PBS patients were about three times more likely than family members of controls to report panic disorder[3,11]. Likewise, first degree relatives of patients with panic disorder were up to three times more likely than control family members to report IC/PBS symptoms, suggesting a familial and possibly genetic linkage between these two seemingly disparate conditions.
Taken together, previous investigations suggest substantial comorbidity between IC/PBS and psychological distress indicators in primarily clinic-based or tertiary care patient samples. Additionally, there is some evidence that familial factors may play a role in the relationship between IC/PBS and panic disorder. However, to our knowledge no studies have examined if familial influences contribute to the relationship between multiple indicators of psychological distress and IC/PBS symptoms. The aims of the present study were to assess if indicators of psychological distress, namely symptoms of PTSD, depression, anxiety, and perceived stress, were associated with urological symptoms commonly found in IC/PBS among female twins enrolled in a community-based twin registry, and elucidate the role of familial factors in this relationship. We chose these specific distress indicators because they have most often been studied in relation to urological symptoms in clinical samples. We hypothesized that compared to twins without urological symptoms, twins with these symptoms would report higher levels of psychological distress and this finding could be partially explained by familial influences.
MATERIAL AND METHODS
Sample
The University of Washington Twin Registry is a community-based sample of twins derived from the drivers’ license applications of the Washington State Department of Licensing. Full details of the construction and characteristics of the University of Washington Twin Registry are described elsewhere[12]. In brief, Washington State drivers’ license numbers are derived from a person's name and date of birth, thus, the Department of Licensing asks every new applicant if s/he is a twin to avoid issuing duplicate license and identification numbers to twins. Because state agencies in Washington are permitted by law to share data, the Department of Licensing provides a list of all new drivers' license applicants who are twins to the University of Washington. Registry staff contacts each twin to obtain informed consent, complete a brief survey, and join the Registry on an ongoing basis. Co-twins are contacted using information provided by the index twin. Registry procedures have been approved by the Washington State Attorney General and the University of Washington Human Subjects Review Committee.
Data Collection
A comprehensive health survey with information on demographics, health habits, and psychological distress indicators was mailed to all twins in two waves. In addition, a set of three questions asked female twins about urological symptoms commonly found in IC/PBS.
Psychological Distress
Several brief, standardized questionnaires were used to assess psychological distress variables over the past four weeks. Symptoms of PTSD were assessed with a 5-item scale that asked about hypervigilance, avoidance, and re-experiencing in relation to a traumatic event. This measure was developed for use with primary care patients and has similar characteristics to other brief screening measures for anxiety[13]. Scores range from 0-15 and have good reliability estimates (Cronbach's alpha = 0.86). Symptoms of depression were assessed with the Patient Health Questionnaire-2 (PHQ-2)[14], a brief measure of key depressive symptoms, with scores ranging from 0-6. The PHQ-2 has good validity and reliability estimates (Cronbach's alpha = 0.78)[15]. To evaluate anxiety symptoms, we used the anxiety subscale of the Brief Symptom Inventory[16], commonly administered in medical and psychiatric populations. Scores range from 0-24, and the anxiety subscale is valid and has good reliability estimates (Cronbach's alpha = 0.84)[17]. The Cohen Perceived Stress Scale[18], which assesses subjective reactions to demands from stressful experiences, was used to measure stress. This instrument yields scores ranging from 0-38 and is reliable (Cronbach's alpha = 0.78)[19].
Although the psychological distress variables were based on continuous scales, initial examination of the data found them to not be normally distributed. Therefore, each psychological distress variable was categorized into four quartiles, representing increasing levels of distress. The PTSD scores were categorized as 0, 1, 2-3, and ≥4. The depression scores were categorized as 0, 1, 2, and ≥3. Anxiety score categorization was 0, 1-2, 3-4, and ≥5. Perceived stress scores were categorized as 0-9, 10-14, 15-19, and ≥20.
Urological Symptoms
Three questions asked about urological symptoms commonly found in IC/PBS. Female twins were asked if they had: 1) “pain, pressure, or discomfort in the pelvis, groin, or upper thigh that worsens when your bladder fills?”; 2) “pain, pressure, or discomfort in the pelvis, groin, or upper thigh that is relieved or improved by emptying your bladder?”; and 3) if they urinated frequently. Twins were considered positive for urological symptoms if they responded positively to the first question and positively to either the second or third question[20].
Other Data
Demographic information consisted of age, sex, race/ethnicity, marital status, education, and income. To assess zygosity, we used questions about childhood similarity that reliably classify zygosity with an accuracy of 95 – 98% compared with zygosity determined by biological indicators[21].
Statistical Analyses
Descriptive statistics for participant characteristics were calculated using means and standard deviations for continuous variables and percentages for categorical variables. Generalized estimating equation (GEE) regression models with the appropriate link function were used to assess differences for demographic characteristics in twins with and without urological symptoms. GEE models adjust standard error estimates to account for correlation within twin pairs[22].
Our analytic approach was to first estimate the overall association between psychological distress indicators and urological symptoms in all female twins, and then estimate the within-pair effects (i.e., comparison of the twin who is positive for urological symptoms to the co-twin who is not) that are adjusted for familial influences. Because twin pairs share a similar family environment and a portion of their genes (100% in monozygotic and on average 50% in dizygotic pairs), within-pair estimates are adjusted for familial and some genetic influences. If within-pair associations are attenuated and rendered non-significant compared to the overall effect obtained in our initial regression analyses, we can conclude that familial factors contribute to these associations. Alternately, a within-pair association that remains robust compared to the overall effect provides evidence that familial factors do not play a prime role in the association between psychological distress and urological symptoms.
We used GEE ordinal logistic regression to examine the association between psychological distress and urological symptoms. We first modeled the overall associations between psychological distress and urological symptoms in all twins. We adjusted for age as a potential confounder by including it as an independent variable in regression models. We report age-adjusted odds ratios (OR) and 95% confidence intervals (CI) that compare the odds of more versus less psychological distress in twins with urological symptoms to the odds in twins without urological symptoms. These overall analyses did not control for shared familial factors. Next, we conducted a second set of regression analyses that used the additional information on familial factors available in the twin sample. We examined the within-pair associations between psychological distress and urological symptoms after adjusting for the between-pair effect[23]. We used Stata/SE 10.1 software (StataCorp; College Station, TX) for all statistical analyses.
RESULTS
The health survey was mailed to 2,188 female twins, of which 1,419 (65%) returned a completed survey. Of these, 254 were excluded from analyses because they had a male co-twin, leaving 1,165 female twins. Table 1 describes the characteristics of the sample as a whole, and stratified by urological symptom classification. The mean age of the twins was 36 years, 64% were monozygotic, 87% were White, 48% were married or living with a partner, 43% obtained at least a bachelor's degree, and 26% had a household income of $80,000 or higher. Nearly 8% of the sample was positive for urological symptoms based on two out of three questions. Twins with urological symptoms were older (p < 0.01) and with less education (p < 0.05) than twins without symptoms. The groups did not differ in zygosity, race/ethnicity, marital status, or income.
Table 1.
Characteristics of female twins in the University of Washington Twin Registry health survey.
| All Twins | Urological Symptoms | ||
|---|---|---|---|
| Characteristics | (n = 1,165) |
Yes (n = 91) |
No (n = 1,074) |
| Age, mean years (SD)** | 36 (15) | 41 (17) | 36 (15) |
| Monozygotic, % | 64 | 73 | 63 |
| White, % | 87 | 85 | 87 |
| Married or living with a partner, % | 48 | 53 | 47 |
| Education, %* | |||
| Less than high school graduate | 3 | 7 | 2 |
| High school graduate | 10 | 13 | 9 |
| Some college, no degree | 33 | 29 | 34 |
| Technical/vocation school graduate | 12 | 20 | 12 |
| Bachelor's degree or higher | 43 | 32 | 43 |
| Annual household income, % | |||
| < $20,000 | 21 | 26 | 21 |
| $20,000 – $39,999 | 22 | 27 | 21 |
| $40,000 – $59,999 | 18 | 20 | 17 |
| $60,000 – $79,999 | 13 | 9 | 14 |
| ≥ $80,000 | 26 | 19 | 27 |
p < 0.01;
p < 0.05 signifies significant differences between those with and without urological symptoms.
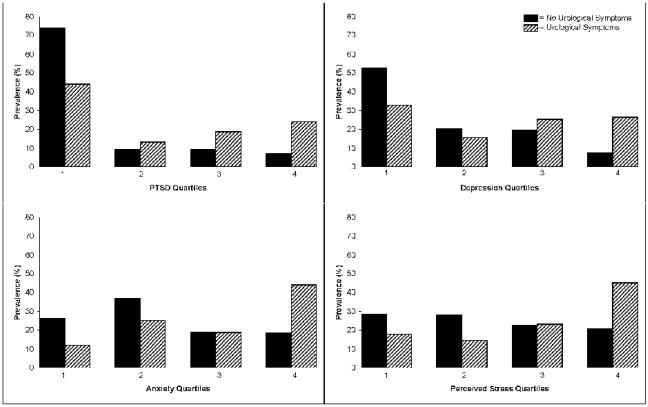
Figure 1 depicts the distribution of psychological distress scores by urological symptom status. Although the majority of twins denied any PTSD or depression symptoms, a larger proportion of twins positive for urological symptoms were in the higher distress categories for both PTSD (e.g., 24% versus 7% in the highest quartile) and depression (e.g., 26% versus 8% in the highest quartile). The anxiety and perceived stress scores were more evenly distributed across distress categories, however, twins positive for urological symptoms were overrepresented in the highest distress categories for both anxiety (44% versus 18%) and perceived stress (45% versus 21%).
Figure 1.
Distribution of categorized psychological distress scores by urological symptom status.
Table 2 presents the age-adjusted ORs and 95% CIs for the overall and within-pair associations between psychological distress indicators and urological symptoms. The overall analyses revealed significant associations of PTSD symptoms, depression, anxiety, and perceived stress with urological symptoms. Compared to twins without urological symptoms, twins with urological symptoms were 3.1 – 3.9 times more likely to have higher levels of psychological distress. After adjusting for familial factors in the within-pair analyses, the relationships with depression and anxiety were diminished. The associations with PTSD (OR = 2.2; 95% CI = 1.3 – 3.5) and perceived stress (OR = 2.2; 95% CI = 1.2 – 3.8) were attenuated but remained significant.
Table 2.
Odds ratios and 95% confidence intervals for the age-adjusted associations between psychological distress indicators and urological symptoms in female twins.
| Overall | Within-pair* | |||
|---|---|---|---|---|
| Psychological Distress | OR | (95% CI) | OR | (95% CI) |
| Posttraumatic stress disorder symptoms | 3.9 | (2.6 – 5.8) | 2.2 | (1.3 – 3.5) |
| Depression | 3.1 | (2.0 – 5.0) | 1.6 | (0.8 – 3.0) |
| Anxiety | 3.4 | (2.3 – 5.2) | 1.8 | (1.0 – 3.3) |
| Perceived stress | 3.2 | (2.1 – 4.9) | 2.2 | (1.2 – 3.8) |
Adjusted for familial contributions;
OR = odds ratio; CI = confidence interval
DISCUSSION
In this study, twins with urological symptoms experienced greater psychological distress, namely higher levels of PTSD, depression, and anxiety symptoms, and perceived stress, than their counterparts without urological symptoms. These findings from a community-based sample are consistent with reports from clinical populations that compare rates to healthy controls[2]. The prevalence of urological symptoms among the twins was 7.8%, falling within the limits of previously reported estimates from community studies of women[24-26]. Further, the twins without urological symptoms reported comparable rates of psychological distress to the general population [27]. Because our findings from a community-based sample were consistent with previous studies of clinical patients, it is likely that the increased rates of PTSD, depression, anxiety, and perceived stress seen in clinical samples with IC/PBS are not an artifact of clinical ascertainment. .
This is the first study of psychological distress and urological symptoms in twins. After adjusting for shared familial factors, we found that the relationship between depression and anxiety and urological symptoms were diminished, consistent with familial factors partially explaining these relationships. These findings also are consistent with the role of familial factors in the association of psychological distress and other unexplained pain conditions, such as chronic widespread pain, temporomandibular joint disorder, and migraine headaches [28-30]. Greater concordance rates for IC/PBS among monozygotic twins has been reported[7] and common genetic factors may explain the co-occurrence between IC/PBS and anxiety disorders[3,6]. Specifically, a chromosome 13 syndrome characterized by a mutation in one or more genes has been described that may increase vulnerability to several conditions, including panic and other anxiety disorders, IC/PBS, mitral valve prolapse, thyroid problems, and chronic headaches[3]. Our findings are consistent with these reports of a familial influence between urological symptoms and anxiety disorders; however, this was only a partial explanation.
The associations between PTSD and perceived stress and urological symptoms remained significant even after controlling for familial factors, suggesting that unique environmental factors made further contributions. These significant relationships even after controlling for familial factors indicate environmental factors such as trauma, chronic environmental stress, or medical illness may play a role, perhaps by increasing urological symptoms or altering pain processing. In addition, lifestyle factors, such as poor coping, deficient self-care, or reduced physical activity may increase pain perception as well as psychological distress levels. Taken together, these findings are consistent with prevailing theories on the multi-faceted nature of IC/IBS[31]. Thus, our findings support the need for a comprehensive evaluation of patients' urological symptoms as well as psychosocial and environmental needs.
This study had several limitations. First, self-reported assessment of urological symptoms was sub-optimal and may not accurately correlate with clinical diagnosis of IC/PBS. Second, our sample was predominately White, female, and educated, thus limiting the generalizability of our findings to other populations. Third, brief screening measures for psychological distress may yield false positive cases of true psychiatric conditions, especially in nonclinical populations. While the rates of positive screens in the overall sample were comparable to results found in primary care samples[14], our findings should be replicated by using more detailed diagnostic interviews with independent clinician ratings. Fourth, although our findings showed that only the association between PTSD and perceived stress and urological symptoms remained significant after controlling for familial factors, the within-pair findings for depression and anxiety approached significance. This suggests that these results may have been hampered by sample size constraints and reduced power and should be replicated with a larger sample of twins. Fifth, the conditions assessed were based on different time scales (i.e., urological symptom were current, whereas psychological distress was assessed for the last four weeks) and age of onset of these conditions were not assessed. Therefore, we were not able to examine the temporal sequence of urological and psychological symptoms. Finally, the psychological distress measures we used likely overlap, hence the results need to be interpreted with caution.
In sum, in our large community-based sample of twins we found psychological distress indicators were consistently related to urological symptoms, an observation explained by shared familial influences and as yet undetermined environmental factors. The confluence of psychological distress, increased symptom severity, and higher rates of disability [32] among individuals with urological and IC/PBS symptoms highlight the need for a biopsychosocial treatment approach. Cognitive-behavioral and self-care interventions have resulted in short-term improvements in IC/PBS symptoms[33]. Future research should examine the possible genetic, environmental, and central nervous system mechanisms that may explain the link between psychological distress and IC/PBS symptoms and can contribute to improved diagnosis and treatment in this population.
Acknowledgments
This research was supported by National Institutes of Health awards R01AR051524 (Dr. Afari) and U01 DK082325 (Drs. Buchwald and Afari). Dr. Afari also is supported by the VA Center of Excellence for Stress and Mental Health. Dr. Johnson Wright is supported in part by R01AR051524. We also thank the twins who are taking part in the University of Washington Twin Registry for their time and enthusiasm. A portion of this research was presented at the 28th Annual American Pain Society meeting in San Diego, CA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Clemens JQ, Meenan RT, O'Keeffe Rosetti MC, Kimes TA, Calhoun EA. Case-control study of medical comorbidities in women with interstitial cystitis. J Urol. 2008;179(6):2222–5. doi: 10.1016/j.juro.2008.01.172. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein HB, Safaeian P, Garrod K, Finamore PS, Kellogg-Spadt S, Whitmore KE. Depression, abuse and its relationship to interstitial cystitis. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(12):1683–6. doi: 10.1007/s00192-008-0712-x. [DOI] [PubMed] [Google Scholar]
- 3.Talati A, Ponniah K, Strug LJ, Hodge SE, Fyer AJ, Weissman MM. Panic disorder, social anxiety disorder, and a possible medical syndrome previously linked to chromosome 13. Biol Psychiatry. 2008;63(6):594–601. doi: 10.1016/j.biopsych.2007.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clemens JQ, Brown SO, Calhoun EA. Mental health diagnoses in patients with interstitial cystitis/painful bladder syndrome and chronic prostatitis/chronic pelvic pain syndrome: a case/control study. J Urol. 2008;180(4):1378–82. doi: 10.1016/j.juro.2008.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clemens JQ, Brown SO, Kozloff L, Calhoun EA. Predictors of symptom severity in patients with chronic prostatitis and interstitial cystitis. J Urol. 2006;175(3 Pt 1):963–6. doi: 10.1016/S0022-5347(05)00351-4. discussion 967. [DOI] [PubMed] [Google Scholar]
- 6.Dimitrakov J, Guthrie D. Genetics and phenotyping of urological chronic pelvic pain syndrome. J Urol. 2009;181(4):1550–7. doi: 10.1016/j.juro.2008.11.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warren J, Jackson T, Meyers D, Xu J. Concordance of interstitial cystitis (IC) in identical twins: preliminary data. Urology. 2001;57(6 Suppl 1):126. doi: 10.1016/s0090-4295(01)01094-9. [DOI] [PubMed] [Google Scholar]
- 8.Gross C, Hen R. Genetic and environmental factors interact to influence anxiety. Neurotox Res. 2004;6(6):493–501. doi: 10.1007/BF03033286. [DOI] [PubMed] [Google Scholar]
- 9.Koenen KC. Genetics of posttraumatic stress disorder: Review and recommendations for future studies. J Trauma Stress. 2007;20(5):737–50. doi: 10.1002/jts.20205. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000;157(10):1552–62. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- 11.Weissman MM, Gross R, Fyer A, Heiman GA, Gameroff MJ, Hodge SE, Kaufman D, Kaplan SA, Wickramaratne PJ. Interstitial cystitis and panic disorder: a potential genetic syndrome. Arch Gen Psychiatry. 2004;61(3):273–9. doi: 10.1001/archpsyc.61.3.273. [DOI] [PubMed] [Google Scholar]
- 12.Afari N, Noonan C, Goldberg J, Edwards K, Gadepalli K, Osterman B, Evanoff C, Buchwald D. University of Washington Twin Registry: construction and characteristics of a community-based twin registry. Twin Res Hum Genet. 2006;9(6):1023–9. doi: 10.1375/183242706779462543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther. 2005;43(5):585–94. doi: 10.1016/j.brat.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 15.Daig I, Herschbach P, Lehmann A, Knoll N, Decker O. Gender and age differences in domain-specific life satisfaction and the impact of depressive and anxiety symptoms: a general population survey from Germany. Qual Life Res. 2009;18(6):669–78. doi: 10.1007/s11136-009-9481-3. [DOI] [PubMed] [Google Scholar]
- 16.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- 17.De Jong MM, An K, McKinley S, Garvin BJ, Hall LA, Moser DK. Using a 0-10 scale for assessment of anxiety in patients with acute myocardial infarction. Dimens Crit Care Nurs. 2005;24(3):139–46. doi: 10.1097/00003465-200505000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. [PubMed] [Google Scholar]
- 19.Mitchell AM, Crane PA, Kim Y. Perceived stress in survivors of suicide: psychometric properties of the Perceived Stress Scale. Res Nurs Health. 2008;31(6):576–85. doi: 10.1002/nur.20284. [DOI] [PubMed] [Google Scholar]
- 20.van de Merwe JP, Nordling J, Bouchelouche P, Bouchelouche K, Cervigni M, Daha LK, Elneil S, Fall M, Hohlbrugger G, Irwin P, Mortensen S, van Ophoven A, Osborne JL, Peeker R, Richter B, Riedl C, Sairanen J, Tinzl M, Wyndaele JJ. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008;53(1):60–7. doi: 10.1016/j.eururo.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 21.Reed T, Plassman BL, Tanner CM, Dick DM, Rinehart SA, Nichols WC. Verification of self-report of zygosity determined via DNA testing in a subset of the NAS-NRC twin registry 40 years later. Twin Res Hum Genet. 2005;8(4):362–7. doi: 10.1375/1832427054936763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diggle PJHP, Liang KY, Zeger SL. Analysis of longitudinal data. Oxford University Press Inc.; New York: 2002. [Google Scholar]
- 23.Begg M, Parides M. Separation of individual-level and cluster-level covariate effects in regression analysis of correlated data. Stat Med. 2003;30(22):2591–2602. doi: 10.1002/sim.1524. [DOI] [PubMed] [Google Scholar]
- 24.Ibrahim IA, Diokno AC, Killinger KA, Carrico DJ, Peters KM. Prevalence of self-reported interstitial cystitis (IC) and interstitial-cystitis-like symptoms among adult women in the community. Int Urol Nephrol. 2007;39(2):489–95. doi: 10.1007/s11255-007-9181-2. [DOI] [PubMed] [Google Scholar]
- 25.Parsons JK, Kurth K, Sant GR. Epidemiologic issues in interstitial cystitis. Urology. 2007;69(4 Suppl):5–8. doi: 10.1016/j.urology.2006.05.050. [DOI] [PubMed] [Google Scholar]
- 26.Parsons CL, Dell J, Stanford EJ, Bullen M, Kahn BS, Waxell T, Koziol JA. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002;60(4):573–8. doi: 10.1016/s0090-4295(02)01829-0. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arguelles LM, Afari N, Buchwald DS, Clauw DJ, Furner S, Goldberg J. A twin study of posttraumatic stress disorder symptoms and chronic widespread pain. Pain. 2006;124(1-2):150–7. doi: 10.1016/j.pain.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diatchenko L, Nackley AG, Slade GD, Fillingim RB, Maixner W. Idiopathic pain disorders--pathways of vulnerability. Pain. 2006;123(3):226–30. doi: 10.1016/j.pain.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 30.Schur EA, Noonan C, Buchwald D, Goldberg J, Afari N. A twin study of depression and migraine: evidence for a shared genetic vulnerability. Headache. 2009;49(10):1493–502. doi: 10.1111/j.1526-4610.2009.01425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Homma Y, Ueda T, Tomoe H, Lin AT, Kuo HC, Lee MH, Lee JG, Kim DY, Lee KS. Clinical guidelines for interstitial cystitis and hypersensitive bladder syndrome. Int J Urol. 2009;16(7):597–615. doi: 10.1111/j.1442-2042.2009.02326.x. [DOI] [PubMed] [Google Scholar]
- 32.Michael YL, Kawachi I, Stampfer MJ, Colditz GA, Curhan GC. Quality of life among women with interstitial cystitis. J Urol. 2000;164(2):423–7. [PubMed] [Google Scholar]
- 33.Webster DC, Brennan T. Self-care effectiveness and health outcomes in women with interstitial cystitis: implications for mental health clinicians. Issues Ment Health Nurs. 1998;19(5):495–519. doi: 10.1080/016128498248926. [DOI] [PubMed] [Google Scholar]