Abstract
Background
The relationships between worker health and productivity are becoming clearer. However, few large scale studies have measured the direct and indirect cost burden of overweight and obesity among employees using actual biometric values.
Objective
To quantify the direct medical and indirect (absence and productivity) cost burden of overweight and obesity in workers.
Subjects
A cross-sectional study of 10,026 employees in multiple professions and worksites across the U.S.
Measures
The main outcomes were five self-reported measures of workers’ annual healthcare use and productivity: doctor visits, emergency room visits, hospitalizations, absenteeism (days absent from work), and presenteeism (percent on-the-job productivity losses). Multivariate count and continuous data models (Poisson, negative binomial and zero-inflated Poisson) were estimated.
Results
After adjusting for covariates, obese employees had 20% higher doctor visits than normal weight employees (CI 16%, 24%, p < 0.01) and 26% higher emergency room visits (CI 11%, 42%, p < 0.01). Rates of doctor and emergency room visits for overweight employees were no different than those of normal weight employees. Compared to normal weight employees, presenteeism rates were 10% and 12% higher for overweight and obese employees, respectively (CI 5%, 15% and 5%, 19%, all p < 0.01). Taken together, compared to normal weight employees, obese and overweight workers were estimated to cost employers $644 and $201 more per employee per year, respectively.
Conclusions
This study provides evidence that employers face a financial burden imposed by obesity. Implementation of effective workplace programs for the prevention and management of excess weight will benefit employers and their workers.
Keywords: worksite health promotion, weight management, obesity, expenditures, health care costs, productivity, workplace wellness
INTRODUCTION
Approximately two-thirds of the U.S. adult population is overweight or obese, with 32 percent being obese (1, 2). Obesity is associated with chronic health conditions including certain types of cancer, type 2 diabetes, heart disease, stroke, high blood pressure, high cholesterol, and sleep disorders (3, 4). Obesity-related medical expenditures are significant, estimated to cost Americans 147 billion dollars annually in 2008 (5).
The causes of obesity are inextricably linked and complicated, as excess weight is linked to certain environmental factors, genetics, individual behaviors, access to health improvement resources and the healthcare system (6). Designing interventions for this complex health problem requires concerted effort among many actors, including those in public and private sectors. A key site of intervention is the workplace since employers have a vested interest in promoting the health and well-being of their workers.
A growing body of literature has valued the cost burden imposed by excess weight on employers, including direct (medical) and indirect (productivity-related) costs. Based on self-reported and biometric data for over 36,000 employees and spouses of a manufacturing company during 2001–2002, Wang et al. found that annual per-person healthcare spending rose in an almost linear fashion for overweight and obese participants (those with BMI ≥ 25), with a $120 (2004 USD) increase in medical spending per unit increase in BMI (7). Likewise, using the 2000 Medical Expenditure Panel Survey (MEPS) for more than 16,000 respondents, Arterburn et al. found that obese respondents had significantly higher medical spending (8). In both studies, spending for overweight respondents was not significantly different than for their normal weight counterparts.
Other studies have examined the relationship between excess weight and healthcare utilization. Contrasting the healthcare utilization patterns of 539 obese (biometric BMI > 27.9) health plan enrollees with a matched sample of non-obese enrollees (BMI 18.5–24.9), Raebel et al. found that inpatient admissions, outpatient visits, professional claims, and prescription drugs were higher for obese patients (9). Another study based on a 1993 survey of 17,188 HMO members showed higher healthcare utilization rates and costs for obese members; however, with few exceptions, utilization and costs for overweight members were the same as or lower than normal weight members (10).
In addition to direct costs, indirect costs associated with excess weight borne by employers have been found to be substantial. Obesity-associated absenteeism costs have been estimated to be approximately $4.3 billion annually in the U.S. (11). Quesenberry et al. found higher medical costs and absenteeism rates were associated with higher self-reported BMI values (12) and Cawley et al. showed that obese workers experienced greater losses in hours of productivity (absenteeism and presenteeism) than overweight or normal weight workers, although overweight and normal weight workers did not differ significantly (13). Gates et al. found a nonlinear relationship between biometric BMI categories and absence and productivity, with moderately and extremely obese employees having higher rates of absenteeism and presenteeism (14).
Indirect costs associated with on-the-job productivity losses (presenteeism) have been found to exceed losses due to absenteeism. Goetzel et al. showed that presenteeism costs associated with specific disorders—primarily migraine, respiratory disease, depression, and arthritis—exceeded costs associated with absenteeism and medical expenditures (15). In a recent study, Durden et al. examined administrative claims, health risk assessment (HRA), and productivity (absence) data for a large commercially-insured population (16). They found that absenteeism costs increased with self-reported BMI, and overweight employees incurred slightly lower healthcare costs than normal weight employees (16).
With this literature as background, the National Heart, Lung, and Blood Institute (NHLBI) funded seven academic centers to study a the effects of introducing environmental interventions at U.S. worksites to stem the incidence of obesity among employees (17). Four of the participating research sites, Emory University, the University of Rochester, the University of Minnesota, and the University of Massachusetts Medical School, pooled baseline data for employee participants in these studies to quantify the direct and indirect costs and overall financial burden imposed by overweight and obesity on workers and their employers.
This study had two primary goals: 1) to analyze the associations between overweight and obesity, as measured using biometric BMI, and self-reported measures of healthcare utilization, presenteeism, and absenteeism; and 2) to estimate the differences in employer costs between obese, overweight and normal weight employees as determined by employee healthcare utilization, absenteeism, and presenteeism. We report the direct and indirect costs of excess weight on healthcare utilization and productivity based on a large sample of diverse workers and worksites. Because of its timeliness, the current study aims to influence further development of effective employer-sponsored interventions by emphasizing the economic implications of this prevalent and costly health risk.
METHODS
Study Design
This research is a part of a larger initiative of seven independent studies examining the impact of environmental obesity management interventions in various worksites across the U.S. Detailed information on study designs, sites, and interventions for each of the seven research sites has previously been published (17). This study builds upon individual center efforts by, for the first time, pooling data across study sites as part of the larger NHLBI initiative. Four of the seven participating research sites contributed data to this study. Sites were included only if they had professionally collected biometric height and weight data and self-reported healthcare utilization, absenteeism, and presenteeism data; thus, three of the seven sites in the NHLBI initiative were excluded because they lacked one or some combination of these data sources.
Although the data collection methods were unique to each study site, a common set of anthropometric and survey measures of interest to this analysis were used. Baseline data collected in late 2005 through early 2007 (prior to the worksite interventions) were provided by the study centers. All of the collected data were de-identified; a site code allowed researchers to distinguish responses across employers. The data were quality-checked and aggregated into a single data set. Research protocols for each site were approved by the Institutional Review Boards (IRBs) at study centers leading the research.
Outcome Variables
The main outcome variables were five self-reported annual health and productivity measures: doctor visits, emergency room (ER) visits, hospitalizations, absenteeism (number of days absent from work), and presenteeism (percent on-the-job productivity losses). Employees were asked to record the number of absent days taken in the previous year and their healthcare utilization (i.e., number of doctor visits, admissions to the hospital, and visits to the ER in the prior year). Self-reported healthcare utilization and productivity data were used because study sites, for the most part, did not have access to administrative claims data. However, as reported in a previous NHLBI-funded study, self-reported healthcare utilization and productivity data may serve be a valid proxy for administrative data when administrative claims data are not available (18). All sites also administered the eight-item Work Limitations Questionnaire (WLQ), an instrument assessing on-the-job productivity losses or presenteeism (19, 20). The WLQ measures reductions in workers’ productivity over and above a standard level of productivity experienced by healthy workers. WLQ responses were scored by Dr. Debra Lerner at the New England Medical Center and incorporated into the final dataset (19, 20).
Explanatory Variables
The main independent variable was BMI. At each worksite, biometric measures (individuals’ weight and height measures taken by trained study personnel) were obtained, which were converted into BMI values using the following formula (where weight is in pounds and height is in inches):
Subjects were grouped into three BMI categories: normal (BMI 18.0 – 24.9), overweight (BMI 25.0 – 29.9), and obese (BMI ≥ 30.0) (21, 22). Seventeen individuals with BMI values below 18.0 were excluded because individuals with those values would be considered underweight or may have serious medical conditions.
Other explanatory (covariate) variables included: age, gender, race/ethnicity, education, profession, and smoking status. Smoking status was included as an explanatory variable because smoking behavior may affect healthcare utilization and absenteeism days (23). Research site was also included as an indicator to control for site-to-site variation. Research site also acted as a proxy for geographic variations likely to affect healthcare utilization.
Statistical Analyses
Regression models
A series of General Linear Models (GLMs) were used to examine the relationship between BMI and outcomes, controlling for covariates. The general model is depicted as follows:
where Visitsi is an outcome variable for an individual i and f indicates the link function for the model. All dependent variables, except presenteeism, were counts of events.
We used the modified Park Test to guide the selection of the appropriate GLM distributions based on whether the raw scale residuals produced overdispersion (24, 25). Use of a Poisson model for count outcomes requires the variance of the dependent variable to be equal to the mean (no overdispersion). In cases where overdispersion was detected through a deviance or Pearson chi-squared value substantially exceeding 1.0, negative binomial models were estimated.
Since no overdispersion was detected when evaluating ER visits, a Poisson model was used. However, overdispersion was detected for doctor visits, thus a negative binomial regression was estimated.
Zero-inflated models
Because not all workers incurred the five outcomes of interest in this study (e.g., not all employees were hospitalized in the past year or were absent from work due to illness), we needed to address the issue of “zero observations” when estimating these outcome measures (26). Two-part and zero-inflated models were used to address this issue. The two-part model included a logistic regression equation designed to estimate relationships between the BMI variable and the likelihood of incurring any medical- or productivity-related expenditures during the study period. The second part of the model included an ordinary least squares (OLS) regression equation that showed relationships between BMI and the outcome of interest, controlling for demographic and other covariates, for individuals who incurred any expenditures during the study period. The zero-inflated model is a variant of the two-part model in that it includes a mix of people, some of whom had zero utilization (27).
In outcomes with a high proportion of zero values (or “excess” zeroes), zero-inflated Poisson (ZIP) models were used to correct for the high proportion of zero values in the dependent variable, in addition to allowing for overdispersion (28). We performed a Vuong test to confirm that a zero-inflated Poisson model was a better fit than the standard Poisson model. For hospitalizations and absenteeism, both overdispersion and a high proportion of zeroes (well over 65% of responses were zero) were detected, and zero-inflated Poisson models were estimated.
Presenteeism Models
Finally, the log-gamma GLM was employed for the presenteeism model where the observed distribution of data was regarded as a reasonable fit to an empirical distribution. The gamma distribution was also verified based on the results of the modified Park test on the raw scale residuals given log link (i.e., λ = 2). Using these regression models, adjusted estimates of utilization and productivity outcomes across the three BMI groups were computed. To hold the distribution of covariates constant across each BMI group, all employees were coded as if they were in the normal BMI category, and the linear combination of the covariates was exponentiated to return the values back to their natural units (e.g., doctor visits). This step was repeated for the overweight and obese BMI groups, and the differences between the predicted values for each group and the normal group (as the reference group) were calculated. Similarly, for the ZIP models, two separate predictions based on the binomial and Poisson distributions were multiplied to account for the two-step model.
A nonparametric bootstrap method (2,000 replications) was employed to estimate the mean utilization for each BMI group and the difference in mean utilization across BMI groups (using the normal weight group as a reference). Nonparametric 95% confidence intervals were calculated by rank ordering each bootstrap sample from the lowest to the highest value and identifying the values representing the 2.5th and 97.5th percentiles (29).
Missing Data
Two-thirds of the observations had complete data available for a regression model, and missing data patterns were nonmonotone. In this case, complete case analysis or listwise deletion would lead to loss of statistical power. Missing values were imputed for independent and dependent variables (e.g., BMI, gender, age) using the Markov Chain Monte Carlo (MCMC) approach, which allows for arbitrary missing data patterns (30, 31). Because a number of employees were missing data on profession, the MCMC imputation was not employed for this variable, and an additional profession category (missing) were included in the regression models. A sensitivity analysis was performed by omitting employees with missing values on any measure, which yielded comparable results.
Financial outcomes
The financial outcomes of the study were medical expenditures calculated by counting the number of inpatient, outpatient, and ER services, and from productivity losses due to absenteeism and presenteeism. To generate these calculations, average medical expenditures for inpatient, outpatient, and ER services were estimated from the 2006 MarketScan Research Databases containing adjudicated claims information for over 16 million enrollees with employer-sponsored health insurance in the U.S. We calculated only the employer liability amount from each claim and determined that the average payment for a doctor visit was $60, an ER visit $563, and a hospitalization $12,321.
To estimate standard dollar losses associated with absenteeism and presenteeism, we used a national average hourly wage for 2006 of $25.67 and calculated an annual average wage of $49,286, assuming 240 work days per year (32). Average expenditures in health service utilization and productivity losses were obtained by multiplying the estimated number of hospital visits, ER use, doctor visits, days absent from work, and unproductive days while at work by their monetized values.
Data management and analyses were performed using SAS 9.1 (33). The nonparametric bootstrap was conducted using STATA 10.0 (34).
RESULTS
Table 1 displays the characteristics of the sample. Over half of the data came from the Emory University research site, about a quarter from the University of Rochester, and the balance from the Universities of Minnesota and Massachusetts. Respondents were employees drawn from the following four industries corresponding to the research centers conducting the studies: Emory – manufacturing; Rochester – manufacturing; Minnesota – transportation; and Massachusetts – healthcare.
TABLE 1.
Characteristics of the Sample (n = 10,026)
| Characteristic | |
|---|---|
| Research site (%) | |
| University of Rochester | 27.70 |
| University of Massachusetts Medical School | 8.94 |
| University of Minnesota | 11.19 |
| Emory University | 52.17 |
| Gender (%) | |
| Female | 31.60 |
| Male | 68.40 |
| Race/Ethnicity (%) | |
| White | 74.81 |
| African American | 12.35 |
| Hispanic | 7.28 |
| Asian | 3.52 |
| Other | 2.04 |
| Profession (%) | |
| Managerial/professional | 35.56 |
| Technological | 17.47 |
| Office/sales | 7.00 |
| Craftsman | 8.22 |
| Laborer | 1.51 |
| Operations | 11.99 |
| Missing | 17.08 |
| Smoking status (%) | |
| Current | 14.26 |
| Former | 25.00 |
| Never | 60.74 |
| Body mass index (BMI) (mean) | |
| Normal (18.5–24.9) | 29.16 |
| Overweight (25.0–29.9) | 31.43 |
| Obese (30.0+) | 39.41 |
| Age, mean (SD) | 45.26 (8.02) |
Approximately two-thirds of the employees were male, almost three-fourths were white, and the average age was 45 years. A variety of professions was represented, mostly white collar, including management (36%) and technology (17%). A quarter of employees were former smokers, 14% current smokers, while nearly 61% had never smoked. Employees were almost equally distributed across the three BMI categories with obese workers (BMI ≥ 30) representing almost two-fifths of the sample (39%), overweight employees (BMI 25 – 29.9) about a third (31%), and normal weight employees (BMI 18.5 – 24.9) slightly under a third.
On average, employees visited a doctor three to four times in the past year (Table 2). Visits to the ERs were less frequent (0.23 – 0.31 visits per employee), and hospitalizations were even less frequent (0.12 – 0.19 admissions per employee). These rates were similar to those found in national databases. For example, the Medical Expenditures Panel Survey (MEPS) reports 3.1 annual per capita doctor visit rates in 2006 for 18–64 years olds with private insurance, compared to our rates of 3.0–3.9; annual visits to the ER as 0.15, compared to 0.2–0.3 reported here, but there is a known underreporting of MEPS ER visit rates; and 0.08 inpatient admission rates compared to 0.12–0.19 found in our analysis.
Table 2.
Average yearly values and standard deviations for each outcome in 2006 (n=10,026).
| BMI (Normal) (n=3,012) | BMI (Overweight) (n=3,180) | p-value* | BMI (Obese) (n=3,834) | p-value* | ||||
|---|---|---|---|---|---|---|---|---|
| Outcome | Mean | S.D. | Mean | S.D. | Mean | S.D. | ||
| Doctor Visits | 3.05 | 4.23 | 2.95 | 3.90 | 0.285 | 3.93 | 7.44 | <.001 |
| Emergency Room Visits | 0.23 | 0.56 | 0.23 | 0.52 | 0.921 | 0.31 | 0.66 | <.001 |
| Hospital Inpatient Admissions | 0.12 | 0.42 | 0.15 | 0.75 | 0.055 | 0.19 | 0.6 | <.001 |
| Absenteeism (Days Absent per year) | 3.98 | 11.03 | 4.30 | 11.79 | 0.193 | 6.05 | 14.97 | <.001 |
| Presenteeism (Proportion productivity lost per year) | 0.018 | 0.029 | 0.020 | 0.031 | 0.037 | 0.019 | 0.032 | 0.025 |
Compared to normal employees using a Wilcoxon Rank Sum test.
In our MarketScan Commercial Claims Database for 2008, we report mean doctor office visits as 3.6, ER visits as 0.3, and hospital admission rates as 0.06. Thus, the one category where our sample may be reporting higher utilization rates is in the area of hospital admissions, but the differences in rates between our sample and other normative groups are not large.
As for productivity measures, employees were absent from work four to six days per year and their presenteeism losses were under 2%. Based on unadjusted data (i.e., prior to conducting the regression analyses), obese employees were associated with higher rates of doctor visits, emergency room visits, inpatient admissions, and absenteeism (all p <0.01) when compared to their normal weight counterparts. Obese employees also reported higher rates of presenteeism than normal weight employees (p < 0.05). On the other hand, outcomes for overweight employees (doctor visits, emergency room visits, inpatient admissions, absenteeism and presenteeism) were no different than those of normal weight employees.
After adjusting for covariates in the multivariate models (Table 3), obese employees had 20% higher doctor visits and 26% higher emergency room visits than normal weight employees. Rates of doctor visits and emergency room visits for overweight employees were no different than those of normal weight employees. Compared to normal weight employees, presenteeism rates for overweight employees were 10% higher and for obese employees they were 12% higher (p < 0.01).
Table 3.
Multivariate results for each outcome using a one or two part model, depending on the frequency of zeroes in the data (n=10,026).
| One Part Models | |||
|---|---|---|---|
| Outcome | Yearly Doctor Visits | Yearly Emergency Room Visits | Yearly Presenteeism |
| Model | Negative Binomial | Poisson | Log-Gamma |
| Coefficient Estimates (reference = Normal) | Count Model | ||
| Overweight | −0.012 | 0.035 | 0.101*** |
| Obese | 0.202*** | 0.260*** | 0.119*** |
| Two Part Models | |||
| Outcome | Yearly Hospital Admissions | Yearly Absenteeism | |
| Sample Size | |||
| Model | 2 part Zero-Inflated Poisson | 2 part Zero-Inflated Poisson | |
| Coefficient Estimates (reference = Normal) | Always-Zero Model | ||
| Overweight | 0.240 | −0.149** | |
| Obese | −0.411* | −0.371*** | |
| Coefficient Estimates (reference = Normal) | Count Model | ||
| Overweight | 0.315 | 0.003 | |
| Obese | 0.011 | 0.147*** | |
p<0.05,
p<0.01,
p<0.001
Obese employees were more likely to be hospitalized than normal weight employees, as indicated by the negative coefficient on the first part of the ZIP models (coefficient = −0.411 p < 0.01) (the “always zero” part, indicating a lower likelihood of zero absences), but once hospitalized, the number of separate hospitalizations was no different from normal weight employees. For overweight employees, the likelihood of ever being admitted to the hospital and the number of admissions for those who were admitted did not differ from utilization patterns for normal weight individuals.
Both overweight and obese employees were more likely to have been absent from work than normal weight employees, as indicated by the negative coefficient on the first part of the ZIP models (coefficient = −0.149, p < 0.01 overweight; −0.371, p < 0.01 obese). In the second part of the model, the number of days absent for obese employees was 14.7% higher than normal weight employees (p<0.01), but absent days for overweight employees were no different than normal weight employees.
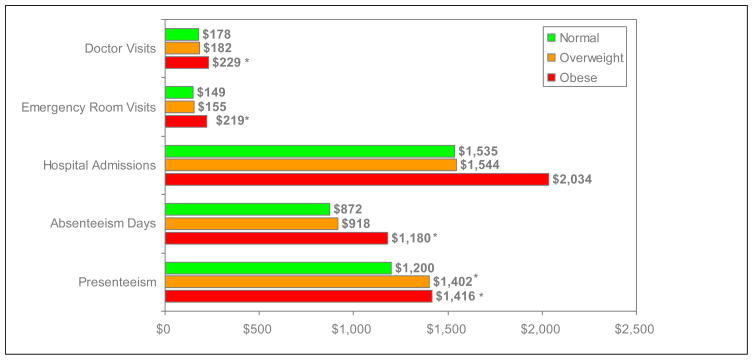
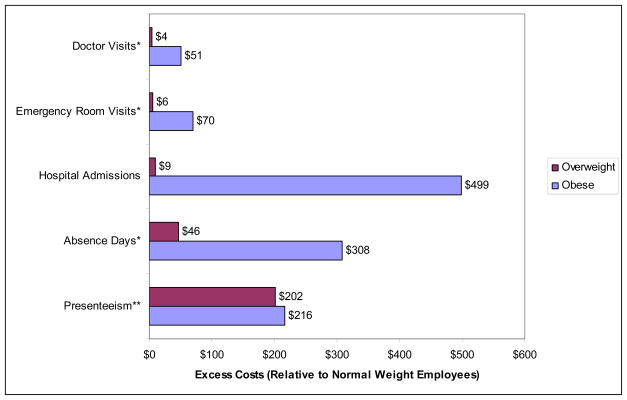
After adjusting for covariates, converting the model estimates to predicted values for each of the outcomes and converting these predicted values into dollar equivalents, we calculated that obese employees had significantly higher costs for all outcomes except inpatient admissions. For doctor visits, spending for obese employees averaged $229 per year compared to $178 for normal weight employees, resulting in excess costs of $51 per obese employee per year. ER visits resulted in excess spending of nearly $70 per obese employee per year. Notably, higher rates of absence resulted in $308 of excess spending for obese employees, and annual presenteeism costs were $215 higher. Spending for overweight employees was not statistically different than for normal weight employees for all outcomes except presenteeism, where costs were $201 higher.
Taken together, obese employees were estimated to cost employers $644 more in 2006 dollars across categories where statistically significant differences were found when compared to normal weight workers (i.e., doctor visits [$51] + ER visits [$70] + absenteeism [$308] + presenteeism [$215] = $644). For overweight employees, the only category found to produce excess costs was presenteeism ($201 per employee per year).
DISCUSSION
This study analyzed self-reported healthcare utilization and productivity measures for over 10,000 workers in different professions, across multiple employers in various regions of the country. Our aim was to estimate the excess costs imposed on employers associated with overweight or obese workers, compared to normal weight workers.
As expected, we found that obese employees experienced significantly greater rates of doctor visits, ER visits, hospitalizations, absenteeism, and presenteeism than normal weight employees. Unlike other studies, we quantified the relative financial impact of excess weight on five different measures of healthcare utilization and productivity. Notably, the magnitude of obesity-related spending for absenteeism and presenteeism ($2,596 per employee per year in 2006 dollars) was roughly equivalent to spending for doctor visits, ER visits, and hospitalizations ($2,482) (Figure 1).
Figure 1. Estimated Annual Costs of Healthcare Utilization, Absenteeism, and Presenteeism by BMI Category.
* p<0.05
Note: Differences between the values presented in the figure and text are due to rounding.
However, when considering only those categories that were significantly higher, excess indirect costs for obese workers were almost five times greater than excess direct costs ($524 in excess costs related to productivity losses compared to almost $121 in excess costs associated with more doctor and ER visits for obese employees), thus demonstrating the importance of including productivity measures in estimates of the total financial burden of obesity to employers.
While excess per employee per year costs may seem modest (approximately $644 per obese employee), within this sample these costs totaled nearly $2.47 million ($644 multiplied by the 3,834 obese employees). Taken in aggregate, these additional costs represent a large financial burden borne by employers who may be motivated to institute effective obesity management programs that improve workers’ health and may save their organization some portion of these excess costs. To benefit financially from such programs, employers in our sample would have had to spend less than that amount on weight management programs.
It should be noted that some portion of excess costs attributable to obesity may ultimately be passed onto employees as well. While employers pay 83% of the premium costs for single coverage and 73% of the premium costs for a family, employees pay the balance and their contributions to premiums have increased by 128% between 1999 and 2009 (35). Similarly, absenteeism and presenteeism costs are not only borne by employers. Economic theory suggests that workers in a competitive labor market are paid commensurate to the value of their marginal contribution to the firm, so if obese people are less productive, they may be paid less than their normal weight counterparts.
Our results parallel those of previous investigations examining the relationship between BMI and medical care and productivity costs. Findings from this study are similar to those reported by Durden et al., who found that overweight individuals’ overall healthcare utilization patterns were comparable to normal weight employees (16). Durden et al. also observed that obese and overweight employees had more absences than the normal weight employees. They calculated similar excess direct costs for obese employees ($712) as did we ($620).
However, it should be noted that the two studies were different in their design, data sources, and calculations of excess costs. For example, Durden et al.’s estimates of healthcare spending included employer and employee payment amounts and pharmaceutical expenditures. Our study only included healthcare costs borne by the employer and not pharmaceutical costs. Further, their study relied on self-reported BMI measures while we used professionally collected biometric data related to height and weight.
Our findings corroborate previous studies that found the effects of excess weight on direct and indirect costs are most evident among obese employees (7), (8), (9), (10), (16), (36). In our study, overweight was not associated with higher direct medical utilization and spending but was associated with productivity losses. Studies remain mixed on the effects of being overweight on productivity outcomes. Other studies have found that while overweight may not have a financial impact on more overt health-related financial measures it does have a financial impact on the day-to-day performance of workers (15), (14). Presenteeism is often more difficult to quantify than absent days or costs associated with healthcare use due to illness. However, the costs associated with presenteeism among overweight employees in our study were still substantial, given that approximately one-third of the workforce in the sample was overweight. Some studies based on self-reported height and weight may underestimate the prevalence of overweight and obesity, as height may be overestimated and weight underestimated (37), (38). Because evidence remains unclear, further study of the effects of overweight on health and productivity are warranted.
A strength of this study is the use of biometric measures of weight and height, compared to previous studies that have relied on self-reported data, thus resulting in more accurate findings (37). Known biases in self-report, particularly social desirability bias, for example, were therefore avoided (37),(38). This study has several limitations. First, while BMI is not a perfect measure of excess weight,(11) a recent review found that BMI and measures of overfat and adiposity are highly correlated indicating that for large-scale population studies BMI is an adequate and practical measure of overweight and obesity (39).
Second, the cross-sectional study design could also present a limitation, as differences in utilization, absenteeism, and presenteeism between employees in various BMI categories were assessed at a single point in time rather than longitudinally over longer time periods. Future studies need to prospectively determine the impact of change in weight over time, including weight gain and weight loss on health care utilization and productivity outcomes.
Third, while a large and geographically diverse sample was analyzed, results may not be generalizable to employee groups dissimilar to this sample.
Fourth, our analysis likely presents conservative estimates of the cost burden to employers of overweight and obesity among workers. Our study relied upon self-reported healthcare utilization, absenteeism, and presenteeism which are often subject to recall bias. Short et al. showed that self-reported healthcare utilization and absenteeism can serve as a proxy for administrative data. Respondents to surveys were able to accurately report the number of emergency room visits and inpatient hospital admissions over the past year but only 30% and 37% could accurately recall the number of doctor visits and absent days, respectively, in the previous 12 months (18). For those with inaccurate recall, the majority under-reported their utilization, reporting fewer visits or days compared to administrative data. Given these findings, self-reported absent days and doctor visits in this study are likely underestimated, making our results more conservative.
Further, the accuracy of the self-reported data may be affected by respondents’ BMI values. In the Short et al. study, individuals classified as overweight or obese were less likely to accurately remember the number of annual doctor visits, annual inpatient hospital admissions, and annual absence days they experience (18). This was probably because these individuals had more encounters with the health care system and were absent more frequently than normal weight respondents.
A fifth limitation is that this study also did not include pharmacy spending, which could impact the cost estimates, as excess weight is associated with a myriad of chronic health conditions that often require maintenance medication.
Finally, productivity costs were estimated using Bureau of Labor Statistics (BLS) average wage estimates; however, two-thirds of the sample was employed in managerial/professional positions. Thus, our productivity-related losses estimates may be underestimated.
CONCLUSION
We estimated the financial burden that obesity, and to a lesser extent, overweight, place on businesses in the U.S. by measuring these health risks across industries and occupations. To address the health and economic impacts of overweight and obesity among workers, employers are encouraged to implement evidence-based obesity management programs aimed at improving the health and well-being of employees. Future research should build upon our work to examine the relationship between classes of obesity and costs borne by employers, as well as the differential effects on costs across various demographic groups.
Figure 2. Estimated Excess Annual Medical and Productivity Costs Relative to Normal Weight Employees.
*Significant for obese employees at p<0.05
**Significant for overweight and obese employees at p<0.05
References
- 1.National Center for Health Statistics. Prevalence of Overweight and Obesity Among Adults: United States, 2003–2004. 2004. [Google Scholar]
- 2.Centers for Disease Control and Prevention. State-Specific Prevalence of Obesity Among Adults--United States, 2005. Morbidity and Mortality Weekly Report. 2006;55:985–988. [PubMed] [Google Scholar]
- 3.Gregg EW, Cheng YJ, Cadwell BL, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. J Amer Med Assoc. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 4.Calle E, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 5.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28:w822–831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Contributing Factors. Overweight and Obesity:An Overview. 2008 [Google Scholar]
- 7.Wang F, McDonald T, Bender J, Reffitt B. Association of Healthcare Costs with Per Unit Body Mass Index Increase. J Occup Environ Med. 2006;158:466–472. doi: 10.1097/01.jom.0000225045.77734.f4. [DOI] [PubMed] [Google Scholar]
- 8.Arterburn DE, Maciejewski ML, Tsevat J. Impact of morbid obesity on medical expenditures in adults. Int J Obes (Lond) 2005;29:334–339. doi: 10.1038/sj.ijo.0802896. [DOI] [PubMed] [Google Scholar]
- 9.Raebel MA, Malone DC, Conner DA, Xu S, Porter JA, Lanty FA. Health services use and health care costs of obese and nonobese individuals. Arch Intern Med. 2004;164:2135–2140. doi: 10.1001/archinte.164.19.2135. [DOI] [PubMed] [Google Scholar]
- 10.Quesenberry CP, Jr, Caan B, Jacobson A. Obesity, health services use, and health care costs among members of a health maintenance organization. Arch Intern Med. 1998;158:466–472. doi: 10.1001/archinte.158.5.466. [DOI] [PubMed] [Google Scholar]
- 11.Cawley J, Rizzo JA, Haas K. Occupation-specific absenteeism costs associated with obesity and morbid obesity. J Occup Environ Med. 2007;49:1317–1324. doi: 10.1097/JOM.0b013e31815b56a0. [DOI] [PubMed] [Google Scholar]
- 12.Bungum T, Satterwhite M, Jackson AW, Morrow JR., Jr The relationship of body mass index, medical costs, and job absenteeism. Am J Health Behav. 2003;27:456–462. doi: 10.5993/ajhb.27.4.17. [DOI] [PubMed] [Google Scholar]
- 13.Ricci JA, Chee E. Lost productive time associated with excess weight in the U.S. workforce. J Occup Environ Med. 2005;47:1227–1234. doi: 10.1097/01.jom.0000184871.20901.c3. [DOI] [PubMed] [Google Scholar]
- 14.Gates DM, Succop P, Brehm BJ, Gillespie GL, Sommers BD. Obesity and presenteeism: the impact of body mass index on workplace productivity. J Occup Environ Med. 2008;50:39–45. doi: 10.1097/JOM.0b013e31815d8db2. [DOI] [PubMed] [Google Scholar]
- 15.Goetzel RZ, Guindon AM, Turshen IJ, Ozminkowski RJ. Health and productivity management: establishing key performance measures, benchmarks, and best practices. J Occup Environ Med. 2001;43:10–17. doi: 10.1097/00043764-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Durden ED, Huse D, Ben-Joseph R, Chu BC. Economic costs of obesity to self-insured employers. J Occup Environ Med. 2008;50:991–997. doi: 10.1097/JOM.0b013e318182f730. [DOI] [PubMed] [Google Scholar]
- 17.Pratt CA, Lemon SC, Fernandez ID, et al. Design Characteristics of Worksite Environmental Interventions for Obesity Prevention. Obesity. 2007;15:2171–2180. doi: 10.1038/oby.2007.258. [DOI] [PubMed] [Google Scholar]
- 18.Short ME, Goetzel RZ, Pei X, et al. How Accurate are Self-Reports? Analysis of Self-Reported Health Care Utilization and Absence when Compared with Administrative Data. J Occup Environ Med. 2009;51:786–796. doi: 10.1097/JOM.0b013e3181a86671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lerner D, Amick IBC, Rogeres WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Med Care. 2001;39:72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Lerner D, Reed JI, Massarotti E, Wester LM, Burke TA. The Work Limitations Questionnaire’s validity and reliability among patients with osteoarthritis. J Clin Epidemiol. 2002;55:197–208. doi: 10.1016/s0895-4356(01)00424-3. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. About BMI for Adults. 2008. [Google Scholar]
- 22.Agency for Healthcare Research and Quality. What’s New from the USPSTF. 2003. Screening for Obesity in Adults. [Google Scholar]
- 23.Bertakis KD, Azari R. The Influence of Obesity, Alcohol Abuse and Smoking on Utilization of Health Care Services. Fam Med. 2006;38:427–434. [PubMed] [Google Scholar]
- 24.Park R. Estimation with heteroskedastic error terms. Econometrica. 1966;34:88. [Google Scholar]
- 25.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 26.Dunn G, Mirandola M, Amaddeo F, Tansella M. Describing, explaining or predicting mental health care costs: a guide to regression models. Methodological review. Br J Psychiatry. 2003;183:398–404. doi: 10.1192/bjp.183.5.398. [DOI] [PubMed] [Google Scholar]
- 27.Bao Y. Predicting the Use of Outpatient Mental Health Services. Do Modeling Approaches Make a Difference? Inquiry. 2002;39:168–183. doi: 10.5034/inquiryjrnl_39.2.168. [DOI] [PubMed] [Google Scholar]
- 28.Lambert D. Zero-Inflated Poisson Regression with an Application to Defects in Manufacturing. Technometrics. 1992;34:1–14. [Google Scholar]
- 29.Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. New York: Oxford University Press; 2007. [Google Scholar]
- 30.Little RJA, Rubin DB. Statistical Analysis of Missing Data. New York: Wiley and Sons; 2002. [Google Scholar]
- 31.Allison PD. Missing Data. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 32.Bureau of Labor Statistics. Employer Costs for Employee Compensation--December 2006. United States Department of Labor; Washington: 2007. p. 11. [Google Scholar]
- 33.Ariyanayagam-Baksh SM, Baksh FK, Swalsky PA, Finkelstein SD. Loss of heterozygosity in the MXI1 gene is a frequent occurrence in melanoma. Mod Pathol. 2003;16:992–995. doi: 10.1097/01.MP.0000087421.44975.1C. [DOI] [PubMed] [Google Scholar]
- 34.Mullan B, Snyder M, Lindgren B, Finkelstein SM, Hertz MI. Home monitoring for lung transplant candidates. Prog Transplant. 2003;13:176–182. doi: 10.1177/152692480301300303. [DOI] [PubMed] [Google Scholar]
- 35.The Kaiser Family Foundation and Health Research & Educational Trust. The Kaiser Family Foundation and Health Research & Educational Trust. 2009. Employer Health Benefits: 2009 Summary of Findings; pp. 1–8. [Google Scholar]
- 36.Ricci JA, Chee E. Lost Productive Time Associated with Excess Weight in the U.S. Workforce. J Occup Environ Med. 2005;47:1227–1234. doi: 10.1097/01.jom.0000184871.20901.c3. [DOI] [PubMed] [Google Scholar]
- 37.Rowland M. Self-reported weight and height. American Journal of Clinical Nutrition. 1990;52:1125–1133. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- 38.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. quiz 35-26. [DOI] [PubMed] [Google Scholar]
- 39.Bouchard C. BMI, fat mass, abdominal adiposy and visceral fat: where is the ‘beef’? Int J Obes (Lond) 2007;31:1552–1553. doi: 10.1038/sj.ijo.0803653. [DOI] [PubMed] [Google Scholar]